Home » NHS (Page 4)
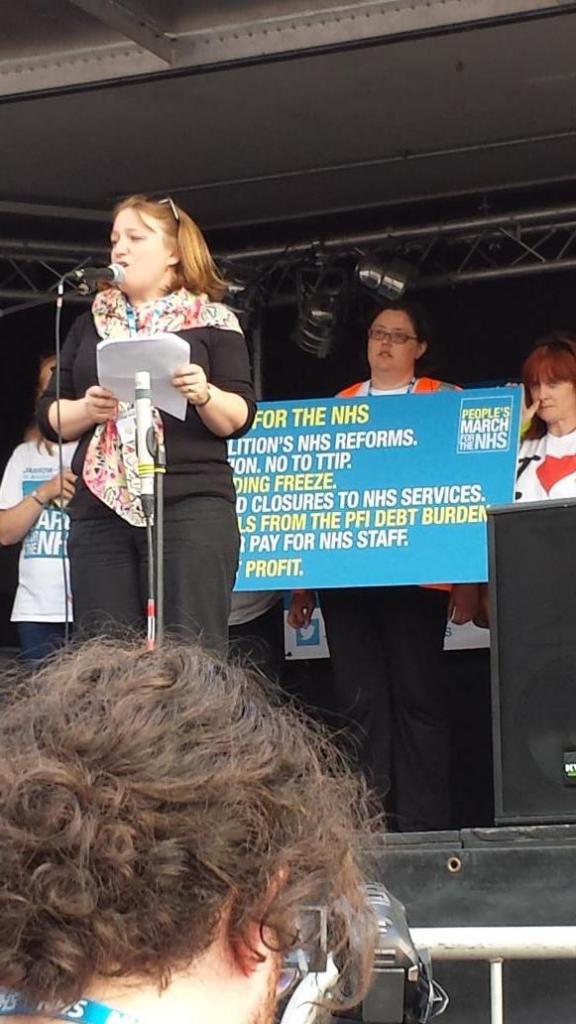
A triumph of optimism defeats cynicism as the Darlo Mums arrive in Trafalgar Square
The stench of sleaze from the backdoor lobbying culminating in the Health and Social Care Act (2012) was unable to overcome the sheer sense of euphoria and triumph of optimism defeating cynicism yesterday. Yesterday was history in the making, as all political parties were put on notice:
“Whose NHS is it? It’s our NHS”.
Whilst numerous governments have elaborated at length about the politics of ownership of public services, the message from the crowd of five thousand or so, within hearing distance of the Houses of Parliament, was loud and clear.
Many famous Labour members of parliament could be seen watching proceedings as the afternoon progressed, including Diane Abbot, Clive Efford, Jeremy Corbyn, Sadiq Khan, as pictured here.
It was a very sunny day here in Central London. There was a charged sense of energy, optimism and solidarity as about five thousand people attended a pro-NHS rally in Trafalgar Square, the culmination of a 300-mile march organised by a group of mothers from County Durham.
The group from Darlington, the Darlo Mums, are opposingthe privatisation of the NHS. It was very emotional when Rehana Azam announced the names of the Darlo Mums, “the most amazing people I’ve just spent the last three weeks with.”
The warmth of the #999CallfortheNHS campaign was evident throughout the whole afternoon. The event was immaculately organised, and was a thoroughly enjoyable event for all.
About 30 people had taken three weeks to march the full 300 miles from Jarrow in South Tyneside, organisers said.
Darlo Mums founder Joanna Adams said: “It’s been magic really. You only have to look over there [at the protesters gathered] to see people are behind the NHS and support what we’re saying. Joanna Adams described the mums as “ordinary”, but I beg to differ – they are entirely extraordinary in my opinion.
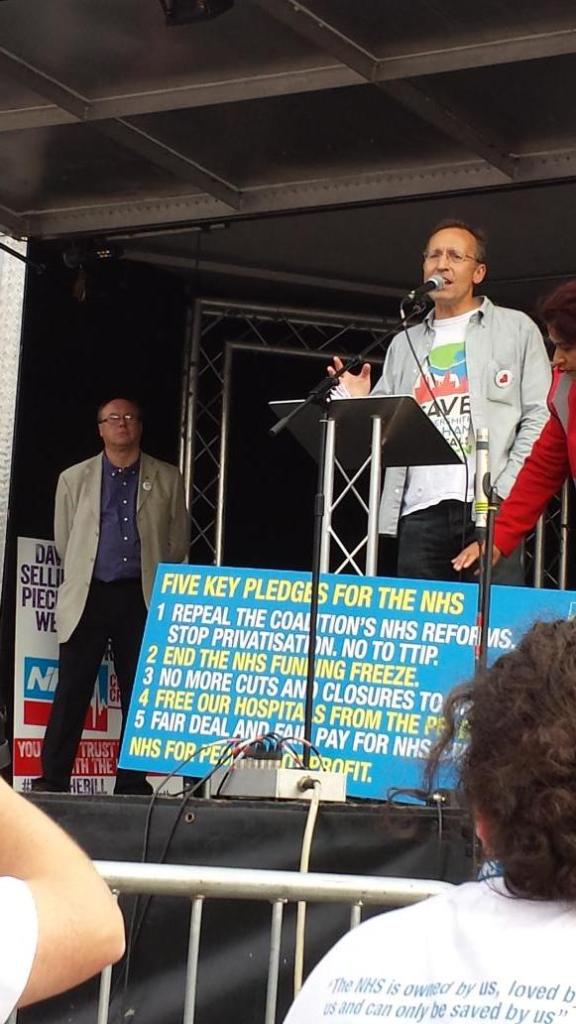
Andy Burnham MP, Shadow Secretary of State for Health, broke off all prior arrangements to attend, emphasising the indecency that would have occurred had he not come to represent the political party which had legislated for the birth of the NHS in 1945. Burnham’s speech was equally positive and optimistic about the future, speaking of the need to remedy public over privatisation, integration over fragmentation, people before profit, and collaboration over competition. Again, as is usual for Burnham who has great political gravitas, there was a sense of the current Government simply treading water in office until a person with substantial experience resumes office once again.
Burnham emphasised yet again that an incoming Labour government will repeal the Health and Social Care Act (2012) in its first Queen Speech, and said that it would then negotiate the UK out of TTIP, the transatlantic US-EU free trade treaty. Currently discussions are held in secret.
Sadiq Khan MP said the #Darlomums were the best England have had since 1966. As the MP for Tooting, Khan has been an ideal position to witness the effect the NHS changes have had on the nation’s capital.
Clive Efford MP described his Private Member’s Bill to repeal the damaging competition rules that the Tory-led Government inflicted on the NHS in its Health and Social Care Act 2012. The speech was very well received.
Even Dr Clive Peedell, Co-Chair of the NHS Action Party, called Andy Burnham’s speech “great”, having run 66 km himself to be there. It was announced that Dr Louise Irvine, an inner city GP and BMA council member, would be standing against Jeremy Hunt MP in the South West Surrey seat. Dr Peedell has of course seen at first hand the impact his specialty (oncology) has had on national politics, in the case of Aysha King.
