Home » Dementia
The delirium OSCE. We need to talk about this.
When I sat finals in clinical medicine in Cambridge in 2001, student doctors would be given ‘short cases’ and a ‘long case’. It was all a bit of a carnival in short cases, where you’d be taken to various patients and you might be given a few minutes with them.
For example, in the ‘old days’, you might be taken to a patient wearing a wig, and the discussion might be causes of hair loss. Or even, you might be taken to a patient with a glass eye with a successfully resected choroidal melanoma, and the discussion might be on melanoma.
There is no wish from me to be nostalgic about this. This was a very hit or mess method of assessment, and suited those people who treated clinical medicine exams like a game show. Exactly twenty years later I find myself writing a station for an ‘objective structured clinical examination’ – the OSCE – where student doctors are given a finite amount of time to take a history or to do a focused clinical examination, and examiners mark off certain competences against checklists to provide a rating overall.
Once qualified, student doctors after a period of pre-registration will become registered by the General Medical Council. This means that they are considered ‘fit to practise’, and their primary duty is to the patient and to observe patient safety. For a qualifying examination, you would therefore expect the candidate, a student doctor hoping to qualify in clinical medicine, to interact with a ‘real patient’ or a ‘simulated patient’ or even mannequin.
The key word here is ‘patient’ not ‘carer’.
When I first embarked on an academic journey into dementia, which led to my first book on dementia published in 2014 entitled ‘Living well with dementia’, it was very much the case that the narrative was individuals with newly diagnosed dementia were individuals in their own right. They had autonomy, independence and are deserving of dignity. It was argued that the stigma and prejudice surrounding people with dementia came from persistent media distortions representing people with dementia as devoid of credible speech and other behaviours.
But it is clear that carers are relevant to patients in all sorts of contexts – such as improving health and wellbeing, shared decision making and integrated care and support planning.
Delirium might be a presenting syndrome in someone who later goes on develop a full-blown cognitive impairment of some sort. In many cases, delirium is said to ‘unmask’ the dementia, comparable to how a urinary tract infection might reveal underlying vulnerabilities in an older person with frailty.
The issue here is that a person with delirium might have no idea who he or she is, might be talking gibberish, might fall asleep mid-sentence, or might not know where he or she is. Therefore, taking a traditional history off him or her might be very challenging, to say the very least. We should like student doctors to feel confident in identifying accurately a patient with delirium. With time, we should expect doctors to be able to complete successfully a quick 4AT on someone with delirium.
Delirium is worth diagnosing because what it isn’t in all cases is totally reversible with no sequelae. With, for example, recurrent delirium episodes, somebody might become more cognitive impaired, lose indeependence, become deteriorated in functional activities of daily living, and might even die earlier than expected. Carers often say to me in person that they have a really awful time communicating with doctors in the NHS. Carers in reality are friends or close family, often, and the bad communication is not intention.
Carers end up being quite important in health and social care services, including unpaid family carers. These family carers are often with a ringside seat to observe an acute change in consciousness and cognition or behaviour over hours or days. They invariably end up being care partners during somebody’s hospital admission which tends to be emotionally demanding for all, including healthcare professionals. They are clearly important at the point of discharge, especially if somebody loses abilities temporarily including physical deconditioning.
I find myself coming full circle studying a Masters in medical education at Nottingham. In designing an OSCE for delirium, I find myself drawing on experience as a family carer, and my situated learning of delirium in that context. As it happens, I am also a physician by training.
I am drawn to the immense distress the delirium episode provides for me as a carer, the loved one (the patient) and the clinician.
If I am to write an effective OSCE for delirium it is therefore to emphasise its position as a medical emergency. This is because delirium is often the ‘canary in the mineshaft’, i.e. the warning for something more sinister like severe constipation or an infection of some sort.
It is therefore a test of the art of diagnosis.
