Home » 2014 (Page 2)
Yearly Archives: 2014
We need to talk about the NHS
I’m essentially in two minds about whether the NHS is ‘a political football’.
On the one hand, I don’t think it should be.
I felt the way Mid Staffs meant some hardworking staff in that region came to be pilloried and demonised by the media was more than indecent.
On the other hand, I think you can clearly apportion blame for the current Government’s performance about A&E waiting times and other key metrics.
On balance, I’d like Labour to have a strong majority to get through repeal of the Health and Social Care Act (2012), without say relying on the Liberal Democrats who enacted it in the first place.
There’s also important legislative work to be done in bringing together health and care; and also an Act of parliament to consolidate regulation of clinical professionals.
While I have much sympathy for NHS campaigners, I most certainly do not want a weak Tory-led Government because of incessant criticism of Labour.
There is a huge amount to discuss about the NHS.
I believe, for example, that the private finance initiative, whilst it had a useful aim in improving the infrastructure of buildings of the NHS, clearly did not represent value for money.
I don’t think it’s ever justifiable to bring in the private sector because the NHS can’t ‘cope’. I don’t see why you should want to bring in locums either, because of ‘unforeseen circumstances’.
And, in total agreement with Jackie Ashley at a fringe meeting of the Fabians this year, there needs to be had somewhere a discussion of how health and care sectors are to be properly funded.
There is almost universal agreement that the NHS cannot function at anywhere near its best with social care in such chaos.
I do blame a supine media for not allowing discussion of ‘whole person care’, or discussion of topics that even Labour would like to talk about (such as PFI; see Margaret Hodge’s remarks).
We’ve got some brilliant brains involved – Prof Allyson Pollock, whose brilliant analysis of PFI shines, has had some very pertinent points about the Clive Efford Bill with Peter Broderick. Yes, Andy Burnham MP does not support ISPS/TTIP, but this policy is still being left hanging in an uncomfortable way.
I am fundamentally a socialist, so I take the perspective that if we’ve got money for war we’ve got money for the health service. And I think with debt going through the roof, and with the economy being fuelled with insufficient till receipts, we are a long way from the energy which saw the NHS created in the first place from the spirit of ’45.
Whilst supporting Labour, I don’t wish this to descend into tribalistic nonsense. I will support anyone who has decided that the current performance of the NHS is unacceptable, but I have no intention of actively campaigning against Labour.
I personally wish to see policy for living well with dementia progress under Labour, irrespective of whether Ed Miliband can eat a chip butty.
Whatever, we certainly need there to be a public discourse about the NHS more than Europe or immigration, for example. Socialism is social-ism; if you want to see how collectively we can pull through, just look at the energy generated by Jon Swindon (here) or Eoin Clarke (here).
The importance of the ‘lived experience’ at the Alzheimer’s Disease International conference in 2015
This year, the Alzheimer’s Disease International under Marc Wortmann has done outstanding work.
It is known for its huge impact in allowing nation states to flourish with dementia strategies
Its output is phenomenal (see for example this latest paper). I have no doubt whatsoever ADI will continue to flourish under Glenn Rees, the incoming Chair (currently Chair Elect).
I’m still very excited about the 30th International Conference of Alzheimer’s Disease International “Care, Cure and the Dementia Experience – A Global Challenge” 15-18 April, Perth, Australia, next year.
People who are very close to me will be there.
It is, also, a lovely city.
The conference website is here.
It was always emphasised that this conference would showcase the lived experiences of people with dementia. People living with dementia and caregivers were indeed encouraged to attend.
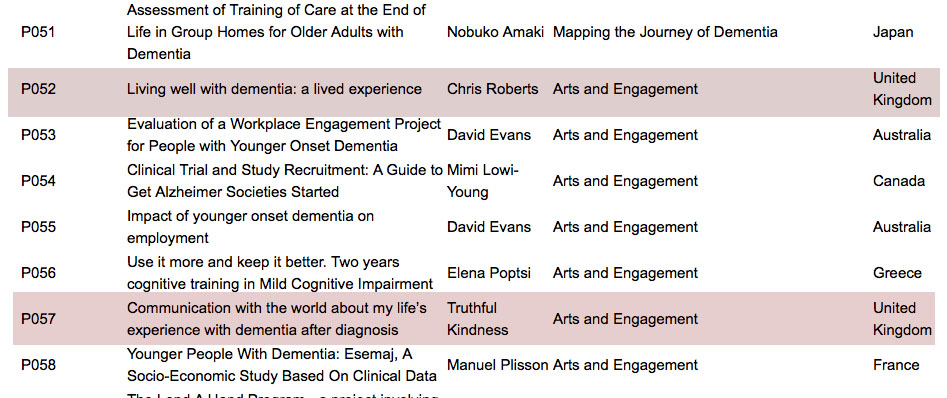
This is a part of the list of posters to be presented on Thursday 16 April 2014.
The two submitted by Chris Roberts and Truthful Kindness are shaded in a dark red.
The titles most clearly say ‘lived experience’ in the titles.
They were submitted as oral presentations, as the two people involved did not want them as poster presentations.
Indeed they did not opt for the ‘poster/oral’ option specifically for that reason.
P057
Communication with the world about my life’s experience with dementia after diagnosis
Truthful Kindness
Arts and Engagement
United Kingdom
P052
Living well with dementia: a lived experience
Chris Roberts
Arts and Engagement
United Kingdom
