Home » Shibley’s Own
The ‘NHS Five Year Forward Plan’ is a clever marketing stunt, and is barely a statement of strategy
There’s no “magic money tree”, except when you’re signing off HS3 on a ‘nod and a wink’ for £7 billion, or interventions in Iraq and Afghanistan for £30 billion.
As a piece of marketing, for Simon Stevens to set out a stall for the rôle of the NHS in a global economy, “the five year plan” was nice and succinct. As a piece of strategy, it is dreadful. It’s dreadful – even if you decide to take the view that health policy is entirely market-driven or “value-based”, and not in any way written through a sophisticated clinical prism.
The irony of a “five year plan” for the National Health Service is pretty quick to see. “Five year plans” were, of course, used by Stalinist Russia. Nazi Germany preferred ‘four year plans’ as a strategy for war readiness, in comparison.
It is reported that the “Five Year Forward View”, published last week by NHS England, is a collaboration between six leading NHS groups including Monitor, Health Education England, the NHS Trust Development Authority, Public Health England, the Care Quality Commission and NHS England.
And yet ironically the future of two of the contributing organisations is under doubt. In a fringe meeting earlier this at the Labour Party Conference, it was again mooted what the precise function of Monitor might be. This is because it is definite that an incoming Labour Party government, in its first Queen Speech, will repeal the Health and Social Care Act (2012), a much loathed piece of legislation. This leaves the precise functions of Monitor uncertain.
One possibility which Burnham is seriously contemplating is whether Monitor, if it continues to exist, serves to regulate the integration of services as would be expected in ‘whole person care’. Burnham intends to introduce ‘NHS preferred provider’, which could insist on the NHS being the lead provider in contracts for as long as ten years in the ‘prime contractor model‘.
And the future of the Care Quality Commission was put on a cliff-edge with the report of the Sir John Oldham Commission, again to do with whole person care. It would make much more sense to reform the regulators to oversee health and care with a single regulator in future. This would again be in line with the regulation of health and care professionals, much needed, and proposed by the English Law Commission, but kicked into the long grass by the current Government as it ran out of time.
The “5 year Forward View” to all intents and purposes reads like a marketing document, a wish-list for further privatisation of the NHS. It may ‘pack a punch‘, from the BBC which has unreservedly succeeded in throttling any discussion of the NHS reforms. But talk of ‘accountable care organisations’, as developed in Spain and the United States, and the emphasis on preventive health packages so keenly sold by multinational corporates, are paradigmatic of a wish-list of a privateer.
The document is a naked shill, intended to carry on the ‘case for change’ which has been made exhaustively by think tanks such as the King’s Fund which, some might say, were instrumental in giving the catastrophic policy of market competition in the National Health Service some legs in the first place.
But the runes are clearly there.
Take, for example, the seemingly-modest proposal of “integrated care commissioning”. The policy of personal budgets in the full glare of sunlight looks incredibly anaemic. Unanswered questions exist how a universal health system is going to be successfully merged with a means-tested care system. NHS England tried, unsuccessfully, to head this issue off at the pass as far back as in 2012.
Personal health budgets, which Simon Stevens has continued to speak moistly of, are the perfect vehicle for introducing ‘top ups’ and ‘copayments’, threatening the fundamental principle of universal, free-at-the-point-of-need.
And moves, not contained in the ‘5 year plan’, spell out an ominous direction of travel. It has just been announced that the much maligned contract for processing ATOS, given under the last Government to ATOS, is to be given to a company called Maximus, which has a proven track record in handing long term care packages in other jurisdictions.
“Independent” think tanks have never shrugged off successfully the “power of the prepaid cards”, see for example the DEMOS initiative. It has always been vehemently denied that there will be no merging of universal credit and healthcare provision, although Liam Byrne’s account of Jennie Macklin in Australia painted a rather different story in an article in the Guardian provocatively entitled “Let’s help disabled people achieve their full potential“.
Like a multi-national corporate document, the “5 year plan” is high on marketing but poor on strategy. A good example of this is given on page 36 in relation to a ‘threat’ facing the National Health Service, that of recurrent pay freezes to the majority of nurses whilst the economy is reputed to be recovering.
The seemingly innocuous line, at the end of page 35, reads: “For example as the economy returns to growth, NHS pay will need to stay broadly in line with private sector wages in order to recruit and retain frontline staff.” But it is well known that any wish to pay nurses a wage that reflects the value that runs through their work like letters in a stick of rock will be strongly resisted by the Treasury, while the Conservative Party will prefer further to tattoo the words of low taxes onto his breast plate of ideology.
There are other clear examples of the document clearly lacking in clarity. For example, page 33 sees a promotion of ‘personalised medicine’, how the NHS and “our partners” (meaning in the third and private sector, actually) might deliver the genome based ‘revolution’. Again, the document’s thrust is one of marketing, not clear strategy. There is no mention of the changes in resource allocation which would be required to serve this revolution, essentially seeing hardworking taxpayers subsidise the shareholder dividends or surpluses of large corporate-like charities. There is absolutely no mention of the changes in the legislative framework that would be needed, as in the United States, to prevent genetic information non-discrimination. But here again the document serves its marketing function – as a prospective prospectus for would-be investors wishing to spot lucrative opportunities in the NHS as a data mine.
Like there is no mention of “NHS preferred provider”, unsurprisingly there is no mention of “whole person care”. And yet, even if Labour fail to win an outright majority, it will seek to implement this being the largest party in Government. And this policy is set to see a profound change in the landscape of health and care provision for England.
In any business strategy, one is obliged to think of the political, economic, social, technological, legal and environmental headwinds (affectionately known as “PESTLE” to business strategists). A good example of social changes in the five years might have been, for example, a change in direction of the NHS being seen as resentment as costing much money, despite its striking efficiency, but one which values its workforce (for example in the salary of most of its nurses).
Looking at the political headwinds, it is quite incredible for example there is no mention of trade agreements such as TTIP and the investor-to-state dispute settlement clauses. If this ‘5 year forward plan’ had been at all serious, it would have been included, not least as it is a headwind which could drastically throw off course further the direction of travel of the NHS as a state-run health service.
Simon Stevens’ vision is a ‘charismatic vision’ of sorts. But a vision does not have to be particularly credible for it to get populist appeal or succeed. It just needs to be communicated clearly, with supine and compliant supporters in the trade media.
If the document were a ‘heads up’ for how we could afford a NHS through general taxation which was genuinely universal and free at the point of need, this document would have served a function. As it is, the document is a lubricator for mechanisms which could optimise the part that the private sector has to play, with no mention of the dogs being unleashed in the global marketplace – in much the same way Cameron refused to signpost “the top down reorganisation”. It is impossible for a strategy document for the NHS simply to airbrush out the political and legal factors which will be at play in the lifetime of the next Government. As it is, the NHS ‘5-year forward view’ is a basic piece of marketing, which as a strategic plan scores 0/10.