And in the court of public opinion, according to the Daily Mirror last night, Dr Irvine was significantly more popular than Jeremy Hunt. We do know, of course, that the Daily Mirror do not comprise natural friends of Jeremy Hunt.
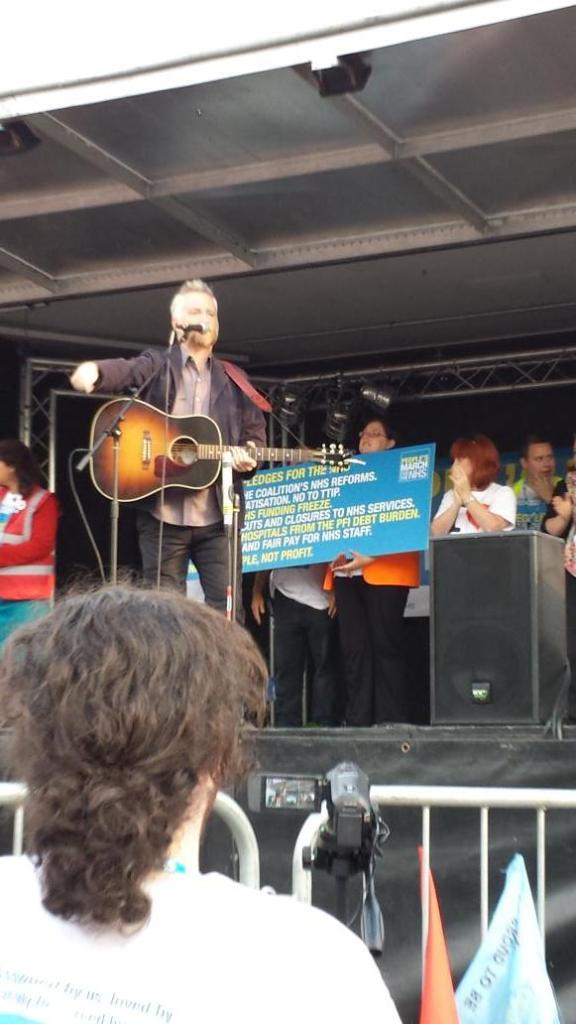
‘We keep on being told the NHS is unaffordable. THAT IS A LIE.”, said Rufus Hound. This lie has of course been one of the most powerful tools of the media who have called the consistent underfunding of services “unsustainable”.
Billy Bragg warned against blaming all cynicism on what one read in the media, saying that much cynicism was in people’s hearts – and this remained an obstacle for change.
Rehana Azam, as one of the marchers, NHS campaigner and leading light in GMB, and working mum, was one of the stars of yesterday’s event, explaining the necessary steps to get the NHS back on track.
Andy Slaughter, MP for Hammersmith and Fulham, recounted the demolition of his local NHS services, whilst Grahame Morris gave his account, as MP for Easington, of the fight against the Tories to protect the NHS. Andy Slaughter of course has a huge following in West London, and one of the key organisers of yesterday’s event Jos Bell was obviously pleased with the success of the event together with Andy Slaughter.
And finally, Question Musiq explained how he owes his life to the fast action of the Lewisham Hospital A&E in diagnosing his burst appendix, and performed his catchy rap song. Proceeds go to the Lewisham campaign.
A huge well done to everyone! A truly inspiring and memorable event.
Why the ‘999 March of the NHS’ is an important statement of democracy
There is no doubt that one should fight your battles to the hilt, but it is equally true that you should pick the right battles first. Two major battles to be had are whether NHS contracts should be aggressively pimped to the private sector, and whether the NHS should be up for sale to the highest international bidder. That is not to say that other battles are not important, but fighting these battles, I feel, will be able to tell us the future direction of travel of Labour. It’s well known that the political heart of Labour is possibly social democratic, but I feel that the ‘999 March for the NHS’ shows noteworthy twangs of democratic socialism, which has rather disparagingly been referred to as ‘left-wing populism’ previously elsewhere.
Getting Labour embroiled in a turf war over semantics I reckon is an infertile ground. The history of Labour and state ownership has long been a complicated one, as evidenced by previous Labour governments under Hugh Gaitskell and Tony Blair. When it was first established, the NHS was set up on the basis of social solidarity – everyone contributed to the cost of providing the NHS through taxes, and in return healthcare was provided by the state and available for those who needed it, when they needed it. This feeling of solidarity is indeed embed in the ‘999 Call for the NHS’.
The situation in 2014 is that rail fares are rising again, faster than average earnings. Whilst perhaps somewhat over egged, there is a genuine ‘cost of living crisis’ in England, with bills far outstripping real term wages. Employment for some is a very flimsy construct, being held together by a zero term contract. But it is true that, as under previous administrations, inequality is a problem in policy, and taxpayer subsidies are being diverted towards company profits and shareholders. Far from a smaller state, we have ended up with an unaccountable outsourced state. We have had the highest fares in Europe with profits extracted to pay shareholder dividends. In 2012/13 Northern Rail, Transpennine Express and Virgin alone paid almost £100m in dividends to shareholders after receiving over £1bn in public subsidy. Evidence shows that about £1bn per year is wasted due to privatisation, and if saved, this could fund an 18% cut in fares.
Why should the ‘People’s March for the NHS’ become so popular? Is it another example of “left-wing populism”? Left-wing populism is supposed to be a political ideology which combines left-wing politics and populist rhetoric and themes. Such a narrative normally consists of anti-elitist sentiments, opposition to the system and speaking for the “common people”, including themes of anti-capitalism, social justice, pacifism and anti-globalisation, whereas class society ideology or socialist theory is not as important as it is to traditional left-wing parties. The turbo-boosting of the privatisation of the NHS and the decimation of legal aid in England have therefore been good reasons for left-wing populism to gain momentum.
Robert Peston once famously asked, “Who runs Britain?” And looking at the recent elections to the House of Lords, one wonders how certain people get to such elevated heights of power. Meanwhile, Democratic socialists believe that both the economy and society should be run democratically—to meet public needs, not to make profits for a few. For a good such as water, where there is nothing to tell the difference between one brand of water and the next, it is hard to see how a privatised utility system is of benefit other than to corporate shareholders whether here or abroad. Democratic socialists do not want to create an all-powerful government bureaucracy, but likewise they do not want big corporate bureaucracies to control our society either. And some of the private providers in running public services, whether NHS, security, or probation, or otherwise, have been a disaster.
People often criticise Labour of having lost its roots. Indeed, it is hard to see how the most loyal Tony Blair critic should think of the Jarrow March as particularly Blairite? Jarrow is a small industrial town near to the southern mouth of the River Tyne, situated six miles east of the city of Newcastle. Despite the efforts of industrialist and Member of Parliament Sir John Jarvis, by September 1935, Jarrow had lost most of its heavy industry, and unemployment stood at 72.9%. The march was to find jobs to support Jarrow men and their families. It was also a bid for respect and recognition, not only for the people of Jarrow, but for others in a similar situation all over the country. The marchers had no resources other than their own determination, and some good boots supplied by the public. The irony about keeping wages stagnant in the NHS is that this is at a time when the country’s economy is supposedly improving, and when demand for the NHS is outstripping supply.
