where you see * you can click to the hyperlink to bring you to the original website source of the direct quote.
I was recently reminded of a debacle under a Labour government in 2006 which the Guardian reported as follows*:
“A secret plan to privatise an entire tier of the NHS in England was revealed prematurely yesterday when the Department of Health asked multinational firms to manage services worth up to £64bn.
The department’s commercial directorate placed an advertisement in the EU official journal inviting companies to begin “a competitive dialogue” about how they could take over the purchasing of healthcare for millions of NHS patients. …
The advertisement asked firms to show how they could benefit patients if they took over responsibility for buying healthcare from NHS hospitals, private clinics and charities. The plan would give private firms responsibility for deciding which treatments and services would be made available to patients – and whether NHS or private hospitals would provide them.” (The Guardian)
“How to create money” in the NHS has always been one about denigrating the views of its professional social capital, and thinking about ways of maximising income.
As we approach the ‘E day’, May 7th 2015, when we know that the UK will go to the polls, it is useful to consider now the end-game of NHS privatisation.
False reassurances have been a-plenty.
Privatisation, when you apply common sense, is simply diversion of resources into the private sector from the public sector. Outsourcing (enacted through section 75 Health and Social Care Act (2012) and its regulations) is a key part of that.
But it’s not the full story. You’d have to be a complete idiot to wish to maintain that the NHS is not being privatised.
Some people, it seems, are prepared to perform that rôle.
The end-game
Nearly a year ago, before the section 75 regulations had been discussed in parliament, I introduced here how this somewhat ignored clause would fix the NHS into a competitive market.
I wrote a blogpost on the predictable trajectory of the NHS privatisation which clearly argues that this had started with shifts in policy from the Thatcher and Major governments.
If you want to understand the model, it’s worth tracking it back to the horses’ mouths: Conservative MPs Mr John Redwood and Dr Oliver Letwin.
In a now seminal article, “Opening the oyster: the 2010-1 NHS reforms in England” by academics Dr Lucy Reynolds and Prof Martin McKee for the Journal of the Royal College of Physicians of London (2012), known as “Clinical medicine”, the background to this journey to full privatisation is laid bare [Clin Med, April 1, 2012 vol 12 no 2, pp. 128-132.]
Reynolds and McKee argue in their conclusion*:
“Enthoven’s description of the HMO model, which he explicitly stated was at least as problematic but more expensive than the NHS, has somehow been adopted as a blueprint for the privatisation of the NHS. It was recently reported that the newer ‘accountable care model’ now finds favour with the secretary of state for health. This flexible model is a successor to the HMO model, although it is not greatly different in concept or operation. It involves a managed care arrangement in which the private sector primary care gatekeeper receives a subsidy from the government to pay all or part of the individual premiums due for the people registered with it, with the individuals concerned expected to pay any shortfall between the personal budgets provided by government and the amount charged by the accountable care organisation.
… Fulfilment of the longstanding ambition, documented by Redwood and Letwin, to expand private financing of the healthcare system through user contributions is thus now imminent. Enthoven’s reasoned view that market-based healthcare provision is more expensive and less universal than the NHS system consistently has been overlooked. …” (Reynolds and McKee, 2012)
“Commissioning support units” are for the time-being part of the new NHS landscape. Here they are discussed by Veronika Thiel on the King’s Fund website (linking to an article in the HSJ)*:
“Commissioning support units are set to take on important functions in the new NHS structure. They will support clinical commissioning groups by providing business intelligence, health and clinical procurement services, as well as back-office administrative functions, including contract management.” (Thiel, King’s Fund website)
The immediate future steps are something like this:
