It was a real honour and privilege to be invited to give a talk to a group of medical Doctors who were currently suspended on the GMC Medical Register this morning (in confidence). I gave a talk for about thirty minutes, and took questions afterwards. I have enormous affection for the medical profession in fact, having obtained a First at Cambridge in 1996, and also produced a seminal paper in dementia published in a leading journal as part of my Ph.D. there. I have had nothing to do with the medical profession for several years now, apart from volunteering part-time for two medical charities in London which I no longer do.
I think patient safety is paramount, and Doctors with addiction problems often do not realise the effect the negative impact of their addiction on their performance. No regulatory authority can do ‘outreach’, otherwise it would be there forever, in the same way that Alcoholics Anonymous or Narcotics Anonymous do not actively go out looking for people with addiction problems. I personally have doubts about the notion of a ‘high functioning addict’, as the addict is virtually oblivious to all the distress and débris caused by their addiction; the impact on others is much worse than on the individual himself, who can lack insight and can be in denial. Insight is something that is best for others to judge.
However, I have now been in recovery for 72 months, with things having come to a head when I was admitted in August 2007 having had an epileptic seizure and asystolic cardiac arrest. Having woken up on the top floor of the Royal Free Hospital in pitch darkness, I had to cope with recovery from alcoholism (I have never been addicted to any other drugs), and newly-acquired physical disability. I in fact could neither walk nor talk. Nonetheless, I am happy as I live with my mum in Primrose Hill, have never had any regular salaried employment since my coma in the summer of 2007, received scholarships to do my MBA and legal training (otherwise my life would have become totally unsustainable financially apart from my disability living allowance which I use for my mobility and living). I am also very proud to have completed my Master of Law with a commendation in January 2011. My greatest achievement of all has been sustaining my recovery, and my talk went very well this morning.
The message I wished to impart that personal health and recovery is much more important than temporary abstinence, ‘getting the certificate’ and carrying on with your career if you have a genuine problem. People in any discipline will often not seek help for addiction, as they worry about their training record. Some will even not enlist with a G.P., in case the GP reports them to a regulatory authority. I discussed how I had a brilliant doctor-patient relationship with my own G.P. and how the support from the Solicitors Regulation Authority (who allowed me unconditionally to do the Legal Practice Course after an extensive due diligence) had been vital, but I also fielded questions on the potential impact of stigma of stigma in the regulatory process as a barrier-to-recovery.
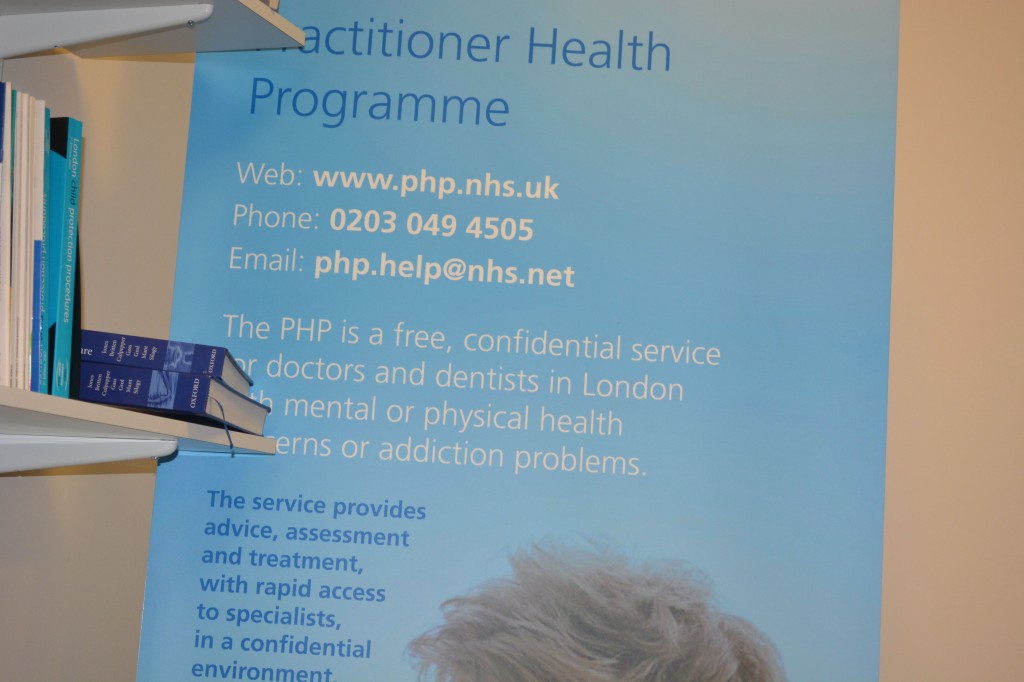
I gave an extensive list of my own ‘support network’, which included my own G.P., psychiatrist, my mum, other family and friends, the Practitioner Health Programme, and ‘After Care’ at my local hospital.
The Practitioner Health Programme, supported by the General Medical Council, describes itself as follows:
The Practitioner Health Programme is a free, confidential service for doctors and dentists living in London who have mental or physical health concerns and/or addiction problems.
Any medical or dental practitioner can use the service, where they have
• A mental health or addiction concern (at any level of severity) and/or
• A physical health concern (where that concern may impact on the practitioner’s performance.)
I was asked which of these had helped me the most, which I thought was a very good question. I said that it was not necessarily the case that a bigger network was necessarily better, but it did need individuals to be open and truthful with you if things began to go wrong. It gave me a chance to outline the fundamental conundrum of recovery; it’s impossible to go into recovery on your own (for many this will mean going to A.A. or other meetings, and discussing recovery with close friends), but likewise the only person who can help you is yourself (no number of expensive ‘rehabs’ will on their own provide you with the ‘cure’.) This is of course a lifelong battle for me, and whilst I am very happy now as things have moved on for me, I hope I may at last help others who need help in a non-professional capacity.
Best wishes, Shibley
My talk [ edited ]