Home » Posts tagged 'General Medical Council'
Tag Archives: General Medical Council
The perfect storm around #BawaGarba was a long time coming
As a result of my erasure in 2006 from the register of medical professionals in the UK, I had a lot of time to reflect on the events leading up to it. I have from time to time also reflected on this following my restoration in 2014. In the meantime, I had re-trained in law, paradoxically inspired by my experience of the judicial process. This was not a brief Masters in medical law, but both my Bachelor and Masters of Law, as well as the pre-solicitor training course. To do the last bit, I had to be approved as a fit and proper person by the legal regulator, the Solicitors Regulation Authority. I enjoyed my study of the English legal system, and reflect that if I had never studied law I would never have met the late Prof Gary Slapper – a formidable academic with an interest in conspiracy theories and corporate manslaughter.
This is all rather awkward, not least because Charlie Massey and Jeremy Hunt get on well, despite having divergent views on the implications of the #BawaGarba judgment. In a way, the General Medical Council (GMC) does not actually do ‘personal’, although ensuing events do rather appear like a hate campaign. It has become traditional to issue a sop to the ‘victim’ of misfeasance of a Doctor, and I do genuinely feel that there can be few things worse than the mental anguish of a grieving relative. The GMC and Medical Practitioners Tribunal Service maintain separation of powers, and, whilst I feel that the GMC can move in mysterious ways, I feel that the GMC believe that they are doing their very best to maintain public safety and confidence in the medical profession. This blogpost is therefore not an easy one to write, and inevitably will mean that I could accidentally cause offence. I am reflecting on issues to the best of my ability, and, if I fall short, I do apologise.
#BawaGarba found herself in a perfect storm. There are various systemic factors arguably out of direct control of the GMC. These are the exact funding of the NHS, including whether there is a sufficient number of doctors on rotas in individual hospitals. Notwithstanding, the GMC has a statutory duty in education and training, and, from what I know, will intervene in cases where NHS Trusts offer a suboptimal training experience. But there are important other systemic factors. It is quite common for non-white British trainees, once a GMC alert has been triggered, to be ‘thrown to the wolves’ from the regulatory process, but whether this achieves statistical significance is worth exploring. The trend has been for, once these Doctors have been reported, for all positive references to be withdrawn, and, often, although the source of the leaks are never identified, for the Doctors to receive a barrage of unfavourable press prior to any hearing. A media presence seems to defy any traditional notion of contempt of court, or right to a fair trial, as Doctors are subject to a total monstering and humiliation in the media. But it is not uncommon for papers in the English media, and their class of readers, also to subject groups of Doctors, such as EU Doctors, to an utter monstering as well, allowing xenophobia and outright racism to flourish. The scope for moral panic is enormous. But to lay these problems at the foot of the GMC, I feel personally, is unfair.
The GMC indeed also has an important statutory duty for patient safety under section 1 of the Medical Act 1983. The “There but the grace of God go I” used alarmingly frequently by white, English doctors on Twitter might reflect the observation that some Doctors are safer from attacks from institutional racism than others. This is particularly problematic if the NHS Trusts continue on its trend to trigger an official regulatory complaint effectively to cover their own backs rather than a genuine attempt to improve the performance, health and wellbeing of their Doctors employed under employment contracts. This has indeed been witnessed in the enforcement of the junior doctors’ contracts, arguably. Also, the “There but” observation is also problematic from the point of view that it seems to signal an admission that registers an admission that registered Doctors go to work knowingly taking risks and making mistakes. Most Doctors will admit to having taken risks and having made a mistake, and the number of mistakes reported daily in the NHS, a mere fraction of the real number, must urge a need for an open and transparent culture where people can learn from mistakes. But the GMC and the higher courts will tend not to tolerate any mistakes, or catalogues of error, whatever the mitigating factors. This might include an unblemished record for 30 years. The issue is that if the performance is way below a standard, there can be no excuse for it. If somebody has died, the threshold for mitigation has to be high, most reasonable persons might argue. And if a court of law has found someone guilty of manslaughter, whatever the process involved for doing so or the people involved, it is hard to leave no sanction on the Doctor, it is argued, whatever the need for organisational learning. Both the GMC and higher courts have consistently argued that public trust and confidence in the medical profession are more important than any individual doctor’s career.
The argument that ‘We go to work and are caught between a rock and a hard place’ merits scrutiny too. This comes down to the nature of how a crime is satisfied in English law – there can be intention to do the crime, and, although there is some finesse about the jurisprudence, there might be recklessness. The law in this is fairly well settled since R v Adomako. It might seem unfair to blame a Doctor having to cover seven bleeps one morning, but the point in law is that the Doctor by carrying those bleeps has assumed a duty of care to his or her patients, and any breach therefore of this duty of care, given the issues of causation and remoteness, is negligence. It might be argued that in tort the Doctor has assumed this responsibility under duress, but in reality most Doctors pick up the bleep from an office in the Hospital without any altercation. And Doctors are entitled to resign if they feel that there has been a fundamental breach of a contract, including a bilateral feeling of trust and confidence, between employer and employee. In reality, Doctors never do, despite the potential risks for patient safety.