1. CSUs spun off as private entities, to private equity firms.
2. CSUs provide support to CCGs.
3. CCGs commission services from providers.
4. Each of us given a voucher worth what it is predicted we will cost.
5. We then exercise our choice to find an option that meets our expectations.
6. If the value of our voucher is insufficient, we top it up ourselves.
7. There’s some safety net for the very poor perhaps (and there’s a bit of lee-way here for anti-immigration politics).
8. CCGs compete with each other.
Commissioning support units and private equity
Roy Lilley, a health commentator, only this week reported on the big problem with the CSUs in an article entitled “Trojan Horse”*:
“The DH has a problem. By 2016 CSUs have to be off the NHS’s books as their grace period as chaperoned NHSE organisations comes to an end. They could be taken over and run by their staff, as a social enterprise or the private sector encouraged to buy-in. The usual suspects, Capita, Serco, Atos, and McKinsey are having a look. KPMG are not. …
Will they make money? Not now, not next year, but assuming there is no political upheaval in 2015, CSUs, as a long term punt, with payback measured in years not months might make them Primary Care’s Trojan Horse.” (Roy Lilley)
On 3 November 2013, the Financial Times had reported the following*:
“The NHS has approached private equity companies about taking over organisations that help buy billions of pounds of services for hospitals and GPs. The talks focus on the 19 commissioning support units (CSUs) set up last year to provide services to the new doctor-led commissioning groups that spend more than two-thirds of the NHS budget. …
CSUs were created as part of contentious healthcare reforms pushed through by the coalition government last year in the teeth of fierce opposition from Labour and much of the medical profession. Although the turnover of the 19 units range from just £21m to £62m a year, together they employ nearly 9,000 staff, designing health services and providing back office IT, procurement and payroll services to clinical commissioning groups. While the CSUs are subsidised by the NHS, they are expected to become self-sufficient profitmaking businesses or form joint ventures with the public or private sectors by 2016.” (Financial Times)
The public’s lack of appetite for privatisation
The public generally think that all privatisations work with a lot of publicity like the BT or Royal Mail one. Where ‘word-of-mouth advertising’ has usually effective (e.g. “Tell Sid”), campaigns anti-NHS privatisation can all too easily go viral (pooled efforts of NHS activists on the section 75 regulations, which saw withdrawal of the original statutory instrument.)
The situation of the ongoing NHS privatisation, across a number of successive UK administrations, is fundamentally different, as in this case the whole project can only work if the public do not realise that they are being duped. Many organisations, politicians, and other leaders can rightly share the blame for not been truthful about the situation. What in fact is most incredible that the process of privatisation of the NHS has been so vehemently denied by politicians and think-tanks, when it is all so incredibly blatant.
There are still a few ‘barriers’ to the ultimate end described below, but these are not impossible for the ‘privateers’ given the right environment.
These include the election of a government which can implement the final steps (this could be any of the main political parties based on their past performance), a NHS IT system ‘fit for purpose’, a method of allocating funds for CCGs depending on individuals’ contributions, a method for allowing top-up payments, to name but a few. However the privateers will be encouraged by the privatisation ‘progress’ which has been made in the last few years.
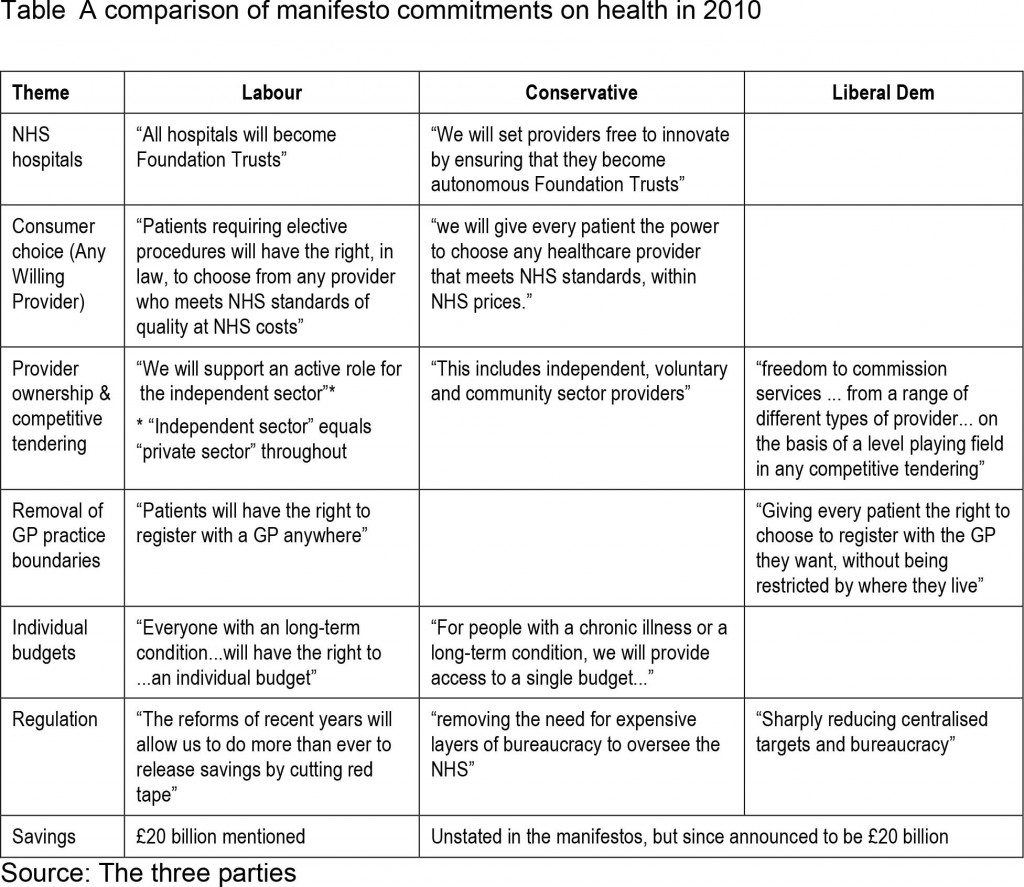
Appetite for privatisation had failed to increase prior to the last election, despite little manoeuvres like the NHS logo available to private companies to make it hard for patients to distinguish between services provided by them and the NHS proper; and permitting private hospitals to compete to sell whichever procedures they wish to offer. With all three main major political parties having converged on the market, there was barely a cigarette paper’s difference between these parties from which to choose.
