Home » Posts tagged 'Living well with dementia' (Page 3)
Tag Archives: Living well with dementia
Why I’m on a mission to explain the science of decisions to people living with mild dementia
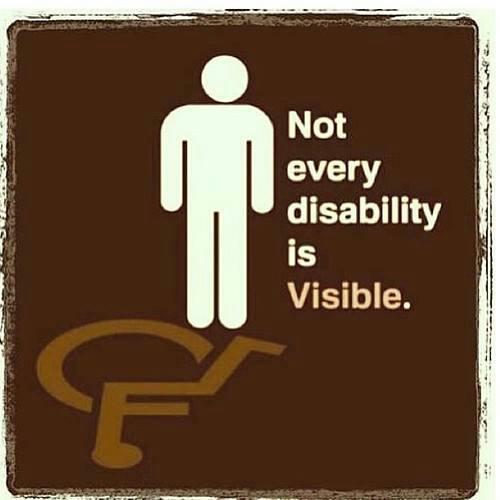
As a person who is physically disabled, and who has a speech impediment due to a meningitis from 2007, I am more than aware of how people can talk down to you in a patronising way.
It’s why I am very sensitive about language: for example, even with the best intentions in the world, “dementia friendly communities” conjures up an intense feeling of ‘them against us’.
It’s really important to not do anything which can cause a detriment to any group of people.
If you happen to be living with a condition which could cause you to have difficulties, this is especially important.
A “dementia” might be a disability under the Equality Act, and the person you’re speaking to might not obviously to you be living with a disability – it’s a ‘so-called invisibility’.
But – I’m deadly serious this. People shouldn’t be judged on what they can’t do. We all have failings of some sort. People should be encouraged for what they can do whenever possible. I don’t, likewise, consider the need for policy to embark on ‘non-pharmacological interventions’ as if what I’m talking about is second fiddle: living well with dementia is a complete philosophy for me.
In any other disability, you’d make reasonable adjustments. I see the need to explain how decisions are made to people with dementia as absolutely no different, both under the Equality Act (2010) and morally for a socially justice-oriented nation.
The excitement about how ‘decisions’ are made was recently described in the book by Prof Daniel Kahneman, “Thinking fast and slow”.
How we hold information for long enough to weigh up the pros and cons fascinates me.
Kahnemann, and others, feel that there are two systems.
System 1 is fast; it’s intuitive, associative, metaphorical, automatic, impressionistic, and it can’t be switched off. Its operations involve no sense of intentional control, but it’s the “secret author of many of the choices and judgments you make”. System 2, on the other hand, is slow, deliberate, effortful. Its operations require attention. (To set it going now, ask yourself the question “What is 13 x 27?”
Kahneman is a hero of mine as in 2002 he was awarded the Nobel Prize for economics, but he is essentially a cognitive psychologist.
In 2001, I was awarded a PhD from Cambridge for my thesis in decision-making in frontal dementia. I was the first person in the world to demonstrate on a task of decision-making that people with frontal dementia are prone to make risky decisions, despite having very high scores on standard neuropsychological tests and having full legal capacity.
Now, one coma later following my meningitis, I have done my postgraduate studies in law, and I have become fascinated by the rather arbitrary way in which our law has developed the notion of mental capacity, based on our ability to make decisions.
People with dementia can lose their ability to make decisions, so decision-making is a fundamental part of their life. As neuroscience and law straddle my life, I should like to make it my personal mission to explain the science of decision-making to people with full capacity, and who happen to have a diagnosis of dementia.
I am all in favour of a world sympathetic to the needs of people living with dementia, but this requires from us as a society much greater literacy in what the symptoms and signs of dementia are. I am not convinced we’re anywhere near that.
In the meantime, I think we can aim to put some other people in the driving seat, and they rarely get put in the driving seat: yes, that’s right, it’s time to engage people with mild dementia in the scientific debate about how decisions are made.
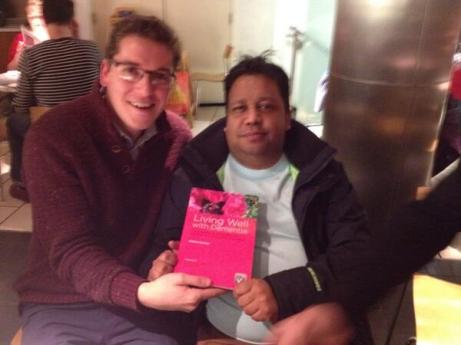
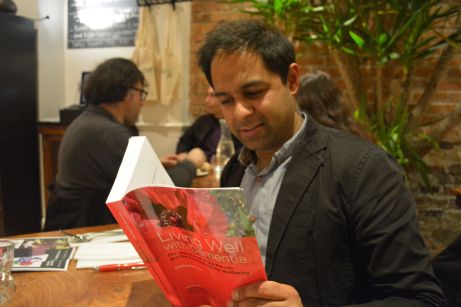
Copies of “Living well with dementia” are doing more cameos than Hitch
English film director Alfred Hitchcock (“Hitch”) made cameo appearances in 39 of his 52 surviving major films.
For the films in which he appeared, he would be seen for a brief moment boarding a bus, crossing in front of a building, standing in an apartment across the courtyard, or even appearing in a newspaper photograph.
This playful gesture became one of Hitchcock’s signatures; and fans would make sport of trying to spot his cameos.
As a recurring theme, he would carry a musical instrument — especially memorable was the double bass case that he wrestles onto the train at the beginning of “Strangers on a Train”.
In “The Birds”, as Melanie Daniels (Tippi Hedren) enters the pet shop, Hitch is leaving with two white Sealyham terriers.
This is a film of every single ‘Hitchcock cameo’.
Here are some recent cameos.
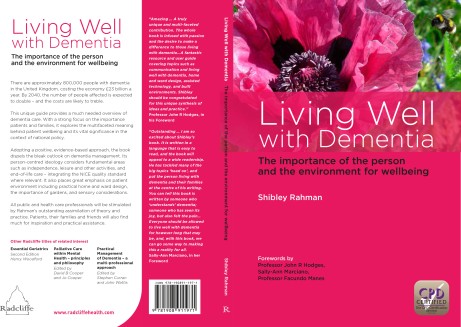
Full details about my book are on the Radcliffe website here.
Here are further ‘tweets of support’.
