Home » Doctors
My medical career finished along ago, but the GMC FTP procedures for ill doctors are still far too dangerous

One of the ways that the General Medical Council will try to pin you down is if you appear blasé in any sense about your own behaviour, or lack insight into its repercussions.
I have a psychiatrist in West London who oversees my recovery. I am a barn door alcoholic now in recovery. One of the wisest things he has ever said to me is that it is impossible to ignore the distress I caused to friends, family and others. I think about this every day of my life in fact. It has left an indelible trace on Google, which I do not wish to forget. That’s why I have never asked for it to be removed.
I get upset that the BBC considers my tragic case of erasure from the Medical Register as ‘entertainment’. Behind this titillating story was someone who was in massive distress, and to some extent continues to be in distress.
I have learnt the General Medical Council (GMC) is only doing its job. Reports, like the latest damning one by Civitas on how the GMC treats sick doctors badly, come and go. And nothing really changes.
But I remember all too well what happened to me. I repeat that I find my behaviour then, as a different person, disgusting and unacceptable. But things came to a head when I was blue-lighted in at the beginning of June 2007 with an asystolic cardiac arrest which I was very lucky to be resuscitated out of. I then spent six weeks in a coma. I was fighting for my life, with drips, a central line, and the full army of Intensive Care machinery. The Consultant at the Royal Free warned people I was not expected to leave the hospital. I was clearly a very sick man.
My late father came to visit every day when I was learning how to walk and talk again at the National Hospital for Neurology and Neurosurgery. That’s where I had spent six happy months, while healthy, learning about general neurology and dementia. It’s where I developed a lifelong interest in neurodegenerative disease, which pervades through my post-doctoral fellowship at the Institute of Neurology thereafter, my mention in the Oxford Textbook of Medicine, and my own book on wellbeing in dementia.
I am happy now that, having learnt how to walk and talk, I was invited to the Alzheimer’s Association International Conference in Copenhagen last month, and I went to the Alzheimer’s Show in Manchester and London this year. My friends include people living with dementia, and they tell me what’s important in policy now.
I remember though the days of having to hide my name on blogposts or my Twitter account. I remember how I was frightened to show myself in public in the last few years. I remember how my circle of friends completely collapsed, though I am happy with the very small number of very close friends I have now. I still continue to get trolled, like no tomorrow, with words like “Disgusting” and “How do you live with yourself?”
I do also remember how the General Medical Council took years with their investigations. I remember the torrent of newspaper articles explaining how likely it would be I would be struck off. I remember thinking how this was an inglorious end to my ten years training to be a Doctor, a profession which I still feel honoured to have been in once.
But the General Medical Council protracts out their investigations. The GMC never got round to appointing a clinical supervisor (very odd) even though my independent clinical examiners had concluded that I had a severe alcohol problem. So it rumbled on for a few years with my mental health in free fall. Dynamite.
This is extremely risky – dangerous – for the sick doctor. If you lack insight or if you’re in denial you can be finished (as indeed the numbers of people reported to have committed suicide while waiting for their Fitness to Practise sessions show).
I remember how I totally ‘lost it’ in 2005 a year before my final hearing. I had long left a medical job, but I just fell apart while still waiting for my GMC hearing. I went on a massive bender sat alone sobbing into my drink in a pub in Notting Hill very close to Portabello Road, ended up being sectioned, and then was suspended by the GMC.
A year after I was erased, with no job and no family or friends virtually, my life really did take a nosedive. I sat in pubs all day from opening time to closing time. I was done for drunk and disorder offences.
But I woke up after a six week coma, newly disabled, but with a new purpose. I did three books on postgraduate medicine, and I became regulated by the Solicitors Regulation Authority. I have three degrees, my Bachelor of Law, my Master of Law, and my Master of Business Administration, as well as my pre-solicitor training.
I didn’t get very far when I bothered going up to Manchester for my restoration application. The GMC hadn’t bothered to do a basic conflicts session, so the meeting was adjourned after one day. My friend Martin Rathfelder made it to support me. He like Jos Bell and Kate Swaffer are true friends.
It’s a miracle that I didn’t have a relapse being in the City where I had been with my late father, where I was erased, with plenty of bars and restaurants, with plenty of memories. It’s like you’re being set up to fail by the GMC – or else they are incredibly incompetent when it comes to dealing with people with mental health issues.
But I did get as far as asking the panel if I could hold the hearing in public this time. I want to explain to the whole world why and how alcohol destroyed my life, and caused distress to others.
I think the GMC did the right thing in getting rid of me from the medical profession, but I am still bemused why one consultant in West London asked me to sort it out by giving me a phone number of the Priory, did not refer me to Occupational Health, and did not offer me sick leave. I am bemused why various consultants described me as looking dishevelled and alcoholic, and yet allowed me to finish my medical jobs in London, without referring me to Occupational Health.
By the time I was erased, the GMC had been given five reports from five independent doctors stating clearly that my primary problem was a severe alcoholic dependence disorder, and that I desperately needed help.
I never received this help until the NHS saved my life a year later.
The GMC will wish to ‘win their case’ and I strictly speaking am not allowed to bring any of this up in case it reaks of bitterness.
The GMC opposed my application to explain all this and my recovery in public. The panel rejected the GMC’s case.
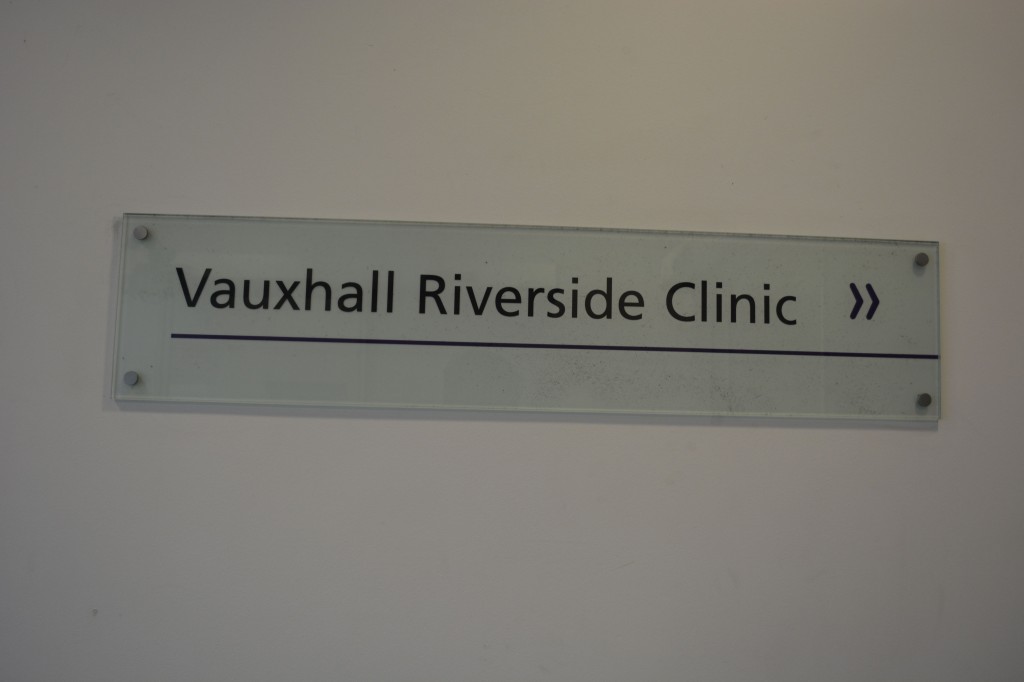
In my view, Clare Gerada’s “Practitioner Health Programme” is a necessary lifeline for those are sick Doctors, and who fall under the London jurisdiction.