But it is also a test of someone’s communication skills and especially empathy. Distress requires attention. Delirium, or the “acute confusional state”, therefore does merit some practical examination of clinical skills. It is virtually never likely to come up as an examinable case for the membership of the Royal College of Physicians, but conceivably could be a 10-minute GP-consultation “CSA” case in the corresponding clinical examination for the Royal College of General Practitioners.
What is striking to me is the lack of published peer-reviewed literature on the examination of communication skills of doctors with carers, or the ability to take an informant or collateral history prior to undergraduate qualification.
We know that that the official curriculum is over-burdened, and hard to put in practise, but delirium is inherently distressing as well as clearly a patient safety matter.
We might be able to do better.
Ships in the night
Like ships in the night, I have seen many millions of opinions shoot past about visiting loves ones in care homes. My loved one is with me at home, but she has advanced dementia. Not everyone who’s a resident in a care home has a dementia. I get that. But I would like to put down on paper a personal opinion about this. This was provoked by an excellent comment made by Vic Rayner in the Commons Health Select Committee this morning.
Vic Rayner emphasised the importance of relationships in social care. I couldn’t agree more. It happens to be a pivotal part of the ground-breaking work that Prof Julienne Meyer led on. Relationships are a crucial part of preventing burnout in staff, and they are also in understanding the resident as a person. It’s impossible to understand a person without understanding his or her social context, people who do or don’t matter to them, and the people who light up a life.
I worry that – and there are many people like me – that mum will soon forget who I am if I leave for too long. I have her nextdoor to me basically. But imagine if I had to be without her for a week. I’d be heartbroken. I often ask her if she remembers who I am, and sometime she hesitates. When she can finally remember, I feel as if I have won the lottery. It’s that one confession that keeps me having a tangible link with my mother. She can remember me. She can possibly remember giving birth to me. She can perhaps taking me up to school or university.
In about 1881, a famous French neurologist published on a theory of the formation of long term memories. Paraphrasing what he said in French, Ribot wrote ‘the old perishes after the new’. Speak to anyone with moderate or advanced dementia of the Alzheimer type, the person will find it much easier to remember what he or she was doing six years ago, compared to six minutes ago. I find that making a connection with me keeps her in the present. I think divorcing mum from me would be very upsetting for her – and very upsetting for me.
But it is also important, I think, to be open about a certain taboo. That family carers are essential care partners. When for example mum has to go into hospital for an acute emergency admission, I get a massive sense of loss as all the care transfers from home to professionals in a hospital. There are, furthermore, certain instances when my account of what has been happening is important, not being hyperbolic about my own contribution. A way of ascertaining whether mum has had an acute change in personality and behaviour, through delirium, is by asking me. Delirium is a medical emergency. Secondly, I know mum’s past medically, and can overcome any cultural including language difficulties. Thirdly, I can act as a reassurrance to mum while she goes through the distress of being a patient with an acute medical emergency. Finally, if care is not appropriate, such that someone does not treat her with dignity or totally misunderstands a situation, I can contribute to help. Unfortunately, it happens to be the case that in health and social care environments people can feel threatened by unwelcome additions to the care team. I’ve experienced this myself when one member of a care team actively makes an official complaint against another. But, when it works well, we can all act together, united, to help the health and wellbeing of people we love.
I understand how this conversation has become one of process and procedure, infection control and even dispute resolution. I could theorise for hours, even days, on the jurisprudence of the human rights involved. But I feel it’s fundamentally a lot more than that – the inhumanity of the separation from people we love. As was put a long time ago, care homes are not fortresses or prisons – they should be somebody’s home. Turning them into prisons is not a proportionate response. It saddens me deeply that so many people have clearly lost their way, but I am heartened by some exceptional leaders such as Kate Lee, Dr Jane Townson, Prof Adam Gordon and Vic Rayner on this.
