Home » NHS (Page 5)
A personal budget approach blind to the underlying neuroscience of dementia is doomed to failure
One of the critical messages in recent public health awareness campaigns about dementia is that there is much more to a person living with dementia than his or her actual diagnosis. This focus on personhood, how the person living with dementia understands himself or herself, in the context of his past, present and relationships, and in relation to his or her own environment, is of course critical. It is likely to be embraced in the overall approach of whole person care in this jurisdiction.
Much of the current policy in England in dementia is driven by a scant existence of relevant evidence, for example the mental distress and lack of appropriate management caused by false diagnoses of dementia not confirmed elsewhere in the system. For example, even in the eight years since the seminal paper by Gail Mountain in the journal ‘Dementia’ in 2006, we have had little progress in the literature on the extent to which people at various stages of different types of dementia are able to manage, or want to manage, their own conditions, depending on their cognitive, affective or motivational abilities. This blogpost is about the form of personal budgets where people with dementia are given the money directly to spend, without any broker.
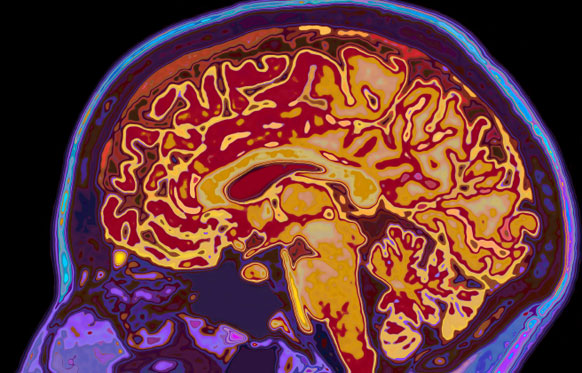
Likewise, the approach of personal budgets in dementia has equal scant regard to an approach necessitated by the cognitive neuroscience. Being able to operate a budget is likely to require a good understanding of mathematics; and it has been known for decades, or if not centuries, that people with disruption of the functioning of a part of the brain known as the parietal cortex can have problems with calculations. This is called ‘dyscalculia’.
Some people with dementia might have real problems in anticipating future outcomes (as shown in the famous Anderson paper) or have problems in making accurate cognitive estimates (as discussed in the famous paper by Shallice and Burgess). The people with dementia for whom these problems are likely to surface are those with disruption of the functioning of a part of the brain known as the frontal lobe.
Also, I showed myself in 1999, published in Brain, that people in early stages of behavioural variant of frontotemporal dementia can be prone to make risky decisions. Others have argued it is more of a problem with impulsivity.
Nobody has any intention of turning people living with early stages of dementia into amateur accountants, but even with the basic budgets you need to have an ability to deal with income, expenditure, costing and reasonable forecasting.
So there is clearly an evidence base emerging that, despite full legal capacity, there are some persons living with dementia who are best not served by direct payments so that they can pursue their ‘choice’. But the introduction of this has been surreptitious, couched in language such as “empowering people with dementia to take control of their own risk behaviour.”
Such flowery language is best kept in marketing manuals, I feel. At a time when report after report has demonstrated that there is not a strong evidence base for improvement in clinical outcomes (such as falls for people with dementia), we must be able to ask for whose benefit are these self-directed budgets for people with dementia?
There is report after report of ‘widening the market’, complaining about the lack of quality ‘control’ of market offerings for dementia. And yet we simultaneously have a care regulator complaining regularly about the quality of dementia services in trusts in England. We have a poor evidence base on what level of budget is sufficient to allow a choice; clearly someone who has an insufficient budget cannot find a choice argument at all compelling.
And is the quality of market offerings being properly regulated to prevent fraud? The last few years has witnessed a series of seemingly attractive offerings for living well with dementia, some of which are extremely good (such as assistive technology, better design of wards and the home), and some of which are poor. There is insufficient evidence here too that the regulator is able to cope confidently except in the clearest examples of fraud.
There is much good work being done in social care and medicine, but with a drive for shiny, instant products, we must never lose sight of the fact that care from social care has been cut consistently over a long period of time. Whenever someone explains the case for personal budgets, there is almost certainly a concomitant explanation of an exploding care budget. However, it would be wrong to slash frontline care while touting ‘The Big Society’ in the same way it would be completely wrong to cut in real terms per caput allocations of care or to pursue backdoor rationing in the name of choice.
Stop telling us we like buffoons and flat taxes. We want a properly run NHS.
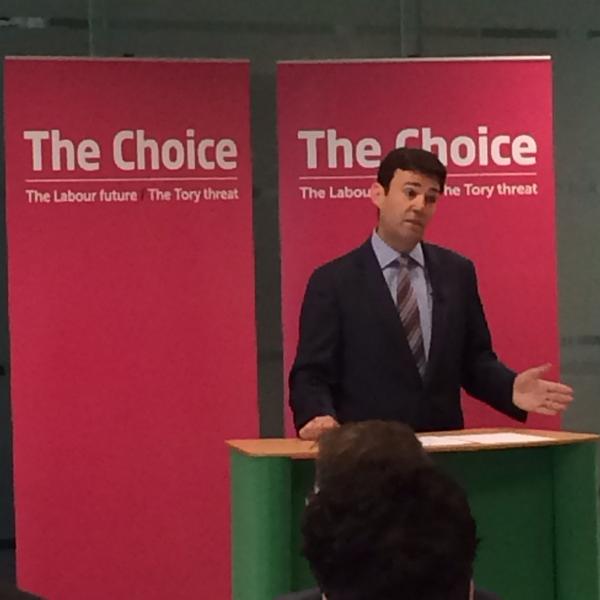
Imagine if Andy Burnham as Secretary of State for Health in a Labour administration just turned up scruffy, tossing around his blonde locks, guffawing loudly.
