Home » Posts tagged 'commissioning'
Tag Archives: commissioning
Specialist nurses should form part of the post-diagnostic care and support network for living well with dementia
Background: There have been numerous concerns that the health and care system in England is too fragmented, and lacks sufficient focus for a person with dementia or caregiver to navigate through the system.
A complex array of health and social care services is needed to support people living with dementia; “carers find navigating systemic issues in dementia care time-consuming, unpredictable and often more difficult than the caring work they undertake.”(Peel and Harding, 2014).
One of the “pillars” of the Scottish strategy invokes a “dementia practice coordinator“.
This rôle is: “a named, skilled practitioner who will lead the care, treatment and support for the person and their carer on an ongoing basis, coordinating access to all the pillars of support and ensuring effective intervention across health and social care”.
There are a number of possible professions which might be involved in this care coordinating role: for example, GPs taking a proactive approach to their patients, or social care practitioners who might have particular expertise in safeguarding issues (e.g. Manthorpe et al., 2007).
The Alzheimer’s Society suggest a “dementia adviser” role.
In this framework, the dementia adviser service would be ‘primarily for people with dementia, as well as their supporters and carers. It provides them with a named contact throughout their journey with dementia. Referrals to the service may come from GPs, CMHTs or other health and social care professionals, or self-referral.’
It is interesting to note that such a rôle was described clearly in the 2009 Department of Health English strategy document for dementia policy: “Living well with dementia”:
Clinical nurse specialists (CNS) in cancer perform a range of complex activities, including the management of care.
Recent evidence from the University of Southampton suggests that a properly trained and educated dementia specialist nurse, undertaking a clearly defined role, and working directly with people with dementia and their carers for a significant proportion of the time, could benefit people with dementia in hospitals. If these benefits addressed only a fraction of the excess stays experienced by people with dementia, a significant return on investment could be obtained.
CNS who practise proactive case management and refocus services in line with best practice represent a good return on investment (Leary and Baxter, 2014).
Recently, calls have been made to expand a pioneering dementia pilot in Norfolk after an almost £110,000 investment resulted in more than £400,000 savings for health and social services in less than a year.
The meaning of the term ‘timely diagnosis’ in dementia has recently come under close scrutiny.
For example, Dhedhi, Swinglehurst and Russell (2014) state that: “Reluctance or failure to make a diagnosis on a particular occasion does not necessarily point to GPs’ lack of awareness of current policies, or to a set of training needs, but commonly reflects this range of nuanced balancing judgements, often negotiated with patients and their families with detailed attention to a particular context.”
The Carers Trust has been working with the Royal College of Nursing to adapt the Triangle of Care to meet the needs of carers of people with dementia when that person is admitted to a general hospital. This approach, which has gathered some momentum in English policy, puts the person living with dementia in a ‘triangle of care’ in a ‘triangle of care’ with professional and carer (see page 6).
There is clearly a potential rôle for a third sector charity, such as Dementia UK, in providing clinical nursing specialist input. The success of Macmillan Cancer in the ‘prime contractor’ model for integrating cancer and end-of-life care in Staffordshire, as an example of outcomes-based commissioning, is, arguably, a very good recent paradigmatic example.
Aim: To conduct a preliminary online survey into citizens’ attitudes to what post-diagnostic support in the English jurisdiction could look like.
Methods: 87 respondents completed the online “Surveymonkey” survey, invited from a Twitter account with around 12000 followers. The survey could only be completed once.
You were invited to be a person who had just received a diagnosis of dementia in the English jurisdiction.
Exclusions: None.
Results:
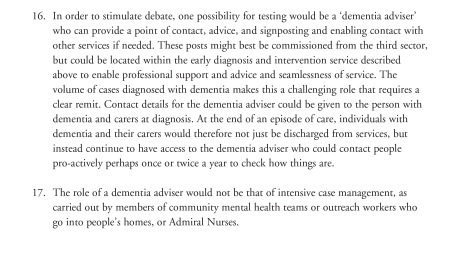
Q1. By far, the most preferred option was to go to see your General Practitioner with a view to receiving, if correct, a diagnosis of early dementia, if you’d noticed a decline in your memory and been aware of a public campaign on dementia (47%); talking about your concerns with your friends or family, to see what they suggest, was the next preferred option (34%).
