Home » NHS Commissioning
David Prior is right, but his solution is wrong. Radical change is needed to abolish the NHS’ internal market.
In an article in the BMJ in 2011, entitled “How the secretary of state for health proposes to abolish the NHS in England” (BMJ 2011; 342 doi: http://dx.doi.org/10.1136/bmj.d1695 (Published 22 March 2011) by Allyson Pollock and David Price), the authors comment:
“The coalition government’s Health and Social Care Bill 2010-11 heralds the most controversial reform in the history of the NHS in England.The government plans to replace the NHS system of public funding and mainly public provision and public administration with a competitive market of corporate providers in which government finances but does not provide healthcare.”
On the other hand, a radical shift in the culture of the NHS is needed to rid it of outdated working practices, cure it of widespread bullying and heal the damaging rift between managers and clinicians, according to David Prior, chairman of the Care Quality Commission (CQC)
Prior has called for serious “transformational change” of the health service, without which it will “go bust”. That is not the radical change the NHS needs.
We need to abolish the internal market of the NHS.
The most significant piece of evidence that supports that view that market failure is the big problem in healthcare delivery is the widespread recognition that price competition actually worsens healthcare outcomes. Economic theory predicts that price competition is likely to lead to declining quality where (as in healthcare) quality is harder to observe than price. Evidence from price competition in the 1990s internal market and in cost constrained markets in the US confirms this, with falling prices and reduced quality, particularly in harder to observe measures.
The opposition to the Health and Social Care Act (2012) ended up being all over the place due to lack of any meaningful media coverage from the BBC and other media outlets, and a failure of supposedly intelligent people to cut through the crap and spin of what the Act was about. The Act was simply about putting in a competitive market, regulating the market, and finding a preliminary mechanism of winding up the ‘unfittest’ so that they couldn’t survive. The Act was nothing to do with patient safety. And we all know what an unmitigated costly fiasco this has been, and decisions have even be made on the basis of competition law rather than the health of the patient.
It’s been a shocking disaster.
The problems of market failure are already well recognised in the UK. Scotland and Wales have both abandoned the purchaser-provider split. In England, the problem of price competition is well recognised and most hospital tariffs/”prices” are fixed. Thatcher’s purchaser provider split (1989) has been well critiqued in the literature and the recent
A Health Select Committee (HSC) report, commissioned by the Department of Health from York University (Karen Bloor), on the current commissioning model was even more damning.
“If it does not begin to improve soon, after 20 years of costly failure, the purchaser-provider split may need to be abolished.”
The HSC report cited that the administrative costs of the purchaser-provider split to be as high as 14% of total NHS budget compared to 5% prior to the purchaser-provider split.
Other examples of where the market has failed the NHS include the use of the Private Finance Initiative (PFI). The NHS IT disaster is a classic case of market failure.
The Baroness Morgan affair has focused attention on the political nature of our unelected quangocrats are. For those unfamiliar with the story, she claims No 10 is “absolutely determined” to ensure that only Tory supporters are appointed to public bodies.
The idea of the free market being the best way of enabling individuals to plan their lives is nonsense. The free market system also generates huge inequalities between countries and regions. In the free market system, investment tends to go already where it is most profitable. Further, the free market system counts or recognises as important considerations only what can be packaged as commodities for individual consumption. The solution is not of course a bureaucratic manipulation of the economy and bureaucratic nationalisation like that being carried out by Bismarck in Germany. Socialist planning does not mean that we want to do away with free markets straight away. Many reasonable individuals recognise that free markets played a huge role in human development, and cannot be dispensed with overnight. Socialist planning is not primarily about faster economic growth. It is not even primarily about increasing control over the economy. It is primarily about decreasing the control of the economy over human lives. Some highly successful capitalist systems, such as Japan’s or South Korea’s, have had effective government planning of major investment. There is no reason to suppose that democratic planning would be less workable.
The importance of planning by the state, within its proper sphere, is unapologetically acknowledged. A free society needs a strong, confident state capable of carrying out on behalf of its citizens its vital role — including the planning required by that role — effectively and efficiently in a world of unpredictable challenges and threats. Under capitalism, there is always a drive for more profit, for this or that new profitable line of production, for increased pressure on the worker to work more. In fact capitalism does not even satisfy the wants which capitalism creates. Signals are sent through the market only by consumers with money, not by human wants or needs. The whim of the rich is satisfied; the desperate need of the poor is not. The real driving principle of capitalist economics is not consumer demand, but profit.
In Japan, they have the most tremendous technology, and they could produce the basics of life with a relatively small effort. It would be possible for people to have a relatively leisured and dignified life. Despite that, something like 70% of Japanese workers say that they constantly feel physically exhausted and mentally exhausted. Socialist planning is not about state planning of people’s whole lives. And even in the area of basic production, we will not be able to plan social needs straightaway. It will take generations before the level of technology, the degree of information and culture, and the spirit of co-operation have developed enough to make the planning of basic economic essentials just an administrative question. Subsidiarity requires that state planning should be restricted to tasks in relation to which individuals and groups cannot plan for themselves, and which cannot be handled by organisations independent of the state and operating in markets, preferably real markets.
It is a highly significant problem that the great majority of the people, toil only to enrich the top 10 per cent, who in Britain own 53 per cent of all marketable wealth and almost all land and shares. Everyone could have a decent job, and the excess of what the workers produce over their own direct consumption would go to social provision and to socially-controlled investment. We could get rid of the vast waste and duplication arising from capitalist competition. A living wage could go a long way to ensuring people are paid a fair amount for their work, giving employees dignity and security
As Alex Andreou wrote earlier this year,
“The richest 85 people in the world have as much wealth as the poorest 3.5 billion – or half the world’s entire population – put together. This is the stark headline of a report from Oxfam ahead of the World Economic Forum at Davos. Is there a reason why the world’s powerful, gathering at the exclusive resort to sip cognac and eat blinis, should care? Well, yes.
If one subscribes to the charitable view that neoliberal philosophy was simply naive or misguided in thinking that “trickle down” would work infinitely, then evidence that it doesn’t, should be cause for concern. It is a fundamental building block of supply-side economic theory – the tool of choice these past few decades for those in charge to make adjustments. The realisation that governments have been pulling at economic levers which, for some time, have been attached to nothing, should be a wake-up call to the deepest sleepers.”
In the absence of free markets, it is said that prices go up or fail to reduce. The way in which companies can collude with each other in delivering excessive profit and poor value-for-money for the consumer is well known in privatised industries. Books have been written on the subject. There are legitimate questions as to the effectiveness of the EU, but hats off to its commission for exposing the scandal of big oil companies allegedly colluding to rig petrol prices for a decade. Prices have risen 80 per cent, from 75p per litre in 2002 to around £1.40 per litre now.
It is also argued that innovation is blocked through collaboration. This is unmitigated rubbish, as collaboration has been well described as a driver for innovation even in the private sector.
“One of the top priorities of the group is to offer consumers innovative products. The ability of its suppliers to propose new solutions and technology and to develop innovative products and services in partnership with the L’Oréal teams makes a direct contribution to the success of new products. This collaborative process is based on trust in an ever more competitive economic climate. L’Oréal establishes an open dialog that stimulates and accelerates innovation for the benefit of consumers.”
Real capitalist markets do not correspond with the “ideal” of efficient, reliable balancing of supply and demand. At almost all times outside wars, capitalist economies generate vast armies of the marginally employed, people defined by the system as “excess supply” of labour-power. Successful service reconfigurations, such as stroke reorganisation in London, involve complex planning and engagement. Market forces cannot be the right way to drive socially responsible and clinically sustainable, equitably distributed and politically palatable service configurations and integration.
David Prior is right. But he’s like a Doctor who’s produced a correct diagnosis of a heart murmur and advised totally the wrong management plan like total bowel resection. The question now is whether a move towards a “NHS preferred provider” is an incremental step, but not sufficiently radical, to abolish the market. The ultimate way to reconcile this would be to have private providers providing NHS and other care services not on a transactional basis, but the choice, as they say, is theirs.