Or if he was pictured in pubs, regularly having pints of bitter, looking like an escapee from your local golf club?
It just wouldn’t wash. What sort of country is it that likes buffoons and not statesmen? One made by the BBC.
The BBC have relentlessly not discussed the Health and Social Care Act (2012). They refuse to admit that it turbo-boosts the awarding of contracts to the private sector.
It doesn’t wish particularly to mention hospital closures, either.
Both Farage and Johnson clearly love themselves, and nobody knows what their policies are on anything.
And yet they represent highly dangerous people. Narcissistic in approach, they are both capable of being fiercely ambitious.
They might seem perfectly innocent, until you consider the danger posed by a Tory-UKIP coalition. Oliver Letwin is thought to think it’s only a matter of time before the general public wishes to discuss ‘the flat tax’. And guess what – Farage has been said to like the flat tax.
This current Government has made a big song and dance of people not paying their own way, the “something for nothing” culture. A favourite is of course that bloke with his curtains drawn, just as off you’re off to work.
But never mind the corporate tax dodgers. There are some people who would love to get away with paying the rock bottom for the NHS. They would happily see social care completely go to pot.
A flat tax would be perfect for those who want to contribute the bare minimum for the NHS. These are the same people that have pedalled the myth that it is the ageing population that is the big driver of the NHS budget: it is not, it is the aggressive pimping of technology by the corporate sector.
But behind these sinister agenda, ably implemented by the BBC, lies two buffoons, for whom butter wouldn’t melt in their mouths.
Andy Burnham would never be able to get away with the lack of policy on health as per Nigel Farage. He would never get away with acting like the faux idiot like Boris Johnson.
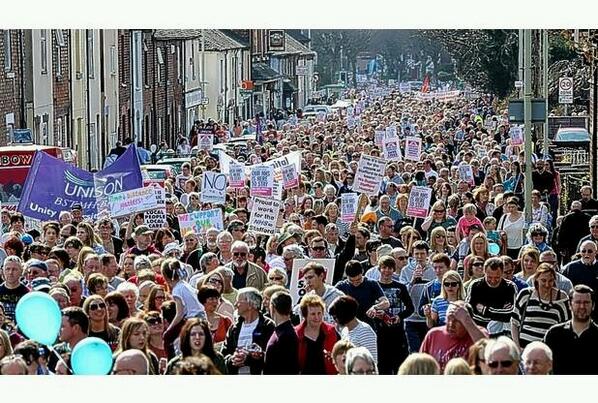
There are millions of people who want a stop to this crap, and want a properly funded NHS, comprehensive, free at the point of need, with a real sense of collaboration and solidarity led by competent statesmen.
What we instead get is a media over-promotion of people who pride themselves on behaving like a couple of airheads, Boris Johnson and Nigel Farage.
Nobody gave this Government permission for the “Great British Sell Off”. Payback time.
There’s a continuous ‘drip drip’ of stuff, prominently from the BBC who couldn’t run a bath when it comes to accurate reporting of anything to do with the NHS or related matters. We hear terms as “the NHS is unsustainable” when people mean “underfunded”, and we hear some parts of West London are “changing” rather than being closed down.
One of the other massive myths is that people couldn’t care about healthcare, and they think all the time about the economy. If that were true, the “feel good” factor would have returned, and we’d all be thinking about prosperity. Except in real life, the cost of living has been an entirely foreseeable consequence of a big corporates running everything. We don’t have a smaller state, we just have an outsourced state, with everything costing the earth.
Anybody wishing to protect a local hospital is lambasted by an expert commentator as a NIMBYist. GPs and nurses are told perpetually to do things quicker and faster and less. It would be like giving a contestant of the ‘Great British Bake Off’ only a bag of flour, and demanding a decorated cake within an hour. Likewise, nobody gave this Government permission for the “Great British Sell Off”. Payback time.
It’s as if the NHS constitution doesn’t exist sometimes. The NHS can be ‘universal’, and yet at the same not to be offering varicose vein extractions free at the point of need. The current Government often spin the phrase, “sunlight is the best disinfectant”, and yet private providers can hide behind the cloak of freedom of information protection, and private providers can trade using the NHS logo.
Last time, what happened was a disgrace. Nobody knew that Andrew Lansley’s vanity piece of legislation to turbo-boost the transfer of resources to the private sector was imminent. There was no mention of it in the Coalition Agreement, which promised enhanced powers to PCTs.
And all of it feels, on one hand, like a giant experiment. That NHS car parks and ambulances are being contracted out to private providers who are simply concerned about the bottom line, and the stroke reconfiguration is based on solid reconfiguration towards centralised centres of excellence.