Arguably, however, it would be quite unfair to blame unilaterally the UK Labour Party with the benefit of hindsight. Labour remain adamant that they would never have enacted a statutory instrument such as the Health and Social Care Act (2012). There is no indication that Labour had intended to publish a similar Act from Hansard. Furthermore, they did consistently fight tooth-and-nail against the Act in the lower House and the House of Lords.
Clinical-based commissioning
Doctors have been sold a bit of a pup, but the media and politicians were adamant that GPs would have a greater rôle in commissioning.
A starting point for understanding the relevance of commissioning to the privatised NHS is the famous Adam Smith Institute’s Pirie and Butler document, which includes a description of their proposed final phase of a switch from a classic NHS to a US-style system. Madsen Pirie and Eamonn Butler are the well known free market gurus at the Adam-Smith Institute. Their entire document reads like a promotion glossy for privatisation, completely bereft of evidence-based academic references.
The end point is a US-style health maintenance organisation (HMO).
The problem of starting new system such as Health Maintenance Organisations is largely avoided by keeping patients with their present GP. In theory, the resources go to the CCG selected by the doctor, although the ultimate choice lies with the patient, who can change CCG by going to a doctor registered with another one. The resources are thus supposed to be directed to the CCGs which are most favoured by doctors and patients.
Nonetheless, it is the CCG who holds the power. As such, CCGs don’t need to have any medical expertise.
Even a Tory MP, Dr Sarah Wollaston, has drawn attention* to how CCGs appear to have gone ‘gun-ho‘ in privatising when David Bennett from Monitor had not felt such a need:
“The existing guidance is widely ignored. David Bennet (sic), the Chief Executive of the regulator Monitor, has set out in a number of settings that commissioners are putting too many services out to tender and yet the waste of resources continues. Perhaps because no commissioners have the spare cash to fight a legal challenge themselves.” (Dr Sarah Wollaston’s blog)
That is why this from Earl Howe is pure ‘smoke and mirrors’ from when the section 75 Regulations were being discussed (shared by Clive Peedell of the National Health Action Party):
Resource allocation and “vouchers”
There are various accounts of how resource allocation works in the NHS, and indeed one of the challenges of understanding NHS privatisation is understanding new parts of the puzzle as they fall into place. NHS England, as Baumann offered in his Health Select Committee evidence this week, will be describing yet another configuration of this formula in December which is apparently going to factor in inequality as well.
In this model, each individual would receive from the state a health voucher, equivalent in value to what he or she approximately is currently ‘consuming’. Making the maths work is of course made a lot easier if the allotted budgets have already been worked out through implementation of ‘personal health budgets‘.
The voucher can be used towards the purchase of private health insurance or exchanged for treatment within the public sector health system. This can easily be sold on the basis of ‘equity’ – that each person has equal access to a ‘National Health Service’ – whereas people actually have access to an inter-tradeable insurance scheme.
Those who opt into private insurance can use the voucher to pay their premiums, and the insurance companies then collect the cash value of the “voucher” from the government. This is the most odd aspect of the model, but easy if you understand the apparent ease with which successive Conservative governments have effectively provided state benefits for their private sector colleagues (see recent outsourcing debacles across a number of sectors.)
The issue of co-payments had been kicked into the long grass.
Sir David Nicholson gave a further reassurance recently (irony klaxon) that it was unlikely that such payments would be introduced imminently on a BBC Radio 4 discussion programme called “Costing the NHS“.
People who decide that health care is particularly important to them are free to add to the amount covered by the voucher and thus purchase more expensive forms of insurance, perhaps covering more unlikely risks or providing superior standards of comfort or convenience.