Whilst there might be outrage about the lack of due emphasis on organisational learning, this organisational learning nor indeed any individual duty of candour are operational at any meaningful statutory level, meaning they exist in an Act of parliament or statutory instruments. And nobody is above the law. If there had been no sanction on #GawaBarba, a possible interpretation might have been that mistakes, whatever the reason, are excusable because of the ‘state of the NHS’. It might then be argued that the correct course of action might be for corporate manslaughter against the Secretary of State for health and social care, for ‘avoidable deaths’, but this has to be proven beyond reasonable doubt – an incredibly difficult offence to fulfil, as the late Prof Gary Slapper I am certain would testify.
I doubt, if #BawaGarba finds herself back on the GMC Register, she will find it easy to find employment again, especially with at least a five year gap in training. The GMC, even with its statutory duty for education and training, as well as patient safety, seems pretty indifferent to the professional rehabilitation and retraining of Doctors put back onto their Register. But the observation that no Doctor can ever be professional rehabilitated does concern me, even with the strong emotions that the ‘punishment should fit the crime’, and the need for a scalp can be overwhelming. For example, #BawaGarba has found that her subsequent good performance had become somewhat irrelevant as far as the regulator and higher courts were concerned.
As the old trope provides, there are no winners. There are only losers. It’s said that the GMC ‘doesn’t do personal’ in the same way a sanction is delivered in the same way a parking ticket is issued, and the GMC’s purpose isn’t, it is argued, to do ‘show trials’. The GMC’s position is that they are not in the business of ‘punishing Doctors’, but, I feel, it is of concern that unintended consequences, including a culture of fear, could continue to be dominant in the medical profession. The GMC doesn’t likewise, perhaps reflecting their perceived concerns from the general public, want to allow free rein on Doctors ‘free to make mistakes’, and good doctors will argue that they are all trying to do the job to ‘the best of their abiility’. The problem facing the GMC is whether ‘the best of someone’s ability’ is simply good enough. The general approach is that there is no shortage of doctors, and it is a honour to be a registered doctor. Whether there is a sufficient number of doctors for the demand is a concern the GMC can decide to involve itself with, or not. There is a clause in the code of conduct – Good Medical Practice, 2013 – stating that it is the responsibility of doctors to identify any shortfall of resources. I doubt all the senior Consultants or even STs in training taking to Twitter outraged about the #BawaGarba judgment are writing this morning to the GMC to warn about shortage of resources in their own hospitals, despite concerns about patient safety. It is noteworthy that the GMC in their statement on the case mentioned this only yesterday even. But individual Doctors have also been rather effective at protecting their own backs?
I can see why some Doctors would be driven to suicide. I was mentally ill, and felt the same with the GMC FTP.
At least 96 doctors have died while facing a fitness-to-practise investigation from the General Medical Council since 2004, though it is not clear how many of these cases were suicide.
I can understand exactly how this has happened.
I had a prolonged GMC investigation between 2004 and 2006. At no point during this process was I told when then this mentally arduous process would come to an end.
I think now, seven years into recovery, that there by the grace of God go I.
The media have a remarkably high level of detail of understanding from the perspective of the General Medical Council about forthcoming cases. It is impossible for the Doctor to get his side across in the media.
The GMC claim they don’t do show trials.
But my father was fully humiliated with the media storm.
My father was faced with a Doctor son who was in denial and lacked insight. My father is now dead, but I should like to say he probably died in complete humiliation of his son.
My experience is of a GMC which plays to people’s weaknesses in low self esteem and low confidence, a personality trait shared by many with addiction disorders.
Not one report in the mainstream media reported that I was severely alcoholic. And yet the GMC, prior to their erasure of me, erased me with five independent reports stating clearly that I had at least a severe alcohol problem; and that I needed help.
One of the referrals to the GMC was when I attended the A&E of a hospital with acute intoxication. In addition to the referral to the GMC by the Consultant in A&E, I was not offered any post-event support for alcoholism.
The GMC know how to present themselves in the media, but this is in contradistinction to the experience of those who have experienced the Fitness to Practise process first hand.
Dr Peter Wilmhurst writes in 2006 in a wide-ranging criticism of the GMC as follows:
In wishing to infer ‘bad character’, the General Medical Council must not go beyond its statutory duty of promoting public safety. Otherwise, there is simply mission creep and a torrent of smears into a hate campaign by the regulator or its company.
In 2005, one year before I was eventually due to see the GMC, I was suspended. This was due to an alcoholic bender in Northwick Park. I was crying all day in a pub because I could not cope with the investigation any more.
I had waved goodbye to my late father, and lied to him saying I was going shopping.
I didn’t. I ended up being sectioned by a psychiatric hospital in North London, and my father spent ages talking to the medical staff there.
I was then suspended. It was at that point, I wished to call it a day.
I phoned the Samaritans, and they talked me out of it.
I have never told anyone this story. I feel very strongly about what the General Medical Council did to me, even though it might have been merely a product of their inefficiency.
Nobody appears to wish to want to change the system. I’m pretty sure that there are juniors who wish to hold tight until they are Consultants.
What happened to me is that I had consultants in two Trusts in West and North London who said I was ‘late for work’, ‘smelling of alcohol’ and ‘dishevelled’.