Non-medical people are often perplexed why it doesn’t matter how long it takes to drive a patient to a stroke centre. That’s because in fact it hugely does. In the space of driving past a local centre which might deliver the appropriate drug and monitor you 24/7, with access to a multidisciplinary team, the “shadow” of the part of the stroke, for example in a type of stroke where lack of oxygen is causing death of brain tissue, is getting bigger. And time matters. This is borne out by decades of evidence.
But this is what happens when the health debate becomes distorted by the media reporting on the views of people without a basic medicine or science degree. And all of it is entirely plausible when the primary driver of health service reform is liberalising the market from people like Oliver Letwin, whose other big turkey is “The Big Society”. That was a big experiment, and another big fiasco.
If politics means anything at all, politicians should be accountable. People often wonder whether Labour was truly held accountable for its NHS Foundation Trust policy, and the part of history when it implemented PFI, as well as when the country went to war against Iraq. But on the other hand, Andy Burnham potentially can fight the forces of evil at play who have taken the NHS debate down the blind alley of competition and quality.
NHS campaigners are furious, and have every right to be. Labour cannot afford to be complacent. Far from it, with most people thinking that Labour will be the largest party if it cannot win an outright majority, it will matter who Labour gets into bed with. And NHS issues, certainly if Andy Slaughter and West London are anything to go by, will matter, as well as the decimation of social care.
The old adage goes, “Who cares about care?”. We’re about to find out.
Whole person care is important in dementia. It should not be used for backdoor privatisation though.
“No matter how busy you are, you must take time to make the other person feel important.” -Mary Kay Ash
People living with dementia are generally not kept ‘in the loop’ about major decisions in the running of their health and social care services.
Whereas some politicians clearly see some capital in promoting dementia, it is hard to distinguish whether this is a genuine interest in dementia or a need to act as a broker for the pharmaceutical multinationals.
Likewise, ‘whole person care’ has all the makings of a great slogan, raising expectations beyond a reality. The concept is, irrespective of funding mechanisms in various jurisdictions, is that you see beyond a list of clinical diagnoses.
You ‘take notice’ of a person when they’re not ill; this has become a very potent concept with realisation that many people live with conditions but are not symptomatic of any illness. And more than ‘taking notice’, you actively help with issues that can help with wellbeing (such as lifestyle, advice about enforcement of legal rights, good quality housing, access to appropriate benefits, proper design of the environment.)
My working definition of ‘personhood’ is somewhat more basic than that of Carl Jung and Tom Kitwood, whose feet I should never wish to tread on intellectually. But my definition is simply that any person living well is at ease with his or her own past, present and future, and his or her environment including community.
In my view, therefore, it is refutable that there are sources of expertise for whole person care outside the medical profession, including unpaid carers, nurses, occupational therapists, physiotherapists and speech and language t harpists, as well as other persons with dementia.
Health and social care in England currently feels like fragmented different worlds, with a complete lack of communication between them. The lack of continuity of care leads to operational problems in offering health and social care. And if you reduce people to a list of diagnoses, you ignore the past of that person.
For example, a concert pianist might have rather different views about developing rheumatoid disease in his fingers than a building site construction worker has about developing the same disease in his.
What is driving the cost of the NHS budget in England, however, in England is technology not the ageing population; half of England’s current NHS budget goes to people below the age of 65 (Iliffe and Manthorpe, 2014).
There is an important how it could be delivered. An anticipated problem is that how the ‘integrator’ will include services including the private sector as well as possibly community care units; in this rôle the integrator ends up subcontracting services, potentially subverting the original ethos of the CCG process. This is a recipe for fast tracking resources away from the State to the private sector, highly dependent on corporates acting like ‘good citizens’.
Certainly, electronic patient records shared between entities would help.
But there is a temptation, and indeed danger, that ‘whole person care’ becomes a wish list for multinational corporations; e.g. “big is best” and implementation of massive IT projects. Focusing on a person’s beliefs, concerns and expectations, however, has been done successfully for decades by many family doctors, who have been subject to the same principles of regulation over confidentiality and disclosure as relevant to IT systems. By this I mean family doctors who spent ages talking to persons and their families in various environments such as home visits, rather than some doctors in modern general practice guillotined by the seven minute time slot.
The current UK Labour opposition is wishing to implement ‘whole person care’ in its next government, and it of course it remains to be seen whether they will be given a mandate for doing so.
But, if so, policy has a delicate balance to run between recognising specialist clinical care in dementia, e.g. through Admiral nurses, in England, and not creating new “silos”, e.g. whole person care nurses in dementia.
Creation of new silos from management and management consultants, apart from all else, encourages insurance-based funding mechanisms for single diseases rather than mechanisms which encourage fair treatment of the whole person in an equitable way.
The strength about the ‘whole person care’ construct is that persons have their physical health, social care and mental health needs considered in the round, with an understanding that comorbities can act both ways: physical illness can cause mental illness, and vice versa.
Whilst it might seem like an experiment in England, and could not have come at a worse time for the NHS with campaigners feeling that changes in health policy are essentially a rouse for backdoor privatisation, the approach of ‘whole person care’ is particularly relevant to dementia, and other jurisdictions, for example California, have already made good progress with it.
