Home » Posts tagged 'London'
Tag Archives: London
The #G8Dementia Summit: a lack of cure for dementia, and tough on the causes of the lack of cure
The setting for today’s #G8Dementia Summit was in Lancaster House, London.
Many thanks to Beth Britton, Ambassador for Alzheimer’s BRACE and campaigner, Anna Hepburn at the Department of Health, and Dr Peter Gordon, Consultant and expert in dementia, for helping understand, with the excellent livestream from the Department of Health, what challenges might be in store for global dementia policy in the near future.
My account is @dementia_2014
The final G8 Summit Communique is here.
The G8 Summit Declaration is here.
There’s a bit of a problem with global dementia policy.
The patients, carers, families, businesses, corporate investors, charities, media, academics (including researchers) politicians, all appear to have different opinions, depending on who you speak to.
Peter Dunlop, a man with dementia of Alzheimer type, received a standing ovation after his speech. He had explained his reactions on receiving a diagnosis, and how has tried to continue enjoying life. He had been a Consultant Obstetrician and Gynaecologist.
Peter Dunlop: “I continue to enjoy life and fishing” – Moving testimony that a good life with #dementia is possible! #G8dementia
— Alzheimer Europe (@AlzheimerEurope) December 11, 2013
Peter Dunlop had a standing ovation from #G8dementia – NEVER underestimate the power of the lived experience of dementia
— Beth Britton (@bethyb1886) December 11, 2013
The people with dementia who appeared did indeed remind the audience, including Big Pharma, why they were there at all.
Trevor Jarvis talks about person-centered care and need for doctors to fully understand the disease. What an eloquent gentleman. #G8dementia
— Romina Oliverio (@RominaOliverio) December 11, 2013
And that there was more to life than medications:
AE Chair Heike von Lützau-Hohlbein highlights role of self-help movement and successful advocacy work #G8dementia
— Alzheimer Europe (@AlzheimerEurope) December 11, 2013
And this was sort-of touched on even by the Prime Minister:
‘Today is about three things: realism, determination and hope.’ @David_Cameron #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
And personhood was not completely lost on David Cameron MP:
‘… this is about allowing people to live well with dementia, and with dignity’ @David_Cameron #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
And this was indeed music to the ears of people like me, and countless of persons with dementia, their carers, friends and relatives, for example:
Cameron: It’s not just about finding a cure, it’s also about helping people with dementia to lead more fulfilling lives. #G8dementia
— DeNDRoN (@nihrdendron) December 11, 2013
Elephant in the room according to @marcwort is the number of people with #dementia in developing countries #G8dementia
— Alzheimer Europe (@AlzheimerEurope) December 11, 2013
And the carers were listening carefully too..!
listening for David Cameron to tell us some good news for those living with dementia now #G8dementia
— Dementia Skills (@Dementiaskills) December 11, 2013
There was some concern aired that the volunteers and charities would been seen as a valid alternative for a properly supported health and social care system. Whilst everyone agreed that ‘dementia friends’ and ‘dementia friendly communities’ were worthy causes, everyone also agreed that these should not replace actual care.
Please don’t defer the responsibility to volunteers and charities – health and social care need to step up #G8dementia #DAACC2A
— DAA Carers Action (@DAAcarers) December 11, 2013
Part of the aim of today was to foster of culture of diminishing stigma. And yet the media had been full of words such as ‘cruel disease’, ‘robs you of your mind’, ‘horrific’. So the politicians seem conflicted between this utter armageddon and wishing to destigmatise dementia, with generally pitiful results.
Some of the language in the last 24 hours has indeed been truly diabolical. I took a break to watch the main news item on the BBC, and Fergus Walsh was heading up the main item on dementia with extremely terrifying language.
#G8dementia I was going to keep track of how many times the word “Fight” was used today. I have long since lost count! #militarymetaphors
— Peter Gordon (@PeterDLROW) December 11, 2013
But the Summit kept on reverting to the ‘real world’, pretty regularly though.
A pervasive theme, brought up by many health ministers and other interested parties, was how dementia carers themselves needed supported. Dr Margaret Chan even later in the day spoke about a new online resource for carers, which would be fantastic.
“Dementia carers also need our support.” Dr Chan @WHO #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
‘We’re going to develop an online resource to help carers.” Dr Margaret Chan @WHO #G8dementia This is indeed brilliant news.
— Living Well Dementia (@dementia_2014) December 11, 2013
An aspect of why this situation had arisen was not really explained. Prof Martin Rossor, Honorary Consultant for the Dementia and Cognitive Disorders unit at Queen Square, described the dementia issue as ‘a wicked problem’ on the BBC “You and Yours”. However, Dr Margaret Chan from WHO was much more blunt.
“This is yet another case of market failure.” Dr Margaret Chan @WHO #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
Big Pharma had failed to ‘come up with the goods’, despite decades of trying.
Dr Chan: In terms of a cure (for #dementia), or even treatments that can modify the disorder or slow its progression, we are empty-handed
— WHO (@WHO) December 11, 2013
But few speakers were in any doubt about the societal impact of dementia, though much of the media resorted to scare tactics as usual in their messaging.
London-G8HealthMinisters on dementia. One of the most important challenges for ageing societies.Huge human,social and economic impact.#OECD
— Yves Leterme (@YLeterme) December 10, 2013
The speakers on the whole did not wish to discuss how care for people could be reconfigured. The disconnect between the health and social care systems is clearly a concern in English policy. And indeed this was even raised.
Integrated approach for the delivery of services bridging health and social care is needed, says @yleterme #G8dementia
— Alzheimer Europe (@AlzheimerEurope) December 11, 2013
All was not lost regarding wellbeing.
Hazel Blears, Labour MP for Salford, explained how her mother was living with dementia, so it was vital that policy should do everything it could do to help people live with dementia.
“We need to find the evidence for non-pharmacological interventions as well.” @HazelBlearsMP #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
I met the Salford Institute for Dementia, a brand new Twitter account, for the first time this afternoon, which was in fact one of the highlights of my day.
Salford Institute for Dementia launched to use research to improve the lives of people with dementia #G8dementia http://t.co/BgDw3X9Xw9
— Inst for Dementia (@InstforDementia) December 11, 2013
Although not pole position compared to ‘cures’ and ‘disease modifying drugs’, it was clear that the #G8summit were keen to support assistive technology, telecare and telemedicine. This could be in part due to the generous research grants from various jurisdictions for innovation, or it could be a genuine drive to improve the wellbeing of persons living with dementia.
‘Homecare is arguably one of the best means of care because of quality of life – we should all think of innovative ways to keep ppl at home’
— Anna Hepburn (@AnnaHepburnDH) December 11, 2013
At just before lunchtime, I suddenly “twigged it”.
I must admit I was angry at myself for having been “slow on the uptake”.
I now understand what this ‘data sharing’ drive is about. It’s for DNA genomic collaboration to develop personalised treatment. #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
As it was, the discussion appeared to swing periodically between two ends of an extreme during the course of the day. At one end, the discussion was about ‘big data’ and ‘open data’ sharing.
Vivienne Parry , then said how she preferred the term ‘safe data’ to ‘open data’, but Twitter was at that point awash with queries as to whether a rose by any other name would smell as sweet?
@vivienneparry has hit the nail on the head; ‘unsafe’ data sharing could be perceived as reducing risk for corporate investors. #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
People conceded the need for persons and patients voluntarily to contribute to these data sets, and for international organisations such as WHO to attempt to formulate standardised harmonised templates for these data. At the other end, people were very keen to talk about genetic information, presumably DNA, being the subject of DNA genomics data scrutiny at a personal level.
