Home » NHS (Page 6)
This is not scaremongering or conspiracy. Personal health budgets do promote privatisation.
The question is not whether personal health budgets will promote privatisation. The more interesting question is how they will do so.
I have been concerned that anyone who legitimately raises concerns about the current direction of travel from the main political parties has been dismissed as a ‘quack’. The scope for conspiracy theories hypothesising is of course enormous, but any CEO trying to formulate strategy will wish to think a few steps ahead.
“Personal health budgets” (PHBs) are normally sold under the truncheon of “look at how it’s worked for X’, and of course single case anecdotes of where they have worked for people are good to hear.
I would be the first to accept David Cameron’s approach, that it is not where you have come from it’s where you’re going to. But I cannot accept this in this scenario.
I do not wish to play the man not the ball here. But to ignore his career experiences would be daft, given that his CV would have contributed to get him his job as CEO of NHS England in the first place.
From 1988 to 1997 Stevens worked as healthcare manager in UK and internationally.
In 1997 he was appointed Policy Adviser to two Secretaries of State for Health (Frank Dobson and Alan Milburn) and from 2001-4 was health policy adviser to Tony Blair. He was closely associated with the development of the NHS Plan 2000.
From 2004-6 he was President of UnitedHealth Europe and moved on to be Chief Executive Officer of UnitedHealthcare Medicare & Retirement and then President, Global Health and UnitedHealth Group Executive Vice President of UnitedHealth Group.
He is more than aware of how the private insurance system works.
Let’s get this straight – it is simply untrue that PHBs are ‘great for mental health‘. Take for example a young lady poorly medicated for bipolar affective disorder, really at risk of making impulsive choices. She goes on a spending spree, thus blowing at one go her PHB.
Or take a 52 yr old man with behavioural variant frontotemporal dementia with normal memory. He is also prone to risk taking behaviour as part of his condition. He goes on a spending spree too, thus blowing his budget.
So we can all play the anecdote game.
Clinical Commissioning Groups do not have any requirement to be populated by clinicians, though ideally this would help. They are responsible for working out how to spend NHS money amassed legitimately from the taxpayer. Therefore the NHS is not strictly speaking free, although a founding value has thus far that it is free at the point of need.
They are also interested in the demographics of their population – how ‘risky’ subgroups might contribute in generating a hefty bill for the local population. That’s why there are gizmos such as the ‘dementia prevalence calculator’, for example. To that end, clinical commissioning groups in allocating resources according to risk function exactly like insurance entities. They just happen to be in the state.
The ‘money following the patient’ strap line hasn’t come from nowhere. It would be perfectly feasible for you with your allocated budget to transfer it to a private insurance entity without any obstacles. This is one of the main concerns of ‘competitive markets’.
The idea that PHBs might be best for people with long term conditions not best for people who are fit and healthy is setting up the NHS for a fall, though. Lord Norman Warner talked this week of how he would like the NHS to be serving people to ‘live well’.
But if people with long term conditions are ‘looked after’ in the early stages of the policy, and people who’ve had good experiences can encourage other people to adopt them, and if ‘brokers’ who have something to gain financially from the introduction of this policy can get their message across, they might endorse this plan.
The plan though is dangerous for them as they’re the ones who are left voluntarily in the State’s system, leaving politicians with the right mood music for healthy living people to leave the system, and to seek private insurance. That is the real danger of the way the system is going.
None of the above is far fetched. None of it is inaccurate. It is simply a statement of fact.
Sir David Nicholson has often remarked that private insurance markets would not work for certain complex conditions such as dementia, where it might be possible to ascertain with a high degree of certainty an individual’s risk of developing some family forms of the condition.
And you can see where this is heading can’t you? Certain people with dementia with strong risk factors for dementia genetically will be obliged to disclose this information to private insurers, here or abroad, and face astronomic premiums (sic) as insurance companies will not want to take on the risk.
And not all old people ‘cost’ the NHS – it is the last few months of life which are really expensive for any healthcare system.
Nicholson is right.
Andy Burnham MP, as Shadow Secretary of State for Health, must have as his primary interest, whatever the inglorious past of some policy decisions of Labour, the concerns of the voters.
They have said clearly on numerous occasions that they do not wish for ‘privatisation through the back door’, whatever one’s views on the private v State debate.
If voters do not want privatisation through the back door, the UK Labour Party should be very wary of going further with this policy. An unintended consequence is that, conspiracy or not, this policy might ultimately be setting up the NHS to fail. And it might be a perfectly intended consequence for some.
Now it is clear that patients must be offered real choice – at the ballot box
What brand of washing powder would Sir like?
Nobody really has a need for a thousand different types of washing powder, unless it happens to be the case that you’re physically allergic to particular brands. And similar arguments can be put forward for gas and water. Or a hernia operation.
Will the patient be aware that he has a particular congenital abnormality in his tummy wall requiring his surgeon to go in a particular route to repair his umbilical hernia?
It is hard to see how this constitutes patient choice. And also, if the market agrees amongst itself, certain providers will do the hernias, and others will do the excision of sebaceous cysts, how much choice will there be if a number of large providers settle on a ‘market price’ for these services? However, the service is essentially the same.
People who support ‘choice’ by and large say that it is not a matter of ideology, but paradoxically then continue to talk about choice as a matter of a human right. But choice must be meaningful. Choice cannot be properly exerted if you are in fact being sold a pup literally. Or it can’t be true choice if the money has run out – money doesn’t grow on trees, remember.