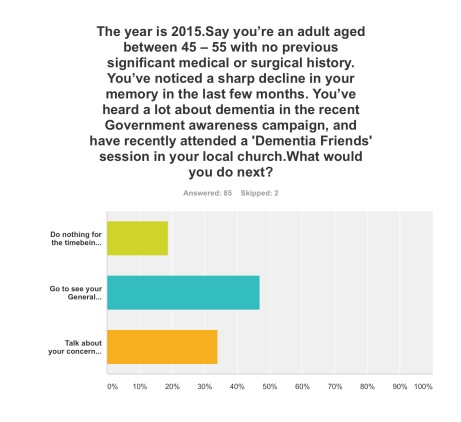
Q2. This was extremely finally balanced. One option was most preferred (38%), that of staying with your GP, but attending for the next couple of years regular six-monthly meetings with a hospital neurologist to observe follow-up with CPN support; but only just, as staying with your GP, who can help organise care and support for you and your closest consisting of a multidisciplinary team, was the next preferred option (36%). The option to stay with your GP, but ring up a local charity helpline to see what they can suggest to help you, regarding information and life choices, was the least preferred (26%).
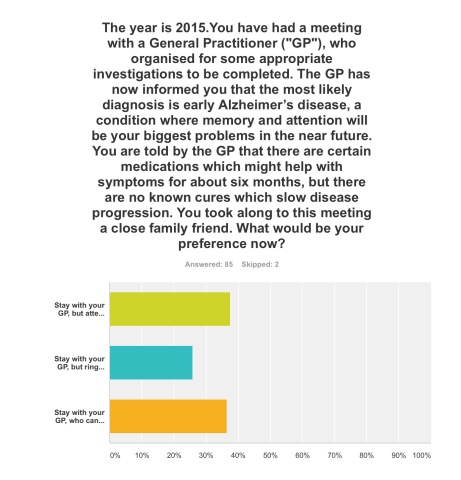
Q3. The option where a clinical nursing specialist had been added incrementally to a speech and language therapist and clinical psychologist was by far the most popular option (72%).
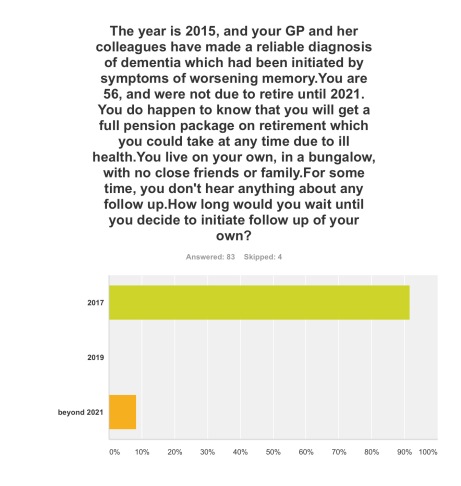
Q4. The option where you initiated follow-up for post-diagnosic support following diagnosis as soon as possible, relatively in 2017, was by far the most popular option (92%).
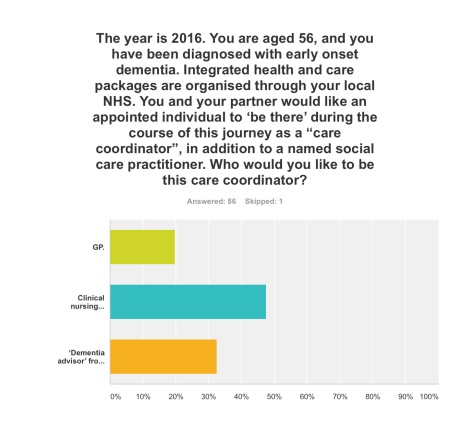
Q5. Three options were given for who the ‘care coordinator’ could be. A clinical nursing specialist was by far the most preferred option (48%), then ‘dementia adviser’ from a well known charity (33%), and then the GP last (19%).
The rôle of the ‘dementia adviser’, particularly at the earlier stages of the condition at least, is clearly worth considering in future policy such as the English dementia strategy 2015-20.