Lucy Reynolds is back – a chat with Bob Gill on how the marketing of NHSprivatisation has been tweaked
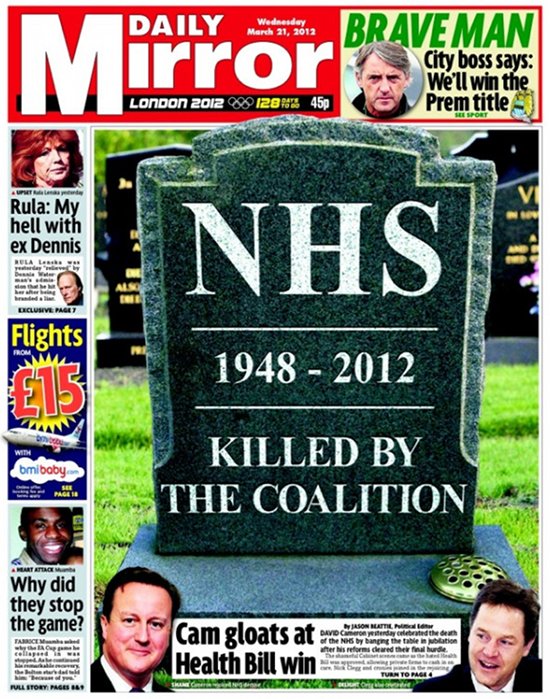
This was the front page of the Daily Mirror at the time.
The original video is here.
This video is a follow up on Dr Lucy Reynolds’ earlier analysis of the government’s ongoing programme to privatise the NHS by stealth.
Talking to local GP Dr Bob Gill (@drbobgill), she also elaborates on measures people can take to head off this programme, particularly in relation to the House of Lords debate on April 24th.
Will looking for blame in the ‘prime contractor model’ end up like one giant “pass-the-parcel”?
In a previous article of mine, “Outsourcing has become a policy drug, and they need to kick the habit”, I explained how the aspiration to have a smaller State had led to “reform” of the public services where the situation was now far worse.
Public money is being siphoned off into private sector shareholder dividends. Worse still, some performance monitoring of ongoing contracts is terrible. Furthermore, many outsourcing companies are currently embroiled in criminal allegations of one sort of another, mainly fraud.
It does seem a laudable aim to integrate healhcare (including mental health care) and social care. Indeed, by calling it ‘whole person care’, you temporarily get round the comparison to the ‘integrated shared care plans” of the United Staes.
The Health and Social Care Bill initially started life as the tr0jan horse of competitive markets into the NHS. Once this approach under Earl Howe blatantly fell apart, Norman Lamb was left to bring up the policy rear by talking about “integrated care”. However, the problem with integrated care is that it is yet again being launched as a launchpad for private providers to rustle together huge packages across a number of different areas through subcontracting.
Of course, one can argue that it’s great that a private provider can take control of so many different diverse services. But remember when the same argument was used to attack the NHS as ‘outdated’, ‘bloated’ and ‘Stalinist’? Such arguments for economies of scale or promotion of a coherent national health policy were jettisoned in favour of a fetish for introducing the market into the NHS at high speed. Unfortunately this policy has been totally discredited.
On the “prime contractor model”, the eminent health commentator Roy Lilley remarks:
Is this novel contacting or dumping the problem on someone else. Imaging trying to unpick a problem in the pathway. Everyone will blame someone else. This is a giant game of pass the parcel, isn’t it? The prime contractor may be accountable but they will pass the accountability up the line, delays will occur in getting answers. They will become a CCG-lite.
The prime contractor model involves a single organisation subcontracting work to other providers to integrate services across a pathway. A proportion of payments is dependent on the achievement of specific outcomes. Dozens of clinical commissioning groups are already said to be devising “innovative” contracts in which a lead provider receives an outcomes based payment to integrate an entire care pathway. For example, if the £120m deal is finalised, Circle ? which also runs Hinchingbrooke Health Care Trust ? will be financially and clinically accountable to commissioners for the whole pathway. The CCG said this previously involved 20 contracts across primary, secondary and community services. That news came after Bedfordshire CCG was named private company Circle as its preferred bidder to be “prime contractor” for an integrated musculoskeletal service.
Outsourcing companies don’t particularly appear to care what sectors they operate in, whether it’s in the running of healthcare, asylum seeking or probation services. Such an approach therefore lends itself easily to each citizen becoming a number not a name. The idea of us all having a special ‘services mastercard’ is not that far-fetched now, and if one day NHS budgeting is linked up with benefits, we’ll be yet closer to this ‘brave new world’.
In March 2012, G4S won a massive £30 million UK Border Agency contract to house asylum-seekers in the Midlands, the East of England, the North East, Yorkshire and Humberside. Using the “prime contractor model”, which G4S tells investors is “attractive”, the company granted subcontracts to UPM and the charity Migrant Help. And yet, in July 2013, Stephen Small, G4S managing director for Immigration and Borders, and Jeremy Stafford, Serco CEO for the UK and Europe were forced to defend their record before the Home Affairs Committee into the asylum system.
Serco’s evidence to the Committee revealed that in the North West it directly manages homes for asylum seekers through what the chair Keith Vaz described as ‘around twenty subcontractors from Happy Homes Ltd to First Choice Homes and Cosmopolitan Housing’.
Jeremy Stafford of Serco claimed this apparent recipe for housing management disaster was in fact a proven way of outsourcing and privatisation. It is ‘a very effective model and we do that in a number of the services we deliver’, he said.
This confidence in the ‘new delivery model’ of privatisation in the COMPASS contracts seems somewhat misplaced in the context of the JRF evidence. For it reveals that Reliance, the other security company with asylum housing contracts in London, the South West and Wales, sold on the privatised contracts after only two months to Capita and Clearel. The new provider, Clearel, did not fulfil the requirements of the contracts as tendered.
Only this week, the Serco boss quit. Four of the government’s biggest suppliers – G4S, Serco as well as rivals Capita and Atos – have been called to appear before a committee of British lawmakers next month for questioning about the outsourcing sector. Serco, which makes annual revenue of around 4.9 billion pounds, has continued to win deals in its other markets, such as a 335 million pound tie-up to run Dubai’s metro system, though it has encountered some problems abroad.
But back to G4S. There is even some reference to problems in the past on the G4s Welfare to Work website:
G4S Welfare to Work knows that most of the services needed to support workless people into meaningful, progressive employment in the UK already exist. What has been missing is an effective structure for managing and coordinating that provision.
… We are:
…
Operating a unique model for the delivery of welfare-to-work services that learns from mistakes made in previous Prime Contracting models, and builds on what works.
As I have described also in a previous article on this blog, one facet of globalisation is that it has become extremely difficult to regulate the behaviour of multinational corporations involved in healthcare.
G4s has now been ‘accused of “shocking” abuses and of losing control at one of South Africa’s most dangerous prisons‘. The South African government has temporarily taken over the running of Mangaung prison from G4S and launched an official investigation. It comes after inmates claimed they had been subjected to electric shocks and forced injections. G4S says it has seen no evidence of abuse by its employees. However, the BBC has obtained leaked footage filmed inside the high security prison, in which one can hear the click of electrified shields, and shrieking. It also shows a prisoner resisting a medication.
I have previously on this blog described the legal problems with the “prime contractor” model.
I have said before, and I will say it again. Especially since these contracts can be of such a long duration (for example, ten years), it is absolutely essential there are rigorous mechanisms for ongoing and continuous monitoring of performance. This way commissioners can spot easily and early on when providers are running into difficulties.
The English law gives a complex message on whether a private provider can still take the money and run, even if it doesn’t fulfill part of its side of the bargain in a contract.