Prof Gerada is a true inspirational NHS leader.
Needless to say, I’ve never had an alcoholic drink for more than seven years, since my coma. I’m one of those guys who has no off switch after one drink, such that I’ll either end up in A&E or in a police cell.
My case will now be held in Manchester beginning August 20th 2014. If you want to begin to understand how sick doctors cope, or do not cope, please feel to come along.
My experience of being a sick Doctor
“Anything can happen to anybody at any time.”
This one principle does guide what I think about people and health.
It’s what I think when a friend of mine living with dementia suffers a bereavement. It’s what I think when a friend of mine gets told he has bladder cancer.
It’s also how I come to rationalise my six week coma in 2007 due to acute bacterial meningitis. I was rushed into the intensive care unit of the Royal Free Hospital Hampstead, having been resuscitated successfully by somebody I used to work with in fact. He knows who he is.
His team stopped me fitting in an epileptic seizure. His crash team got a pulse back on their third cycle of jumping down on my chest after I had been flatlining in cardiac asystole. He managed to put a tube down me as I had stopped breathing.
I then spent six weeks in a coma, and my mother and late father came to visit me every day in intensive care, and in the neurorehabilitation unit (Albany Ward) at the National Hospital for Neurology and Neurosurgery, London (a hospital in which I had worked in 2002 in a rotation which included an interest of mine, dementia).
I am now living with physical disability. I can now walk, and I remember my protracted time in a wheelchair. I remember people’s reactions to you in the street. I remember how ‘available’ black cabs would simply drive past. I was, in effect, taught how to work again by inpatient and community physiotherapy.
Due to my meningitis, I could barely speak; the “speechies” helped me with that. I had difficulty planning a cup of tea; the “OTs” helped me with that.
I can relate to all the current NHS concerns how you become stripped of identity in the modern NHS: you become a bed number, or at best a surname.
But in many ways, as my late father kept reminding me shortly before his own death in November 2010, that meningitis in a way saved my life.
I then engaged properly with the NHS as a patient. I used to see my GP regularly.
As a medical student, I had felt as if I was too busy to see my own GP. Big mistake.
As a young house officer in hepatology, I used to be surrounded with very pleasant patients; but for whom I had to perform an abdominal paracentesis, as they were often bright yellow due to liver failure (but awaiting a liver transplantation).
I slowly became alcoholic and isolated. I have often been asked when did I start to drink heavily. This is very difficult for me to place, as most people like me go through a phase of problem drinking.
My official diagnosis for the alcoholism is severe alcohol dependence syndrome in remission. I have now not drunk alcohol for seven years. I know I am an alcoholic as it is unsafe for me to have an alcoholic drink. If I have an alcoholic drink, I would either end up in A&E or in a police cell. I am incapable of having a social drink.
Receiving a medical diagnosis for my mental health condition, in my particular case, helped me to rationalise the cause of my problems which had caused so much distress to others including especially my mother and late father.
I was listening to LBC last night and the presenter was joking that he had a listener rung up “I am an alcoholic. I haven’t had a drink for 35 years.” But seriously folks, it is like that.
I am now regulated by the legal profession. I spent 9 years at medical school, doing my basic degrees for medicine and surgery, and my PhD in the early diagnosis of frontal dementia. As a junior in the medical profession, walking around as the most junior member pushing the Consultant’s trolley and writing in the notes, the thought that you might be ill did seem an alien one.
And yet I was extremely ill. For all people in addiction, there becomes a time when you are in complete denial and lack complete insight. That’s when it is impossible for you to be regulated.
I also have a lot of sympathy for the regulators who regulate people who I think can be best be described as a “dry drunk patients” – i.e. they spend months or even years dry before relapsing. They are, I feel, “living by the seat of their pants”, or “whiteknuckling” it.
The alternative is recovery – where you are not merely abstinent, but where you embrace a life which is utterly content, but in the absence of your addiction of choice.
I indeed find this hard to explain to people who have never experienced addiction. I do not wish to compete with ‘patient leaders’, or think tanks who go on and on and on and on about patient involvement.
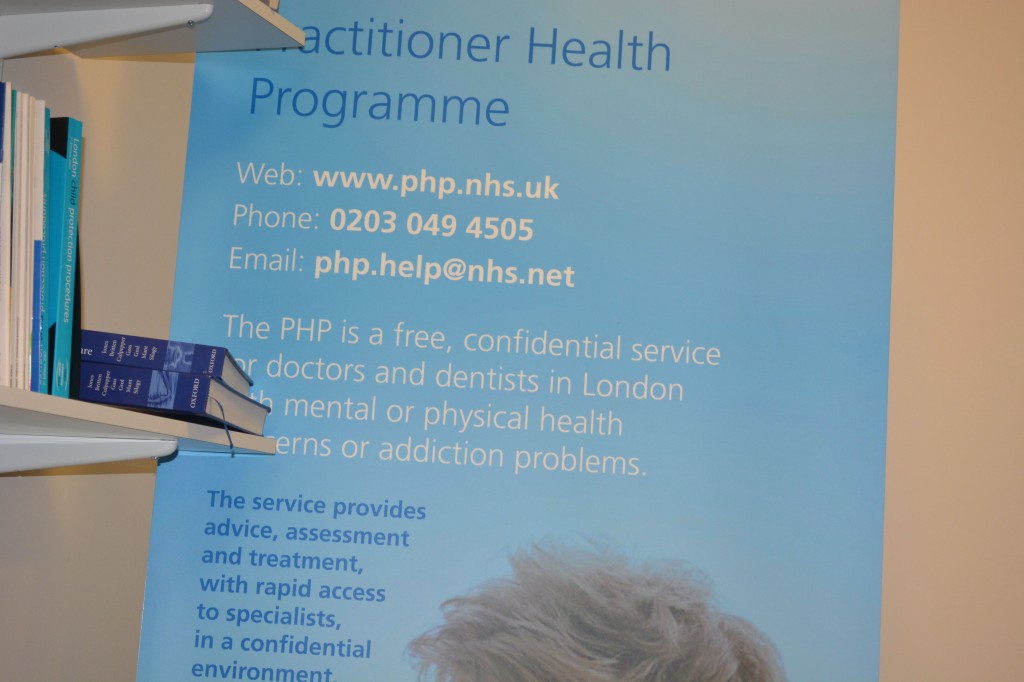
But I do wish to recommend to you, if you are in their catchment area, the Practitioners Health Programme (PHP). An incredible ambition of Prof Clare Gerada, the programme is a lifeline to doctors who are ill. It’s been shown in numerous numerous surveys that an ill doctor under-functions as much ‘use’ as a doctor who is completely out of the service. I would simply say to anyone who is ill in the medical profession, put your own health ahead of your career. Your patients deserve that too. Do not be blinded by your own career. I am proud to attend regularly PHP.