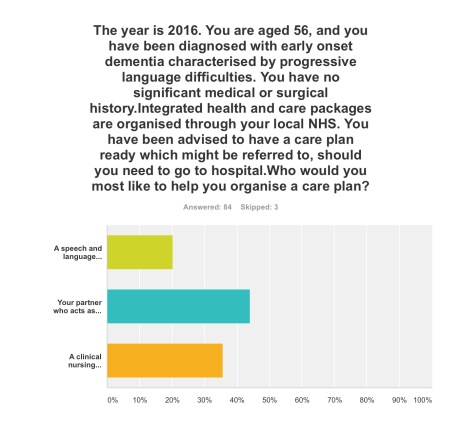
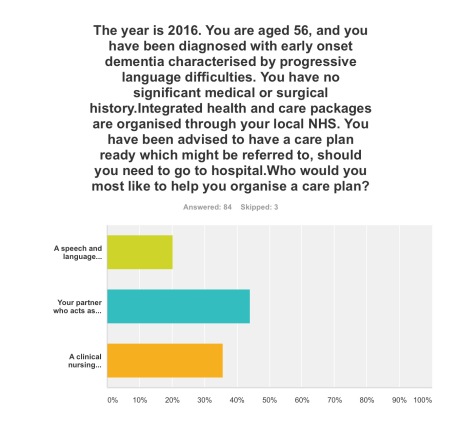
Q6. This question asked who you would like the most to organise your care plan with you: your primary caregiver was the most popular choice (44%), with a clinical nursing specialist the next popular choice (36%).
Q7. Here it was introduced that a clinical nursing specialist was one of the options in the new English dementia strategy (2015-20). The rationale for this, most felt, should come from clinical outcomes (76%), then financial considerations from the funding situation of the NHS and care (14%). The option where powerful lobbying from charities (“third sector”) should be the driver for specialist nurses was the least preferred (10%).
Discussion: The results confirm previous anecdotal reports of the need for timely post-diagnostic support following ‘timely diagnosis’. They paint a picture of a person who has become aware of dementia awareness campaigns and noticed possible symptoms in himself wishing to trust to see a General Practitioner to receive a diagnosis. On receipt of that ‘timely diagnosis’, he or she would be keen to initiate post-diagnostic support as soon as possible, with a multidisciplinary team; it is striking that a clinical nursing specialist was preferred to the rôle of the ‘dementia adviser’ from a charity previously mooted; and that the decision in policy to implement clinical nursing specialists should be made on the basis of clinical outcome, not financial pressures in which the NHS and care find themselves. Notwithstanding that, the results support heavily a ‘triangle of care’ involving a caregiver and a professional, such as a person living with dementia, in the formation of a personalised care plan.
Limitations: There are no geographical data of the locations, or other demographic data, of the respondents to this online survey. Responses might be biased by the nature of the Twitter threads which had invited respondents to participate, or the nature of the followers of those threads. The questions assume a working knowledge of what the key personnel in a multidisciplinary team for dementia care and support do.
Although respondents were advised to select one of the options, however inadequate the options were, it is a limitation of this study that options did not include social care practitioners. Social care practitioners will, however, have a critical rôle in dementia post-diagnostic care and support.
Conclusions: The findings taken together provide important considerations for future policy-makers regarding post-diagnostic support for dementia in the English jurisdiction, urging the need for a rôle for clinical nursing specialists in delivering prompt post-diagnostic support and in avoiding, on the basis of clinical need, inappropriate care in hospitals.
Selected readings
Carers Trust/Royal College of Nursing. (2013) The triangle of care. Carers Included: A Guide to Best Practice for Dementia Care
Dhedhi SA, Swinglehurst D, Russell J. (2014) ‘Timely’ diagnosis of dementia: what does it mean? A narrative analysis of GPs’ accounts, BMJ Open, Mar 4, 4(3):e004439.
Leary A, Baxter J. (2014) Impact of lung cancer clinical nurse specialists on emergency admissions, Br J Nurs, Sep 25, 23(17), pp. 935-8.
