Home » NHS
The lack of coherent strategy for the mental health of NHS employees in the 5YFV is a mess
It seems Simon Stevens and supporters are rallying around a need to form a consensus on what needs to be done about the NHS. After a period of traumatic disturbance, this might seem a laudable approach. And yet putting sticks in the sand, marking your territory, is not particularly helpful if you are unelected.
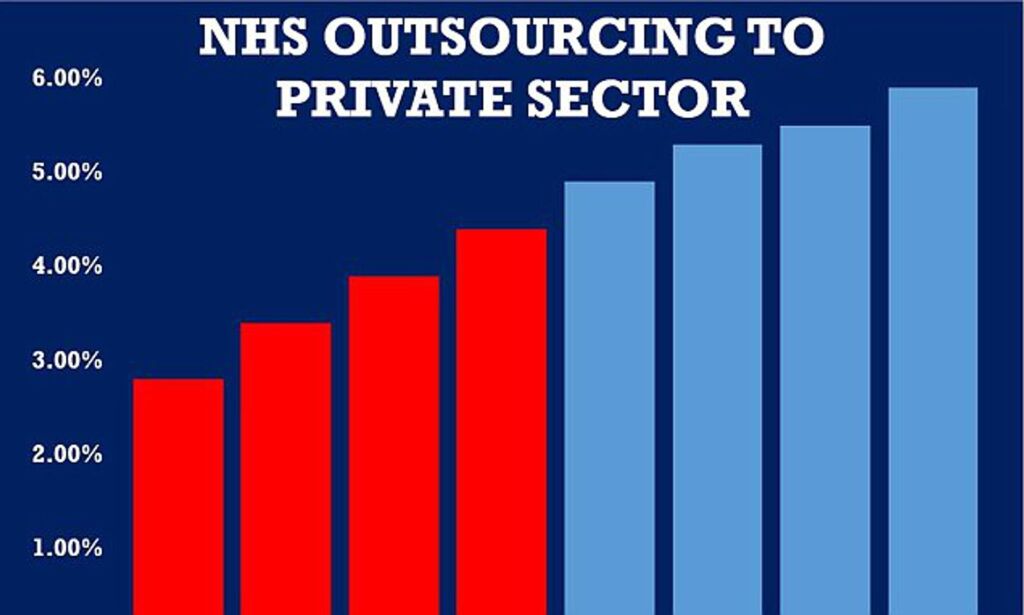
I dare say whichever party or parties come into office early this year, the issues about integrated care will have to be negotiated. I am less certain about how the NHS and social care are to be funded, in the absence of a clear debate about the extent to which social value bonds and private finance initiatives will continue. Whatever your take on the details of the 5 year forward view, it is hard to deny that the emphasis is managerial, with an emphasis on systems and processes.
A tweet which Phillip Blond, Director of ResPublica, once set one morning made me think about how non-centrist parties were the new “disruptive parties”. In other words, there’s been a reversal of roles. Whichever party can drag themselves away from the centre position to form a new settlement might scoop up.
There’s an element of nostalgia about where we have come from. It’s hard to deny the ‘feel good factor’ brought about by images such as this.
But the world we live in is a very different one.
I don’t think I’d particularly like to be graduate in the current environment, entering a world with poorer job security, having to pay off loans for university education, and so on.
And it’s a crying shame, that many of us have seen the NHS in this context.
It’s not a question of being hyperbolic about criticism. People in the communities which are referred to in the 5 year forward view are sick of their local hospitals (or A&E departments) shutting without warning in the name of reconfiguration.
I was personally aghast how little concern there is in the 5 year Forward View for the mental health of employees. I know from my own time working in busy district general hospitals and London teaching hospitals that the workload is incredibly stressful in acute medicine. None of this is helped by having low numbers of staff having to work at breakneck pace, while politicians and other hanger-ons talk about ‘compassion’. We know that the public have been recently ‘activated’ by the talk of tax evasion, and people buying influence in political parties. This discussion of greed and corruption seemed to have carved through the election morass as cleanly as a butter knife. While some people want low taxes, they simultaneously don’t want public services to be stripped of all funds. Social care has not been ring fenced since 2010, leaving a desperate situation with people not being discharged from hospital in a timely manner. But the need to fund social care is not simply about delayed discharges – social care is pivotal.
There’s absolutely no need to make the Secretary of State devoid of responsibility for the NHS, unless you literally only see the NHS as a fig leaf logo for other providers; or unless you see the role of Government to regulate at arm’s length a market. The Health and Social Care Act (2012) went badly wrong as nobody voted for it, and it did not have the support of the professionals (apart from the surgeons possibly) and the public. That Act of parliament did not have anything useful to say about quality of health and care. It was left up to Jeremy Hunt to rubbish bits of the NHS, without reference to the failing Keogh Trusts under his Government.
But I come back to how little care there is for the mental health of the workforce of the NHS. There has recently been discussion of whistleblowing in the NHS, but the solutions for this appear to have been a damp squib. And people have been rather late to the party in opining about whistleblowing in social care (including private nursing homes). And there are still staff in NHS hospitals who are being sent vexatious complaints through human resources, while the same human resources departments fail to educate their workforce on harassment, victimisation, direct discrimination, or making a public interest disclosure. And yet these are precisely the tools needed for hospital staff to fight their over zealous managers who are paid by results themselves.
The culture of the NHS will never be fixed whilst it ignores the mental health of its employees. We know of the suicides of people awaiting outcomes to their protracted investigation by the General Medical Council. We also know that sick doctors can be a danger to themselves, as well as their patients, and can feel totally unsupported.
The mental health of NHS staff should have been more prominent in the NHS Five Year Forward View apart from a few isolated mentions, and certainly there was no mention of how the NHS prefers outsourcing to the regulator to competent performance management.
The rather bitty and random way in which this topic was addressed is nothing other than vulgar.
Different newsreader, different script
With a new Secretary of State for health and social care, it might look like ‘business as usual’. Different newsreader, but same script?
The script might be more or less the same. But with a possible massive political realignment, the Conservatives and UKIP party, GB News, free market economics and libertarianism, anti-woke culture, all in the ascendancy, the NHS might be about to get ‘cancelled’. And then we have the ‘scorched earth’, provided both by Brexit and the COVID-19 pandemic.
The argument is not at all any more 3 seconds to “save the NHS”, which has been a popular mantra for Labour for decades. But Labour has rarely had such an effective leader, or opposition. Labour is nowhere on all policies, but its opposition to Brexit, COVID-19, and even Matt Hancock’s latest conduct, has been non-existent. There has never been a better time for the Conservative Party to go for it. GB News viewers regularly buy into the “levelling up agenda”, in no way blaming the Conservatives for their policy of austerity. Labour is too busy imploding to intervene. GB News viewers regularly stick up for “home grown” nurses and medics, and make strongly anti-immigration noises, saying that the infrastructure can’t cope with the additional population. Matt Hancock did a ‘brilliant job’, oblivious to the disastrous care home policy or corrupt contracts. Hancock is determined to make a return when the time is right, and it looks as if Boris Johnson will give him his full support. Matt Hancock is one of those people who should be ‘forgiven’ as “we all make mistakes”, according to some. Except – had been a doctor he would have struck off years ago.