The People’s March for the NHS will arrive at its destination in London this Saturday, 6 September 2014, when campaigners will be joined by thousands of demonstrators for the final leg from Red Lion Square to Westminster. Started by a group of working mums from Darlington committed to stopping the privatisation of the NHS, the ‘999 Call for the NHS’ march left Jarrow on 16 August and has been winding down the country for the last three weeks following the route of the original Jarrow Crusade. The Chair of the London Socialist Health Association (@SocHealthLondon), Jos Bell (@jos21) has helped with some of the organisation over The final leg of the march, which will start at 2.30pm from Red Lion Square, Holborn, in London, with campaigners gathering from 1.45pm. There will be a rally in Trafalgar Square form 3.30pm with speakers including columnist and author Owen Jones. Further details can be found here.
But I feel that this march is much more than a publicity stunt or an item of ‘left populism’. It for me goes to the heart of a social democracy malaise gone wrong. It is indeed true that many northern European countries enjoy tremendous prosperity and relative economic equality as a result of policies pursued by social democratic parties. Social democratic parties supported strong labor movements that became central players in economic decision-making.
But globalisation of neoliberalism can be seen as a threat as well as an opportunity. With the globalisation of capitalism, the old social democratic model becomes ever harder to maintain. Stiff competition from low-wage labour markets in developing countries and the constant fear that industry will move to avoid taxes and strong labour regulations has diminished (but not eliminated) the ability of nations to launch necessary economic reform on their own. The idea of the NHS participating in this race to the bottom, where radiology opinions are outsourced in a disruptive manner to a foreign jurisdiction which we cannot easily regulate, strikes many people with fear.
Many have long felt that social democratic reform must now happen at the international level. Multinational corporations must be brought under democratic controls, and workers’ organising efforts must reach across borders. The European Commission is currently involved in negotiating a free trade arrangement of unprecedented scale between the US and European Union (EU). This is the Transatlantic Trade and Investment Partnership (or TTIP). The process is also undemocratic as the substance of on-going negotiations is largely kept from our MPs, MEPs, as well as the public. Once the treaty is signed by negotiators, the UK parliament, like other EU member states, will only be able to vote to accept or reject the treaty as a whole: they will not be able to amend it in any way.
Many believe that one of the biggest prizes of the agreement for transnationals will be the NHS. The Health and Social Care Act (2012) and the regulations for implementing it (Section 75) have changed the fundamental nature of the NHS. By fragmenting the NHS, opening it up to competition law and turning the NHS into a market in which private companies can compete for NHS funding for patient services, the Health and Social Care Act contains a toxic tool which can put profit before people, and lead to the piecemeal destruction of the NHS. Labour has pledged to repeal the Health and Social Care Act (2012), which of course they must do to avert the biggest sale of the century.
Identifying people who “might” have dementia is simply not good enough
Imagine you are a 45 year old lady who goes to see a GP with a lump on the breast.
Just pretend the lump on the breast is not a sinister cancer, but a small harmless fatty collection of fatty cells called a lipoma.
Would you appreciate that GP labelling you as having breast cancer because of a Government target to improve the number of diagnoses of breast cancer nationally?
Whilst it might be good for that GP ‘hitting the target’, the GP is certainly ‘missing the point’, as he or she has inadvertently given the patient much distress through the misdiagnosis.
In medicine of course you do not necessarily need to progress to a surgical biopsy to lead to a confident diagnosis. It happens that it is relatively most unusual for a diagnosis of dementia to warrant a neurosurgical brain biopsy unless it might be for a rarer condition such as Variant Creutzfeld Jacob, or a potentially treatable cerebral vasculitis (inflammation of the brain).
It is known that a sizeable minority of people we think have dementia do not actually turn out to have dementia on post mortem. Indeed, according to Professor Seth Love? Department of Neuropathology, University of Bristol Institute of Clinical Neurosciences, “In most published series, the accuracy of clinical diagnosis of the different diseases that cause dementia is of the order of 70–80%.”
The definitive diagnosis of dementia is achieved post mortem.
Whilst it is laudable that there is a strong drive to improve the diagnosis of rate of dementia in England, it is absolutely imperative that this diagnosis should be reliable. Otherwise the scenario arises where a 85 year-old man who lives on his own, recently widowed, suffering from profound clinical depression can inadvertently get mislabelled as having a dementia, and this diagnosis in itself makes him even more depressed.
In recent years, large corporate-acting charities have been largely responsible for touting the concept of identifying people ‘before they have the disease’, for example overweight people who are likely to develop type II diabetes. Likewise, in dementia, professionals have received massive pressure from non-professionals for finding that ‘pot of gold’ of people who most likely might develop dementia. Despite much obfuscation and smoke and mirrors, it is known reliably now that the ‘mild cognitive impairment’, of ‘minor’ dementia-like symptoms, is not that pot of gold, as many individuals with this condition never go onto develop dementia.
But having a roadside MOT in primary care has been argument popularised by large charities and politicians who have been successfully lobbied by them. Without adequate resources going into service provision or training of people in the service, this approach runs the risk of creating an unprecedented demand for people who are in fact ‘worried well’.
Robert Aronowitz (2009) argues that risk of disease and actually having the disease have become conflated.
“Imagine two women, one who is suffering from breast cancer and the second, “merely” at risk for the disease. The first woman is fifty-eight years old. Two years earlier, she detected a lump in her left breast. After an aspiration biopsy revealed cancerous cells, she had a lumpectomy and removal of lymph nodes in her armpit (none of which contained cancer), followed by a course of local radiation and then six months of chemotherapy. After this acute treatment, she was put on a five-year course of the “anti-estrogen” Tamoxifen. She now closely follows developments in breast cancer. At the moment, she is concerned about whether to start another kind of hormonal therapy after her course of Tamoxifen ends and whether she should begin getting screening breast MRIs and/or more frequent mammography. For these and other questions, she frequently searches the web and attends meetings of breast cancer survivor and advocacy groups.”
“The second woman also is fifty-eight years old. She took birth control pills during her twenties, had her first child at age thirty-four, and, at the urging of her gynecologist, took supplementary estrogen pills starting at age fifty because of menopausal symptoms and to prevent heart disease and osteoporosis. A few years later her doctor told her to stop taking these pills because new medical evidence had conclusively shown that their risks—especially an increased risk of developing breast cancer—outweighed their putative benefits. Since age forty, she has been getting annual mammograms. Four years ago, she had an abnormal mammogram, which led to an aspiration biopsy that did not show cancer. Fearful of developing breast cancer, she is attentive to media reports and periodically browses the Internet for new information on cancer prevention. She has seen direct-to-consumer advertisements for Tamoxifen as a preventive measure for women at high risk of breast cancer. She understands that she has multiple risk factors for breast cancer, such as being middle-aged, being postmenopausal, having had her first child after thirty, having earlier used hormone replacement therapy, and having a history of a benign breast biopsy. She has sought advice from friends, doctors, and breast cancer advocacy groups about whether to take Tamoxifen and/or to find other means of reducing her risk of breast cancer.”
