CCGs are technically “state-owned insurance schemes”, as this answer from Dr Lucy Reynolds to Jill Mountford explains:
JILL MOUNTFORD: You made reference to CCGs and how they come into play from 1 April. Can you tell us a little bit about the size of the budget that they’re going to be holding, the power, the massive power shift that’s going to take place and what this means?
LUCY REYNOLDS: The health service is being restructured on to an insurance compatible footing, and the CCGs are technically state-owned insurance schemes. So they are going to be taking on around 80% of the NHS budget and they are going to be parcelling it out to providers. They have been told that they are going to have a lot of autonomy in that and that they will be able to represent the interests of their patients in the matter.
That bit doesn’t appear to be able to be delivered when we have these regulations in place because what the regulations say is that commissioners will put out contracts according to competition law, and they will decide according to competition law. If anybody that didn’t get the contract feels that they don’t like the decision and that it could be faulted on failure to comply with competition law, they are permitted to complain to the sector regulator, Monitor, which is required to enforce competition law. So once everything gets put through the market, the CCGs won’t actually have any autonomy in the matter.
And the reason we have been told about GP empowerment and patient empowerment is firstly to lure the doctors into complying with this. They are belatedly starting to understand that this has been a trick.
The second reason GPs have been told that in CCGs they would have the chance to advance the interests of patients is because it’s very important for our politicians that nobody blames them. The public has been induced to believe that the GPs are taking over and will be in control so in five years when the whole thing is complete chaos and you can’t get decent care, it won’t be the politicians’ fault.
In a sense, funding of the NHS is already working backwards. Most people concede a need for there to be tight fiscal management of the NHS budget especially if ‘austerity’ is going to last longer for the wider economy for longer than expected. ‘Efficiency savings’ are being implemented against a cost of never-decreasing demand on the NHS, and demands such as increased costs of goods and services needed to run it and changing demographics of the patient population. Therefore, given this backdrop, it is perfectly feasible in a neoliberal approach to the NHS whether CCGs could ‘compete’ for patients. It could be tenuously argued by health policy wonks that such competition could ‘drive up’ quality, although evidence for competition driving up quality in the rest of English healthcare policy can only be described as extremely flaky.
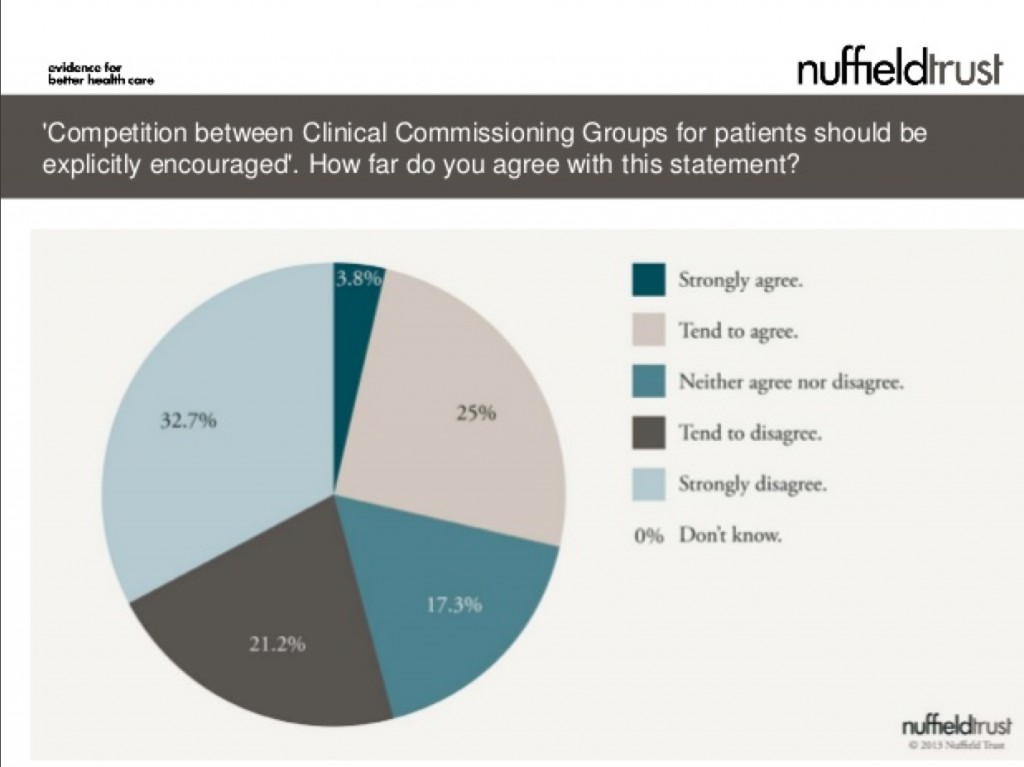
This is a very interesting observation from the recently published survey from the Nuffield Trust (see slide 14 in this slideshow here):
The results in summary are:
53.8% tending to disagree or strongly disagreeing
17.3% neither disagreeing or agreeing
28.8% tending to agree or strongly agreeing
Therefore because of the “don’t knows”, the results are actually quite confusing.