The “disastrous” performance of this Tory-led government was not accidental. It was entirely deliberate.
One conversation I once had with Jos Bell (twitter here), an incredibly productive campaigner and chair for the independent Socialist Health Association London division, had much more of a profound impact than I thought at the time.
I simply remarked that the Conservative-led government had been ‘disastrous’.
Jos disagreed. She pointed out that the term of office had gone extremely successfully for the few who’ve made shedloads of money through private equity and hedge funds.
A massive assumption we’re all prone to make, some more than others, is that the political class largely represent us and our interests.
The number of ‘lost votes’ is the reminder to all of us of how disconnected parliamentary politics have become with our needs and concerns.
There are, of course, some truly outstanding MPs, however.
Another realisation for many, almost a right of passage, is the “lightbulb moment” that some leading ‘independent’ health and care think tanks have not been offering useful reliable impartial advice after all.
The performance of some on the issue of competition, a shoo-horn for neoliberal markets, against the wishes of many professionals, is a testament to them.
Dodgy advice was used to prop up the business case for the Health and Social Care Act (2012), and it is going to take a long time to unwind from this.
I know of the misery that the ‘welfare reforms’ have had on the morbidity and mortality of disabled citizens. This does not prevent ATOS from fulfilling a lucrative contract, which was made under the last Government (Labour).
There are accusations and counter-accusations of the effects of injection of private capital, the private finance initiative, which many hope will be addressed properly by the incoming government next year. City financiers and law firms continue to benefit from this sustained policy which has reaped havoc on various ‘local economies’ of the NHS.
The sale of Royal Mail, and various other projects, into the private sector at an undervalue (it is alleged) clearly has not been to the best benefit of the taxpayer. But again many in the City, some alleged to be close to the current Government, have benefited personally (it is alleged).
Through the prism of me and my friends, this Conservative-led Government has been ‘disastrous’. But they’ve actually achieved a lot for themselves in the last few years in the tenuous argument of ‘austerity’.
The buzzword for George Osborne was ‘choice’, and you could hear a pin drop literally at George Osborne’s reassurance in his speech yesterday, “We’re all in it together”.
I simply can’t agree with political commentators who wish to pollute the discussion with their meme that ‘Labour do not wish like a party who wish to govern.”
Many grassroots activists in Labour are desperate to sort out the mess the country finds itself in.
They certainly detest the idea of a Tory-UKIP coalition.
The repeal of the Health and Social Care Act (2012) will be in the first Queen’s Speech of an incoming Labour government.
This Act of parliament turbo-boosted the aggressive pimping of NHS contracts into private sector providers. Correct – another set of beneficiaries from this government, led by the Conservatives but the lifeblood of which is currently provided by the Liberal Democrats.
In many ways, the next period of office is a ‘poisoned chalice’ once again, with debt in the last four years 4 x as much as the debt amassed by Labour in 13 years.
But, to repeat David Cameron, “we can’t go on like this”.
And the goalposts keep on moving.
An identifiable threat still remains having a means-tested social care service bolted onto the ‘universal’ health system, like a badly soldered “lemon car”.
A threat, less visible on the event horizon, is the corporatisation of general practice in the English jurisdiction.
I suspect that, despite the noise produced by UKIP and LibDems, the NHA Party will fail to make inroads in seats in the actual election. This will be of great sadness to me, despite the fact I wish all Labour candidates very well, as they are clearly campaigning on many relevant issues.
I feel that Labour will win the next general election. But I am terrified that, like the aftermath of 1997, it will be another missed opportunity for us.
The story of me
I’ll be giving a talk on Thursday 25th September 2014 on my personal experiences of alcoholism and interacting with the GMC, at a meeting called “Regulation, Respect and Health Practitioners” in London.
This is a draft of the text of my talk.
** Please check against delivery. **
Thank you for inviting me to speak for about 15 minutes on my viewpoint of the creation of a healthier regulatory process to benefit doctors and patients.
My speaking here comes at a time when there is a genuine drive for care and compassion in national policy in healthcare.
I believe that there should be a mutual respect between junior and senior clinicians, and the clinical regulator. In fact, I think this respect should be cherished and nurtured.
Last month, I had a hearing arranged by the Medical Professionals Tribunal Service (“MPTS”) to hear my application for restoration to the GMC register. This was just weeks after my 40th birthday.
I was asked by one of the panelists there what I had learnt most from my time off the register.
It is, of course, a necessary requirement that all Doctors on the GMC register have kept their skills up to date. This is so that Doctors can fulfill their obligations of performance, skills and knowledge. One of the benefits of having had at least five years out is that I’ve read the doctors’ code of conduct, “Good medical practice”, very many times. But I gave an answer which I don’t regret now for a moment.
I said, “Most of all, I finally know what is like to be a patient.”
I was erased in July 2006. At the time, it was uncertain what my ultimate diagnosis was, but a number of psychiatrists were in no doubt that I was suffering from an alcohol dependence syndrome. After I erased, I then spent heavily drinking alcohol a year in a pub. I used to go to local pubs at opening time, and leave at closing time. They say that unemployment is a big risk factor for mental illness.
Not being regulated at all by the medical profession was a big part of losing what I had perceived to be my identity. There was absolutely no structure or goal to my life. My life hit rock bottom. But, as an alcoholic, you soon realise that, however low you have gone, you can always go even further.
I had been first referred to the GMC a few years earlier. At the beginning of the process, no-one ever told me how long the regulatory process would last. This uncertainty about the future was a huge part, I feel, in my subsequent precipitous decline in mental health. I was erased ultimately for deficiencies in conduct and performance, and poor health, in 2006.
Whilst I was not punished for being ill, it was clear that the professional regulator could in no way condone my undisputed shortfalls in conduct and performance. The question about whether the clinical regulator views health to be intimately linked to professional conduct and performance is an important one. I do. This matter is also relevant to ‘revalidation’. I feel a junior must not ignore his own personal ill health first selfishly, above the needs of patients. He needs to get help as soon as possible. With the benefit of hindsight, I so wish I had sought help sooner.
When I was erased, I felt I became “public enemy number one”. However, they say that self-pity is a huge risk factor for drinking relapse. It was at one level a private shame . My father, who later passed away in 2010, was deeply humiliated by the whole experience, even though he had caused none of it. My father had been a GP for about 25 years. Therefore he adored the GMC. He felt GMC was “God”. But God moves in mysterious ways? As a loving father, he stuck by me throughout. As did my mother, with whom I still live.
The whole thing was, however, also a very public shame. You can still find reams and reams of it adorning Google. The avalanche of news reports about this, while creating a moral panic, virtually invariably never mentioned my severe alcohol illness. But that, as such, doesn’t matter to me any more even though I am keen on one aspect. I am still keen to remind myself of the distress I caused while I was powerless over alcohol. That’s why I have never asked for any of it to be deleted off Google in this jurisdiction.