@legalaware Thanks for the RT! You seem to be having huge success with your book. Delighted to see the wonderful tweets about it. Well done!
— Rebecca Huxley-Binns (@BexHuxBinns) March 26, 2014
@legalaware not ‘improvement’ but sidewards step into further dementia excursions! a great book, proud to be in it & have it in the toolkit!
— James Murray-White (@sky_larking) March 25, 2014
@charbhardy @legalaware I just read a lovely book by Laurie Lee and these words made me think of you both pic.twitter.com/CQo3SjLh63
— Peter Gordon (@PeterDLROW) March 24, 2014
@legalaware Should think so too – most important and thought-provoking book on dementia for quite a while IMHO. Don’t sell yourself short.
— Steve Milton (@SteveMilton1) March 21, 2014
Reading beautiful written, highly relevant dementia book http://t.co/sN9egivjSn by brilliant @legalaware Beg/borrow/buy if u can. Just gr8 x
— Lisa Rodrigues (@LisaSaysThis) February 22, 2014
And above all…
I intend to promote the need of high quality wellbeing research at the SDCRN 4th Annual Conference on dementia in Glasgow today
This is the programme for today which I’m looking to enormously today.
I will be promoting heavily the cause of living well with dementia, to swing the pendulum away from pumping all the money into clinical trials into drug trials for medications which thus far have had nasty side effects.
In keeping with this, I have been given kind permission to give out my G8 Dementia Summit questionnaire to look at delegates’ perception of what this conference was actually about.
We need also not to lose sight of the current persons with dementia, to ensure that they have good outcomes in the wellbeing.
This can be achieved through proper design of care environments, access to innovations including assistive technology, meaningful communities and networks for people with dementia to be part of and to lead in, and proper access to advocacy support services and information which empower choice and control.
There’s a lot to do here – and we need to have high quality research into all of this arm of research too.
Coming back home to Scotland is like travelling back in time for me.
I was born in Glasgow on June 18th 1974, and my lasting memory of leaving Glasgow for London 37 years ago was how relatively unfriendly Londoners were in comparison.
Of course the train journey through the beautiful England-Scottish border countryside brought it back to me. There’s a lot to be said for getting out of London. It’s an honour to be here back in Scotland.
I had absolutely no idea I would have such a warm welcome here in Scotland. Still feeling incredibly emotional I’m here at all in Glasgow.
— shibley (@legalaware) March 24, 2014
@legalaware @tommyNtour @theRSAorg @PeterDLROW Enjoy the #SDCRN conference tomorrow all. I will be watching for tweets 
— SJ (@YeWeeStoater) March 23, 2014
@legalaware @YeWeeStoater @RealTaniceJudge Peters & Lee welcome home you’ve been gone 2 long come in& close the door http://t.co/LHQvVMprcc
— youcanmakedifference (@tommyNtour) March 23, 2014
Burst into tears on arriving home in #Glasgow just now @tommyNtour @YeWeeStoater @realtanicejudge pic.twitter.com/UG64xKc4GK
— shibley (@legalaware) March 23, 2014
@legalaware Lucky you. You will get a warm Scots welcome I’m sure!
— alison eaton (@doctorsnoddy) March 23, 2014
Penultimate stop in Carlisle. In my 40th year returning to #scotland at long last. pic.twitter.com/og6OAGSc66
— shibley (@legalaware) March 23, 2014
@legalaware @BarbaraACannon @Johnrashton47 Glad there are blues skies to greet you Shibley! Have a great conference!
— Dr ShirleyLockeridge (@DrShirleyLock) March 23, 2014
@legalaware welcome up north! Anything exciting?
— #hellomynameis Paul (@pauljebb1) March 23, 2014
At Penrith – nearly back home in Scotland @YeWeeStoater @tommyNtour pic.twitter.com/ZLpchE3YxE
— shibley (@legalaware) March 23, 2014
@DrShirleyLock @BarbaraACannon @Johnrashton47 now waving (not drowning) at Lancaster pic.twitter.com/ubphOxFF4W
— shibley (@legalaware) March 23, 2014
Welcome to Preston! pic.twitter.com/LQ1i67Dgx4
— shibley (@legalaware) March 23, 2014
Warrington still England surely? 3 hrs til Glasgow @BendyGirl pic.twitter.com/XFhyOKw5Ku
— shibley (@legalaware) March 23, 2014
Surprise surprise this Virgin train left on time from Euston at 1228 pm @SocialistHealth
— shibley (@legalaware) March 23, 2014
My book ‘Living well with dementia’ is here.
Contents
Dedication • Acknowledgements • Foreword by Professor John Hodges • Foreword by Sally Ann Marciano • Foreword by Professor Facundo Manes • Introduction • What is ‘living well with dementia’? • Measuring living well with dementia • Socio-economic arguments for promoting living well with dementia • A public health perspective on living well in dementia, and the debate over screening • The relevance of the person for living well with dementia • Leisure activities and living well with dementia • Maintaining wellbeing in end-of-life care for living well with dementia • Living well with specific types of dementia: a cognitive neurology perspective • General activities which encourage wellbeing • Decision-making, capacity and advocacy in living well with dementia • Communication and living well with dementia • Home and ward design to promote living well with dementia • Assistive technology and living well with dementia • Ambient-assisted living well with dementia • The importance of built environments for living well with dementia • Dementia-friendly communities and living well with dementia • Conclusion
Reviews
Amazing … A truly unique and multi-faceted contribution. The whole book is infused with passion and the desire to make a difference to those living with dementia…A fantastic resource and user guide covering topics such as communication and living well with dementia, home and ward design, assisted technology, and built environments. Shibley should be congratulated for this unique synthesis of ideas and practice.’
Professor John R Hodges, in his Foreword
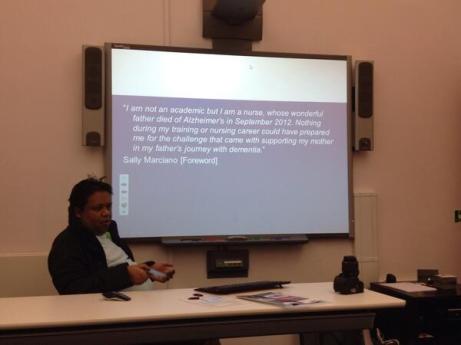
‘Outstanding…I am so excited about Shibley’s book. It is written in a language that is easy to read, and the book will appeal to a wide readership. He has tackled many of the big topics ‘head on’, and put the person living with dementia and their families at the centre of his writing. You can tell this book is written by someone who ‘understands’ dementia; someone who has seen its joy, but also felt the pain…Everyone should be allowed to live well with dementia for however long that may be, and, with this book, we can go some way to making this a reality for all.’ –Sally-Ann Marciano, in her Foreword
Thanks to Gill (@whoseshoes) for capturing the happiness of friends at my book launch for ‘Living well with dementia’
I don’t go to “trade fairs” where people display their latest ‘products’ for dementia. I am an outsider, and very happy to be so so.