I understand why there have been so many deaths of Doctors waiting GMC FTP. That could easily have been me.
At least 96 doctors have died while facing a fitness-to-practise investigation from the General Medical Council since 2004, though it is not clear how many of these cases were suicide.
I can understand exactly how this has happened.
I had a prolonged GMC investigation between 2004 and 2006. At no point during this process was I told when then this mentally arduous process would come to an end.
I think now, seven years into recovery, that there by the grace of God go I.
The media have a remarkably level of detail of understanding from the perspective of the General Medical Council about forthcoming cases. It is impossible for the Doctor to get his side across in the media.
The GMC claim they don’t do show trials.
But my father was fully humiliated with the media storm.
My father was faced with a Doctor son who was in denial and lacked insight. My father is now dead, but I should like to say he probably died in complete humiliation of his son.
My experience is of a GMC which plays to people’s weaknesses in low self esteem and low confidence, a personality trait shared by many with addiction disorders.
Not one report in the mainstream media reported that I was severely alcoholic. And yet the GMC, prior to their erasure of me, erased me with five independent reports stating clearly that I had at least a severe alcohol problem; and that I needed help.
One of the referrals to the GMC was when I attended the A&E of a hospital with acute intoxication. In addition to the referral to the GMC by the Consultant in A&E, I was not offered any post-event support for alcoholism.
The GMC know how to present themselves in the media, but this is in contradistinction to the experience of those who have experienced the Fitness to Practise process first hand.
Dr Peter Wilmhurst writes in 2006 in a wide-ranging criticism of the GMC as follows:
In wishing to infer ‘bad character’, the General Medical Council must not go beyond its statutory duty of promoting public safety. Otherwise, there is simply mission creep and a torrent of smears into a hate campaign by the regulator or its company.
In 2005, one year before I was eventually due to see the GMC, I was suspended. This was due to an alcoholic bender in Northwick Park. I was crying all day in a pub because I could not cope with the investigation any more.
I had waved goodbye to my late father, and lied to him saying I was going shopping.
I didn’t. I ended up being sectioned by a psychiatric hospital in North London, and my father spent ages talking to the medical staff there.
I was then suspended. It was at that point, I wished to call it a day.
I phoned the Samaritans, and they talked me out of it.
I have never told anyone this story. I feel very strongly about what the General Medical Council did to me, even though it might have been merely a product of their inefficiency.
Nobody appears to wish to want to change the system. I’m pretty sure that there are juniors who wish to hold tight until they are Consultants.
What happened to me is that I had consultants in two Trusts in West and North London who said I was ‘late for work’, ‘smelling of alcohol’ and ‘dishevelled’.
None of this got reported in the main media.
I was erased. To this day, I still have no idea who retrospectively complained in graphic detail about my alcoholism did not offer me sick leave, or help with occupational health.
One of them even had the gall to write in his witness statement for the GMC that he gave me the phone number of a private clinic.
I find this particularly ironic as I was later done for incompetence, when that North London trust had allowed me to finish my medical job there, successfully running cardiac arrests there. I passed my Advanced Life Certificate there. I even have the certificate to prove it.
I feel disgusted by the way that the General Medical Council goes about its business.
Far too many one-sided media reports appear in the media containing detailed accounts, as yet unproven. There’s a sense of being hung before you even go to the gibbet.
I am now in my seventh year in recovery. I have done four books, and my Bachelor of Law, Master of Law and Master of Business Administration.
I even completed my pre-solicitor training, as I am regulated by the Solicitors Regulation Authority.
My late father died two months before the Solicitors Regulation Authority gave me permission to finish my legal training, after a meticulous consideration of various factors including details of my erasure.
I am now applying to be restored. And so everything gets racheted up again. The dogs will get unleashed.
And so far they’ve dragged me up to the City where I was struck off, without my late father, surrounded by the same bars and clubs and restaurants. I didn’t have a relapse. Care and compassion are simply two words which are not in the GMC’s dictionary.
I am even applying to go to a desk, non “facing job”. I am now following my erasure newly disabled, so I would not wish to do clinical medicine in any form.
I do not want to be in public health with the stigma of having been erased, for a period of life when I was very ill, and the undoubted discrimination that that would entail.
I had one year of sitting in a pub all day after I was eventually erased in 2006.
This was an extremely dangerous part of life. For my father, it was unbelievably distressing. Nonetheless, he came to visit me every day on the ITU when I was in a coma due to this a year later.
I so understand why there have been so many deaths of Doctors waiting GMC FTP. That could easily have been me.
But I am fighting fit now, and looking forward to my hearing very much.
If Labour wishes to make pledges that do not cost anything, why not an all-out attack on private insurance?
The narrative goes something like this.
Personal health budgets are the stepping stone to private health insurance. You’re given a fixed amount of money, which, as time goes on, is not nearly enough to pay for your health and social care needs. But not to worry, you can top up the budget, like you top up your pay-as-you-go phone account. And if you don’t want to spend your budget in the NHS, you can transfer to private insurance firms like a voucher.