None of this got reported in the main media.
I was erased. To this day, I still have no idea who retrospectively complained in graphic detail about my alcoholism did not offer me sick leave, or help with occupational health.
One of them even had the gall to write in his witness statement for the GMC that he gave me the phone number of a private clinic.
I find this particularly ironic as I was later done for incompetence, when that North London trust had allowed me to finish my medical job there, successfully running cardiac arrests there. I passed my Advanced Life Certificate there. I even have the certificate to prove it.
I feel disgusted by the way that the General Medical Council goes about its business.
Far too many one-sided media reports appear in the media containing detailed accounts, as yet unproven. There’s a sense of being hung before you even go to the gibbet.
I am now in my seventh year in recovery. I have done four books, and my Bachelor of Law, Master of Law and Master of Business Administration.
I even completed my pre-solicitor training, as I am regulated by the Solicitors Regulation Authority.
My late father died two months before the Solicitors Regulation Authority gave me permission to finish my legal training, after a meticulous consideration of various factors including details of my erasure.
I am now applying to be restored. And so everything gets racheted up again. The dogs will get unleashed.
And so far they’ve dragged me up to the City where I was struck off, without my late father, surrounded by the same bars and clubs and restaurants. I didn’t have a relapse. Care and compassion are simply two words which are not in the GMC’s dictionary.
I am even applying to go to a desk, non “facing job”. I am now following my erasure newly disabled, so I would not wish to do clinical medicine in any form.
I do not want to be in public health with the stigma of having been erased, for a period of life when I was very ill, and the undoubted discrimination that that would entail.
I had one year of sitting in a pub all day after I was eventually erased in 2006.
This was an extremely dangerous part of life. For my father, it was unbelievably distressing. Nonetheless, he came to visit me every day on the ITU when I was in a coma due to this a year later.
I so understand why there have been so many deaths of Doctors waiting GMC FTP. That could easily have been me.
But I am fighting fit now, and looking forward to my hearing very much.
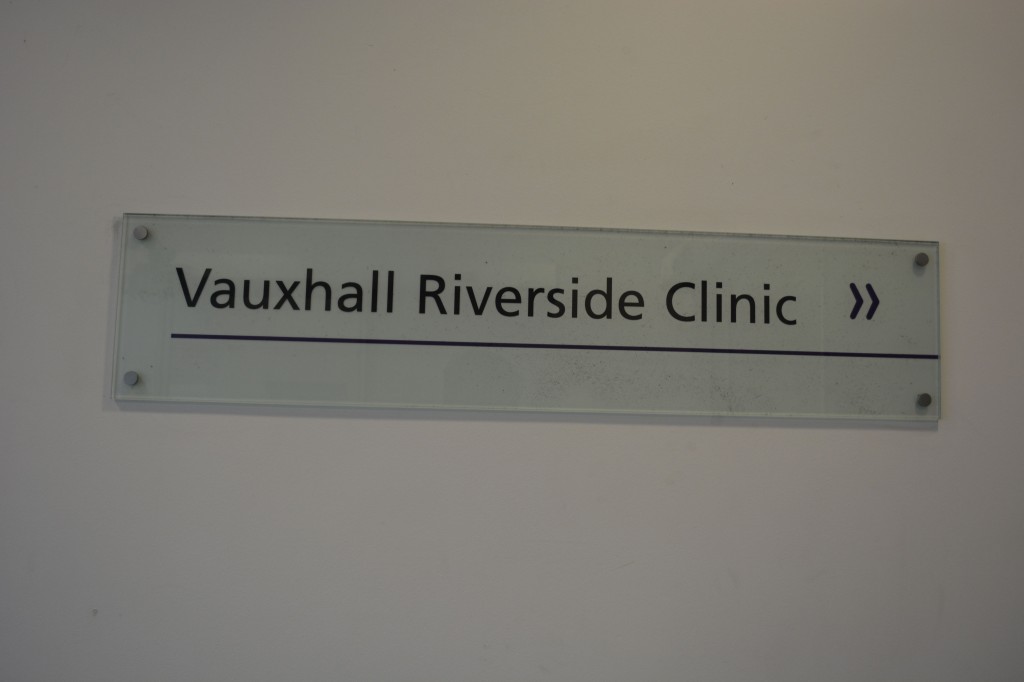
A personal statement about what I will say to the General Medical Council tomorrow morning
I will be giving my evidence tomorrow, to seek humbly restoration to the General Medical (“GMC”) Medical Register. I’m encouraged that the GMC states clearly it wishes to support sick doctors, through initiatives such as the Practitioner Health Programme, with leadership on this matter from their CEO, Niall Dickson. I intend to present my evidence to the GMC that I want to draw a line on my former self, which I do not substantively recognise at all. If anything else, I have now chronic disabilities and have pursued recovery from severe alcohol dependence syndrome since my life threatening coma of six weeks in 2007. The cardiac arrest and epileptic seizures which I had were possibly the defining end to a very painful period in my life.