I don’t do much apart from hundreds of blogs for the SHA, or campaigning for people living with dementia. But I am at least at last content.
Update: I (Dr Shibley Rahman) was returned to the GMC Register for the UK 26 August 2014. I had been in recovery from alcohol since the onset of my coma due to meningitis in June 2007.
Is Sir Malcolm Grant’s new idea of a short medical course a beneficial disruption or a ‘race to the bottom’?
Sir Malcolm Grant is Chair of NHS England. He helpfully presented an overview of commissioning in the NHS under ‘clinical commissioning groups’ yesterday afternoon at Olympia. Grant was until very recently the President and Provost of UCL in London, having had an accomplished career elsewhere including at Cambridge.
Grant’s talk was an optimistic vision of how commissioning might work in this new era following the Health and Social Care Act (2012). He emphasised that the roll-out of CCGs effectively was “the dog that didn’t bark”. I asked a question whether he felt disappointed that the participation of GPs wasn’t greater in CCGs. Grant said, “If I’m being honest, yes”, which was a frank reaction to the observation that CCGs may not be ‘led’ by GPs and that indeed many GPs are unwilling to participate in the CCGs.
At first, Grant’s suggestion that there could be more providers on CCGs might seem ludicrous, but, in terms of policy, might reflect a genuine concern of the providers’ viewpoint to be expressed too. In any case, there are numerous allegations of GPs having ‘conflicts of interests’ in also sitting on CCGs for the commission of services where they potentially have a direct financial interest.
Part of the raison d’être of clinical commissioning groups, and actively promoted as a ‘catalyst for change’, was that primary care physicians could ‘drive’ commissioning. The history of CCGs, however, can be delineated from two sources. One is the evolution of health maintenance organisations in the US, and the second is Pirie and Butler’s “The Health of Nations” discussion document for the Adam Smith Institute a while ago.
CCGs are functionally insurance bodies which assess risk in a given population. Grant cited that there had been great flexibility in the population sizes being served by CCGs. In insurance terms, there is nothing particularly emotional about it, however. The greater the size of population, the more accurate your assessment of risk might potentially be.
One of the most striking suggestions by Grant was that the undergraduate medical curriculum could be much ‘shorter’, reflecting how easily information could be looked up on electronic search engines at the drop of a hat. Grant correctly pointed out that most of the audience probably had the equivalent of 32GB in their hand.
By suggesting this, Grant is of course admitting that ‘knowledge is power’, a sensible thing in itself. However, the narrative that ‘all information is knowledge’ is a dangerous one, given the sheer volume of irrelevant information.
Making decisions in the real world, in business management, has been much influenced recently by the field of ‘bounded rationality’, that fundamentally we have to make quite quick decisions having paid selective attention to parts of the world around us. When you do a Google search, you can’t possibly read all of the search results.
The drive towards a ‘quick medical course’, say 2 years rather than 6 years, comes from the idea that you could get rid of time wasted in learning material available elsewhere more easily. For example, a medical student would no longer be required to show a ‘fact dump’ of the point of origin, insertion, action and nerve supply of every muscle in the body? Likewise, a medical student would no longer be required to present every chemical involved in the biochemical cascade leading from activation of a particular receptor for a drug?
There is certainly a case that an undergraduate medical student learns a lot of useless information in 5-6 years, which is not good preparation for the pre-registration junior doctor jobs in a busy hospital, when other skills such as practical procedures or time management might be more beneficial. Certainly, even in the current curriculum, a medical student might do a maximum of one month in General Practice, or one clinical lecture on dementia and delirium.
It is also, unfortunately, the case that, at many medical schools, the preclinical medical school is overloaded by overly detailed lectures by basic scientists expert in their fields (but these scientists have never seen a patient in their life.)
A ‘provider’ offering a short medical curriculum might have business ‘competitive advantage’ as a shorter curriculum is likely to be shorter and cost less. The General Medical Council will of course wish to ensure that the end-product of a short medical course is a Doctor who is safe for the public.
A short medical course could therefore be a ‘genuine disruption’ which dislodges the power of the ‘incumbents’. In other words, one simple change to the way the medical curriculum is changed to focus on skills of learning how to learn rather than sheer volume might benefit the student and public alike. Grant, correctly perhaps, feels that the emphasis should be on lifelong learning through CPD (and to extend his concept lifelong regulation through mechanisms such as ‘revalidation’).
At worst, the short medical curriculum could be interpreted as a ‘race to the bottom’, reducing the ‘barriers to entry’ in educational provider, producing Doctors at high volume and low cost. This might lead to a glut of unemployed Doctors. The needs of individual Doctors are not higher than the needs of the profession, but it is a valid presumption that the public prefers Doctors to be as highly skilled as possible.
Anyway, it is clear that Sir Malcolm Grant has not got an attitude of ‘mission accomplished’, but instead Grant seems genuinely fired up about all his challenges ahead.
Time to rate how Doctors are treated in the NHS?