The typical media question, in fact used by Robert Peston last week on Newsnight on Andy Burnham last week, is: “Do you have any fundamental objection to healthcare, as long as its cost-effective and of high quality, being provided by the public sector?”
An answer to this normally involves an answer which revolves around transfer of resources from the public sector to the private sector, or a bit of a fudge saying there’s no ideological objection to private providers, so long as there’s a NHS “preferred provider”.
Labour is obsessed about one thing: the deficit. From this, Labour is prepared to swallow all unpopularity, such as not spending money on pay increases in the public sector, or spending money on benefits (even if the benefits are totally legitimate).
When Ed Miliband was asked later in the week about the “funding gap” on LBC, Ed Miliband gave an answer in the style of ‘some of my best friends are midwives’, and then gave the customary fudge-answer on how he would like the NHS to make better use of the money it’s got.
Except, this won’t wash. There are currently more papers in the business management press along the lines of ‘why belt tightening still won’t make you fit in your trousers’ than Ed Miliband’s been to friends’ bar mitzvahs.
And yet the more blunt way of saying we will preserve the NHS is to go out for an all out attack on the City or private insurance. Labour supporters have to ask why he won’t do this. Is it because Ed Miliband does not wish to be seen to be anti-aspiration? To give you some context, Labour is planning to give hedge fund boss, Michael Farmer, a top honour.
Labour, in saying it does not wish to promote private insurance, does not spend any money. It might though nark off previous Secretaries for State for Health in the Labour Party who work for private healthcare funds.
People pay into the National Health Service, knowing that it is there for them. There is a genuine sense of solidarity and pooling of risk, and equity: free at the point of need. It’s a moot point whether the service is as comprehensive as it could or should be.
But Simon Stevens in bigging up personalised medicine has nailed his colours to the mast without saying so.
Many have alluded to, as indeed the previous CEO of NHS England – Sir David Nicholson has, the fact that knowing the precise risk of a condition with a strong genetic contribution, such as in rare causes of dementia, would mean that that person and their family would end up paying much higher premiums than in the National Health Service.
Ultimately it seems voters want to go for the least costly option – which is why Ed Balls and Ed Miliband would rather wire themselves up to the National Grid than to discuss with Andy Burnham how social care is going to be funded comfortably.
So if Labour tells voters in an all out private insurance system some people will be paying through the roof, and the NHS will go to pot, this will play very nicely to those people who are dead against private insurance in the country’s healthcare.
It will play nicely: if Labour actually mean it.
How do you solve a problem like Andy?
When I first met Andy Burnham MP at the Methodist Central Hall, Westminster, in 2010, where I was later to have a University graduation, he wasn’t as I expected him to be.
He was there for the leadership debate for Labour’s leader. And I remember thinking what a good idea a National Care Service would be.
I have now met Andy on several occasions, and he always waves and says hello. But it’s hard to describe the quality he has to somebody who’s never met him.
He has exactly the same quality as HM The Queen, whom I remember meeting in 1987. I had just been awarded a scholarship to Westminster School, and her husband asked me, “So tell me Shibley, what do you spend my wife’s money on? I bet you it’s booze, fags and wild women.”
The quality I mean is that the Queen has a real ability, despite her status, to make you feel completely at ease. Andy Burnham has this quality too. The thing you end up being struck by is his considerable gravitas.
Having met him, I’ve tuned into this in how he deals with TV interviews or shows such as Question Time. He speaks as somebody who knows the brief backwards, and who doesn’t need to say a lot to impress people.
You get this feeling when you hear a report that Sir Bruce Keogh has apologised to him for the alleged smear attacks. You get this feeling with Sir Andrew Dilnot writes to Andy over the latest statistics screw up.
But I concede it must be driving the Conservative Party potty. The Conservatives trump card is there is a groundswell of opinion that Labour ‘crashed the economy’. While not true, it’s been an opinion which has been hard to shift.
I don’t doubt the NHS will be at least number 2 on the list of factors affecting most people’s voting intentions, but opinions tend to divide amongst people who’ve experienced the NHS and those who haven’t.
There are people who’ve had a terrible time which they will never forget. At another end of the spectrum, there are some people who’ve had a positive experience, but think perhaps ‘they’ve been one of the lucky ones’.
So how do you solve a problem like Andy if you’re a Conservative? Extremely tricky, as Andy Burnham by a long margin is one of the most popular members of the Shadow Cabinet.
Whilst his speech in Manchester was a litany of the current Government’s failings, and the usual critics of Labour piped up to say “what about PFI?” and all that, Andy does not have to say much to impress further people who believe in him.
There’s a group of people who feel that they can never vote for Labour ever again, due to where Labour has taken them in the past. But it’s not at all clear how they will vote, given that the most likely outcome is that Labour will be the largest party at least.
There are people in other NHS campaign groups who really are not convinced that Labour ‘mean it’, and not nearly going enough to address their complaints about the NHS. But they will need at some stage to collaborate with Andy Burnham, not compete with him, if they wish to go anywhere.
Andy Burnham said today, “By starting to bring social care into the NHS, we will build a health service for the whole person.” One suspects that Burnham will have to bring in a person-centred approach, encouraging professional communication between different disciplines looking after a person with, say, dementia, but not go anywhere near personal budgets which have turned out to be a poisoned chalice.