“At present, the first woman does not experience any symptoms of cancer but nonetheless undergoes intensive surveillance, has concerns about the long-term effects of previous treatments, and faces the future with caution. The experience of the second women is not very different. She may well decide to take Tamoxifen to prevent breast cancer. Like the first woman, she undergoes frequent surveillance and faces the future with caution. Both women face an array of similar choices and seek guidance in similar places. They share fears for the future, feelings of randomness and uncertainty, and pressures for self-surveillance. Both seek ways to regain a sense of control and face difficult decisions about preventive treatment and consumption. They are part of a larger breast cancer continuum, both in how scientists understand breast cancer and as a mobilized group for advocacy, fund-raising, and awareness (Klawiter 2002).”
In dementia, people who might be ‘at risk’ are those with strong genetic risk factors, or have a particular constellation of risk factors (hypothetically food intake low in zinc or high in cholesterol etc.) Industries allied to medicine would love to open up new markets by finding these people and offering them treatments early on. However, the drugs currently used to treat Alzheimer’s disease only impact on symptoms for some for a short while, and there is no consistent robust evidence that they slow down the disease course in humans.
In October 2014, I will be presenting data in the Alzheimer’s Europe conference in Glasgow about how precise identification of people most likely to develop dementia will lead those people to have insurance premiums which go through the roof, in a private insurance system, compared to a system where we all pool risk in the National Health Service.
I blogged on this study originally here.
The direction of travel for dementia with influences from private industry is a malign one. It consists of actively seeking out people are who are yet to develop dementia at the risk of completely ignoring the needs of the current cohort of people trying to live well with dementia. The pharmaceutical companies have been spectacular in the minimisation of failures over the last few decades in therapeutic treatment of dementia, and the current case finding approach in the English national health service has the potential to produce as much distress as much benefit.
But people have been warning about major fault lines in our dementia policy, correctly, for some time. See, for example, the excellent work by Margaret McCartney and Martin Brunet.
We can’t go on like this. Identifying people who “might” have dementia is simply not good enough. A properly funded National Health Service, where we are all “in it together”, where the concerns of professionals are listened to as well as the spokesmen of the new ‘dementia economy’, is a necessary start. Besides, the service for post-diagnostic support for those individuals who have been correctly identified as having a dementia needs to be far better resourced and organised so that people don’t feel they are being sent from pillar to post.
It’s time Jeremy Hunt justified the costly NHS reforms rather than pontificated about hospital food
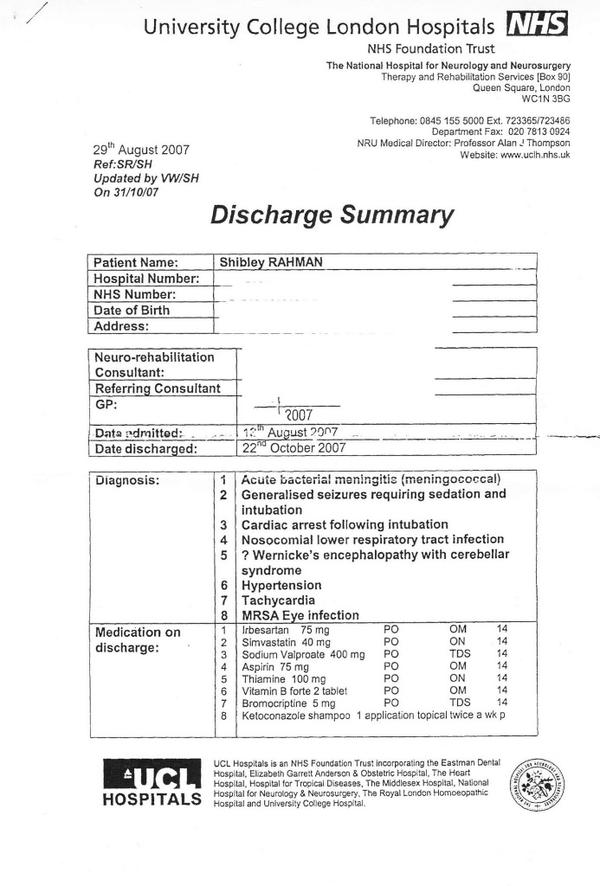
I remember my stay at the National Hospital for Neurology and Neurosurgery as an inpatient.
Actually, I don’t remember hospital food being that bad. In fact, I can’t remember it at all. When the physiotherapists were teaching me how to walk again, and the speech and language therapists were teaching me how to speak again, after my six weeks in a coma due to meningitis, the quality of food was not top of my mind.
What did irk me was pressing the bedside buzzer, and occasionally people not answering. Or not knowing when the ‘investigations’ which I was down for were due to happen.
But I suppose I understand why Jeremy Hunt focuses on hospital food. I would be surprised if he’d spent a lengthy stay in hospital as an inpatient. I know he never studied medicine or nursing.
But having a headline on hospital food is either some weird denial of problems in the rest of the service, or a genuine desire to promote the quality of nutrition in inpatients.
Either way, what is aggravating is Jeremy Hunt’s steadfast refusal to explain what the point of the NHS reforms was.
We know it cost about £2 billion, at a time when the UK is supposed to be tightening its belt.
We know it led to a large number of contracts being awarded to the private sector.
We also know there is not a single clause on patient safety in the Health and Social Care Act (2012), which amounts to about five hundred pages, apart from the abolition of the National Patient Safety Agency.
But Jeremy Hunt clearly does not want to discuss the NHS reforms, despite the fact that the Conservatives and Liberal Democrats were determined to get this legislation through parliament.
He needs to explain to the English voter in what way the NHS reforms have improved the quality of the patient experience. Did I miss a clause on hospital food in the Health and Social Care Act?
Otherwise, this is a lunatic Government with a detached Secretary of State for Health who seems completely incapable of explaining the current policy on the NHS.
Lynton Crosby may not want to talk about the NHS, but he may find that mission quite unachievable as a huge army of people converge upon Trafalgar Square for the climax of the modern-day Jarrow March.
It could be that Jeremy Hunt feels that the average voter is too stupid to discuss the privatisation of the NHS, but can cope instead with a conversation about the quality and quantity of chips in an average NHS meal.
People do not go to hospitals for a great hôtel like experience, in the same way that people do not stay in hotels to get their hernias seen to.