It appears that the idea of CCGs “competing against each other” has not gone totally unnoticed. This is an intriguing post dated March 16 2013, entitled “Are CCGs in Competition with Each Other?“:
“The history of Clinical Commissioning Groups (CCGs), short as it is, has conspired to set CCGs up in competition with each other. At a time when many are already predicting the demise of CCGs, it is critical that CCGs work together to be successful.
So how has this situation come about? The primary reason is the authorisation process. This created a competition between CCGs (‘What wave were you in?’, ’How many conditions do you have?’ etc etc), that is neither helpful now, nor conducive to future success.
This competitiveness stems from the origins of CCGs as self-selected groupings of GP practices. These groupings often set up around historic alliances and rivalries. Once practices made a choice as to where their allegiances should lie, they naturally wanted to validate this decision making by demonstrating that ‘their’ CCG was better than the CCG they had chosen not to join. This has meant that the biggest barriers to joint working exist between neighbouring CCGs with whom the strongest alliances are most important.
Some CCGs have already had to deal with some of these turf wars as different groups have had to come together to form a larger whole. Making this work internally has taken such effort that building relationships with other CCGs has understandably taken a back seat.
The limited management allowance, and the fact that many GPs are carrying out the commissioning role in 1, 2 0r 3 days per week, mean that the capacity for collaborative working between CCGs has not existed, even when the desire to do so does. Completing the collaborative agreement template that exists for CCGs remains on the to do list of most CCGs, rather than the tasks completed list.
The time has now come to draw a line under the past and put an end to any competition. It is incomprehensible that at this stage any one CCG has all the answers. It is critical that CCGs learn from each other, because ultimately we will succeed or fail as a collective.
CCGs are totally new organisations. There are sets of issues that CCGs are dealing with that predecessor organisations such as PCTs never had to, such as creating effective governance as a membership organisation of GP practices, developing meaningful and sustainable practice engagement, managing the NHS Commissioning Board, and making commissioning support effective.
So what can we do to learn from each other? How can we recognise the constraints that we all operate under, and yet create the capacity to learn from and support each other?
The starting point is for CCGs, individually and collectively, to commit to doing this. It is critical we are active in this, and do not leave it to others (in particular the NHS Commissioning Board) to arrange on our behalf. We must decide for ourselves what good is, and find ways of sharing and learning that are effective for us.
This website is one opportunity for sharing between CCGs. One of the most common requests we receive is for case studies on how individual CCGs have successfully met some of the challenges they face. So here are three things that you personally can do to help the development of collaboration between CCGs:
- Request information and advice from other CCGs. Use this site to pose questions that you want the answers to.
- If you or your CCG has a case study of success in any of the categories in the sidebar of this site, send them to us and we will gladly publish them to make them accessible to others. We have had specific requests for examples of how CCGs have created strong practice engagement, and of where CCGs have developed effective primary care strategies, so if you have examples particularly in either of these areas we would be more than happy to publish them.
- Finally, tell other people who work in CCGs about this site. The more we share and learn together, the stronger we will be!”
In this new neoliberal NHS, are the key actors going to start eating each other? These are exciting times.