With the main political parties converging on various forms of the market, personal health budgets, the need for ‘efficiency savings’ (even if that leads to dangerous unsafe staffing while PFI loan repayments are made), an assumption of continued unnegotiated PFI contracts, how much choice does the electorate have?
Presumably Labour will continue to campaign on its ‘Only Labour can save the NHS’ meme, and looking around there is some justification of this with the firestorm closure of accident and emergency units here in London.
But whichever party comes into power, the question has to be: will very much change?
Personal health budgets are an extremely good example of this. The main political parties continue to tout this policy plank, with the continued maelstrom of ‘success stories’ as well as severe warnings. And yet nothing much seems to change.
The same providers promote them. The same campaigners oppose them.
Like any proposed European referendum, it is hard to know whether many members of the general public are in charge of the real facts – such as whether there are important safeguarding issues to protect people with certain types of dementia? Or to prevent people going through a manic phase of bipolar affective disorder to go through a phase of reckless manic spending?
I feel that all parties must now accept that many voters do feel severely disenfranchised, and it is hard to know how remedy this information asymmetry without, say, doing a LBC debate presented by Nick Ferrari or a BBC debate presented by David Dimbleby.
But the tragedy remains, that while we keep on being told that ‘choice is good for us’, the scope for real choice, many say being an attribute of neoliberal multinational corporate activity, is a phoney one.
Put your money where your mouth is. Campaign for the NHS not incessantly whinge.
We might disagree on various things to do with the NHS, but there’s no doubting the robust commitment of ‘Keep Our NHS Public’ (@KeepNHSPublic) and the ‘National Health Action Party’ (@NHAParty) Despite their obvious clear antagonism to the Labour Party, I think the last thing they want is another Conservative government, this time propped up by UKIP. Twitter’s where it’s at, and both Dr Jacky Davis (@DrJackyDavis) and Dr Clive Peedell (@cpeedell) are extremely ‘media savvy’. Marcus Chown (@MarcusChown) is indeed known to be one of the high-impact ‘influencers’ of Twitter.
But bloody Nora. You can even order on the internet a box of 500 wristbands in a colour of your choice, with lettering in a font of your choice.
It’s tempting to buy a box of 500 with the words, “Make PFI history”, or “Make the internal market history”.
Or “Make the purchaser-provider split history”.
But you’d have to make the lettering increasingly smaller to make it all the criticisms about previous Labour health policy fit onto a small wristband.
But there is every chance that the general election will make “Make Miliband history”.
So far, there’s not even been a smidgeon of what Ed Miliband intends to do about the private finance initiative in the context of NHS infrastructure, or what he intends to do to prevent accident and emergency departments being selectively killed off during the lifetime of the next Government.
All of this is very awkward. If the bacon-butty haters are onto something, Ed Miliband (@Ed_Miliband) won’t be in the next Prime Minister after all that. And we could see the privatisation of the National Health Service receive atomic rocket boosters.
You won’t get whole person care either. The decline in social care inevitably will reach apocalyptic proportions.
And yet on the coalface we’ve got Jos Bell (@jos21), Chair of the Socialist Health Association London division, actively campaigning. Here is her excellent interview on LBC.
This was shortly followed by Andy Slaughter (@hammersmithandy), elected as the MP for Hammersmith in 2010.
With the lack of reporting on the NHS on the BBC at all-time new lows. there will inevitably be a lot of benefit in campaigning from those who are savvy with the social media. But I don’t think the battle for the soul of the NHS will be won on the pages of the Guardian newspaper, either.
If certain “campaigners” spent less time writing voluminous emails and documents which go nowhere, and learnt how to use Twitter instead, this would help the cause immensely. Éoin Clarke (@DrEoinCl) in a relatively short space of time has gained a massive following, and his observations are highly influential – much more so than the official press office of Labour, some might say.
Gabriel Scally (@GabrielScally) has been tireless in myth busting on Twitter. Kailash Chand (@KailashChandOBE) is personally a very supportive bloke, in addition to producing a prolific output of articles, in for example Pulse or GP magazine. Both are not ‘terrified of Twitter’.
And the superb Shadow Secretary of State for Health – Andy Burnham (@andyburnhammp) and the outstanding Labour Health Team (@LabourHealth) are leading by example.
The Shadow Minister for Care and Older People is Liz Kendall (@leicesterliz) and is highly influential too.
Jamie Reed (@jreedmp), Debbie Abrahams (Debbie_Abrahams), Andrew Gwynne (@gwynnemp), and Luciana Berger (@lucianaberger), are all in the front guard too.
Dr David Wrigley is an outstanding campaigner (@DavidGWrigley); and for another inside view from the profession, a great blog and twitter timeline are from Dr Jonathon Tomlinson (@mellojonny).
They all tweet even when the going gets tough.
@LabourPress is a great way to catch up with key speeches by leading members of @UKLabour nationally.
You will find few truer advocates of the #saveourNHS campaign than Grahame Morris (@grahamemorris), Chair of @LabourLeft, and MP for Easington. Grahame is always polite, fair and precise in his questioning for the House of Commons Health Select Committee. Possibly a future Chairman of this committee?
Tweeters can only ignore @Jeremy_Twunt at their peril. No cruelty in his compassion. Never knowingly behind a tree.
There’s a battle still to be won, if you’re up for it.