I’ve never had a salaried job for the last eight years following erasure. In the only two job interviews I had for legal posts I was asked about my Google footprint of the GMC case.
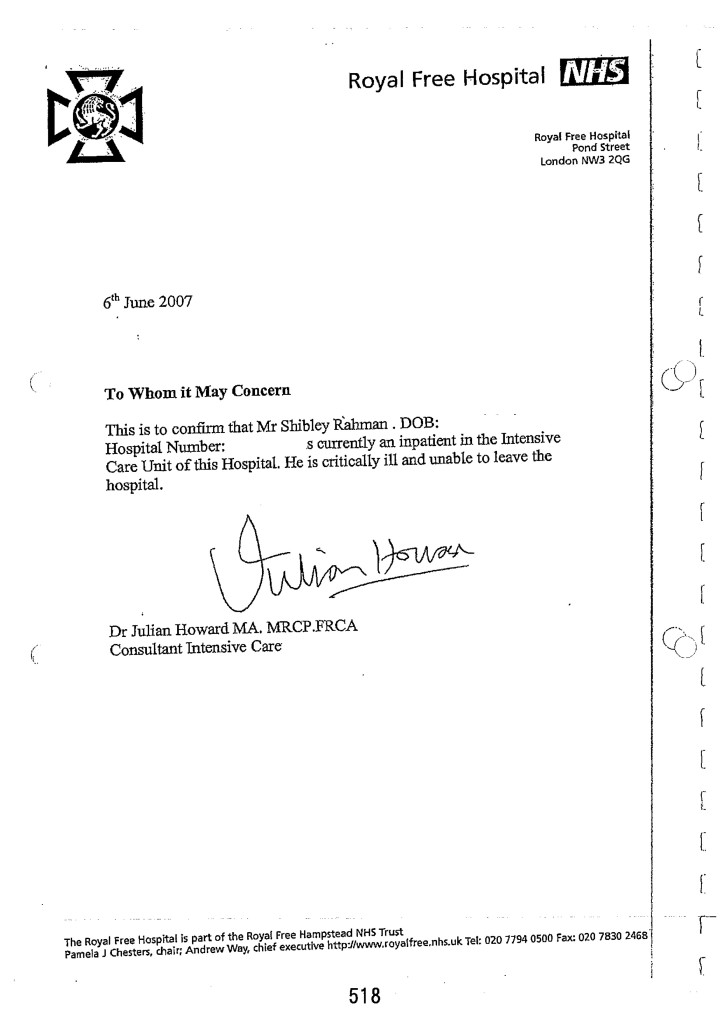
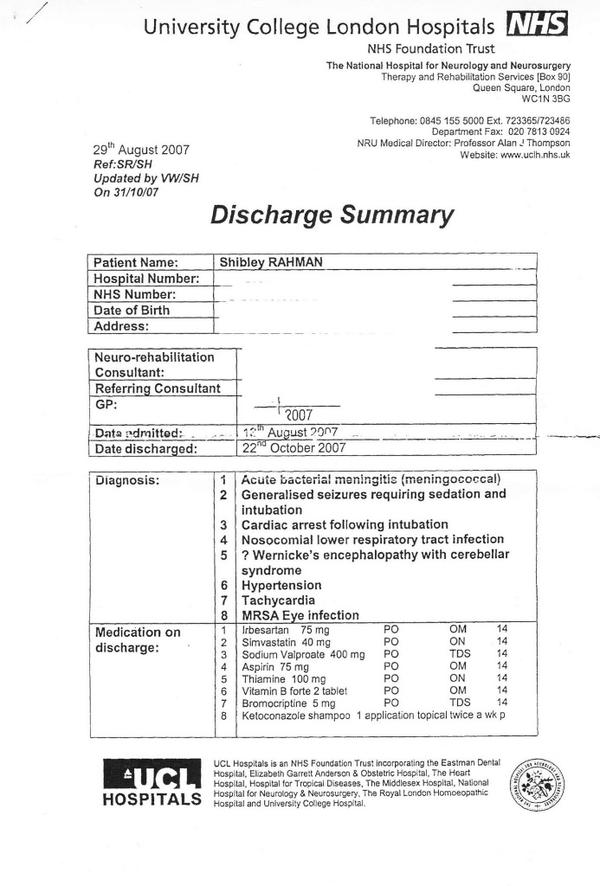
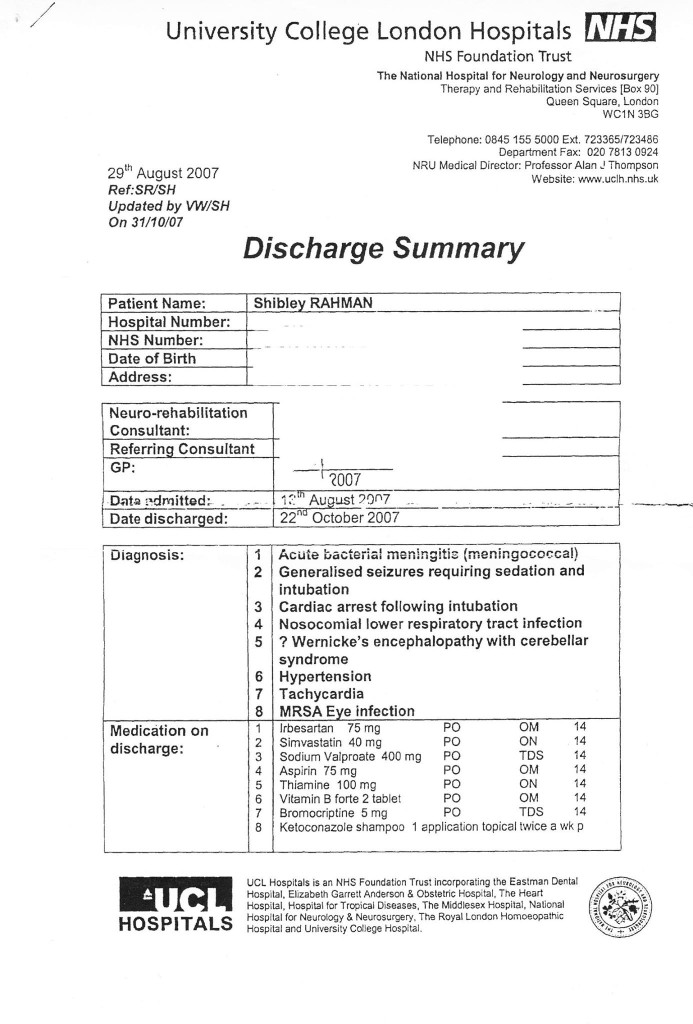
On a day at the beginning of June 2007, I was ‘blue lighted’ into the Royal Free. I had had an epileptic seizure, but the crash team lost my airway. They tried to intubate me, but I then had a cardiac arrest, from which I was successfully resuscitated. I literally owe my life to the NHS. I was kept alive for six weeks, while completely unconscious in a coma. When I woke up, I could not walk or talk. I became newly physically disabled. But the neurorehabilitation team at the National Hospital for Neurology and Neurosurgery, where I was in fact a junior doctor, then taught me how to walk and talk again. I remember how the occupational therapist taught me how to shop in a supermarket. I learnt, from scratch, how to perform basic tasks, such as making a cup of tea.