Also, the discussion itself swung from personal tales (such as Beth Britton’s) to a discussion of looking at societal information as to what sorts of data clusters might show ‘susceptibility’ in their genetic information decades before the onset of clinical dementia. Big data, like 3D printers, has been identified as ‘the next big thing’ by corporates, and it’s no wonder really that big data should of interest to big Pharma corporates.
Having failed spectacularly to have produced a cure or disease-modifying drugs across a number of decades, Pharma are left with two avenues. One is that they look at the individual response to therapy of drugs at a single case level using radio-active binding studies (radio-ligand binding studies), and monitor any slowing of build-up of abnormal protein in the brain as a response to treatment. How much this actually benefits the patient is another thing.
Or Big Pharma can build up huge databases across a number of continents with patient data. Researchers consider this to be in the public interest, but patients are clearly concerned about the data privacy implications.
Here, it was clear that Big Pharma could form powerful allies with the charities (which also acted as patient groups):
“Data sharing is absolutely essential to make the advances needed across the world.” Harry Johns, Alzheimer’s Association #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
And of course this agenda was very much helped by Sir Mark Walport being so enthusiastic about data sharing. Having been at the Wellcome Trust, his views on data sharing were already well known though.
“There are concerns about ‘Big Data’ around the world.” Sir Mark Walport CSO #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
If it were that regulators could allow data sharing more easily, justified presumably on public policy grounds such that freedom of information was more important than data protection according to the legal doctrine of proportionality, this plan could then considerably less risky for corporate investors wishing to invest in Big Pharma.
Andrea Ponti from JP Morgan gave this extremely interesting perspective, which is interesting given the well known phenomena of ‘corporate capture’ of health policy, and ‘rent seeking behaviours’ of corporates.
The G8 have a great opportunity to altering the risk and return ratios, important for investors.” Andrea Ponti @jpmorganfunds #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
It has been argued that waiting for valid consent from the patients would take too long, so presumed consent is more of a practical option. However, this ethically is an extremely tricky argument. The Pharma representatives were very keen to emphasise the ‘free flow’ of data, and the need to ‘harmonise regulation'; but they will be aware that this will requiring relaxing of the laws of more than one country.
And so, during the course of the day, the agenda of Big Pharma became clear. They intended to be tough on the lack of cure for dementia, and tough on the causes of that cure. Some might say, that, as certain anti-dementia drugs come to the end of their patents (and evergreening is not an option), they have suddenly converged on this idea to tackle dementia, as it is a source of profitability to enhance shareholder dividend. They now need new business models to make it succeed (and various charities and research programmes which benefit from this corporate citizenry might be able to make it work too.)
“We have introduced approaches which encourage personalisation and individualisation of care.” Madame Marisol Touraine #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
But during the course of the day those ‘pesky’ tweets about person-centred care kept on coming…
As #G8Dementia summit about to start – see the person not the diagnosis with @SCIE_socialcare award winning film http://t.co/PJ58m6xWB9
— Andrea Sutcliffe (@Crouchendtiger7) December 11, 2013
Some of the tales were truly heart-breaking.
“I lost friends. Well I say friends. If they can’t cope with a diagnosis of dementia, they’re not really friends.” @BethyB1886 #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
But I was happy because Beth was happy at the reception of her film. She is so utterly passionate, and totally authentic, about the importance of her father who had dementia. It was a privilege for us to see how well the film had been received by all there at the #G8summit.
Our montage film, featuring people with dementia & carers (inc me), well received at #G8dementia
— Beth Britton (@bethyb1886) December 11, 2013
And those pesky tweets kept on coming…!
Watch our award winning #SocialCareTV film ‘Getting to know the person with #dementia‘: http://t.co/tivbpYkb8Z
— SCIE (@SCIE_socialcare) December 11, 2013
But indeed there was a lot to be positive about, as research monies if well spent could provide a cure or disease-modifying drugs. Big Pharma and the researchers know that they are not only trying to tackle the big one, the dementia of the Alzheimer type, but also other types such as the vascular dementias, frontotemporal dementias and diffuse Lewy body disease.
EU announces Horizon 2020 call dementia & neurodegenerative disease in 2014/2015 €1.2 billion #G8dementia @isgtw @martinrossor
— DeNDRoN (@nihrdendron) December 11, 2013
Beth’s input today was invaluable.
“I would really like to make a plea, on behalf of the delegates, for non-pharmacological interventions. Thank you.” @BethyB1886 #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
And Dr Peter Gordon loved it!
@bethyb1886 and @HazelBlearsMP well said, both of you. We need balance in our approach. Your voices matter so much #foryourfolk
— Peter Gordon (@PeterDLROW) December 11, 2013
But the best comment of the day must certainly go to Dr Margaret Chan, a V sign to those obsessed with Big Data spreadsheets and molecular biologists looking at their Petri dishes:
‘We’re going to develop person-centred care, not talk about people as collections of organs or diseases’ Dr Margaret Chan @WHO #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
In summary…
It smelt like a corporate agenda.
It looked like a corporate agenda.
It sounded like a corporate agenda.
And guess what?
All the ingredients of ‘corporate capture’ were in attendance: big data, personalised medicine, genomics, data sharing. They’d have managed a full house had the world leaders found a use for 3D printers in all of this.
Related articles
- The G8 Dementia Summit cannot just be about “Pharma-friendly communities” (livingwelldementia.org)
- All stick and no carrot? How much diagnosis, but how much actual care, of dementia? (livingwelldementia.org)
- The #G8Dementia Summit – hopefully a chance for real campaigners, not an international trade fair (livingwelldementia.org)
- Dementia cure ‘within our grasp’, says David Cameron (standard.co.uk)
Is a new sophisticated brain scan desirable to diagnose dementia?
Wouldn’t it be lovely Prime Minister, David Cameron MP, could announce a breakthrough which nails the problem of the diagnosis of Alzheimer’s disease?
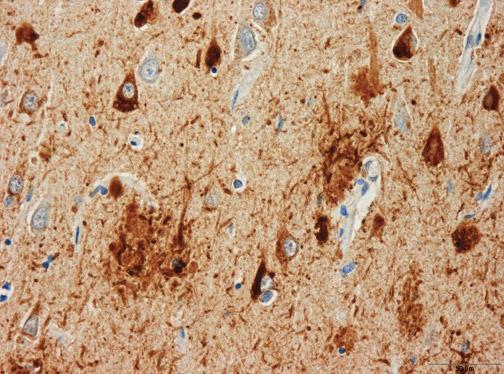
The definitive diagnosis of dementia of the Alzheimer type (DAT) comes post mortem (though in practice various techniques while the patient is alive can be used to tell whether a patient has a type of dementia).
The full armoury of tests includes thinking tests or cognitive neuropsychology, a sample of the fluid from the spine (cerebrospinal fluid), the clinical history and examination of the patient, brain waves (the EEG), or even (rarely) a brain biopsy; that’s even before considering types of scan, like the ‘CT scan’, the ‘MRI scan’, or ‘functional scan’.
The trick of the clinician, varying with levels of expertise, is to make the diagnosis reliably such that a person living with dementia might be able to ‘access’ appropriate care in the system; and those without dementia aren’t given an incorrect label of ‘dementia’.
DAT is one of the hundreds of causes of dementia (although most of the media use ‘Alzheimer’s Disease’ and dementia unhelpfully synonymously.)