But I do feel my book is having an impact slowly with the right people.
For example:
@a_carers_voice sitting in sunshine London garden reading @legalaware living well with dementia – what a read … Brilliant Shibley …
— Ann Pascoe (@a_carers_voice) March 16, 2014
and
@dementia_2014 utterly brilliant, very much reflects current thinking, covers a big topics succinctly.. enjoyed reading it
— Caroline Bartle (@3SpiritUKNZ) March 14, 2014
These are just some of the messages in the ‘little black book’ I was given at my book launch for ‘Living well with dementia’ (details here). Ones not shown have not been excluded out of any malice. I am hugely proud of people who kindly made it to Camden to celebrate my book on February 15th 2014. I am of course hugely indebted to Gill Phillips (@WhoseShoes) for presenting me with this ‘little black book’, which I promise to cherish forever. #KoalaHugs
I received a special book of good luck messages for my book launch. I really don’t deserve friends like @WhoseShoes. pic.twitter.com/3fQZVA7D3s
— shibley (@legalaware) March 16, 2014
One of the really special moments of my book launch was meeting @WhoseShoes‘ close friends David and Linda.
— shibley (@legalaware) March 16, 2014
This was a lovely message by David and Linda for my book launch. @WhoseShoes pic.twitter.com/zudB1uRBh2
— shibley (@legalaware) March 16, 2014
Really honoured Lee @dragonmisery made it to my book launch! Her ‘dementia challengers’ website is truly amazing. pic.twitter.com/6KwoRPDuYW
— shibley (@legalaware) March 16, 2014
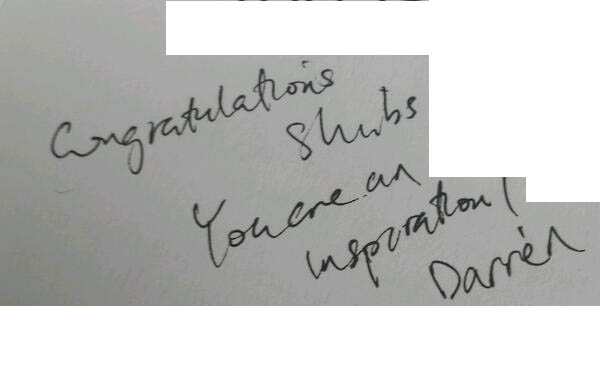
@MrDarrenGormley is one of my amazing friends. He also totally ‘gets’ personhood. pic.twitter.com/uBgeHIR8EZ
— shibley (@legalaware) March 16, 2014
The amazing @RachelNiblock – grateful for all her brilliant insights into dementia and carers. pic.twitter.com/WOJrvq6nDw
— shibley (@legalaware) March 16, 2014
Definitely a case of #koalahugs from the unique @KateSwaffer – my soulmate! pic.twitter.com/OzSZfkq8B7
— shibley (@legalaware) March 16, 2014
This made me laugh so much from @SarahReed_MHR – thx to sarah and @WhoseShoes for this lovely msg about my book! pic.twitter.com/xoGN5pzfDw
— shibley (@legalaware) March 16, 2014
Am chuffed to bits to have included @bethyb1886‘s outstanding work in my book on living well with dementia. pic.twitter.com/UPMRMHZdur
— shibley (@legalaware) March 16, 2014
With incredible ppl like @lucyjmarsters at the coalface of dementia care I am hugely optimistic. pic.twitter.com/c25aPL8IVX
— shibley (@legalaware) March 16, 2014
Incredibke that @mkilll completed a really long journey to be at my book launch on living well with dementia. pic.twitter.com/lLXqKm6qNz
— shibley (@legalaware) March 16, 2014
Simply amazing from Jo. pic.twitter.com/5z5s7S9tab
— shibley (@legalaware) March 16, 2014
Indeed here’s to ‘living well with dementia’ @sky_larking pic.twitter.com/9pFUY9HVQB
— shibley (@legalaware) March 16, 2014
I love @HLCLC – who epitomise the ethos of living well with dementia pic.twitter.com/Eh9hJqCbtH
— shibley (@legalaware) March 16, 2014
@helenbevan for a long time has been a massive influence as an external radical in living well with dementia. pic.twitter.com/AXq6iRsiHP
— shibley (@legalaware) March 16, 2014
And the last word is left to #KoalaHugs:
My name is Shibley, and I’m addicted to buying my own book ‘Living well with dementia’
I’ve sat in more recovery sessions than you’ve had hot dinners….
.. possibly.
So I get a surge of dopamine whenever I receive yet more copies of my book from Amazon.
Worth every penny.
I am Shibley. and I’m addicted to buying my own book.
But I also have a weird habit of getting people I know to sign my copy of my book.
I get withdrawal symptoms from not having enough copies.
I also get tolerance – I need to have an increasing number of copies to get the same “kick” from my book.
Thanks enormously to the following ‘well wishers’, though, who have signed my book.
A huge thanks to Gill (@WhoseShoes) for her unflappable support of me and my book.
Here’s Gill’s blogpost.
And here we are!
I felt very happy to give a copy of my book to Prof Sube Banerjee, newly appointed Chair of Dementia at Brighton and Sussex Medical School. Sube has in fact been the lead for England for dementia – his work is quoted in my book, and I think he’s made an enormous contribution to the living well with dementia literature.
And what does the future hold for ‘living well with dementia’?
Other ‘signatories’ include:
I’ve known Lisa for yonks on Twitter. Lisa is one of the few people who’ve supported me through the bad times too.
But now you can ‘Look Inside’ to get a flavour of my book – as there is now a Kindle edition (thanks to Alice in my book publishers @RadcliffeHealth)
Here it is on Amazon.
