“Citizens have become consumers with status proportional to purchasing power, and former public spaces have been enclosed and transformed into private malls for shopping as recreation or “therapy.” Step by step, private companies, dedicated to enriching their owners, take over the core functions of the state. This process, which has profound implications for health policy, is promoted by politicians proclaiming an “ideology” of shrinking the state to the absolute minimum. These politicians envisage replacing almost all public service provision through outsourcing and other forms of privatisation such as “right to provide” management buyouts. This ambition extends far beyond health and social care, reaching even to policing and the armed forces.”
And so write Jennifer Mindell, Lucy Reynolds and Martin McKee recently about ‘corporate capture’ in the British Medical Journal.
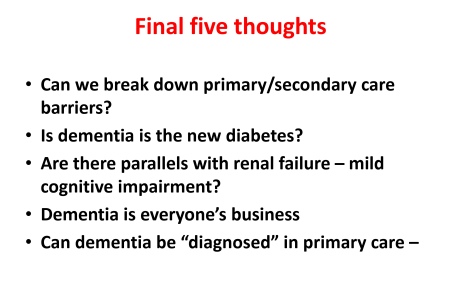
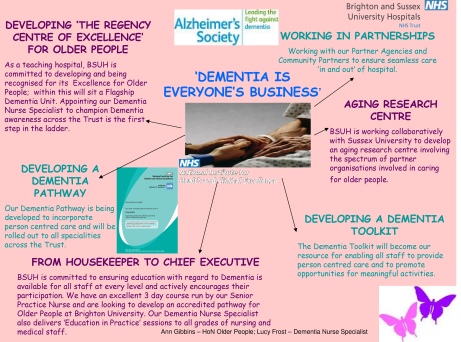
Alistair Burns, England’s clinical lead on dementia, recently concluded a presentation on the clinical network for London with the following slide:
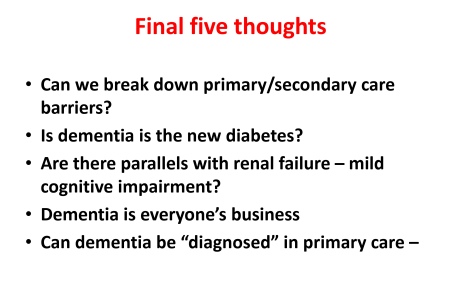
Alistair clearly does not mean ‘Dementia is everyone’s business’ in the “corporate capture” sense. Instead, he is presumably drawing attention to initiatives such as Brighton and Sussex Medical School’s initiative to promote dementia awareness at all levels of an organisation (and society).
The comparison with diabetes is for me interesting in that I think of living well with diabetes, post diagnosis, as conceptually similar to living well with dementia, in the sense that living well with a long term condition is a way of life. And with good control, it’s possible for some people to avoid hospital, becoming patients, when care in the community would be preferred for a number of clinical reasons.
Where I feel the comparison falls flat is that I do not think that it is possible to measure outcomes for living well with dementia easily. Sure, I have writen on metrics used to measure living well with dementia, drawing on the work of Sube Banerjee, Alistair’s predecessor.
It might be possible to correlate good control with a blood test value such as the HBA1c, and it steers the reward mechanism of the NHS for rewarding clinicians for failure of management (e.g. laser treatment in the eye, foot amputation, renal dialysis), but the comparison needs some clinical expertise to be pulled off properly.
The issue of breaking down ‘barriers’ between primary and secondary care is an urgent issue, and ‘whole person care’ or ‘integrated care’ may or may not help to facilitate that.
But the question of who gives the correct diagnosis of dementia, or even verifies it, won’t go away.
Having done Dementia Friends myself, a Public Health Initiative delivered by the Alzheimer’s Society, I feel the initiative is extremely well executed from an operational level. I think it’s pushing it for a member of the public to think that an old and doddering lady crossing the lady might have dementia and requires help, as medicalising ageing into dementia is a dangerous route to take.
The £2.4 million programme is funded by the Social Fund and the Department of Health.
There are a number of important clinical points here.
People with dementia need to be followed up across a period of time for a diagnosis of dementia to be reliably made, and ‘in the right hands’, i.e. of a specialist dementia service.
Some people have ‘mild cognitive impairment’ instead, and will never progress to dementia.
There are 149,186 dementia friends currently. This number is rapidly increasing. The goal is one million.
Furthermore, there are many people given a diagnosis of dementia while alive who never have it post mortem. And the diagnosis can only be definitively made post mortem.
Seth Love’s brilliant research (and he is an ‘Ambassador’ to the Alzheimer’s BRACE charity) is a testament to this.
This policy plank for me will also go back to the issue of whether policy is putting sufficient resources into the diagnostic process and beyond. Stories of people being landed with a diagnosis out of nowhere and given not much further information than an information pack are all too common. A well designed system would have counselling before the diagnosis, during the diagnosis, and after the diagnosis.
Ideally, an appointed advisor would then see to continuity of care, allowing persons with dementia to be able to feel confident about telling their diagnosis to friends and/or family. The advisor would ideally then give impartial advice on social determinants of health, such as housing or education.