Amyloid build-up and the diagnosis
There has been a popular idea that the build up of a substance called amyloid which builds up in the brain might hold the clue to early diagnosis of Alzheimer’s Disease.
In recent years, the emphasis has swung to ‘timely diagnosis’, with the national clinical lead for dementia, Prof Alistair Burns, emphasising that the diagnosis should be made at a time appropriate for the person himself or herself.
A ‘quick fix’ in a test for DAT seems very attractive, but it’s important to remember that the dementia of the Alzheimer type is only one (but the most common) cause of dementia across all age groups.
How to use the test in a safe way
The way in which this diagnosis could be made has also come under scrutiny. A method which uses a radioactive label to which at how much label can bind to abnormal amyloid in the brain, to be practical, should not be excessively time-consuming to administer. It also should not be prohibitively expensive.
Also critically, it should be reliable. In other words, it shouldn’t show up ‘positives’ in otherwise well people, who never go onto develop dementia. A critical problem is that there are many causes of memory loss in older people, including of course depression.
To make things even more complicated, there is a very interesting group of people whose thinking and memory are normal, even late in life, yet their brains are full of amyloid beta plaques that appear to be identical to what’s seen in dementia of the Alzheimer type. How this can occur is an important clinical research question.
Hard plaques made of a protein called amyloid beta are always present in the brain of a person diagnosed with the dementia of the Alzheimer type. But the simple presence of plaques does not always result in impaired thinking and memory. In other words, the plaques are necessary – but not sufficient – to cause DAT.
Is it the type of amyloid which matters?
Earlier this year a paper was published in the prestigious journal in the US (Esparza TJ, Zhao H, Cirrito JR, Cairns NJ, Bateman RJ, Holtzman DM, Brody DL. (2013) Amyloid-? oligomerization in Alzheimer dementia versus high-pathology controls. Ann Neurol. 73(1):104-19. doi: 10.1002/ana.23748. Epub 2012 Dec 7.)
An important clue may come from still come from a form of amyloid beta, but not necessarily in the form of plaques. Instead, smaller molecules of amyloid beta appear more closely correlated with whether a person develops symptoms of dementia; these are called “amyloid beta oligomers“.
Earlier this year, this group developed a way of measuring these amyloid beta oligomers in minute quantities, without binding to similar things.
These amyloid beta oligomers were detected in samples of brain from patients with DAT and nondemented patients with amyloid plaque pathology. However, amyloid beta oligomer concentrations in samples from patients with DAT were tightly correlated with amyloid plaque coverage (correlation very high), but this relationship was weaker in those from nondemented patients (correlation very low) despite equivalent amyloid plaque pathology.
The results raise the intriguing hypothesis that the linkage between plaques and oligomers may be a key pathophysiological event underlying DAT.
This test would be clearly potentially profitable for people who have developed this test, and the critical issue is whether if you scan real patients whether the amount of radioactive binding will reliably distinguish between people with dementia and those without.
Would a new brain scan be helpful?
Looking for amyloid in people who might be developing dementia has been a story going on for ages. The Telegraph newspaper reports a “breakthrough” in a scan, but the description is that of plaques (leading to the possibility of people having lots of plaques found on imaging who later never develop dementia):
“The scan was developed by scientists in London. The test involves giving a patient exhibiting signs of dementia a small amount of a radioactive substance, which will allow amyloid plaques to show up in a brain scan.
The presence of the plaques in the brain is one of the main signs of Alzheimer’s, although it does not make the disease inevitable, so doctors using the test would be sure of giving a patient the all-clear only if the plaques were absent.
It is the first time doctors have been able to detect the plaques while a patient is alive.”
The desire ‘to catch Alzheimer’s early’ – and the actual pitfalls
A major issue is going to be which people should be put forward for such an imaging technique; there has been intense scrutiny of whether bedside tests can reliably tell the difference between people who have a ‘mild cognitive deficit’ and those who have dementia.
A political drive, almost in total parallel led by the current UK and US governments, to “screen” older people for minor memory changes could potentially be leading to unnecessary investigation and potentially harmful treatment for what is arguably an inevitable consequence of ageing. There are no drugs that prevent the progression of dementia according to human studies, or are effective in patients with mild cognitive impairment, raising concerns that once patients are labelled with mild cognitive deficits as a “pre-disease” for dementia, they may try untested therapies and run the risk of adverse effects.
The idea itself that there is a “pre-disease” stage before the full-blown course of the dementia of Alzheimer type is itself erroneous, if one actually bothers to look at the published neuroscientific evidence. A mild cognitive impairment (“MCI”) is a clinical diagnosis in which deficits in cognitive function are evident but not of sufficient severity to warrant a diagnosis of dementia (Nelson and O’Connor, 2008).
However, the evidence of progression of MCI (mild cognitive impairment) to DAT is currently weak. This has been much to the frustration of some researchers where it had been hoped for years that this could be used to identify DAT at an early stage. It might be attractive to think that MCI is a preclinical form of dementia of Alzheimer Type, but unfortunately the evidence is not there to back this claim up at present: only approximately 5-10% and most people with MCI will not progress to dementia even after ten years of follow-up (Mitchell and Shiri-Feshki, 2009).
It’s the post-diagnosis support anyway…
Either way, there should still be adequate post-diagnosis support, which is a problem which simply won’t go away.
Therefore, this result of a ‘breakthrough’, for one of the more common causes of dementia, has to be sufficiently exciting for the drug companies to have a ‘return on investment’ who have developed them.
However, in a week which has seen increasing scrutiny as to whether pharmaceutical-based approaches have been a waste of dawn, particular interest will be paid as to whether this is in fact yet another “false dawn”.
Other references
Mitchell, A.J., and Shiri-Feshki, M. (2009) Rate of progression of mild cognitive impairment to dementia -meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand, 119(4), pp. 252-65.
Nelson, A.P., and O’Connor, M.G. (2008) Mild cognitive impairment: a neuropsychological perspective, CNS Spectr, 13(1), pp. 56-64.
Related articles
- NHS scan to rule out Alzheimer’s (telegraph.co.uk)
- How Brain Scans Might Change the Way Doctors Diagnose Alzheimer s (scientificamerican.com)
- Hardening of Arteries Linked to Plaques in Brain (fightaging.org)
Living well with dementia: diet not drugs?
There is no cure for dementia currently. The available treatment strategies offer mainly symptomatic benefits. Thus, strategies to prevent or delay onset of dementia by changes in lifestyle factors, such as diet, are therefore important, given finite resources. There is no doubt it’d be wonderful if, after many many years of trying, there might be a breakthrough.
But physicians and politicians have a responsibility to the general public to be honest about what is genuinely achievable. It’s in the interests of charities and research groups which depend on income for their research to raise money for a cure; or in the interests of those research groups wishing to raise money for research which appears linked to that somehow. It’s in the interest of Big Pharma-ceutical companies to raise money for their research funds; and they have a legal duty to their shareholders too. The public appreciate a truthful debate about what might work; and where a lot of monies would in fact would be better spent elsewhere.
It’s certainly low hanging fruit for politicians to support this worthy cause.
However, the scant attention to living well with dementia in many statements, in contrast to drug treatments, is very telling. The Department of Health will, however, be livestreaming the #G8dementia summit proceedings later this week. Details are here.
Not all dementia occurs in the elderly. Nonetheless, it is possible that health problems related to aging (including dementia of the Alzheimer type) are projected to add to the high clinical, social, and economic burden of caring for persons with dementia.