Could the “social impact bond” help to improve services in dementia care?
This blogpost first appeared on the ‘Living well with dementia’ blog yesterday.
It’s impossible to ignore the occasional spate of reports of ‘care home scandals’, including Winterbourne View and Orchid View.
Whilst a direction of travel might be to advance people living ‘successfully’ as long as possible independently, there’ll be some people for whom a care home might be appropriate. There are particular aims of policy designed to support living well with dementia, such as combating loneliness and providing meaningful leisure activities, which can possibly be achieved through high quality care homes.
It’s pretty often that you hear of social care being “on its knees”, due to drastic chronic underfunding. A concern about attracting investment from the private sector is that this will help to accelerate the lack of financial resource allocation from the State. And yet this is the opposite to the argument of resources ‘leeching’ out of the public sector into the private sector.
In terms of the ‘business model’, there are concerns that, to maximise shareholder dividend, staff will not be incentivised to ‘care well’, if they are barely meeting the requirements of the national minimum wage. Whilst the employer emphasises ‘flexibility’ of zero hours contracts, for many such contracts are symbolic of a lack of commitment for sustained employment by the employer.
So the idea of bonds being used to prop up dementia care, currently one of the three big arms of the Prime Minister’s Dementia Challenge, has gained some momentum, for example here. Bonds are effectively “IOUs“, and concerns remain for them as in the private finance initiative – such as who actually benefits, the prolonged threat of penalty for not being able to meet your loan repayments, the issue of who decides the outcomes by which performance will be assessed, and who actually manages or controls the enterprise.
Social Impact Bonds (SIBs) are depicted as “a way of enabling innovation, creating flexible contracts around social outcomes and providing linked investment“. But for some, they are a vehicle for enabling ‘privatisation by stealth’.
The current Labour opposition officially is trying to distance itself from any mechanisms promoting the privatisation of the NHS, and yet it is known Chris Ham and Norman Lamb wish to publish a report imminently on the possible use of SIBs in policy under the auspices of the King’s Fund.
This is the title slide of Hazel Blears’ presentation for the Alzheimer’s Show on Friday.
And here is a section of her talk.
[apologies for the sound quality]
Hazel has a strong personal attachment to campaigning on dementia, and is particularly interested and influential in the direction of travel, not least in her rôle as Vice Chair of the All Party Parliamentary Group on dementia, a cross party group made up of MPs and Peers with an interest in dementia.
Andy Burnham MP, Shadow Secretary of State for Health, has made it clear that it is his firm and settled intention to repeal the Health and Social Care Act (2012). The current Prime Minister’s Dementia Challenge is to come to an end officially in March 2015.
Dementia UK set up some time ago its innovative ‘Admiral Nurses’ scheme, to provide specialist nurses who could help people with dementia and family carers to improve the quality of life of people with dementia and family carers.
Burnham has also let it be known that he intends to subsume social care within the NHS under the construct of ‘whole person care’. Whichever various formulations of ‘whole person care’ you look at, you tend to find a ‘care coordinator’ somewhere. The exact job description of the care coordinator, nor indeed which specialisms might be best suited to accomplish this rôle, is somewhat unclear presently.
But it is all too common to hear of people being diagnosed with dementia being ‘lost in the system’, sometimes for years without follow up.
A “care coordinator” might help to boost access to the following services: emotional support, enable short breaks for people with dementia and anyone in a caring role, promote nutritious meals, ensure medications are given on time, ensure the correct medications have been subscribed (for example avoiding antipsychotic medications in individuals who might be unsuited to these), advice about suitable housing (including downsizing), ensure all physical commodities are properly medically managed; and so the list goes on.
I feel it’s pretty likely there’ll be a ‘first mover advantage‘ effect for any entity which takes up this coordination rôle in dementia care. But the tension between this and the Opposition’s policy is palpable: one cannot talk of this entity being ‘the first to enter the market’, as many wish (and expect) Labour to abolish the internal market in health care.
Such a coordinating entity could well be a recipient of a SIB – but is this like the PFI of social care? PFI by and large has an incredibly negative press amongst members of the general public.
But on the other hand, is it vindictive to prevent a social enterprise from pitching from such a service? If that entity has the technical ‘know how’ to run operations nationally competently and at a reasonable price, would that be preferable to the State running such services when projects such as NHS IT and universal credit have not gone terribly well?
In our jurisdiction, private companies can hide easily being a corporate veil, and are for example currently not readily accountable through freedom of information legislation. This is despite numerous requests to Jeremy Hunt in parliament about parity in disclosure requirements from both private and public providers.
And the track record of some outsourcing companies in the private sector, it is said, has been terrible.
Jeremy Hunt and Norman Lamb are currently in control of NHS and care policy, but there might be a fundamental change in direction from the next Government.
Or there might not be.
Campaigners – your NHS needs you!
Andy Burnham MP recently commented,
“David Cameron used to say that his priority could be summed up in three letters: NHS. Now, it seems, he prefers not to talk about it. The word in Westminster is that, on the advice of Lynton Crosby, the Prime Minister has asked his ministers for a period of pre-election silence on the NHS. So the Queen’s Speech came and went without even a mention of Mr Cameron’s erstwhile priority.”
The NHS says 299,031 patients arrived at A&E departments last week – the highest number on record.
The NHS is set to be a key battleground at the general election and Labour intends to keep it at the forefront of the public mind in the coming months. The plan is now it will use a private member’s bill to lay out how it would repeal the coalition government’s controversial Health and Social Care Act (2012), which had a number of after shocks.