Truthful Kindness’ affiliation is Dementia Alliance International, Iowa; it was never submitted as United Kingdom. The irony about Truthful’s intended oral presentation is that she wished to explain how people with dementia can use all sorts of media to express themselves artistically and creatively. Arts and creativity is a huge policy plank in living well with dementia internationally.
It would have been clear to any diligent reviewer of these abstracts, from their submitted biographies, that both Chris and Truthful were genuinely living well with dementia.
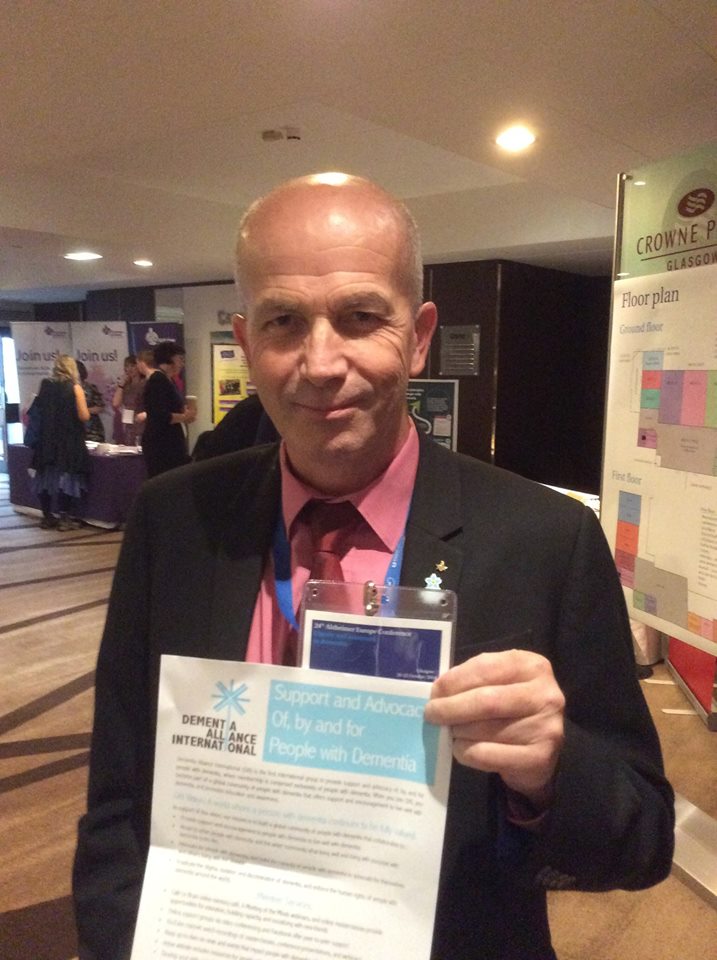
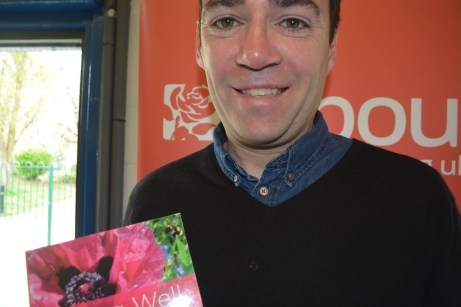
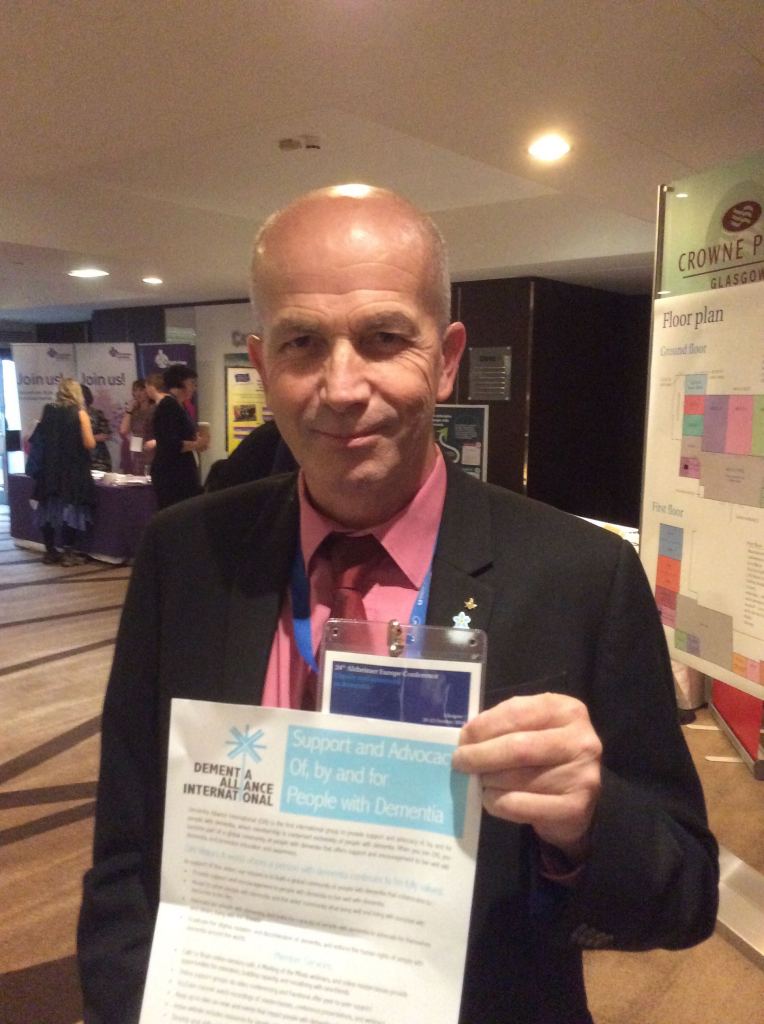
Here’s Chris even holding the flyer of the Dementia Alliance International group, at Glasgow earlier this year in the Alzheimer’s Europe conference on dignity and autonomy in dementia.
Chris is currently a Board member of the Dementia Alliance International.
I understand, from having spoken to one of the juniors at the Alzheimer’s Disease International, that there may even be a chance for poster presenters to give short oral presentations of their work. But I think this possibly may be worse.
It has been explained to me that the environment for the poster sessions is very off putting. It is a crowded room, with not much space for the poster itself. It is a very noisy environment, which is very distracting. In other words, this can be an environment which is potentially disadvantageous to people with early dementia who wish to present.
I am, of course, pleased that the keynote speakers for this conference include two friends of mine, and whom I admire massively, and who are living well with dementia, Kate Swaffer and Helga Rohra.
As is known, I consider Kate to be exceptional in every way.
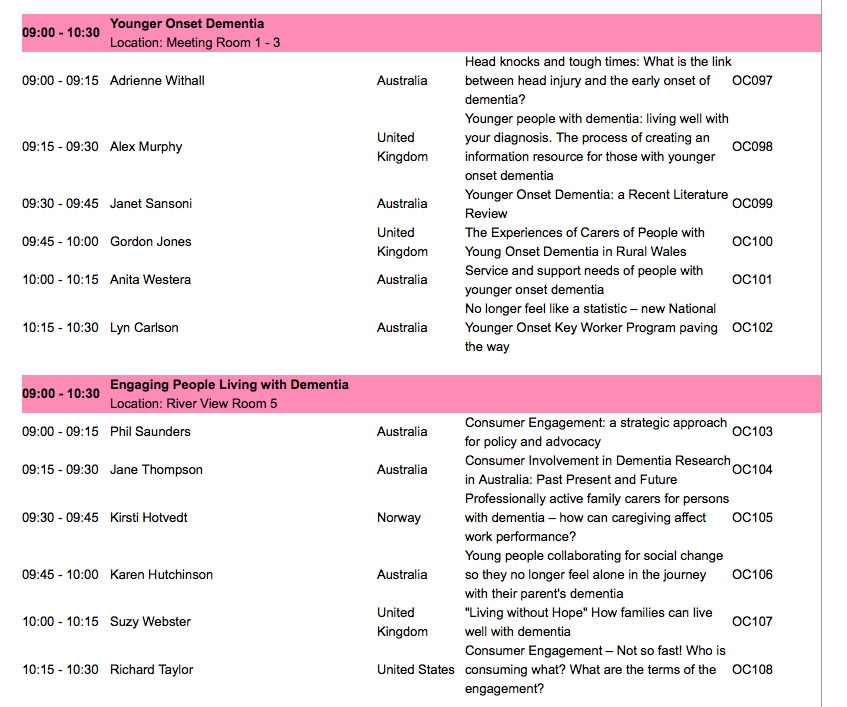
These are two symposia from the scientific programme in which they might have appeared: “younger onset dementia” and “engaging people living with dementia”. From eyeballing the titles of these talks, I don’t see many speakers talking about their own personal lived experiences.
The only parts of the conference yet to be revealed are the ‘workshops’.
The details of the workshops are given as follows:
Day 2 Dementia Friendly Communities
Day 2 “How to” topic to be confirmed
Day 3 Clinical trials
Day 3 “How to” topic to be confirmed
Day 3 Arts and dementia
Day 4 World Alzheimer’s month
Day 4 “How to” topic to be confirmed
I am extremely honoured to be on the international advisory board for the 2015 conference. I should therefore not want to criticise the organising committees in any way for their hard work.
But I cannot be a silent bystander to this either. The whole point about viewing dementia as a cognitive or behavioural disability secondary to a brain disease is that it then comes under international and domestic laws (for example, for UN Convention for people with disabilities and the Equality Act).
Ignoring two people’s wishes to have an oral presentation, as they cannot do poster presentations, is not making reasonable adjustments for their disability, one could easily argue.
I understand that the number of people with dementia fluctuates year on year, so it can be difficult to predict the number of people with dementia who wish to present. But, even with the limited number of places for the two symposia I have cited above, there doesn’t appear to me a big representation of people living well with dementia amongst the speakers, but I could be wrong. This also seems to be the case for other symposia, notably the one on “dementia friendly communities”?
I think the Alzheimer’s Disease International conference 2015 will turn out to be a brilliant opportunity for us to meet up; and we will also get a chance to discuss ‘cure’, ‘care’ and ‘living well’.
But Richard Taylor, living himself with a dementia, is right in his presentation from last year – where is the representation of evidence of psychosocial techniques?
I’d like to ask where is the evidence looking at ‘living well’, such as GPS trackers, design of wards, design of houses, the wider built environment, incontinence, eating well, assistive technology, ambient assisted living, advocacy, and so on?
On that note, I do strongly applaud the work of ‘Dementia Alliance International‘, which is truly representing the community of people living with dementia.
We hear words such as ‘challenge’ being used all the time in relation to dementia.
Hopefully the organisers will rise to the ‘challenge’ of living up to the reasonable expectations of those people with lived experiences wanting to take part fully in the ADI conference 2015 in a format they feel most comfortable with (and which makes reasonable adjustments if required).
A wellbeing economics prism to ‘dementia friendly communities’
There has been some startling consensus over the national political settlement, including as it applies to English dementia policy.
There has generally been cross-party agreement about personal budgets, even though the ‘direction of travel’ from the UK Labour Party is to favour a ‘rights based approach’ to advance choice and control rather than merely though a financial budget.
