Home » Posts tagged 'cultural change'
Tag Archives: cultural change
Change
Somebody once advised me in my 20s that destiny is when luck meets preparation.
When I was younger, I used to think that you could prepare yourself out of any situation. But wisdom and events proved me wrong. I soon discovered that what you did yesterday though can affect today, and what can affect today can affect tomorrow. The only thing you can predict pretty comfortably, apart from death and taxes, is change. When I was younger, I used to think I could live forever. All this changed when I woke up newly physically disabled, after a six week coma on a life support machine on the Royal Free Hampstead. The National Health Service saved my life. Indeed, the on call Doctor who led the crash team the day of my admission, when I had a cardiac arrest and epileptic seizure was in fact a senior house officer with me at a different NHS trust in London.
This feeling of solidarity has never left me. I do also happen to believe that anything can happen to anybody at any time. I studied change academically in my MBA in the usual context of change management and change leadership. It’s how I came to know of Helen Bevan’s work. I’ve thought a lot about that and the highly influential Sirkin paper. But I don’t think I honestly ‘got‘ change until this year. In 2007, I was forced to change, giving up alcohol for life. I realised that if I were to have another drink ever I would never press the off switch; I would either end up in a police cell or A&E, and die. This is no time for hyperbole. It was this forced change, knowing that I had an intolerance of alcohol as serious as a serious anaphylactic shock on eating peanuts, that heralded my life in recovery. I later came to describe this to both the legal regulator and the medical regulator as the powerful driver of my abstinence and recovery, rather than a ‘fear based recovery‘ from either professional regulator.
But I feel in retrospect my interpretation of this change, as due totally to an externality, is incorrect. As I used to attend my weekly ‘after care’ sessions with other people newly in abstinence from alcohol or other toxins, or from gambling, or sex, I discovered that the only person who can overcome the addiction is THAT person; and yet it is impossible to read about this path of recovery from a book, i.e. you can’t do it on your own. So ‘command and control’ is not the answer after all. Becoming physically disabled, and a forced change of career and professional discipline, and a personal life which had become obsessed by alcohol, meant I had no other choice. I had to ‘unclutch’ myself gear-wise from the gear that I was in, and move into a different gear. But I did find my new life, living with mum, and just getting on with my academic and practitioner legal and business management training intensely rewarding.
In 2014, I attended a day in a hotel close to where I live, in Swiss Cottage. One of the speakers was Prof Terence Stephenson. After his speech, I went up to thank him. I found his talk very moving. He was later to become the Chair of the General Medical Council (GMC). I was later to become regulated once again by the GMC. Two lines of his has kept going through my mind repeatedly since then. The subject of the day was how sick doctors might get salvation despite the necessary professional regulation process. Stephenson claimed: “If you’re not happy about things, I strongly urge you to be part of the change. You being part of the change will be much more effective than hectoring on the sidelines.” This was not meant as any threat. And as I came to think more and more about this I came to think of how much distress my behaviour had caused from my illness, how I wish I had got help sooner, and how looking for someone to something to blame was no longer a useful use of my energies. I am now physically disabled. I get on with pursuing a passion of mine, which is promoting living better with dementia. But if there are any people who are worthy of retribution I later decided then their karma might see them implode with time. Not my problem anyway.
I now try to encourage others where possible if they feel that they have hit rock bottom; I strongly believe that it’s never too late for an addict to break out of the nasty cycle. If you think life is bad, it unbelievably could be much worse. I think businesses like persons get comfortable with their own existence and their own culture, but need to adapt if their environment needs it. I think no-one would wish to encourage actively social care on its knees such that NHS patients cannot be discharged to care, if necessary, in a timely fashion. I don’t think anyone designing the health and care systems would like them to be so far apart deliberately, with such bad communication between patients, persons and professionals. Above all, I feel any change has to be authentic, and driven by people who really desperately want that change. I think change is like producing a work of cuisine; you can follow the recipe religiously in the right order, but you can recognise whether the end result has had any passion put behind it. For me, I don’t need to ‘work hard’ at my recovery, any more. I haven’t hit the ‘pink cloud‘ of nirvana, but I am not complacent either. Change was about getting from A to B such that I didn’t miss A, I was in a better place, and I didn’t notice the journey. If I had super-analysed the change which was required to see my recovery hit the seven year mark this year, I doubt I would have achieved it.