Manthorpe J, Clough R, Cornes M, Bright L, Moriarty J, Iliffe S; OPRSI (Older People Researching Social Issues). (2007) Four years on: the impact of the National Service Framework for Older People on the experiences, expectations and views of older people, Age Ageing, Sep, 36(5), pp. 501-7.
Peel E, Harding R. (2014) ‘It’s a huge maze, the system, it’s a terrible maze': dementia carers’ constructions of navigating health and social care services. Dementia (London), Sep, 13(5), pp. 642-61. d
We've just had a huge debate about the NHS. It's just a pity that it's been the wrong one.
Think of how much time we’ve just all spent, in thinking about the way in which services will be mostly put out for competitive tendering in the National Health Service. One of the first rules in law is that you fight your battles to the hilt, but, at first, you pick the right battles first. This is precisely what Labour appears not to have done. When Harriet Harman recently said on Question Time that the Conservatives are definitely not ‘to be trusted with the NHS’, Harriet curiously did not refer to the battle and war just won by the Conservatives (and Liberal Democrats) over NHS procurement. And yet the public desperately want Labour to stand up for the NHS. One member even suggested that, if Labour gave its unequivocal backing for restoring the NHS, Labour could even find itself with a massive vote winner.
Labour is clearly going through policy strands with a fine tooth comb, looking at, for example, the way in which multinational companies might employ workers at below the national minimum wage; effectively, controlling immigration through a wage policy. It does not appear to have worked out unequivocally whether it would reduce the rate of VAT, meaning possibly that the state borrowing requirement would temporarily increase. But do you see what they all did there? For days, weeks, or even months, we have been subjected to a relentless debate about EU immigration, when most surveys probably place the issue at number ten on the list of voters’ concerns. Unsurprisingly, the economy remains in ‘pole position’, but the ability of Labour to turn the opinion of the public, particularly in the South of England, away from the idea that Labour is ‘fiscally incontinent’ remains unconvincing. Labour is still considered to be the “tax and spend” party, for example, and Miliband appears painfully aware of that. So, when it comes to policy, there seems to be an odd combination of Labour shooting itself in the foot, or completely picking the wrong battles. And then you add in a complete inability to look at elephants in the room. Labour, to state the obvious, has no ability to implement any of its policies, if it is unable to win a General Election, and the confidence of Labour to win an election on its own is reflected accurately in Lord Adonis promoting his book that ‘if he were to form a new Lib-Lab pact, he wouldn’t start from here.‘
The NHS remains pivotal in Labour’s electoral chances, and Labour has been unable to use the resentment over the section 75 NHS regulations to maximise political capital. Why this should have happened in itself is interesting, as Andy Burnham, MP for Leigh, is a more than capable Shadow Secretary of State for Health. One of the issues is an ability to choose the right battle, possibly. Burnham, with some support from the right-wing media and thinktanks, has been banging on about integrated and whole-person care. Whether through conspiracy or cock-up, there will be short-term interest in how integrated care might be delivered. Think about a justification for State spending in the ‘mission impossible’ of implementing a NHS IT system. Why on earth would a right-wing libertarian government promote something which is national? Why on earth should you abort an ethos of ‘bonfire of the QUANGOs’ to introduce the biggest QUANGO in the country, viz NHS England? Whether you’re into conspiracy or cock-up, the integration of financial and medical information (including mental, physical and social care systems) allows for the perfect infrastructure for an insurance-based system. Insurance works on the basis of misrepresentation or non-disclosure to invalidate claims, so ‘big data’ serve a perfect storm for this. It won’t have escaped anybody’s attention that Labour (as indeed the Conservative Party) has been heading towards an insurance-based system for social care, so it does not require a massive ideological leap to think how this could be extended for all care with time. This does not involve any degree of paranoia, please note.