I will argue that it has taken years of support from my friends to arrive at a place where I have come to terms with such an unpleasant past. I will offer a full apology to the medical profession therefore, and ask forgiveness for disgusting events which caused the medical profession disrepute. I hope that, through various books and articles on postgraduate medicine and English health policy, I have shown my commitment to a profession, which I should like to give a re-birth following a nine year undergraduate degree in medicine at Cambridge (1993-2001).
It was honour to speak to a group of suspended Doctors on the Practitioner Health Programme this morning about recovery
It was a real honour and privilege to be invited to give a talk to a group of medical Doctors who were currently suspended on the GMC Medical Register this morning (in confidence). I gave a talk for about thirty minutes, and took questions afterwards. I have enormous affection for the medical profession in fact, having obtained a First at Cambridge in 1996, and also produced a seminal paper in dementia published in a leading journal as part of my Ph.D. there. I have had nothing to do with the medical profession for several years now, apart from volunteering part-time for two medical charities in London which I no longer do.
I currently think patient safety is paramount, and Doctors with addiction problems often do not realise the effect the negative impact of their addiction on their performance. No regulatory authority can do ‘outreach’, otherwise it would be there forever, in the same way that Alcoholics Anonymous or Narcotics Anonymous do not actively go out looking for people with addiction problems. I personally have doubts about the notion of a ‘high functioning addict’, as the addict is virtually oblivious to all the distress and débris caused by their addiction; the impact on others is much worse than on the individual himself, who can lack insight and can be in denial. Insight is something that is best for others to judge.
However, I have now been in recovery for 72 months, with things having come to a head when I was admitted in August 2007 having had an epileptic seizure and asystolic cardiac arrest. Having woken up on the top floor of the Royal Free Hospital in pitch darkness, I had to cope with recovery from alcoholism (I have never been addicted to any other drugs), and newly-acquired physical disability. I in fact could neither walk nor talk. Nonetheless, I am happy as I live with my mum in Primrose Hill, have never had any regular salaried employment since my coma in the summer of 2007, received scholarships to do my MBA and legal training (otherwise my life would have become totally unsustainable financially apart from my disability living allowance which I use for my mobility and living). I am also very proud to have completed my Master of Law with a commendation in January 2011. My greatest achievement of all has been sustaining my recovery, and my talk went very well this morning.
The message I wished to impart that personal health and recovery is much more important than temporary abstinence, ‘getting the certificate’ and carrying on with your career if you have a genuine problem. People in any discipline will often not seek help for addiction, as they worry about their training record. Some will even not enlist with a G.P., in case the GP reports them to a regulatory authority. I discussed how I had a brilliant doctor-patient relationship with my own G.P. and how the support from the Solicitors Regulation Authority (who allowed me unconditionally to do the Legal Practice Course after an extensive due diligence) had been vital, but I also fielded questions on the potential impact of stigma of stigma in the regulatory process as a barrier-to-recovery.
I gave an extensive list of my own ‘support network’, which included my own G.P., psychiatrist, my mum, other family and friends, the Practitioner Health Programme, and ‘After Care’ at my local hospital.
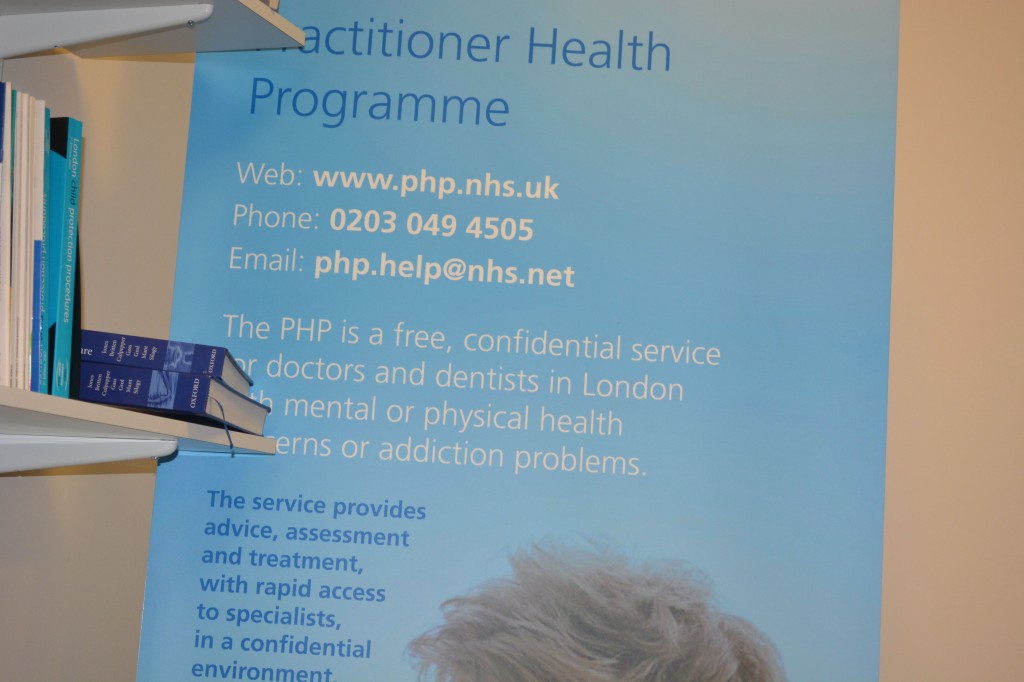
The Practitioner Health Programme, supported by the General Medical Council, describes itself as follows:
The Practitioner Health Programme is a free, confidential service for doctors and dentists living in London who have mental or physical health concerns and/or addiction problems.