The easiest way of not addressing the pensions issue in the NHS, the workforce crisis, the crisis in mental health or social care, the backlog in clinical care across the board in the NHS, would be literally to rip up the NHS and start again. Sajid David has still been a paid JP Morgan advisor, and it is well known that JP Morgan have long wanted to get into private healthcare. For the people who dislike the NHS, this is their chance to get rid of it. The anti-wokists, contrary to their usual feelings about the ‘cancel culture’, would happily get rid of the NHS, thinking of it as an inefficient relic of yoke culture, which believes too much in equity, equality and fairness. They feel their views criticising the NHS should not be cancelled. Free speech, and ‘polite debate’, is welcome, so long as you don’t disagree. There would be no imperative to provide a comprehensive NHS, nor indeed mental health care, if it is not profitable, even if the demand is there. Social care, for all the initiatives about ‘social care future’, would simply be whatever the multinational corporates propose – and persons with learning difficulties or dementia might not be high priorities. If you believe racism doesn’t exist, racial discrimination won’t happen. If you are out of the EU, then the EU working time directive doesn’t apply. See what I did there?
We live in interesting times. With Labour having killed itself, and with the help of sabotage from the ‘left wing media’, there is the real material prospect of George Galloway depriving Labour of a win in Batley and Spen. The spin will be that the Conservatives ‘won’ Batley and Spen, reflecting how the public don’t really care about infidelity and corruption, in the same way that they don’t actually care about expensive wallpaper. With more dead cats than can be accommodated in a cattery, the privatisation of the NHS has never looked so good. It won’t be a big IPO – no need to tell Sid. Learning from the utilities, the new NHS England CEO will take care to fragment the NHS into further pieces before transferring the units to the private sector. And with the new NHS reforms, and no immediate blueprint for the social care sector, absolutely anything can happen. And it probably will.
Delirium in an era of Covid has brought rights-based approaches into sharp focus
Covid in care and nursing homes in the UK has become the latest disaster, for example, “the disease may be circulating in more than 50% of nursing homes and mortality is significantly higher than official figures.”
Persons with cognitive impairment, examples of which include delirium and dementia, at the best of times can present a challenge for what we frame as “person-centred care”.
At a practical level, certain individuals who have been living with a chronic, progressive dementia for some time may lose all sense of what time of day it is. At night-time, they may get up repeatedly to check that the front door is locked, and get very anxious about this obsession unless that compulsive check is made. And, because they forget quickly, this can go on many times at night.
Or else, a person may suddenly have a drastic change in behaviour and thinking, and get quite aggressive or agitated, hyperactive, or even quite grandiose and flamboyant in behaviour. Such a flip into ‘hyperactive delirium’ might appear out of nowhere, but could result in a person also wanting to roam around, apparently without an easily understandable purpose.
Both dementia and delirium are significant issues in the era of “Covid19″, infection with the novel coronavirus. Dementia is a “frailty syndrome”, conveying the notion that people with dementia have an increased vulnerability, such that they never quite bounce back to where they were after a challenge such as an infection. The abrupt change which we call delirium can have a number of causes, which we largely view as predisposing or precipitating factors, but it’s relevant to Covid that a respiratory infection can cause hypoxia, electrolyte imbalances and sepsis/encephalopathy which all can produce or exacerbate a delirium.
I should like to focus here on delirium. Helpfully, the HELP team (“Hospital Elder Life Program”) has “created a resource page for all things COVID-19 and delirium, including a Patient Toolkit with all the materials necessary to help older adults maintain cognitive and physical functioning – and prevent delirium“. Delirium can occur out-of-the-blue in any care setting, including the acute hospital, care or nursing home, or at home. It’s tempting to ‘suspend’ personhood in someone experiencing an episode of delirium, as he is ‘not himself’. But this is a slippery slope, to denying personhood, identity of that person, and, at worst, might lead to denial of human rights. Human rights and person-centred care are enshrined in the clinical regulation of professionals, practitioners and institutions, so it would be unfeasible for delirium (and dementia) care to deny human rights or personhood. We know that there has been a number of attempts, presented as ‘social movements’, of activists, said to be ‘living with dementia’, publicised as upholding their rights. This has, of course, got a formidable precedent in the disability movement; dementia under English law is classified as a disability under the Equality Act because of the chronic effects of it. But such rights-based approaches, mainly presented en masse from charities and social enterprises, have tended to focus on a formulation of rights in an almost consumerist way, in a manner where they can be easily marketed through public communication channels such as the social media.
I believe rights are indeed important and indeed crucial – but such an approach has been rather to trivialise the significance of rights. The intentions are formidable, for example in raising awareness of rights and to try to stop and rail against elder abuse, which can lead to loss of fundamental rights such as liberty, privacy or dignity.
But such a simplistic, yet fundamentally important, approach can ignore what rights actually are. Rights have been the subject of considerable scrutiny in jurisprudence theory, as they are of course fundamental to the law. The late Prof Ronald Dworkin was professor of jurisprudence at UCL, and, through his seminal work, we are encouraged to believe that there are two fundamental frameworks; that rights are normally limited, but in exceptional circumstances absolute, or, otherwise, rights are normally absolute, but in exceptional circumstances limited. This led Dworkin to frame his ‘rights as trumps’ viewpoint, and, as an eminent lawyer trained under HLA Hart at Oxford, his thesis is certainly seminal.
But we all live in a civil society, meaning that rights come with responsibilities, and my ‘right’ has an effect on yours. In other words, you could argue that a resident with dementia can’t be allowed to roam around limitlessly, ignoring physical distancing, because of the risk of infecting others with a highly infectious agent. So it might be tempting, particularly if there are staff cutbacks (for example due to staff being ‘off sick’), to use pharmacological rather than non-pharmacological intervention in such a resident experiencing delirium.
In a recent ‘good practice guide’ from the British Geriatrics Society, entitled “Coronavirus: Managing delirium in confirmed and suspected cases”, it is mooted that, “here these interventions are ineffective or more rapid control is required to reduce the risk of harm to the patient and others, it may be necessary to move to pharmacological management earlier than would normally be considered.” And, observing the legal doctrine of proportionality, fundamental to English law where interventions are deemed both necessary and proportionate, this is a very sensible response to prevent other individuals becoming infected, and possibly because of underlying frailty themselves, difficult to treat.
But this is an admission that human rights are not in fact absolute, universal and inalienable, arguably. We have been conditioned to think that we can’t ‘pick and choose’ our human rights, or certainly can’t choose how or why we would choose to apply them, like an à la carte menu – in the same way we can’t choose which individuals to extradite (because readers of certain newspapers believe strongly that human rights are abused in certain circumstances.)