There is overwhelmingly an intellectual depravity in the bereft notion of producing policy through poll results and focus groups. New Labour clearly loved focus groups, with Philip Gould in ‘The Unfinished Revolution’ having devoted much airspace to developing a product in line with customers’ wishes. Of course, the Conservatives have a special affinity for polling organisations themselves, Nadhim Zadawi, in 2000 he co-founded YouGov and on its flotation became its CEO. YouGov is now one of the world leaders in political and business information gathering, polling and analysis. It employs over 400 staff on three continents and is listed on the London Stock Exchange. Again – it begs the question on why should Labour should wish to outdo the Conservatives on its own ability to use polling data? One of the polls which has become a toxic meme is how a high proportion of all voters would not mind who provides the NHS services, as long as it’s free at the point of use. However, this is intrinsically linked to other questions. Would you be prepared more in national insurance if it meant the NHS were able to provide a more comprehensive (universal) service?
It is indeed correct to state that the costs of renationalising the NHS might be overwhelming, although no accurate costings of this have ever been discussed properly. We do know, however, that the current cost of the NHS reorganisation is in the region of £3bn, but estimates of the actual cost inevitably have to be taken with a pinch of salt, as say the cost of Margaret Thatcher’s funeral. But to use this issue as a wish to stop discussion of this area is lazy, as one of the issues, as indeed as with Thatcher’s funeral, is that is this a sensible use of money compared to how it could be used elsewhere (so called “opportunity cost“)? Some people argue that the marketisation of the NHS has failed, in that any money spent on restoring a state-funded NHS would be money well spent. Restoring a state-funded service would get out of the idea of private companies being driven by maximising their profit margin, and not running a ‘more for less’ approach for delivering a service. Cynics might argue that the cost of restoring a state-run service is peanuts compared to waging a war abroad. Many remain unconvinced about the mantra that economic competition drives up quality, when it is the professional standards of healthcare staff, including doctors, nurses and allied health professionals, which appear to be at the heart of quality. The debate we have just had about the mode of procurement in the NHS was not one any of us as such elected; in other words, it has no mandate. If the Conservatives and the right-wing media appear so pre-occupied about having a referendum next parliament on our membership of the EU, many are (rightly) asking why Ed Miliband cannot ask for a mandate to take sensible decisions about the nature of the NHS. It is a given that there will always be a proportion of services which are outsourced to the private sector, but the question should be ‘how much’. Whilst a full-blown privatisation of the NHS has not happened yet, we have not even had a discussion of how much of the NHS should be outsourced.
And anyway Labour has to ask what really concerns all voters? In Mid Staffs and Cumbria, it is reported that there have been concerns about patient safety, and it may be mere coincidence that Labour failed to convince the voters in both places in the local elections over their offerings. However, there is certainly a ‘debate to be had’, about whether “efficiency savings” in the NHS are justified to produce surpluses in the NHS which get ploughed back into the Treasury (and therefore might be used for international overseas aid rather than frontline care.) Labour equally seems unable to look another ‘white elephant’ in the eye. That is of course the concept of a NHS hospital going bust. Should a NHS Trust which is in financial difficulty be simply allowed to go insolvent after a period of administration, or should the State pump money into it to maintain a local service to people in the community? This requires a fundamental reappraisal of how important “solidarity” and “social democracy” are, in fact, to Labour, and whether it wishes to use its extensive brand loyalty to have a mature, if sobering, discussion of the extent to which it wishes to fund a SOCIALIST National Health Service. Whilst in extremis it can be argued that a nostalgic return to ‘The Spirit of ’45” is not attainable, and is the wrong solution for the wrong times, there is a genuine perception that Labour has lost sight of its founding values. And why has this not been addressed in focus groups? It is well known that, in marketing, if you ask the wrong questions, you ubiquitously get the wrong answers.
