Home » Posts tagged 'corporates'
Tag Archives: corporates
The future of general practice in England
One of the most striking aspects of the biggest reorganisation in the history of the NHS in recent years, estimated to cost about £3bn, is that it manifests glaring gaps in legislation. There is not a single clause on patient safety, save for abolishing the National Patient Safety Agency. It also does not discuss general practitioners themselves. It does contain a nice legislative framework however for the law anticipated for scenarios (sic) quite close to asset stripping, in the event that NHS Trusts have to be wound up due to insufficient funds.
I took a relative to have her ear syringed this morning in a local general practice, and I was thinking only this morning how general practice would be likely to have a backdoor reconfiguration in the next parliament whoever is in power.
I personally am fed up of even hearing about, let alone discussing, the “Tony Blair Dictum”. I prefer to think of it now as “The Deceptive London Cab Analogy“. The Dictum in its various manifestations states that it doesn’t matter who provides my NHS services, as long as it’s of good quality and free at the point of use et cetera. I have always found the idea of private providers freeloading on the goodwill and reputation of the NHS as odd, when presumably they wish to establish the quality and kudos of their own distinctive services. I think the “Deceptive London Cab Analogy”, in that I don’t particularly care if it is actually a London cab, as long as it looks like a London Cab, and gets me from A to B (for example the Royal College of Surgeons in Lincoln’s Inn Fields to the Royal College of Physicians in St Andrew’s Place). It’s a bonus actually if it costs me less. I don’t care how it gets me there; in effect, there’s no difference between using a SatNav or somebody who has done 4 years of “The Knowledge” and has been examined accordingly.
Primary care is of course “the elephant” in the room, in that everyone knows that certain multi-nationals, assisted by liberalisation of international free trade, are licking their lips. It’s yet another one of those unmentioned topics in policy, like the NHS McKinsey efficiency or productivity savings, co-payments or personal health budgets. The whole world knows the existence of policy forks in the world, except none of the established traditional parties wish to discuss precisely the details. And people within thinktanks can continue to spin their motherhood and apple pie, in the hope that they can curry favour with an incoming administration. But it’s important for us who have other views on this to make such views known clear, otherwise a political party, including Labour, could legislate through the backdoor based on conversations also done behind-the-scenes. The public, whilst fed up about this ‘democratic deficit‘, are relatively powerless over it.
In 2010, Apax Partners published a revealing document entitled, “Opportunities: Post Global Healthcare Reforms“. The Apax Partners Global Healthcare Conference, which took place in New York in October 2010, sought opinions about the future of healthcare from some interested stakeholders. The ideology of the document is clear:
“With over 1.3 million employees, the UK’s National Health Service (NHS) is the world’s fourth largest employer and one of the most monolithic state providers of healthcare services.”
It is the ultimate nirvana for a businessman to find a new market. And general practice is articulated in those terms in the Apax document:
“The other change that (Mark) Britnell sees in the UK is even more fundamental: “In future, The NHS will be a state insurance provider not a state deliverer.”
Mark Britnell has been previously mooted as a possible contender for the replacement of Sir David Nicholson in the Health Services Journal.
The main problem about the current NHS top-down reorganisation is that it is important to identify the correct problem before producing an appropriate solution. If the problem which the Government wished to address was how to outsource and increase the number of private providers in the NHS, the solution, if implemented successfully, can be considered to be appropriate. When McKinsey sneezes, English health policy catches a cold. In this regard, McKinsey’s document, entitled “Five strategies for improving primary care” (“Report”; to download, please follow this link) provides some useful pointers. Affirming the importance of this market, the authors (Elisabeth Hansson and Sorcha McKenna) begin with the statement, “Primary care is pivotal to any health system.” Indeed, the first identified problem is that ‘in many countries, patients are dissatisfied with their ability to see GPs in a timely fashion.’ This is of course a problem which the operations management of any State-run service can address too. It is reported that, in Sweden, for example, many patients report that they cannot get timely access to their GP, especially by telephone. This is conceivably something which patient groups or the Royal College of General Practitioners could collect data on (and there is no shortage of data collection in primary care in the name of QOF) to improve the quality of the service.
It is mooted that, “the productivity of British GPs, for example, has dropped sharply in the past 15 years despite the fact that the government has markedly increased what it pays them“, on page 71, but this will be strongly contested by British GPs one assumes. The Report specifically discusses QOF thus:
“The United Kingdom has attempted to improve the quality of its primary care services through a new program, the Quality and Outcomes Framework (QOF), which gives GPs additional payments if they meet specified outcome metrics (for instance, the percentage of hypertensive patients whose blood pressure is lowered to the normal range). The program has been successful in focusing attention and improving scores on those metrics, but it has become clear that a GP’s performance on those metrics does not always reflect the overall quality of his or her practice.”