It might also suggest that our application of human rights in delirium care is context-dependent, which seems disturbing at an intuitive level. But this in itself is not a problem. We know from the recent furore elsewhere that guidelines are not meant to be applied in a blanket way, but should, rather, be tailored at a personal, individual level. The recent (excellent) SIGN 157 guidelines, “Risk reduction and management of delirium, a national clinical guideline”, March 2019, says carefully in the quick summary, “There is insufficient evidence to support a recommendation for the use of antipsychotics, dexmedetomidine, acetylcholinesterase inhibitors or benzodiazepines in the treatment of patients with delirium. Expert opinion supports a role for medication in specific situations such as in patients in intractable distress, and where the safety of the patient and others is compromised.” It says rather, “Healthcare professionals should follow established pathways of good care to manage patients with delirium“, referring to a suite of non-pharmacological multi-component interventions.
The problem with guidelines is that, in actual clinical practise, what originally seemed like a good academic idea can be impractical. Infection control is a key aim of treating the delirium in suspected or proven Covid, and we know that the medical regulator prioritises the prioritisation of treatment. We already know the range of arguments against the use of antipsychotics in delirium, which have been extensively studied elsewhere (for example this Cochrane review), but patient safety is the ultimate issue. The case for pharmacological intervention in residential homes for delirium can be easily made, but what happens in home care or domiciliary care where family members can find themselves easily stressed by a relative roaming around but where pharmacological intervention is not possible? Many persons with advanced dementia are living at home, and this indeed has been a goal of national policy, encouraging ‘independent living’ as far as possible.
Furthermore, it can be difficult to distinguish a propensity to roam around, pejoratively called ‘wandering’, resulting from advanced dementia – traditionally and unhelpfully called BPSD – from delirium. So not all people wandering around, with hyperactive delirium, will have Covid. We already know that older people can present altogether atypically, so not all people who are symptomatic or asymptomatic with Covid may have mounted a temperature or an obvious dry cough. So here does the precautionary principle apply, “a strategy for approaching issues of potential harm when extensive scientific knowledge on the matter is lacking. It emphasizes caution, pausing and review before leaping into new innovations that may prove disastrous“? Does erring on the ‘side of caution’ tip the balance from non-pharmacological to pharmacological interventions?
Arguably, there is a need for vigilance over this matter.
Look at the WHO definition of “elder abuse”.
“Elder abuse is a single or repeated act, or lack of appropriate action, occurring within any relationship where there is an expectation of trust, which causes harm or distress to an older person. This type of violence constitutes a violation of human rights and includes physical, sexual, psychological, and emotional abuse; financial and material abuse; abandonment; neglect; and serious loss of dignity and respect.”
Inappropriate use of antipsychotics in “BPDD” in dementia or delirium, especially in the context of vulnerable individuals in society behind ‘closed doors’ with no visitors such as friends or relatives, might be an unintended consequence of behaviour in a pandemic that was intended as proportionate.
But, if all else fails, the whole issue for me has brought into sharp focus the relationship between rights and delirium in the context of person-centred care, and this is to be welcome.
Delirium. Why so little and so late?
My most recent experience of delirium was truly terrifying, to the point that, as a care partner of a close relative with dementia experiencing delirium, I felt I needed counselling about this admission to a London teaching hospital. I have witnessed delirium ‘around the clock’ for half a month so far.
Delirium is not for me a matter of Twitter hashtags, gimmicks or infograms, but a very serious issue I wish to be taken much more seriously. Traditionalists in neurology, for example in the tradition of Gall or Broca, pride themselves on localisation of function – in other words a particular constellation of signs will tell you where the lesion is. But this reason for me is insufficient why academic neurologists and psychiatrists should be disinterested in delirium. Where for example is the research which explains the neural substrates of hypoactive and hyperactive delirium? How long do ‘sleep episodes’ last for? Is it a good idea to wake someone up while he is sleeping? Are there are any neuroprotective agents which prevent long term deterioration after delirium? How much of the delirium will the person experiencing it actually remember?
In a paper by Profs. John Young and Sharon Inouye, the following case scenario is presented:
“An elderly man is recovering from a heart attack and seems to want to lie in bed. He is polite when approached, but sleepy, and he doesn’t seem interested in eating or drinking. Sometimes his speech is incoherent and he doesn’t seem to follow what is said to him.”
Yet this is virtually a carbon copy of the state of my relative when discharged under ‘discharge to assess’. The relative, who also could not mobilise at all (due to the delirium and viral pneumonia), was unmanageable for me at home. I live with her, and unfortunately she had to boomerang bang into the same hospital three days after being discharged ‘medically fit for discharge’. As it happens, for virtually all of the nineteen-day hospital re-admission, many factors conspired to ensure my relative stayed bed-bound, totally unusual for her. It was with a very heavy heart that I decided to call ‘999’, as the hospital environment itself often precipitates or exacerbates episodes of delirium..
The diagnosis at that stage was hypoactive delirium, although the picture became more mixed in the subsequent few days. My relative was admitted, and thought to have a respiratory tract infection, constipation and dehydration. She also lives with frailty and dementia.
It is claimed that, ‘for the family and health-care staff, clear communication, education, and emotional support are vital components to assist with decision making and direct the treatment care plan’, but I felt all three were lacking in this admission. Nobody told me about what to expect in the delirium, or offered me any support for my distress.
If you read the page on “Dementia UK” website about delirium, you are offered the following advice:
“keep calm and reassure the person”
A different HCA in the bay every day and every night is not reassuring.
“observe the person to see if they are in any pain”
The paracetamol was written up prn. My relative could not remember if she was in pain, and none of the nursing staff asked me as her full-time carer if she was in pain.
“avoid too much stimulation”
the ward had a noisy bleeping air mattress which was bleeping all the time, and at night the lights were often bright.
“if possible offer them drinks to maintain hydration”
this simply didn’t happen
Whilst my own regulator, the General Medical Council, takes heavy criticism on a daily basis, I can frankly say that the GMC code on communication (“Communicate effectively” in “Duties of a Doctor”) was flatly ignored in my relative’s admission:
31. You must listen to patients, take account of their views, and respond honestly to their questions.
32. You must give patients he information they want or need to know in a way they can understand. You should make sure that arrangements are made, wherever possible, to meet patients’ language and communication needs.
33. You must be considerate to those close to the patient and be sensitive and responsive in giving them information and support.
34. When you are on duty you must be readily accessible to patients and colleagues seeking information, advice or support.”
John’s Campaign, for me, has to be more than allowing care partners to sit by patients’ beds for longer than a few hours. To make delirium management work, care partners, where available, should be fully involved. I was not asked once by clinician how my relative’s function had dropped off a cliff, nor indeed what she was capable of doing prior to admission.
For me, the initial ‘head rush’ of my relative was astonishing – she was agitated with a blood pressure of 200/110. I subsequently discovered that high levels of cortisol had been suggested to be associated with acute stress in precipitating and/or sustaining delirium. (Neuroimmunomodulation. 2005;12:60–66).
Of course, I agree with letting the treating physicians to ‘get on with it’, but it was staggering how none of the rationalisation of the medications was ever communicated with me (including the discontinuation of the cholinesterase inhibitor). The cholinergic system has a key role in cognition and attention, and it is not surprising, therefore, that there is some evidence to support a role for cholinergic deficiency in delirium. For example, anticholinergic drugs can induce delirium and often contribute substantially to the delirium seen in hospitalized patients, and cholinergic deficiency is commonly implicated in the pathophysiology of delirium.