A large scale cultural national transformation is needed to drive whole person care in dementia
I’ll be blunt. It’s my dream for the #NHS to run a proactive not reactive service, promoting the whole person living well with dementia.
The Australian jurisdiction have recently provided some helpful inroads here.
The narrative has changed from one of incessantly referring to people living with dementia as a ‘burden’ on the rest of society. For example, to push a sense of urgency that we have an ‘ageing population timebomb’, the cost of the ageing people with dementia flies completely in the face of other public health campaigns which emphasise, for example, “dementia is not a natural part of ageing”.
“The NHS as a whole and individual hospitals recognise that dementia is a significant, growing and costly problem for them” is the opening gambit of the Alzheimer’s Society “Counting the cost” report.
An easy to use online resource, Valuing People from Alzheimer’s Australia has been developed in collaboration with community aged care providers who have helpful in stablishing a person centred approach to service delivery.
Person centred care is a development to provide ervices provided in a way that is respectful of, and responsive to, the preferences, needs and values of people and those in the care and support network.
I cannot recommend this resource highly enough. The main source is here.
In fact, it summarises succinctly the conclusions I came to after my exploration of personhood in my book ‘Living well with dementia’. The late great Prof Tom Kitwood said of personhood, “It is a standing or status that is bestowed upon one human being, by others, in the context of relationship and social being. It implies recognition, respect and trust”.
If a Labour government is elected on May 8th 2015, the first necessary step is to legislate for the repeal of the Health and Social Care Act (2012) and to enact new legislation to allow for integrated packages provided they are justified by clinical outcome. For this to happen, it will be necessary for Labour to undergo a ‘conscious uncoupling’ from all the baggage of EU competition law. For this, it is essential also that the UK government is able to carve out provisions from the investor protection clauses and/or the rest of the EU-US free trade treaty (TTIP).
The “whole person care model” has become attractive to those who wish to break down silos between different physical health, mental health and social care “silos”. It has been worked up in various guises by various parties.
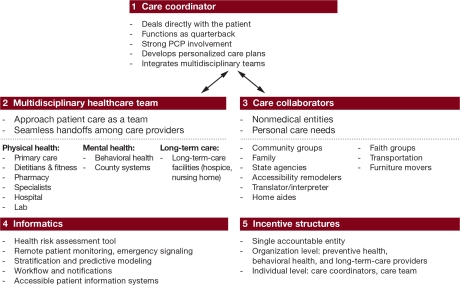
A helpful construct is provided in the document, “Healthcare for complex populations: the power of whole-person care models” originally published by Booz & Company in 2013.
A major problem with dementia care, however it is delivered, is that it is full of divisions: public vs private care, fragmented vs national care, competitive vs integrated models. Operating in silos can’t work because of the nature of the dementias: the mood and cognition of a person with dementia profoundly affects how they might interact with the outside world, for example perform activities in the outside world. And we know that taking part in leisure activities can promote a good quality of life.
Their model is, though, a useful starting point.
Dementia cannot be only addressed by the medical model. In fact, it is my sincere belief that it would be highly dangerous to put all your eggs in the physical health basket, without due attention to mental health or social care. For example, last week in Stockholm, the international conference on Parkinson’s disease, a condition typified by a resting tremor, rigidity and slowness of movement, which can progress to a dementia, often is found to have as heralding symptoms changes in cognition and mood.