Sticks and stones may break my bones
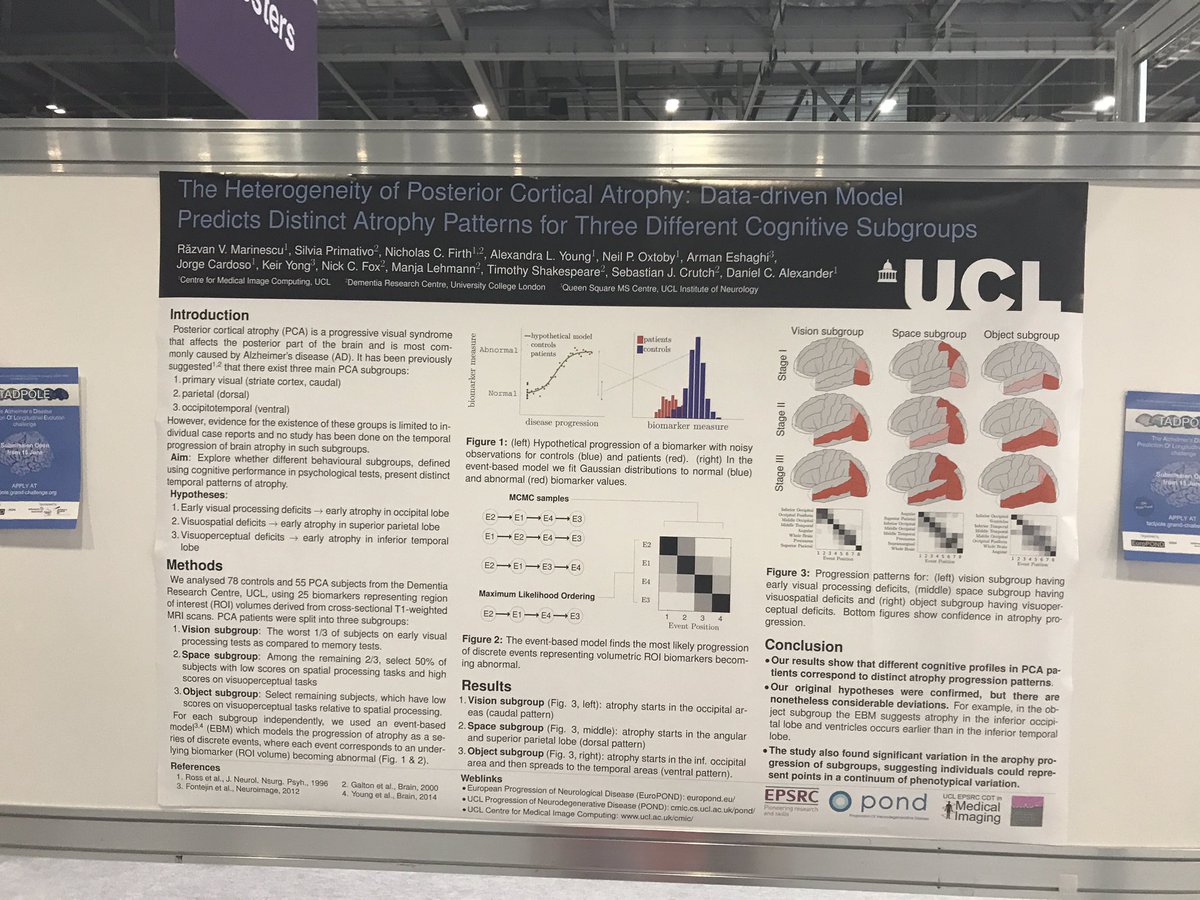
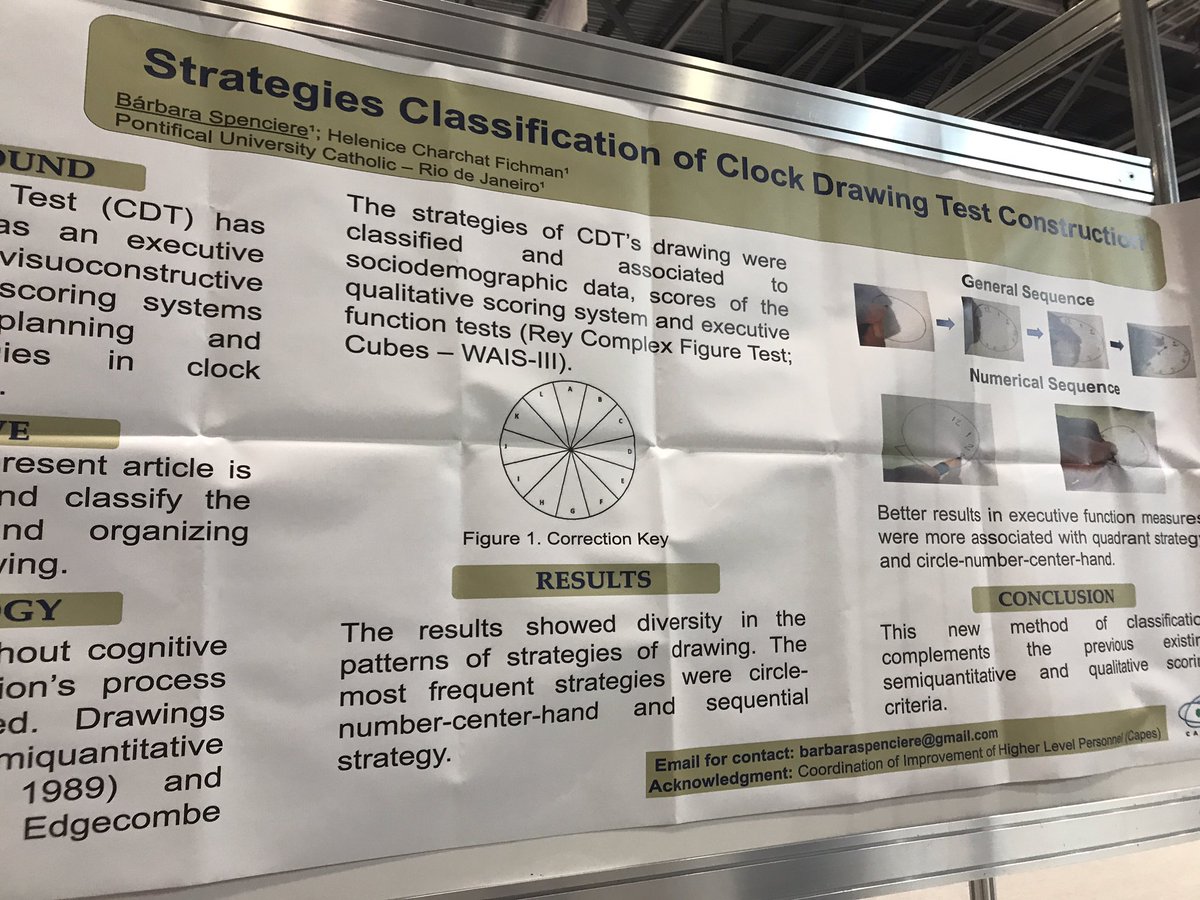
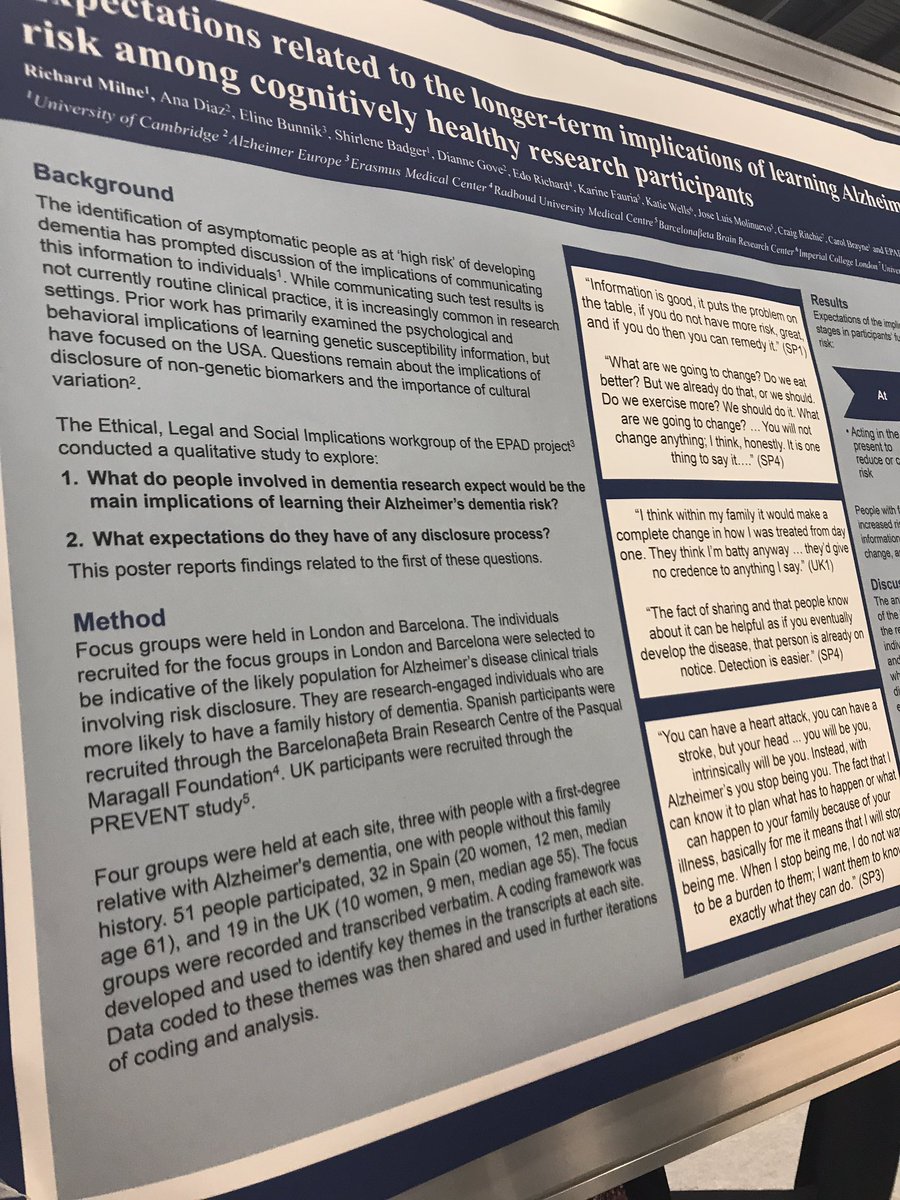
I had first become interested in the language surrounding dementia in 2014, when I presented a poster on the G8 pitch, at the Alzheimer’s Europe conference in Glasgow.
At that point, I realised that sticks and stones could break my bones, but words could hurt me.
I have long since not attended any national or international conferences, not simply because I found the same topics being discussed in perpetuity, but because I felt the conferences were for an in-house cliques who were far more into massaging their own egos and putting themselves up in flash hotels than the reality of dementia.
But I later returned to the issue of language, in relation to stigma, in my second book on dementia ‘Living better with dementia’ published in 2015 by Jessica Kingsley Publishers. As my own mother lives with me, and as her dementia advances, I’ve genuinely found my own book to be a source of information and support. For example, only last night I was reading up on my own thoughts of the ‘sweet tooth’ in dementia and the neuroscientific evidence for why it occurs. Latterly, I’ve toyed with the idea of writing a cookbook for unpaid carers, living with limited resources including scarce money and time, of people living with dementia. I would love to work with someone who’s interested in this specialist field, such as a nutritionist or dietician, to help me.