Bidzan and Bidzan (2012) have described a 62-year-old female diagnosed with Alzheimer’s disease, who on sudden discontinuation of donepezi experienced a worsening of the dementia symptoms, culminating in delirium. When donepezil was re-prescribed, the delirium resolved and the patient’s mental state stabilised. I would also find lorazepam and midazolam prescribed to my relative, without any communication with us, when it is believed by some that these can actively worsen delirium.
None of the following points from ‘Concise guidance to good practice’ from the Royal College of Physicians of London on delirium (2006) were followed in the course of my relative’s hospital admission.
“A history from a relative or carer about the onset and course of the confusion is essential to help distinguish between delirium and dementia
Patients at high risk should be identified at admission and prevention strategies incorporatedinto their care plan
Many patients with delirium are unable to provide an accurate history. Wherever possible, corroboration should be sought from the carer, general practitioner or any source with good knowledge of them.
The patient should be nursed in a good sensory environment and with a reality orientation approach, and with involvement of the multidisciplinary team.Keep the use of sedatives and major tranquillisers to a minimum.
Review all medication at least every 24 hours.
Senior doctors and nurses should ensure that doctors in training and nurses are able torecognise and treat delirium.”
I feel that non-pharmacological strategies are the first-line treatments for all patients with delirium, and yet as a care partner I was offered absolutely no help with this. I was not encouraged over any reorientation and behavioral intervention, or advised on pretty standard advice such as using clear instructions and make frequent eye contact.
The hospital bed itself had a bed rail. But it is advised that, “physical restraints should be avoided because they lead to decreased mobility, increased agitation, greater risk of injury, and prolongation of delirium.”
As the ultimate insult, the hospital in question refused to talk to me about my experience of the admission as part of their ‘Friends and Family’ feedback, only because the relative in question had limited memory of the actual admission itself.
As a medical student, I thought of delirium as a list of causes, and, even as a foundation doctor, I had little experience of it. But I do feel now it should no longer remain in the blindspot of some doctors, particularly as the experience was so distressing for me.
Carers have to be valued, not treated as an inconvenience
I think before a physician comes to the conclusion that his or her patient has had ‘an acute deterioration of dementia’, he or she should make some effort to get a clear history of the time scale of events.
It amazed me how I was not asked at the Royal Free by any of the admitting physicians what the timescale of my mum’s decline in communication, behaviour or mobility had been. This was not a focal problem in the acute assessment and treatment area, but has been throughout the ten day admission so far.
I genuinely do wonder how useful, if at all, junior doctors are in the daily ward round of my mum with delirium, on a background of dementia. A message to you all – it is not a big success to say that my mum’s chest is clear, and proclaim she is medically fit for discharge, when she has been stuck in bed for the whole admission, her food and drink intake has fallen off a cliff, and she occasionally talks complete mumbo jumbo.
The ward round model is totally unsuited for managing delirium. The junior doctors do not involve the carers in any sort of history, and nor do any of the staff on the ward. There is absolutely no discussion of the management, including calming techniques if your mum happens to be agitated, the avoidance of chemical or physical restraints, orientation in time and place, and sleep hygiene, for example. No discussion at all.
It’s almost as if delirium was never taught at medical school to any of the staff in the hospital. To be honest, I have been totally amazed how my mum, who had suddenly fallen asleep during the middle of the day with hypoactive delirium, would have ‘nothing wrong’ in the eyes of the healthcare assistants.
It’s not enough to give carers passports, although that helps a lot. Carers need to be there to be as far as possible on the ward round, to know what medications have been crossed off without the patients’ or family’s knowledge, to know what the rough plan is, and to be able to ask questions.
It’s often the case that healthcare assistants aren’t able to feed patients with dementia. The reason for this is that it’s not just the actual food which counts, although that’s a big part of it, but also the entire mealtime environment, including how comfortable the patient feels about eating the often dire hospital food. And often the food is dumped miles away from the patient.
And if, like mum, her mobility and independence had relatively suddenly dropped off a cliff, the therapists need to know this. I’ve had absolutely no discussion or goals set by the therapists of what they hope to do with mum. Mum is a frail lady who has experienced a number of shocks, viz change of environment, weight loss, delirium, dementia, infection, dehydration, and there’s been no discussion of her frailty despite this apparently being a priority of the NHS.
There has been no discussion of her management of dementia, with her cholinesterase inhibitor having been crossed off, nor her wider needs beyond discharge. The whole thing is entirely pitiful, as if the two long term conditions my mum has been living with in the community are entirely irrelevant to this hospital admission.
And her meds for osteoporosis have been crossed off. And for her high blood pressure.
I have often thought that doctors don’t want to communicate with carers there, often because they don’t want them interfering with their ill-informed medical plans. This is hugely insulting to those of us who are 24/7 trying our best for our loved ones.
It’s not just about having a dementia friendly clock, or reminiscence room. Carers have to be valued, not treated as an inconvenience.
Why might there be a divide between patients and doctors?
The case against Bawa Garba (“Bawa Garba”) has thrown up some fairly strong opinions from people who support Bawa Garba and from those who don’t.
The feelings on the social media seem to have ignited some long-held views about whether the medical profession is working with patients, or simply against.
All opinions lie on a range, and some of the opinions lie at an extreme, such as the notion that doctors regularly lie and cover up.
Much of the discussion on Twitter seems to refer to some power imbalance, but it is the case that all regulated medical professions on Twitter run the danger of being reported to the regulator if their behaviour is called into question. The vast majority of registered doctors, one assumes, does not want to be abusive to any patients, who are not even their own.
The idea that registered doctors regularly cover up their mistakes is a conclusion from the admissions on Twitter that doctors regularly make mistakes and also that doctors are not regularly reporting themselves or others to any regulator about their mistakes.
I feel the question of what actually is a ‘mistake’ or error needs some airing too, however. We accept that there is a range of errors, some which do not cause any substantial harm to decisions which are outright dangerous. The word ‘mistake’ itself is binary, but it does often take a judgment from peers as to whether a pattern of decision-making was clearly abnormal.
No two doctors will always make the same clinical decisions, and even specialists working in exactly the same field might have differing views about the direction in which to take their patients.
But the binary nature of ‘doctor’ and ‘patient’ is at once called out when one realises that many doctors are themselves patients or doctors, so have direct experience of what it’s like on the other side of the fence. Admittedly, most doctors have to switch off emotionally about their patients to protect themselves from going into an emotional meltdown.
This defensive mechanism of not becoming too close to your patients lies in conflict with the democratisation of opinions on Twitter. It would be wrong to feel that all opinions, however, have exactly the same merit. For example, even the most ferocious denial of the Holocaust will fall down.
The information asymmetry between doctors and patients has long existed, and it is probably right that tensions between doctors and patients have resurfaced following Bawa Garba. Some patients will feel strongly that the diagnoses or management plans from their doctors are palpably wrong, given what they might have learnt elsewhere from other sources, and feel powerless to speak out.