The bill, proposed by Clive Efford MP, would rewrite the rules that put competitive market tendering of services as the default option until proven otherwise. It will be debated in the Commons in November and Labour candidates in marginal seats will call on Tory and Lib Dem incumbents to back the bill, while highlighting examples of how current rules waste money and fragment care.
In fact, this legislative manoeuvre is necessary whichever party comes to power on May 8th 2015. The current legislative framework makes it very difficult for services to be commissioned which promote integration, for fear of breaching competition regulation.
The Shadow health secretary claimed the vote on the bill would “without doubt be the defining moment of what remains of this parliament”.
This private member’s bill is designed, presumably, to keep the NHS on the political and news agenda. Given the blanket reluctance of the BBC to discuss this £3bn re-disorganisation, campaigners will mainly have to resort to the social media to get their message across.
The bill is also designed to drive a wedge between the Conservatives and the Liberal Democrats. At some stage before the general election on May 7th 2015, the Liberal Democrats might wish to distance themselves from the current Conservative policy. It is nonetheless noteworthy that Paul Burstow remains adamant that opposition to hospitals suddenly closing from Labour will not work in the long run.
The Liberal Democrats, to put it simply, need this ‘differentiation strategy’ to survive. Otherwise, it will be completely annihilated as a political force. The Liberal Democrats were instrumental in getting the Lansley Act onto the statute books in both the lower and upper houses. The concept of them repealing their own legislation in a coalition after 2015 is completely unacceptable for many in the Labour Party.
And there is plenty that all NHS campaigners can unite upon, whatever political creed.
First and foremost, it would be motherhood and apple pie for the duty of the Secretary of State for Health for the National Health Service to be restored.
Secondly, it is likely that Labour will wish to see the increase in the ‘private patient income cap’ abolished. I have written about it in great detail here.
The current situation regarding the “private patient income cap” (more correctly an “income cap for non-NHS work“) in the Health and Social Care Act, through s. 164(1)(2A), is described as follows:
An NHS foundation trust does not fulfil its principal purpose unless, in each financial year, its total income from the provision of goods and services for the purposes of the health service in England is greater than its total income from the provision of goods and services for any other purposes.
In an interesting development reported this morning, hospitals are to be banned from charging patients up to £72 a day to park their cars under plans being drawn up by ministers. It is reported that some hospitals charge up to £4 an hour – and in some areas £72 per day – for parking spaces, with costs running to hundreds of pounds for those who make repeated visits for treatment.
It is also claimed that the worse-affected include cancer patients who cannot take public transport because they have reduced levels of immunity, and the parents of premature babies, whose children are often kept in hospital for several weeks.
The abolition of this lifting of the income cap for non-NHS work would go far wider than the Coalition’s targeted strike on car park charges.
A grave concern has been that competition rules ‘hold back quality‘. I first wrote about this at the beginning of January 2013 on this blog. The provision (“section 75″) puts rocket boosters into aggressive pimping of NHS services in the private sector, and the rest as they say was history.
In October 2013, it was reported that two NHS hospital trusts in Dorset would not merge on the basis of clinical need, according to the Competition Commission, an economic regulator overseeing the implementation of competition law applying to this country.
Whilst Jeremy Hunt never mentions the Lansley Act, there’s no doubt that Labour will wish to repeal it in the first Queen’s Speech of a Labour government. It appears to have appeared to have come from nowhere, though a very good description of how it came about comes from Matthew d’Ancona’s outstanding “In it together” and Nick Timmins’ outstanding “Never again”.
It’s undoubtedly a turgid piece of law, which reads like a patchwork quilt of commercial and corporate law relating to competition, regulation and insolvency. There’s only clause on patient safety, and that enables the abolition of the National Patient Safety Agency. In fact, the Draft Bill on regulation of clinical professionals, proposed by the English Law Commission, thought to be a landmark piece of legislation to promote patient safety, has been bounced into the lifetime of the next parliament.
Despite its length, the Lansley Act has three clear aims: firstly, to outsource NHS services into the private sector as easily as possibly, to bolster the functions of an economic regulator (“Monitor”), and to accelerate the managed decline of NHS units which run into financial trouble. It is indeed a result of a need to ‘liberalise the NHS market’, but as Iceland found out in their large experiment of deregulating the banks, the Lansley Act experiment may be just about to go horribly wrong. NHS campaigners, if they unite, can help to seal its fate.
Fighting each other on the left is a waste of resources
We keep on being told that there is a finite amount of resources to share. So why on the left are we not channeling our energy into things we care about?
Among the various things I have been witness to in the last year have been endless discussions on procedure and constitution. Such discussions while possibly well intended by some have virtually ended up being circular and being presented in summary in an incredibly unimpressive manner.
There are serious matters afoot. There was a draft Bill proposed by the Law Commission, which didn’t make it into the Queen’s Speech, on the regulation of clinical professionals. This promises to be a landmark piece of legislation, and has now been bounced into the next parliament’s lifetime. Clearly this Bill will prioritise patient safety, on which there was not a single clause in the Health and Social Care Act (2012) apart from abolition of the National Patient Safety Agency.