And one of his examples was particularly telling.
“So what happened? The trust launched a private treatment service for varicose veins – using NHS facilities – as they were permitted to do under the new freedom to earn up to half of their income from treating private patients.”
Nye Bevan is possibly the most outstanding Secretary of State for Health which the Labour Party has ever had.
In 1951, Bevan was moved to become minister of labour. Shortly afterwards he resigned from the government in protest at the introduction of prescription charges for dental care and spectacles.
I complete understand the staunch skepticism that Labour is any different to how they used to be under Blair, with Hewitt and Milburn as the Secretary of States for Health.
Lynton Crosby has advised the Conservatives that they should play ‘on their side of the pitch’.
Fine – and it could be that many voters are still concerned about the economy.
But as Carville himself said, “It’s the economy stupid, but don’t forget about healthcare.”
It’s convenient if you think it’s an image thang, but Labour needs answers to big problems
Miliband has indeed called the right shots on certain issues, such as phone hacking and energy bills, but he is wrong to think all of his woes are due to a fixation with image.
This is Ed Miliband who recently posed with a copy of the Sun newspaper remember, despite rather vociferous opposition of the Liverpool MPs in the aftermath of the Hillsborough disaster.
It’s pretty likely now that the Conservatives have screwed up in a sufficiently large number of areas for them not to be able to win an overall majority on May 8th 2015. This all leaves Labour looking as if it will be the largest party at least. The indictment list for the Coalition is massive: real problems in access to justice through the decimation of law centres, operational failures in access to acute medicine, the distress caused to disabled citizens through their withdrawal of disability benefits, and so it goes on.
And indeed it’s pretty likely now both the Conservatives and the Liberal Democrats have done enough to lose the next general election.
But Miliband’s fixation on image is odd. It’s odd particularly he has always claimed he never reads the papers, like an aloof academic who never reads bad reviews of his work. The “I am not worried about my image” story presents an inherent paradox that Miliband is intensely worried about his image. But he should be worried about other things.
Labour is looking, policy-wise, in healthy shape. The UK Labour Party is relatively united, and the list of policy proposals look coherent.
But the Labour Party, like all parties, have ‘questions to answer’. It needs to answer whether it would be prepared to safeguard the NHS budget as the inequality gap gets bigger. If it is indeed the case that Greg Dyke, who considers himself reasonably well off, is happy to pay a larger amount of taxes to not have a NHS on its knees, should Labour be bringing that discussion openly to the public?
Labour says it cannot do much about the TTIP investor state dispute settlement negotiations as they’re being done in private, but Labour still gives an impression of being led by events not being in control of them. Likewise it is committed to negotiating a new settlement for PFI literally, not solely the problem of the Labour Party, but PFI does not seem to be a discussion out in the open. It clearly is not a niche subject when it can affect the reconfiguration of local hospitals.
And the general public are not convinced about the NHS being run on the model of a supermarket. Members of the public include disgruntled former employees of the NHS who have found the culture oppressive and stifling, with abuse of power by people in authority. And nothing much seems to change.
Ultimately there is always enough money for wars, and inquiries into war, and you never hear of the Prime Minister saying we can’t intervene because we’ve overspent our budget. People who used to vote Labour want some sort of ideological reassurance that the NHS will not be sold off to the highest bidder, and our utilities won’t be owed by foreign oligarchs. Yes, the left is capable of “doing” patriotism too.
For the record, I have never been one to dismiss the National Health Action Party or Keep Our NHS Public as cranky pressure groups who have no credibility in their mission. They are speaking up for massive faultlines in our NHS policy, and, whilst Labour is clearly speaking out against the current Government, many former Labour voters simply put their face in their palm when Miliband dismisses the problem as image.
It is not.
Time for a new regeneration. The New Secretary of State for Dementia.
Ed Miliband looks a bit awkward eating a bacon sarnie, or simply looks a bit “weird”. This man doesn’t look like your next Prime Minister?
But switch back into the reality. A cosmetic reshuffle where the present Coalition had to ditch a Secretary of State more toxic than nuclear waste from Sellafield to transport in a catwalk of tokenistic young hopefuls, “governing for a modern Britain”.
And engage a bit with my reality: where English law centres have been decimated, nobody is feeling particularly “better off” due to the cost of living crisis, GPs have been pilloried for being “coasters”, criminal barristers have gone on strike, or you can’t get your passport on time.
Whisper it quietly, and nobody wants to admit it, that despite all the concerns that Labour will front another set of middle-class neoliberal policies, Labour is in fact going to walk it on May 8th 2015 as the new UK government.
This will obviously be quite a shock to the system, and you can already feel the Civil Service behind the scenes mentally preparing themselves for a change in flavour for the dementia policy.
The current dementia policy had “Nudge” fingerprints all over it. “Customer facing” corporates could become dementia friendly so as to allow market forces to gain competitive advantage for being ‘friendly’ to customers living with dementia.
The Alzheimer’s Society got thrust into the limelight with the Prime Minister’s Dementia Challenge, ably supported by Alzheimer Research UK, to offer the perfect package for raising awareness about dementia and offering hope for treatment through basic research. This private-public partnership was set up for optimal rent seeking behaviour, with the pill sugared with the trite and pathetic slogan, “care for today, and cure for tomorrow.”