In the run up to the general election, the opposition parties should maintain pressure on the Government to explain quite why they were so desperate to implement the costly NHS reforms. These reforms not only cost a lot of money, but further extended the democratic deficit between political parties and the average voter. It is clear that Andy Burnham MP as Shadow Secretary of State for Health has maintained his wish to repeal the ‘Lansley Act’, but the current Government should not be allowed to get away with its wish to talk about Douglas Carswell or terror alerts rather than the current state of the health service, aided and abetted by supine media organisations.
Health and social care are ‘better together’, but a new government should still be cautious in delivery
Being cautious does not mean not changing things.
But for any change you have to take the key people with you.
For people who come into contact with the National Health Service or social care, the services are currently too bitty. It’s quite difficult to navigate your way through them.
There are further structural problems with how the service is organised for the NHS.
Ideally, there should be a consensus amongst members of political parties in doing something about the private finance initiative, or moving towards abolition of the purchaser-provider split?
Also, if ‘reconfigurations’ of NHS entities are deemed necessary, great thought should be put into the best clinically-driven as well as health economy method of doing so, involving meaningful engagement with persons and patients.
GPs, the backbone of the NHS, who are essential in providing a ‘proactive’ service for both health and illness, should not have their attention diverted into political attacks denigrating their value or into wondering whether their practices will have to shut.
With the default option now competitive tendering, this has generated a need for people who are savvy at making pitches and knowing the law. This is clearly a push of resources away from frontline care, the deliverers of which are expected to do ‘more for less’.
A brave Government will therefore have to organise better communication between the health and social care systems, and the person or patient.
It will also have to make technical adjustments to the law which currently puts competition law above clinical need (see for example the issue of mergers.)
Previous Governments in England have been great ‘reformers’, for example the Gladstone tenure.
Indeed, this Coalition inflicted a 493 page Act of parliament which had three aims: turbo boost a market, turbo boost getting rid of financially distressed hospitals, and pumping resources into an economic regulator.
This Act of parliament, accompanied by a £2 bn ‘reorganisation’, had nothing to do with patient safety. Indeed, the only clause in the Act acts to abolish the National Patient Safety Agency.
The new Government will have to be brave about funding.
For a Government of socialist flavour, this will mean avoiding at all costs compulsory personal budgets which are the shoo-horn for neoliberalism; and avoiding co-payments, which end up being a tax on the ill.
The focus of the new Government should be offering a pleasurable experience for any person using health and social care services, such that each member of the public is treated as an unique individual.
That individual is not merely a ‘collection of problems’, but has a past, present, and future, and interacts with his or her own social networks, community and environment.
The discussion to be had will at stage have to be a serious one, and there will be a need to engage the mainstream media in such a way that they evidently have had enthusiasm for (over Douglas Caswell, UKIP or Nigel Farage).
So the next Government is likely to introduce integrated or whole person care, but this should be clinically driven. Serious thought should be making each pound of healthcare spending go as far as possible, but ultimately there should be an acknowledgement that you get what you pay for.
And furthermore an ‘unsustainable’ NHS does not merely mean a NHS you wish to starve of adequate funds.
The NHS and social care systems do contain outstanding, hardworking professionals, and with the correct leadership the NHS can continue to be the ‘envy of the world’.
Hundreds of thousands of people are marching to London for September 6th to show just that.
Out of sight, out of mind
Please note: This blogpost has been edited since the first publication, due to a factual inaccuracy of mine this morning where I stated the Tavistock Clinic was private.
It is not private. I do sincerely apologise for this mixup. It was an entirely accident error of mine.
I have also changed the word ‘aggressive treatments’ to ‘thorough interventions’ on the advice of two different people.
I am further posting Kate’s very helpful comment below the end of this article.
I am extremely grateful to Kate for her comment.
________________________________________________________________________________________
I have previously written openly about my personal experiences as a sick doctor and beyond (please see here). Thank you if you were one of the 2000 or views of that blogpost on that particular day.
In 2008, the Department of Health under the previous government funded a two year pilot to commission and provide a specialist, confidential, service, the Practitioner Health Programme (PHP).
The service was free to all doctors and dentists in London with:
- mental health or addiction concern (at any level of severity); and,
- physical health concern (where that concern was potentially impacting on the practitioner’ performance).
The PHP complemented existing NHS GP, occupational health and specialist services. It demonstrated the need for the service (over 500 patients have now been treated, many with complex problems) and how savings could be achieved through swift, safe return to work.
The 2009 Boorman review of the health of the NHS workforce reported that:
- the direct costs of ill-health in NHS staff are in the region of £1.7 billion p.a.;
- the agency staff bill for the NHS is around £1.45 billion p.a. (spending closely related to sickness absence and staff turnover); and 2,500 ill-health retirements (some possibly preventable) each year cost the NHS £150m p.a.
The Chief Executive of the General Medical Council, Niall Dickson, commenting on the PHP said:
“We know of the stress and anguish experienced by doctors who become sick and how this can affect their work. There is not enough good support at local level and the PHP programme has shown what can be done.”
It is now pretty widely felt that prevention and early intervention could save the NHS millions of pounds, and employers can achieve huge savings by supporting doctors and ensuring they remain fit to practise, whilst maintaining or improving quality. The potential savings for employers far outweigh the likely cost of establishing a nationwide service (estimated at around £6 million). There is therefore a real economic case, as well as averting tragedies in human lives training in the NHS.
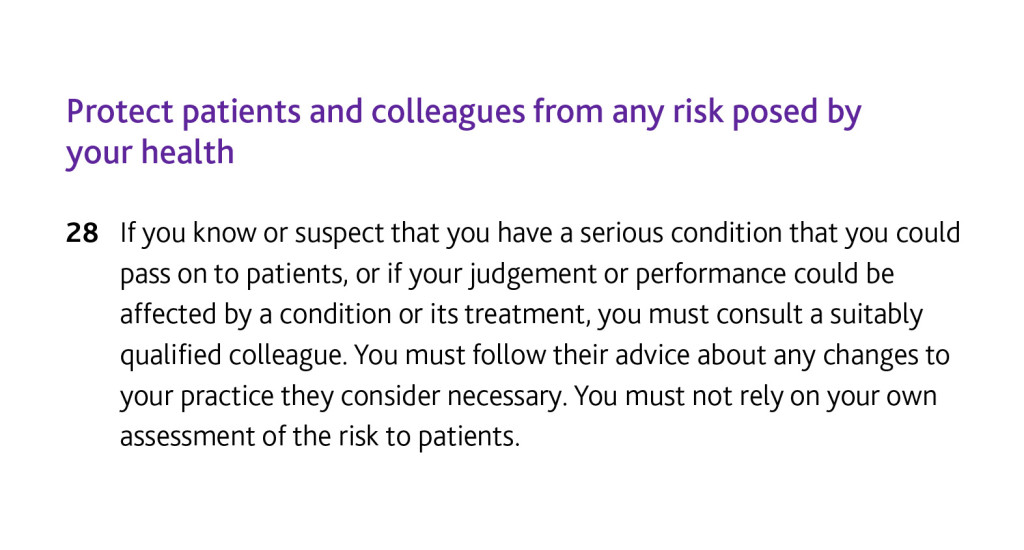
If you’re a sick Doctor, ‘Good medical practice’, the GMC’s code of conduct, is triggered under domain 2 for quality and safety by the following clause.