The Mediterranean diet has been associated with reduced risk for a wide range of age-related conditions such as stroke, type 2 diabetes, cardiovascular disease, and all-cause mortality. The traditional Mediterranean diet refers to a multinutrient dietary profile characterized by high intake of fruits, vegetables, cereals, and legumes; low consumption of saturated fats with olive oil as the main source of fat; moderate consumption of fish; low to moderate intake of dairy products (in the form of yogurt and cheese); low consumption of red meat and meat products; and moderate amount of alcohol (especially wine) usually consumed during meals.
Recently, a number of peer-reviewed pieces in the reliable academic literature have presented evidence for an association between a Mediterranean-type diet and decreased risk of dementia. Findings from prospective studies suggest that greater adherence to Mediterranean diet may be associated with slower cognitive decline and reduced risk of Alzheimer disease. In the light of these findings, it has been suggested that improving adherence to the Mediterranean diet may delay or prevent the onset of dementia.
A really helpful review was published by Lourida and colleagues earlier this year in the “Epidemiology” journal (Jul;24(4):479-89). Twelve eligible papers (11 observational studies and one randomized controlled trial) were identified, describing seven unique cohorts.
Despite methodological heterogeneity and limited statistical power in some studies, there was a reasonably consistent pattern of associations. Higher adherence to Mediterranean diet was associated with better cognitive function, lower rates of cognitive decline, and reduced risk of Alzheimer disease in nine out of 12 studies, whereas results for mild cognitive impairment were inconsistent.
Published studies suggest that greater adherence to Mediterranean diet is associated with slower cognitive decline and lower risk of developing Alzheimer disease. Further studies would be useful to clarify the association with mild cognitive impairment and vascular dementia. Long-term randomised controlled trials promoting a Mediterranean diet may help establish whether improved adherence helps to prevent or delay the onset of Alzheimer disease and dementia.
Only today, leading doctors warned the Government the battle against dementia should focus on the benefits of a Mediterranean diet rather than ‘dubious’ drugs. In an open letter to the Health Secretary, they said persuading people to eat fresh fruit and vegetables, nuts, fish and olive oil was ‘possibly the best strategy currently available’ for preventing Alzheimer’s and other memory-robbing diseases.
The letter’s signatories include Prof Clare Gerada, the former chairman of the Royal College of General Practitioners, and Dr David Haslam, chairman of the National Obesity Forum.
It reads:
‘We hope this crisis can be seen as an opportunity towards a real policy change, namely towards a Mediterranean diet, rather than towards the dubious benefits of most drugs.’
It goes on to say the evidence ‘strongly suggests’ that improvements to lifestyle will have a ‘far greater effect’ on the rising tide of dementia than drugs.
The call comes as dementia experts from the G8 countries prepare to travel to London for a summit hosted by the Prime Minister.
Dr Simon Poole, the GP who organised the letter, said: ‘It is all about looking at what pharmaceutical companies can do, which is actually not very much.
‘They talk up their medicine and then it is very often a damp squib. We want some sort of focus on prevention. Educating all generations, including our children, in the importance of a good diet in maintaining health in old age is a project which will take years, but is absolutely essential.’
‘We are calling upon policymakers to not only support the care and treatment of those who are already suffering from dementia, but to make significant investments in work which will see benefits beyond the period of one or two parliaments.’
There has also been a focus on individual components of the Mediterranean diet, such as [omega]-3 fatty acids or olive oil as the main source of monounsaturated fats. Although the advantages of Mediterranean diet are relevant for non-Mediterranean populations, it is often argued that studies are not always comparable because there are substantial differences in dietary composition among countries.
A more detailed examination reveals this is perhaps especially true for fatty acids. Although olive oil is the hallmark of Mediterranean diet, differences in the origin of monounsaturated fats or cooking style (eg, baked vs. fried) could partly explain these inconsistencies. Studies comparing types of olive oil concluded that compared with refined oil, virgin olive oil (rich in phenolic content) has additional anti-inflammatory and antioxidant properties beneficial to cellular function and cardiovascular health.
The Mediterranean diet may exert its effects on cognitive health through multiple biological mechanisms. Relationships with reduced risk of coronary heart disease, hypertension, diabetes, dyslipidemia, and metabolic syndrome have been observed, and these conditions have also been associated with mild cognitive impairment, vascular dementia (a dementia associated with general factors affecting the cardiovascular system such as smoking, cholesterol, diet, family history), or disease of the Alzheimer type.
Sticking to this Meditteranean diet may also facilitate metabolic control because it has been related to improved insulin sensitivity and glucose metabolism. Insulin is a chemical acting in the body which can affect our metabolism – it is an important “hormone” for us.
Furthermore, “oxidative stress” increases with age and results in “oxidative damage”—a state often observed in the brain of patients with Alzheimer disease. Typical components of the Mediterranean diet (namely fruits, vegetables, wine, and virgin olive oil) are rich in antioxidants such as vitamin C and E, carotenoids, and flavonoids. Decreased oxidative stress found in people adhering to a Mediterranean-type diet could partially explain their lowered risk for dementia.
And there’s a plausible biological mechanism for all this. Brain cells (neurone) are protected against oxidative stress by specialist chemicals, called “neurotrophins” (basic proteins) such as the brain-derived neurotrophic factor. There is some evidence that Mediterranean diet may increase plasma brain-derived neurotrophic factor concentrations. Inflammatory processes have also been suggested for Alzheimer pathogenesis. Higher concentrations of C-reactive protein, a nonspecific marker of inflammation, have been associated with increased risk for cognitive decline, Alzheimer disease, and vascular dementia, whereas better adherence to Mediterranean diet has been associated with lower levels of C-reactive protein.
Access to medicine has become a really important issue in the NHS. Already we are getting stories of rationing in the NHS emerging during the period of this Government (such as varicose veins stripping), so it is not particularly surprising if drugs which do have modest effect on memory for dementia are not a top priority. Encouraging people to learn about diet and how this might prevent thinking problems is therefore a worthy aim, as it might actually work better than many of the drugs ‘on offer’. Senior doctors have advised this approach in fact.
Just because it’s not coming from Big Pharma with their massive marketing budgets doesn’t mean it’s a dead duck.
Related articles
- Healthy diet ‘may prevent dementia’ (skynews.com.au)
- Mediterranean Diet is the Key to Preventing Dementia (medindia.net)
- How To Live Longer: Mediterranean Diet Proven To Help Women Live Past 70 (medicaldaily.com)
- Dementia fight must focus on diet, say experts (yorkshirepost.co.uk)
The #G8Dementia Summit – a curious lack of a person-centred approach in the research strategy
David Cameron should be given credit for making ‘dementia’ the topic for discussion of the G8 on 11th December 2013. But the event runs the risk of being a trade fair for the pharmaceutical industry, becoming increasingly desperate to prove their worth in dementia and society.
However, it is widely acknowledged that cholinesterase inhibitors, drugs that boost levels of acetylcholine in the brain to improve attention and memory, have a modest effect if that in the majority of patients with early dementia of the Alzheimer type (‘dementia of the Alzheimer type’). There is no robust evidence that they slow down disease progression in humans from human studies of patients.
Many senior academic experts feel conversely that there has been insufficient attention put into interventions that actually do help people to live well with DAT. Such interventions include improving the design of the home, design of the built environment (including signage and pavements), non-statutory advocacy, dementia-friendly communities, assistive technology and ambient living innovations.