There has been, particularly since Kenneth Clarke’s “The Health of the Nation” paper in the 1980s, an enthusiasm for GPs to be paid to collect data, but such data has to be meaningful.
Consistent with the Health and Social Care Act (2012), and the pivotal section 75 which acted as the rocket boosters for introducing competitive tendering formally into the English NHS, the document argues that:
“In both tax-based and insurance-based systems, competition is a way to increase GP productivity and the quality of care, because it signals to physicians that they will have to perform better if they want to retain their contracts and patients.”
This has only this week been powerfully rebutted by Professor Amanda Howe (MA Med MD FRCGP), Honorary Secretary of Council the Royal College of General Practitioners, in her response to Monitor as a member of Council (as linked here):
“The RCGP welcomes Monitor’s stated aim to better understand the challenges faced by general practice at a time when it is operating under increased pressure. However, we would strongly caution against the assumption that the challenges faced by general practice are caused by a lack of competition, or that the best lever to reduce perceived variability in access and/or quality would be an increase in competition.”
One of the most powerful levers described by the Report is “changing the operating model”.
“This lever is conceptually simple but often difficult to implement. For example, it often makes a great deal of sense to move physicians away from small (often solo) practices and into larger primary care practices or polyclinics (which include a wider variety of services, including diagnostics and outpatient clinics). Larger practices and polyclinics allow physicians to achieve economies of scale in some areas, such as administration. Furthermore, having a mix of physicians working together can improve quality and provide a more attractive working environment for new physicians (which might then help increase the workforce supply).
If a health system does decide to change its primary care operating model, it should consider a question even more radical than where physicians should work—it should ask whether certain primary care services need to be delivered by physicians at all. In the United States, for example, certain nurses with advanced training (nurse practitioners) are legally able to perform physical examinations, take patient histories, prescribe drugs, and administer many other basic treatments. Nurse practitioners can usually provide these services at a much lower rate than physicians typically can, but with comparable quality.”
This is a powerful summary, as it is consistent with the view that certain jobs can be better done by cheaper workforce. This is i itself a constructive idea potentially, simply in organising functions within the workforce for the people most suitable to deliver those functions. For example, many NHS hospitals have employed “physician assistants” to put in venflons or insert catheters, freeing up junior doctors to get on with other tasks in their busy schedule too. There comes a problem as to whether diagnostic services should be ‘liberalised’ on demand, i.e. so that the ‘worried well’ establishing their autonomy can pay to have their blood pressure checked ‘on demand’ if they want it. Provided that the equipment works, and the user of the diagnostic equipment does not use that equipment negligently, and that the investigation itself did not do any harm or damage, a regulator might not intervene, depending on the exact circumstances of course.
The second “big lever” is integration, described as follows:
“As we discussed earlier, GPs are typically responsible for coordinating with all the other health professionals and organizations (sic) that provide care for a patient. Coordination is hampered, however, by the fact that few health systems have effective methods for ensuring that information is transmitted to the appropriate places. Ensuring that such communication takes place does not require that all providers be part of a single organization (sic). However, it does require that all providers commit to sharing information and coordinating care and that a strong IT system operating on a joint platform is available to facilitate data exchange. Payors can encourage this type of alignment through their contracting (for instance, by requiring the providers to report the same set of metrics).”
And there is still a hangover of the integrated healthcare model from the US health maintenance organisations. Here it is possibly more of a case of joined-up thinking in some different ways. Regulators should be mindful of referrals being made between primary care and secondary care (where VerCo GP practice refers to Verco NHS Trust) not on the basis of clinical need but for shareholder dividend, though the cases of clinical regulators making sanctions on the basis of unethical conflicts of interest are currently sparse for whatever reasoning. It is also remarkable how keen and enthusiastic many corporates are on building the IT infrastructure for primary care, and indeed these noises of data sharing and paperless records are echoed by Jeremy Hunt. Ultimately, if one so wishes, whoever ‘owns’ primary care, whether it is a state-run service or not, this IT system could be ultimately linked to the private insurance system; a minority feel that that is where an aspect of integrated care is ultimately aiming towards.