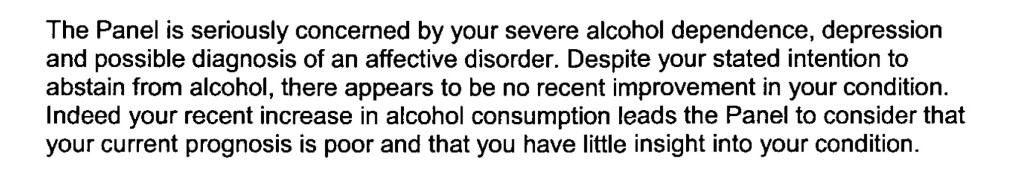
In my own particular case, it is recorded in two detailed witness statements that I tried to discuss in detail the alcohol problem that was concerning me with two Consultant Physicians in London.
In neither case was I offered a programme of alcohol management. I confided in them personal details.
It is a real pity that I did take up an offer by a Consultant who recommended the Tavistock Clinic, as I erroneously thought it was private not public. Notwithstanding that, no offer of sick leave was made, but that is my fault for not having let the discussion get that far.
But I really don’t wish to play any ‘blame game’ – for example I failed in not being under a General Practitioner at the time, as I was at that stage absolutely petrified that that GP would have reported me to the GMC subjecting me to years of investigation. I had years of investigation anyway, but without the critical help I needed.
Being under a General Practitioner for a medical professional is a requirement of their Code of Conduct according to rule thirty.
I think many aspects of my dire situation reflects a fundamental misunderstanding of the medical profession thinking that if a sick Doctor is ‘aware’ of his problem he has full insight into the distress the problem is causing to friends, family and beyond.
I feel that, had my problem been aggressively dealt with earlier, the subsequent failures in my alcohol management would not have occurred (three years later).
My erasure for me was perceived by me as the ultimate personal failure for having been through a public hearing, treated still in the media as a “show trial”, and a personal failure for not having got clinically better. On a note of wider contrition, however, I have no objection to the issues I was found proven to this day, and I think the GMC ultimately made the correct sanction.
Media reports, despite public humiliation, distressing not just for me but my late father at the time, make no reference to my underlying medical problems. I was sectioned in May 2006 due to alcoholism. It’s as if the establishment wishes purposefully to airbrush doctors being sick.
I was distraught on my erasure, for having no solution to my mental health problems in sight. The regulatory process exacerbated my misery, with psychiatrists not being able to rule out at anxiety and depressive component while I was heavily drinking.
I know I was ‘aware’ of my problem with empty drunk bottles of red wine, but it doesn’t mean that I had the motivation to take time off work then to do something about it.
Likewise, the GMC code (see clause twenty eight above) assumes that the sick Doctor has full insight.
In my case, it had a very unpleasant end.
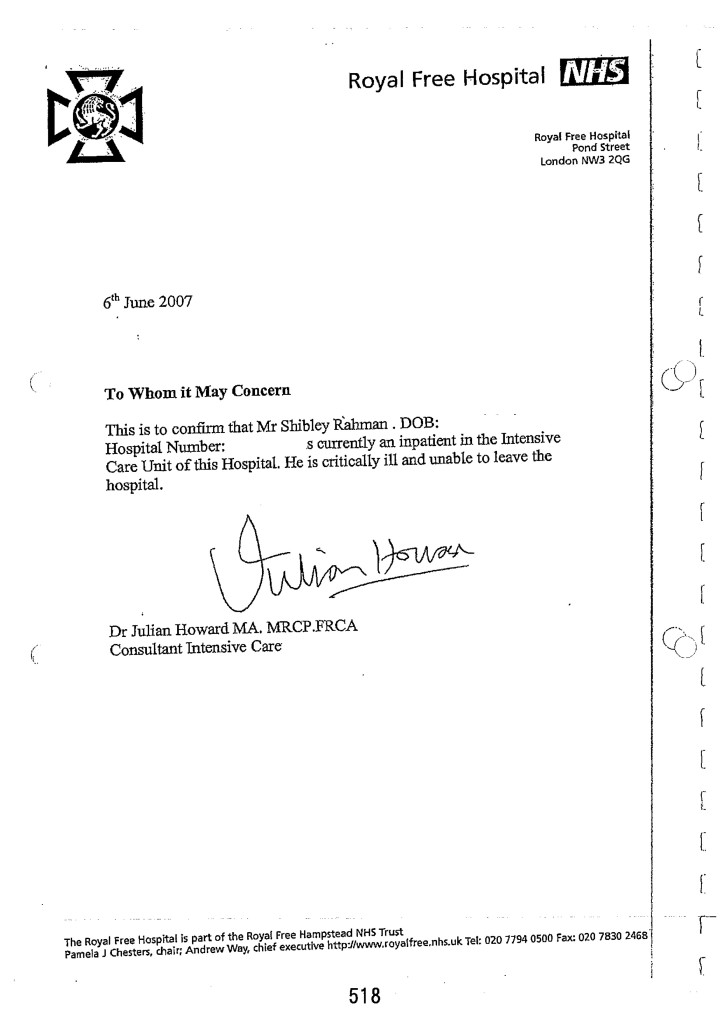
Not just this, days before my 33rd birthday,
but this six week coma and two month neurorehabilitation (the full discharge diagnosis from a place where I used to be a junior clinical physician once with no health problems.)
I think it is incredibly hard for anyone to understand outside of the system how you get raped of your dignity and integrity by the regulator when you fail to improve from mental illness. And often this mental illness is exacerbated by the regulatory process, as 86 deaths of Doctors awaiting Fitness to Practice during the same period of my investigation might appear to testify.
As I never had a performance assessment or clinical supervisor during my regulatory process, despite four different consultants concluding I had a severe alcohol problem at least between August 2004 and spring 2005, I feel I was put into managed decline long before the final hearing in July 2006.
I think personally the system for sick doctors undergoing the regulatory process from the General Medical Council could be much better, but that might be just be an unfortunate personal experience: ‘there’s nothing to see here’.
But a good first management step for me would be to roll out the Practitioner Health Programme to a jurisdiction wider than London. Lives truly depend on it, and the general public deserve better from seniors in the medical profession. This, for me, is absolutely necessary to maintain trust in the medical profession, domain 4 of the current GMC Code of Conduct. The GMC need to make the dealings open in this regard, fundamentally.
As far as the Consultants who contributed to my 2006 erasure were concerned, I have been out of sight and out of mind. In fact, I haven’t spoken to them for a decade and needless to say they have not wished to contact me.
I may be newly physically disabled following 2007.
I don’t personally wish the GMC any ill will. I believe in rehabilitation being a regulated student member of the law profession now – but do they?
I am back now.
Kate’s really helpful comment:
The Med Net service IS FREE and confidential.