This is where the right-wing are able to allow for the fact that people who want to pay more can. People on the centre and left, however, interpret this as producing potentially a ‘two tier system’. It is currently not that difficult to find stories of how inadequate the US Medicaid services are currently, and it is a national disgrace of theirs that there are some citizens who are too poor or too ill to be able to afford an insurance-based healthcare.
The voucher would not force people into private insurance, although it certainly makes the option of going private instantly available to everyone. Those who want to use the state service will continue to receive it, their voucher being their ticket to free treatment just as their national insurance number is at the moment.
The distinction between a public health service which does what it can on a take-it-or-leave-it basis, and a private system for the rich which offers choice and competition begins to overlap.
The demise of the CCGs
“Integration” is the standard weapon in the war of words which tries to legitimise the smuggling of the US health insurance industry into running the NHS. The insurance/voucher system fits snugly into such “integration” (or even “whole person care”), and could see one arm of the system (e.g. “universal credit”) enmeshing with another (e.g. “personal health budgets”) for whole person care. This is of course is hugely dangerous without the proper safeguards. Successsive governments have tried so hard to shore up the NHS IT system, under various pretences such as “the paperless NHS”, precisely for this purpose.
A possible relationship between universal credit and whole person credit was mooted here in the mysteriously insightful article by Jennie Macklin and Liam Byrne.
Why are MasterCard so keen on working on payment mechanisms? This article explores possibly why.
The public sector CCGs, taking responsibility for total health care of NHS patients, are not too far removed in structure from private insurance and management bodies. The funds for premiums are publicly provided, but the same competition and incentives operate, and the same choices are made available. Experience, however, from the US is that it is difficult for a patient to sue a CCG directly if a problem arises.
So the Clinical Commissioning Group (CCG) still remains a favourite means of achieving the NHS privatisation ‘end game’. The CCG format simply lays the groundwork and the basis for further changes at a later stage.
One of the first things to happen is that CCGs receive their population-based allowances. Whilst it is likely that this will be done on an incremental basis from what the current allocations might be, as CCGs become more sophisticated, they might make use of other techniques such as ‘the dementia prevalence calculator‘ which appears to have achieved somewhat of a pedestal status in dementia public health.
Another trick in the ‘registration process’ is hoping that some members of the public never register and so never receive their allowance. This is known to be a trick of the Department of Work and Pensions which have often failed to notify benefit claimants that their welfare benefits have come to an end.
CCGs might become themselves sitting ducks for becoming insolvent.
The Department of Health will have to conjure up increasingly imaginative methods of arranging CCG funding sharing so as to not make them look like cuts (and find a mouthpiece to publicise them).
A final change of direction for the NHS hoped by some?
Nick Seddon has recently been reported to have caused some controversy by proposing NHS cuts and GP charges. He of course has been the Deputy Director of the think-tank Reform. In 2008, published during the time of a Labour government, Reform produced a pamphlet entitled, “Making the NHS the best insurance policy in the world “.
Their “top recommendations” included the following*:
“These incentives could be introduced by changing the National Health Service to a National Health Protection System. Taxpayer funding and guaranteed access would continue, but individuals would be empowered to decide which approved Health Protection Provider to use. Custody of individual health outcomes would be made independent; it would no longer be in the hands of politicians.
This would mean the following for individuals:
- A “healthcare protection premium” of £2,000 per year would be paid out of general taxation, equivalent to the current NHS cost per individual in England. NB this is similar to the cost of health insurance in France and the Netherlands.
- A choice of where to spend the health protection premium, between Health Protection Providers (HPPs). Coverage for a wide, core level of health treatment, including all essential operations and treatments.
- Extra services, such as gym membership, and rebates for healthy living, for example smoking cessation, offered by HPPs to attract customers.
- Regulation of HPPs by government to ensure they reach minimum standards.
- The ability to top-up their premium to have extra services such as certain drugs, cosmetic surgery or better accommodation in hospitals. People in the UK already value their healthcare enough to spend £1,600 per family per year on health and fitness.The current Departmental review of top-up payments for cancer drugs and the draft EU Directive on cross-border healthcare are likely to lead to greater clarity over what individuals are entitled to and to a new market in insurance for top-up payments.
- Guaranteed accident and emergency cover through a general agreement with insurers, on the model of the Dutch compulsory insurance system.
Because of the positive developments in the UK, this is a task of evolution rather than revolution which could be complete in three to five years. The key steps would be turning Primary Care Trusts (PCTs) into Health Protection Providers; allowing other insurers to join the system; and defining the core entitlement to healthcare.