Here is a sample chapter from my book ‘What is living well?’
‘Living well’ is not some bogus mantra for the hell of it. It is an ideological standpoint which serves to promote the dignity of our fellow citizens who happen to also have a clinical diagnosis of dementia.
And here are the “beautiful people” who came to my book launch at the Arlington Centre, Camden, one afternoon in February. I can’t believe that this wasn’t even a month ago now!
One of the happiest days, as well, was giving Joseph a copy of my book as a gift.

Joseph was in fact my carer when I could hardly walk or talk, when I was in physical recovery from meningitis on ITU (where I was unconscious in 2007).
And those were the days…
And THIS is the famous poppy.
This picture was taken by Twitter pal, @charbhardy, first amongst equals in the #dementiachallengers.
After I said I was buying my own copies, @KateSwaffer asked:
But Kate has read a copy of my book from cover to cover:
And as @Norrms says – how can ‘living well with dementia’ fail?
Living well with dementia and the #Oldham review of whole person care
There were of course huge structural problems in the much heralded Oldham report on whole person care was published this week.
It’s officially called ‘One Person, One Team, One System‘.
These structural problems are, not least, to what extent will the NHS be paid for out of general taxation in the long term. The issue is not fudged altogether, in that Oldham calls for a future government to look into this as a priority.
Nonetheless, the Oldham Commission does fudge the issue of how much integrated and social care systems can rely on private not state provision. This is a strange ‘elephant in the room’, given the emphasis of the report on individualised budgets (call them what you will, personal budgets or personal care budgets).
Oldham does however concede helpfully that ‘financial arrangements in the adult social care system are equally fragmented, with complex and overlapping funding and provision arrangements between private and public funding sources, and private and public providers of care. The multitude of private care providers adds to this complexity.’
The need to repeal section 75 Health and Social Care Act is pivotal to all this. In fact, a repeal of the whole Act, as Labour (as Andy Burnham and Ed Miliband have indeed promised), would be helpful. This is, quite simply, because legally integration might offend the competition legal infrastructure established by section 75 and its associated Regulations, and of course sit uneasily with EU competition law.
At the moment, the NHS and social care services are geared up to ‘reacting to events’. And this is reflected in the payment by results mechanism (a reincarnation of ‘activity based costing’).
“Public funding has increasingly focused on those with greatest needs – particularly as rationing of care has become more severe – driven by a reactive, crises oriented approach rather than a focus on early intervention and wellbeing.”
Wellbeing is of course not just the opposite of illbeing, though lessons can be learnt from poor hydration and nutrition, for example, in individuals with advanced dementia.
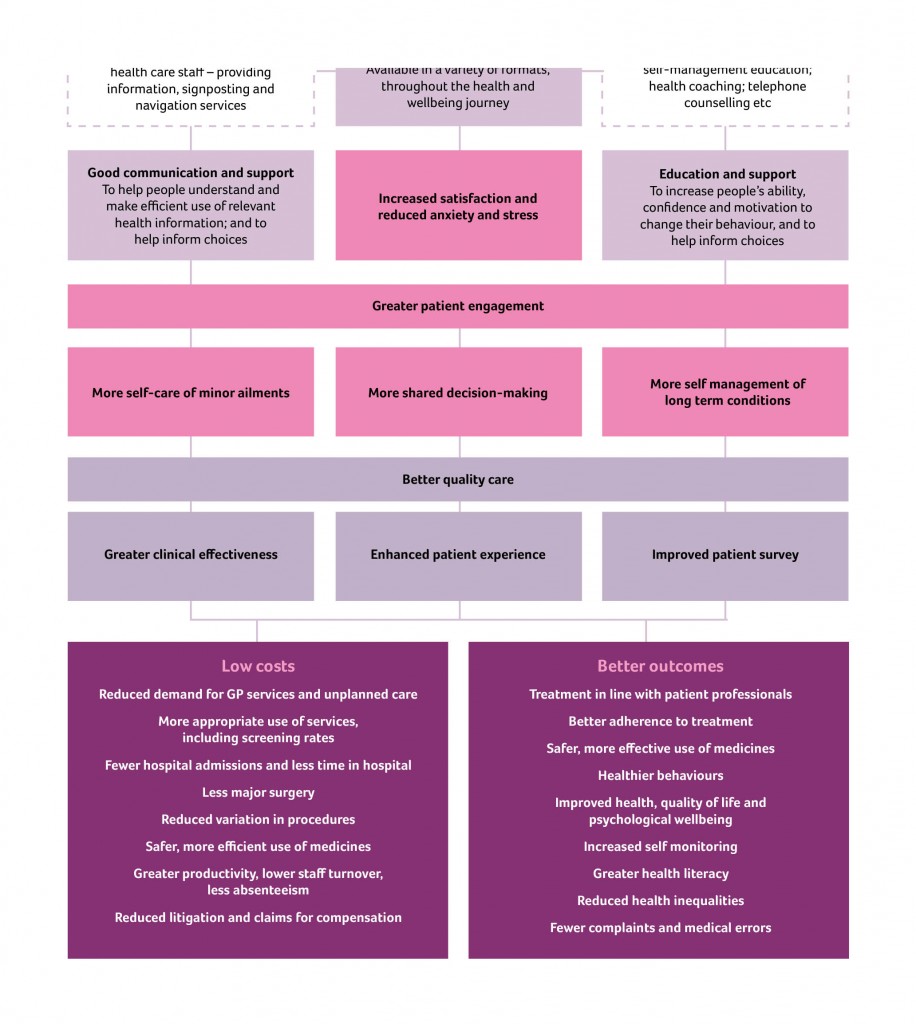
The Oldham Commission view health and wellbeing boards as a vehicle for collective system leadership for whole person care,” involving the leaders of existing organisations working together to coordinate care and align incentives across their geography.” And therefore it is critically important that they are fluent in what wellbeing is, and how to promote it. This is especially important for dementia, but I would say that wouldn’t I.
Information is obviously vital in decision-making along a path to wellbeing however defined. I, in fact, devote a whole chapter to decision-making in my book ‘Living well with dementia’.
The exact mechanism of integration of voluntary organisations and health and care services to provide a combination of medical and non-medical support as part of the care pathway for older people living with multiple long term conditions needs of course to be put under greater scrutiny.