The drumbeat from McKinsey’s and Apax is therefore providing a structural set-up and culture such that there can be a greater number of private providers in the holy grail of primary care. The notion that GPs are ‘only interested in their wallet’ (as famously said by Kenneth Clarke) is not at all borne out by the evidence from the professional bodies or regulators, and whilst there have been many touting GPs as businessmen (including some isolated opinions from the leadership of the Socialist Health Association (“SHA”) which have to be read in context, e.g. as in this recent blogpost by Martin Rathfelder (Director of the SHA)):
“The issue is blurred anyway as many GPs have found ways to “profit” through taking interests in companies providing services.”
People who do not hold the same views as McKinseys’ and Apax should be allowed to influence an incoming Labour government, whether they are or have been the leadership of the SHA or not. It is hoped that these alternative views do not merely act as a boring echochamber, and genuinely reflect the founding values of the NHS.
Many posts like this have originally appeared on the blog of the ‘Socialist Health Association’. For a biography of the author (Shibley), please go here.
Shibley’s CV is here.
Health screening: corporates, the third sector, the NHS and the media “in it together”? BBC One’s “Long Live Britain”
The All Party Parliamentary Group Primary Care & Public Health published yesterday their ‘Inquiry Report into the Sustainability of the NHS “Is Bevan’s NHS under Threat?”‘. In their excellent report, they provided that “Preventative illnesses are overwhelming the NHS; illnesses caused by obesity, smoking, alcohol and lack of exercise. Diabetes, for example takes up 10% of the NHS budget, of which 90% is spent on dealing with preventable complications.”
The Faculty of Public Health response was follows:
“The need to treat lung cancer is waste – smoking cessation works and is far more cost effective at prolonging life than treatment for lung cancer. The need to treat heart disease is a waste – increasing physical activity levels, stopping smoking, improving diet are all preferable and cheaper. Treating measles is a waste – increasing vaccination uptake rates is more efficient; every case of HIV is a waste when it is easily preventable. There are barriers to smoking cessation (quality of services, access to services for vulnerable groups) as well as things that can be done to prevent people smoking in the first place (standardised tobacco packaging). There are barriers to preventing heart disease – transport systems and public open space that do not encourage incidental physical exercise; the availability of cheap high fat / salt / sugar food actively marketed to vulnerable populations (e.g. children); smoking (see above).”
Two issues have dominated the headlines in politics and public health this week; one is the issue of standardised packaging of cigarettes and the other is minimum alcohol pricing. A new BBC One two-part series, Long Live Britain, claims to be an “one-off, record-breaking televised event that will challenge the way we tackle three of Britain’s biggest preventable diseases.” On Saturday 25 May, Long Live Britain says it “will attempt to host Britain’s biggest-ever health screening, potentially testing thousands of possible undiagnosed sufferers for the three secret killers that collectively kill 200,000 each year and affect an estimated 11 million people each year – Type 2 diabetes, cardiovascular disease and liver disease. Presented by Julia Bradbury, Phil Tufnell and Dr Phil Hammond (@drphilhammond), it is claimed that, “the fascinating results will be screened on BBC One over one night in early summer.”
However, this is a delicate issue in reality. A group of practising Doctors have set up a website, Dr Pete Deveson (GP in Epsom, Surrey) (@PeteDeveson) , Dr Margaret McCartney (GP in Glasgow) (@mgtmccartney), Dr David Nicholl (Consultant Neurologist in Birmingham) (@djnicholl), Dr Jonathon Tomlinson (GP in Hackney, London) (@mellojonny), and and Professor Charles Warlow (Emeritus Professor of Medical Neurology University of Edinburgh) because they are concerned that the promotion of private screening tests in the UK is potentially unfair to people reading many of their adverts. They indeed have complained to the Advertising Standards Authority and the General Medical Council. Some changes have been made to the adverts after their complaints (see here and here. Clearly adequate choice can only be made on complete and accurae information.
Screening is a complicated issue. Prostate cancer is a good example. If a man is showing none of the symptoms associated with Prostate Cancer why should he consider having a screening? GP Dr Pete Deveson and Dr Tony Rudd, who is a consultant stroke physician, have both publicly voiced their concerns over private health checks. Margaret McCartney (above) was written passionately on this issue in the Guardian:
“The NHS offers many screening programmes, from the heelprick test for newborn babies to breast screening for women over 50. But screening – testing well people as opposed to people who already feel unwell or who have symptoms, like a lump, or palpitations – always has the potential to harm, and is a constant balance of pros and cons. There is a risk of false positives, false negatives and false reassurance, and the problem of sometimes giving people a diagnosis they don’t need, or subjecting them to treatment they won’t benefit from. Noninvasive tests may cause few hazards, but the way the knowledge from a positive or negative scan is used may result in harm to the patient for no benefit.