When medical trainees encounter difficulties, college tutors, clinical tutors, programme directors and educational supervisors are encouraged to signpost them to Med Net. It was very positive that the consultant, who was not your educational supervisor, took sufficient pastoral interest in your welfare to give you the Med Net contact details. Ultimately, it is down to junior doctors to contact the service. Had you sought an appointment with your trusts OH team, they’d have given you the same contact details. It would have still been down to you to make contact. (< Indeed. Thanks , noted )
Alcohol-related disorders are outside the Mental Health Act, so it is impossible to compel people to undergo “treatment”. “Treatment” is an unfortunate term, as there is little that therapists can do until an individual wants help or becomes so incapacitated that they cease using. Even then, the notion of “treatment” as something that is done “to” people is inappropriate. This is one of the reasons why addictive disorders are outwith the MHA. Compulsion doesn’t work. “Aggressive treatment” is a particularly unhelpful concept more appropriate for the treatment of leukaemia rather than substance misuse disorders. Intense cycles of chemo-irradiation may induce remission in oncology, but intense input achieves nothing in addiction.
Kate then said it was a pity that I did not take up the offer of that Consultant, which I absolutely agree with.
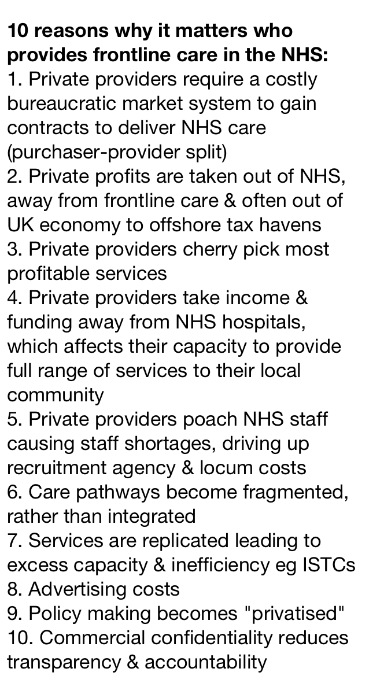
Why it matters who provides the NHS – from Dr Clive Peedell
This is a graphic from a tweet by @cpeedell, Dr Clive Peedell, Consultant Physician and co-leader of the National Health Action Party.
Source: https://twitter.com/cpeedell/status/500931152639975426/photo/1
Click on the picture to expand it.
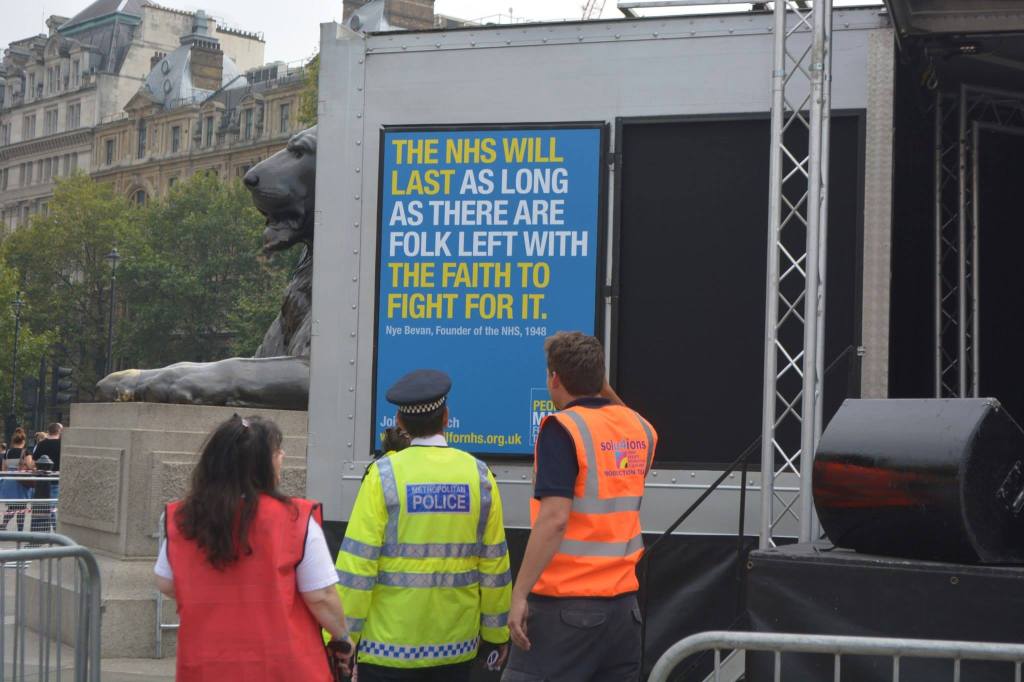
The NHS will last as long as there are folk left with the faith to fight for it
Aneurin Bevan, the Labour Health Minister who created the NHS, famously said: “The NHS will last as long as there are folk left with the faith to fight for it”.
On 16 August 2014 a group of mothers from County Durham will set off from Jarrow to march to the Houses of Parliament, following in the footsteps of those who marched the route in 1936 to protest against mass unemployment. They did this as a bold but peaceful protest against the current NHS policy.
Whilst the Government can clearly influence the State media, it might also be true that the NHS will last as long as there are folk left in the social media and also those willing to show their democratic stand against the undemocratic demolition of a publically-owned NHS.
That people care about NHS issues, for example, is shown by the enormous affection held by many for groups such as the “NHS Action Party” and “Keep our NHS Public”, as well as the trades unions.
There have been some Labour MPs, especially, who have served in an outstanding way to represent the views of their constituents and beyond over health and social care policy.
The lack of credibility from the Department of Health is demonstrated in their statements below:
The first statement read, “We’re committed to an NHS which continues to be free at the point of use for everyone who needs it.”
The critical thing for the next Government not to do, of whatever political variety, is to introduce compulsory unified personal budgets and a system of co-payments, as that will torpedo in an onslaught against the free-at-the-point-of-need principle.
It clearly is a problem if one part of the system which is means-tested is soldered onto another part which is not means-tested, like a dodgy banger.
The second statement read, “By taking tough financial decisions elsewhere, this government has been able to increase the NHS budget by £12.7 billion during this parliament.”
Last year, the UK Statistics Authority upheld a complaint by Labour about government claims the NHS budget had increased in real-terms in the past two years.
And members of the current Government keep on lying about this.
The current Government took the public for granted in inflicting on them a £1.5bn top down reorganisation, turbo-boosting the awarding of contracts to the private sector.
Lynton Crosby, PR guru of the Conservative Party, does not want to talk about the NHS, it appears.
But now it is clear that people should make clear what type of NHS they wish to have.
Furthermore, the next Labour government will be seeking to fuse the NHS and social care, and to pool their budgets. This will be a huge step, and could have massive implications for the national roll-out of a shift from hospital to community care to promote wellbeing and health rather than acute crisis management.
People who have had their local hospital services shut down will also have a chance to make their opinions known. It is well know that many people do not want a ‘platinum service’ miles away, if they do not have ready access to an emergency service on their doorstep.