So it’s pretty clear to me that we will have to embark on a system of multidisciplinary professionals who could all have a part to play in the wellbeing of a person with dementia, depending on his or her own stage in life, and ability or need to live independently. “Care coordinators” have traditionally been defined incredibly badly, but we do need such an identity to navigate people with dementia, and actors in the care and support network, through the maze.
“Care collaborators” in their construct are very wonkily articulated, like “pre-distribution”, but the concept is not stupid. In fact it is very good. One idea is that people with dementia could act as support as other people with dementia, for people on receiving a diagnosis of dementia. The rationale for this is that people living with long term conditions, such as for example recovery from alcoholism, often draw much support from other people living with other long term conditions, away from a medical model. There needs to be safeguards in the system to safeguard against a lot of unpaid goodwill (which currently exists in the system.)
Informatics would have a really helpful rôle here, being worked up in telecare and assistive technology. But even simple disruptions such as a person living with dementia at risk of falling from problems with spatial depth perception being able to ‘hot email’ a care coordinator about perceived problems could trigger, say, an early warning system. And with various agents in the provision of care being involved in differing extents it will be up to NHS England to work out how best to implement a single accountable tariff. Falls are just the sort of ‘outcome metric’ which could be used to determine whether this policy of ‘whole person care’ for people living with dementia is working. And, even though everyone ‘trots it out’, the performance on avoided hospital admissions could be put into the mixer. It’s already well recognised that people with dementia can become very disoriented in hospital, and, and despite the best efforts of those trying to improve the acute care pathway, people with dementia can often be better off away from hospital in the community. But it’s imperative that care in the community is not a second-rate service compared to secondary care, and proper resourcing of community whole person care is essential for this before any reconfiguration in acute hospital services.
But the private sector has become such a ‘bogey term’ after arguably the current Government overplayed their hand with the £3bn Act of parliament which turbo-boosted a transfer of resource allocation from the public to private sector. Any incoming government will have to be particularly sensitive to this, as this is a risk in strategy for the NHS.
In October 2005, Harold Sirkin, Perry Keenan and Alan Jackson published a highly influential article in the Harvard Business Review entitled “The hard side of change management“. Whilst much play has in fact been made of politicians having to be distant from running the NHS, a completely lubricous line of attack when it is alleged that Jeremy Hunt talks regularly to senior managers and regulators in the NHS, the benefits of clear political leadership from an incoming Labour government are clear.
Andy Burnham MP has already nailed his colours to the mast of ‘whole person care’ on various occasions, and it is clear that the success of this ambitious large scale transformation depends on clear leadership and teamwork from bright managers. Take for example the DICE criteria from Sirkin, Keenan and Jackson:
But this is perfectly possible from an incoming Government. The National Health Service has a chance to lead on something truly innovative, learning from the experience of other jurisdictions such as Australia and the USA.
As alluded to in the new resource from the Alzheimer’s Australia, this cultural change will require substantial ‘unfreezing’ from the current mindset for provision of care for people with dementia. It will require a change in explicit and implicit sources of knowledge and behaviours, and will need to be carefully brought about by learning from the successes and failures of pockets of implementation.
The whole project’s pretty high risk, but the rewards for people living with dementia, and members of the care and support network, are potentially vast. But it does require the implementation of a very clear vision.
[First posted on the 'Living well with dementia' blog]
Can the English NHS enter a ‘period of calm’ if it wishes to introduce integrated care?
Sir David Nicholson, KCB, CBE, is Chief Executive of NHS England.
In 2010 Nicholson jokingly described NHS reform plans, the implementation of the Health and Social Care Act (2012), as the biggest change management programme in the world – the only one “so large that you can actually see it from space.”
Andy Burnham MP gave a speech to The King’s Fund on 24 January 2013, entitled “‘Whole-Person Care’ A One Nation approach to health and care for the 21st Century”.
And the Conservative Party, with Jeremy Hunt MP as Secretary of State for Health, have been eyeing up ‘integration‘ too.