There are good reasons not to put many eggs into the personal budget basket for dementia; these include how the range of ‘products and services’ for dementia can be in places rather underdeveloped, and the formidable potential safeguarding issues for certain vulnerable individuals living with dementia.
Another consensus is to be found in wellbeing, or living well.
I was struck by a recent recommendation from the first ever report by the All Party Parliamentary Group on Wellbeing Economics, entitled “Wellbeing in four policy areas” (published September 2014):
“Health and Wellbeing Boards should bring together public health professionals, Clinical Commissioning Groups, GPs, and other stakeholders to develop strategies for ‘whole person care’ which effectively integrate mental and physical health.”
Unknown to me, they had been doing great work even prior to the last UK election. Their ultimate aim, unsurprisingly, is to make wellbeing into a pervasive policy strand that straddles across all areas of life.
This ‘wellbeing prism‘ has impacted on various areas of policy, I suspect, in the past, like ‘The Big Society’. I have always felt that the ‘dementia friendly communities’ policy in England, heralded in the Prime Minister Dementia Challenge, although clearly having some roots in the Japanese ‘caravans’ ‘befriending’, fits well into the ‘Big Society’ ethos.
One of the problems with both ‘dementia friendly communities’ and the ‘Big Society’ has been whether the civic sense of solidarity might diminish statutory obligations.
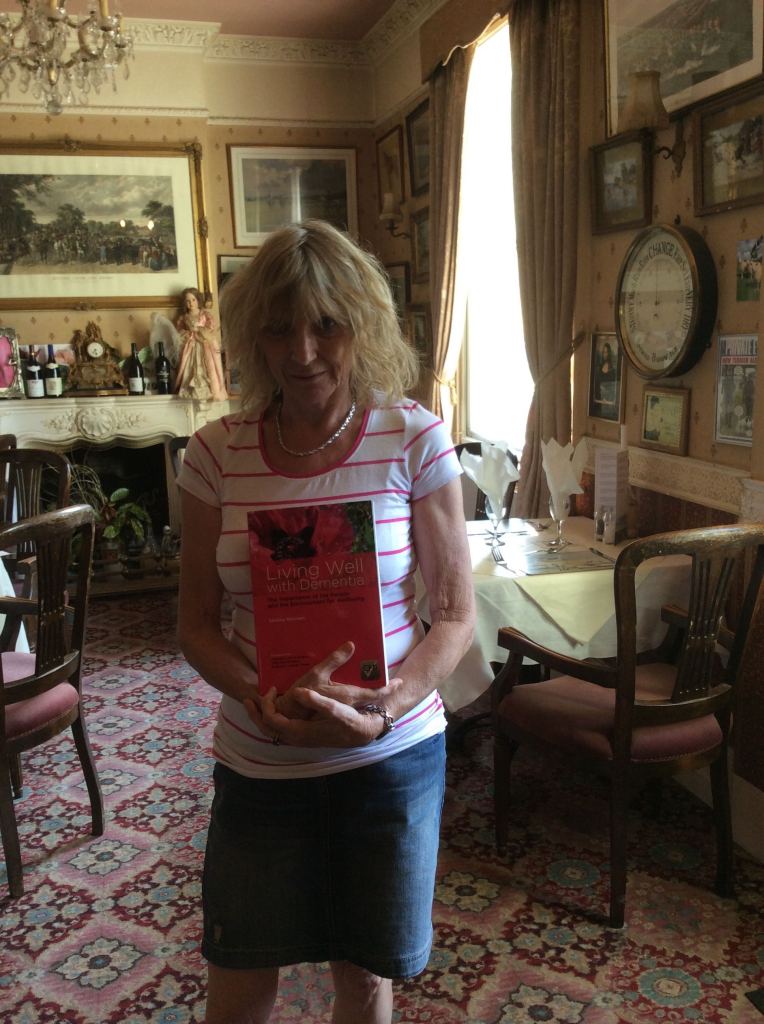
I have witnessed the problems with this, first hand, in writing my book ‘Living better with dementia: champions for enhanced communities’ which I hope to publish next year. The same tensions exist in statutory obligations in the form of equality and human rights law, and statutory entities, and non-statutory community-driven ones there too.
As the O’Donnell Report puts it, wellbeing:
‘leads us to place greater weight on the human factors that explain the big differences in wellbeing, but that tend to be pushed to the margins in traditional policy making’.
There has been some focus on how we need an ‘alternative measure to GDP’. Cynics unsurprisingly argued that such a measure might inevitably gather political momentum given the problems we have had with economic growth in the last few years.
But the general arguments from the APPG on wellbeing economics make an enormous amount of sense to me. Julian Huppert is the current MP for Cambridge, and I dedicated my current book to his mother Prof Felicia Huppert, Professor of Wellbeing at Cambridge. Julian is, to my knowledge, on the APPG on wellbeing economics.
The next parliament, I hope, will see a continuation of a focus on wellbeing in policy. As pointed out in their first report, there is considerable overlap with the wellbeing field and that of the ‘social determinants of health’.
In my next book, I continue with analysing this overlap, using housing as an example. Housing is clearly an area which impacts upon the quality of life of people living well with dementia, not just from architectural perspectives of design, but also how spaces are organised to facilitate personal interaction.
Similarly, planning in the built environment is important, with considerations of inclusivity and accessibility.
These are all ‘desirable’ (or even ‘essential’?) attributes of the ‘dementia friendly communities’.
Unpaid caregivers and paid carers, like professionals, are vital in the social capital of these communities too.
It is said elsewhere that while there has been a strong focus on GDP-style economics the lack of focus on wellbeing means that we do not touch upon many policy areas, such as strife caused by marital breakdown.
I feel that this touches upon another tension of dementia policy, this time at a global level.
We know, for example, loneliness is an important source of emotional morbidity for people who have received a probable diagnosis of dementia all around the world.
Also, jurisdictions have been encouraging the aspiration of people living with dementia to live independently; in other words, not institutionalised in some form, as long as possible. This, I think, is intuitively right, so long as it is not perceived as a ‘failure’ if somebody does need the support and care provided from an institution.
There are some people who believe that the ‘successful ageing’ and ‘ageing in place’ movements have overplayed their hand; with cynics pointing out they fit nicely into the ‘small state’ narrative, a rather individualistic narrative, which takes little account of our cohesion as a society.
But this I genuinely think would be to analyse the issue too much but with one important proviso.
That proviso is that I don’t think you can value people simply in terms of their economic productivity.
I refer to this ‘equality of wellbeing’ even in my Introduction to my new book. Such equality of wellbeing throws a different light on equality driven by a purely economic sense.
In summary, in reference to the first ever report from the APPG in wellbeing economics, as the next Government and the Civil Service turn their minds into thinking about wellbeing and health policy, it will be forefront in their minds that we are about to embark on a huge behavioural change bringing together the NHS and social care.
This transformative change to ‘whole person care’ will bring great opportunities, I feel, as well as formidable challenges, not least funding considerations at a local and national level.
But I feel like the current Government, and like future ones hopefully, that a focus on wellbeing is desirable. O’Donnell is reported to have said, “If you can measure it, cherish it!”
Ideally, it would be nice to have some form of metric to see whether wellbeing interventions have any effect. I am mindful of the excellent work by Prof Sube Banerjee and colleagues on DemQoL, but others exist. And of course we should not want to end up where we started: in a target driven culture which hits targets but misses the point (as famously phrased by Sir David Nicholson).
There might be desirable effects of such metrics, though. They could be formally put into grants for research for living well with dementia; to see whether some activities are more beneficial in care homes, where there is a high proportion of people living with dementia often, than others.
The Baroness Sally Greengross asked me to put in a chapter on arts, music and creativity in my current book; so I did.
But, as the new APPG report on dementia this year rightly discusses, such a metric could be used to incentivise the use of the arts and creativity to improve the quality of life of individuals in society. And I have no doubt whatsoever that arts and creativity are a linchpin of dementia friendly communities too.
The APPG in dementia earlier this year, under Sally’s leadership, urged the importance of high quality commissioning in post-diagnostic support for dementia.
If we have more a ‘joined up’ approach to commissioning and policy, in parallel with the breaking down of silos needed for ‘whole person care’, I think England can consolidate its formidable lead in the ‘dementia friendly communities’ policy in the world.