Sir Gus O’Donnell said famously, “If you treasure it, measure it”. This is happening in the medical profession too, with a policy drive that the best people to rate the NHS are the users of the service. These are the patients (or “customers” if you’re that way inclined). The ‘Friends and Family Test’ has come under fierce criticism, not surprising given that it has never been subject to proper analytical rigour, and the criticisms of it have been well rehearsed elsewhere. There is a fundamental difference in assessing your hospital stay, compared to “Trip Advisor”, but it is all part of the information revolution. Information, according to people interested in innovation like me, is not the same as knowledge, and not all information is useful. Whilst the corporates, who introduced their love for Big Data to the rest of the world are fully aware there is a lot of redundant, useless data, and the importance of certain datasets need to be explained carefully, this has completely passed the NHS by. The introduction of the vascular surgery rates was held by some to be a shambles, due to the poor explanation of these data as well as data inaccuracy. Forgetting the fact that certain fields in vascular surgery (e.g. abdominal artery aneurysm repairs for aneurysms diameter > 6.5 cm are considered riskier than sclerosing varicose veins, for example), or that safety is a team activity (though the root cause of a problem can be identified to a single reason), the data explosion is envisaged as empowering patients and persons with ‘choice’.
Enter the market. Jeremy Hunt continues to dodge completely the question why private sector entities under freedom of information legislation introduced by a Labour government are not under obligation to disclose data because of their ‘commercial interest’. As they are not public bodies, they are not amenable to judicial review either. Moving swiftly on, choice is supposed to empower the patient with information. How is that possible, that a patient will be equally fluent as a Doctor of about 7 years’ standing who has achieved registration with the General Medical Council? Very good question. Is it the case that vascular surgeons have a need to improve their mortality data because they are now operating (quite literally) in a free (pseudo)market? No, categorically not. The Royal Colleges of Surgeons and the General Medical Council are responsible for general professional training and higher specialist training standards in surgery. Doctors are increasingly seen as employees in a business case, with Trusts salami-slicing how much they want to spend on staff to achieve their efficiency savings as mandated by Sir David Nicholson and the Department of Health. They are that respect no more essential than an import of horsemeat for lasagna to improve the profitability of a venture capital investment. Registered Doctors are professionals though, and legal.
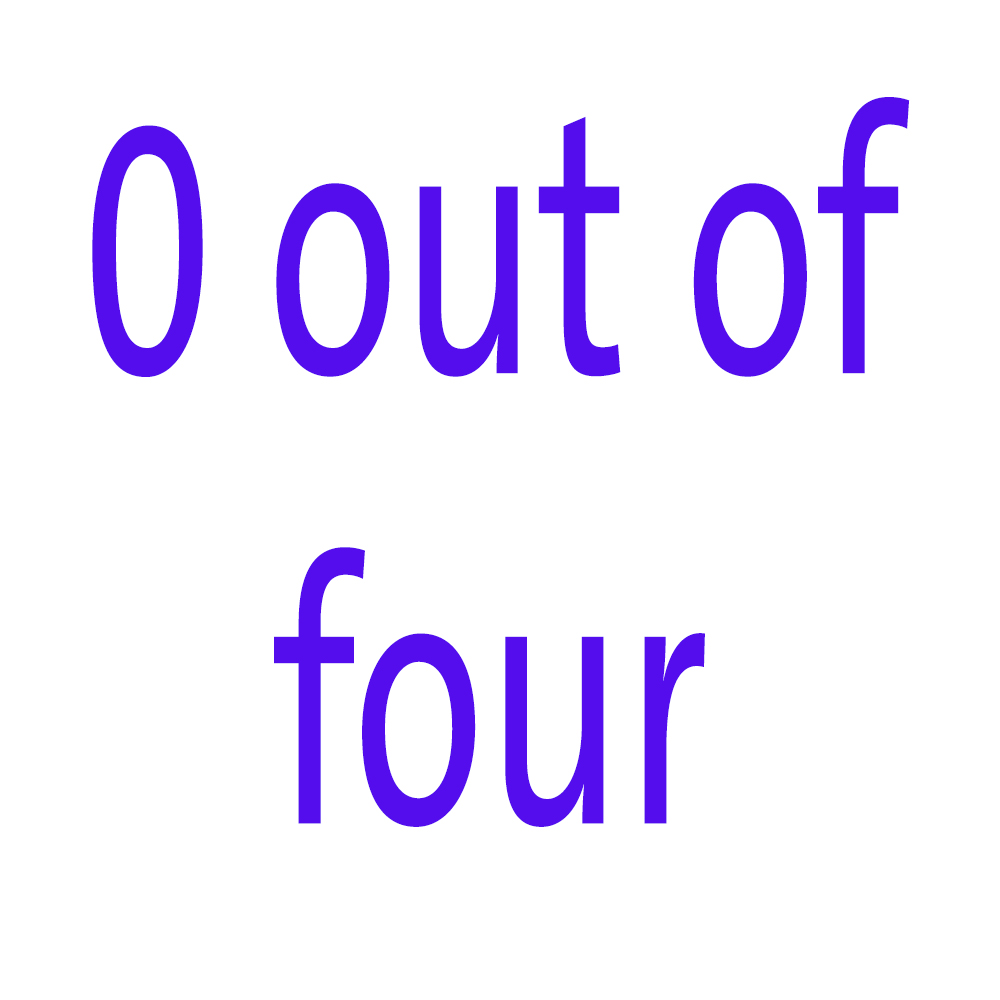
It has been noted that trust in GPs has plummeted from 70% to 30% since the implementation of the Health and Social Care Act (2012)? I, for one, would quite like to rate how management consultants conducted this important strategic implementation. This £3bn reorganisation had a critical piece of legislation, the “section 75 regulations”, which produced competitive tendering as the default option. The first set of Regulations were so bad they had to be withdrawn. The Medical Royal Colleges, the BMA and RCN all say the Act won’t work. The first rule of strategic implementation is that you involve all the stakeholders and engage in a realistic conversation about what is intended to be achieved, how, why, or when. None of this happened. That is why I award the Department of Health, despite what can be best described as “shuttle diplomacy” by Earl Howe, a big fat result thus:
 And why has trust in GPs plummeted? Is it anything to do with the fact the media and politicians have been force-feeding the public with stories that GPs opted out of out-of-hours some time ago, and they got a deal which was quite lucrative? Or is it because there are now anecdotal reports of GPs having to advise non-NHS care to their patients in the hope that they can jump a lengthy NHS queue? It is very hard to tell. But certainly it is true that GPs have become first in the firing line for the NHS reforms. They in fact opposed the reforms, with clear leadership by Prof Clare Gerada, Chair of the Royal College of General Practitioners. The Government PR went into overdrive that “GPs are at the heart of commissioning”, the ‘clinical commissioning groups’, but this was obviously never the intention. CCGs are merely a vehicle for holding funds and assessing risk in a pooled population, in a manner of ‘statutory insurance schemes’. This has always been the case, and always will be. For all the talk of ‘entrepreneurial GPs’, the public do not appear to warm to the idea of GPs as businessmen (and GPs do not particularly wish to represented as businessmen). Germane to this is the “dual agent” problem, very well known in insurance markets. That is the idea that no person can have “two masters”, without a significant conflict of interest: this might be for example a GP’s professional duty to his or her patient, and his or her duty to the people who ultimately provide the funding. This issue of trust is possibly bound to get worse, as ‘scandals’ are drip fed to the media of a system in distress. The reason this score is nothing to do with Prof Gerada is because Prof Gerada, as the new “NHS SOS” book explains (edited by Dr Jacky Davis and Prof Ray Tallis), was one of the few NHS leaders to have a clear vision and have the charisma to set this out in confidence, a textbook example of a “charismatic leader”, who deservedly was one of the hundred most influential individuals in health. And, very clearly, she appeared to be representing patients as well as GPs.