Labour needs a mandate to confront these issues. And it should not be afraid to look for a resounding mandate, either. Whilst it might stick its fingers in its ears, and claim it’s nothing to do with them (arguing instead for integrated, “whole person” care), unless these ideological issues are confronted, NHS policy will continue to go down a right-wing path. For example, there is not much further to see GP ‘businesses’ being offered by the private sector, and the NHS pays for them; in this model, GP ‘businesses’ could operate under a standard 5-year contract, using NHS branding, under a ‘franchising’ model like Subway. And “The Tony Blair Dictum” is far from resolved, although currently there are issues more worthy of ‘firefighting’ in service delivery, such as the fiasco over ‘1111’. Labour’s problem is that it does not see the NHS as a ‘vote winner’, in the same way it doesn’t see the plight of disabled citizens experiencing difficulty with their benefits or people feeling genuinely threatened by ‘the bedroom tax’ as a top priority. Whilst Labour is unable to prioritise its issues in a way to align its aspirations with the concerns of the general public, there is no way on Earth it can hope to govern a convincing majority. If Labour wishes to learn a really useful trick from marketing, it could no better than to look at the ‘GAP analysis’ – looking at what the current situation is, and what the expectations of people are, and thinking how to get to a position of what people want. If people actually want a socialist universal, comprehensive NHS, paid for not in a private insurance system, Labour can be expected to work hard for a mandate to deliver this. If it doesn’t, that’s another matter, and it can witter on about whole-person care to its heart’s content.
We've just had a huge debate about the NHS. It's just a pity that it's been the wrong one.
Think of how much time we’ve just all spent, in thinking about the way in which services will be mostly put out for competitive tendering in the National Health Service. One of the first rules in law is that you fight your battles to the hilt, but, at first, you pick the right battles first. This is precisely what Labour appears not to have done. When Harriet Harman recently said on Question Time that the Conservatives are definitely not ‘to be trusted with the NHS’, Harriet curiously did not refer to the battle and war just won by the Conservatives (and Liberal Democrats) over NHS procurement. And yet the public desperately want Labour to stand up for the NHS. One member even suggested that, if Labour gave its unequivocal backing for restoring the NHS, Labour could even find itself with a massive vote winner.
Labour is clearly going through policy strands with a fine tooth comb, looking at, for example, the way in which multinational companies might employ workers at below the national minimum wage; effectively, controlling immigration through a wage policy. It does not appear to have worked out unequivocally whether it would reduce the rate of VAT, meaning possibly that the state borrowing requirement would temporarily increase. But do you see what they all did there? For days, weeks, or even months, we have been subjected to a relentless debate about EU immigration, when most surveys probably place the issue at number ten on the list of voters’ concerns. Unsurprisingly, the economy remains in ‘pole position’, but the ability of Labour to turn the opinion of the public, particularly in the South of England, away from the idea that Labour is ‘fiscally incontinent’ remains unconvincing. Labour is still considered to be the “tax and spend” party, for example, and Miliband appears painfully aware of that. So, when it comes to policy, there seems to be an odd combination of Labour shooting itself in the foot, or completely picking the wrong battles. And then you add in a complete inability to look at elephants in the room. Labour, to state the obvious, has no ability to implement any of its policies, if it is unable to win a General Election, and the confidence of Labour to win an election on its own is reflected accurately in Lord Adonis promoting his book that ‘if he were to form a new Lib-Lab pact, he wouldn’t start from here.‘
The NHS remains pivotal in Labour’s electoral chances, and Labour has been unable to use the resentment over the section 75 NHS regulations to maximise political capital. Why this should have happened in itself is interesting, as Andy Burnham, MP for Leigh, is a more than capable Shadow Secretary of State for Health. One of the issues is an ability to choose the right battle, possibly. Burnham, with some support from the right-wing media and thinktanks, has been banging on about integrated and whole-person care. Whether through conspiracy or cock-up, there will be short-term interest in how integrated care might be delivered. Think about a justification for State spending in the ‘mission impossible’ of implementing a NHS IT system. Why on earth would a right-wing libertarian government promote something which is national? Why on earth should you abort an ethos of ‘bonfire of the QUANGOs’ to introduce the biggest QUANGO in the country, viz NHS England? Whether you’re into conspiracy or cock-up, the integration of financial and medical information (including mental, physical and social care systems) allows for the perfect infrastructure for an insurance-based system. Insurance works on the basis of misrepresentation or non-disclosure to invalidate claims, so ‘big data’ serve a perfect storm for this. It won’t have escaped anybody’s attention that Labour (as indeed the Conservative Party) has been heading towards an insurance-based system for social care, so it does not require a massive ideological leap to think how this could be extended for all care with time. This does not involve any degree of paranoia, please note.