Any medical or dental practitioner can use the service, where they have
• A mental health or addiction concern (at any level of severity) and/or
• A physical health concern (where that concern may impact on the practitioner’s performance.)
I was asked which of these had helped me the most, which I thought was a very good question. I said that it was not necessarily the case that a bigger network was necessarily better, but it did need individuals to be open and truthful with you if things began to go wrong. It gave me a chance to outline the fundamental conundrum of recovery; it’s impossible to go into recovery on your own (for many this will mean going to A.A. or other meetings, and discussing recovery with close friends), but likewise the only person who can help you is yourself (no number of expensive ‘rehabs’ will on their own provide you with the ‘cure’.) This is of course a lifelong battle for me, and whilst I am very happy now as things have moved on for me, I hope I may at last help others who need help in a non-professional capacity.
Best wishes, Shibley
My talk [ edited ]
It was honour to speak to a group of suspended Doctors on the Practitioner Health Programme this morning about recovery
It was a real honour and privilege to be invited to give a talk to a group of medical Doctors who were currently suspended on the GMC Medical Register this morning (in confidence). I gave a talk for about thirty minutes, and took questions afterwards. I have enormous affection for the medical profession in fact, having obtained a First at Cambridge in 1996, and also produced a seminal paper in dementia published in a leading journal as part of my Ph.D. there. I have had nothing to do with the medical profession for several years now, apart from volunteering part-time for two medical charities in London which I no longer do.
I think patient safety is paramount, and Doctors with addiction problems often do not realise the effect the negative impact of their addiction on their performance. No regulatory authority can do ‘outreach’, otherwise it would be there forever, in the same way that Alcoholics Anonymous or Narcotics Anonymous do not actively go out looking for people with addiction problems. I personally have doubts about the notion of a ‘high functioning addict’, as the addict is virtually oblivious to all the distress and débris caused by their addiction; the impact on others is much worse than on the individual himself, who can lack insight and can be in denial. Insight is something that is best for others to judge.
However, I have now been in recovery for 72 months, with things having come to a head when I was admitted in August 2007 having had an epileptic seizure and asystolic cardiac arrest. Having woken up on the top floor of the Royal Free Hospital in pitch darkness, I had to cope with recovery from alcoholism (I have never been addicted to any other drugs), and newly-acquired physical disability. I in fact could neither walk nor talk. Nonetheless, I am happy as I live with my mum in Primrose Hill, have never had any regular salaried employment since my coma in the summer of 2007, received scholarships to do my MBA and legal training (otherwise my life would have become totally unsustainable financially apart from my disability living allowance which I use for my mobility and living). I am also very proud to have completed my Master of Law with a commendation in January 2011. My greatest achievement of all has been sustaining my recovery, and my talk went very well this morning.
The message I wished to impart that personal health and recovery is much more important than temporary abstinence, ‘getting the certificate’ and carrying on with your career if you have a genuine problem. People in any discipline will often not seek help for addiction, as they worry about their training record. Some will even not enlist with a G.P., in case the GP reports them to a regulatory authority. I discussed how I had a brilliant doctor-patient relationship with my own G.P. and how the support from the Solicitors Regulation Authority (who allowed me unconditionally to do the Legal Practice Course after an extensive due diligence) had been vital, but I also fielded questions on the potential impact of stigma of stigma in the regulatory process as a barrier-to-recovery.
I gave an extensive list of my own ‘support network’, which included my own G.P., psychiatrist, my mum, other family and friends, the Practitioner Health Programme, and ‘After Care’ at my local hospital.
The Practitioner Health Programme, supported by the General Medical Council, describes itself as follows:
The Practitioner Health Programme is a free, confidential service for doctors and dentists living in London who have mental or physical health concerns and/or addiction problems.
Any medical or dental practitioner can use the service, where they have
• A mental health or addiction concern (at any level of severity) and/or
• A physical health concern (where that concern may impact on the practitioner’s performance.)
I was asked which of these had helped me the most, which I thought was a very good question. I said that it was not necessarily the case that a bigger network was necessarily better, but it did need individuals to be open and truthful with you if things began to go wrong. It gave me a chance to outline the fundamental conundrum of recovery; it’s impossible to go into recovery on your own (for many this will mean going to A.A. or other meetings, and discussing recovery with close friends), but likewise the only person who can help you is yourself (no number of expensive ‘rehabs’ will on their own provide you with the ‘cure’.) This is of course a lifelong battle for me, and whilst I am very happy now as things have moved on for me, I hope I may at last help others who need help in a non-professional capacity.