And why has trust in GPs plummeted? Is it anything to do with the fact the media and politicians have been force-feeding the public with stories that GPs opted out of out-of-hours some time ago, and they got a deal which was quite lucrative? Or is it because there are now anecdotal reports of GPs having to advise non-NHS care to their patients in the hope that they can jump a lengthy NHS queue? It is very hard to tell. But certainly it is true that GPs have become first in the firing line for the NHS reforms. They in fact opposed the reforms, with clear leadership by Prof Clare Gerada, Chair of the Royal College of General Practitioners. The Government PR went into overdrive that “GPs are at the heart of commissioning”, the ‘clinical commissioning groups’, but this was obviously never the intention. CCGs are merely a vehicle for holding funds and assessing risk in a pooled population, in a manner of ‘statutory insurance schemes’. This has always been the case, and always will be. For all the talk of ‘entrepreneurial GPs’, the public do not appear to warm to the idea of GPs as businessmen (and GPs do not particularly wish to represented as businessmen). Germane to this is the “dual agent” problem, very well known in insurance markets. That is the idea that no person can have “two masters”, without a significant conflict of interest: this might be for example a GP’s professional duty to his or her patient, and his or her duty to the people who ultimately provide the funding. This issue of trust is possibly bound to get worse, as ‘scandals’ are drip fed to the media of a system in distress. The reason this score is nothing to do with Prof Gerada is because Prof Gerada, as the new “NHS SOS” book explains (edited by Dr Jacky Davis and Prof Ray Tallis), was one of the few NHS leaders to have a clear vision and have the charisma to set this out in confidence, a textbook example of a “charismatic leader”, who deservedly was one of the hundred most influential individuals in health. And, very clearly, she appeared to be representing patients as well as GPs.
Anyone who wishes to defend the NHS is accused of protecting a ‘national religion’. And yet the NHS is accused of being ‘monolithic’, ‘inefficient’, ‘dangerous’, ‘expensive’, and every negative adjective under the sun. Politicians are responsible for this deprofessionalisation of key non-managerial workers in the NHS, with talk of ‘it doesn’t matter who provides my care as long as it is the…’ (a saying which in the legal and medical sectors has increasingly been completed with the word “cheapest”). Every conceivable thing is blamed for the pressures under which the NHS functions; such as the “burden of the ageing population” and the equally pathetic and untrue myth that high-quality healthcare is dependent on expensive equipment. Tell that to the cardiologist who can discern an early diastolic murmur with a pulmonary hypertensive ‘heave’ due to a crappy £20 stethoscope, not a £5000 portable digital echocardiogram machine. The number of lies in the drive to make the NHS attractive financially to outsourcers and privatisers has been breath-taking. In view of this, isn’t it time perhaps we either rate how Doctors are actually treated in the NHS, or time to turn the tables and rate our NHS management and politicians?
It was honour to speak to a group of suspended Doctors on the Practitioner Health Programme this morning about recovery
It was a real honour and privilege to be invited to give a talk to a group of medical Doctors who were currently suspended on the GMC Medical Register this morning (in confidence). I gave a talk for about thirty minutes, and took questions afterwards. I have enormous affection for the medical profession in fact, having obtained a First at Cambridge in 1996, and also produced a seminal paper in dementia published in a leading journal as part of my Ph.D. there. I have had nothing to do with the medical profession for several years now, apart from volunteering part-time for two medical charities in London which I no longer do.
I think patient safety is paramount, and Doctors with addiction problems often do not realise the effect the negative impact of their addiction on their performance. No regulatory authority can do ‘outreach’, otherwise it would be there forever, in the same way that Alcoholics Anonymous or Narcotics Anonymous do not actively go out looking for people with addiction problems. I personally have doubts about the notion of a ‘high functioning addict’, as the addict is virtually oblivious to all the distress and débris caused by their addiction; the impact on others is much worse than on the individual himself, who can lack insight and can be in denial. Insight is something that is best for others to judge.
However, I have now been in recovery for 72 months, with things having come to a head when I was admitted in August 2007 having had an epileptic seizure and asystolic cardiac arrest. Having woken up on the top floor of the Royal Free Hospital in pitch darkness, I had to cope with recovery from alcoholism (I have never been addicted to any other drugs), and newly-acquired physical disability. I in fact could neither walk nor talk. Nonetheless, I am happy as I live with my mum in Primrose Hill, have never had any regular salaried employment since my coma in the summer of 2007, received scholarships to do my MBA and legal training (otherwise my life would have become totally unsustainable financially apart from my disability living allowance which I use for my mobility and living). I am also very proud to have completed my Master of Law with a commendation in January 2011. My greatest achievement of all has been sustaining my recovery, and my talk went very well this morning.
The message I wished to impart that personal health and recovery is much more important than temporary abstinence, ‘getting the certificate’ and carrying on with your career if you have a genuine problem. People in any discipline will often not seek help for addiction, as they worry about their training record. Some will even not enlist with a G.P., in case the GP reports them to a regulatory authority. I discussed how I had a brilliant doctor-patient relationship with my own G.P. and how the support from the Solicitors Regulation Authority (who allowed me unconditionally to do the Legal Practice Course after an extensive due diligence) had been vital, but I also fielded questions on the potential impact of stigma of stigma in the regulatory process as a barrier-to-recovery.
I gave an extensive list of my own ‘support network’, which included my own G.P., psychiatrist, my mum, other family and friends, the Practitioner Health Programme, and ‘After Care’ at my local hospital.
The Practitioner Health Programme, supported by the General Medical Council, describes itself as follows:
The Practitioner Health Programme is a free, confidential service for doctors and dentists living in London who have mental or physical health concerns and/or addiction problems.