The powerlessness to speak out is rife within medicine and nursing anyway, explaining to some extent why ‘whistleblowers’ like Chris Day have such a terrible time. It’s also fair to say that the communication between doctors and patients can be horrific too. I found medications regularly crossed off and added to my mum’s prescription chart without any discussion with anyone.
Whilst it is lovely and fluffy to ‘believe in’ shared decision making and co-production, it is worth considering why it is so widely felt that there is a tense power dynamic between doctors and patients, epitomised by the aloofness of doctors on ward rounds who only see a snapshot of the lives of patients and carers.
I believe that doctors can learn a lot from patients and carers, particularly for frailty, dementia and delirium where the corroborative history is key. This is not just about a sop to visiting hours. This is actually about making the diagnosis and care plans less susceptible to failure.
So whether or not you feel the GMC was too ‘lenient’ with Bawa Garba is neither here nor there compared to the unresolved issues, of a perception of arrogance of some doctors by some patients, or a perception of excess victimhood by some patients in the eyes of some doctors.
The idea of doctors and patients being on opposite sides of the fence is entrenched by the idea of clinicians going into battle ‘on the front line’. Whilst doctors continue to make decisions on their patients albeit in a well meaning and paternalistic way, they will always be accused of playing ‘God’.
What’s the difference between a doctor and God? God doesn’t think he’s God.
Does the GMC believe in patient safety or public confidence?
I am sure that the GMC are interested to a small extent in promoting patient safety or public confidence, but the impression they give out to me is that they see themselves more like the Spanish Inquisition.
For the General Medical Council (GMC), which indeed currently regulates me, to promote patient safety or public confidence it cannot pretend to be apolitical. The wider systemic issues why both safety and confidence are at threat on a daily basis, due to political, economic, and financial issues, simply cannot be ignored any longer.
To some extent, the GMC feels that it can deal with issues without getting its ‘hands messy’ reminiscent to me how the law courts tried to deal with legal issues about welfare payments without making any political or social inquiry. But this is clearly untenable.
If a laboratory is unable to be resourced sufficiently, or there aren’t enough doctors to carry bleeps safety, or there is somehow a wider cultural breakdown in communication between healthcare professionals, it is not reasonable for a ‘just culture’ to fixate on a sanction for a single doctor when much wider issues go simply unaddressed.
I don’t feel it is possible that the public can have confidence in the wider state of the health service if patients with chest pain or an acute asthma attack are queuing up on trolleys in corridors, and the target for assessing acute emergencies is regularly breached nationally.
“Bawa Garba” was clearly a show trial, for the GMC to show to Daily Mail readers that a single mistake of this gravity will not be tolerated. But this does not in itself improve service provision, and, arguably worsens it by throwing in a ‘dead cat’ into the debate.
“Bawa Garba” did not address the central issues of intention to kill or recklessness in medical manslaughter, and, even more worryingly, seemed to signal that the GMC was not only above its own tribunal but potentially above the law in general in wishing to make ‘judge made law’.
I think this is a huge strategic mistake by the GMC, and, if this was a marketing strategy from the GMC, it has gone very badly wrong. Without the legal framework to give some definition of the scope of ‘patient safety’ and ‘public confidence’, the definitions for both are too wooly, and basically issues the GMC a free licence to get rid of anyone it doesn’t like the look of.
You can argue, for example, that a surgeon etching his initials onto a transplanted liver worsens public confidence in the medical profession, as legally there is no implied consent for a surgeon to etch this on property which is not his (a body part). That is common assault and battery in the law, and has been since 1861 in statute law.
Everyone has a bad day at work, and clearly some clinical mistakes are much worse than others. But to pretend that doctors cumulatively in the NHS don’t make thousands of mistakes daily in the NHS is simply complete rubbish, and many medical errors are not made deliberately. To promote both patient safety and public confidence adequately, we do need an approach to the law which is not simply retribution, but potentially rehabilitative too.
After all, it’s not as if we’re not short of doctors in the UK for the demands of the population.
And the GMC does need to operate in the law. It says it does not wish to go behind decisions of the courts, but even the most basic circumspect analysis of the law will tell you the assessment of fitness to practise is a different question is to whether a jury is satisfied criteria are met for a specific offence.
The GMC’s wish not to go behind decisions means that they are in serious danger of running roughshod over double jeopardy in English law, which means you cannot be convicted of the same crime twice.
The GMC really does need, in my opinion, to change tack drastically, as indicated by the disapproval of the Professional Standards Authority at the “Bawa Garba” decision. Otherwise, it will stay as a faceless, self-righteous mass that some of us can really have any faith in.
Everything about the Royal Free management of delirium is completely abnormal
For a start, the Royal Free’s obsession with ‘medically fit for discharge’ does not seem to include whether my mum’s intake of food and drink had fallen off a cliff. She was incoherently rambling, and looked as if she was sedated and half-asleep. This is typical hypoactive delirium, and made my mum’s discharge to assess last week unsurprisingly a complete nightmare for me, her full time carer with whom she lives.
It seems totally unimportant to the therapists on this ward at the Royal Free that she has lucid intervals when she can interact with people. Instead, the therapists are uniquely focused on their task-centered care, performing tasks at their time and convenience, irrespective of which persons are awake or which family is around. As a proponent of person-centred care, I find this totally objectionable, as we now enter two whole weeks of mum deconditioning in bed. For all the attention to ‘end PJ paralysis’, I doubt thanks to the inattention of the therapists at the Royal Free, mum will ever gain her independence again. Her food and drink intake, despite palliation needs, had fallen off a cliff, due to the delirium. She was totally ambulant before. The label of ‘dementia’ rather than opening doors has sent her instead hurtling down a route of ‘terminal’ and ‘end of life’, when she was to all intents and purposes ‘living well’ in the community.
My mum is very light-weight, and is very frail. The diagnosis of dementia, with all drugs crossed of including her cognitive enhancers, never mind rebound of an anticholinergic delirium, has become like a noose round her neck, with the frailty completely ignored. Twice I have had to request the medical team to cross off benzodiazepines, midazolam and lorazepam, off the drug chart, which most people accept can be deliriumogenic. The ward has often been very noisy at night, making it unsurprising many patients are so sleepy during the way, whether or not they have been written up for sedating drugs without any discussion with patient or family. The nurses on the ward, however, are truly outstanding.
Some healthcare assistants are very good. Some overreach themselves with banal phrases such as ‘the blood pressure is PERFECT’ and deliberating facing the electronic blood pressure monitor so that the reading is out of sight. The culture is positively antagonistic, with some threatening to ‘report you for being abusive’, if a cleaner sweeps under your feet while you’re sitting at a chair without any warning, or if you wish to connect Mum on Skype with Kate Swaffer in Australia as a bit of reminiscence. Incidentally, the same healthcare assistant who reported me for that Skype was later sat in the corner with her headphones on chatting on her mobile phone, while patients were calling, and also was feeding my mum at high velocity even when she had not cleared the current mouthful.