Best wishes, Shibley
My talk [ edited ]
A failure of leadership and management: toxic cultures, ENRON and the Francis Report
 Robert Francis has an incredibly difficult task. It is difficult for people who have not qualified, even managers and leaders of healthcare think tanks, to understand how this situation has arisen. Being a senior lawyer, his approach will necessarily involve “the law is not enough”. The NHS is currently a “political football”, but the overriding objective must be one of patient safety. Whatever your views about managers following financial targets religiously, and regulatory authorities pursuing their own targets sometimes with equal passion, it is hard to escape from the desire for a national framework for patient safety. This is at a time indeed when it is proposed that the National Health and Patient Safety Agency should be abolished, which indeed has oversight of medical devices and equipment. Indeed, one of the findings of the Francis Inquiry is that essential medical equipment was not always available or working. A general problem with the approach of the Health and Social Care Act (2012) has been the abolition of ‘national’ elements, such as abolition of the Health Protection Authority. (more…)
Robert Francis has an incredibly difficult task. It is difficult for people who have not qualified, even managers and leaders of healthcare think tanks, to understand how this situation has arisen. Being a senior lawyer, his approach will necessarily involve “the law is not enough”. The NHS is currently a “political football”, but the overriding objective must be one of patient safety. Whatever your views about managers following financial targets religiously, and regulatory authorities pursuing their own targets sometimes with equal passion, it is hard to escape from the desire for a national framework for patient safety. This is at a time indeed when it is proposed that the National Health and Patient Safety Agency should be abolished, which indeed has oversight of medical devices and equipment. Indeed, one of the findings of the Francis Inquiry is that essential medical equipment was not always available or working. A general problem with the approach of the Health and Social Care Act (2012) has been the abolition of ‘national’ elements, such as abolition of the Health Protection Authority. (more…)
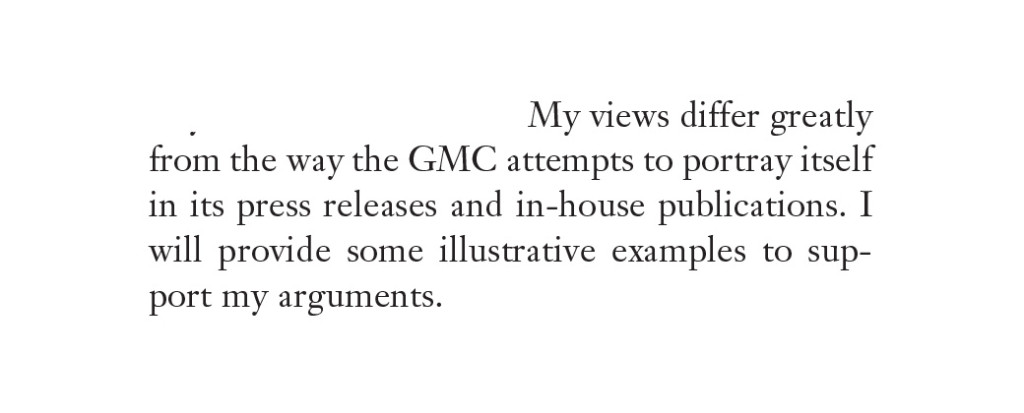
I am finally discharged from Queen Square!
Monday was a highly emotional day for me. I was finally charged from the Neurorehabilitation clinic at the National Hospital for Neurology and Neurosurgery, Queen Square.
I must say that my medical team looking after me are fantastic. A dedicated team of clinicians, including neurologists at various stages of their training, the occupational therapists, the physiotherapists, and the speech-and-language therapy (SALT) people looked after me. My father and mother used to visit me religiously every day. My mother still has memories of coming to see me during visiting hours, with cooked food. My father passed away in November 2010.
The Hospital makes me extremely proud, as I practised neurology there long before I came alcoholic. I had the pleasure and honour of being on the movement disorders, cognitive disorders and dementia, neurogenetics and general neurology teams. I think the National Hospital for Neurology and Neurosurgery, Queen Square, is the best hospital in the world. Therefore, while it gives me great happiness in that I no longer have seizures (my last one was on admission in 2007) and I am now physically almost back to normal, it is of massive unhappiness I will probably never go there again.
I still actively research in dementia, working for a leading UK charity in Alzheimer’s Disease. I love it there, as I make contributions to their groundbreaking work on quality-of-life and wellbeing in dementia environments. I will be writing an open letter to the General Medical Council, having done my two degrees in law and MBA by that stage, with 57 months in recovery in 2013. The GMC can have a careful read of the transcripts now which provide that their Consultant gave in the hearing, that if erased my drinking would explode. This is exactly what happened, and it’s well known within medicine that you’re at extremely high risk of meningitis if you drink heavily.
I currently have the privilege of being able to complete my legal training, and I still have unanswered questions of my own about the treatment of sick doctors.
I look forward to the challenge. My father insisted that I should fight this fiercely, on a matter of principle. Thankfully, I have an excellent consultant. The BBC will be interested to follow my submissions particularly. I think both the medical and legal professions are wonderful, though, notwithstanding what I’ve said. I must thank the regulators for law for looking at my case fairly which allows me to pursue my current dreams.