Any medical or dental practitioner can use the service, where they have
• A mental health or addiction concern (at any level of severity) and/or
• A physical health concern (where that concern may impact on the practitioner’s performance.)
I was asked which of these had helped me the most, which I thought was a very good question. I said that it was not necessarily the case that a bigger network was necessarily better, but it did need individuals to be open and truthful with you if things began to go wrong. It gave me a chance to outline the fundamental conundrum of recovery; it’s impossible to go into recovery on your own (for many this will mean going to A.A. or other meetings, and discussing recovery with close friends), but likewise the only person who can help you is yourself (no number of expensive ‘rehabs’ will on their own provide you with the ‘cure’.) This is of course a lifelong battle for me, and whilst I am very happy now as things have moved on for me, I hope I may at last help others who need help in a non-professional capacity.
Best wishes, Shibley
My talk [ edited ]
Coping being a professional in recovery: some personal thoughts for my talk
I’ve accepted an invitation to give a talk on May 10th 2013 on coping with being a professional in recovery.
I am posting my notes here in the hope that they may be useful to people one day.
Coping being a professional in recovery
Complicated area – personal thoughts – “no right answer!”
A. Being in recovery is a way of enjoying what life has to offer, not being dominated by your ‘drug of choice’.
There’s a temptation to think of some addictions as ‘morally superior’ to others: e.g. ‘alcoholism is not as bad as heroin addiction’. This is not all true – they are all equally destructive.
Common question on Twitter: “How do I know if I am an alcoholic?”
in a reply not giving any medical advice, “Because you can never stop at one drink.” (either end up in a police cell or in Medical Admissions.
Never ‘too late’ to enter recovery – even if you think your life cannot get any more disastrous. It can get more disastrous, surprisingly.
B. The legal doctrine of proportionality
Not personal – can seem that way.
GMC have a statutory duty for patient safety – their application of the law has to obey the legal doctrine of proportionality (necessary/legitimate aim) vs the ‘needs’ of the individual. This is undoubtedly a tricky balance to decide upon.
C. The media
Feb 2012, Daily Mail: Special Investigation: Why ARE so many doctors addicted to drink or drugs?
Can be a reactionary issue like foreign doctors/immigration etc.
“Disturbing new research reveals that one in six doctors has been hooked on alcohol or drugs. How has this happened – and what are the implications? According to shocking new figures, up to one in six doctors will have been addicted to drink or drugs – or both – at some stage in their medical career, raising the horrifying prospect that these highly-paid carers may have your life in their trembling hands.”
November 2012, Independent: The doctor battling drink and depression will see you now …
“Thousands of doctors are continuing to treat patients while hiding their own problems with drink, drugs and depression because of a “culture of invincibility” among health professionals. Each year hundreds of medics are treated for addiction and mental health issues, according to official statistics. But researchers investigating the issue say that this masks a much bigger problem, with thousands of doctors concealing their symptoms.1,384 doctors who had been assessed for underlying health concerns over the past five years. Of these, 98 per cent were diagnosed with alcohol, substance misuse or mental health issues.”
D. Some immediate thoughts
- Insidious progression between problem drinker and ‘serious alcoholic’.
- Patient safety – extremely important, but also important for regulators to resist any urge to find scapegoats.
- Poor performance management of trainees ?needs supervisors to be alert to and sensitive to problems (health, pt. safety, training record, needs of hospital).
- A referral to a regulatory body should not be a ‘substitute’ for sorting out performance issues for health locally.
- Need to build a culture of trust.
- A referral to a regulatory body can be used by all staff involved for the purposes of ‘covering their backs’, but not actually dealing with the problem as it arose.
- Tendency to airbrush
- Prone to overintellectualise – attributes of an alcoholic: telling lies, conceal the truth. Mitchell and Hirschman (2006) : “Forty-one of those patients (87%) kept the drinking hidden from treatment staff.” This project examined the frequency of within treatment drinking and surreptitious drinking among patients who attended a brief substance abuse treatment program that mandated within treatment abstinence.
E. Playing the blame game
Regulators hate it if the patient blames everyone except him or herself.
However this should not ignore widespread issues of culture which need a mature sensitive debate (can healthcare staff ‘whistleblow’ constructively on other staff in the pursuit of patient safety?)
Learning from mistakes – rehabilitation v retributive justice. “Zero fault” approach
Problems with the ‘blame game’ – denial and lack of insight by the patient himself or herself Duffy (1995)
If you have a drinking problem, you may deny it by:
- Drastically underestimating how much you drink
- Downplaying the negative consequences of your drinking
- Complaining that family and friends are exaggerating the problem
- Blaming your drinking or drinking-related problems on others and lack of insight
F. The “steps”
Step 1: WE ADMITTED WE WERE POWERLESS OVER ALCOHOL – THAT OUR LIVES HAD BECOME UNMANAGEABLE. (Step One consists of two distinct parts: (1) the admission that we have a mental obsession to drink alcohol and this allergy of the body will lead us to the brink of death or insanity, and (2) the admission that our lives have been, are now, and will remain unmanageable by us alone.)
The “steps” in full:
- We admitted we were powerless over alcohol – that our lives had become unmanageable.
- Came to believe that a power greater than ourselves could restore us to sanity.
- Made a decision to turn our will and our lives over to the care of God as we understood Him.
- Made a searching and fearless moral inventory of ourselves.
- Admitted to God, to ourselves, and to another human being the exact nature of our wrongs.
- Were entirely ready to have God remove all these defects of character.
- Humbly asked Him to remove our shortcomings.
- Made a list of all persons we had harmed, and became willing to make amends to them all.
- Made direct amends to such people wherever possible, except when to do so would injure them or others.
- Continued to take personal inventory, and when we were wrong, promptly admitted it.
- Sought through prayer and meditation to improve our conscious contact with God as we understood Him, praying only for knowledge of His will for us and the power to carry that out.
- Having had a spiritual awakening as the result of these steps, we tried to carry this message to alcoholics, and to practice these principles in all our affairs.
G. How do you know if you have a drinking problem?
You may have a drinking problem if:
- Feel guilty or ashamed about your drinking.
- Lie to others or hide your drinking habits.
- Have friends or family members who are worried about your drinking.
- Need to drink in order to relax or feel better.
- “Black out” or forget what you did while you were drinking.
- Regularly drink more than you intended to.
- Start drinking before you go out socially
- Drink on your own in bars
- Go to off-licences or supermarkets to buy cheap alcohol
- Don’t care if you’re ‘performance’ is substandard at work.