So, like many areas of policy such as the private finance initiative, personal budgets or ‘efficiency savings’, there might be considerable consensus amongst the main political parties about implementing a further transformational change in the English NHS.
In that famous King’s Fund speech, Burnham comments, “Second, our fragile NHS has no capacity for further top-down reorganisation, having been ground down by the current round. I know that any changes must be delivered through the organisations and structures we inherit in 2015. ”
This is coupled with, “While we retain the organisations, we will repeal the Health and Social Care Act 2012 and the rules of the market.”
The Health and Social Care Act (2012) as a legislative instrument, whatever the political bluster, had three main legislative aims.
It aimed to implement competitive tendering in procurement as the default option, thus expediting transfer of resources from the public sector to the private sector; it beefed up the powers of the economic regulator (“Monitor”) for this “market”; and it produced a preliminary mechanism for the managed decline of financially unviable entities in the NHS.
Therefore repealing the Act can be argued as a necessary and proportionate move for taking out the ‘competition jet engines’ of the NHS “market”.
Experience from a number of jurisdictions provides that the legal challenges in allowing integration (and bundling) within the framework of competition law are formidable.
There is a clinical case for integrated care, in allowing more co-ordinated care of the person across various disciplines, for example medical, psychiatric or social, for both health and disease.
If community services are ‘wired up’ with hospital services, provided that community services are not starved of money at the same time as hospital services, there is a good rationale in that the health of certain people, followed closely in the community, might not freefall so badly that they require admission to a medical admissions unit.
There is also a financial argument that integrated or whole person care might work, but clearly no political party will wish to prioritise this ahead of quality of clinical care, particularly given the current tinderbox of cuts in medical and social care.
But whichever way you look at it, ‘whole person’ care involves a huge cultural change; this has repercussions for how all professions conduct themselves in their care, especially with regards to community care, and has consequences for training of staff in NHS England.
And it is impossible to think that, whichever political party ultimately becomes responsible for introducing a whole person or integrated care approach, it won’t cost money.
For example, setting up the infrastructure for data sharing, whether clinical or for the purposes of unified budgets, has a long history of being expensive.
Estimates of the cost of the reorganisation just gone are a bit confused, but they tend to range between £2.5 and £3 bn.
The risk of turbulence can be, to some extent, mitigated against by known people at the helm, such as Andy Burnham or Liz Kendall, but the last thing the general public will wish is another period of massive upheaval.
It can be argued that these changes are ‘a good idea’, and it’s only a question of explaining the benefits to the general public, but, following the Health and Social Care Act and caredata, the track record of this current Government is nothing to write home about.
Twitter: @legalaware
It’s not just the structural disorganisation which has to be reversed. Parts of NHS culture must change too.
The political problem for David Cameron is that all of the current problems of the National Health Service can be blamed on this current Government ‘diverting’ around £2.4 bn resources into implementing a complicated disorganisation.
Lansley, a co-author of ‘Equity and excellence: liberalising the NHS’, the key White Paper of 2010, has always argued that this was never a ‘top down reorganisation’. It was a ‘devolving reorganisation’, according to him re-distributing power to clinical commissioning groups inter alia.
If the Thatcher and Major decades could be characterised as implementing a sort of ‘market’, with purchasers and providers, the Blair (and less so Brown) years might be characterised as a restructuring period for the NHS. This is after all where the PCTs were originally created.
One of the biggest criticisms of how the NHS was run in the latter period of the last Labour government is that CEOs sought to ‘game’ markets so that NHS Trusts could without any difficulty obtain ‘foundation trust status’. Some Trusts for budgetary reasons employed unsafe staffing. With a weak regulator at the time, with culpable CEOs simply moving onto different jobs, the rest of NHS (and some relatives tragically) have been left to pick up the pieces.