Take for example the case of Sumpter v Hedges [1898] 1 QB 673 in the English Court of Appeal.
This was a matter where the plaintiff was contracted to erect certain buildings on the grounds of the defendant for a lump sum of 565 pounds, but the plaintiff was only able to do part of the work to a value of 333 pounds, with the defendant subsequently completing the rest of the work. As a result, the plaintiff sued on quantum meruit (as much as he or she has earned) appealing from the judgment of the trial judge who awarded the plaintiff for the value of the materials used, but nothing in respect to the work done.
The Court of Appeal upheld the trial judge’s decision and held that the plaintiff could not recover from the defendant in respect to the work done as part of quantum meruit due to the fact that the contract was for a lump sum, and there was no evidence that an agreement for part performance was formed.
While spinners are giving themselves multiple orgasms over ‘transparency and disclosure’ in the new Jerusalem of the NHS, it appears that “the fair playing field” of private and public health providers regarding basic patient safety is a complete fiasco.
Grahame Morris MP recently reviewed the gravity situation on the influential “Our NHS” website:
While public services are being outsourced to the private sector, especially in the NHS, Freedom of Information responsibilities are not following the public pound. Private health care companies can hide behind a cloak of commercial confidentiality when barely transparent contracts are awarded.
At the start of the bidding process private providers already receive a competitive advantage due to unequal disclosure requirements.
Private companies are free to use the Freedom of Information Act to gain detailed knowledge of a public sector provider, which can then be used to undercut or outbid the same public body when the contract is put out for tender.
NHS bodies must answer Freedom of Information requests relating to costs, performance and staffing. Yet a private provider has no similar duty of disclosure despite the fact they could have treated private patients for many years.
Once a contract is awarded, there is little that can be done if a private provider refuses to supply details to allow commissioning bodies to answer Freedom of Information requests. As they are not subject to Freedom of Information laws, the Information Commissioner has no power to investigate private contractors. They cannot serve notices for an investigation, and neither can they take enforcement action if a contractor destroys information or fails to comply with a request.
As a result of the decision in Sumpter and other similar decisions, the common law had subsequently recognised some exceptions to the general rule other than that performance of a contract must be exact and complete according to the terms. Furthermore, there is nothing preventing parties to a contractual relationship to vary or discharge the agreement, and can do so in a few ways.
One such way is “mutual discharge”, where both parties agree to release one another from what was agreed upon before either party has performed any of the acts promised. Another way is “release by one party”, where one party has completed their contractual promise, and agrees to release the other party from further performance of the contract.
Anyway, the “pass the parcel” analogy may not be entirely accurate.
It more be of the case that someone is holding a highly explosive bomb eight years into a ten year “prime contractor model” contract when it suddenly blows up.
And you can bet your bottom dollar that the Secretary of State for Health will definitely not be to blame.
Is Sir Malcolm Grant’s new idea of a short medical course a beneficial disruption or a ‘race to the bottom’?
Sir Malcolm Grant is Chair of NHS England. He helpfully presented an overview of commissioning in the NHS under ‘clinical commissioning groups’ yesterday afternoon at Olympia. Grant was until very recently the President and Provost of UCL in London, having had an accomplished career elsewhere including at Cambridge.
Grant’s talk was an optimistic vision of how commissioning might work in this new era following the Health and Social Care Act (2012). He emphasised that the roll-out of CCGs effectively was “the dog that didn’t bark”. I asked a question whether he felt disappointed that the participation of GPs wasn’t greater in CCGs. Grant said, “If I’m being honest, yes”, which was a frank reaction to the observation that CCGs may not be ‘led’ by GPs and that indeed many GPs are unwilling to participate in the CCGs.
At first, Grant’s suggestion that there could be more providers on CCGs might seem ludicrous, but, in terms of policy, might reflect a genuine concern of the providers’ viewpoint to be expressed too. In any case, there are numerous allegations of GPs having ‘conflicts of interests’ in also sitting on CCGs for the commission of services where they potentially have a direct financial interest.
Part of the raison d’être of clinical commissioning groups, and actively promoted as a ‘catalyst for change’, was that primary care physicians could ‘drive’ commissioning. The history of CCGs, however, can be delineated from two sources. One is the evolution of health maintenance organisations in the US, and the second is Pirie and Butler’s “The Health of Nations” discussion document for the Adam Smith Institute a while ago.
CCGs are functionally insurance bodies which assess risk in a given population. Grant cited that there had been great flexibility in the population sizes being served by CCGs. In insurance terms, there is nothing particularly emotional about it, however. The greater the size of population, the more accurate your assessment of risk might potentially be.
One of the most striking suggestions by Grant was that the undergraduate medical curriculum could be much ‘shorter’, reflecting how easily information could be looked up on electronic search engines at the drop of a hat. Grant correctly pointed out that most of the audience probably had the equivalent of 32GB in their hand.
By suggesting this, Grant is of course admitting that ‘knowledge is power’, a sensible thing in itself. However, the narrative that ‘all information is knowledge’ is a dangerous one, given the sheer volume of irrelevant information.
Making decisions in the real world, in business management, has been much influenced recently by the field of ‘bounded rationality’, that fundamentally we have to make quite quick decisions having paid selective attention to parts of the world around us. When you do a Google search, you can’t possibly read all of the search results.
The drive towards a ‘quick medical course’, say 2 years rather than 6 years, comes from the idea that you could get rid of time wasted in learning material available elsewhere more easily. For example, a medical student would no longer be required to show a ‘fact dump’ of the point of origin, insertion, action and nerve supply of every muscle in the body? Likewise, a medical student would no longer be required to present every chemical involved in the biochemical cascade leading from activation of a particular receptor for a drug?
There is certainly a case that an undergraduate medical student learns a lot of useless information in 5-6 years, which is not good preparation for the pre-registration junior doctor jobs in a busy hospital, when other skills such as practical procedures or time management might be more beneficial. Certainly, even in the current curriculum, a medical student might do a maximum of one month in General Practice, or one clinical lecture on dementia and delirium.
It is also, unfortunately, the case that, at many medical schools, the preclinical medical school is overloaded by overly detailed lectures by basic scientists expert in their fields (but these scientists have never seen a patient in their life.)
A ‘provider’ offering a short medical curriculum might have business ‘competitive advantage’ as a shorter curriculum is likely to be shorter and cost less. The General Medical Council will of course wish to ensure that the end-product of a short medical course is a Doctor who is safe for the public.
A short medical course could therefore be a ‘genuine disruption’ which dislodges the power of the ‘incumbents’. In other words, one simple change to the way the medical curriculum is changed to focus on skills of learning how to learn rather than sheer volume might benefit the student and public alike. Grant, correctly perhaps, feels that the emphasis should be on lifelong learning through CPD (and to extend his concept lifelong regulation through mechanisms such as ‘revalidation’).
At worst, the short medical curriculum could be interpreted as a ‘race to the bottom’, reducing the ‘barriers to entry’ in educational provider, producing Doctors at high volume and low cost. This might lead to a glut of unemployed Doctors. The needs of individual Doctors are not higher than the needs of the profession, but it is a valid presumption that the public prefers Doctors to be as highly skilled as possible.
Anyway, it is clear that Sir Malcolm Grant has not got an attitude of ‘mission accomplished’, but instead Grant seems genuinely fired up about all his challenges ahead.
Cutting the NHS cake. Who benefits from NHS competitive tenders?
In game theory and economic theory, a “zero-sum game” is a mathematical representation of a situation in which a participant’s gain (or loss) of utility is exactly balanced by the losses (or gains) of the utility of the other participant(s). If the total gains of the participants are added up, and the total losses are subtracted, they will sum to zero. Consider cutting a cake, where taking a larger piece reduces the amount of cake available for others; it is a zero-sum game if all participants value each unit of cake equally. In contrast, non–zero sum describes a situation in which the interacting parties’ aggregate gains and losses are either less than or more than zero.