Many of us have allowed the narrative to be articulated in terms of ‘sustainability’, in other words we can’t afford the National Health Service – but curiously can afford war, and afford a lengthy inquiry into the legality of it. We have allowed a ‘there is no alternative’ closure of ‘failing’ hospitals, but have not addressed the principal issue of how clinicians and patients can be in charge of their own services without a firestorm by the Trust Special Administrator.
We have lost time on how we can make the health service function nationally, not in a piecemeal fragmented way like the privatised railway industry. We have lost time on implementing serious methods of keeping vulnerable frail patients out of hospital, or people living with dementia, in cases where they’d be better off with some proactive intervention out of hospital.
It is simply impossible to have this sort of discussion of what the left wishes to do in terms of solidarity, justice, equity and equality, while certain people are at each other throats. Whilst I am not a big fan of Tony Blair by any stretch of the imagination, it cannot be said that the previous Labour administrations can be the root of all of the ills of the National Health Service.
Basic things being done well matter a lot to people, like seeing their local GP or being attend an A&E unit in a timely matter. Andy Burnham MP has a golden opportunity to make sure medical records are shared freely between one part of the health and care service with the other, to prevent reduplication and poor medical decision-making based on information asymmetry. There is a key chance to break down barriers between health and social care, so urgently need, for example, in my academic field of living well with dementia.
There are many people who are now publicly concerned about the effect of competition in English health policy. Margaret Heffernan, of ‘wilful blindness’ fame, is just about to have a bestseller on her hands on this subject.
So can we cut the incessant concerns about how the Labour Party is still a cover for corporate Britain? That Labour hasn’t learned anything from the past, which includes John Major activating the private finance initiative initially before badly negotiated contracts under the early years of the Blair administrations?
It is impossible to divorce the needs of physical and mental health of a person from social care needs. So we can we put a sock in the movement that integrated care of any variety can only be a Trojan Horse for privatisation? There is a possibility that a future Labour government might be able to provide a fully funded national care service, if there were a momentum of public support.
Labour’s position on personal health budgets (“PHBs”) for the last few years has been clear. Whilst there are noteworthy successes, there have been a plethora of concerns, including safeguarding issues for people with dementia. It was never intended that they should be compulsory, despite the subject of PHBs at all being promoted previously by some very senior in the Labour Party.
There’s a battle to be fought indeed, but the outcome of that battle should not a Conservative-UKIP coalition. You’ll find that they will not be the answer to all your concerns about the NHS.
As regards the NHS, Dave Cameron is also being a tad economical with the truth
We keep on being told from the right wing that “money does not grow on trees”, but the Chilcot Inquiry on the Iraq War has so far cost millions (the actual war was costly in many senses too.)
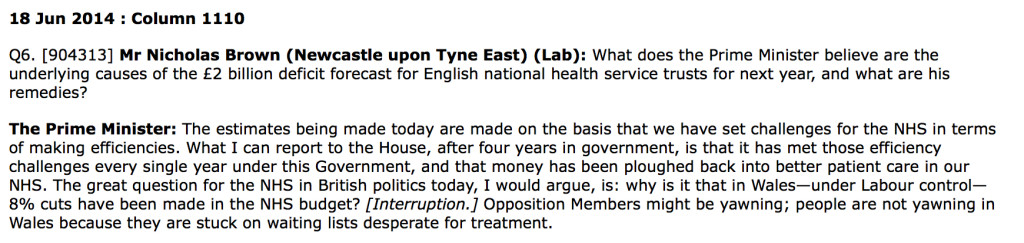
These are #pmqs from my 40th birthday.
Nick Brown MP asks the Prime Minister about the underlying causes of the £2bn forecast deficit for NHS Trusts, and what the remedies might be.
This topic hit the headlines big time yesterday, but it had been copiously discussed by John Appleby by the King’s Fund in one of their documents previously.
The exchange as reported in Hansard went as follows:-
Specifically, the Prime Minister contends that, “money has been ploughed back into better patient care in our NHS.”
This is likely to be true as a half-truth as he does not say “the” before the word “money”.
But where did the money actually go?
It appears it has traditionally gone to HM Treasury, NOT directly to the Department of Health budget.
Everyone knows that the pay settlement for the NHS was tight this year, given the pay freeze discussed at the #RCNCongress this year.
Crispin Dowler reported in the HSJ in October 2012:
“The Department of Health has returned nearly £3bn of its funding to the Treasury over the past two years, despite facing its tightest financial settlement for five decades.
“A Treasury spokesman this week confirmed to HSJ the department had handed back around £1bn of the funding it was allocated for health spending in 2011-12. Just £316m of the £1.4bn that the DH left unspent last financial year has been carried over for it to use in 2012-13.
“The final sum clawed back from last year’s health allocation is double the £500m estimate that was published in chancellor George Osborne’s March Budget.”
Sofia Lind in the Pulse magazine reports a similar story in 2013.
My brief Twitter chat yesterday with @DaveWWest went as follows.
about #NHS ‘efficiency savings’ 12.17 pm PM ‘..that money has been ploughed back into better patient care in the NHS’ true? @DaveWWest
— shibley (@legalaware) June 18, 2014
@legalaware largely paid for increased activity, so yes in a sense but you could point to the annual DH underspends til 13/14, which are not — Dave West (@Davewwest) June 18, 2014
@Davewwest Thanks Dave. I’ve never worked out where in fact the surplus goes – I had thought it goes back into HM Treasury not DoH.
— shibley (@legalaware) June 18, 2014
@legalaware yes you’re right — Dave West (@Davewwest) June 18, 2014
There did seem, however, to be a record number of questions on the NHS in #pmqs?