There is overwhelmingly an intellectual depravity in the bereft notion of producing policy through poll results and focus groups. New Labour clearly loved focus groups, with Philip Gould in ‘The Unfinished Revolution’ having devoted much airspace to developing a product in line with customers’ wishes. Of course, the Conservatives have a special affinity for polling organisations themselves, Nadhim Zadawi, in 2000 he co-founded YouGov and on its flotation became its CEO. YouGov is now one of the world leaders in political and business information gathering, polling and analysis. It employs over 400 staff on three continents and is listed on the London Stock Exchange. Again – it begs the question on why should Labour should wish to outdo the Conservatives on its own ability to use polling data? One of the polls which has become a toxic meme is how a high proportion of all voters would not mind who provides the NHS services, as long as it’s free at the point of use. However, this is intrinsically linked to other questions. Would you be prepared more in national insurance if it meant the NHS were able to provide a more comprehensive (universal) service?
It is indeed correct to state that the costs of renationalising the NHS might be overwhelming, although no accurate costings of this have ever been discussed properly. We do know, however, that the current cost of the NHS reorganisation is in the region of £3bn, but estimates of the actual cost inevitably have to be taken with a pinch of salt, as say the cost of Margaret Thatcher’s funeral. But to use this issue as a wish to stop discussion of this area is lazy, as one of the issues, as indeed as with Thatcher’s funeral, is that is this a sensible use of money compared to how it could be used elsewhere (so called “opportunity cost“)? Some people argue that the marketisation of the NHS has failed, in that any money spent on restoring a state-funded NHS would be money well spent. Restoring a state-funded service would get out of the idea of private companies being driven by maximising their profit margin, and not running a ‘more for less’ approach for delivering a service. Cynics might argue that the cost of restoring a state-run service is peanuts compared to waging a war abroad. Many remain unconvinced about the mantra that economic competition drives up quality, when it is the professional standards of healthcare staff, including doctors, nurses and allied health professionals, which appear to be at the heart of quality. The debate we have just had about the mode of procurement in the NHS was not one any of us as such elected; in other words, it has no mandate. If the Conservatives and the right-wing media appear so pre-occupied about having a referendum next parliament on our membership of the EU, many are (rightly) asking why Ed Miliband cannot ask for a mandate to take sensible decisions about the nature of the NHS. It is a given that there will always be a proportion of services which are outsourced to the private sector, but the question should be ‘how much’. Whilst a full-blown privatisation of the NHS has not happened yet, we have not even had a discussion of how much of the NHS should be outsourced.
And anyway Labour has to ask what really concerns all voters? In Mid Staffs and Cumbria, it is reported that there have been concerns about patient safety, and it may be mere coincidence that Labour failed to convince the voters in both places in the local elections over their offerings. However, there is certainly a ‘debate to be had’, about whether “efficiency savings” in the NHS are justified to produce surpluses in the NHS which get ploughed back into the Treasury (and therefore might be used for international overseas aid rather than frontline care.) Labour equally seems unable to look another ‘white elephant’ in the eye. That is of course the concept of a NHS hospital going bust. Should a NHS Trust which is in financial difficulty be simply allowed to go insolvent after a period of administration, or should the State pump money into it to maintain a local service to people in the community? This requires a fundamental reappraisal of how important “solidarity” and “social democracy” are, in fact, to Labour, and whether it wishes to use its extensive brand loyalty to have a mature, if sobering, discussion of the extent to which it wishes to fund a SOCIALIST National Health Service. Whilst in extremis it can be argued that a nostalgic return to ‘The Spirit of ’45” is not attainable, and is the wrong solution for the wrong times, there is a genuine perception that Labour has lost sight of its founding values. And why has this not been addressed in focus groups? It is well known that, in marketing, if you ask the wrong questions, you ubiquitously get the wrong answers.