We’ve seen this in prostate cancer screening: initial enthusiasm for PSA (prostate-specific antigen) screening was followed by the realisation that around a third of men operated on would suffer impotence as a result and a fifth would have incontinence.
These might be acceptable risks if the treatment was death-delaying, butmost prostate cancers don’t kill and the evidence suggests that PSA screening does not reduce death rates.
This led Richard Albin, who discovered PSA, to tell the New York Timesthat screening for it had been a “public health disaster” in the US.
So screening is often counterintuitive and harmful. Because of these inherent problems, people need to make good choices about whether to be screened based on evidence. We know, for example, that when men are given better information about PSA screening, fewer want it.”
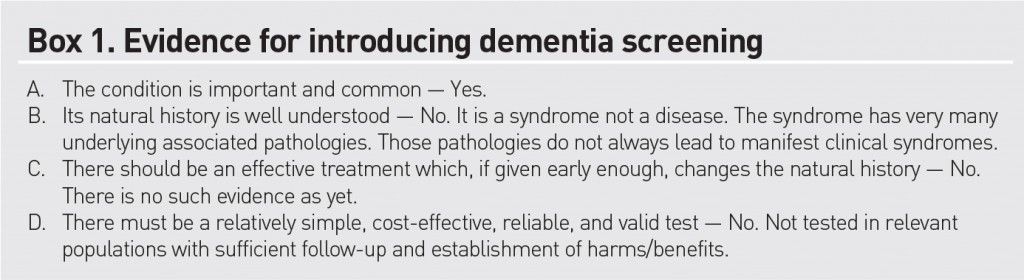
Screening has not been advocated for dementia, but this is ripe for corporate profiteering (and third sector colleagues who wish to be part of this agenda.) In an outstanding article published in British Journal of General Practice, Prof Carol Brayne and colleagues tackle this issue head on. Carol Brayne identifies the possible efficacy of ‘awareness’ campaigns in ‘generating fear’, and elaborates on these concerns:
“Turning to the private sector. It is quite possible that considerable ‘market’ can be generated through capitalisation of fear of dementia and cognitive decline. Direct-to-consumer advertising already exists for cancer (specific insurance schemes) and stroke (carotid and risk screening). Taking the example of stroke risk ‘screening’, individuals may receive, through population listings, materials that promote testing in centres sometimes hosted by primary care settings, which gives an apparent endorsement that this is evidenced practice. Could this happen with cognition? It seems likely, including the online potential. Does this matter? It depends on the outcome of the testing. If positive in some way where will these individuals turn for support? How much investigation will reassure them? How many people will be tested unnecessarily and for those who are identified as having a problem will there be sufficient resources to support them? In a publicly-funded system this will fall to their GP, who will therefore have less time for those who attend with existing concerns. In a private model these individuals may seek help elsewhere, paying for imaging and further tests. These may or may not provide reassurance or further indication of problems, but doing such tests is not, at present, justified on the basis of evidence. For some a remediable condition may be found, but as with general health screening, it will be impossible to say who has been harmed and who helped by such efforts.”
Brayne and colleagues do not feel that dementia fits the traditional Wilson-Jungner criteria for screening:
Either way, it is beginning to become clear, pursuant to an Act of parliament which enabled the outsourcing and award of contracts to the private sector in the National Health Service, and where the income in the NHS can come from private sources in up to 50%, screening is yet another issue which can be gamed by the private sector. How much the media wishes to have a genuine debate about raising awareness of clinical issues, as indeed is the agenda of the Faculty of Public Health, or gets embroiled in complex rent seeking behaviour for profitability or surplus generation of corporates and the third sector is a different matter. Of course, corporates, charities and the media, like the National Health Service, can have the best of intentions too.
Why the NHS Health and Social Care Bill doesn’t make sense to me
This post is inspired by brief discussions I’ve had with Sunny Hundal where Sunny asked me lots of questions I couldn’t answer!
Of course, Labour is clear that they oppose the NHS Health and Social Care Bill. What they had not been clear to me about is why they oppose it, though I am very grateful to Sunny Hundal for pointing me in the direction of the ‘Drop the Bill’ website which establishes five important alleged concerns of the Bill: postcode lottery, longer waiting times, privatisation, damaged doctor-patient relationship, and waste.