On Wednesday 4th December 2013, a ‘research summit’ was held for the press for “research into dementia”. The main focus of this research summit was how can one best predict who will get dementia or when, do we even know what causes dementia yet, what “cures” are there in the pipeline, what can be done to prevent dementia, what obstacles are pharmacological researchers facing, does Pharma have sufficient resources, and what needs to be done to make the Dementia Summit a success.
The focus of this ‘summit’ into ‘research into dementia’ was not living well with dementia, which is a gobsmacking tragedy for all those involved in promoting living well with dementia.
What is overwhelmingly absent is a ‘person centred approach’ which has been a major force for good in contemporary dementia care in England.
The panel members, according to the brief, were: Dr Doug Brown, Director of Research and Development, Alzheimer’s Society; Prof Nick Fox, Professor of Neurology, MRC Senior Clinical Fellow, Institute of Neurology, University College London; Prof Simon Lovestone, Professor of Old Age Psychiatry, Director of NIHR Biomedical Research Centre for Mental Health at the South London and Maudsley NHS Trust and Institute of Psychiatry, King’s College London and Lead for the Translational Research Collaboration in Dementia (a network of 6 centres established by the NIHR); Prof Peter Passmore, Professor of Old Age Psychiatry, Queen’s College Belfast and Lead for Dementia for The British Geriatrics Society; and Dr Eric Karran, Director of Research, Alzheimer’s Research UK.
To show how little there was on wellbeing, and discussing innovative ways to allow people to live well with dementia, here’s the official write up from the BMJ this week:
“Nick Fox, professor of neurology and a Medical Research Council senior clinical fellow at the Institute of Neurology at University College London, said, “We should be asking the G8 collectively to double the research spending on dementia within five years.
“And I think there is a lovely equitable way of looking at this. We ask the G8 countries to commit 1% of their dementia costs to add another doubling of research spending within 10 years.”
Brown said the aims of the research were to enable more accurate and timely diagnosis of dementia; to create disease modifying treatment to try to stop, slow, or reverse the condition; and to find drugs to treat the symptoms. Most importantly, he said, researchers needed to understand how dementia developed to enable the risk to be reduced and onset of dementia to be prevented or at the very least delayed. “If we could delay the onset by five years we could probably cut the numbers of [people with] dementia in half,” he said.
Fox said that past trials of treatments had concentrated on people with symptoms of the disease, which was “like trialling chemotherapy when people are already in a hospice.” Now, he said, treatments were beginning to be tested in people who were at higher risk of dementia because they had a family history or other genetic risk factors or because scans had shown early features of the disease.
Scans and other techniques could then be used to track the effects of treatment before symptoms appeared. “Only if we can identify people where we can see whether our therapies are having an effect will we ever make progress,” Fox said.
Peter Passmore, professor of old age psychiatry at Queen’s College Belfast and the British Geriatrics Society’s lead on dementia, said that as more was known about the mechanism of dementia, researchers were looking at drugs licensed for other conditions that might impinge on those mechanisms. “That’s cheaper drug development: those drugs are off patent,” he said.”
Many thanks to @sam4wong for sharing this with us on Twitter this morning.
Sadly, this representation of research for #G8dementia has taken on more of an appearance of a corporate international trade fair, which is a crying shame. This is, ironically, in the week that the World Trade Organization has apparently agreed its first-ever global deal aimed at boosting commerce.
A trade fair (trade show, trade exhibition or expo) is an exhibition organised so that companies in a specific industry can showcase and demonstrate their latest products, service, study activities of rivals and examine recent market trends and opportunities. In contrast to consumer fairs, only some trade fairs are open to the public, while others can only be attended by company representatives (members of the trade, e.g. professionals) and members of the press, therefore trade shows are classified as either “Public” or “Trade Only”. However, the G8 next week would be at considerable risk of being hijacked by market forces, if it were not for the valiant efforts of the Department of Health and people who have devoted their lives to raising dementia awareness too. Trade fairs are helpful for marketing of products to a wider audience.
James Murray-White (@sky_larking) is a film-maker, and campaigns perennially for raising dementia awareness. James announced yesterday that he was proud to be part of a central network of dementia ‘activists’ on Twitter, but had just reported on the same media network that he had recently been refused ‘press accreditation’ for #G8dementia.
Earlier this year, filmmakers and scientists came together at this event to increase the public understanding of dementia. This event comprised series of short films about dementia, curated by Murray-White, will precede a discussion with researchers from the University of Bristol and other institutions supported by @AlzheimersBRACE, a local charity that funds research into Alzheimer’s disease and other forms of dementia. Panel speakers included: Professor Seth Love (Professor of Neuropathology); Laura Palmer (South West Dementia Brain Bank Manager); James Murray-White (filmmaker).
However, all is not lost, by any means. Beth Britton (@BethyB1886) will be participating in a short film for #G8dementia. Prof Alistair Burns (@ABurns1907), the Clinical Lead for Dementia in England, has written of Britton:
“Beth Britton has been a breath of fresh air in the discussions and debates around dementia. She brings a clarity of thought and originality of ideas which I have always found very refreshing and helpful when considerations and discussions of the importance of people with dementia and their carers are concerned. She has a unique writing style and a gifted ability to convey ideas and experiences”
Beth is one of the U.K.’s leading campaigners on dementia. Her experience of supporting her father, who was living with dementia, and her professional background, give her unparalleled insight into effective ways of campaigning for change, it is widely felt.
There are people who are simply interested in individuals with people – the person not the drug. For example, Lucy Jane Masters (@lucyjmasters) is a dementia nurse specialist, advocating for change, an educator, and primarily passionate about that person with dementia and those who care for him or her.
Alistair has for long time emphasised the importance of “a timely diagnosis”, rather than an “early diagnosis”. This is very much in keeping with the notion that the potential diagnosis should be offered at a time personally appropriate to any particular individual. Alistair also believes, in his rôle as part of NHS England, that there should be a reasonable level of “post-diagnosis support”. Academics generally agree that the tenure of Alistair as the National Lead for Dementia in England has been a very successful experience for all involved.
There are few people as inspirational too as Norman McNamara, who has campaigned tirelessly to dissolve the stigma which can surround dementia. He can be very easily found on Twitter for example (@NormanMcNamara). McNamara has written poignantly about his own personal experiences of ‘living with dementia’.
Sally (@nursemaiden) was a senior nurse, but likewise now promotes heavily wellbeing in dementia, with her father with dementia of the Alzheimer type having passed away on 1st September 2012.
And it truly is an international ‘effort': Kate Swaffer (@KateSwaffer) in Australia – who has just met up with Gill Phillips who advocates ‘paths to personalisation’, has written brilliantly about her experiences of the dementia diagnosis.
Indeed, it would not be hyperbolic to say that many people have given up much free time into the world of the dementias, as a vocation. Lee (@dragonmisery) has produced an incredible information provision website for carers of people with dementia, and this has advanced the policy plank promoting choice and control in wellbeing.
Twitter has been particularly successful at giving people a voice at last. Charmaine Hardy (@charbhardy) is one of the most prominent members of this very close community. Her profile reveals that her husband, whom she adores, has a rare dementia known as primary progressive aphasia. Anyone following Charmaine knows exactly the emotional intensity of someone caring for somebody with dementia.
Likewise, Thomas Whitelaw (@TommyNTour) has literally been ‘on tour’ talking with amazing authentic emotion, affectionately, about his mother, Joan Whitelaw, who had been living with dementia.