As I have consistently maintained with others, although the only reason I know about this at all is due to Dr Lucy Reynolds at the London School of Health and Tropical medicine, the purpose of section 75 Health and Social Care Act (2012) was to ensnare the NHS in a free market. This market would be run according to competition rules, governed by European rules regulating ‘economic activity’, and the big corporates Circle, Virgin and Serco, for example, would have massive competitive advantage through their supplier power, economies of scale, and known expertise in procurement across a number of sectors. The National Health Service, which does not have the resources or expertise in complex procurement yet, would be at disadvantage, and unable to compete effectively.
That the market was not ideal for ‘our National Health Service’, as Prof Sir Bruce Keogh, Medical Director of the NHS, affectionally calls it has been seen in a number of recent instances. One for example is the furore with the privatisation of ‘Plasma Resources UK‘, with concerns about asset-stripping type behaviour of private equity firms for future transactions. The NHS has also not be able to implement ‘patient choice’ in complex rules about mergers, seen entirely through the competition law prism. As such Tony Blair’s dictum that ‘it doesn’t matter who’s providing my services, as long as they’re of the highest quality and I’m not paying for them’ runs into four big problems professionally.
- Firstly, if you have a carousel of different providers in your care, this is a major barrier to continuity-of-care. Continuity-of-care helps for the reason that fewer mistakes are made by clinicians, and also saves on repeating transaction costs for doing the same thing, such as medical investigations, again-and-gain (with no change in results).
- Secondly, outsourced services obtained through price competitive tendering might cost less, but profit becomes more important than value in the return on investment in services run by the private sector on the NHS’ behalf (this is why the legal profession wisely decided to abandon competitive tendering on the basis of lowest price, because of the overwhelming criticism from senior lawyers of ‘a race to the bottom’).
- Thirdly, it is a deception to the public, who feel that their services are being run by the NHS, whereas they are in fact being run by a totally alien entity in NHS uniforms.
- Fourthly, it is not an innocuous ‘zero sum game’. For every gain in the private sector, there is a loss in the NHS both in morale, sustainable business plan and resources. This matters for the future of the NHS in its ability to run a comprehensive, universal service, but this will not matter if the Secretary of State absolves responsibility for running the NHS under law, and this aspiration gets deleted in time from the NHS constitution.
The NHS Support Federation have reported that commercial companies look set to gain £1.5 billion pounds worth of NHS funding from contracts issued within the last three months. This surge in commercial activity follows the government’s new competition rules (section 75 of the Health and Social Care Act (2012), which came into force in April.) Over a hundred opportunities have been advertised according to figures compiled by the NHS Support Federation. The latest contract notice is the biggest so far, to run community services in Cambridgeshire, and is worth £800 million over 5 years. The private sector is easily winning in this competitive market, since April 2013, a sample of clinical services contracts taken from official tenders websites found that only 2 had been awarded to the NHS with 16 going to the independent sector.
The data set used for this research was taken from two procurement websites where NHS competitive tenders notices are advertised in keeping with UK practice and contract law - TED OJEU and supply2health
- NHS clinical contract Notices Apr-Jun: (source: TED OJEU);
- NHS clinical contract Awards from April 2013 (source: TED OJEU);
- Contract Notices: Supply2Health from April 2013).
NHS competitive tenders have risen steeply. Contracts awarded since April 2013 show 16 to the private sector only 2 to the NHS. An estimated £1.5 million worth of contracts have emerged in the first 3 month since the competition regulations were passed by Parliament. Outsourcing is increasing fastest in diagnostics, mental health, domicillary care and pharmacy. The largest appeared on the TED website at the end of the sample period, a contract to provide a wide range of community health services in Cambridgeshire. It is worth £800m over five years. The contract trumps the value of similar arrangements that have been made with Serco and Virgincare to run services in Suffolk (130m) and Surrey (500m). There were around twice the number of NHS competitive tenders for clinical services compared with the same quarter last year advertised on the Official Journal to the European Union – TED. Their sample is made up of 106 clinical contracts, so not those involving the pure supply of goods. Pharmacy contracts are included as a service that involves providing medical advice, but the supply of medical equipment is not. Ambulance contracts listed include those for blue light and patient transport.
It was predicted that the section 75 regulations (that passed through Parliament in April) would result in a sharp increase in the use of NHS competitive tenders as method of purchasing. The government, helped primarily by Lord Clement-Jones and Baroness Williams in the House of Lords, consistently argued that the section 75 regulations would not give primacy to the mechanism of ‘price competitive tendering’. The business problems of price competitive tendering are certainly infamous in other sectors, and, as a result of this ideological drive, outsourcing through price competitive tendering is being thrust upon the NHS (and also resisted) by the judicial system. In the NHS, there has been an increase in tendering activity in the April-June period 2013 compared to the same period last year, where a search through TED archives showed that around half the number contracts for clinical services were advertised compared to 28 contract notices (worth £1,045,668,000) in the Apr-Jun quarter a year later. There were a further 57 notices published on the supply2health website, of which the majority were competitive tenders, although in some cases the purchasing method appears not to have been finalised. There is a wide range of opportunities to run services being advertised, from a £50m group of ambulance services in Exeter, including blue light, to an advert inviting competition to provide a package of care for a single patient in Corby. The range of services is also widening. As mentioned above last year the government asked PCTs to increase competition and patient choice by extending their use of AQP for commissioning. A list of thirty nine treatments and types of care was produced.
There is growing list of care types that are being commissioned through NHS competitive tenders. These contain some of the largest contracts and have attracted interest from large companies like Virgin and Serco. In Devon Virgin recently began a contract to run children’s health services after a legal challenge failed to prevent the contract going forward.Despite well publicised problems with outsourced contracts for GP out of hours in several areas involving Harmoni and Serco, five further contracts have been advertised in five new areas (East Midlands, Hackney, North East, Surrey and Sussex, Sutton). Our local City & Hackney doctors have worked for two years to put together a new not-for-profit social enterprise (City& Hackney Urgent Healthcare Social Enterprise – CHUHSE) , which involves City and Hackney doctors varying their contract in order to provide an Out of Hours service. In February 2013, a GP-led social enterprise in Hackney lost its bid to take responsibility for out-of-hours care from private provider Harmoni, when the company’s contract expires on March 31. The service to be run by GPs had been intended to be be non-profit – i.e. local doctors are prepared to give up their evenings and weekends to ensure local people get the quality and continuity of service they need. However, Harmoni did not perform well elsewhere. In May 2013, it was reported that Care Quality Commission inspectors have found private company Harmoni in offence of running the out-of-hours (OOH) GP service for Hackney with so few doctors they are potentially placing patient’s safety at risk. The Care Quality Commission (CQC) had previously been reviewing staffing levels at Harmoni North Central London.The company admitted there had been no doctors based at Homerton Hospital on the evening of Easter Sunday, despite being contracted to provide a service when GP practices are closed. The CQC report has been published and concluded “there were not enough qualified, skilled and experienced staff to meet people’s needs”.
The way in which Labour had opened up the service, and brought in the “Tony Blair Dictum” is well known. The problem now is that there is an active competitive market, where there is no overall direction. Clinical Commissioning Groups are not GP-led in the majority, but followers of English policy know they were never intended to be. They were simply intended as state insurance schemes in the seminal ‘The Health of the Nations’ from the Adam Smith Institute. Recently, the following observations were made on May 19 2013:
“As only 22% of CCGs have a GP as accountable officer, there are those who believe that CCGs are simply management run organisations supported by a few enthusiastic GPs – PCTs in all but name.
Many of those working in CCGs would refute the suggestion, pointing to the fact that they are a membership organisation, and that the GPs are not supporters but the real engine of the CCG.
According to Wikipedia, ‘CCGs are clinically led groups that include all the GPs in their geographical area. The aim of this is to give GPs and other clinicians the power to influence commissioning decisions for their patients’. But are CCGs really clinically led?