Other jurisdictions might even follow suit.
Recommended reading:
Gus O’Donnell (Chair) – and Angus Deaton, Martine Durand, David Halpern and Lord Richard Layard(2014). Wellbeing and Policy. London: Legatum Institute. Accessible at: http://www.li.com/docs/default-source/commission-on-wellbeing-and-policy/commission-on-wellbeing-and-policy-report—march-2014-pdf.pdf?sfvrsn=2
Wellbeing in four policy areas: Report by the All-Party Parliamentary Group on Wellbeing Economics (September 2014). Accessible at: http://b.3cdn.net/nefoundation/ccdf9782b6d8700f7c_lcm6i2ed7.pdf
All-Party Parliamentary Group on Dementia assesses progress of the National Dementia Strategy for England
2014 report: The National Dementia Strategy: Change, progress and priorities
Accessible at: http://www.alzheimers.org.uk/site/scripts/download_info.php?downloadID=1447
Continuity of care and support is vital in dementia policy. We are a long way from that.
In a way, the second ever English dementia policy poses more of an acid test than the first one. The reason for this is because we already have a set of yardsticks by which the first five years can be assessed, with a view to projecting forewards.
I don’t doubt the enthusiasm with which we have tried to close the ‘diagnosis gap’ in England. The heart of this is the high quality diagnosis, as stipulated in the original policy co-authored by Prof Sube Banerjee at Brighton and Sussex Medical School. What we have tended towards, rather, is a culture of high volume mediocre quality. And people readily admit they would rather wait that little bit longer to get the correct diagnosis.
I do not subscribe to the idea that anyone can easily make a diagnosis of dementia. When a diagnosis of dementia is finally given, it’s given not just to the person with dementia, but to his or her friends, or her family. As Kate Swaffer says, she is not a person with dementia primarily; she is a person with friends, family and feelings.
This approach prioritising the person has to be right from the word go. We are all persons, but we become patients when we become ill enough to present to the health and care services or not. We become paying consumers when we part with money. We are consumers if we spend any resources from the pot of money paid into from national insurance.
And so on. This analysis of money is a sideshow only as far as to how to service is delivered is actually matters. If you have services in dementia and support commissioned in a highly piecemeal manner, at worst from clinical commissioning groups who don’t know what wellbeing is, nor what they’re looking for, it can be a mess.
The hunt is definitely on for effective commissioning as well as any commissioning at all. The next Government will have to provide much better clarity on this, and some objective guidelines on how, say, the delivery of wellbeing might be ensured on an ongoing basis, not just at the start and finish of a commissioning contract.
But it is the fragmented approach from different providers which is a threat. Low pay of carers, not meeting the national minimum wage, or zero hour contracts, is a problem, and the reason specifically why private providers can be an issue here is that large corporates with scrupulous employment practices can hide behind a veil of being unperturbed from freedom of information legislation.
It is very easy to argue that entire health policy, and even dementia policy, is not political. I don’t believe this is justifiable for a minute. How we prioritise care at all is a reflection of our collective solidarity as a society, and our success in ‘pooling risk’. If I know for example I have a high genetic risk of developing a dementia from my genetic make up, my insurance premiums is likely to go through the roof unless there is tight anti-genetic discrimination law in place in England (which there isn’t).
Having a piecemeal system promotes lack of continuity of care. I think this is fatal for any new English dementia strategy. I think this piecemeal system, whether an artefact of private markets or not, or political ideology, can adversely affect people living with dementia and carers in a number of different ways.
First of all, the caregiver relationship, whether paid or unpaid as carer, fundamentally depends on that caregiver knowing the person with dementia. The happiest relatives I have ever spoken to are the ones who report that they haven’t had a regular changing of the guard as regard carers. This is important for building meaningful relationships with time, as people with Alzheimer’s disease for much of their time, even if they have weak memories for events have strong enduring memories for emotions. Besides, change here can be very distressing, and mental distress can impact on lack of physical wellbeing (although ill being is not necessarily the same as lack of wellbeing).
Secondly, continuity of care by a physician or an appropriate specialist in clinical psychology acts as a safeguard to check the actual diagnosis is right. Some initial cognitive impairments do not progress – they remain mild. A ‘wrong diagnosis’ of dementia does not necessarily mean someone has goofed up as such – it could mean that something that was predicted to progress didn’t. The drive to diagnosing dementia, particularly with financial incentives, could mean we accidentally mislabel mild cognitive impairment as dementia, and this is clearly a tragedy for all involved.
Therefore, a diagnosis disclosure can never be a single hit and run event. There needs to be follow up from the system, whether it’s by the same GP, a hospital physician or psychiatrist, a different member of the memory clinic possibly somewhere totally different; a second ‘set of eyes’ to see whether the initial diagnosis is correct. Granted I agree that knowing what the diagnosis is can be the key to opening services, being armed with information and hence empowered, and all the usual arguments, but the diagnosis must be correct. There is no alternative on this.
Say, for example, you are in fact depressed, not living with dementia, and a clinician in a hurry informs you you are living with dementia. You have presented in response to the question, “Do you have problems with your memory?”. Such a misdiagnosis is likely to make you even more depressed; and not receiving effective treatment for depression, whether as a psychological therapy or medication, or otherwise.
Thirdly, somebody who knows a person well will be able to spot when a person with dementia changes in any way. This could be a ‘difference’, such as the development of a sweet tooth, a ‘deterioriation’ such as in memory, or even an ‘enhancement’ as in acquisition of a love of music, or artistic and creative talents. You can only ascertain this with time. This is where the idea of the review has to change fundamentally.
I don’t feel this review should take place in the hands of medics who repeat scans and tests, ask a few random questions, and document the decline (as dementia is progressive if it is not ‘reversible’ such as vitamin deficiency). Implementation of a ‘year of care’ for dementia, or a national network of clinical specialist nurses, will be able to manage a caseload of individuals living well in a pro-active fashion, each with an individualised care plan; where the goal is to live well, not to firefight in a crisis.
Fourthly, the fundamental crunch time for a person living with dementia is an inability to retain information for a decision, an inability to make that decision, and an inability to communicate that decision. The starting point is that we can make decisions or have ‘capacity’. This capacity can come or go; and it’s dangerous if we get into the mindset that capacity is all or nothing, but that is the legal shortcut we have in place.
But this capacity needs review on a regular basis, as it fundamentally changes our view as to whether a person can consent or not. People living with diffuse lewy body dementia, for example, can notice themselves one day they’re performing quite well, other days not so well. If we don’t get into the good practice of reviewing capacity and consent on a regular basis, through continuity of care, we will easily arrive at a situation where people are languishing inappropriately on medications. It’s generally felt that, while appropriate for some, antipsychotics prescribing is too high, often inappropriately; some side effects such as drooling of the mouth can be very distressing. It’s currently, rightly, a plank of policy to address the inappropriate prescription of antipsychotics particularly in care homes.
In summary, the ideal would be somebody to accompany a person from the point of diagnosis to the time of end of life; not chopping and changing. I was told by a senior specialist nurse at the National Hospital for Neurology and Neurosurgery, Katy Judd, that one of the most disturbing phenomena for persons with dementia and families is when their ‘contacts’ have ‘moved on’ on such a frequent basis. There clearly needs to be proper signposting with the system, known as care coordinators, but we need to avoid the situation where there is an abundance of signposts and a dearth of frontline care.
But I feel fundamentally continuity of care and support is critical. Having the same mutual followers on a social network on Twitter has the potential to improve wellbeing, and having somebody there by you that you trust is likely to have the same effect. People living with dementia who are stimulated psychologically by positive experiences are likely to find their experience fundamentally of a different nature to those who don’t.
For these reasons I feel that, whatever tactics are used, and whichever government is in office and/or power in England, for the next few years, an overall strategy of prioritising the continuity of care is pivotal.
The spirit of 2015
In the Peasants’ Revolt in 1381, John Ball said, “Nothing will go well in England until all things shall be held in common”.