The ‘deal‘ between the Department of Health and the Alzheimer’s Society in promoting ‘Dementia Friends’ is of course welcome in promoting awareness of dementia. But we do need to be careful that, firstly, other dementia charities do not suffer in a ‘zero sum gain’ manner. Secondly, we need to be doubly sure that charities are not expected to pick up any shortfall in state provided services. Already there’s valid criticism of the way in which private companies can legitimately ‘cherry pick’ services to maximise their shareholder dividend.
Oldham’s group is right to refer to “a strong evidence base now exists to target key risks to health independence and wellbeing in old age.” Clearly there’s a balance to be struck between independence through assistive technologies perhaps of persons living with dementia in their own homes, and social inclusion with other persons face-to-face. Online communities offer great value for persons with dementia nonetheless.
Oldham’s team also helpfully reviews how Preventive aspects of whole person care must therefore pay attention to environmental factors. The emphasis in the Report is on diet, but this is valid too for dementias in the context of vascular dementias. Vascular dementias are common in older age groups, and certainly medical professionals, dieticians and others are keen at considering cholesterol and diet, and their interaction with other factor such as smoking.
Therefore, one of the conclusions is that, “Whole person care should not only include joining up services …”
It is inescapable that whole person care should include ‘joined up services’. Data sharing different disciplines, despite the concerns about #caredata, needs to involve a more effective dialogue with the general public, one expects.
The report also picks up on a number of other important issues.
One is the possible interaction with benefits. People with disabilities, for example, are right to wonder if benefits might be taken away if the system drives towards ‘whole person care’. On the other hand, it does not perhaps make intuitive sense for the care and benefits situation to work in isolation?
This is of course an intense political quagmire, given ATOS’ role in both the GP extraction scheme and the implementation of the much criticised disability and employment benefits.
Also, it turns out that 70% of people over 75 live with a major long term condition and a quarter live with two or more. Many persons living with dementia also live with otherconditions.
Furthermore, the Report notes that, “in all groups in society, housing has a large impact on people’s health and wellbeing.” As perhaps care embraces personhood in the true meaning of Kitwood or otherwise, the influences of other people in society, such as housing or the criminal justice system to name but a few, may become apparent.
But what the State is by that stage is anyone’s guess. In the meantime, the Oldham Report is fully consistent with my book ‘Living well with dementia’.
I had expected this to be the case. In fact, there’s a paragraph on whole person care in my book.
Living well with dementia – lessons for ‘whole person care’
There were of course huge structural problems in the much heralded Oldham report on whole person care was published this week.
It’s officially called ‘One Person, One Team, One System‘.
These structural problems are, not least, to what extent will the NHS be paid for out of general taxation in the long term. The issue is not fudged altogether, in that Oldham calls for a future government to look into this as a priority.
Nonetheless, the Oldham Commission does fudge the issue of how much integrated and social care systems can rely on private not state provision. This is a strange ‘elephant in the room’, given the emphasis of the report on individualised budgets (call them what you will, personal budgets or personal care budgets).
Oldham does however concede helpfully that ‘financial arrangements in the adult social care system are equally fragmented, with complex and overlapping funding and provision arrangements between private and public funding sources, and private and public providers of care. The multitude of private care providers adds to this complexity.’
The need to repeal section 75 Health and Social Care Act is pivotal to all this. In fact, a repeal of the whole Act, as Labour (as Andy Burnham and Ed Miliband have indeed promised), would be helpful. This is, quite simply, because legally integration might offend the competition legal infrastructure established by section 75 and its associated Regulations, and of course sit uneasily with EU competition law.
At the moment, the NHS and social care services are geared up to ‘reacting to events’. And this is reflected in the payment by results mechanism (a reincarnation of ‘activity based costing’).
“Public funding has increasingly focused on those with greatest needs – particularly as rationing of care has become more severe – driven by a reactive, crises oriented approach rather than a focus on early intervention and wellbeing.”
Wellbeing is of course not just the opposite of illbeing, though lessons can be learnt from poor hydration and nutrition, for example, in individuals with advanced dementia.
The Oldham Commission view health and wellbeing boards as a vehicle for collective system leadership for whole person care,” involving the leaders of existing organisations working together to coordinate care and align incentives across their geography.” And therefore it is critically important that they are fluent in what wellbeing is, and how to promote it. This is especially important for dementia, but I would say that wouldn’t I.
Information is obviously vital in decision-making along a path to wellbeing however defined. I, in fact, devote a whole chapter to decision-making in my book ‘Living well with dementia’.
The exact mechanism of integration of voluntary organisations and health and care services to provide a combination of medical and non-medical support as part of the care pathway for older people living with multiple long term conditions needs of course to be put under greater scrutiny.
The ‘deal‘ between the Department of Health and the Alzheimer’s Society in promoting ‘Dementia Friends’ is of course welcome in promoting awareness of dementia. But we do need to be careful that, firstly, other dementia charities do not suffer in a ‘zero sum gain’ manner. Secondly, we need to be doubly sure that charities are not expected to pick up any shortfall in state provided services. Already there’s valid criticism of the way in which private companies can legitimately ‘cherry pick’ services to maximise their shareholder dividend.
Oldham’s group is right to refer to “a strong evidence base now exists to target key risks to health independence and wellbeing in old age.” Clearly there’s a balance to be struck between independence through assistive technologies perhaps of persons living with dementia in their own homes, and social inclusion with other persons face-to-face. Online communities offer great value for persons with dementia nonetheless.
Oldham’s team also helpfully reviews how Preventive aspects of whole person care must therefore pay attention to environmental factors. The emphasis in the Report is on diet, but this is valid too for dementias in the context of vascular dementias. Vascular dementias are common in older age groups, and certainly medical professionals, dieticians and others are keen at considering cholesterol and diet, and their interaction with other factor such as smoking.
Therefore, one of the conclusions is that, “Whole person care should not only include joining up services …”
It is inescapable that whole person care should include ‘joined up services’. Data sharing different disciplines, despite the concerns about #caredata, needs to involve a more effective dialogue with the general public, one expects.
The report also picks up on a number of other important issues.
One is the possible interaction with benefits. People with disabilities, for example, are right to wonder if benefits might be taken away if the system drives towards ‘whole person care’. On the other hand, it does not perhaps make intuitive sense for the care and benefits situation to work in isolation?