Labour needs a mandate to confront these issues. And it should not be afraid to look for a resounding mandate, either. Whilst it might stick its fingers in its ears, and claim it’s nothing to do with them (arguing instead for integrated, “whole person” care), unless these ideological issues are confronted, NHS policy will continue to go down a right-wing path. For example, there is not much further to see GP ‘businesses’ being offered by the private sector, and the NHS pays for them; in this model, GP ‘businesses’ could operate under a standard 5-year contract, using NHS branding, under a ‘franchising’ model like Subway. And “The Tony Blair Dictum” is far from resolved, although currently there are issues more worthy of ‘firefighting’ in service delivery, such as the fiasco over ‘1111’. Labour’s problem is that it does not see the NHS as a ‘vote winner’, in the same way it doesn’t see the plight of disabled citizens experiencing difficulty with their benefits or people feeling genuinely threatened by ‘the bedroom tax’ as a top priority. Whilst Labour is unable to prioritise its issues in a way to align its aspirations with the concerns of the general public, there is no way on Earth it can hope to govern a convincing majority. If Labour wishes to learn a really useful trick from marketing, it could no better than to look at the ‘GAP analysis’ – looking at what the current situation is, and what the expectations of people are, and thinking how to get to a position of what people want. If people actually want a socialist universal, comprehensive NHS, paid for not in a private insurance system, Labour can be expected to work hard for a mandate to deliver this. If it doesn’t, that’s another matter, and it can witter on about whole-person care to its heart’s content.
There should be a senior public health physician on the NHS Commissioning Board
The current NHS Commissioning Board include Sir David Nicholson, who has apologised for the deaths numbering in the region of 400-1200 at Mid Staffs and who is alleged to have been warned by NHS whistleblower about serious patient safety issues, and Dame Barbara Hakin, “..who was then head of the East Midlands strategic health authority and is now national director for commissioning development at the NHS Commissioning Board, ordered him to meet the national targets regardless of demand.” The General Medical Council has launched an investigation into a complaint against national director for commissioning development Dame Barbara Hakin, according to the HSJ.
The UK Faculty of Public Health (FPH), part of the Royal Colleges of Physicians (London college), is the standard setting body and the leading professional body for public health specialists in the UK. It aims to advance the health of the population through three key areas of work: health promotion, health protection and healthcare improvement. In addition to maintaining professional and educational standards for specialists in public health, FPH advocates on key public health issues and provides practical information and guidance for public health professionals. The Faculty of Public Health, of the Royal College of Physicians, responded to a consultation on the document “Liberating the NHS: commissioning for patients”.
In their response, the Faculty of Public Health set out a very clear case of how public health professionals could and show be involved in commissioning, for example:
“Specialist commissioning should be integrated with the work of GP consortia by the establishment of national subgroups for the relevant specialities of the NHS Commissioning Board. The relevant National Clinical Directors should sit on these groups, and the groups should provide guidance for consortia. GP consortia should have leads for specialised commissioning who link up with the relevant clinical subgroups. These leads would meet regionally/subnationally and would engage with secondary care colleagues and public health specialists. Specialist public health and commissioning advice would also be essential to ensure that specialised commissioning is responsive to local need, is prioritised appropriately and takes into account the primary prevention aspects of the clinical conditions for which it is responsible; and to ensure that commissioning plans integrate prevention, primary and secondary healthcare and social care. Resource allocation decisions should be scrutinised to ensure that they are consistent with priorities for health and wellbeing. Specialist public health advice will ensure that only cost and clinically effective interventions are commissioned and that appropriate account is taken of overall population health.”
Indeed, in November 2012, the NHS Commissioning Board (NHS CB) and the Department of Health published their detailed agreement showing how the NHS CB will drive improvements in the health of England’s population through its commissioning of certain public health services. The agreement sets out the outcomes to be achieved in exercising these public health functions and provides ring fenced funding for the NHS CB to commission public health services. The services commissioned as part of this agreement are those where there is, for example, alignment with national clinical pathways and added value of central commissioning. Please refer to this document which details how public health functions to be exercised by the NHS Commissioning Board.
Whether you think the burden of opinion should be on the balance of probabilities or beyond reasonable doubt, there is a strong arguable case that there should be a Director of Public Health on the NHS CB. However, bodies which might have protected against problems in national health policy, such as the Food Standards Agency, the Health Protection Agency, and the National Patient Safety Agency, are all being abolished. Also, the fate of the NHS Commissioning Board itself after 2015, a body which has been called “the biggest QUANGO ever“, is uncertain.