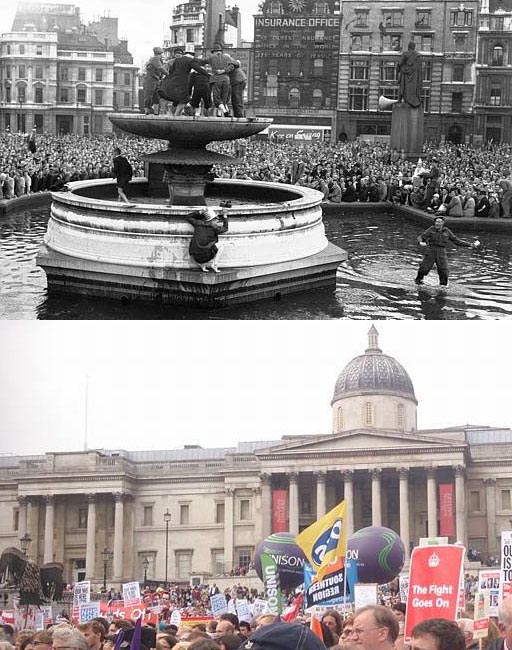
I went to Trafalgar Square, just downstream from Piccadilly, in London for a huge NHS rally earlier this year. It’s where crowds had also gathered in 1945, for VE day to celebrate winning the Second World War.
As we face a general election on May 7th 2015, something akin to the ‘spirit of ’45” arguably needs to be mobilised. It is sometimes easy to escape seeing the wood from the trees, with discussions firmly footed in the immediate, such as a leaked memo by Labour on immigration, or a brouhaha between Russell Brand and Nigel Farage.
We still need the same type of military discipline to build a Britain fit for purpose for peacetime. Successive mainstream governments have allowed themselves to sing to the neoliberal tune. It’s clear that in some places this hand has been overplayed, such as the ‘benefits’ of competition to the NHS. Because of the ‘market’ in the NHS for the first time under this Government, a hospital merger reasoned on the basis of clinical need could not take place because of competition law.
We’ve been sucked into this false narrative, and we are still not free of it. But if we return to a collective spirit anything is possible.
Whilst both Margaret Thatcher and Winston Churchill clearly wanted the words of FA Hayek (“The Road to Serfdom”) to be widely read, it is a sad admission that the market is not in fact liberalising; it can be best described as positively “enslaving”.
Markets free from public ownership are dogged with waste and inefficiency. Water and gas are homogenous products; they form natural monopolies which need to be organised properly.
In 1947, the UK parliament set up the British Transport Commission. One of the first steps was to abolish in Euston around the time, the ‘clearing house‘ of hundreds of clerk to oversee the administration of transactions between private companies.
Move forward to the time of this Government, some private outsourcing companies have also been dogged further with illegal fraud allegations. They also escape the Freedom of Information Act.
Very few of us want a NHS where your access is treatment is dependent upon your ability to pay. But only today it was reported that acute dermatology services would be taken out of scope in Nottingham and Lincoln for example.
It remains the case that Governments should respond to people’s needs, and have people with a strong public service interest to organise facilities around these needs. The primary driver cannot be profit, especially excessive profit. The section 75 clause of the Health and Social Care Act ram raided the NHS with competitive market tendering. The result has been some mouth watering contracts go to the private sector; this is privatisation, meeting the WHO’s own definition of the transfer of resources.
We want a world where the world is adapted for needs, and democratic.
It’s not a question of buying influence with money. The most effective route to exerting influence is the careful use of the democratic vote. A vote on Farage is likely to be an opportunity missed, when you could vote for the full integration of health and care services or ‘whole person care’.
We should NOT fight with each other.
Nurses should not struggle on and on, many without pay rises, creating value in the NHS, while private equity cream off proceeds from the wealth that they create through a series of abstract transactions.
Nurses and all workers including allied health professionals and doctors OWN the National Health Service – the City shouldn’t.
The Beveridge Report spurred us on as a country to combat five giant evils.
As described in an article in the Guardian earlier this year,
“Beveridge, however, was on to something in basing his report on the need to tackle five “giant evils”: want, disease, ignorance, squalor and idleness. His list has stood the test of time so well that when the IPPR thinktank published recently its Condition of Britain analysis, it revisited the five topics for an update. Verdict: work still in progress.”
“Want” is still a problem with many people needing to ‘top up’ their income with working tax credits. It doesn’t matter if we have a record number of people in employment, if these people are underemployed. They are working, but they are still poor. A spirit of 2015 needs to address abuses of zero hour contracts. Too many paid carers are providing care in fifteen minute slots, not being paid a proper wage, and not being paid adequately as power towards scrupulous employers has again swung too far.
Idleness is not a criticism easily levelled at men and women who are working extremely hard, and finding it hard to make ends meet with a rampant cost of living crisis. We want resources to be distributed properly, so no longer fat cats are sitting on huge salaries while there’s misery.
What has happened over welfare benefits, with an army of disabled citizens burnt out with worry, is a public disgrace. The UK should be proud of its value where we all pool risks and we all feel responsible for everyone else: we are our brothers’ keepers. As a civilised country, we should be ashamed if we don’t care for disabled or elderly members of our society, for example.
If resources could be organised properly in the Second World War, our resources can be organised properly now. Why has inequality got considerably worse under Thatcher’s government and beyond?
Things are so bad that members of the general public have utter ignorance about their legal rights being demolished. 2012 saw the Legal Aid and Sentencing and Punishment of Offenders Act and annihilation of English law centres. Furthermore, Chris Grayling who has never done a law degree so can be reasonably expected to be ignorant about aspects of the law has presided over demolition of judicial review and privatisation of probation.
The Commonwealth Fund found recently that the UK has one of the best health systems in the world. Put simply, the NHS won’t be able to survive another unexpected top down NHS reorganisation from the Conservatives designed to privatise the NHS yet further. We have 800 000 people living with dementia, and yet we have social care on its knees. Despite the high profile ‘Prime Minister’s Dementia Challenge’ and G8 dementia, one can rightly moot whether Pharma has benefited more than people living with dementia or caregivers.
No party wishes to doubt the prestige of the National Health Service, even though the Conservatives and Liberal Democrats produced the legislation in 2012 to turboboost its destruction.
Whereas Nye Bevan joked at the time of the creation of the NHS, ‘doctors’ mouths were stuffed with silver’, almost seventy years later corporate competition lawyers’ mouths were stuffed with silver.
Squalor does exist still. It is tempting to want to believe squalor doesn’t exist. But it does (as shown here).
As Tony Benn warned numerous times, politicians go round and round in circles.
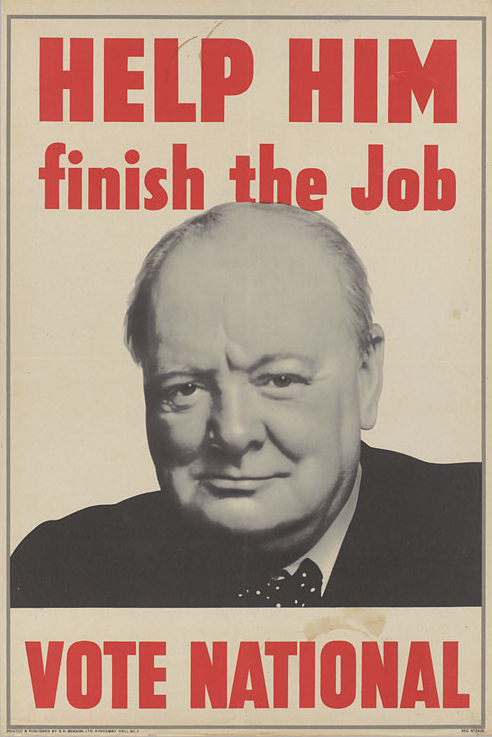
Winston Churchill wanted after 1945 for the Conservatives to lead the UK to prosperity.
Winston Churchill wanted in 1945 to be given “the tools to finish the job”.
The Daily Express on the morning of the general election in 1945 urged voters to return Mr Churchill.
Clem Attlee for Labour, on the other hand, won with a landslide.
In 2014, David Cameron has asked for a mandate to lead the UK to prosperity and to ‘finish the job’.
You know what to do.
Am I in a better place than I was last year? Yes. Definitely.
When I finally got a chance to meet the General Medical Council this year, the Chairman of the Fitness to Practise panel asked one of the witnesses, a Professor, whether I was in a better place compared to a few years ago.
That witness said, “Well, I wouldn’t say necessarily ‘better’. He is successfully living with a disability, but he has been in recovery for seven years now.”