So why such a focus on pharmacology?
Why so little on ‘person centred care’?
This glaring omission of person centred care in #G8 dementia apart from representations below is utterly embarrassing and humilating for the thousands of researchers and practitioners who work in this area. @MrDarrenGormley‘s award-winning blog is a most useful introduction to this area.
And, although deeply enmeshed in the English health policy which has sometimes been far from controversy, the efforts of the Department of Health itself have been most impressive.
Anna Hepburn (@AnnaHepburnDH) is Digital Communications Manager for Social Care at the Department of Health. Anna is well known to be genuinely interested in the views of people living with dementia, and those closest to them.
Anna remarked recently,
“When people with dementia and their partners were invited to the Department of Health recently, there was one simple statement that stuck in my mind: “We are still people”. It came as a bit of a shock coming from one of the articulate and funny people gathered round the table. But it says it all about the misconceptions and stigma surrounding dementia.”
Anna Hepburn continued,
“On 18 November, I had the privilege of meeting more people with dementia, as well as current and former carers of people with dementia, who came to London to make short films to show at the G8 dementia summit. This is so we can bring their voices – and the reality of dementia – into the room on 11 December.”
But as a result of the research summit and other efforts from the media and select researchers, the headlines have been rather sensational and sadly all too predictable, viz:
“Unprecedented breakthrough in the hunt for a dementia drug within ‘five years'” (Independent)
“G8 ministers warned to prepare for global dementia ‘time bomb’” (Times)
“Monthly injection to prevent Alzheimer’s in five years” (Telegraph)
“Jab to slow Alzheimer’s ‘is just five years away': Monthly treatment could be given a decade before symptoms” (Daily Mail)
“Dementia cases ‘set to treble worldwide’ by 2050” (BBC)
The last one has been the most difficult for real experts in the research community with real knowledge of the problems facing international research.
On the other hand, Mr Jeremy Hughes, chief executive of the UK’s Alzheimer’s Society, according to that final BBC report cited above, said: “Dementia is fast becoming the biggest health and social care challenge of this generation.”
“We must tackle dementia now, for those currently living with the condition across the world and for those millions who will develop dementia in the future.”
There has been much media interest in improving diagnosis rates in England, driven more by the dementia charities than public health physicians or GPs. Whilst undoubtedly a ‘cure’ for dementia would be wonderful, it is rarely reported that dementia rates are in fact considered to be dropping. Medical doctors such as Dr Peter Gordon (@PeterDLROW; a NHS Consultant Psychiatrist) and Dr Martin Brunet (@DocMartin68; a NHS General Practitioner) have been invaluable as “thought leaders” in forging ahead with an evidence-based approach to this complex issue, cutting through the media garb and spin (and promotional copy).
Very recently in the prestigious New England Journal of Medicine, it was reported that, “Although demographics will drive an increase in the number of dementia cases, recent reports — generally based on population-based community studies or survey data — point to declining age-specific prevalence or incidence rates among people born later in the first half of the 20th century”
You can follow live digital coverage of the G8 dementia summit on the Dementia Challenge site on 11 December 2013. Well done to all those involved, particularly the grassroots campaigners, Anna Hepburn, and the Department of Health!
Background to the world of assistive technology
It is widely propagated in the media that the two major drivers for ‘increased costs of caring’ for the National Health Service (NHS) comprise the ageing population, as well as the increasing rôle that technological advances will play. Both factors are of course subject to ferocious debate regarding the economic sustainability for the NHS, but certainly one potent myth is that assistive technologies are always expensive. This is not true, and the field of assistive technologies is ever expanding.
David Gems (2011) argues that gerotechnology is at the heart of living well in the context of aeing:
[Another] goal of research on ageing is to improve the health of older people. Here, biogerontology is akin to other biomedical research topics, sharing with them the goal of understanding the biological mechanisms that underlie pathology. The particular value of such understanding is that it enables the development of therapeutic treatments, leading to improved health and wellbeing.
A formidable challenge still remains in the relative lack of evidence for pursuing good design principles as well as assistive technologies in improving living well with dementia. For example, the National Dementia Strategy (2009) provides the following.
The evidence base on design principles is sparse, but there is consensus on key principles and a number of good practice checklists are available. There is a more substantial evidence base to show the opportunities offered by assistive technology and telecare to enable people with dementia to remain independent for longer, and in particular to help the management of risk. But the data on newer approaches are still sparse and inconclusive. An evaluation of one scheme demonstrated cost effectiveness and reports of improved quality of life. Large-scale [Department of Health] field trials of such technology are currently under way.
Dementia conditions have the potential to make day-to-day life more difficult. It is clearly very difficult to ‘know’ what an individual feels in terms of his or her wellbeing, even if he or she is unaffected by dementia, even though a conceptual framework of general consciousness is now under way (see, for example, Crick and Koch, 2003). Indeed, as Greenfield (2002) explains, the relationship between the words ‘consciousness’ and ‘mind’ merit attention.
Emotions play a critical role in the evolution of consciousness and the operations of all mental processes (Izard, 2009). Little things like mislaying keys, forgetting to turn off the taps or leaving the gas unlit can prove frustrating or even create hazards.
Orpwood (2007) has argued that mechanisms underlying consciousness and qualia are likely to arise from the information processing that takes place within the detailed micro-structure of the cerebral cortex. It looks at two key issues: how any information processing system can recognise its own activity; and secondly, how this behavior could lead to the subjective experience of qualia. In particular, it explores the pattern processing capabilities of attractor networks, and the way that they can attribute meaning to their input patterns and goes on to show how these capabilities can lead to self-recognition. That paper suggests that although feedforward processing of information can be effective without attractor behaviour, when such behaviour is initiated, it would lead to self-recognition in those networks involved. It also argues that attentional mechanisms are likely to play a key role in enabling attractor behaviour to take place.
There has become a growing feeling that ‘assistive technologies’ (AT) may provide more support for the carer than for the individual with dementia (Kinney et al., 2004), or to ease service provision. However, there have been some noteable exceptions to this focus on security and safety, such as the work of Topo and colleagues (Topo et al., 2004) on the enjoyment of music, and Alm and colleagues (Alm et al., 2005) on general reminiscence.
However, the influence of engineering on the quality of life research has come to a fore in most recent years (for example Orpwood et al., 2007). The INDEPENDENT study has been specifically aimed at designing technology to support quality of life. This collaborative project involved academic engineers, social scientists and architects, together with representatives of user groups and a manufacturer. The design work was based on a comprehensive user survey in which people with dementia themselves highlighted the factors which affected their quality of life. These data were analysed through a series of multidisciplinary workshops through the whole consortium.
There have been, nonetheless, a number of concerns raised about the assistive technology. Roger Orpwood submitted the following comment to the consultation held by the Nuffield Council on Bioethics summarised in ‘Dementia: ethical issues’ between May 2008 and July 2008.
Care professionals often express concern about the use of assistive technology because they see it as something to replace human care. There is no doubt that there is a real danger that some purchasers may see it in this way, either to save money on the part of local authorities, or to reduce the need for direct support on the part of relatives. Those of us involved in developing such equipment see it more as augmenting human care rather than replacing it. However there are some things technology can do that is better than human support. It doesn’t get tired or frustrated, it can operate 24 hours a day, and it clearly doesn’t get upset by the behaviour of the person with dementia. There is evidence from our own work that technology can provide a much clearer picture of how the user is getting on than can care staff. Our last client in London had a major sleep problem that no-one had picked up, but as soon as our sensor network was turned on the problem shouted at us. So technology has an important role to play, and can do some things better than human carers, but it cannot be a replacement for human care, and all the expression of feeling, empathy and understanding that humans can provide. There are major ethical concerns if it is viewed as a replacement.