Shibley Rahman on why all non-prescription drugs are life-threatening to him, so he doesn’t need them
Drugs including alcohol and tobacco products are a major cause of harms to individuals and society. Some drugs are therefore scheduled under the United Nations 1961 Single Convention on Narcotic Drugs and the 1971 Convention on Psychotropic Substances. These controls are represented in UK domestic legislation by the 1971 Misuse of Drugs Act (as amended). Before 1971, the UK had a relatively liberal drugs policy and it was not until US influence had been brought to bear, particularly in the aforementioned circles, that controlling incidental drug activities was employed to effectively criminalize drugs us. Other drugs, notably alcohol and tobacco, have long been regulated by taxation, sales, and restrictions on the age of purchase.

On 3rd June 2007, I was admitted to the Royal Free Hospital at the end of several years suffering from a severe alcohol dependence syndrome 2003-2007. Alcohol treatment for me is now obligatory. I have been in recovery for 40 months, living a very fulfilled life in the abstinence of alcohol, and I now have insight into the disastrous effect it had on my personal and personal life. I was admitted to the Royal Free having sustained a cardiac arrest and an epileptic seizure, spent two months in a coma, but then emerged – not brain-damaged, but disabled.

I completed my postgraduate medical training as a physician in 2005. Whilst I am not a practising physician, I have passed all my exams that prove that I understand medicine, and alcohol-related medicine. However, I must admit to not understanding the impact of alcoholism until my recovery. I used to wake up in the morning, and have to have a ½ bottle of gin. I used to go to the news agents to buy alcohol at 11am in the morning, and I couldn’t function at all. I had lost my job in 2005 anyway, and got erased from the General Medical Register in 2006/7. The General Medical Council were aware of my problem as far back as 2003, but I was left on the general medical register until 2006 when I was provisionally erased. I resent this lack of treatment, but it was not for the General Medical Council to treat me under any legal obligation of ‘duty-of’care’. I would argue that they have some sort of quasi-moral one, simply because of the Hippocratic Oath which governs the behaviour of all doctors to patients, even if their patients are other doctors. Therein lies the conundrum of treatment for professionals – you don’t wish to admit you have a problem, and you don’t have insight anyway; obviously, you have nobody apart to blame, apart yourself, if you go down this route. In recovery, on the other hand, the paradox is that you certainly need the help of others, but you can’t make it on your own. Anyway, ‘every cloud has its silver lining’. I was able to complete both my Bachelors and (nearly) my Masters of Law, where my interests in law and philosophy have converged on the notion that legal responsibility is very hard to define where the extent of a defendant’s voluntariness has been compromised by mental illness. That issue is for another day but I have much enjoyed analyzing (and agreeing with) the arguments of LJ Sedley of the House of Lords (now the Supreme Court).
Enough about me suffice to say that I love my life, and indeed proselytizing about recovery to others. I am always taken aback by how common alcohol problems are, as a member of society not as a doctor, ahead of problem drinking or alcoholism. The vast majority of people are capable of being social drinkers, and do not benefit from interference with their lifestyles. I am different. If I have another drink, it will kill me, because I wouldn’t be able to stop drinking until I drop. I would just keep going on, and going, and going. I have seen others do it every night in Clerkenwell Road, vomiting in the streets, but they wake up the following with the hangover; some may even go as normal to work. I now detest this lifestyle. I used to be a ‘revolving door’ patient, but I don’t wish to pay Russian Roulette with my life. Last time I did, I woke up on the top floor of the Royal Free, having been written off by the superb NHS consultants, disabled, having received a catheter and tracheostomy, but alive.
I sent Prof. David Nutt an e-mail this morning. He is absolutely adored by his patients, and by all the national and international experts that I have ever met in addiction disorders. Genuinely, I find him a wonderful and inspiring man. I take what he says very seriously; he is often misquoted, and he makes clear that no drug is safe. If you’re the one in the million that reacts adversely, a mass of statistics won’t impress you particularly. Nutt had his latest paper published in the Lancet around midday today. Indeed, on the Centre for Crime and Justice Studies (UK) website which funded this study, Professor Nutt today is remarked to have said:
`No one is suggesting that drugs are not harmful. The critical question is one of scale and degree. We need a full and open discussion of the evidence and a mature debate about what the drug laws are for – and whether they doing their job?‘
There is no point us burying our heads in the sand pretending there is no problem as member of the Big Society. By August 2010, David Cameron deduced a problem with very cheap alcohol being sold by supermarkets which people were drinking before heading out for the evening. The House of Commons Health Select Committee and NICE have voiced strong support for minimum pricing. Hospital admissions due to alcohol have risen by 825 a day in five years to almost a million, researchers found today. The Alcohol Commission has recommended a ban on selling drink at below the “floor price” of the cost of production, plus the cost of duty and VAT. Recent data suggest that northerners were found to be the hardest drinkers but the most alcohol-related crimes were committed in London. (from the Liverpool John Moores University’s Centre for Public Health in the “Lape Report”).
There were 945,469 admissions to hospital for alcohol-related harm in England in 2008/09. The data from CIVITAS make staggering, and depressing reading, The overall annual cost of crime and anti-social behaviour linked to alcohol misuse is estimated at £8-£13bn a year. In 2004, the approximate figure had been £7.3bn. Thankfully, detoxification is available on reception in all local and remand prisons: during 2002-3, around 6,400 prisoners received alcohol detoxification and 7,000 combined drug and alcohol detoxification. Indeed, Alcoholics Anonymous run services in around 50% of prisons currently. The use of such drugs including might not only result in physical and mental harm for the user, but can also present great burdens to society, such as aggression, car accidents, poverty, job absence, and health-care costs.