And so it went on.
The GMC asked me what my favourite areas of law are.
I explained curtly, “Whistleblowing”.
“Are there any areas of corporate law which interest you?”
“Yes – compromise agreements”.
I think the GMC smelt a rat at that stage.
“And your MBA? What did you enjoy the most?”
“Leadership”
“Why?”
“Because I don’t think the NHS has any effective leaders.”
And so it went on.
The purpose of this blogpost is to thank the people who’ve made my year.
I should like to thank my witnesses for my GMC hearing for helping me to return to the UK medical register. I consider it a massive honour to be a practising Doctor on that Register.
Being chucked off it ripped me apart. Going back to it was the most unbelievable happy event of my life.
I should like to thank Jos – though I have no photos of us. Jos Bell is simply smashing for keeping me going – for being interested – for not accepting any crap.
I should like to thank Kate Swaffer. I regret that the only time I met her, I didn’t know her at all. I chat with her on Facebook when I can, very frequently. My life would be utterly devoid without her.
Chris and Jayne also made my year. I feel as if I’ve known them ages. And Monica.
And it’s been a delight I’ve met in my world of dementia policy.
You see, I haven’t had a job since 2005. There’s an important reason for that. Dementia policy for me is not a hobby or a job – it is a passion. I don’t get paid for any of it, apart from very basic royalties.
I funded myself to go to Alzheimer’s Europe in Glasgow, and Alzheimer’s Association in Copenhagen – though I had a wonderful time.
Toby Williamson really ‘got it’. I can’t thank him enough for ‘getting’ the importance of the disability lens to dementia policy, as well as with a mutual friend of ours Grainne in Ireland.
It was truly wonderful to chat with Prof Martin Rossor who used to be my boss at Queen Square more than a decade on the dementia and cognitive disorders firm at the National Hospital at Queen Square.
Possibly the kindest man I’ve ever met (apart from my late father.)
I’ll be going to Perth and Adelaide next year – hopefully will catch up with Tru, Kate, Chris, Jayne, Pete and Boris.
I loved meeting Charmaine and the whole Hardy clan – and Tony and the Ostrich in Robertsbridge of course!
Thanks to Martin from the Socialist Health Association for keeping me going during my numerous visits to Manchester.
Thanks to Dr Phil Hammond whose article on alcoholism and the medical profession was the best thing to have happened to me for years.
Dementia is not a brand.
But here are some random memories.
Have met some remarkable people for the very first time – like Tommy Whitelaw and Sam – both feisty Scots!
Good luck Andy Burnham next year! I will be intensely proud when you get a chance to bring together the NHS and social care, and to begin to make whole person care a reality for me and many people living with dementia (and the caregiver community.)
Living better with dementia: a “Year of Care” for dementia?
This is an extract from my book ‘Living better with dementia’ by me (Forewords by Prof Alistair Burns, Kate Swaffer, Chris Mason and Dr Peter Gordon), to be published by Jessica Kinglsey Publishers 2015. It comes from the chapter on whole person care (chapter 10).
Acute medicine is ideally suited to the medical model where you make a diagnosis on the basis of investigations, and then you immediately implement a management plan. There should of course be prompt action on acute situations for people living with dementia, but this is rather different to the usual needs of a person trying to live better with dementia. A person with a long term condition “lives with the condition day by day for their whole life and it is the things they do or don’t do that will make the difference to their quality of life and the long term outcomes they will experience” (Royal College of General Practitioners, 2011).
Shirley Ayres (2014) argues in her article entitled “The long term care revolution: a provocation paper” that “people in later life offer wisdom, experience, perspective and a wide range of skill sets and capacities”, reflecting that that long term institutional care is not the correct setting for them. This argument also holds true, perhaps, for people living well with advanced dementia.
The burning question still remains, as it was in the genesis of the first English dementia strategy, how a framework of post-diagnostic support for people living with dementia could best take place in England. I have already discussed earlier in chapter 10 of my book the policy of ‘whole person care’, and the critical rôle of social care practitioners and clinical nursing specialists in a multidisciplinary approach. It is also worth noting that the “year of care” initiative has seen some crystallisation of the approach for living well. It offers a framework that supports delivery of the Domain 2 of the NHS Outcomes Framework ‘Enhancing quality of life for people with long-term conditions’. Through this, it is hoped that ‘far more people will have developed the knowledge, skills and confidence to manage their own health’, but there are clear implications for the implementation of whole person care, namely, “care which feels more joined-up to the users of services”, and “care [which] centres on the person as a whole, rather than on specific conditions” (Year of Care website, accessed December 2014).
There will always be the criticism that self management, rather than having the prime goal of encouraging health and wellbeing, is meant as a ‘cover’ for essential services being cut. Benefits of “self management” which have previously been proposed are, nonetheless, proposed in Box 1.
—————
Box 1. Benefits of ‘self management’ [Source: Royal College of General Practitioners (Clinical Innovation and Research Centre) (2011) (authors: Nigel Mathers, Sue Roberts, Isabel Hodkinson and Brian Karet) Care Planning: Improving the Lives of People with Long Term Conditions]
When people self care and are supported to do this, they are more likely to:
- experience better health and well-being
- reduce the perceived severity of their symptoms, including pain
- improve medicines compliance
- prevent the need for emergency health and social services
- prevent unnecessary hospital admissions
- have better planned and co-ordinated care
- remain in their own home
- have greater confidence and a sense of control
- have better mental health and less depression
—————
Indeed, this policy agenda has been slowly ‘cooking’ for about year. For example, nearly a decade ago, Department of Health (2005) issued its document “Supporting People and integration with Long Term Conditions – An NHS and Social Care Model to support local innovation: Improving Care Improving Lives” had proposed a number of key priority areas, namely:
- To embed into local health and social care communities an effective, systematic approach to the care and management of patients with a long term condition.
- To reduce the reliance on secondary care services and increase the provision of care in a primary, community or home environment.
- Patients with long term conditions need high-quality care personalised to meet their individual requirements.
This follows on from an elegant analysis from one of Derek Wanless’ numerous reports, this time “Securing our Future Health: Taking a Long-Term View” from 2002. This one envisages one scenario for the future involving full public engagement.
Wanless (2002) describes this as,
“levels of public engagement in relation to their health are high. Life expectancy increases go beyond current forecasts, health status improves dramatically and people are confident in the health system and demand high quality care. The health service is responsive with high rates of technology uptake, particularly in relation to disease prevention. Use of resources is more efficient.”
(Derek Wanless, Public Enquiry Unit (2002))
It has become increasingly acknowledged that under this approach, the “care plan” is pivotal. The care plan “should set out the patient’s agreed health objectives and care needs, including what the individual can contribute towards their own self care, and what each professional and agency will do to help them meet these. It will include preventive and health promotion actions (such as avoiding accidents, reducing infection or nutrition).” (Department of Health, 2005).
In a pamphlet from the King’s Fund (2013), entitled “Delivering better services for people with long-term conditions”, the authors, Angela Coulter, Sue Roberts and Anna Dixon describe a co-ordinated service delivery model – the ‘house of care’ – that incorporates learning from a number of sites in England that have been working to achieve these goals.
They describe that the “house of care” model differs from others in two important ways:
- it encompasses all people with long-term conditions, not just those with a single disease or in high-risk groups;
- and it assumes an active role for patients, with collaborative personalised care planning at its heart.
This model is a system innovation, as applied to dementia, as it proposes a shift in power from professionals to persons living with dementia play an active part in determining their own care and support needs. Such an approach, it is hoped, would respect autonomy dignity, promote independence and offer maximum choice and control for need help from the health and care systems. The philosophy of “whole person care” moves the NHS towards an integrated health and care system, which is concerned about individuals during health as well as disease, a critical time when the coordination between the NHS and social care could not possibly be worse.
Self care is about individuals, families and communities taking responsibility for their own health and wellbeing. It includes actions people take in order to stay fit and maintain good physical and mental health, meet their social and psychological needs, prevent illness or accidents and care more effectively for minor ailments and long term conditions.