I always had loved medicine. I got the second highest First in neuroscience in my undergraduate course in Cambridge. I got my PhD in 2001 in identifying an innovative way of diagnosing behavioural variant frontotemporal dementia. I later passed my diploma of the membership of the Royal College of Physicians. I have published three books for junior physicians negotiating each of the three components of this demanding examination for core medical training.
My late father, however, emphasised to me that that coma, in many respects, saved my life. I agree with him now. It heralded the start of my period of abstinence from alcohol. I have now been in recovery from alcohol continuously for seven years. I take one day at a time. I am content now.
Since my coma, I have obtained my Bachelor of Law, Master of Law and my Master of Business Administration, and completed my pre-solicitor training. I adore the law as well, and I am fully signed up to the legal doctrine of proportionality, where the law must balance competing interests where they exist. I became regulated in 2011 by the Solicitors Regulation Authority after an extensive due diligence process.
Last month, my application for restoration onto the GMC Medical Register was approved.
This is not, however, by any means the ‘endpoint’ to my new life. I am not only keen to learn lessons for myself from the experience, but I am now also keen to help others. This is why I regularly attend, voluntarily, the ‘suspended Doctors group’ for “The Practitioner Health Programme”. I am under a psychiatrist, whom, without being hyperbolic, I feel saved my life.
I look back on the psychiatry reports of me when I was ill during 2004-2006 with utter disbelief. I was hugely in denial – had no insight into all how I at all junctures minimised the catastrophic effects of my active drinking. The “paradox” for dealing with a drink problem is that you cannot ‘do it’ on your own, and yet you must get help for the problem and realise your powerlessness over it. For me, it’s very simple – I can’t ever have a casual drink ever again. One alcoholic drink is one too many, and yet one drink is never enough. It ruined my life.
For me, the critical key to success is having a close circle of people in a social network, including an after care group in my local hospital, would be able to spot and intervene early in problem behaviour. For the first time in 2007, after my coma, I fully engaged with my General Practitioner. I had numerous ‘false starts’ in dealing with my alcoholism between 2004 and 2007.
I personally found the pressure of being investigated and dealing with my illness, during this period, unbearable. A part of me wishes, in retrospect, that I had been “better managed” in terms of performance at the time. Witness statements report me as looking ‘alcoholic’ and ‘dishevelled’ while on the wards, when my performance was clearly poor. A part of me wishes I had been “made to go to occupational health”, when these problems first surfaced.
But a part of me strongly resists my transference of blame onto other parties. As I admitted to my restoration panel, I made plenty of mistakes of my own: for example, I never engaged properly with my own G.P. until my coma.
I was most obviously, prior to my coma, a clear threat to patient safety. And it states clearly in s.1 (1A) Medical Act 1983, the GMC must promote patient safety. So I strongly believe the original sanction was the correct one.
But now, next month, as a different person, I’ll be presenting my research, based on an online survey, on the funding of dementia care. This will be at the prestigious Alzheimer’s Europe conference in Glasgow. This January, I published a popular book entitled, “Living well with dementia”. I feel that, with my truncated medical training thus far, and my postgraduate degrees in law, medical research and business management, I can be an asset to the public health and health policy arm of the medical profession.
For me, my return to the GMC register, after completion of the identity check, will be a huge privilege.
Sadly, it can be rather too easy for colleagues to gang up on individuals and ringfence problems, rather than solving the problems at root to make the health and care services better. I am sure that many juniors feel: “there for the grace of God go I”.
One cannot away from the enormity of the problem of unwell Doctors in the NHS, however. I felt totally abandoned during the regulatory process and could have done with more support at a time when I especially needed it? In conclusion, the public including staff would like to have pride in the medical profession and its regulator. I too would like to see this goal come to fruition one day.
It is a massive honour to be able to return to the GMC Medical Register. A dream come true.
Yesterday, I went for lunch with my friend and colleague, Prof Facundo Manes. Facundo kindly wrote a Foreword to my book ‘Living well with dementia”, an essay on the importance of personhood and interaction with the environment for persons living with dementia. We were just a stone’s throw from all those bars and pubs in Covent Garden I knew well in a former life.
I spent nine years at medical school, and very few as a junior doctor.
I’ve now been in recovery for just over seven years.
But in that time I do remember doing shifts starting at Friday morning and ending on Monday night. I remember the cardiac arrest bleep in Hammersmith at 4 am, and doing emergency catheters at 3 am in Norfolk.
I had an unusual background. I loved medical research at Cambridge. In fact, my discovery how to diagnose the behavioural variant of frontotemporal dementia is cited by the major international labs. It is in the current Oxford Textbook of Medicine.
Being ensnared by the General Medical Council in their investigation process devastated my father. He later died in 2010. I remember kissing him goodbye in the Intensive Care Ward of the Royal Free, the same ward which had kept me alive for six weeks in 2007.
I of course am completely overwhelmed by those events widely reported, especially in the one in 2004. The newspapers never report I was blind drunk. The media when they do not mention my alcohol dependence syndrome are missing out a key component of the jigsaw.
Until I die, I will never be safe with one alcoholic drink. I will go on a spiral of drinking, and that one event I am certain would either see me in a police cell or in A&E.
One event did change my life. I was blue lighted in, after a year of heavy drinking after I was erased by the GMC in 2006, having had a life-threatening epileptic fit. The crash team attempted emergency intubation, but I ended up having a cardiac arrest which was successfully resuscitated.
I do not wish to enter any blame games about what happened a decade ago. It turns out that the Trust which reported me as dishevelled and alcoholic, and having poor performance simultaneously, is in the Daily Mail this morning for a running a ‘chaotic’ A&E department.
It also turns out that another Trust in London which reported me as dishevelled and alcoholic, and having poor performance simultaneously, had its A&E department shut down this week.
I have written previously here about my experience as a sick doctor.
I was in denial and had no insight. Hindsight is a wonderful thing, but I needed sick leave and a period of absence and support. But I do not wish to blame anyway for those events I wish had never happened some time ago.
But the GMC referrals were absolutely correct. I had a proper medical plan put in place for me when I awoke from my coma. I followed religiously my own GP’s advice too.
I am now physically disabled, and have had no regular salaried job since 2005. But I am content. I live in a small flat with my mother in Primrose Hill. I regularly go out to cultural events. I maintain my interest in dementia, going to a fourth conference this year for Alzheimer’s Europe in October, where I have been chosen to give one of the research talks. It’s actually on an idea which David Nicholson inspired me over.
I’ve done four books on medicine, including one on living well with dementia. The Fitness to Practice panel in their judgment note my contribution there, which I am pleased about.