Dementia care in the whole person care age
The Australian jurisdiction have recently provided some helpful inroads here.
The narrative has changed from one of incessantly referring to people living with dementia as a ‘burden’ on the rest of society. For example, to push a sense of urgency that we have an ‘ageing population timebomb’, the cost of the ageing people with dementia flies completely in the face of other public health campaigns which emphasise, for example, “dementia is not a natural part of ageing”.
“The NHS as a whole and individual hospitals recognise that dementia is a significant, growing and costly problem for them” is the opening gambit of the Alzheimer’s Society “Counting the cost” report.
An easy to use online resource, Valuing People from Alzheimer’s Australia has been developed in collaboration with community aged care providers who have helpful in stablishing a person centred approach to service delivery.
Person centred care is a development to provide ervices provided in a way that is respectful of, and responsive to, the preferences, needs and values of people and those in the care and support network.
I cannot recommend this resource highly enough. The main source is here.
In fact, it summarises succinctly the conclusions I came to after my exploration of personhood in my book ‘Living well with dementia’. The late great Prof Tom Kitwood said of personhood, “It is a standing or status that is bestowed upon one human being, by others, in the context of relationship and social being. It implies recognition, respect and trust”.
If a Labour government is elected on May 8th 2015, the first necessary step is to legislate for the repeal of the Health and Social Care Act (2012) and to enact new legislation to allow for integrated packages provided they are justified by clinical outcome. For this to happen, it will be necessary for Labour to undergo a ‘conscious uncoupling’ from all the baggage of EU competition law. For this, it is essential also that the UK government is able to carve out provisions from the investor protection clauses and/or the rest of the EU-US free trade treaty (TTIP).
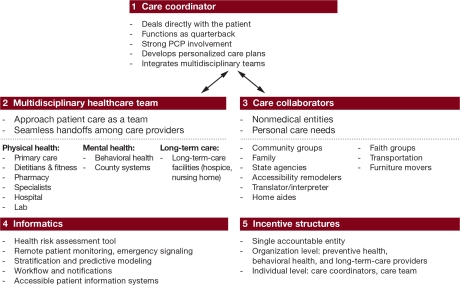
The “whole person care model” has become attractive to those who wish to break down silos between different physical health, mental health and social care “silos”. It has been worked up in various guises by various parties.
A helpful construct is provided in the document, “Healthcare for complex populations: the power of whole-person care models” originally published by Booz & Company in 2013.
A major problem with dementia care, however it is delivered, is that it is full of divisions: public vs private care, fragmented vs national care, competitive vs integrated models. Operating in silos can’t work because of the nature of the dementias: the mood and cognition of a person with dementia profoundly affects how they might interact with the outside world, for example perform activities in the outside world. And we know that taking part in leisure activities can promote a good quality of life.
Their model is, though, a useful starting point.
Dementia cannot be only addressed by the medical model. In fact, it is my sincere belief that it would be highly dangerous to put all your eggs in the physical health basket, without due attention to mental health or social care. For example, last week in Stockholm, the international conference on Parkinson’s disease, a condition typified by a resting tremor, rigidity and slowness of movement, which can progress to a dementia, often is found to have as heralding symptoms changes in cognition and mood.
So it’s pretty clear to me that we will have to embark on a system of multidisciplinary professionals who could all have a part to play in the wellbeing of a person with dementia, depending on his or her own stage in life, and ability or need to live independently. “Care coordinators” have traditionally been defined incredibly badly, but we do need such an identity to navigate people with dementia, and actors in the care and support network, through the maze.
“Care collaborators” in their construct are very wonkily articulated, like “pre-distribution”, but the concept is not stupid. In fact it is very good. One idea is that people with dementia could act as support as other people with dementia, for people on receiving a diagnosis of dementia. The rationale for this is that people living with long term conditions, such as for example recovery from alcoholism, often draw much support from other people living with other long term conditions, away from a medical model. There needs to be safeguards in the system to safeguard against a lot of unpaid goodwill (which currently exists in the system.)
Informatics would have a really helpful rôle here, being worked up in telecare and assistive technology. But even simple disruptions such as a person living with dementia at risk of falling from problems with spatial depth perception being able to ‘hot email’ a care coordinator about perceived problems could trigger, say, an early warning system. And with various agents in the provision of care being involved in differing extents it will be up to NHS England to work out how best to implement a single accountable tariff. Falls are just the sort of ‘outcome metric’ which could be used to determine whether this policy of ‘whole person care’ for people living with dementia is working. And, even though everyone ‘trots it out’, the performance on avoided hospital admissions could be put into the mixer. It’s already well recognised that people with dementia can become very disoriented in hospital, and, and despite the best efforts of those trying to improve the acute care pathway, people with dementia can often be better off away from hospital in the community. But it’s imperative that care in the community is not a second-rate service compared to secondary care, and proper resourcing of community whole person care is essential for this before any reconfiguration in acute hospital services.
But the private sector has become such a ‘bogey term’ after arguably the current Government overplayed their hand with the £3bn Act of parliament which turbo-boosted a transfer of resource allocation from the public to private sector. Any incoming government will have to be particularly sensitive to this, as this is a risk in strategy for the NHS.