Both dementia and diabetes mellitus can be viewed as disabilities, and each may be a co-morbidity of the other. Sinclair and colleagues (2014) have outlined the key steps in an integrated care pathway for both elements of this clinical relationship, produced guidance on identifying each condition, dealt with the potentially risky issue of hypoglycaemia, and have outlined important competencies required of healthcare workers in both medical/diabetes and mental health settings to enhance clinical care. In the overall construct, people living with a long term condition, disability or a minor illness, as well as carers, can benefit enormously from being supported to self care.
The ‘Common Core Principles to Support Self Care’ aim to help health and social care services give people control over, and responsibility for, their own health and well-being, working in partnership with health and social care professionals (Skills for Care/Skills for Health, 2007) Seven principles have been elaborated. These are shown in Box 2 below.
—————
Box 2. Seven principles to support ‘self care’ [Source: Skills for Care/Skills for Health (2007)“Common core principles to support self care: a guide to support implementation” http://www.skillsforcare.org.uk/document-library/skills/self-care/commoncoreprinciples.pdf]
- Ensure individuals are able to make informed choices to manage their self care needs
- Communicate effectively to enable individuals to assess their needs, and develop and gain confidence to self care
- Support and enable individuals to access appropriate information to manage their self care needs
- Support and enable individuals to develop skills in self care
- Support and enable individuals to use technology to support self care
- Advise individuals how to access support networks and participate in the planning, development and evaluation of services
- Support and enable risk management and risk taking to maximise independence and choice.
—————
The “NICE quality standard for supporting people to live well with dementia: information for the public” is intended to support people to live well with dementia. It sets out how high-quality social care services should be organised and what high-quality social care should include, so that the best support can be offered to people with dementia using social care services in England (NICE, 2013). This has provided a very useful yardstick against which services which purport to improve the quality of life of people with dementia can be judged.
It is, further, reported that the ‘Year of Care’ (YOC) programme was successful in implementing the key features of care planning in diabetes, for example. The YOC Programme has two components, according to ‘Diabetes UK’ (2011). Firstly, it enhances the routine biomedical surveillance and ‘QOF review’ with a collaborative consultation, based on shared decision making and self management support, via care planning; and then it ensures there is a choice of local services people need to support the actions they want to take to improve their health, wellbeing and health outcomes.
People are involved in the care of their diabetes in quite a new way and enjoying it. People are setting personal goals and action plans relevant to their everyday life; take up of education programmes has improved and in very disadvantaged populations, poor attendance rates, biomedical outcomes and service use are also improving.
(Royal College of General Practitioners, 2011)
It is likely that the health and care sectors will seek to engineer the ‘best’ solutions on offer for post diagnostic support, within a framework of ‘whole person care’.
Such solutions might include ‘dementia advisers’, ‘clinical nursing specialists’, or ‘a year of care’. The solutions most appropriate for “living better with dementia” might be drawn, for example, from best practice in other long term conditions, such as diabetes or cancer. The quality of local commissioning, undoubtedly, is going to be pivotal in this. It will be a sensitive policy balance to make the argument that responsibilities of the State are not shunted across to the third sector in an unaccountable or unorthodox manner. But many will argue that there is valid and crucial role for the third sector to play. Actually, the policy imperative for this could not be clearer – many persons living well with dementia report not expecting to see a professional until the end of life phase, having seen one for the initial diagnosis. This is clearly not on if policy truly wishes to promote living better with dementia in England.
References
Department of Health (2005) “Supporting People and integration with Long Term Conditions – An NHS and Social Care Model to support local innovation: Improving Care Improving Lives”, accessed 6 December 2014,available at: http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/Browsable/DH_4965951
Diabetes (UK) “Year of Care: Report of findings from the pilot programme” (date June 2011), accessed 6 December 2014,available at: http://www.diabetes.org.uk/upload/Professionals/Year%20of%20Care/YOC_Report.pdf
Innovate UK (2014) The long term care revolution: a provocation paper. (author Shirley Ayres), accessed 6 December 2014,available at: https://connect.innovateuk.org/documents/15494238/0/LTCRprovocationPaper.pdf/45cf1947-c477-4f21-913e-4eb3f9061aa0
King’s Fund (2013) (authors: Angela Coulter, Sue Roberts and Anna Dixon, October 13) “Delivering better services for people with long-term conditions”, accessed 6 December 2014,available at: http://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/delivering-better-services-for-people-with-long-term-conditions.pdf
NICE quality standard 30 April 2013 NICE quality standard for supporting people to live well with dementia: information for the public, accessed 6 December 2014,available at: https://www.nice.org.uk/guidance/qs30
“Policy: A Year of Care”, accessed 6 December 2014,available at: http://www.yearofcare.co.uk/policy-0
Public Enquiry Unit (2002) “Securing our Future Health: Taking a Long-Term View. Final Report” (author Derek Wanless), accessed 6 December 2014, available at: http://si.easp.es/derechosciudadania/wp-content/uploads/2009/10/4.Informe-Wanless.pdf
Royal College of General Practitioners (Clinical Innovation and Research Centre) (2011) (authors: Nigel Mathers, Sue Roberts, Isabel Hodkinson and Brian Karet) Care Planning: Improving the Lives of People with Long Term Conditions, accessed 6 December 2014, available at: http://www.impressresp.com/index.php?option=com_docman&task=doc_view&gid=75&Itemid=70
Sinclair AJ, Hillson R, Bayer AJ; National Expert Working Group. Diabetes and dementia in older people: a Best Clinical Practice Statement by a multidisciplinary National Expert Working Group. Diabet Med. 2014 Sep;31(9):1024-31. doi: 10.1111/dme.12467.
Skills for Care/Skills for Health (2007) “Common core principles to support self care: a guide to support implementation”, accessed 6 December 2014,available at: http://www.skillsforcare.org.uk/document-library/skills/self-care/commoncoreprinciples.pdf
The presentation may be awful, but sharing of information can be very useful for clinical decision making

Whenever I hear of somebody refer to ‘Big Data’ and the NHS, it’s an immediate ‘facepalm’.
When I saw a blogpost shared by a Twitter pal shared yesterday, a blogpost written by Sir Jeremy Heywood, my first instinct was completely to ignore it.
I am, though, mindful of the Civil Service’s prolonged campaign to measure wellbeing; this first came across my RADAR from Lord O’Donnell.
I have a disclaimer to make: I am not a corporate shill.
Having done certain training, I am aware of the hard sell of ‘Big Data’ as the next big thing by the multi-national corporates. “Big data” seem to have been given a somewhat pedestal status, like 3-D printers.
We are often told how intelligent technology rather than being a costly burden to the NHS could bring great benefits and outcomes for the NHS.
Undoubtedly, a lot of democratic deficit damage was done by the Health and Social Care Act (2012). At close to 500 pages, it was very easy to say it was too incomprehensible to be analysed. I always felt the Act, for anyone trained in commercial and corporate law, was in fact relatively straightforward.
The Health and Social Care Act (2012), often called “the Lansley Act”, has three essential prongs of attack: one to introduce a competitive market through legislation for a heavy penalty for non-one-commissioning not going out to tender, a beefed up regulator for the market (Monitor), and some detail about insolvency regimens (but not all).
In this, it was completely consistent with work by Carol Propper; and other noises from ‘independent think tanks’, such as the King’s Fund.
However, the acceleration of this Act through parliament by two parties which are extremely sympathetic to the free movement of multinational capital has done long-lasting damage.
I think there are problems with having data so transparent. When I did my Masters of Law practice-focused dissertation in cloud computing law, I unearthed a huge literature on data security and data confidentiality/sharing.
When I later did my pre-solicitor training, I discovered the regulatory requirements on the balance between confidentiality and disclosure to be complicated.
When I later came to revise ‘Duties of a Doctor’ (2013), the General Medical Council’s code of conduct, I found there to be equally onerous considerations.
I am aware of the problems in my own field of work; about concerns that NHS patients will be scared from going to see their GP for fear of being diagnosed, incorrectly, with ‘incipient dementia’ because of a GP’s practice wanting to meet a financial target.
Or a junior Doctor not wishing to share his alcoholism with his own Doctor, for fear that this information will end up with the clinical regulator, with a super-un-sympathetic sanction. This is a subject close to my heart, as you will well know.
Indeed, if you’ve been following me on Twitter, you’ll know that a year after erasure by the GMC (in 2006 to be endorsed by the High Court in 2007), I spent a year sitting in a pub with no family or job. I later was then admitted to the Royal Free Hospital having had a cardiac arrest and epileptic seizure, then to spend six weeks in a coma.