These are indeed testing times for the NHS and social care, but Jeremy Hunt fails to command a leadership necessary to lead the NHS beyond 2015, many feel.
Politicians need to wipe the blood from their hands from liberalising the NHS
All the main political parties in England have “blood on their hands”, and we’re never going to get anywhere near the Chilcot Inquiry to sort out how it happened. The ‘weapons of mass destruction’ unleashed by corporate agents seeded everywhere in think tanks, media and politics have gone out of the way on a tirade of abuse against workers in the public sector. There are so many nexuses which have become uncoupled, that the NHS and social care systems no longer have anything like a situation approaching credibility.
Top CEOs in the NHS in England can still receive generous renumeration, even if their patient records are worse than the Black Hole of Calcutta. Even if multinational corporates do not perform adequately on a contract, the NHS does not have the legal know-how to ‘performance manage’ these contracts, and will not wish to spend the money. The NHS is scared of imposing any penalties, because of the powerful lawyers of multinational corporates. Above all, in addition to ‘patient safety’, that other secret weapon is used, namely ‘continuity of care’. Continuity of care is another chameleon wheeled out in a guise which suits its purpose at any one time.
Whilst the Blairites continue to espouse that it does not matter who is a Doctor at any one time, corporates are equally happy to use the legal stun gun of saying continuity of care will suffer if contracts are disrupted.One of the lessons from social care should have been that there are pockets of extremely poor social care, fragmented and expensive. As the next Government wishes to integrate care, with or without whole person care, one suspects that merging a means-tested system with one which isn’t will not be “no problem” as some senior health commentators have pretended. The idea that a self-directed budget where you pay for your service is “free at the point of use” is twisting the truth beyond all banality.
And these privatised contracts are neither accidental or insubstantial. One is a 10-year contract worth £1.2 billion for providing cancer services in Staffordshire, and there is also a five-year contract worth £800 million for the care of older people in Cambridge to last for the duration of the next Parliament. Both Labour and the Conservatives set in the present and previous administrations set the mood music for this, and politicians need to wipe the blood from their hands of the stains of neoliberalism. The new Jerusalem offered by private companies fraudulently (but legally) using the NHS logo has clearly run its course. Some in the UK Labour Party should be ashamed of itself for not articulating more clearly their opposition to such obscene onslaughts to the socialist founding principles of the NHS. The public clearly want a properly funded NHS. It is up to a credible party to provide that. Co-payments are a tax on the sick. Even “Pat” Hewitt, the doyenne of a previous Labour administrator, gave a speech to the London School of Economics in 2007 saying it would be madness to go down this route.
And some of the performance of companies to which the NHS has been outsourced is an insult to taxpayers, hardworking or not. Outsourcing giant Serco today announced plans to withdraw from the clinical health services market in a move precipitated by a multimillion pound loss on its NHS contracts. It is possible that Serco’s planned withdrawal could influence significantly how other private firms view the prospect of bidding for contracts involving patient facing services.
The group had already made an early exit from its contracts to provide Cornwall’s out of hours services and clinical services to Braintree Community Hospital.
Introduction of competition into the liberalised market generally has been a policy disaster of totemic proportions, producing sources of corporate fraud and misfeasance, a policy crowbar which can make mergers on the basis of clinical need unlawful, a mechanism for introducing substantial additional transaction costs, and a way of introducing private providers where profit goes into shareholders’ pockets not as surpluses in improving the service. Think tanks which aggressively pimped this have blood on their hands. And they will need to backpedal fast on their prostitution of the purchaser-provider split too.
Earlier this year, it was hailed as a success that the first private sector operator of an NHS hospital has halved its losses in the year to December. AIM-quoted Circle Holdings took over the running of Hinchingbrooke Hospital in Cambridgeshire in 2012 in a controversial part-privatisation. Private companies though wish to have their cake and eat it. They want to hide behind the cloak afforded by the Freedom of Information Act from Tony Blair’s reign. And why should the private providers get protection they haven’t earnt like a welfare claimant so despised by Iain Duncan Smith and Rachel Reeves? Private patients cannot complain to the Public Services Ombudsman for Wales unless they have received treatment commissioned and funded by the NHS. But the Welsh government has now said it has has no plans to bring private health providers within the ombudsman’s remit. Would the private sector like to contribute towards the education and training of the healthcare workforce?
This debacle from Serco, in fact, follows hot on the heels of news from Musgrove Hospital, Taunton, Somerset, where it turns out that dozens of people have been left with significant damage after undergoing operations provided by a private healthcare company at an NHS hospital. The routine cataract operations were carried out by the private provider, Vanguard Healthcare, in May to help to reduce a backlog at Musgrove Park. But the hospital’s contract with Vanguard Healthcare was terminated just a few days after thirty patients, most elderly and some frail, reported complications, including blurred vision and signs of inflammation including pain and swelling.
Laurence Vick, a medical negligence lawyer and the head of the clinical negligence team at Michelmores solicitors in Exeter, had been approached by some of the patients for whom there had clearly been a breakdown of a duty of care. Vick further said the case highlighted the “uneasy relationship” between the NHS and the private sector. He said the question of who paid – when outsourced NHS treatment – failed was of growing importance as more services were handed over to the private sector. This “uneasy relationship” which Vick refers to is likely to get massively worse as one cannot pin down who is legally accountable for failure for performance by subcontractors in “the prime contractor model”, where a main contractor can lead subcontracts for contracts say lasting ten years.
So Tony Blair was blatantly wrong: it does matter who provides NHS care. Blairites have unleashed ideological weapons of mass destruction on the Welfare State, and someone should pay the penalty for this. And it’s worse than that – you don’t know any more who’s in receipt of your taxes when you pay for what you think is the NHS. The Welfare State is being killed softly: and all English neoliberal parties have blood on their hands.
Polling firm ComRes recently found that 49% of people would be prepared to pay more tax to help fund the health service, one in three (33%) people said they would not be ready to do so, and 18% did not know either way. The public’s willingness to pay extra tax to help the NHS has reached its highest level in over a decade amid growing concern about hospitals slipping into the red, waiting lists lengthening and the service becoming unsustainable. The plan always was from the neoliberal advocates to produce a small state with low taxes, but what we have ended up is a moderate state with moderate-high taxes to fund the shareholder dividends of the outsourced companies in a range of sectors, including probation and health.
The Conservatives feel that their voters do not like ‘unfairness’ with one person obtaining an unfair advantage over another, but what we’ve got now is outsourced companies still be paid for unbelievably bad performance, and top CEOs in private providers experiencing a world nothing like their nursing counterparts in the NHS.
Labour will always try to woo the City all it wants, as per
But if disenfranchises hardworking nurses maintaining the fabric of the NHS, and brown nosing the City, it will find it does not get elected. And many socialists in Labour will not want to have blood on their hands in being part of Labour either. This because there is no obvious disinfectant yet.
All a far cry from the Spirit of ’45.