Common ‘issues’:
- Repeatedly neglecting your responsibilities at home or work, because of your drinking. ?house untidy, deferring ‘activities of daily living’ e.g. culture, shopping
- Using alcohol in situations where it’s physically dangerous, such as drinking and driving, or drinking the day before a heavy workload
- Experiencing repeated legal problems on account of your drinking. ?how many Doctors facing suspension voluntarily offer their PNC or CRB ?should Doctors be asked to submit this information as part of the revalidation process in future (note comments about outreach)?
- Continuing to drink even though your alcohol use is causing problems in your relationships.
- Drinking as a way to relax or de-stress/coping with ‘success’. Many drinking problems start when people use alcohol to self-soothe and relieve stress. Getting drunk after every stressful day, for example, or reaching for a bottle every time you have an argument with your boss.
H. Why are “professionals” particularly vulnerable?
Gossop et al. (2000): “There are several reasons why doctors and other health care professionals may be at risk of drug and alcohol misuse. The long years of medical training are characterized by intense competition, excessive workload and fear of failure, and few occupations face the intense stresses experienced in the daily practice of medicine”.
Personal experience from recovery meetings: city lawyers, traders, hospital managers, journalists
I. “Presenteeism” – seeking help is seen as getting a criminal record?
Dr Max Henderson, from King’s College London’s Institute of Psychiatry, believes that these numbers represent the tip of the iceberg because “doctors are often deterred from admitting that they are sick and need time off by feelings of shame.
A recent study led by Dr Henderson showed that medics who do fall ill fear being perceived as “weak” or “a failure” by colleagues. “There is a feeling among doctors, that illness shouldn’t happen to them – that they should somehow be invincible,” said Dr Henderson.
“Doctors are particularly vulnerable to ‘presenteeism’ and we know they are reluctant to use mainstream healthcare services and will sit on their symptoms and not share them with anyone. So they may treat themselves or they try to get their friends to treat them through what are known as ‘corridor consultations’.”
J. The difference between recovery and abstinence / white knuckling
For most serious alcoholics, it is easier to abstain altogether, rather than to engage in controlled, responsible, non-intoxicated drinking.
The idea of controlled drinking (or controlled drug use) is the one hope almost every addict brings to his or her initial encounter with treatment. As one AA veteran put it: “If it were possible for a majority of alcoholics to revert to controlled drinking, every alcoholic in AA would have found out about it a long time ago.”
The ‘dry drunk’ phenomenon: This describes a phenomenon in which a person stops drinking and using, but does not make any other significant changes in his life. They are known as “dry drunks” because even though they are sober, their behavior mirrors that of someone who is drinking.
Specialist advice for disulfiram and acamprosate, e.g.
K. Features of alcohol dependence
Alcoholism is the most severe form of problem drinking. Alcoholism involves all the symptoms of alcohol abuse, but it also involves another element: physical dependence on alcohol. If you rely on alcohol to function or feel physically compelled to drink, you’re an alcoholic.
Tolerance: The 1st major warning sign of alcoholism
Do you have to drink a lot more than you used to in order to get buzzed or to feel relaxed? Can you drink more than other people without getting drunk? These are signs of tolerance, which can be an early warning sign of alcoholism. Tolerance means that, over time, you need more and more alcohol to feel the same effects.
Withdrawal: The 2nd major warning sign of alcoholism
Do you need a drink to steady the shakes in the morning? Drinking to relieve or avoid withdrawal symptoms is a sign of alcoholism and a huge red flag. When you drink heavily, your body gets used to the alcohol and experiences withdrawal symptoms if it’s taken away.
These may include:
- Anxiety or jumpiness
- Shakiness or trembling
- Sweating
- Nausea and vomiting
- Insomnia
- Depression
- Irritability
- Fatigue
- Alcohol withdrawal fits
- Loss of appetite
- Headache
Waking up in the morning – needing to go to a pub
L. Two myths of ‘alcoholism’
a. I’m not an alcoholic because I have a job and I’m doing okay.
You don’t have to be homeless and drinking out of a brown paper bag to be an alcoholic. Many alcoholics are able to hold down jobs, get through school, and provide for their families. Some are even able to excel.
The myth about “the high functioning addict”.
b. Drinking is not a “real” addiction like drug abuse.
Alcohol is a drug, and alcoholism is every bit as damaging as drug addiction. Alcohol addiction causes changes in the body and brain, and long-term alcohol abuse can have devastating effects on your health, your career, and your relationships. Alcoholics go through physical withdrawal when they stop drinking, just like drug users do when they quit.
M. Recovery is an ongoing process
Recovery is a bumpy road, requiring time and patience.
The GMC fitness to practise procedures are reported by many, anecdotally, to be time consuming, but they also involve a huge commitment from GMC staff, panel members and specialist advisors. The problem comes to ensure that the mental health of people under investigation does not deteriorate in the lengthy process.
Stress can make addictive symptoms worse, but if right regulatory process can help encourage people in recovery.
Regulators should avoid giving any impression of criminalising people for illness, or humiliating people unnecessarily in the course of their proceedings. There should be a real effort to preserve the dignity of ill people, as Doctors can be patients too. This requires a commitment of being proportionate in a definite drive for destigmatisation, whilst preserving the duty of public safety in the utmost. This requires a shift in mindset of a view where some people cannot be treated for mental illness such as addiction.
N. Support networks
Tendency to ‘get the certificate’ than to understand the process of recovery.
1. Practitioners Health Programme
Dr Clare Gerada, Chair of the RCGP and PHP’s medical director, said: “We are seeing more sick doctors, more GPs in particular, more shame, more presenteeism, as doctors are worried about their futures. ”
2. British Doctors and Dentists Group – all ages, diverse backgrounds
The British Doctors and Dentists Group was formed originally for doctors who were attempting to recover from alcohol dependency and other substance abuse over 30 years ago. The late Dr Max Glatt encouraged some of the early members to form a group which met for mutual support on a monthly basis.
3. After Care
4. Psychiatrist/GP (nb GMC Good Medical Practice)
5. Friends/family/peers
6. ?Regulatory bodies
7. AA or similar entities.
END
Instead of “coasting clinicians”, target your wrath at those mediocre meddling managers
“Great spirits have always encountered violent opposition from mediocre minds.” Albert Einstein
Not all managers are ‘mediocre and meddling’ but some are. I was told by a English NHS consultant last night how nurses in his outpatients clinics are now clocking him in and clocking him out, and gives him permission to leave the clinic when he’s done his allotted time, instead of frontline nursing. Also, he is now expected to stay on site in his 40s during certain hours at night. This has actually caused much resentment across the Consultant workforce in his Trust, such that the managers bombed in their recent staff survey apparently. But these results are not going to be made public. It is easy to target ‘coasting’ from clinicians in the NHS, but it is overwhelmingly clear there are hotspots of meddling, mediocre poor management in the NHS, of overpaid NHS managers making the wrong decisions, but making the wrong decisions quite efficiently for their generous salary. That is why they will never become leaders.