Today, Professor David Nutt’s team published their latest findings on the relative risk of alcohol. Their findings supported previous work in the UK and the Netherlands, confi rming that the present drug classification systems have little relation to the evidence of harm. They accord with the conclusions of previous expert reports that aggressively targeting alcohol harms is a valid and necessary public health strategy. The authors argued, to provide better guidance to policy makers in health, policing, and social care, the ‘harms’ that drugs cause needed to be properly assessed, but the authors readily admitted that a major issue is how you assees ‘harm’ in the first place.
Members of the Independent Scientific Committee on Drugs (ISCD) 1-day interactive workshop were invited to score 20 drugs on 16 criteria: nine related to the harms that a drug produces in the individual and seven to the harms to others. Drugs were scored out of 100 points, and the criteria were weighted to indicate their relative importance. Findings showed that heroin, crack cocaine, and metamfetamine were the most harmful drugs to individuals, whereas alcohol, heroin, and crack cocaine were the most harmful to others. Overall, alcohol was found to be the most harmful drug, with heroin and crack cocaine in second and third places. The correlations between the Independent Scientific Committee on Drugs (ISCD) overall scores and the present classification of drugs based on revisions to the UK Misuse of Drugs Act (1971) is 0·04, showing that there is effectively no relation. The ISCD scores lend support to the widely accepted view that alcohol is an extremely harmful drug, both to users and society; it scored fourth on harms to users and top for harms to society, making it the most harmful drug overall.
Different regulatory approaches have therefore been used to restrict the adverse effects of licit and illicit drug use, varying from punitive prohibition, to partial liberalisation, to full legislation of the drug market. An area of work which I will be followed in the near future is whether the behaviour of addicted individuals can be ‘incentivized’ – can an alcoholic be ‘nudged’ to give up under the right circumstances? Such libertarian paternalism is of course gathering some momentum in the US and here. Notwithstanding, experts have argued that overt and explciit criminalisation of drug use has low efficacy in reducing the prevalence of drug misuse, and even seems to promote petty and organised crime
As such, these new data provide an extremely valuable contribution for the re-evaluation of current drug classifi cation in the UK. A major point not addressed in the study, because it was outside the investigators’ scope, is polydrug use, which is highly prevalent in recreational drug users. The major funding must be surely that, for the discussion about drug classification, the two legal drugs assessed — alcohol and tobacco —score in the upper segment of the ranking scale, indicating that legal drugs cause at least as much harm as do illegal substances.
For me, it’s simple. I have never touched any drug apart from alcohol, but I can’t even risk having any of these drugs for the rest of my life, including alcohol or tobacco. For me – it’s simples – if I do, I will be dead!
Dr Shibley Rahman is happily in recovery for 40 months now, has done 2 books, nearly 2 law degrees, has become a company director and an Associate of the IoD as well as a FRSA, in that time.
Plea to the BBC : I have never been a stalker
Public confidence is a big deal to the regulatory bodies in law and medicine. Likewise, I feel that it is time for me to protect myself at long last against three stories on the BBC that call me a stalker. They have refused to get rid of this despite months of me asking them to do so (via BBC Complaints). Of course, I’m upset as the BBC ran this story during the actual hearing itself. There is in fact such a thing as article 6 to protect against this sort of thing – right to a fair trial. I believe that this was a big reason why the GMC (General Medical Council) took a somewhat kneejerk reaction to erase me off the medical register, when everyone knows I’ve had a long and now successful battle against alcoholism. I was unconscious in a coma for 2 months in 2007 the year after beings struck off, and I have never touched a drop of alcohol since. The thing actually I feel most embittered about is that the GMC never appointed a health supervisor whilst I was on the register for 2004-2006, in other words they breached their own ‘duty of care’ towards doctors, and that they have only suspended doctors for plagiarism, attempted manslaughter/murder or failure to detect child abuse in the subsequent years. I was a sick doctor who needed treatment. I am under a psychiatrist today, and I am very proud of recovery. I have done two law degrees, set up my own private limited company, done two books and written three research paper.
I am however thoroughly sick of it, as I have six degrees, and when people do a search on my name they find the offending article. It stops me possibly getting jobs. I applied for 30 jobs last year, and didn’t get any of them. So I would like to say something about public confidence. The public should not be confident in a huge organisation such as the BBC making mincemeat out of someone bordering on defamation. I am too poor to go to a lawyer such as Carter Ruck who would sort this sort of rubbish out instantly. Read the letter below. All my friends on Facebook are too polite to mention it. I would like to think that a lot of my friends there are genuine and see beyond the spin. I won’t even go into why this story has been given rocket boosters by BBC. I find it insulting that after 10 years in medicine including a PhD I ended up in the Entertainment section, with a picture of my elderly frail father there against his will. The BBC first became aware of this in December 2009 and refused to do anything about it. I am really sick of it, as I keep on being told it undermines public reputation in me.
I believe in a new innovative approach to reform of the criminal justice system and mental illness, as one would expect!