Except the problem was that they were unable to become critical lobbying organisations against this Government, as social care cuts hit and dementia care went down the pan. Dementia UK hardly got a change to get a look in, and it looked as if a policy of specialist nurses (such as Admiral nurses) would get consigned to history. They are, after all, not mentioned in the most recent All Party Parliamentary Group report on dementia.
It is widely expected that Labour’s NHS policy will be strongly frontloaded with a promise of equality, which the last Labour government only just managed to get to the statute books. Insiders reckon that this policy will be frontloaded with an election pledge with equality as a strong theme.
In the last few years, it has become recognised that caregivers feel totally unsupported, people get taken from pillar to post in a fragmented, disorganised system for dementia with no overall coordinator, and there are vast chasms between the NHS and social care treatment of dementia.
The next Government therefore is well known to be getting ready for ‘whole person care’, and it now seems likely that the new Secretary of State for Health and Care under a new government will have to deliver this under existing structures. This will clearly require local authorities and national organisations to work to nationally acceptable outcomes for health and wellbeing through empowered Health and Wellbeing Boards. This will help to mitigate against the rather piecemeal patchwork for commissioning of dementia where contracts tend to be given out to your friends rather than the quality of work. Health and Wellbeing Boards are best placed to understand wellbeing as an outcome (which can become missed in research strategies of large corporate-like charities which focus on care, cure and prevention).
And the switch in emphasis from aspirational friendly to a legal equality footing is highly significant. The new policy for dementia under the new Secretary of State will be delivering what people living with dementia have long sought: not “extra favours”, but just to be able to given equal chances as others. Environments will have signage as reasonable adjustments for the cognitive disabilities of people living with dementia in the community under the force of law, rather than leaving up to the whim of a corporate to think about with with the guidance of a fundraising-centred charity to implement.
With the end of the Prime Minister’s Dementia Challenge in March 2015, which has been highly successful in places in delivering ‘dementia friendly communities’, a commitment to improved diagnosis rates and improved research, it is hoped that the next government will be able to take the baton without any problems. It will be quite a public ‘regeneration’ from Hunt to Burnham, but one which many people are looking forward to.
My medical career finished along ago, but the GMC FTP procedures for ill doctors are still far too dangerous

One of the ways that the General Medical Council will try to pin you down is if you appear blasé in any sense about your own behaviour, or lack insight into its repercussions.
I have a psychiatrist in West London who oversees my recovery. I am a barn door alcoholic now in recovery. One of the wisest things he has ever said to me is that it is impossible to ignore the distress I caused to friends, family and others. I think about this every day of my life in fact. It has left an indelible trace on Google, which I do not wish to forget. That’s why I have never asked for it to be removed.
I get upset that the BBC considers my tragic case of erasure from the Medical Register as ‘entertainment’. Behind this titillating story was someone who was in massive distress, and to some extent continues to be in distress.
I have learnt the General Medical Council (GMC) is only doing its job. Reports, like the latest damning one by Civitas on how the GMC treats sick doctors badly, come and go. And nothing really changes.
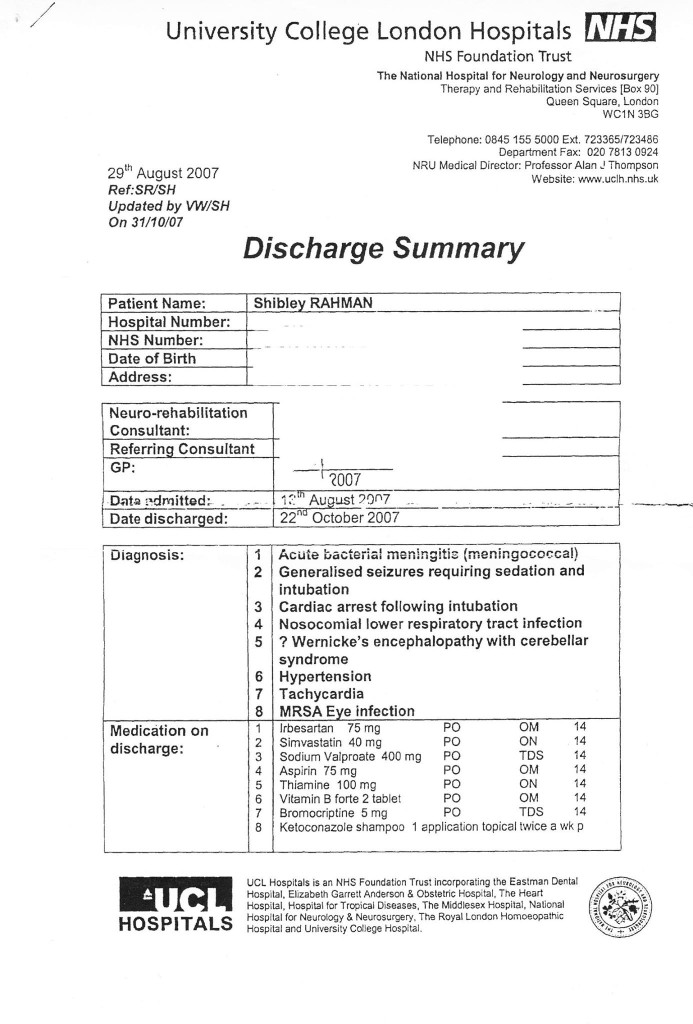
But I remember all too well what happened to me. I repeat that I find my behaviour then, as a different person, disgusting and unacceptable. But things came to a head when I was blue-lighted in at the beginning of June 2007 with an asystolic cardiac arrest which I was very lucky to be resuscitated out of. I then spent six weeks in a coma. I was fighting for my life, with drips, a central line, and the full army of Intensive Care machinery. The Consultant at the Royal Free warned people I was not expected to leave the hospital. I was clearly a very sick man.