One good aspect about the Francis Report is that the NHS seems to be able to tolerate failure. Failure on quite a large scale – distressed relatives of loved-ones who saw patients drinking water out of flower vases, and clinical regulatory authorities which have yet to make a single sanction years down the line. For all the discussion about the independence and autonomy of entities within the National Health Service, as the toxic culture which might have caused this disaster appears so widespread, it has been argued that there is little point in ringfencing the blame. The problem with this approach is that it is possibly tantamount to be giving up on ‘contagion’, and indeed it is most unlikely that Mid Staffs represents an isolated locus of pathology within the NHS. There is still the unresolved issue about the use of ‘gags’ and ‘supergags’, paid for through the tax payer, of NHS managers, and an overall acceptance that we have to put up with a culture of mediocrity in management in the NHS.
It is very hard to think of ‘great managers’ in the NHS, partly because managers are supposed to be doing things right rather than being identified for doing the right things. Therefore, you are more likely to identify a “good manager” because a disaster has not happened. And yet you never hear of anyone (who isn’t on the NHS graduate management scheme) who says, ‘Yeah, I really want to be a NHS manager’. Compared to a leading cardiologist or brain surgeon, nobody says, ‘I want to be the next David Nicholson’. This is because David Nicholson can be said to be the epitome of ‘coasting'; of someone who is virtually unsackable, as he is surrounded by too many ‘supporters’ in the establishment who ‘need’ him to implement these unpopular, costly, flawed reforms. Whilst the salary for junior doctors is far worse, and the conditions considerably worse (for example a week of nights, often carrying ‘the arrest bleep’), junior doctors on-the-whole are highly motivated people. This of course will be unknown to Jeremy Hunt, who never trained in the NHS, or many on the corporate healthcare lobbying circuit, but this is the reality of gifted people in the NHS. If anything, the brilliance of these junior doctors has been potentially suppressed by relatively poor pay for anyone who has completed effectively a seven-year intensive degree, and the sheer knowledge and skills required to ‘make it’ in medicine far outweighs those needed to command a bonus as an investment banker.
It is not uncommon for junior physicians who wish to train with the “best”, for example be on the clinical firm of Sir Richard Thompson, President of the Royal College of Physicians, in gastroenterology, or Professor Sir Ian Gilmore, the previous President, a hepatologist. However, the mediocrity culture of management is striking here. People who want to train with Sir David Nicholson probably do so more because they consider themselves using it as a passport to getting a well-paid position in the NHS, rather than the fact they wish to ‘train with the best’. Indeed, if you wished to be superb in management in the NHS, many younger people would prefer to do a sabbatical in Harvard Business School, and work with someone like Professor Clay Christensen, Professor of Innovation at Harvard, or Professor Michael Porter, Professor of Strategy at Harvard, than work with Sir David Nicholson. This is possibly an unintended consequence of a deep-seated ethos of mediocrity in NHS management.
When you look at the actual business management and leadership literature, you can see immediately the intimate relationship between leadership and dissipation of mediocrity. Take for example the effect of Fox Conner on a young Eisenhower; Fox Conner is a shining example of ‘one-to-one’ nurturing of a junior talent by somebody senior who wished to give up some of his time. Conner first met Eisenhower in 1919 at the Infantry Tank School at Camp Meade and the two men immediately developed a great mutual respect. Following his promotion to brigadier general in the Regular Army April 27, 1921, Conner took command of the 20th Infantry Brigade in Panama. He invited Eisenhower to join his staff and for three years Conner conducted a systematic course of study for Eisenhower that ranged from extensive readings in military history to daily practical experience writing field orders for every aspect of the command.
Mediocrity was probably at most about a sixth of Jeremy Hunt’s famous speech. However, it has generally been interpreted as a demoralising influence on the workforce of the NHS at a critical time, from a person who is known to have said disparaging things about the NHS, and who indeed is reputed to have not wanted the Danny Boyle item in the Olympics ceremony which he raved about at the beginning and end of that speech. The problem was that Hunt cames from a position of low integrity in criticising the medical profession. He has never worked as a medical professional in the NHS, so has no moral fitness-to-criticise about mediocrity in the NHS. Furthermore, he didn’t as such offer any solutions. This is exactly akin to a GP who tells you you have a cancer, but changes subject before he or she gets a chance to tell you about a possible treatment. Maybe this is because Jeremy Hunt knows the problems over his treatment: there is no Fox Conner figure to look up to. There is a plethora of people who’ve done the Jeremy Hunt job, like Hewitt, Dobson or Milburn, but who have not been there for a very long distance; they can perhaps offer their ‘expertise’ elsewhere. These are people who are unlike the junior doctors who qualify into the NHS at the age of 24 and possibly become Consultant at the age of 40. Secondly, Hunt cannot point to a single NHS manager who is not mediocre; who is a great visionary, or who has been known to be NHS management equivalent of Fox Conner. To be honest, Hunt has very little experience in NHS management himself, but this may be a growing trend in how the UK is run (take for example the report of a headteacher at the weekend who has never taken a lesson, indeed cf the Secretary of State for Education.)
Of course, these criticisms do not, in themselves, invalidate Jeremy Hunt’s argument. One of the major problems that the NHS, whilst it cannot be elevated to a position of immunity from criticism, is repeatedly cited as one of the most efficient health systems in the world; for example the US which spends much more has worse outcomes. And the corollary of this is that there is plenty of mediocrity in the private sector; indeed many ‘fat cats’ are truly ‘coasting’ as their shareholder dividends rocket from a flatlining performance in a market where it is impossible to fail (such as privatised gas, water, or telecoms). But medicine and nursing are professions, and Hunt’s language is inappropriate, because pervasive in Hunt’s thinking is that he treats medicine and nursing as commodities, parts of which can be readily packaged for private equity companies to make a ‘fast buck’. That is the distorted perverted concept of ‘wealth creation’, popular with some. That is possibly the biggest threat to the NHS becoming ‘mediocre’, and restoring dignity to a battered pair of professions at a time when they have been undermined by a complex reform they never asked for, would help to motivate its workforce. Calling them ‘mediocre’ from a position of relatively little authority, however, is utterly futile.