The number of management directors varies according to the size of the CCG. Most (over three quarters) have a manager as Accountable Officer, and all have a Chief Financial Officer. Larger CCGs may also have a management director for quality, for strategy or commissioning, even for contracting. Where there is a director there is generally a management team, and so the risk is that much of the organisation can start to operate outside of the GPs’ control.”
Therefore, there is a good arguable case that “cutting up the NHS cake”, as first introduced by Thatcher and Major through its locking-in of PFI deals aka marketisation approach, regretfully advanced by Labour through continuation of the PFI approach and an addition of ‘independent sector treatment centres’ for good measure, and the Coalition’s continuation through advancing outsourcing with a view to final privatisation, does not necessarily benefit the patient. To provide balance, Andy Burnham has promised to repeal the Health and Social Care Act (2013), drive the competition arrangements into “reverse gear” in Part 3, and to introduce the ‘NHS preferred provider’. The patient ultimately cannot be ethically called a ‘consumer’ as it is a rigged market, and half of the relevant information, at least, is not available. It is clearly not a ‘fair playing field’ as private healthcare providers are able to make profits for shareholders, do not contribute to the training of junior doctors or nurses in the NHS, are immune from judicial review, and are immune from freedom of information requests. “Cutting up the NHS cake” was an unnecessary shot in the foot in English health policy. But if it means that the result is that private providers ‘cherrypicks’ the most profitable services, leaving the NHS with the most expensive and clinically challenging cases, this could see the whole leg requiring amputation. Otherwise, the NHS will die of septic shock, through a toxic combination of the policies of the Conservative, Labour and Liberal Democrat Parties in the House of Commons and House of Lords over time.
In this new neoliberal NHS, are the key actors going to start eating each other?
CCGs are technically “state-owned insurance schemes”, as this answer from Dr Lucy Reynolds to Jill Mountford explains:
JILL MOUNTFORD: You made reference to CCGs and how they come into play from 1 April. Can you tell us a little bit about the size of the budget that they’re going to be holding, the power, the massive power shift that’s going to take place and what this means?
LUCY REYNOLDS: The health service is being restructured on to an insurance compatible footing, and the CCGs are technically state-owned insurance schemes. So they are going to be taking on around 80% of the NHS budget and they are going to be parcelling it out to providers. They have been told that they are going to have a lot of autonomy in that and that they will be able to represent the interests of their patients in the matter.
That bit doesn’t appear to be able to be delivered when we have these regulations in place because what the regulations say is that commissioners will put out contracts according to competition law, and they will decide according to competition law. If anybody that didn’t get the contract feels that they don’t like the decision and that it could be faulted on failure to comply with competition law, they are permitted to complain to the sector regulator, Monitor, which is required to enforce competition law. So once everything gets put through the market, the CCGs won’t actually have any autonomy in the matter.
And the reason we have been told about GP empowerment and patient empowerment is firstly to lure the doctors into complying with this. They are belatedly starting to understand that this has been a trick.
The second reason GPs have been told that in CCGs they would have the chance to advance the interests of patients is because it’s very important for our politicians that nobody blames them. The public has been induced to believe that the GPs are taking over and will be in control so in five years when the whole thing is complete chaos and you can’t get decent care, it won’t be the politicians’ fault.
In a sense, funding of the NHS is already working backwards. Most people concede a need for there to be tight fiscal management of the NHS budget especially if ‘austerity’ is going to last longer for the wider economy for longer than expected. ‘Efficiency savings’ are being implemented against a cost of never-decreasing demand on the NHS, and demands such as increased costs of goods and services needed to run it and changing demographics of the patient population. Therefore, given this backdrop, it is perfectly feasible in a neoliberal approach to the NHS whether CCGs could ‘compete’ for patients. It could be tenuously argued by health policy wonks that such competition could ‘drive up’ quality, although evidence for competition driving up quality in the rest of English healthcare policy can only be described as extremely flaky.
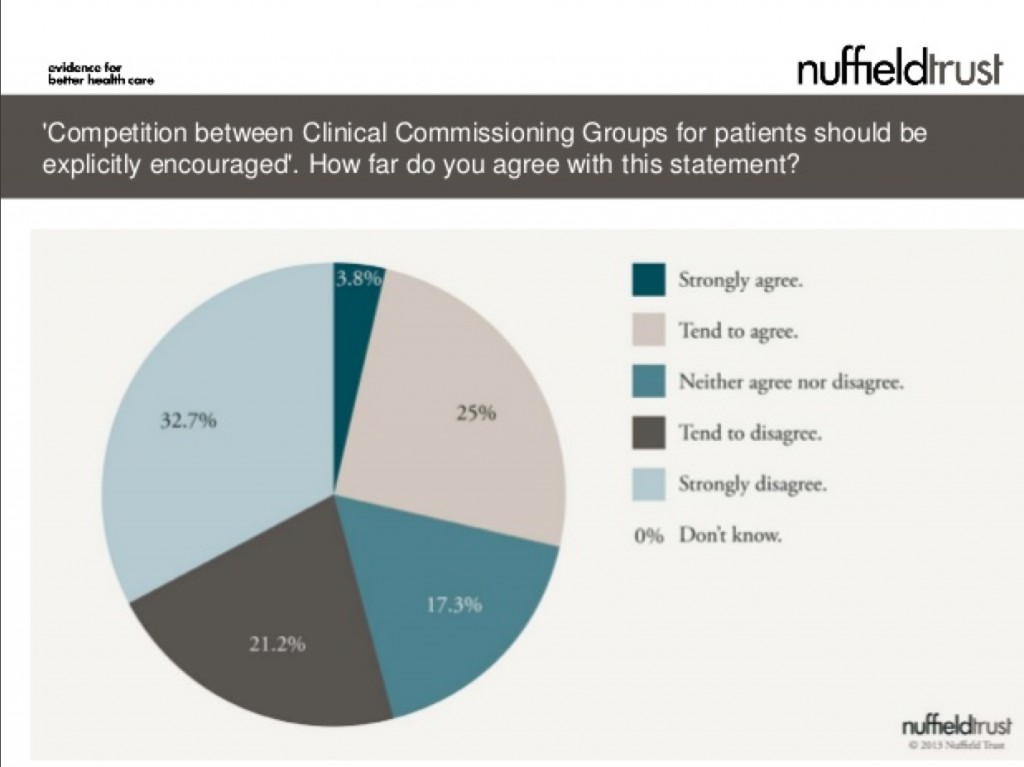
This is a very interesting observation from the recently published survey from the Nuffield Trust (see slide 14 in this slideshow here):
The results in summary are:
53.8% tending to disagree or strongly disagreeing
17.3% neither disagreeing or agreeing
28.8% tending to agree or strongly agreeing
Therefore because of the “don’t knows”, the results are actually quite confusing.
It appears that the idea of CCGs “competing against each other” has not gone totally unnoticed. This is an intriguing post dated March 16 2013, entitled “Are CCGs in Competition with Each Other?“:
“The history of Clinical Commissioning Groups (CCGs), short as it is, has conspired to set CCGs up in competition with each other. At a time when many are already predicting the demise of CCGs, it is critical that CCGs work together to be successful.
So how has this situation come about? The primary reason is the authorisation process. This created a competition between CCGs (‘What wave were you in?’, ’How many conditions do you have?’ etc etc), that is neither helpful now, nor conducive to future success.
This competitiveness stems from the origins of CCGs as self-selected groupings of GP practices. These groupings often set up around historic alliances and rivalries. Once practices made a choice as to where their allegiances should lie, they naturally wanted to validate this decision making by demonstrating that ‘their’ CCG was better than the CCG they had chosen not to join. This has meant that the biggest barriers to joint working exist between neighbouring CCGs with whom the strongest alliances are most important.