But all this requires money and skill. There is no quick fix.
The areas of action for the Prime Minister’s Dementia Challenge are: dementia friendly communities, health and care and improving research.
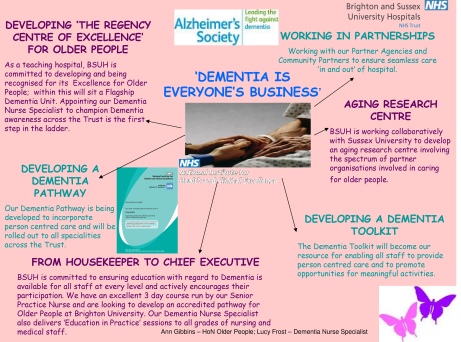
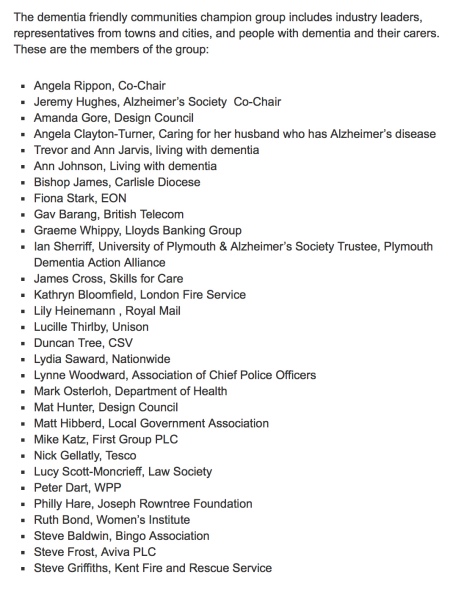
The term ‘dementia friendly communities’ is intrinsically difficult, for reasons I have previously tried to introduce. A concern must be the ideology behind the introduction of this policy in this jurisdiction. The emphasis has been very much on making businesses ‘business friendly’, which is of a plausible raison d’être in itself. This, arguably, is reflected in the list of chief stakeholders of the dementia friendly communities champion group.
It happens to fit very nicely with the Big Society and the ‘Nudge’ narrative of the current government. But it sits uneasy with the idea that it is in fact a manifestation of a small state which bears little responsibility apart from overseeing at an arm’s length a free market.
And meanwhile, the care system in England is on its knees. Stories of drastic underfunding of the care system are extremely common now.
An army of millions of unpaid family carers are left propping up a system which barely works. There appears to be little interest in guiding these people, with psychological, financial and/or legal burdens of their own, to reassure them that all their hard work is delivering an extraordinary level of person-centred care.
But this for me was an inevitable consequence of ‘corporate capture’. The G8 World Dementia Council does not have any representatives of people with dementia or carers.
That is why ‘Living well with dementia’ is an important research strand, and hopefully one which Prof Martin Rossor and colleagues at NIHR for dementia research will give due attention to in due course. But all too readily research into innovations, ambient assisted living, design of the ward, dementia friendly communities, assistive technology, and advocacy play second fiddle to the endless song of Big Pharma, touting how a ‘cure’ for dementia is just around the corner. Yet again.
So what’s the solution?
The answer lies, I feel, in what happens in the next year and beyond.
The Prime Minister’s challenge on dementia was developed as a successor to the National Dementia Strategy, with the challenge of delivering major improvements in dementia care, support and research. It runs until March 2015.
Preparatory work to produce a successor to the Challenge from the Department of Health (of England) is now underway in order that all the stakeholders can fully understand progress so far and identify those areas where more needs to be done.
The Department of Health have therefore commissioned an independent assessment of progress on dementia since 2009.
There are a number of other important pieces of work that are underway, which will provide information and evidence about progress and gaps. For example the All Party Parliamentary Group on Dementia chaired by The Baroness Sally Greengross OBE are producing a report focused on the National Dementia Strategy, and the Alzheimer’s Society has commissioned Deloitte to assess progress and in the autumn will be publishing new prevalence data.
Indeed the corporate entity known as Deloitte Access Australia (a different set of management consultants in the private sector) produced in September 2011 a report on prevalence of dementia estimates in Australia.
Deloitte themselves have an impressive, varied output regarding dementia.
But of course they are not interested in dementia solely. “Deloitte” is the brand under which tens of thousands of dedicated professionals in independent firms throughout the world collaborate to provide audit, consulting, financial advisory, risk management, tax, and related services to select clients.
Apparently, once all this work has been concluded a decision will be made on the focus and aims of the successor to the PM’s challenge.
The current Coalition government has been much criticised in parts of the non-mainstream media for the representation of corporate private interests in the Health and Social Care Act (2012).
I believe people who are interested in dementia, including persons with dementia, caseworkers and academics, should make their opinions known to the APPG in a structured articulate way in time. I think not much will be achieved through the pages of the medical newspapers.
And only time will tell whether the new dementia strategy will emerge in time before the next general election in England, to be held on May 7th 2015.
It could be a case of: all change please.
This blogpost first appeared on the ‘Living well with dementia’ blog.