Labour and supporters bandy around the statement ‘It is privatising the NHS’. This is indeed a very good way of looking at it, as the fundamental thesis is that there will be a greater role for the private sector in the provision of health services for England. To ignore the existing contribution of the private sector in the NHS is complete nonsense, however. NHS budgets operate millions of pounds, and the private sector is clearly involved. Most people in the general public have heard of NHS procurement, or “NHS logistics”; many people, in both the private and public sector are somehow enmeshed in the NHS ‘supply chain’. In fact, at least with privatisation, according to the aspiration of Baronesss Thatcher, there is public ownership of the infrastructure. The worrying aspect here is that NHS entities can be bought by hedge funds or even foreign investors, as part of a multinational investment, and indeed Ed Miliband might be right after all – corporate entities might wish to sell bits off the NHS ‘for a quick buck’ in his much derided speech on corporate social responsibility last year. There is as such not illegal, but many will not agree with this sensitive corporate handling of key infrastructure assets.
A more mature intelligent debate is to consider why precisely the NHS Health and Social Care Bill does not make sense. It firmly places the NHS in private hands, and it is worth scrutinising carefully at this point what the legal entity of the NHS Trust is.
If it is a private limited company under law, it is under legal obligation to maximise shareholder dividend, and the question then becomes who exactly are the shareholders, and how will their profits from NHS patients be used? One assumes that NHS Trusts will be subject to all aspects of company law, such as insolvency law and competition law inter alia. How is competition going to work? And are entities going to offer products or services that are ‘profitable’? What about dementia, for example? I am worried about the fact that this could lead to major imbalances in service provision at both primary care level and in NHS Trusts. How is the Tory-led Government going to ensure that apples are not unfairly compared to bananas in this new free market of the NHS? This involves a complex understanding of how products and services are going to be costed in the new NHS; will they be simply the cost of providing the products or services, or will some corporate entities wish to undercut other suppliers by ‘penetration pricing'; or will some suppliers price themselves at a high price to denote high brand value, for example for ‘the best hip operation in town’? For that matter, how does the Bill deal with measuring benefits and outcomes for the patient, rather than the corporate supplier?
I believe strongly that we will almost have to invent a new entity in law to cover NHS trusts, if it is not the private limited company or charity under the Companies Act or Charities Act. I do not feel that such strategic change will succeed in management for one clear reason, anyway. In any such rushed strategic change, you must have follower support; so even if the LibDems in the lower and upper Houses act as the lubricant for the Conservative engine in allowing this Bill a clear path to Royal Assent, the implementation of the NHS Bill will almost certainly fail due to lack of support from many GPs, the Royal Colleges, many other health staff, and most importantly the patient. I also feel that, in management, it is going to impossible to implement such organisational structural and cultural change in such a hurry.
Calling the BMA a ‘trade union’ itself is not a trivial point. Trade Unions protect the rights of employees rather than shareholders (unless stakeholders are also shareholders), and therefore if the NHS Bill is enacted without key stakeholder support it will fail. This is because the members of this trade union are not involved in the strategic change process at all well, and feel it is being inflicted without their consent. They also will have much tacit implicit knowledge about the NHS, as well as codified principles, which will be harder to shift without specialist change managers.
However, there is no doubt that somebody does need to look at the management structure of the NHS, which is why I should rather Labour has a constructive input into the debate, on behalf of public sector workers, and if it decides it wishes for blanket obstruction, it should consider urgently an alternative, because it is currently the case there are parts of the NHS which are financial disaster zones. Furthermore, the NHS does not always work well; very many nurses work with poor pay and conditions, but stories about suboptimal care unfortunately do rumble on (especially in elderly care). Finally, there is a strong part of me that believes in a system where we all share risk in a National Health Service by paying a contribution – this is where reform of the tax system is vital, as the NHS is currently paid for out of income tax mainly to my knowledge. If private enterprises are allowed wholly to run the NHS, it could be that the business entities which go out of business are those where there are particular ‘hotspots’ of disease due to an unfortunate combination of nature and nurture, for example chronic obstructive airways disease in coal miners in Wales, or high incidence of cardiovascular disease in Bengali immigrants in Tower Hamlets. Health inequalities are a serious problem for medical care, and replacement of the NHS with increased private input for entities to run at a profit would be a serious threat to that.
That’s the sort of debate I wish for why I oppose the NHS Health and Social Care Bill. And what about Dilnot also?
This is a personal view of @legalaware, and does not represent the views of the BPP Legal Awareness Society, nor of BPP.