The Panel also crucially made the link in their judgment that my poor performance in conduct and competence coincided with my period of illness, the alcohol dependence syndrome, for which I am now under a psychiatrist.
I go to AA sometimes, and the weekly recovery support group at my local hospital. Being in contact with other people who are starting the same process of getting their life back continues to inspire me. I also attend the suspended doctors group for the Practitioner Health Programme, which helps me understand myself too.
I believe that there is no higher law than somebody’s health. I understand the pressures of why trainees preventing them from seeking help in the regulatory process.
But I do have an unusual perspective. First and foremost, I am a patient myself, and proud of it.
Secondly, I am regulated by the Solicitors Regulation Authority. I can become a trainee solicitor, if I want to be. I had a careful due diligence process in 2010, and I thank the legal profession for rehabilitating me.
Thirdly, I will now be regulated once again by the General Medical Council pending a successful identity check on October 7 2014. Having my application to be restored to the UK medical register is a massive honour for me. I caused a lot of hurt to others during my time with the medical profession last time, and this time I would like things to be different, and be of worth.
This, I hope, will mean a lot to my late father.
I am grateful to all the people at the Medical Practitioners Tribunal Service, and to the GMC prosecutor for presenting a fair case on behalf of the GMC who need to promote patient safety.
I am encouraged that the GMC’s new Chair, Prof Terence Stephenson, “gets” change for the better for the profession, and has an excellent track record as a clinical leader.
I genuinely feel it’s only a matter of time before the giant supertanker which is the medical profession changes its bearings to acknowledge that sick people in their profession exist. Dr Phil Hammond has done a superb article on this.
I love my law school, BPP Law School. They got me through this. I have become a non executive director of their Students Association now. There’s a lot of work to be done there, but I am lucky that there are two colleagues there of mine who are simply the best: Shahban Aziz and Shaun Dias.
I am now about to be regulated by two professions. I could not be happier.
Thanks for your support. I couldn’t have done it without you.
It’s time Jeremy Hunt justified the costly NHS reforms rather than pontificated about hospital food
I remember my stay at the National Hospital for Neurology and Neurosurgery as an inpatient.
Actually, I don’t remember hospital food being that bad. In fact, I can’t remember it at all. When the physiotherapists were teaching me how to walk again, and the speech and language therapists were teaching me how to speak again, after my six weeks in a coma due to meningitis, the quality of food was not top of my mind.
What did irk me was pressing the bedside buzzer, and occasionally people not answering. Or not knowing when the ‘investigations’ which I was down for were due to happen.
But I suppose I understand why Jeremy Hunt focuses on hospital food. I would be surprised if he’d spent a lengthy stay in hospital as an inpatient. I know he never studied medicine or nursing.
But having a headline on hospital food is either some weird denial of problems in the rest of the service, or a genuine desire to promote the quality of nutrition in inpatients.
Either way, what is aggravating is Jeremy Hunt’s steadfast refusal to explain what the point of the NHS reforms was.
We know it cost about £2 billion, at a time when the UK is supposed to be tightening its belt.
We know it led to a large number of contracts being awarded to the private sector.
We also know there is not a single clause on patient safety in the Health and Social Care Act (2012), which amounts to about five hundred pages, apart from the abolition of the National Patient Safety Agency.
But Jeremy Hunt clearly does not want to discuss the NHS reforms, despite the fact that the Conservatives and Liberal Democrats were determined to get this legislation through parliament.
He needs to explain to the English voter in what way the NHS reforms have improved the quality of the patient experience. Did I miss a clause on hospital food in the Health and Social Care Act?
Otherwise, this is a lunatic Government with a detached Secretary of State for Health who seems completely incapable of explaining the current policy on the NHS.
Lynton Crosby may not want to talk about the NHS, but he may find that mission quite unachievable as a huge army of people converge upon Trafalgar Square for the climax of the modern-day Jarrow March.
It could be that Jeremy Hunt feels that the average voter is too stupid to discuss the privatisation of the NHS, but can cope instead with a conversation about the quality and quantity of chips in an average NHS meal.
People do not go to hospitals for a great hôtel like experience, in the same way that people do not stay in hotels to get their hernias seen to.
In the run up to the general election, the opposition parties should maintain pressure on the Government to explain quite why they were so desperate to implement the costly NHS reforms. These reforms not only cost a lot of money, but further extended the democratic deficit between political parties and the average voter. It is clear that Andy Burnham MP as Shadow Secretary of State for Health has maintained his wish to repeal the ‘Lansley Act’, but the current Government should not be allowed to get away with its wish to talk about Douglas Carswell or terror alerts rather than the current state of the health service, aided and abetted by supine media organisations.
Out of sight, out of mind
Please note: This blogpost has been edited since the first publication, due to a factual inaccuracy of mine this morning where I stated the Tavistock Clinic was private.
It is not private. I do sincerely apologise for this mixup. It was an entirely accident error of mine.
I have also changed the word ‘aggressive treatments’ to ‘thorough interventions’ on the advice of two different people.
I am further posting Kate’s very helpful comment below the end of this article.
I am extremely grateful to Kate for her comment.
________________________________________________________________________________________
I have previously written openly about my personal experiences as a sick doctor and beyond (please see here). Thank you if you were one of the 2000 or views of that blogpost on that particular day.
In 2008, the Department of Health under the previous government funded a two year pilot to commission and provide a specialist, confidential, service, the Practitioner Health Programme (PHP).
The service was free to all doctors and dentists in London with:
- mental health or addiction concern (at any level of severity); and,
- physical health concern (where that concern was potentially impacting on the practitioner’ performance).
The PHP complemented existing NHS GP, occupational health and specialist services. It demonstrated the need for the service (over 500 patients have now been treated, many with complex problems) and how savings could be achieved through swift, safe return to work.
The 2009 Boorman review of the health of the NHS workforce reported that:
- the direct costs of ill-health in NHS staff are in the region of £1.7 billion p.a.;
- the agency staff bill for the NHS is around £1.45 billion p.a. (spending closely related to sickness absence and staff turnover); and 2,500 ill-health retirements (some possibly preventable) each year cost the NHS £150m p.a.
The Chief Executive of the General Medical Council, Niall Dickson, commenting on the PHP said:
“We know of the stress and anguish experienced by doctors who become sick and how this can affect their work. There is not enough good support at local level and the PHP programme has shown what can be done.”
It is now pretty widely felt that prevention and early intervention could save the NHS millions of pounds, and employers can achieve huge savings by supporting doctors and ensuring they remain fit to practise, whilst maintaining or improving quality. The potential savings for employers far outweigh the likely cost of establishing a nationwide service (estimated at around £6 million). There is therefore a real economic case, as well as averting tragedies in human lives training in the NHS.
If you’re a sick Doctor, ‘Good medical practice’, the GMC’s code of conduct, is triggered under domain 2 for quality and safety by the following clause.