This is of course an intense political quagmire, given ATOS’ role in both the GP extraction scheme and the implementation of the much criticised disability and employment benefits.
Also, it turns out that 70% of people over 75 live with a major long term condition and a quarter live with two or more. Many persons living with dementia also live with otherconditions.
Furthermore, the Report notes that, “in all groups in society, housing has a large impact on people’s health and wellbeing.” As perhaps care embraces personhood in the true meaning of Kitwood or otherwise, the influences of other people in society, such as housing or the criminal justice system to name but a few, may become apparent.
But what the State is by that stage is anyone’s guess. In the meantime, the Oldham Report is fully consistent with my book ‘Living well with dementia’.
I had expected this to be the case. In fact, there’s a paragraph on whole person care in my book.
My book launch of “Living well with dementia” – special guest messages from Peter, Kate and Norman
I held a private book launch for guests of mine, who are interested in dementia at the grassroots level.
The talk was dedicated to Charmaine Hardy (@CharBHardy), whose husband has a very rare type of dementia known as primary progressive non-fluent aphasia. The publishers picked her poppy to be the cover of my book.
This for me, as was later suggested, as the book itself is dedicated to the memory of my late father (who did not have dementia but had a severe back pain which severely limited his quality of life in his final years.)
A special mention to Thomas Whitelaw (@tommyNTour) – a true gentleman and a Scot (!)
It was wonderful to meet Darren (@MrDarrenGormley) for the first time. Darren’s clearly someone who sees the person; with superb empathy skills, Darren and colleagues will need to be the change catalysts to break down obstructive silos.
It was a massive honour Beth Britton (@BethyB1886) could make it. Beth, like many in the room, of course knows this subject inside-and-out, and I am personally grateful to Beth for campaigning for the use and validation of more effective assessment of wellbeing approaches.
Here are some happy photos of my book launch.
I really couldn’t have been happier.
I am strongly against promoting my thesis about wellbeing with involvement of people as marketing ‘window dressing’
On the other hand, it gives me enormous pride to present to you the video presentations recorded by Norman McNamara, Kate Swaffer and Dr Peter Gordon which I played to my guests at the Arlington Centre in Camden on Saturday.
Friends of mine, who happen to be currently living with dementia, are also reading the book.
I mention during my presentations the ‘Purple Angels’, including Lynette Richards, Julie Line, Kim Pennock, Jane Moore, and of course Norman McNamara.
And no I am not a retainer from Ostrich Care! x
I feel it would have been it would have been “defeating the object”, if the book could not be read by people living lives with dementia.
Dr Peter Gordon is the only one of the three who does not have a dementia. He is a Consultant Psychiatrist working in this field. It was incredibly nice of him to put together his film for me, shown below.
Kate Swaffer (@KateSwaffer)
Norman McNamara (@norrms)
Dr Peter Gordon (@peterDLROW)
Living Well with Dementia from omphalos on Vimeo
Contents
Dedication • Acknowledgements • Foreword by Professor John Hodges • Foreword by Sally Ann Marciano • Foreword by Professor Facundo Manes • Introduction • What is ‘living well with dementia’? • Measuring living well with dementia • Socio-economic arguments for promoting living well with dementia • A public health perspective on living well in dementia, and the debate over screening • The relevance of the person for living well with dementia • Leisure activities and living well with dementia • Maintaining wellbeing in end-of-life care for living well with dementia • Living well with specific types of dementia: a cognitive neurology perspective • General activities which encourage wellbeing • Decision-making, capacity and advocacy in living well with dementia • Communication and living well with dementia • Home and ward design to promote living well with dementia • Assistive technology and living well with dementia • Ambient-assisted living well with dementia • The importance of built environments for living well with dementia • Dementia-friendly communities and living well with dementia • Conclusion
Sample chapter
The slides of the presentations
Reviews
Amazing … A truly unique and multi-faceted contribution. The whole book is infused with passion and the desire to make a difference to those living with dementia…A fantastic resource and user guide covering topics such as communication and living well with dementia, home and ward design, assisted technology, and built environments. Shibley should be congratulated for this unique synthesis of ideas and practice.’
Professor John R Hodges, in his Foreword
‘Outstanding…I am so excited about Shibley’s book. It is written in a language that is easy to read, and the book will appeal to a wide readership. He has tackled many of the big topics ‘head on’, and put the person living with dementia and their families at the centre of his writing. You can tell this book is written by someone who ‘understands’ dementia; someone who has seen its joy, but also felt the pain…Everyone should be allowed to live well with dementia for however long that may be, and, with this book, we can go some way to making this a reality for all.’ –Sally-Ann Marciano, in her Foreword
Extracts from my talks
This talk was given by me (Dr Shibley Rahman) on Saturday 15th February 2014 to a group of personally invited guests. Guests included persons with dementia, carers (past and present), campaigners, academics in social care, innovation and service provision, dementia club coordinators, and dementia nursing specialists.
1. This is the first segment of the first talk.
Particular things to look out for include:
James Murray-White (@sky_larking) 6 mins
Beth Britton (@BethyB1886) 7 mins
and their @AlzheimersBRACE work
Norman McNamara’s message at 15 mins
@mason4233 (Chris Roberts)’s tweet at 19 mins
2. I start off by thanking Prof John Hodges for his kind Foreword (0) and a clear description from Sally Marciano (@nursemaiden) why she, kindly, felt the book might be helpful. I am honoured at Sally’s personal contribution to my book.
I introduce the topic of personhood, using Tom Kitwood’s seminal work as a brief introduction only, but clearly the topic is huge. I then touch upon the practical difficulties academics and practitioners have had for their definitions of ‘living well’, and the implications therefore for its measurement.
There’s a clearly a debate to be had about why diagnosis might have been so problematic, using @edanaming’s research (Edana Minghella) as a springboard. At around 9’55”, I then use the problems in giving a potential diagnosis of dementia to a person is LGB or T as an illustration.
Gill Phillips (11′ 30″) kindly gives a brief description of the background and philosophy behind ‘Whose Shoes’, a modern application of personalisation which allows service users, including persons and patients with dementia, a say on what they wish to achieve from their person-centred care.
At around 16’30” Lucy Jane Masters (@lucyjmasters), a specialist nurse in dementia, explains the remarkably successful ‘Dementia is my business’ initiative, innovative badges which have acted as an ‘ice breaker’ for bringing about a cultural change in dementia care even amongst health professionals.