I had no choice but to seek my mum to get mum admitted, for dehydration and her falling oxygen saturations, even though the admission itself worsened delirium. There is no attempt to reorient mum in a normal sleep-day cycle, and the regular ‘observations’ have the opposite of a calming effect. The precise diagnosis for mum is a mixed delirium, as she can be agitated. I would never dare to inflict my diagnosis or management on mum, given the code of conduct for registered medical professionals. There seems culturally a reluctance to negotiate with the clear diagnosis of delirium, or a discussion of how function may be recoverable, as the underlying pneumonia is ‘cured’ (or more like delirium does not get coded properly as a diagnosis). There seems to be little appreciation that delirium is worth spotting, and is a significant serious risk itself. When you consider that nobody introduces themselves or what they do, apart from a significant outstanding minority, you have to acknowledge there are good reasons for patients being so confused.
I’ve been really appalled with the ‘acute deterioration of dementia’ being such a prevalent attitude, and no willingness to embrace mum’s function prior to the admission. That is entirely in keeping for the reluctance of everyone to know what mum’s function was like prior to admission. It says on mum’s board that she likes word searches. I can say hand on heart that she has never done a word search in her life.
And whilst medically ‘fit’, she now can’t walk – and that’s new from this admission.
The perfect storm around #BawaGarba was a long time coming
As a result of my erasure in 2006 from the register of medical professionals in the UK, I had a lot of time to reflect on the events leading up to it. I have from time to time also reflected on this following my restoration in 2014. In the meantime, I had re-trained in law, paradoxically inspired by my experience of the judicial process. This was not a brief Masters in medical law, but both my Bachelor and Masters of Law, as well as the pre-solicitor training course. To do the last bit, I had to be approved as a fit and proper person by the legal regulator, the Solicitors Regulation Authority. I enjoyed my study of the English legal system, and reflect that if I had never studied law I would never have met the late Prof Gary Slapper – a formidable academic with an interest in conspiracy theories and corporate manslaughter.
This is all rather awkward, not least because Charlie Massey and Jeremy Hunt get on well, despite having divergent views on the implications of the #BawaGarba judgment. In a way, the General Medical Council (GMC) does not actually do ‘personal’, although ensuing events do rather appear like a hate campaign. It has become traditional to issue a sop to the ‘victim’ of misfeasance of a Doctor, and I do genuinely feel that there can be few things worse than the mental anguish of a grieving relative. The GMC and Medical Practitioners Tribunal Service maintain separation of powers, and, whilst I feel that the GMC can move in mysterious ways, I feel that the GMC believe that they are doing their very best to maintain public safety and confidence in the medical profession. This blogpost is therefore not an easy one to write, and inevitably will mean that I could accidentally cause offence. I am reflecting on issues to the best of my ability, and, if I fall short, I do apologise.
#BawaGarba found herself in a perfect storm. There are various systemic factors arguably out of direct control of the GMC. These are the exact funding of the NHS, including whether there is a sufficient number of doctors on rotas in individual hospitals. Notwithstanding, the GMC has a statutory duty in education and training, and, from what I know, will intervene in cases where NHS Trusts offer a suboptimal training experience. But there are important other systemic factors. It is quite common for non-white British trainees, once a GMC alert has been triggered, to be ‘thrown to the wolves’ from the regulatory process, but whether this achieves statistical significance is worth exploring. The trend has been for, once these Doctors have been reported, for all positive references to be withdrawn, and, often, although the source of the leaks are never identified, for the Doctors to receive a barrage of unfavourable press prior to any hearing. A media presence seems to defy any traditional notion of contempt of court, or right to a fair trial, as Doctors are subject to a total monstering and humiliation in the media. But it is not uncommon for papers in the English media, and their class of readers, also to subject groups of Doctors, such as EU Doctors, to an utter monstering as well, allowing xenophobia and outright racism to flourish. The scope for moral panic is enormous. But to lay these problems at the foot of the GMC, I feel personally, is unfair.
The GMC indeed also has an important statutory duty for patient safety under section 1 of the Medical Act 1983. The “There but the grace of God go I” used alarmingly frequently by white, English doctors on Twitter might reflect the observation that some Doctors are safer from attacks from institutional racism than others. This is particularly problematic if the NHS Trusts continue on its trend to trigger an official regulatory complaint effectively to cover their own backs rather than a genuine attempt to improve the performance, health and wellbeing of their Doctors employed under employment contracts. This has indeed been witnessed in the enforcement of the junior doctors’ contracts, arguably. Also, the “There but” observation is also problematic from the point of view that it seems to signal an admission that registers an admission that registered Doctors go to work knowingly taking risks and making mistakes. Most Doctors will admit to having taken risks and having made a mistake, and the number of mistakes reported daily in the NHS, a mere fraction of the real number, must urge a need for an open and transparent culture where people can learn from mistakes. But the GMC and the higher courts will tend not to tolerate any mistakes, or catalogues of error, whatever the mitigating factors. This might include an unblemished record for 30 years. The issue is that if the performance is way below a standard, there can be no excuse for it. If somebody has died, the threshold for mitigation has to be high, most reasonable persons might argue. And if a court of law has found someone guilty of manslaughter, whatever the process involved for doing so or the people involved, it is hard to leave no sanction on the Doctor, it is argued, whatever the need for organisational learning. Both the GMC and higher courts have consistently argued that public trust and confidence in the medical profession are more important than any individual doctor’s career.
The argument that ‘We go to work and are caught between a rock and a hard place’ merits scrutiny too. This comes down to the nature of how a crime is satisfied in English law – there can be intention to do the crime, and, although there is some finesse about the jurisprudence, there might be recklessness. The law in this is fairly well settled since R v Adomako. It might seem unfair to blame a Doctor having to cover seven bleeps one morning, but the point in law is that the Doctor by carrying those bleeps has assumed a duty of care to his or her patients, and any breach therefore of this duty of care, given the issues of causation and remoteness, is negligence. It might be argued that in tort the Doctor has assumed this responsibility under duress, but in reality most Doctors pick up the bleep from an office in the Hospital without any altercation. And Doctors are entitled to resign if they feel that there has been a fundamental breach of a contract, including a bilateral feeling of trust and confidence, between employer and employee. In reality, Doctors never do, despite the potential risks for patient safety.
Whilst there might be outrage about the lack of due emphasis on organisational learning, this organisational learning nor indeed any individual duty of candour are operational at any meaningful statutory level, meaning they exist in an Act of parliament or statutory instruments. And nobody is above the law. If there had been no sanction on #GawaBarba, a possible interpretation might have been that mistakes, whatever the reason, are excusable because of the ‘state of the NHS’. It might then be argued that the correct course of action might be for corporate manslaughter against the Secretary of State for health and social care, for ‘avoidable deaths’, but this has to be proven beyond reasonable doubt – an incredibly difficult offence to fulfil, as the late Prof Gary Slapper I am certain would testify.