In my own particular case, it is recorded in two detailed witness statements that I tried to discuss in detail the alcohol problem that was concerning me with two Consultant Physicians in London.
In neither case was I offered a programme of alcohol management. I confided in them personal details.
It is a real pity that I did take up an offer by a Consultant who recommended the Tavistock Clinic, as I erroneously thought it was private not public. Notwithstanding that, no offer of sick leave was made, but that is my fault for not having let the discussion get that far.
But I really don’t wish to play any ‘blame game’ – for example I failed in not being under a General Practitioner at the time, as I was at that stage absolutely petrified that that GP would have reported me to the GMC subjecting me to years of investigation. I had years of investigation anyway, but without the critical help I needed.
Being under a General Practitioner for a medical professional is a requirement of their Code of Conduct according to rule thirty.
I think many aspects of my dire situation reflects a fundamental misunderstanding of the medical profession thinking that if a sick Doctor is ‘aware’ of his problem he has full insight into the distress the problem is causing to friends, family and beyond.
I feel that, had my problem been aggressively dealt with earlier, the subsequent failures in my alcohol management would not have occurred (three years later).
My erasure for me was perceived by me as the ultimate personal failure for having been through a public hearing, treated still in the media as a “show trial”, and a personal failure for not having got clinically better. On a note of wider contrition, however, I have no objection to the issues I was found proven to this day, and I think the GMC ultimately made the correct sanction.
Media reports, despite public humiliation, distressing not just for me but my late father at the time, make no reference to my underlying medical problems. I was sectioned in May 2006 due to alcoholism. It’s as if the establishment wishes purposefully to airbrush doctors being sick.
I was distraught on my erasure, for having no solution to my mental health problems in sight. The regulatory process exacerbated my misery, with psychiatrists not being able to rule out at anxiety and depressive component while I was heavily drinking.
I know I was ‘aware’ of my problem with empty drunk bottles of red wine, but it doesn’t mean that I had the motivation to take time off work then to do something about it.
Likewise, the GMC code (see clause twenty eight above) assumes that the sick Doctor has full insight.
In my case, it had a very unpleasant end.
Not just this, days before my 33rd birthday,
but this six week coma and two month neurorehabilitation (the full discharge diagnosis from a place where I used to be a junior clinical physician once with no health problems.)
I think it is incredibly hard for anyone to understand outside of the system how you get raped of your dignity and integrity by the regulator when you fail to improve from mental illness. And often this mental illness is exacerbated by the regulatory process, as 86 deaths of Doctors awaiting Fitness to Practice during the same period of my investigation might appear to testify.
As I never had a performance assessment or clinical supervisor during my regulatory process, despite four different consultants concluding I had a severe alcohol problem at least between August 2004 and spring 2005, I feel I was put into managed decline long before the final hearing in July 2006.
I think personally the system for sick doctors undergoing the regulatory process from the General Medical Council could be much better, but that might be just be an unfortunate personal experience: ‘there’s nothing to see here’.
But a good first management step for me would be to roll out the Practitioner Health Programme to a jurisdiction wider than London. Lives truly depend on it, and the general public deserve better from seniors in the medical profession. This, for me, is absolutely necessary to maintain trust in the medical profession, domain 4 of the current GMC Code of Conduct. The GMC need to make the dealings open in this regard, fundamentally.
As far as the Consultants who contributed to my 2006 erasure were concerned, I have been out of sight and out of mind. In fact, I haven’t spoken to them for a decade and needless to say they have not wished to contact me.
I may be newly physically disabled following 2007.
I don’t personally wish the GMC any ill will. I believe in rehabilitation being a regulated student member of the law profession now – but do they?
I am back now.
Kate’s really helpful comment:
The Med Net service IS FREE and confidential.
When medical trainees encounter difficulties, college tutors, clinical tutors, programme directors and educational supervisors are encouraged to signpost them to Med Net. It was very positive that the consultant, who was not your educational supervisor, took sufficient pastoral interest in your welfare to give you the Med Net contact details. Ultimately, it is down to junior doctors to contact the service. Had you sought an appointment with your trusts OH team, they’d have given you the same contact details. It would have still been down to you to make contact. (< Indeed. Thanks , noted )
Alcohol-related disorders are outside the Mental Health Act, so it is impossible to compel people to undergo “treatment”. “Treatment” is an unfortunate term, as there is little that therapists can do until an individual wants help or becomes so incapacitated that they cease using. Even then, the notion of “treatment” as something that is done “to” people is inappropriate. This is one of the reasons why addictive disorders are outwith the MHA. Compulsion doesn’t work. “Aggressive treatment” is a particularly unhelpful concept more appropriate for the treatment of leukaemia rather than substance misuse disorders. Intense cycles of chemo-irradiation may induce remission in oncology, but intense input achieves nothing in addiction.
Kate then said it was a pity that I did not take up the offer of that Consultant, which I absolutely agree with.
The NHS will last as long as there are folk left with the faith to fight for it
Aneurin Bevan, the Labour Health Minister who created the NHS, famously said: “The NHS will last as long as there are folk left with the faith to fight for it”.
On 16 August 2014 a group of mothers from County Durham will set off from Jarrow to march to the Houses of Parliament, following in the footsteps of those who marched the route in 1936 to protest against mass unemployment. They did this as a bold but peaceful protest against the current NHS policy.
Whilst the Government can clearly influence the State media, it might also be true that the NHS will last as long as there are folk left in the social media and also those willing to show their democratic stand against the undemocratic demolition of a publically-owned NHS.
That people care about NHS issues, for example, is shown by the enormous affection held by many for groups such as the “NHS Action Party” and “Keep our NHS Public”, as well as the trades unions.
There have been some Labour MPs, especially, who have served in an outstanding way to represent the views of their constituents and beyond over health and social care policy.
The lack of credibility from the Department of Health is demonstrated in their statements below:
The first statement read, “We’re committed to an NHS which continues to be free at the point of use for everyone who needs it.”
The critical thing for the next Government not to do, of whatever political variety, is to introduce compulsory unified personal budgets and a system of co-payments, as that will torpedo in an onslaught against the free-at-the-point-of-need principle.
It clearly is a problem if one part of the system which is means-tested is soldered onto another part which is not means-tested, like a dodgy banger.
The second statement read, “By taking tough financial decisions elsewhere, this government has been able to increase the NHS budget by £12.7 billion during this parliament.”
Last year, the UK Statistics Authority upheld a complaint by Labour about government claims the NHS budget had increased in real-terms in the past two years.
And members of the current Government keep on lying about this.
The current Government took the public for granted in inflicting on them a £1.5bn top down reorganisation, turbo-boosting the awarding of contracts to the private sector.
Lynton Crosby, PR guru of the Conservative Party, does not want to talk about the NHS, it appears.
But now it is clear that people should make clear what type of NHS they wish to have.
Furthermore, the next Labour government will be seeking to fuse the NHS and social care, and to pool their budgets. This will be a huge step, and could have massive implications for the national roll-out of a shift from hospital to community care to promote wellbeing and health rather than acute crisis management.