I am now knowledgeable about what both the legal and medical regulators expect me to do, as I am regulated by them.
The next Government will be wishing to implement ‘whole person care’. While I think some of Jeremy Heywood’s claims are a tad hyperbolic (for example saying unleashing data will lead to wellbeing improvements), and while I don’t feel he currently ‘owns’ the data (the data are confidential property of the people who provide the data), there are clinically-driven merits to information sharing.
From now on, I will avoid the word ‘data’ and use the word ‘information’. But ‘information’ does not necessarily mean ‘knowledge'; and it certainly doesn’t necessarily mean ‘wisdom’.
One scenario is somebody prescribed Viagra for erectile dysfunction in the morning. He then has sex with his partner in early evening, and has Angina. He has longstanding ischaemic heart disease, and then takes his GTN spray. His blood pressure then goes through the floor, and he collapses. He then is blue lighted into his local emergency room.
Do not take this anecdote as ‘medical advice’ or any such like where I could get into regulatory trouble please.
Viagra is a class of drug which can interact with the GTN spray to send blood pressure through the floor. If this information were known to an admitting Doctor in the emergency room, this would be useful.
I can come up with countless examples.
A lady from a care home turns up in hospital at 4am. An admitting Doctor wishes to prescribe a heavy-duty blood pressure lowering drug, but notes she has had a series of falls. This is found out by looking at her electronic medical record. She indeed has a history of osteoporosis; weak bones could mean that she might fracture a bone if she had another fall.
But I could come up with countless examples. And I won’t.
I am not a corporate shill. I understand completely the concerns about the loopholes in current legislation meaning that ‘big data’ could go walkies to drug companies, though this is vehemently denied.
I am also aware of ‘cloud failures’ – the Playstation one for some reason springs to my mind.
That’s another reason to keep an eye on ‘My NHS’.
But we do need, I feel, to take a deep breath and to discuss this calmly.
Labour needs to keep scrutinising PFI and the NHS
Nigel Farage’s supporters often say that at least UKIP is forcing the main political parties onto the ‘immigration agenda’, despite the main parties not wishing to discuss immigration.
Critics have argued that UKIP have discussed moving the NHS towards a private insurance system, whereas Nigel Farage, leader of UKIP, on Question Time, argued that the matter had indeed been discussed but later rejected by their party.
It is reported that the Labour Party wishes to make the NHS its ‘number 1 electoral priority’, and that Lynton Crosby, the current strategist and tactician for the Conservative Party, is desperate not to make it so.
Labour themselves have criticised heavily how PFI represented poor value for the NHS, while most people generally concede that the NHS has suffered from lack of capital for its various necessary infrastructure projects.
“Take the PFI contracts – the private finance initiatives”, Farage mentioned on Question Time in a lengthy answer on the NHS.
Through PFI, large debts have been stored up for future taxpayers – at some stage need to be repaid. PFI debts do not form part of the deficit balance sheet.
“New hospitals were built, but rather than going to borrow money rather than going to the gilts market in that horrible City place, where they’re all crooks, Labour went to really rich people in private equity – and we borrowed £50 billion sterling to build new hospitals, which we built, but the repayments are £300 billion sterling.”
PFI deals were invented in 1992 by the Conservative government led by Sir John Major, but became widespread under Labour after 1997.
The schemes usually involved large scale buildings such as new schools and hospitals, or infrastructure projects which would previously have been publicly funded by the Treasury.
The projects are put out to tender with bids invited from building firms and developers who put in the investment, build new schools, hospitals or other schemes and then lease them back.
Love them or loathe them, the people in the City understand finance.
I suspect Nigel Farage does too.
Debt finance is a loan – an “IOU” – where you pay back the money, together with debt interest payments.
Equity finance is the bread-and-butter of the City and its lawyers.
For a pot of money, you buy a stake in a project which you can later sell at a profit. The critical thing about equity finance, which is why some people don’t like it, is that this stake buys you a slice in the management and control of projects.
Equity financiers, by buying stakes in PFI, exert from a distance a lot of control on our current NHS. This is a subject that no mainstream politician wishes to talk about; except…. bless him… Nigel Farage.
Nigel Farage may have become public enemy number 1 over their previous commments suggestive of privatising the NHS, but it is still not out of the question that Nigel Farage or Alex Salmond become Deputy Prime Minister in a formal coalition or a supply-and-confidence government led by Labour following May 8th 2015.
According to a Guardian analysis of contracts that were sanctioned by the Treasury dating from 2012, the cost of Britain’s controversial private finance initiative will continue to soar for another five years and end up costing taxpayers more than £300bn.
Andy Burnham MP continues to argue that Labour will return to the NHS to ‘people before profit’.
But Burnham has previously admitted PFI is problematic.
And all the mood music sounds as if Burnham is ‘seeing red over PFI’. Literally.
“We made mistakes. I’m not defending every pen-stroke of the PFI contracts we signed.”
Due to the costs of PFI, many NHS hospitals have found themselves struggling to pay for safe staffing in their budgets. It was recently reported that half of NHS workers would not receive a 1% pay rise.
Despite recent coalition criticism suggesting that the government was going cold on the scheme, published figures from the current Government have indicated that repayments will continue ballooning until they peak at £10.1bn a year by 2017-18.
According to the Guardian newspaper from 2012, the 717 PFI contracts currently under way across the UK are funding new schools, hospitals and other public facilities with a total capital value of £54.7bn, but the overall ultimate cost will reach £301bn by the time they have been paid off over the coming decades.
Equity investors have helped to deliver many public sector infrastructure projects via the Private Finance Initiative and have managed them in ways from which the public sector can learn.
Against a background of limited information, evidence gathered by the National Audit Office raises concern that the public sector is paying more than it should for equity investment. This report was published in February 2012.
The report still makes for interesting reading.
“Banks or bondholders provide around 90 per cent of the project funding for a PFI project on the condition that the remaining money is provided by the investors as risk capital or equity, which will be lost first if the project runs into difficulty.”
“Investors are rewarded for taking risks. The risks the investors bear are mainly the costs of bidding; that their contractors may fail to perform; or that other project costs the investors bear the risk for will be higher than envisaged. However, the investors limit their risk by passing it to their contractors. In addition, the government is a very safe credit risk and many projects such as hospitals and schools are repeat projects.”
“The Treasury and departments to date have relied on competition to secure efficient pricing of the contract but have not gathered systematic information to prove the pricing of equity is optimal. The NAO report identifies three potential inefficiencies in the pricing of equity. These are the time and costs of bidding; minimum rates set by investors, which sometimes do not reflect the actual risks the project will face; and bank requirements.”
The NAO report argued that, generally, public sector authorities have not been equipped with the skills and information required to challenge investors’ proposed returns rigorously. The NAO shows how further analysis during the bidding process would help authorities to assess the reasonableness of the investor returns. As an illustration, the NAO estimates that around 1.5 per cent to 2.2 per cent of the annual service payments in three projects it analysed were difficult to explain in terms of the main risks investors said they were bearing.
“Some investors in successful projects have gone on to sell shares in their equity to release capital and fund new projects. This has also resulted in accelerating the receipt of their returns. Analysis by the NAO has shown that investors selling shares early have typically earned annual returns of between 15 per cent and 30 per cent. The NAO recommends that the Treasury should use its current review of PFI to consider alternative investment models that limit the potential for very high investor returns in relation to risk.”
A future Labour Government will have to confront PFI, as it is an integral component of why the NHS is facing difficulties. A future Government could have the power to cancel or substantially renegotiate PFI projects where it could be proved that taxpayers were not receiving value for money.
It is also critical that the Government has the critical skills and expertise to use its huge buying power to obtain better deals, if it remains keen to pursue this policy route. It is already hardly coping with the deluge of contracts being put out to tender under section 75 Health and Social Care Act (2012), but Labour plans to repeal that Act in its first Queen’s Speech of the next parliament.
Unfortunately, total repeal of the Health and Social Care Act (2012) will have absolutely no effect on the operational or strategic management of PFI in the NHS.
Margaret Hodge has thankfully spoken out very vociferously about the problems with PFI under successive Governments.
“A rotten deal”
I agree with Margaret (full account here).
Andy needs to keep up the pressure on this.