Andy Burnham MP is thought to be fairly safe in his Shadow Secretary of State job until 2015 at least. Whether he can remain spend a helpful period of time as a Labour Secretary of State in health, implementing ‘whole person care’, is quite a different matter.
Burnham has categorically pledged to repeal the Health and Social Care Act (2012). He has pledged to reverse part 3 – the section on competition. He insists that he ‘will ask to the same structures to do different things’. This approach is to avoid the accusation that Labour will embark on yet another costly disorganisation, knowing that the public know there have been quite aggressive cuts in nursing staff numbers already.
This might seem fine – but it will not address any latent pathology in culture in the NHS. Unless Labour attempts to consider this build up of pathology, which has taken decades across both Labour and the Conservatives, it is possible that it could become really malignant again. At worst it could kill the NHS.
Evidence that the pathology is relapsing is, for example, given by the recent ongoing debacle at Colchester.
Ecosystems do change however.
Look at Death Valley.
The wettest year on record in 2004/5 transformed the forbidding wilderness of scruffy mountains and scorched earth into a vividly unfamiliar world of wildflowers and reflecting pools, triggering ecological cycles not seen before on so large a scale.
The intense heat was swapped for an environment which living things could flourish.
Against a background of snowcapped peaks, the region’s lands suddenly became populated by bright yellow, pink, white and deep purple blossoms spreading out in all directions.
And why did markets cause so much a problem?
We turned from a market economy to a market society.
Why is this a problem? According to Sandel, two reasons: First, inequality. As money becomes important to access to the essentials of the good life — such as decent healthcare — inequality becomes more and more important.
And the second reason is that when market thinking and values enter the sphere of certain social goods and practices, they change the meaning of those practices — and crowd out attitudes and norms worth caring about.
Sandel gives the example of cash incentives in schools.
Some schools in New York, Chicago and Washington DC have begun programs to motivate students from disadvantaged backgrounds by offering money for grades: $50 for an A, $35 for a B, and so on. A program in Dallas offers students $2 for every book they read.
What was observed at the end of the experiment was that all was more was offered for students reading books, students did indeed read more books with greater financial motivation. But they also read shorter books.
What this illustrates is a false assumption held by many economists, says Sandel: that markets are inert and don’t taint the goods they exchange. This, Sandel argues, may very well be true with material goods, but not so with medical services, engaging in civic life. According to his thesis, market thinking can actually change the “character” of these social practices, so we have to really think about where markets belong and where they don’t.
Look at how GP practices are paid to collect some data under QOF – the use of some of this data is not at all clear.
The National Health Service is in an intrinsically human phenomenon. It is not adequately encapsulated by a series of equations concerning industrial productivity.
Margaret Heffernan gives another striking example.
Gayla Benefield uncovered an awful secret about her hometown that meant its mortality rate was 80 times higher than anywhere else in the U.S. But when she tried to tell people about it, she learned an even more shocking truth: people didn’t want to know.
It turned out the hometown was full of a substance called asbestos, causing individuals to breathe in asbestos and develop fatal lung disease.
In the best organisations, those charged with leading the organisation welcome challenge because it helps the organisation to learn.
But the recent history of the NHS is littered with the casualties of the fear of acknowledging error, especially where such errors might be the tip of a very large iceberg, in an organisation that is more systematically flawed.
Kim Holt, Gary Walker, David Drew, and Steve Bolsin – the list of those who have had the courage to blow the whistle is a long and honourable one.
But people who have tried to speak out have invariably suffered in some form themselves.
The NHS will be doing its ‘change day’ soon in 2014. Part of a way with dealing with a problem, whether it is an assumption of market values not to the benefit of the patient, or a lack of a safe environment to ‘speaking out safely’, is admitting the problem exists.
Only then can you unfreeze yourself from this ‘frozen culture’, shift culture, and move to a new cultural destination.
Whatever is legislated about structures, this change must happen in the next government. It will also be essential for the safe implementation of ‘whole person care’, or similar.