I doubt, if #BawaGarba finds herself back on the GMC Register, she will find it easy to find employment again, especially with at least a five year gap in training. The GMC, even with its statutory duty for education and training, as well as patient safety, seems pretty indifferent to the professional rehabilitation and retraining of Doctors put back onto their Register. But the observation that no Doctor can ever be professional rehabilitated does concern me, even with the strong emotions that the ‘punishment should fit the crime’, and the need for a scalp can be overwhelming. For example, #BawaGarba has found that her subsequent good performance had become somewhat irrelevant as far as the regulator and higher courts were concerned.
As the old trope provides, there are no winners. There are only losers. It’s said that the GMC ‘doesn’t do personal’ in the same way a sanction is delivered in the same way a parking ticket is issued, and the GMC’s purpose isn’t, it is argued, to do ‘show trials’. The GMC’s position is that they are not in the business of ‘punishing Doctors’, but, I feel, it is of concern that unintended consequences, including a culture of fear, could continue to be dominant in the medical profession. The GMC doesn’t likewise, perhaps reflecting their perceived concerns from the general public, want to allow free rein on Doctors ‘free to make mistakes’, and good doctors will argue that they are all trying to do the job to ‘the best of their abiility’. The problem facing the GMC is whether ‘the best of someone’s ability’ is simply good enough. The general approach is that there is no shortage of doctors, and it is a honour to be a registered doctor. Whether there is a sufficient number of doctors for the demand is a concern the GMC can decide to involve itself with, or not. There is a clause in the code of conduct – Good Medical Practice, 2013 – stating that it is the responsibility of doctors to identify any shortfall of resources. I doubt all the senior Consultants or even STs in training taking to Twitter outraged about the #BawaGarba judgment are writing this morning to the GMC to warn about shortage of resources in their own hospitals, despite concerns about patient safety. It is noteworthy that the GMC in their statement on the case mentioned this only yesterday even. But individual Doctors have also been rather effective at protecting their own backs?
The Day judgement reveals either the law needs correcting or public policy on junior doctors is unwell
Whilst the machinery of how the operations and strategy work in the NHS may leave many people baffled, even the hardened specialists, patient safety undoubtedly touches us all.
As you’d expect, all registered Doctors, including obviously those with a ‘national training number’ denoting the Doctor has been selected for the demanding higher specialist training, are regulated by the General Medical Council. The statutory duty of the General Medical Council is, inter alia, “to protect, promote and maintain the health, safety and well-being of the public”.
There is therefore a positive obligation on all registered Doctors to promote patient safety, and this includes speaking out on such matters if need be. The regulator’s official line is to be sympathetic to the concerns of “whistleblowers”, but there exists a sad litany of victims who have blown the whistle who have failed to achieve gainful employment ever again.
There has been much concern about whether the Public Interest Disclosure Act (1999) as a statutory instrument is essentially “fit for purpose”. A general consensus is that it, in fact, isn’t.
Benedict Cooper is an excellent article in the New Statesman explains how Chris Day’s specific case has come about.
“It all started one night back in January 2014. Day was working through the night on ICU at Queen Elizabeth Hospital, part of Lewisham & Greenwich NHS Trust. When two locum doctors failed to turn up to work on another ward, Day found himself dangerously stretched having to treat critically ill patients outside of ICU. Under what’s known as ‘protected disclosure’, he raised the matter and urged his manager to find locums ready to come in. It sounds innocuous enough – it’s been anything but since. Why? Because his case has revealed a major flaw in the system; a flaw that has cost him dearly. Unlike almost every other branch of the medical profession, junior doctors aren’t protected when they blow the whistle in the way Day did that night.”
The Chris Day is truly David v Goliath stuff. Health Education England, like the NHS in general, has access to powerful expensive corporate lawyers; and yet lawyers often talk of decisions being made ‘on public policy grounds’ referring, as the former Master of Rolls Lord Denning did, to “deep pockets” and “floodgates”. A consideration, albeit a pretty immoral one, is that Chris Day’s case might open other litigants to take action against Health Education England which has a huge budget.
The actual judgment is as follows.
For me, and I really do go into this with an open mind, the judgement was concerning as to how the decision-making of judgements occurs. There was, for me, a sense of reverse engineering of making the law fit the conclusion the Judge wanted to produce. This is a well known logical fallacy called “post hoc ergo propter hoc” fallacy.
The law always look behind the substance behind the form, so the English law is more interested in what the employment relationship is rather than what is called. It’d have been much more helpful for the Judge ‘to go back to basics’, in thinking about the nuts and bolts about the nature of Day’s daily work as well as his training, through the lens of the seminal Ready Mix Concrete v Minister for Pensions [1968].
The Judge should not have got wound up in detail but should have sought to produce an accurate picture of Day’s daily duties.
This is indeed advised in Hall v Lorimer [1993].
Nolan L.J. agreed with the views expressed by Mummery J. in the High Court where he said:
“In order to decide whether a person carries on business on his own account it is necessary to consider many different aspects of that person’s work activity. This is not a mechanical exercise of running through items on a check list to see whether they are present in, or absent from, a given situation. The object of the exercise is to paint a picture from the accumulation of detail. The overall effect can only be appreciated by standing back from the detailed picture which has been painted, by viewing it from a distance and by making an informed, considered, qualitative appreciation of the whole. It is a matter of evaluation of the overall effect, which is not necessarily the same as the sum total of the individual details. Not all details are of equal weight or importance in any given situation. The details may also vary in importance from one situation to another.
The process involves painting a picture in each individual case.”
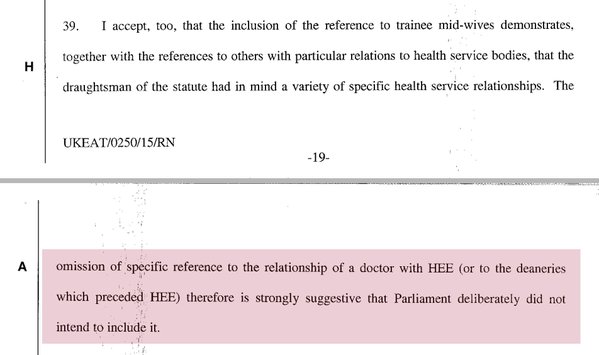
The Judge then curiously pinned his reverse logic, which of course he is entitled to do as a lawyer of high standing, on what ‘parliament must have intended’.
This is, arguably, the most jaw dropping clause in the whole judgement.
But the law as presented is left with startling lacunae, if the Judge is definitely correct.
Take for example this observation from Day himself on Twitter:
@dr_shibley student nurse watching operation has career covered by whistleblowing law. Registrar performing it not covered.If judgment right
— Chris Day (@drcmday) March 13, 2016
This based on the issue that s.43(k) Employments Right Act gives protection for a student nurse watching the operation ‘whistleblowing’, but not the doctor himself on the Specialist Register doing the said operation.
Normally, even the most junior law students would be advised to seek out any statutory aids to help to guess what Parliament might have intended. But only one year previous to the Employment Rights Act (1999), parliament enacted what it thought was extensive protection for whistleblowers, including in the NHS, in the Public Interest Disclosure Act (1998) as discussed here. Therefore, the same parliamentarians, led by the first Blair executive, were responsible for both statutory instruments. It is therefore inconceivable that it could be intended that junior doctors in training would be given protection in one statutory instrument, but not the other.