In January 2008 the Prime Minister described the NHS as “the best insurance policy in the world”. That is the right idea. It means radical change, to combine universal coverage with the focus on the patient evident in other countries. Success would see the UK rejoin the top rank of international health systems and become again the envy of the world.” (Reform Report, 2008)
I remember when I was once in a cab in London, and the cabbie was telling me how, for some private care his wife had received, the insurer had refused to pay for certain aspects of after-care. This is somewhat reminiscent for me of the following criticism made by Reynolds and McKee (2012) in relation to the Reform report*:
“This plan is alluded to in the 2010 white paper in the opaque phrase ‘money will follow the patient’. This refers to the impending roll-out of personal health budgets for all those registered with the NHS. These have been greeted with enthusiasm by patient groups, somewhat strangely when one considers that the NHS currently undertakes to cover all costs of care, whereas the concept of a finite budget implies that it is possible that the actual costs of care could exceed that budget, leaving the patient to cover the excess.” (Reynolds and McKee, 2012)
Andy Burnham MP: “I admit it – we let the market in too far”
Andy Burnham MP is reported on June 9th 2013 as saying the following*:
“When Shadow health lead Andy Burnham MP visited Lewisham the previous evening, he began his speech:
“I admit it – we let the market in too far and now on the 65th anniversary of the NHS we need to renew our commitment to Bevan’s NHS: public service over privatisation; collaboration over competition and people’s wellbeing before self-interested profit.”” (“Left Foot Forward” blog)
This was an important statement to have made.
And Burnham is reported in the same article as wishing to put a stop to the neoliberal firestorm of hospital reconfigurations:
“Later in the day Burnham left his Lewisham audience in no doubt as to his feelings and his intention :
“I give my full support and backing to Lewisham Hospital. 25,000 people marching through the streets is a remarkable achievement. We support the campaign.””
Conclusion
It’s all fairly predictable.
Or so it might appear. You could mount an argument that the present system is far better (having “liberalised” the NHS with non-NHS providers) than having an insurance-based system.
Indeed, indeed Andrew Lansley, the former Secretary of State for Health preceding Jeremy Hunt in the current government, claimed to be opposed to be against such a method of funding the NHS when the Bill was beginning to reach a climax in its discussions.
(see beginning of this video)
Aside from who exactly is in the market post 2015, whether it’s Andy Burnham MP’s “NHS preferred provider” or the Coalition’s “Any qualified provider”, it’s still of concern that there’s still a market. As a first step, Burnham in October 2012 asked for a block on the further ‘roll out’ of “any qualified provider”.
There’s no ‘conspiracy theory’ about it.
For anyone with a training in business and commercial or corporate law, it’s dead obvious.
If you wish to look at what we might be heading to, this overview of the ‘current problems’ of the US healthcare system is a good introduction.
‘Competition’ was used to crowbar the market in. Everyone knows that. People who aggressively pimped competition as a means of improving quality know exactly how faulty their reasoning was (see my previous blogpost). Unfortunately this has done massive damage to English health policy.
This video’s quite useful as it approaches some topics which will are likely to become inevitable for us in this jurisdiction, if we should decide to go down this route: what the process of transformation will cost, how the insurance packages are likely to have to be controlled, competition between CSUs and competition between CCGs in the private market (we know quite how successful competition has been in the energy market), what clinical services will still become out-of-scope, and so on.
The current ‘state of play’ is that Labour has stated categorically to repeal the Health and Social Care Act (2012) on many occasions. This is a determined attempt to ‘turn back the tide’ on NHS privatisation, which is a highly popular move amongst potential Labour voters.
Specifically, Labour wishes to put the stuff on competition in part 3 of the Act into reverse. Both Andy Burnham MP and Ed Miliband MP have stated their intention for this independently. Andy Burnham MP is reported as recently as 25 September 2013 as emphasising that he will end ‘fast track privatisation’.
A shift in emphasis from competition to collaboration will make it difficult to run the NHS as a market based on the rules of EU competition, with the correct adjustments in legislation from the Executive.
Many brilliant NHS activists have had landmark successes in opposing Government policy, too.
Never have the stakes been higher for the NHS with the election of the next UK Government, to take place during the course of May 8th 2015.
Try to talk to someone else about it to see what they think?





Pingback: NHS Privatisation: The end-game | SteveB's Poli...()
Pingback: NHS Privatisation: The end-game | Welfare, Disa...()
Pingback: The “official top 40″ of my most viewed articles on the SHA website this year()
Pingback: Report on SHA Web presence 2013()