Some CCGs have already had to deal with some of these turf wars as different groups have had to come together to form a larger whole. Making this work internally has taken such effort that building relationships with other CCGs has understandably taken a back seat.
The limited management allowance, and the fact that many GPs are carrying out the commissioning role in 1, 2 0r 3 days per week, mean that the capacity for collaborative working between CCGs has not existed, even when the desire to do so does. Completing the collaborative agreement template that exists for CCGs remains on the to do list of most CCGs, rather than the tasks completed list.
The time has now come to draw a line under the past and put an end to any competition. It is incomprehensible that at this stage any one CCG has all the answers. It is critical that CCGs learn from each other, because ultimately we will succeed or fail as a collective.
CCGs are totally new organisations. There are sets of issues that CCGs are dealing with that predecessor organisations such as PCTs never had to, such as creating effective governance as a membership organisation of GP practices, developing meaningful and sustainable practice engagement, managing the NHS Commissioning Board, and making commissioning support effective.
So what can we do to learn from each other? How can we recognise the constraints that we all operate under, and yet create the capacity to learn from and support each other?
The starting point is for CCGs, individually and collectively, to commit to doing this. It is critical we are active in this, and do not leave it to others (in particular the NHS Commissioning Board) to arrange on our behalf. We must decide for ourselves what good is, and find ways of sharing and learning that are effective for us.
This website is one opportunity for sharing between CCGs. One of the most common requests we receive is for case studies on how individual CCGs have successfully met some of the challenges they face. So here are three things that you personally can do to help the development of collaboration between CCGs:
- Request information and advice from other CCGs. Use this site to pose questions that you want the answers to.
- If you or your CCG has a case study of success in any of the categories in the sidebar of this site, send them to us and we will gladly publish them to make them accessible to others. We have had specific requests for examples of how CCGs have created strong practice engagement, and of where CCGs have developed effective primary care strategies, so if you have examples particularly in either of these areas we would be more than happy to publish them.
- Finally, tell other people who work in CCGs about this site. The more we share and learn together, the stronger we will be!”
In this new neoliberal NHS, are the key actors going to start eating each other? These are exciting times.
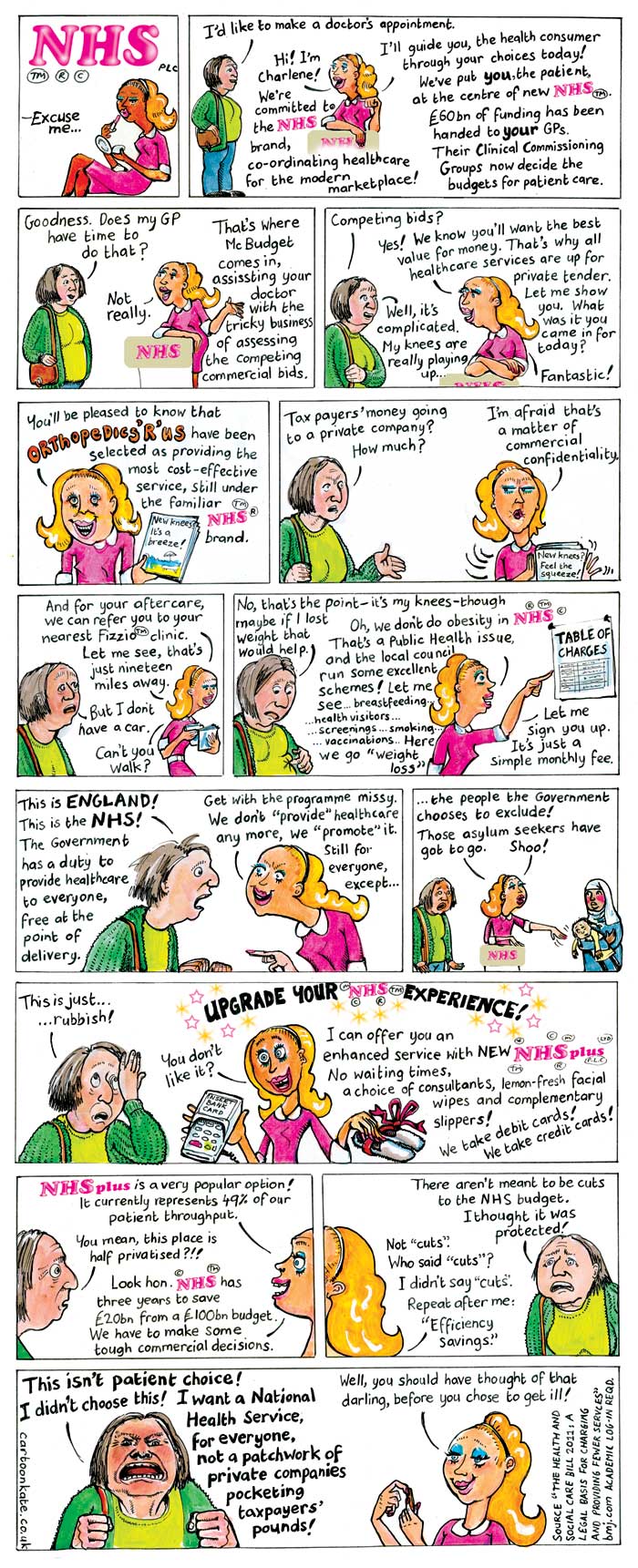
Thank you to “Cartoon Kate” for her brilliant cartoon about the NHS privatisation
Thank you to “Cartoon Kate” for her brilliant cartoon about the privatisation of the NHS. We spoke just now, and she’s given me permission very kindly to share this cartoon with you.
The original link to the cartoon is http://www.cartoonkate.co.uk/nhs-plc/.
This cartoon is really a Godsend for those of us who feel we’ve failed in getting our message across to the wider general public about why this satisfies the standard international and domestic published definitions of “privatisation”.
Kate is a very pleasant person, and I strongly encourage you to support her work here. She can be emailed using her ‘Contact us’ page, and can be reached easily on her phone number here.
Slide presentation version shared this afternoon:
There should be a senior public health physician on the NHS Commissioning Board
The current NHS Commissioning Board include Sir David Nicholson, who has apologised for the deaths numbering in the region of 400-1200 at Mid Staffs and who is alleged to have been warned by NHS whistleblower about serious patient safety issues, and Dame Barbara Hakin, “..who was then head of the East Midlands strategic health authority and is now national director for commissioning development at the NHS Commissioning Board, ordered him to meet the national targets regardless of demand.” The General Medical Council has launched an investigation into a complaint against national director for commissioning development Dame Barbara Hakin, according to the HSJ.
The UK Faculty of Public Health (FPH), part of the Royal Colleges of Physicians (London college), is the standard setting body and the leading professional body for public health specialists in the UK. It aims to advance the health of the population through three key areas of work: health promotion, health protection and healthcare improvement. In addition to maintaining professional and educational standards for specialists in public health, FPH advocates on key public health issues and provides practical information and guidance for public health professionals. The Faculty of Public Health, of the Royal College of Physicians, responded to a consultation on the document “Liberating the NHS: commissioning for patients”.
In their response, the Faculty of Public Health set out a very clear case of how public health professionals could and show be involved in commissioning, for example:
“Specialist commissioning should be integrated with the work of GP consortia by the establishment of national subgroups for the relevant specialities of the NHS Commissioning Board. The relevant National Clinical Directors should sit on these groups, and the groups should provide guidance for consortia. GP consortia should have leads for specialised commissioning who link up with the relevant clinical subgroups. These leads would meet regionally/subnationally and would engage with secondary care colleagues and public health specialists. Specialist public health and commissioning advice would also be essential to ensure that specialised commissioning is responsive to local need, is prioritised appropriately and takes into account the primary prevention aspects of the clinical conditions for which it is responsible; and to ensure that commissioning plans integrate prevention, primary and secondary healthcare and social care. Resource allocation decisions should be scrutinised to ensure that they are consistent with priorities for health and wellbeing. Specialist public health advice will ensure that only cost and clinically effective interventions are commissioned and that appropriate account is taken of overall population health.”