People who have had their local hospital services shut down will also have a chance to make their opinions known. It is well know that many people do not want a ‘platinum service’ miles away, if they do not have ready access to an emergency service on their doorstep.
These are indeed testing times for the NHS and social care, but Jeremy Hunt fails to command a leadership necessary to lead the NHS beyond 2015, many feel.
Politicians need to wipe the blood from their hands from liberalising the NHS
All the main political parties in England have “blood on their hands”, and we’re never going to get anywhere near the Chilcot Inquiry to sort out how it happened. The ‘weapons of mass destruction’ unleashed by corporate agents seeded everywhere in think tanks, media and politics have gone out of the way on a tirade of abuse against workers in the public sector. There are so many nexuses which have become uncoupled, that the NHS and social care systems no longer have anything like a situation approaching credibility.
Top CEOs in the NHS in England can still receive generous renumeration, even if their patient records are worse than the Black Hole of Calcutta. Even if multinational corporates do not perform adequately on a contract, the NHS does not have the legal know-how to ‘performance manage’ these contracts, and will not wish to spend the money. The NHS is scared of imposing any penalties, because of the powerful lawyers of multinational corporates. Above all, in addition to ‘patient safety’, that other secret weapon is used, namely ‘continuity of care’. Continuity of care is another chameleon wheeled out in a guise which suits its purpose at any one time.
Whilst the Blairites continue to espouse that it does not matter who is a Doctor at any one time, corporates are equally happy to use the legal stun gun of saying continuity of care will suffer if contracts are disrupted.One of the lessons from social care should have been that there are pockets of extremely poor social care, fragmented and expensive. As the next Government wishes to integrate care, with or without whole person care, one suspects that merging a means-tested system with one which isn’t will not be “no problem” as some senior health commentators have pretended. The idea that a self-directed budget where you pay for your service is “free at the point of use” is twisting the truth beyond all banality.
And these privatised contracts are neither accidental or insubstantial. One is a 10-year contract worth £1.2 billion for providing cancer services in Staffordshire, and there is also a five-year contract worth £800 million for the care of older people in Cambridge to last for the duration of the next Parliament. Both Labour and the Conservatives set in the present and previous administrations set the mood music for this, and politicians need to wipe the blood from their hands of the stains of neoliberalism. The new Jerusalem offered by private companies fraudulently (but legally) using the NHS logo has clearly run its course. Some in the UK Labour Party should be ashamed of itself for not articulating more clearly their opposition to such obscene onslaughts to the socialist founding principles of the NHS. The public clearly want a properly funded NHS. It is up to a credible party to provide that. Co-payments are a tax on the sick. Even “Pat” Hewitt, the doyenne of a previous Labour administrator, gave a speech to the London School of Economics in 2007 saying it would be madness to go down this route.
And some of the performance of companies to which the NHS has been outsourced is an insult to taxpayers, hardworking or not. Outsourcing giant Serco today announced plans to withdraw from the clinical health services market in a move precipitated by a multimillion pound loss on its NHS contracts. It is possible that Serco’s planned withdrawal could influence significantly how other private firms view the prospect of bidding for contracts involving patient facing services.
The group had already made an early exit from its contracts to provide Cornwall’s out of hours services and clinical services to Braintree Community Hospital.
Introduction of competition into the liberalised market generally has been a policy disaster of totemic proportions, producing sources of corporate fraud and misfeasance, a policy crowbar which can make mergers on the basis of clinical need unlawful, a mechanism for introducing substantial additional transaction costs, and a way of introducing private providers where profit goes into shareholders’ pockets not as surpluses in improving the service. Think tanks which aggressively pimped this have blood on their hands. And they will need to backpedal fast on their prostitution of the purchaser-provider split too.
Earlier this year, it was hailed as a success that the first private sector operator of an NHS hospital has halved its losses in the year to December. AIM-quoted Circle Holdings took over the running of Hinchingbrooke Hospital in Cambridgeshire in 2012 in a controversial part-privatisation. Private companies though wish to have their cake and eat it. They want to hide behind the cloak afforded by the Freedom of Information Act from Tony Blair’s reign. And why should the private providers get protection they haven’t earnt like a welfare claimant so despised by Iain Duncan Smith and Rachel Reeves? Private patients cannot complain to the Public Services Ombudsman for Wales unless they have received treatment commissioned and funded by the NHS. But the Welsh government has now said it has has no plans to bring private health providers within the ombudsman’s remit. Would the private sector like to contribute towards the education and training of the healthcare workforce?
This debacle from Serco, in fact, follows hot on the heels of news from Musgrove Hospital, Taunton, Somerset, where it turns out that dozens of people have been left with significant damage after undergoing operations provided by a private healthcare company at an NHS hospital. The routine cataract operations were carried out by the private provider, Vanguard Healthcare, in May to help to reduce a backlog at Musgrove Park. But the hospital’s contract with Vanguard Healthcare was terminated just a few days after thirty patients, most elderly and some frail, reported complications, including blurred vision and signs of inflammation including pain and swelling.
Laurence Vick, a medical negligence lawyer and the head of the clinical negligence team at Michelmores solicitors in Exeter, had been approached by some of the patients for whom there had clearly been a breakdown of a duty of care. Vick further said the case highlighted the “uneasy relationship” between the NHS and the private sector. He said the question of who paid – when outsourced NHS treatment – failed was of growing importance as more services were handed over to the private sector. This “uneasy relationship” which Vick refers to is likely to get massively worse as one cannot pin down who is legally accountable for failure for performance by subcontractors in “the prime contractor model”, where a main contractor can lead subcontracts for contracts say lasting ten years.
So Tony Blair was blatantly wrong: it does matter who provides NHS care. Blairites have unleashed ideological weapons of mass destruction on the Welfare State, and someone should pay the penalty for this. And it’s worse than that – you don’t know any more who’s in receipt of your taxes when you pay for what you think is the NHS. The Welfare State is being killed softly: and all English neoliberal parties have blood on their hands.
Polling firm ComRes recently found that 49% of people would be prepared to pay more tax to help fund the health service, one in three (33%) people said they would not be ready to do so, and 18% did not know either way. The public’s willingness to pay extra tax to help the NHS has reached its highest level in over a decade amid growing concern about hospitals slipping into the red, waiting lists lengthening and the service becoming unsustainable. The plan always was from the neoliberal advocates to produce a small state with low taxes, but what we have ended up is a moderate state with moderate-high taxes to fund the shareholder dividends of the outsourced companies in a range of sectors, including probation and health.
The Conservatives feel that their voters do not like ‘unfairness’ with one person obtaining an unfair advantage over another, but what we’ve got now is outsourced companies still be paid for unbelievably bad performance, and top CEOs in private providers experiencing a world nothing like their nursing counterparts in the NHS.