I became physically disabled in 2007 after more than a month unconscious on the intensive care unit of a local hospital, where I was invasively monitored for acute meningitis. Although I subsequently read Goffman on stigma about a decade later, I had the misfortune to experience stigma first-hand. The sense of ‘otherness’ is something you experience if you’re in a wheelchair, and a London cab refuses to stop despite the cab having its yellow light on. Of course, I had direct experiences of ‘otherness’ as other medical professionals disowned and excluded me when I needed help the most – both in my alcoholism and in recovery. I am currently doing professional dilemma questions, and the knowledge that senior clinical people I worked with turned a blind eye, or did not know what to do and did not admit it, to my illness still frightens me.
As a result of this, I have a low threshold to calling out ‘otherness’, that is where you define people as different to you, and, more than than that, try to discredit them. This might include supporters of Brexit or not, Jewish or Muslim citizens or not, or even living with a long term condition. I don’t think the key to destigmatising stigma is by segregating people. At worst, this might include the ghettoization of people with dementia or mild cognitive impairment such that they all safely live in the same ‘dementia village’, to all intents and purposes ‘out of sight’ and ‘out of mind’. Care homes used to be criticised, by some, for potentially warehousing individuals if the prescription of chemical or physical restraints was frequently abused, similarly. This is not real integration and inclusion, in other awards appreciating the diversity of individuals, but actually lumping all people together with the same label.
For example, in ‘dementia friendly communities’, we don’t acknowledge individuals have different qualia of cognitive impairments, in memory, language or whatever, at various degrees of severity. We don’t discuss how the social determinants of health impact on the health and wellbeing of people, such as poverty or the shutting of day centres. We just clump all people together as ‘dementia’. This is not a million miles off of creating vast groups comprising unique individuals, such as ‘learning disabilities’ or ‘the elderly’.
Whilst the counter-argument is that identification of these groups of people means that their needs can be serviced, often the opposite is true. Recently, a paper has been published on identifying the most ‘frail’ people so that we can be aware that they are the most intense in resource allocation. But think about this carefully. This can mean that we use the information to discriminate actively against the most vulnerable – ‘equity’ and ‘justice’ are not necessarily compatible ethically.
Above all, I am scared how language is used to legitimise discrimination, ‘otherness’ and to embolden other people’s vulnerabilities and weaknesses.
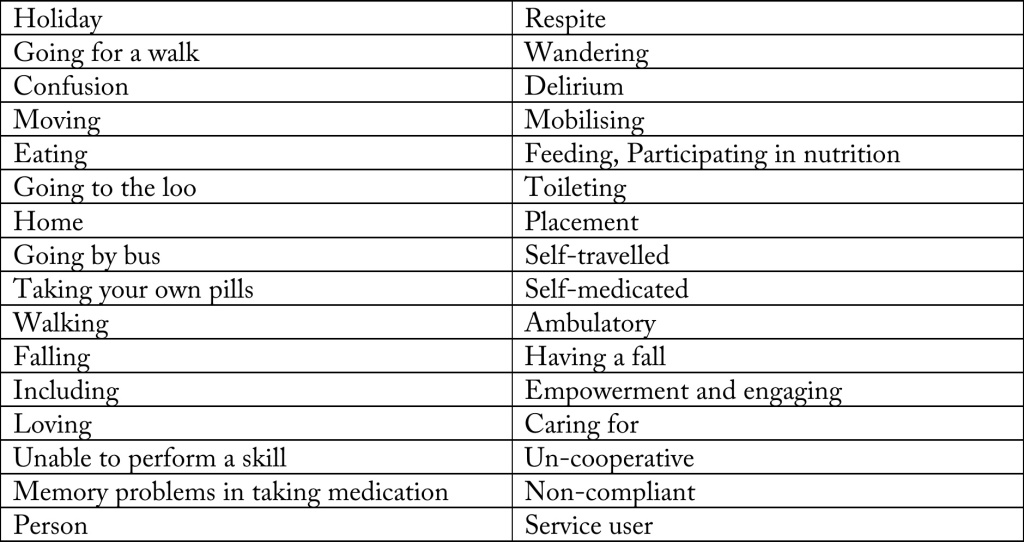
I did a brief scan of some ‘offending’ words, and I compiled them into a table.