Indeed, in November 2012, the NHS Commissioning Board (NHS CB) and the Department of Health published their detailed agreement showing how the NHS CB will drive improvements in the health of England’s population through its commissioning of certain public health services. The agreement sets out the outcomes to be achieved in exercising these public health functions and provides ring fenced funding for the NHS CB to commission public health services. The services commissioned as part of this agreement are those where there is, for example, alignment with national clinical pathways and added value of central commissioning. Please refer to this document which details how public health functions to be exercised by the NHS Commissioning Board.
Whether you think the burden of opinion should be on the balance of probabilities or beyond reasonable doubt, there is a strong arguable case that there should be a Director of Public Health on the NHS CB. However, bodies which might have protected against problems in national health policy, such as the Food Standards Agency, the Health Protection Agency, and the National Patient Safety Agency, are all being abolished. Also, the fate of the NHS Commissioning Board itself after 2015, a body which has been called “the biggest QUANGO ever“, is uncertain.
Competition Regulations issued under Section 75 of the Health and Social Care Act (2012) will lock CCGs into arranging all purchasing through competitive markets
Prior to this reorganisation costing billions, the NHS had been one of the most cost-effective health systems in the developed world, according to a study published in the Journal of the Royal Society of Medicine. Public satisfaction with the NHS reached record levels in March 2011; writing on the BMJ website, Prof. John Appleby said 64% of people were either “very” or “quite” satisfied with the NHS. Now, very shortly, the Regulations which will govern the actual operation of the new NHS market will be passed under Section 75 of Health and Social Care Act [2012], in particular s. 75 (3a):
‘Work in progress’ : Andy Burnham’s 2012 conference speech throws up tough challenges
Andy Burnham has vowed to reverse the “rapid” privatisation of NHS hospitals in England if Labour wins power. In particular, Mr Burnham said he feared the new freedom for hospitals to earn 49% of their income from private work would “damage the character and culture” of the NHS and take it closer to an American model.
The issue of fragmentation of the NHS is a genuine problem in the NHS, as enacted this year. This is manifest in a number of different guises, such as lack of clarity as to which private entity owns what for local services, the abolition of statutory bodies involved in healthcare (such as the National Patient Safety Agency and the Health Protection Agency), and the phenomenon of “postcode lottery” in healthcare provision.
Andy Burnham clearly wishes “Labour values” of collaboration and solidarity to be pervasive in an equitable National Health Service, rather than competition, where there are winners and losers. This is particularly interesting from a business management sense, as it has long been a source of academic interest in innovation management how the “innovators’ dilemma” is solved in the private sector. This is the practical business question posed by Prof Clay Christensen, professorial fellow in innovation at Harvard, as to how it is possible, that, amongst private entities in the market place, business entities can secure competitive advantage, while working together sharing knowledge in seamless collaboration.
It seems pretty likely that, even if Labour win the 2015 general election and the Health and Social Act (2012) is repealed, commissioning will exist in some form, with Labour taking forward ‘best practice’ from the experiences of clinical commissioning groups (CCGs). There is no inkling that, whilst certain structures are in the process of being abolished for some time (such as the PCTs and SHAs), the CCGS and NHS Foundation Trusts will follow suit. Indeed, Professor Brian Edwards, special adviser to the Institute of Healthcare Managers, said he was “appalled and frustrated” at news the Francis Report would not be published until January 2013, and called it “a cruel blow” to the families of victims. This report discusses the failings at hospitals in Mid Staffordshire between 2005 and 2009, and is anticipated to be invaluable in developing further NHS foundation trusts.
Integration in person-centred care has always been a hallmark of excellent medical care, and Burnham keens to bring this out as a dominant theme in components of his new Health Bill in 2015 or 2016 if elected. When patients present to their G.P., they simply do not present as isolated medical diagnoses. For example, if an elderly patient, who may incidentally have a probable diagnosis of dementia, falls, a GP would be concerned with the patient is at risk of a fracture due to underlying osteoporosis, has poor eyesight due to a cataract for example, or leads a life in a cluttered home environment due to lack of social care. There are a plethora of problems which are likely to cause an individual to come into contact with the NHS, and the integration of health and social care is indeed entirely in keeping with Nye Bevan’s original aspiration for the NHS. The ideal would be of course to have an integrated health and social care service, but much time (and money) has been lost by the Coalition kicking the Dilnot review ‘into the long grass’ when we were already supposedly meant to be looking for greater efficiencies through the Nicholson Challenge.
Moves are clearly afoot as to who is providing the services, with various morphologies in terminology (for example “NHS preferred provider”, “any willing provider”, or “any qualified provider”). Closer to home for the current delegates in Manchester, patients will be taken to hospital by a bus company after the North West Ambulance Service (NWAS) failed to win a contract. It will not affect 999 emergency call-outs. Arriva, which run bus services throughout Greater Manchester, will replace NWAS which currently runs the service but was outbid by Arriva after the the service was put out to tender.
Chris Ham, Chief Executive of the Kings Fund, has concerns which are perfectly fair, in response:
“Andy Burnham has outlined a vision for the future of health and social care which accentuates the differences between the Labour Party and the government on the NHS. He is right to stress the need for fundamental change in health and social care services. Our own work has made the case for radical changes to ensure the NHS is fit to meet the challenges of the future as the population ages and health needs change.
This includes moving care closer to people’s homes and re-thinking the role of hospitals which must change to improve the quality of specialist services and better meet the needs of older patients. We also welcome his emphasis on delivering integrated care – the challenge now is to move integrated care from the policy arena and make it happen across the country at scale and pace.
However, while the long term vision is ambitious, the details of Labour’s plans are sketchy. A number of questions will need to be answered in the policy review announced today. For example, it is not clear how local authorities could take on the role of commissioning health care without further structural upheaval. And despite the Shadow Chancellor’s pledge earlier in the week, it is not clear how Labour would ensure adequate funding for social care.”
Text of speech given this morning in Manchester.
Conference, my thanks to everyone who has spoken so passionately today and I take note of the composite.
A year ago, I asked for your help.
To join the fight to defend the NHS – the ultimate symbol of Ed’s One Nation Britain.
You couldn’t have done more.
You helped me mount a Drop the Bill campaign that shook this Coalition to its core.
Dave’s NHS Break-Up Bill was dead in the water until Nick gave it the kiss of life.
NHS privatisation – courtesy of the Lib Dems. Don’t ever let them forget that.
We didn’t win, but all was not lost.
We reminded people of the strength there still is in this Labour movement of ours when we fight as one, unions and Party together, for the things we hold in common.
We stood up for thousands of NHS staff like those with us today who saw Labour defending the values to which they have devoted their working lives.
And we spoke for the country – for patients and people everywhere who truly value the health service Labour created and don’t want to see it broken down.
Conference, our job now is to give them hope.
To put Labour at the heart of a new coalition for the NHS.
To set out a Labour alternative to Cameron’s market.
To make the next election a choice between two futures for our NHS.
They inherited from us a self-confident and successful NHS.
In just two years, they have reduced it to a service demoralised, destabilised, fearful of the future.
The N in NHS under sustained attack.
A postcode lottery running riot – older people denied cataract and hip operations.
NHS privatisation at a pace and scale never seen before.
Be warned – Cameron’s Great NHS Carve-Up is coming to your community.
As we speak, contracts are being signed in the single biggest act of privatisation the NHS has ever seen.
398 NHS community services all over England – worth over a quarter of a billion pounds – out to open tender.
At least 37 private bidders – and yes, friends of Dave amongst the winners.
Not the choice of GPs, who we were told would be in control.
But a forced privatisation ordered from the top.
And a secret privatisation – details hidden under “commercial confidentiality” – but exposed today in Labour’s NHS Check.