Labour will always try to woo the City all it wants, as per
But if disenfranchises hardworking nurses maintaining the fabric of the NHS, and brown nosing the City, it will find it does not get elected. And many socialists in Labour will not want to have blood on their hands in being part of Labour either. This because there is no obvious disinfectant yet.
All a far cry from the Spirit of ’45.
Stop telling us we like buffoons and flat taxes. We want a properly run NHS.
Imagine if Andy Burnham as Secretary of State for Health in a Labour administration just turned up scruffy, tossing around his blonde locks, guffawing loudly.
Or if he was pictured in pubs, regularly having pints of bitter, looking like an escapee from your local golf club?
It just wouldn’t wash. What sort of country is it that likes buffoons and not statesmen? One made by the BBC.
The BBC have relentlessly not discussed the Health and Social Care Act (2012). They refuse to admit that it turbo-boosts the awarding of contracts to the private sector.
It doesn’t wish particularly to mention hospital closures, either.
Both Farage and Johnson clearly love themselves, and nobody knows what their policies are on anything.
And yet they represent highly dangerous people. Narcissistic in approach, they are both capable of being fiercely ambitious.
They might seem perfectly innocent, until you consider the danger posed by a Tory-UKIP coalition. Oliver Letwin is thought to think it’s only a matter of time before the general public wishes to discuss ‘the flat tax’. And guess what – Farage has been said to like the flat tax.
This current Government has made a big song and dance of people not paying their own way, the “something for nothing” culture. A favourite is of course that bloke with his curtains drawn, just as off you’re off to work.
But never mind the corporate tax dodgers. There are some people who would love to get away with paying the rock bottom for the NHS. They would happily see social care completely go to pot.
A flat tax would be perfect for those who want to contribute the bare minimum for the NHS. These are the same people that have pedalled the myth that it is the ageing population that is the big driver of the NHS budget: it is not, it is the aggressive pimping of technology by the corporate sector.
But behind these sinister agenda, ably implemented by the BBC, lies two buffoons, for whom butter wouldn’t melt in their mouths.
Andy Burnham would never be able to get away with the lack of policy on health as per Nigel Farage. He would never get away with acting like the faux idiot like Boris Johnson.
There are millions of people who want a stop to this crap, and want a properly funded NHS, comprehensive, free at the point of need, with a real sense of collaboration and solidarity led by competent statesmen.
What we instead get is a media over-promotion of people who pride themselves on behaving like a couple of airheads, Boris Johnson and Nigel Farage.
I understand why there have been so many deaths of Doctors waiting GMC FTP. That could easily have been me.
At least 96 doctors have died while facing a fitness-to-practise investigation from the General Medical Council since 2004, though it is not clear how many of these cases were suicide.
I can understand exactly how this has happened.
I had a prolonged GMC investigation between 2004 and 2006. At no point during this process was I told when then this mentally arduous process would come to an end.
I think now, seven years into recovery, that there by the grace of God go I.
The media have a remarkably level of detail of understanding from the perspective of the General Medical Council about forthcoming cases. It is impossible for the Doctor to get his side across in the media.
The GMC claim they don’t do show trials.
But my father was fully humiliated with the media storm.
My father was faced with a Doctor son who was in denial and lacked insight. My father is now dead, but I should like to say he probably died in complete humiliation of his son.
My experience is of a GMC which plays to people’s weaknesses in low self esteem and low confidence, a personality trait shared by many with addiction disorders.
Not one report in the mainstream media reported that I was severely alcoholic. And yet the GMC, prior to their erasure of me, erased me with five independent reports stating clearly that I had at least a severe alcohol problem; and that I needed help.
One of the referrals to the GMC was when I attended the A&E of a hospital with acute intoxication. In addition to the referral to the GMC by the Consultant in A&E, I was not offered any post-event support for alcoholism.
The GMC know how to present themselves in the media, but this is in contradistinction to the experience of those who have experienced the Fitness to Practise process first hand.
Dr Peter Wilmhurst writes in 2006 in a wide-ranging criticism of the GMC as follows:
In wishing to infer ‘bad character’, the General Medical Council must not go beyond its statutory duty of promoting public safety. Otherwise, there is simply mission creep and a torrent of smears into a hate campaign by the regulator or its company.
In 2005, one year before I was eventually due to see the GMC, I was suspended. This was due to an alcoholic bender in Northwick Park. I was crying all day in a pub because I could not cope with the investigation any more.
I had waved goodbye to my late father, and lied to him saying I was going shopping.
I didn’t. I ended up being sectioned by a psychiatric hospital in North London, and my father spent ages talking to the medical staff there.
I was then suspended. It was at that point, I wished to call it a day.
I phoned the Samaritans, and they talked me out of it.
I have never told anyone this story. I feel very strongly about what the General Medical Council did to me, even though it might have been merely a product of their inefficiency.
Nobody appears to wish to want to change the system. I’m pretty sure that there are juniors who wish to hold tight until they are Consultants.
What happened to me is that I had consultants in two Trusts in West and North London who said I was ‘late for work’, ‘smelling of alcohol’ and ‘dishevelled’.
None of this got reported in the main media.
I was erased. To this day, I still have no idea who retrospectively complained in graphic detail about my alcoholism did not offer me sick leave, or help with occupational health.
One of them even had the gall to write in his witness statement for the GMC that he gave me the phone number of a private clinic.
I find this particularly ironic as I was later done for incompetence, when that North London trust had allowed me to finish my medical job there, successfully running cardiac arrests there. I passed my Advanced Life Certificate there. I even have the certificate to prove it.
I feel disgusted by the way that the General Medical Council goes about its business.
Far too many one-sided media reports appear in the media containing detailed accounts, as yet unproven. There’s a sense of being hung before you even go to the gibbet.
I am now in my seventh year in recovery. I have done four books, and my Bachelor of Law, Master of Law and Master of Business Administration.
I even completed my pre-solicitor training, as I am regulated by the Solicitors Regulation Authority.
My late father died two months before the Solicitors Regulation Authority gave me permission to finish my legal training, after a meticulous consideration of various factors including details of my erasure.
I am now applying to be restored. And so everything gets racheted up again. The dogs will get unleashed.
And so far they’ve dragged me up to the City where I was struck off, without my late father, surrounded by the same bars and clubs and restaurants. I didn’t have a relapse. Care and compassion are simply two words which are not in the GMC’s dictionary.
I am even applying to go to a desk, non “facing job”. I am now following my erasure newly disabled, so I would not wish to do clinical medicine in any form.
I do not want to be in public health with the stigma of having been erased, for a period of life when I was very ill, and the undoubted discrimination that that would entail.
I had one year of sitting in a pub all day after I was eventually erased in 2006.
This was an extremely dangerous part of life. For my father, it was unbelievably distressing. Nonetheless, he came to visit me every day on the ITU when I was in a coma due to this a year later.
I so understand why there have been so many deaths of Doctors waiting GMC FTP. That could easily have been me.
But I am fighting fit now, and looking forward to my hearing very much.