Suggested readings
Crick F, Koch C. (2003) A framework for consciousness, Nat Neurosci, 6(2), pp. 119-26. [Review.]
Department of Health (2009). Living well with dementia: A NationalDementia Strategy: Putting people first, London: Her Majesty’s Stationery Office, available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/168221/dh_094052.pdf
Gems, D. (2011) Tragedy and delight: the ethics of decelerated ageing, Philos Trans R Soc Lond B Biol Sci, 366(1561), pp. 108-12.
Greenfield, S. (2002) Mind, brain and consciousness, British Journal of Psychiatry, 181, pp. 91-93.
Izard, C. (2009) Emotion theory and research: highlights, unanswered questions and emerging issues, Annu Rev Psychol, 60, pp. 1-25.
McKinney, K.M., Kart, C.S., Murdoch, L.D., and Conley, C.J. (2004) Striving to provide safety assistance to families of elders: the SAFE house project, Dementia, 3, pp. 351-370.
Nuffield Council of Bioethics. (2009) Dementia: ethical issues, available at: http://www.nuffieldbioethics.org/sites/default/files/Nuffield%20Dementia%20report%20Oct%2009.pdf.
Orpwood, R. (2007) Short communication: neurobiological mechanisms underlying qualia, Journal of Integrative Neuroscience, 6(4), pp. 523–540.
Topo, R., Maki, K., Saarikalle, K., Clarke, N., Begley, E., Carhill, S., Arsenlind, J., Holthe, T., Morbey, H., Hayes, K., and Gillard, J. (2004) Assessment of music-based multimedia program for people with dementia, Dementia, 3, pp. 331-350.
I am taking my 11000 Twitter followers all the way in promoting wellbeing in dementia
I am taking my 11000 followers on Twitter (@legalaware) all the way in engagement over the G8 ‘dementia summit’.
Anna Hepburn at the Department of Health will be spearheading implementation of its own digital strategy on 11 December 2013, which I am looking forward to enormously (here).
A friend of mine is a prominent campaigner for dementia. He lives with a type of dementia which is quite common in a certain age group.
I was aghast when he said this week he had attended a clinical commissioning group meeting, but had faced stigmatising language about dementia. The leader of that meeting had referred to someone having ‘a bit of dementia’. My friend was not impressed, but politely wrote to him afterwards. The leader replied with dignity.
But this for me epitomises the uphill battle those of us who genuinely care about dementia really face.
My baptism of fire into the world of dementia is when I did cognitive assessments in Cambridge of patients with frontal dementia, for Professor John Hodges who was chair of behavioural neurology at the time.
Since then, and bear in mind that this is more than ten years ago, I have firmly believed that there is no more important voice than the person with dementia.
Also, it has become apparent to me that there are many in the caring professions, including of course carers who confront challenges to their own health. It seems that they also are expected to tiptoe with effortless ease through the maze of the law and finance, as well as information about the condition itself.
Sure, the drive for a ‘cure’ and ‘better treatments’ for dementia as a ‘key priority’ from the Alzheimer’s Society (their press release on the ‘G8 summit’) is a worthy and commendable one. However, individuals with dementia and the people who are close to them need to have realistic expectations about what the drugs can do – and what they can’t do.
There are invariably going to be pressures on English policy in dementia policy, and dementia itself has to compete with a finite pot of resources compared to other very important long term conditions (such as chronic obstructive airways disease).
In the absence of a magic cure for the more prevalent types of dementia, such as dementia of Alzheimer type, I believe a huge amount of effort morally must be put into improving the quality of life of those loved ones with dementia.
I particularly admire Beth Britton for her work in dementia. Beth on her blog produces a clear first-hand precious witness of her father, whose journey of vascular dementia was for around 19 years. I had the good fortune to meet Beth, Gill Phillips (the force behind the ‘Whose Shoes‘ tool) and Kate Swaffer recently when Kate was visiting from Oz. Kate’s blog on personal experiences of living with dementia is a candid tour de force. Both Beth and Kate have reasonable expectations from society of its reaction to people living with dementia. Their voices have to be heard clearly through the noise of the system.
These are examples of genuine people, who care. Their passion for explaining the importance of the person is authentic. It’s real.
I am nearly 40, and I realised a few years ago that anything can happen to anybody at any time. This crisis of insight occurred precisely at the moment when I woke up from a six week coma in a London NHS Trust, as I had contracted meningitis. It’s how I became physically disabled.
When I studied medicine for all of six years at Cambridge, and did my postgraduate studies in London, I had never heard of Tom Kitwood. Kitwood was, however, remarkable for revolutionising the way we think about dementia.
@PeterDLROW @legalaware @val_hudson @alzheimerssoc @bethyb1886 Kitwood is at the foundation of all thats right about #dementia care
— Lucy Jane marsters (@lucyjmarsters) November 23, 2013
Medics are transfixed on their medical model, but Kitwood put the person in pole position in dementia care. This is extremely potent, corroborated in subsequent policy from SCIE on personalisation and person-centred care. I have indeed devoted a whole chapter to it in my book ‘Living well with dementia’.
Policy makers owe a debt they can never actually repay from people with dementia (such as Norman McNamara) or people who have come up close with dementia (such as Tommy Whitelaw and his late Mum Joan, whom Tom clearly adored).
In a closely-knit group of #dementiachallengers, @charbhardy is also “first amongst equals”! As Charmaine’s Twitter profile says, she is a carer to her husband with ‘PPA’.
PPA is primary progressive aphasia, a rare type of dementia. All the dementias have specific needs.
Charmaine’s poppy is even on the front cover of my book, with kind permission of course! You will see some striking pictures of sterling gardening when you visit her Twitter profile. The flowers at the top of this blogpost are hers.
My book completely rubbishes the view that nothing can be done to help individuals with dementia. Quite the reverse.
A lot CAN be done; whether this is improving the design of the personal home, care home, or ward; improving the outside environments such as paving; improving adaptations and technologies for the home; improving advocacy for people with dementia and their carers; improving networks and social inclusivity (through even the social media); promoting dementia friends and dementia-friendly communities (even banks); encouraging debate (e.g. through Mr Darren Gormley’s excellent blog.)
Or it might include improving information for persons with dementia or their carers. See for example Lee’s “Dementia Challengers” resource which shows ‘choice’ to be more than some minor policy whim; it’s a real thing which can help people to live successfully with dementia.
There is therefore a huge deal which could and should be done.
However, the system is like a giant oil-tanker where it’s really hard to change direction. Beth Britton’s blog is amazing – I can’t praise it highly enough. This, however, upset me about how Beth’s own father had been treated (from a blogpost of Beth from 6 November 2013, entitled “Does the world really stop?”):
I lost count of the young doctors who saw my dad during his 19 years with dementia and questioned the point of treating a man who a) had a terminal disease, b) was immobile (as dad was for many years), c) doubly incontinent, d) had a swallowing problem (for the last four years of his life) and e) apparently in their narrow-minded judgement, had no quality of life whatsoever.