In October 2005, Harold Sirkin, Perry Keenan and Alan Jackson published a highly influential article in the Harvard Business Review entitled “The hard side of change management“. Whilst much play has in fact been made of politicians having to be distant from running the NHS, a completely lubricous line of attack when it is alleged that Jeremy Hunt talks regularly to senior managers and regulators in the NHS, the benefits of clear political leadership from an incoming Labour government are clear.
Andy Burnham MP has already nailed his colours to the mast of ‘whole person care’ on various occasions, and it is clear that the success of this ambitious large scale transformation depends on clear leadership and teamwork from bright managers. Take for example the DICE criteria from Sirkin, Keenan and Jackson:
But this is perfectly possible from an incoming Government. The National Health Service has a chance to lead on something truly innovative, learning from the experience of other jurisdictions such as Australia and the USA.
As alluded to in the new resource from the Alzheimer’s Australia, this cultural change will require substantial ‘unfreezing’ from the current mindset for provision of care for people with dementia. It will require a change in explicit and implicit sources of knowledge and behaviours, and will need to be carefully brought about by learning from the successes and failures of pockets of implementation.
The whole project’s pretty high risk, but the rewards for people living with dementia, and members of the care and support network, are potentially vast. But it does require the implementation of a very clear vision.
[First posted on the 'Living well with dementia' blog]
Yesterday we broke the record for most views of the @SocialistHealth blog website
Here are the official figures for the most ‘viewed’ blogposts yesterday (15 June 2014).
It meant a lot to me having so much positive feedback from people in the #Twitter community on my blogpost which was the first time I’d blogged on my experiences of being a sick doctor in such a public forum.
I reproduce a sample of these tweets here.
It was a really big deal for me to write this, but I wrote it entirely spontaneously this morning. I’ve been churning around these issues every day of my life since waking up from my coma in 2007, and of course on #FathersDay it is impossible to ignore how awful it must have been for my late father.
@legalaware @TriciaHart26 @LisaSaysThis thanks for sharing I admire your struggle and your honesty thank you
— David Nicholson (@DavidNichols0n) June 15, 2014
@legalaware so honest, so transparent, reaching out to many with permission to speak up , weakness can be a true strength , sharing stories
— Tricia Hart (@TriciaHart26) June 15, 2014
@legalaware ….Thank-you Shibs…..always xxx
— Gerry (@archangelolill) June 15, 2014
@legalaware @WOWpetition Excellent blog that!
— Yvonne (@yvonneburko) June 15, 2014
@legalaware A difficult but excellent read Shibs-sharing such a private difficult experience in hope others will benefit-so generous. xxx
— Gerry (@archangelolill) June 15, 2014
@legalaware @archangelolill That was a v interesting, brave, honest piece and I am sure will help many – practitioners AND patients.
— Anne Booth (@Bridgeanne) June 15, 2014
@legalaware *Love* this piece Shibley, thanks for sharing. Will PHP become countrywide @clarercgp ?
— Andrea James (@HealthRegLawyer) June 15, 2014
Beautiful, heartfelt, insightful and searingly honest blog from @legalaware http://t.co/a8pEs18ChB do please read this
— Tim Lloyd-Yeates (@alivetim) June 15, 2014
Very powerful post by the wonderful @legalaware: My experience of being a sick Doctor http://t.co/HUa1HNARwN
— Jonathon Tomlinson (@mellojonny) June 15, 2014
@legalaware thanks for your inspiring piece and truth saying that is constantly needed. Oh and also your kind words!
— Michael Farrell (@MichaelFarrellE) June 15, 2014
@legalaware Love it! As always, u hv fab taste. Hope all ok? Am off 2 bed, v sore throat + lots on this wk #MyLast20Days @withoutstigma xxx
— Lisa Rodrigues (@LisaSaysThis) June 15, 2014
Insightful blog about being a sick doctor @legalaware http://t.co/yxsSUGBB7p See http://t.co/upUJ1lDq0r via @drphilhammond
— Lesley Russell Wolpe (@LRussellWolpe) June 15, 2014
Amazingly honest, insightful blog about being a sick doctor @legalaware ‘anything can happen to anyone at anytime http://t.co/1D01nMwOpY
— Dr Phil Hammond (@drphilhammond) June 15, 2014
@legalaware yes, I read it. I hope it gets the audience it deserves x
— Nicky Richmond (@lawyer_eats) June 15, 2014
@legalaware @deborahbowman @Jos21 @mason4233 @Dr_LEGO_Tom Incredibly moving and powerful Shibley – thank you for sharing — Jo Moriarty (@Aspirantdiva) June 15, 2014
@legalaware fantastic post thank you for sharing. Hopefully openness with help create understanding.
— Deborah Alsina (@DeborahAlsina) June 15, 2014
@legalaware @deborahbowman @Aspirantdiva @Jos21 @Dr_LEGO_Tom excellent Shibley, well done you — Chris Roberts (@mason4233) June 15, 2014
@juliewintrup @legalaware being content is the greatest gift you can offer others. Not everyone manages it! Thanks for sharing your story
— Dr. Lucia Gannon (@LuciaGannon) June 15, 2014
The five core messages of ‘Dementia Friends’ are consistent with the current literature
I first posted this blogpost on my ‘Living well with dementia‘ blog.
“Dementia Friends” is an initiative from the Alzheimer’s Society and Public Health England to raise awareness of the dementias amongst the general public.
Ideally, at the end of a ‘Dementia Friends’ session, each participant will have learned the five key things that everyone should know about dementia, and aspired to turn an understanding into a commitment to action.