Furthermore, in response to the lengthy well articulated submissions on behalf of Dr Chris Day concerning article 10, freedom of expression, the Judge provides barely any discussion at all. This dismissal of fundamental human rights, brought into our domestic law through the Human Rights Act (1999), also legislated for by that first Blair government, is staggering.
The Supreme Court recently had to correct the law as interpreted by the lower Courts on joint enterprise. It is not inconceivable that they will have to correct the lower courts again this time on the Day case. But it is an important policy point – that registered medical doctors in training, despite having a duty to promote patient safety, are not protected in doing so. At a point when Jeremy Hunt’s popularity arguably is at its lowest ebb, his special advisors could do no worse than to encourage Hunt to correct the legislation urgently, a low hanging fruit that would make a huge difference on principle even.
Where does austerity figure in the immediate future direction of the NHS?
Edmund Burke wrote that “government is a contrivance of human wisdom to provide for human wants” (1790, Reflections on the Revolution in France).
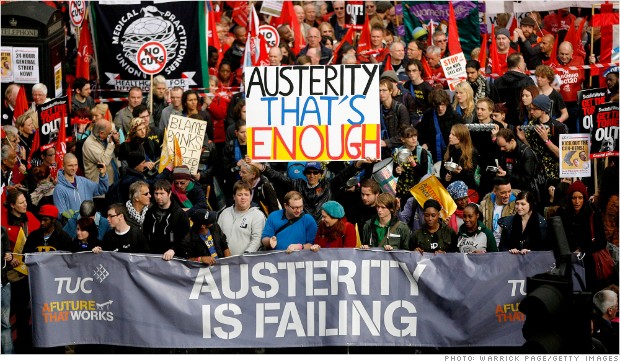
In a lecture at the London School of Economics entitled, “What is the Welfare State? A Sociological Restatement”, given by David Garland, Professor of Sociology at NYU and Shimizu Visiting Professor at LSE Law, a treatise was elaborated where the “welfare state”, however-so defined, is a practical elaboration of systems to solve sociological needs dependent on a thriving economy. Prof Garland’s thesis is partly that pure capitalism can achieve such needs alone, and and one of the final slides is particularly eye-catching:
Scotland’s first minister has described the UK government’s “austerity economics” as “morally unjustifiable and economically unsustainable”. In a speech in London, Nicola Sturgeon recently said a Labour government would have to abandon “failed” austerity policies to win the support of SNP MPs. Ms Sturgeon revealed that the SNP would back £180bn more spending than the coalition government by 2020. What happens in Westminster affects what happens in Scotland. Irrespective of the issue of “English votes for English laws“, the UK Treasury gives a lump sum called a “block grant” to Scotland, Northern Ireland and Wales. It’s up to the devolved administrations to decide how they spend it. The grant to Scotland has been cut (slightly) as part of overall austerity programme.
What? It is alleged that McKinsey helped draft both the government’s £20bn “efficiency” savings and the pro-privatisation health bill, while at the same time selling consultancy services in the aftermath. McKinsey executives and former executives play prominent roles in the NHS regulator, Monitor, and in influential think tanks such as Cambridge Health Network, the King’s Fund and Nuffield Trust.
Jackie Ashley summed up McKinsey’s influence for the Guardian:
“What we are left with are the ambitious plans for the expansion of privately run provision, masterminded it seems by the management consultancy McKinsey, many of whose corporate clients will now bid for work inside the NHS. McKinsey is said to have earned nearly £14m from the government since the election, but this is a drop in the ocean compared with the business that private health organisations working with McKinsey now expect to gain.”
So what? In 2011, the Guardian reported the following:
“Yet the growing evidence from the NHS is that its frontline is being cut, and that NHS organisations are doing what they were told not to do – interpreting efficiency savings as budget and service cuts. While restricting treatments of limited clinical value – such as operations to remove unsightly skin – is uncontroversial, reducing patients’ access to drugs, district nurses, health visitors or forms of surgery they need to end their pain arouses huge concern.
This Guardian investigation detailed evidence of increased cuts – the cuts that, according to the government, should not have been happening – being implemented across a wide range of the NHS’s many care services. With £20bn due to be saved by 2015, and the NHS receiving only a 0.1% budget increase each year until then, experts predict that tough decisions – about the availability of services and treatments, staffing levels and which clinics and hospitals provide care – would become increasingly commonplace.
Meanwhile, across the pond, in September 2014, Obama issued new rules on the crackdown of ‘overseas tax evasion’, including new rules on “hopscotch” loans, new rules on “de-controlling”, limiting the use of the “cash box”, “skinny down” and spin versions. The confluence of activism politics and mainstream politics is an interesting one. Not once yesterday in his questions on tax yesterday in Prime Minister’s Questions did Ed Miliband mention the Occupy movement.
Labour’s posturing on tax avoidance doesn’t once mention @ukuncut. But that’s who put it on the agenda. Activism gets shit done.
— Ellie Mae O’Hagan (@MissEllieMae) February 8, 2015
The “efficiency savings” in the NHS, and broadly have cross party support. And yet there is a clear link between operating unsafe staffing (whether this is low actual numbers or inappropriate skills mix) and quality problems. David Cameron has been ordered to stop saying NHS spending is up; but he continues to disregard this. The multinational corporates have been very manipulative in framing the austerity narrative as the driver for change, in the case of the NHS in making ‘efficiency savings’. While Twitter appears to be populated by innovators perpetuating the meme ‘doing more for less’, there is an equal number of hardworking nurses who are exasperated about having to rush around with insufficient numbers of nurses in the Accident and Emergency or Medical Admissions Units. And of course, all main political parties have bought into the need for austerity.
But elsewhere the evidence is that austerity, rather than making things better, is making things worse.
Despite stringent cuts, Greek debt has actually increased as a proportion of Greek GDP during 2014, from 146% to 175%. Of course, even with falling debts levels, the significant reduction in GDP since 2009 will have meant that the ratio of debt to income will have actually risen. Voters recently handed power to Alexis Tsipras, the charismatic 40-year-old former communist who leads the umbrella coalition of assorted leftists known as Syriza. He cruised to an eight-point victory over the incumbent centre-right New Democracy party, according to exit polls and projections after 99% of votes had been counted. The result surpassed pollster predictions and marginalised the two mainstream parties that have run the country since the military junta’s fall in 1974.
“The sovereign Greek people today have given a clear, strong, indisputable mandate,”, according to Tsipras.
“Greece has turned a page. Greece is leaving behind the destructive austerity, fear and authoritarianism. It is leaving behind five years of humiliation and pain.”
Now what?
Through chance and design, the upcoming general election on May 7th 2015 could be used, through a combination of English and non-English votes, to send a message on the degree to which austerity is acceptable by the voters for the NHS. Coming into this election, the media have been resolutely unsuccessful in engaging the electorate in a mature, sophisticated debate on whether they would be prepared more for a NHS not running with little capacity. However, the electoral arithmetic could mean that parties on the left reject the neoliberal agenda to creating a climate where it might be possible to create a NHS more in keeping with Bevan’s ideals after all.