This next segment concludes with a brief discussion of the ethical issues of diagnosis, through Dr Peter Gordon’s contribution (@PeterDLROW). I use Peter’s letter to the BMJ as an introduction to the seminal four ethical principles of Beauchamp and Childress (1979), i.e. autonomy, beneficence, non-maleficence and justice. I also include Peter’s video which I will also separately upload elsewhere.
3. I then give an overview of some essential topics germane to this academic debate.
The contributions by the medics have not been a complete farce.
There’s been a lot of scrutiny about the ethical framework regarding dementia from people who are medically qualified, such as Dr Peter Gordon (@peterDLROW), Consultant in dementia. This was been necessary to neutralise some of the potent fraudulent memes in the media from elsewhere.
There’s been wonderful work too by @nchadborn on including service users’ views and opinions into the design of health services, from an applied perspective, as part of Nottingham University.
And the cognitive neurologists have been important in delineating the diverse cognitive presentations of dementia. Prof Facundo Manes’ group in Buenos Aires (@manesf) have been identifying how social cognition in the behavioural variant of frontotemporal dementia can be heavily dependent on context. As an example of this, I explain the Ebbinghaus Illusion and Titchener circles. Prof Manes is a colleague of ours in cognitive neurology, and wrote one of the Forewords to my book.
4. Particular things to look out for now include:
12″ Personal dedication to Charmaine Hardy [@CharBHardy] from England for the poppy on the front cover of my book, and being a key member of the #dementiachallengers
15″ The “Purple Angels” in raising dementia awareness and dementia friendly communities worldwide narrative. Jane Moore and Norman McNamara jointly designed this motif.
21″ beginning of the message by Kate Swaffer (@KateSwaffer), based in Adelaide, Australia, to my guests. (this is the beginning of the pre-recorded message; the second half of the message is in a different video.)
5. This last segment of my recordings contains the second part of Kate Swaffer’s message to my guests, and my film ‘Love is a wonderful thing’ for my community of delegates for the book launch.
The book
The book’s Amazon page, with some testimonials, is here.
The publishers’ page (Radcliffe Publishers) is here.
Independent blogposts by Gill Phillips (one of my guests) about my book launch at the Arlington Centre
These blogposts capture for me what was an extremely happy occasion for me.
‘Living well with dementia’ – the launch of Dr Shibley Rahman’s ground-breaking book
In the shoes of … | Dr Shibley Rahman. An intriguing and unique academic
Specialised organisations of persons with dementia and carers are needed to promote the wellbeing agenda
One of the biggest illusions, and this is not a ‘complaint’ about this jurisdiction only, is that large dementia charities represent the views of persons with dementia.
They have a myriad of different influences, and certainly it has become dangerous that they legitimise policy directions from which many persons with dementia and caregivers can become totally disenfranchised.
This leaves persons with dementia two options.
The first option is that they can hope to influence large dementia charities better, but this is an impossible task. They act in organised corporate ways, with much marketing and branding power, so if they decide not to adopt the agenda of persons with dementia and carers it would not be altogether surprising.
The second option is to form strategic alliances with general patient groups, but not all persons with a long term condition are ‘users’ of healthcare services which thus far have typically concentrated on illness rather than health.
The third way, and this is in my opinion the most realistic option is to organise better a national and international network of groups focused on the needs of, and run by, persons with dementia.
There are, however, very impressive carers organisations, and many of their competences and aims align with the person-driven agenda for wellbeing.
The uphill task for those of us pursuing a living well with dementia agenda is truly formidable. Cholinesterase inhibitors, the frontline drugs for treating memory problems in Alzheimer’s disease, have annual sales in the billions, but have very modest effects in the vast majority of patients. They do not reverse or markedly slow down the disease either.
I feel that getting in lost in a definition of wellbeing, and how we measure it, is not the way to win the argument, although clearly relevant to how commissioning for integrated care might happen in future, say through value-based commissioning.
I feel arguments based on cause and effect will be more compelling (and easily supported by supporting evidence). That is, memory reminiscence techniques, improving the design of homes and wards, and introduction of innovations such as the ‘Dementia Dog’, which clearly have had a beneficial outcome for many, are options worth pursuing.
The ’cause’ of attracting monies for high quality research, acting as a foundation for pharmacological interventions, is a very worthy one. As someone who has published in this arena in international journals, I certainly don’t have any weird ideological objection to such work.
But we have to acknowledge, albeit reluctantly, that the world is changing, and whether some of us like it or not becoming more “consumer-driven”.
Citizens have become consumers with status proportional to purchasing power, and there’s now a fine line between data gathering of your personal lifestyle preferences through the ‘recreational’ social media and direct targetted marketing of things to improve your health or prevent illness.
The ultimate prize for industry is to determine government policy, but smaller organisations cannot compete against the large corporations, many of which contribute generously to political organisations too.
Where wellbeing campaigners lobbying may not succeed on economic power, their organising ability might succeed on the basis of facts and logic, in seeking out a constructive alternative to the existing policy, practice, or product.
It is often said that the basic rule of pressuring targets is that politicians react to publicity that reflects on their character, bureaucrats react to disrupting their provision of services and programmes, and corporations react to loss of their product’s reputation.
Wellbeing is an agenda for which politicians could have, and have had, much affinity.
If regulations are to be implemented, it’s often possible, hijack or “capture” the regulatory process. This can become easy if the regulatory process is biased towards a medical model of dementia, e.g. the General Medical Council and NICE, rather than social care institutions which are tacitly not given parity.
A committed opponent, who for the most part we’re not interested in reaching because debate with this individual tends to harden his or her position. Big Pharma, the General Medical Council, NICE and large dementia charities are clearly not targets to promote the wellbeing agenda.
The focus in parliament, through the All Party Parliamentary Group, and to some extent helped by powerful allies in the charity and corporate sector, has been relentlessly medical too.
Prof Felicia Huppert, to which my book is dedicated, ran a Royal Society meeting on wellbeing. There is no doubt that this was very succcessful, but we have never had a corollary in parliament.
A legislative hearing, however, gives the lawmakers the opportunity to hear all sides of an issue and to ask questions and challenge witnesses in a relatively brief span of time.