Our country’s most-valued institution broken up, sold off, sold out – all under a news black-out.
It’s not just community services.
From this week, hospitals can earn up to half their income from treating private patients. Already, plans emerging for a massive expansion in private work, meaning longer waits for NHS patients.
And here in Greater Manchester – Arriva, a private bus company, now in charge of your ambulances.
When you said three letters would be your priority, Mr Cameron, people didn’t realise you meant a business priority for your friends.
Conference, I now have a huge responsibility to you all to challenge it.
Every single month until the Election, Jamie Reed will use NHS Check to expose the reality.
I know you want us to hit them even harder – and we will.
But, Conference, I have to tell you this: it’s hard to be a Shadow when you’re up against the Invisible Man.
Hunt Jeremy – the search is on for the missing Health Secretary.
A month in the job but not a word about thousands of nursing jobs lost.
Not one word about crude rationing, older people left without essential treatment.
Not a word about moves in the South West to break national pay.
Jeremy Hunt might be happy hiding behind trees while the front-line of the NHS takes a battering.
But, Conference, for as long as I do this job, I will support front-line staff and defend national pay in the NHS to the hilt.
Lightweight Jeremy might look harmless. But don’t be conned.
This is the man who said the NHS should be replaced with an insurance system.
The man who loves the NHS so much he tried to remove the tribute to it from the Opening Ceremony of the Olympic Games.
Can you imagine the conversation with Danny Boyle?
“Danny, if you really must spell NHS with the beds, at least can we have a Virgin Health logo on the uniforms?”
Never before has the NHS been lumbered with a Secretary of State with so little belief in it.
It’s almost enough to say “come back Lansley.”
But no. He’s guilty too.
Lansley smashed it up for Hunt to sell it off with a smile.
But let me say this to you, Mr Hunt. If you promise to stop privatising the NHS, I promise never to mispronounce your name.
So, Conference, we’re the NHS’s best hope. Its only hope.
It’s counting on us.
We can’t let it down.
So let’s defend it on the ground in every community in England.
Andrew Gwynne is building an NHS Pledge with our councillors so, come May, our message will be: Labour councils, last line of defence for your NHS.
But we need to do more.
People across the political spectrum oppose NHS privatisation.
We need to reach out to them, build a new coalition for the NHS.
I want Labour at its heart, but that means saying more about what we would do.
We know working in the NHS is hard right now, when everything you care about is being pulled down around you.
I want all the staff to know you have the thanks of this Conference for what you do.
But thanks are not enough. You need hope.
To all patients and staff worried about the future, hear me today: the next Labour Government will repeal Cameron’s Act.
We will stop the sell-off, put patients before profits, restore the N in NHS.
Conference, put it on every leaflet you write. Mention it on every doorstep.
Make the next election a referendum on Cameron’s NHS betrayal.
On the man who cynically posed as a friend of the NHS to rebrand the Tories but who has sold it down the river.
In 2015, a vote for Labour will be a vote for the NHS.
Labour – the best hope of the NHS. Its only hope.
And we can save it without another structural re-organisation.
I’ve never had any objection to involving doctors in commissioning. It’s the creation of a full-blown market I can’t accept.
So I don’t need new organisations. I will simply ask those I inherit to work differently.
Not hospital against hospital or doctor against doctor.
But working together, putting patients before profits.
For that to happen, I must repeal Cameron’s market and restore the legal basis of a national, democratically-accountable, collaborative health service.
But that’s just the start.
Now I need your help to build a Labour vision for 21st century health and care, reflecting on our time in Government.
We left an NHS with the lowest-ever waiting lists, highest-ever patient satisfaction.
Conference, always take pride in that.
But where we got it wrong, let’s say so.
So while we rebuilt the crumbling, damp hospitals we inherited, providing world-class facilities for patients and staff, some PFI deals were poor value for money.
At times, care of older people simply wasn’t good enough. So we owe it to the people of Stafford to reflect carefully on the Francis report into the failure at Mid-Staffordshire Foundation NHS Trust.
And while we brought waiting lists down to record lows, with the help of the private sector, at times we let the market in too far.
Some tell me markets are the only way forward.
My answer is simple: markets deliver fragmentation; the future demands integration.
As we get older, our needs become a mix of the social, mental and physical.
But, today, we meet them through three separate, fragmented systems.
In this century of the ageing society, that won’t do.
Older people failed, struggling at home, falling between the gaps.
Families never getting the peace of mind they are looking for, being passed from pillar to post, facing an ever-increasing number of providers.
Too many older people suffering in hospital, disorientated and dehydrated.
When I shadowed a nurse at the Royal Derby, I asked her why this happens.
Her answer made an impression.
It’s not that modern nurses are callous, she said. Far from it. It’s simply that frail people in their 80s and 90s are in hospitals in ever greater numbers and the NHS front-line, designed for a different age, is in danger of being overwhelmed.
Our hospitals are simply not geared to meet people’s social or mental care needs.
They can take too much of a production-line approach, seeing the isolated problem – the stroke, the broken hip – but not the whole person behind it.
And the sadness is they are paid by how many older people they admit, not by how many they keep out.
If we don’t change that, we won’t deliver the care people need in an era when there’s less money around.
It’s not about new money.
We can get better results for people if we think of one budget, one system caring for the whole person – with councils and the NHS working closely together.
All options must be considered – including full integration of health and social care.
We don’t have all the answers. But we have the ambition. So help us build that alternative as Liz Kendall leads our health service policy review.
It means ending the care lottery and setting a clear a national entitlement to what physical, mental and social care we can afford – so people can see what’s free and what must be paid for.
It means councils developing a more ambitious vision for local people’s health: matching housing with health and care need; getting people active, less dependent on care services, by linking health with leisure and libraries; prioritising cycling and walking.
A 21st century public health policy that Diane Abbott will lead.
If we are prepared to accept changes to our hospitals, more care could be provided in the home for free for those with the greatest needs and for those reaching the end of their lives.
To the district general hospitals that are struggling, I don’t say close or privatise.
I say let’s help you develop into different organisations – moving into the community and the home meeting physical, social and mental needs.
Whole-person care – the best route to an NHS with mental health at its heart, not relegated to the fringes, but ready to help people deal with the pressure of modern living.
Imagine what a step forward this could be.
Carers today at their wits end with worry, battling the system, in future able to rely on one point of contact to look after all of their loved-one’s needs.
The older person with advanced dementia supported by one team at home, not lost on a hospital ward.
The devoted people who look after our grans and grand-dads, mums and dads, brothers and sisters – today exploited in a cut-price, minimum wage business – held in the same regard as NHS staff.
And, if we can find a better solution to paying for care, one day we might be able to replace the cruel ‘dementia taxes’ we have at the moment and build a system meeting all of a person’s needs – mental, physical, social – rooted in NHS values.
In the century of the ageing society, just imagine what a step forward that could be.
Families with peace of mind, able to work and balance the pressures of caring – the best way to help people work longer and support a productive economy in the 21st century.
True human progress of the kind only this Party can deliver.
So, in this century, let’s be as bold as Bevan was in the last.
Conference, the NHS is at a fork in the road.
Two directions: integration or fragmentation.
We have chosen our path.
Not Cameron’s fast-track to fragmentation.
But whole-person care.
A One Nation system built on NHS values, putting people before profits.
A Labour vision to give people the hope they need, to unite a new coalition for the NHS.
The NHS desperately needs a Labour win in 2015.
You, me, we are its best hope. It’s only real hope.
It won’t last another term of Cameron.
NHS.
Three letters. Not Here Soon.
The man who promised to protect it is privatising it.
The man who cut the NHS not the deficit.
Cameron. NHS Conman.
Now more than ever, it needs folk with the faith to fight for it.
You’re its best hope. It’s only hope.
You’ve kept the faith.
Now fight for it – and we will win.