And this was Sally‘s experience (from the Foreword from my book):
Dementia of Alzheimer type destroyed his brain so badly that my father was unable to feed himself, mobilise, or verbalise his needs. He became totally dependent on my mother 24/7. As the condition advanced, my father became increasingly frail, with recurrent chest infections due to aspiration from swallowing difficulties. Each time the GP would be called out, antibiotics prescribed, and so the cycle would begin again. As a nurse, I wanted to see proactive management of my father’s condition. The system locally, however, was quite unable to provide this service. I feel that the dementia of Alzheimer type is a terminal condition, and, as such, should be treated like other similar conditions in care models. What we instead experienced was a “reactive “system of care where the default option was admission to hospital into an environment where my father would quickly decline.
I am lucky as I work closely with international people of the highest calibre around the world; we have a real focus on trying to witness the quality of life resulting from policy, researching it, and doing something about any shortfalls.
Through my 11000 followers, I am hoping to take some people, from all parts of society, on this journey with me. ‘Dementia is everybody’s business’, as this excellent badge from Lucy Jane Marsters shows.
I hope very much you’ll be inspired by Beth, Gill, Kate, Lee, Lucy Jane, Norman, Sally, and Tommy and others to make dementia your concern too. It’s the type of society we all have a stake in and we should not be afraid to learn from brilliant members of society who happen to live with dementia.
Foreword by Prof John Hodges
This is the Foreword to my book entitled ‘Living well with dementia‘, a 18-chapter book looking at the concept of living well in dementia, and practical ways in which it might be achieved. Whilst the book is written by me (Shibley), I am honoured that the Foreword is written by Prof John Hodges.
Prof Hodges’ biography is as follows:
John Hodges trained in medicine and psychiatry in London, Southampton and Oxford before gravitating to neurology and becoming enamoured by neuropsychology. In 1990, he was appointed a University Lecturer in Cambridge and in 1997 became MRC Professor of Behaviour Neurology. A sabbatical in Sydney in 2002 with Glenda Halliday rekindled a love of sea, sun and surf which culminated in a move here in 2007. He has written over 400 papers on aspects of neuropsychology (especially memory and languages) and dementia, plus six books. He is building a multidisciplinary research group focusing on aspects of frontotemporal dementia.
The car crash interview of a Trustee of the King’s Fund about potential payments for the NHS
The political parties have two strands of consensus which at first blush may seem somewhat irreconcilable: a NHS which is universal, and free-at-the-point-of-need, and £15-20 ‘efficiency savings’ within the next few years.
Taxes could rise to increase the size of the public expenditure pot. thereby generating additional funds to flow into public funding for healthcare. There does not seem to be any political appetite for this approach at the moment. While technically possible (tax levels are far higher in Nordic countries than in the UK), this is unlikely to provide an answer in the short term.
The NHS is heading for a “breakdown” if people expect it carry on providing all services for free under increasing demand, the former head of Marie Curie Cancer Care has warned.
Sir Thomas Hughes-Hallett urged us to ‘take more responsibility’, encouraging us to think about what we ‘really need for free'; he gave his view of how to keep the NHS on the road, saying it should – like a a garage – charge “for extras”.
He said people “need a sat-nav” to point them what is “most convenient”, towards chemists or community support centres and “steer them away from the NHS when they don’t need it”.
He further added that people should treat their bodies like a car, with a regular MOT, and that “we need to take more responsibility for our own health”.
Hughes-Hallett, a trustee of the King’s Fund, and Executive Chair of the Institute of Global Health Innovation at Imperial College, London, predicted: “We need to make tough choices for now about what we really need for free”.
Unfortunately, Sir Thomas was a guest on Wednesday’s Daily Politics today, and his defence of his own argument was worse than pitiful as you can see here (at 1 hr 29 minutes).
Andrew Neil started the discussion by enquiring off Hughes-Hallett where he “would draw the line”, mooting gastric banding, acupuncture, and varicose veins.
For fertility treatment, he said: “there is no yes or no answer.”
Neil then replied that some difficult questions would have to be answered.
Alan Duncan MP said: “It’s free-at-the-point of need and that’s not going to change…. but for the mainstream medical needs, that’s not going to change.”
Vernon Coaker MP said: “This is the thin-end-of-the-wedge. The whole point of the NHS is that’s free-at-the-point-of-use, and if you start charging, you’re going to end up with a two tier service, and the poor will be disadvantaged.”
Hughes-Hallett claimed: “Many people are willing to pay.”
The NHS could start to draw in funds from other sources, such as co-payments and supplementary insurance. Again, these could potentially start to challenge existing views on equity, because they inevitably introduce an element of some kind of payment to access services. Exemptions and subsidies can mitigate this to some extent, but the more they are used, the more they offset the expenditure benefits of alternative sources of funding in the first place.
In a recent view, the departing CEO of NHS England said that the introduction of co-payments, imminently, was “unlikely”.
A question still remains over how to deal with services that fall outside the defined core package. If they are significant in the eyes of patients, markets will develop to cover those services, funded either through fee for service or insurance-based mechanisms.
On the one hand, the development of such a market might be regarded as undermining equity (some in society will be able to pay to access health services that are not freely available to all). Others will interpret it as a natural market response that is neither desirable nor sensible to prevent — what matters is ensuring that the core package of services that is available to all is adequate.
It cannot be denied, however, that a growing number of people feel that the marketisation of the NHS has gone far too far.
In fact, many want the market abolished altogether now.
The Knowledge
In this blogpost, I won’t mention the “cab rank rule”, though I will devote the content of this blogpost to the characteristics of the London cabbies. In a nutshell, I think London cabbies are absolutely brilliant! I’m in an unusual situation of virtually having to use up all my quota of journeys in a fortnight. I am given a set number of journeys per year, and I’ve been going to and from Primrose Hill and the St Mary Axe and Holborn sites all year using a private hire cab. It costs me a huge amount of money, but now I have the luxury of spending my ‘ComCab’ card all at once as I’ve saved up so many journeys.
As a profession, I really admire London cabbies who are far superior to private hire cab drivers. It’s not that often they better nous than a satnav; take for example the cabby who avoided Euston Road tonight because of gas works and took me down Hampstead Road to avoid us being stuck in traffic for many minutes. I am talking about the two attributes which they seem to have, as a result of having survived “appearances”. Firstly, I understand examiners weed out any candidate who is prepared to lie to a candidate with questions like ‘Are you sure?’ Cabbies have told me it’s always best to acknowledge when you’ve reached the limits of your knowledge, and simply say when you don’t know something, even though customers like certainty. Secondly, examiners ensure that future cabbies are not easily wound up by the general public by asking provocative questions sometimes, I hear.
You can see how both attributes would be sought after in a City lawyer too…
The next London #tweetup
People will remember that I enjoyed very much the last legal #tweetup that I attended. The next ‘do’ will be at The Old Bank Of England, 194 Fleet Street, London, UK. London TweetingLegals (organised everytime successfully by Shireen Smith of Azrights – personal website of Shireen) is a regular meet-up in the capital to connect lawyers and related professionals, and law bloggers together. Azrights was set up to provide good value Intellectual Property (IP) focused, IT, and Internet law services of high-quality. It is dedicated to providing the innovations the market needs. These are indeed challenging times for professional legal services firms, and the alternative business structures, and the stakeholders within them, as well as, of course, clients, customers, and the general public.
Shireen has a very relevant post here, how lawyers should perhaps position themselves in the new deregulated market.
Are lawyers getting it right giving free advice to prospective clients to impress them with their lawyering skills
For more information contact Shireen Smith, of Azrights info@azrights.co.uk,
To come along, please go to this page. The event is on September 26th, roughly between 6.30 and 9 p.m.