In 1991, the author Michael Frayn wrote a book, A Landing on the Sun, about a British prime minister who tasked his advisers with looking into happiness and what the government could do to promote it. The prize proved elusive, the adviser went mad and died.
Even in November 2010, speaking at the Google Zeitgeist Europe conference, David Cameron suggested, “Wellbeing can’t be measured by money or traded in markets.”
“It’s about the beauty of our surroundings, the quality of our culture and, above all, the strength of our relationships. Improving our society’s sense of wellbeing is, I believe, the central political challenge of our times.”
And this agenda has not sprung out of nowhere.
Aristotle talked about “eudaimonia” – happiness as human flourishing and purpose to life – rather than the modern hedonistic concept. John Maynard Keynes talked about the “art of life” in 1930, and in 1968 Bobby Kennedy told a student audience in Kansas: “We cannot measure national spirit by the Dow Jones average, nor national achievement by the gross domestic product.”
Tacrine was the prototypical cholinesterase inhibitor for the treatment of Alzheimer’s disease. William K Summers received a patent for this use (US Patent No. 4,816,456). Studies found that it may have a small beneficial effect on cognition and other clinical measures, though study data was limited. and the clinical relevance of these findings was unclear.
Tacrine was ultimately discontinued in the US. Unfortunately, it is associated with transaminase elevation in up to 50% of patients. The mechanism of tacrine-induced liver damage is not fully understood, but earlier studies have suggested that genetic factors may play a role.
And now leading Big Pharma companies are involved in an ‘arms race’ to get their drugs to market, and they have powerful allies in large dementia charities worldwide.
Both the AstraZeneca and Merck medicines work by blocking an enzyme called beta secretase that is involved in production of beta-amyloid, a protein that creates brain plaques considered a major cause of Alzheimer’s disease.
Such oral drugs are known as BACE inhibitors and are viewed as a promising new approach to fighting the memory-robbing condition.
BACE inhibitor drugs have taken centre stage after an injectable class of medicines targeting beta-amyloid plaque failed or fell short in trials conducted by Pfizer and Eli Lilly.
Not all experts accept that reducing beta-amyloid is the key to defeating Alzheimer’s, however, and the safety of the new BACE drugs has also been a subject of concern after Lilly pulled the plug on its product due to liver toxicity.
Unlike heart disease and cancer, no major advancements have been seen in Alzheimer’s drug research since the first treatment was approved in 1993 by U.S. regulators.
Of course, the push away from the relative failure of the drug industry should not be the only reason to pursue living well with dementia.
Being disciplined and organising specialist groups to represent only the needs of persons with dementia, both nationally and internationally, will be the only way to promote living well with dementia in the current environment.
They need to ‘capture’ research grant processes, such that we know what psychological interventions work too. They need to ‘capture’ service provision design.
A problem has been the cosiness between the large charities and the Pharma agenda. It is virtually impossible now to detect and act upon material conflicts of interest.
It’s not impossible that the sheer numbers of interested people can act as one large external radical for change. A new organisation, Dementia Alliance International, holds already substantial promise for advocacy for people living with dementia. There is also monumental size of influence of ‘the Carers’ Call to Action’ from the Dementia Action Alliance in this jurisdiction. And size is power.
But I don’t really feel that it should be a competition. The risk, nonetheless, of totally ignoring persons with dementia, their friends, family, or carers, is that the more you ignore them, they more they’ll come back.
Or as Labi Saffre said, “”The higher you build your barriers, the taller I become.”
A week to go
The numbers are very tight because of the venue in Camden.
Do you remember when you used to prepare Cocoa Pops cakes for kids’ birthday parties? Yes, it’s at least that level of excitement and more.
But I am now extremely excited about our private get-together to talk about issues raised in my book ‘Living well with dementia‘. Thanks to Amazon (at last), this book for the time-being is available to order for next-day delivery.
Not being invited to my private book launch, however, has absolutely no significance.
The venue is very small, and it’s been very difficult co-ordinating it thus far.
The guests are: Beth Britton, Charmaine Hardy (and sons), Darren Gormley, Edana Minghella, Gill Phillips (‘Whose Shoes’), Rachel Niblock, James Murray-White, Jo Moriarty, Lee, Lucy Jane Marsters, Margaret Kilby, Marian Naidoo, Mike Clark, Neil Chadborn, Dr Peter Gordon, Shaun Naidoo, Simona Florio, Thomas Whitelaw, Vidal Andreas, Amanda Ramsay, Gillian Nineham, Shirley Ayres, Zoe Harris, Ken Howard, Sally Marciano, Jane Samuels and Tony Jameson-Allen.
I’ve never met some of my guests, but I know them all well through Facebook or Twitter.
It has the feeling of a wedding reception in fact.
I wonder if I should get some special badges for what is effectively a #tweetup?
Indeed, I am looking forward to thanking Charmaine in person for permission to use the photography of her poppy – which was chosen by my publishers out of the ones proposed to them.
I’m also hoping Dr Mitul Mehta and family will be able to ‘drop in’. Despite being a Senior Lecturer at the world-famous Institute of Psychiatry, in their neuroimaging division, Mitul found my discussion of the problems in early cognitive diagnosis of dementia helpful. I also made him read my book recently!
I am excited that Tommy Whitelaw has accepted an invitation to come from Scotland. The distance is perhaps prohibitively long, but in any case I will be massively singing Tommy’s praises. Tommy is genuine. And he’s also a Glaswegian! An amazing contributor, who’s made a massive paradigm shift through his groundbreaking work with Alliance Scotland.
Norman McNamara, in the spirit of all good awards ceremonies, ‘can’t be there’ (the distance from Torbay is prohibitively long.) Nonetheless, Norman is recording a message on YouTube which I hope to be playing in our book launch. It’s impossible to give an account for Norman’s unique accomplishments in this area.
Not only has Norman got a huge amount of organic goodwill and love for his ‘Purple Angel Ambassadors’, but Norman has brought about a discussion on the potential merits of GPS trackers to mitigate against wandering. Whatever one’s precise views, which tend to be always sophisticated and deeply felt, this debate is much needed in my view. I am trying to make suitable arrangements for Purple Angels themselves to be represented in person.
It would be very early for Kate Swaffer to ‘Skype’-in, for Sunday morning her time in Adelaide. I am thinking of recording message by Kate especially for my guests. Kate, living with a dementia, is one of the most well liked and respected advocates for dementia internationally.