I have been much derided for talking about “assets” and “strengths” as well as “deficits”. For example, one person commenting on a piece I wrote in the Guardian remarked similar to, “We don’t need to worry about this patient lying on the operating theatre table with advanced pancreatic cancer. She has great teeth.”
But I strongly believe that it is not difficult to slip into the patronising ‘does he take sugar mentality?’ I don’t wish to turn the medico-legal concept of ‘paternalism’ into a “dirty word”, but, as for our experiences with individuals with special needs, it is a slippery slope to outright dehumanisation and depersonalisation.
I never really understood what it was like to lose your sight until I went blind in one eye last year – but this was surgically operated upon with success. Likewise, I think many of us think we won’t be the ones who get diagnosed with cancer or dementia. But the law of averages means that some of us will be.
And we should think about how “we” would feel if “other people” talked about “us” like that.
The morality of dementia ‘awareness’ while imposing swingeing cuts
The actual reality has been bleak, apart for those for whom ‘dementia awareness’ pays off their mortgages.
In September 2018, the Guardian featured an article on the cuts to social care:
“Nearly all the austerity-era funding cuts to services supporting poor families have fallen in the most economically-deprived areas of England, potentially trapping them in a “downward spiral” of poverty, according to new research. Council areas in the north and Midlands, together with a handful of local authorities in London, have shouldered 97% of the reductions in town hall spending on working age social care, looked-after children and homelessness since 2011, the study says.”
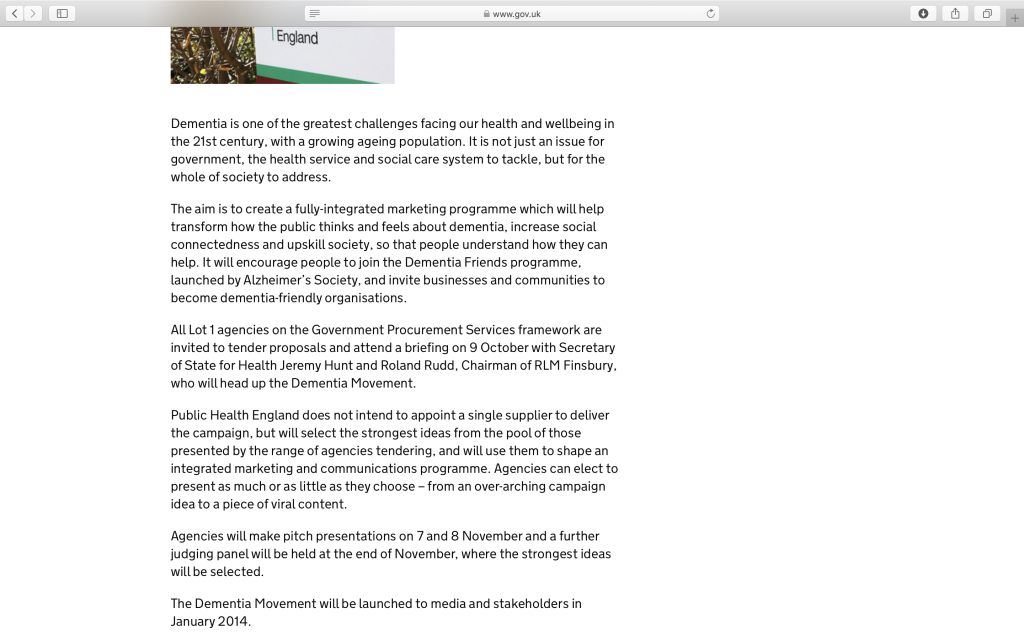
The cost of the ‘Dementia Friends’ programme was always eye watering.