In this blogpost, I wish just to discuss a little bit these messages in a way that is interesting. If you’re interested in finding out more about ‘Dementia Friends’, please go to their website. Whatever, I hope you become interested about the dementias, even if you are not already.
I’ve got nothing to do with writing ‘Dementia Friends’, but the following I reckon is a view which would be given by anyone like me who has worked in this academic field for a very long time.
Anyway, I do wish ‘Dementia Friends’ well, and I hope very much you will book yourself into an information session at the first available opportunity.
1. Dementia is not a natural part of aging.
This is an extremely important message.
However, it is known that the greatest known risk factor for dementias overall is increasing age. The majority of people with Alzheimer’s disease, typically manifest as problems in new learning and short term memory are indeed 65 and older.
But Alzheimer’s disease is not just a disease of old age. Up to 5 percent of people with the disease have early onset Alzheimer’s (also known as younger-onset), which often appears when someone is in their 40s or 50s.
[For a further discussion of this statement, please see another blogpost of mine.]
2. It is caused by diseases of the brain.
Prof John Hodges, who did the Foreword to my book, has written the current chapter on dementia in the Oxford Textbook of Medicine. He also supervised my Ph.D. The chapter is here.
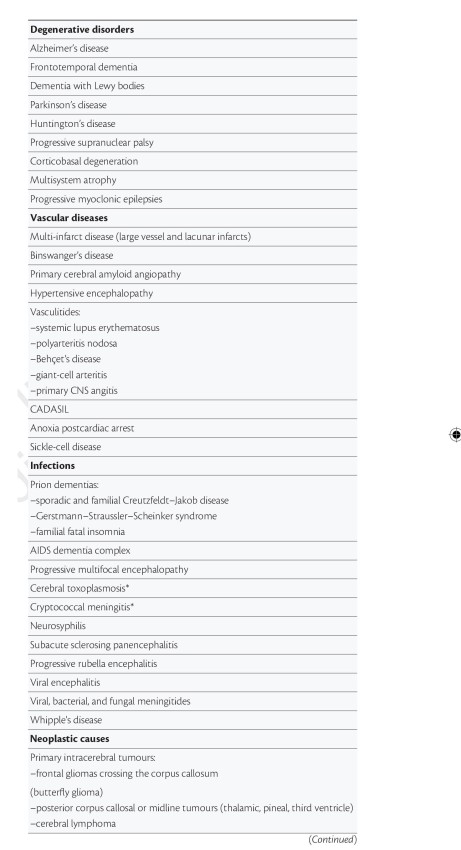
There is a huge number of causes of dementia.
The ‘qualifier’ on this statement is that the diseases affect the brain somehow to produce the problems in thinking. But dementia can occur in the context of conditions which affect the rest of the body too, such as syphilis or systematic lupus erythematosus (“SLE”).
[For a further discussion of this statement, please see another blogpost of mine.]
3. It’s not just about memory loss.
This statement is perhaps ambiguous.
“Not just” might be taken to imply that memory loss should be a part of the presenting symptoms of the dementia.
On the other hand, it might be taken to mean “the presentation can have nothing to do with memory loss”, which is an accurate statement given the current state of play.
John (Hodges) comments:
“The definition of dementia has evolved from one of progressive global intellectual deterioration to a syndrome consisting of progressive impairment in memory and at least one other cognitive deficit (aphasia, apraxia, agnosia, or disturbance in executive function) in the absence of another explanatory central nervous system disorder, depression, or delirium (according to the Diagnostic and Statistical Manual of Mental Disorders , 4th edition (DSM-IV)). Even this recent syndrome concept is becoming inadequate, as researchers and clinicians become more aware of the specific early cognitive profile associated with different dementia syndromes.”
I remember, as part of my own Ph.D. at the University of Cambridge on the behavioural variant of frontotemporal dementia,virtually all the persons with that specific dementia syndrome, in my study later published in the prestigious journal Brain, had plum-normal memory. In the most up to date global criteria for this syndrome, which should be in the hands of experts, memory is not even part of the six discriminating features of this syndrome as reported.
Exactly the same arguments hold for dementia syndromes which might be picked up through a subtle but robust problem with visual perception (e.g. posterior cortical atrophy) or in language (e.g. semantic dementia or progressive (non-) fluent aphasia, logopenic aphasia.) <- note that this is in the absence of a profound amnestic syndrome (substantial memory problems) as us cognitive neuropsychologists would put it.
[For a further discussion of this statement, please see another blogpost of mine.]
4. It’s possible to live well with dementia.
I of course passionately believe this, or I wouldn’t have written a book on it. It is, apart from all else potentially, the name of the current English dementia strategy.
[For a further discussion of this statement, please see another blogpost of mine.]
5. There is more to the person than the dementia.
This is an extremely important message. I sometimes feel that medics get totally lost in their own clinical diagnoses, backed up by a history, examination and relevant investigations; and they become focused on treating the diagnosis rather than the person with medications. But once you’ve met one person living with dementia, you’ve done exactly that. You’ve met only one person living with dementia. And it is impossible to generalise for what a person with Alzheimer’s disease at a certain age performs like. We need to get round to a more ‘whole person’ concept of the person, in not just recognising physical and mental health but social care and support needs, but realising that a person’s past will influence his present and future; and how he or she interacts with the environment will massively influence that.
[For a further discussion of this statement, please see another blogpost of mine.]