My late father came to visit every day when I was learning how to walk and talk again at the National Hospital for Neurology and Neurosurgery. That’s where I had spent six happy months, while healthy, learning about general neurology and dementia. It’s where I developed a lifelong interest in neurodegenerative disease, which pervades through my post-doctoral fellowship at the Institute of Neurology thereafter, my mention in the Oxford Textbook of Medicine, and my own book on wellbeing in dementia.
I am happy now that, having learnt how to walk and talk, I was invited to the Alzheimer’s Association International Conference in Copenhagen last month, and I went to the Alzheimer’s Show in Manchester and London this year. My friends include people living with dementia, and they tell me what’s important in policy now.
I remember though the days of having to hide my name on blogposts or my Twitter account. I remember how I was frightened to show myself in public in the last few years. I remember how my circle of friends completely collapsed, though I am happy with the very small number of very close friends I have now. I still continue to get trolled, like no tomorrow, with words like “Disgusting” and “How do you live with yourself?”
I do also remember how the General Medical Council took years with their investigations. I remember the torrent of newspaper articles explaining how likely it would be I would be struck off. I remember thinking how this was an inglorious end to my ten years training to be a Doctor, a profession which I still feel honoured to have been in once.
But the General Medical Council protracts out their investigations. The GMC never got round to appointing a clinical supervisor (very odd) even though my independent clinical examiners had concluded that I had a severe alcohol problem. So it rumbled on for a few years with my mental health in free fall. Dynamite.
This is extremely risky – dangerous – for the sick doctor. If you lack insight or if you’re in denial you can be finished (as indeed the numbers of people reported to have committed suicide while waiting for their Fitness to Practise sessions show).
I remember how I totally ‘lost it’ in 2005 a year before my final hearing. I had long left a medical job, but I just fell apart while still waiting for my GMC hearing. I went on a massive bender sat alone sobbing into my drink in a pub in Notting Hill very close to Portabello Road, ended up being sectioned, and then was suspended by the GMC.
A year after I was erased, with no job and no family or friends virtually, my life really did take a nosedive. I sat in pubs all day from opening time to closing time. I was done for drunk and disorder offences.
But I woke up after a six week coma, newly disabled, but with a new purpose. I did three books on postgraduate medicine, and I became regulated by the Solicitors Regulation Authority. I have three degrees, my Bachelor of Law, my Master of Law, and my Master of Business Administration, as well as my pre-solicitor training.
I didn’t get very far when I bothered going up to Manchester for my restoration application. The GMC hadn’t bothered to do a basic conflicts session, so the meeting was adjourned after one day. My friend Martin Rathfelder made it to support me. He like Jos Bell and Kate Swaffer are true friends.
It’s a miracle that I didn’t have a relapse being in the City where I had been with my late father, where I was erased, with plenty of bars and restaurants, with plenty of memories. It’s like you’re being set up to fail by the GMC – or else they are incredibly incompetent when it comes to dealing with people with mental health issues.
But I did get as far as asking the panel if I could hold the hearing in public this time. I want to explain to the whole world why and how alcohol destroyed my life, and caused distress to others.
I think the GMC did the right thing in getting rid of me from the medical profession, but I am still bemused why one consultant in West London asked me to sort it out by giving me a phone number of the Priory, did not refer me to Occupational Health, and did not offer me sick leave. I am bemused why various consultants described me as looking dishevelled and alcoholic, and yet allowed me to finish my medical jobs in London, without referring me to Occupational Health.
By the time I was erased, the GMC had been given five reports from five independent doctors stating clearly that my primary problem was a severe alcoholic dependence disorder, and that I desperately needed help.
I never received this help until the NHS saved my life a year later.
The GMC will wish to ‘win their case’ and I strictly speaking am not allowed to bring any of this up in case it reaks of bitterness.
The GMC opposed my application to explain all this and my recovery in public. The panel rejected the GMC’s case.
In my view, Clare Gerada’s “Practitioner Health Programme” is a necessary lifeline for those are sick Doctors, and who fall under the London jurisdiction.
Prof Gerada is a true inspirational NHS leader.
Needless to say, I’ve never had an alcoholic drink for more than seven years, since my coma. I’m one of those guys who has no off switch after one drink, such that I’ll either end up in A&E or in a police cell.
My case will now be held in Manchester beginning August 20th 2014. If you want to begin to understand how sick doctors cope, or do not cope, please feel to come along.