As this press release from 2012 provided,
“Launched the £2.4 million programme, led by Alzheimer’s Society and funded by the Cabinet Office and the Department of Health, to deliver the nation’s biggest ever call to action on dementia to create one million Dementia Friends by 2015.”
I still have deep reservations about ‘cloning’ millions of people to be ‘aware’ of dementia in such a pre-scripted formulaic way.
Take for example this script of how to conduct a ‘Dementia Friends’ information session which can be easily found on the internet. The approach leaves little room for any creativity and innovation by local people to promote awareness of dementia. If there are about 900,000 people in the UK with dementia, you would have thought that they would have had their own personal views of dementia they’d like to share.
But the truth is – this was a massive marketing exercise for the Alzheimer’s Society, with deeply unpleasant political motives. Dementia Friends was never delivered in a genuinely organic way as a social movement. A huge amount of money was put into ‘marketing dementia’ as this press release reveals. There was never any “empathy” as this recent piece from the Harvard Business Review on the topic of change suggested.
In all the intervening years, there has never been an independent report on the return of investment of this programme, despite many many calls for such an analysis of whether the millions of pounds invested ever had any return socially or otherwise.
Take for example the aims of the “marketing programme”:
What have been the tangible results of this? Do the public think or feel any differently about dementia? Has there been a greater sense of social connectedness between people with dementia, carers and others, despite the drastic cuts imposed through austerity in government policy? Has there been any significant upskilling of the workforce in health and social care in dementia?
What ‘dementia friendly’ means has always remained elusive.
It’s even to me, the full carer of a wonderful person – a mum who happens to live with dementia and who requires now full-time care.
It has never convincingly been presented as anything other than a better ‘customer experience’.
Take for example this claim from quite early on:
“When the dementia friends scheme was still in the planning stages, the aim was announced of signing up 200,000 people who, by doing so, would be making a pledge to become ‘dementia-friendly’ contact points for customers they encounter who are living with the condition. With the number of employees having confirmed their support already surpassing 400,000, however, it is clear that the programme is set to be a big success across the country.”
The five core messages of ‘Dementia Friends’ are not beyond reproach either.
Dementia is not a natural part of ageing.
Dementia is caused by diseases of the brain.
Dementia is not just about losing your memory.
It is possible to live well with dementia.
There is more to the person than the dementia.
As you get older, you have an increased chance of developing dementia. With the drive for dementia diagnoses, there has inevitably been more people who have misdiagnosed with dementia when in fact they did have ‘normal ageing’. We know dementia is caused by diseases of the brain, and it is not just about losing your memory – but it would have been sensible at this point to give a brief explanation of the other types of dementia, particularly for those below the age of 65. It’s simply not good enough to say ‘it’s not just memory’. I would never say, as a complete explanation, a ‘supermarket is not simply a delicatessen counter’. That statement provides no information about what a supermarket actually is. Likewise, the statements are consistently half-truths. It is, I am sure, possible to live well with dementia, but it’s also possible for the person with dementia and carer (and others) to suffer enormously, with the emotional pain of not recognising familiar people, not being able to do simple tasks like writing a cheque and so on.
There is more to the person than the dementia is a hollow campaigning slogan when delivered by advocates and charities who relentlessly do not embrace the issue of other social determinants of health, nor indeed any other comorbidities, but want everything to be viewed through the dementia campaigning focus. For example, a simple irregularity is the issue that dementia-friendly communities or behaviour should be friendly to all, unless you genuinely believe that people with dementia are sufficiently homogenous and do not live with any other diversity in their diagnosis or social determinants of health?
Currently, there are nearly 3 million ‘Dementia Friends’.
And my genuine reaction is “So what?”