Home » Posts tagged 'case finding'
Tag Archives: case finding
Identifying people who “might” have dementia is simply not good enough
Imagine you are a 45 year old lady who goes to see a GP with a lump on the breast.
Just pretend the lump on the breast is not a sinister cancer, but a small harmless fatty collection of fatty cells called a lipoma.
Would you appreciate that GP labelling you as having breast cancer because of a Government target to improve the number of diagnoses of breast cancer nationally?
Whilst it might be good for that GP ‘hitting the target’, the GP is certainly ‘missing the point’, as he or she has inadvertently given the patient much distress through the misdiagnosis.
In medicine of course you do not necessarily need to progress to a surgical biopsy to lead to a confident diagnosis. It happens that it is relatively most unusual for a diagnosis of dementia to warrant a neurosurgical brain biopsy unless it might be for a rarer condition such as Variant Creutzfeld Jacob, or a potentially treatable cerebral vasculitis (inflammation of the brain).
It is known that a sizeable minority of people we think have dementia do not actually turn out to have dementia on post mortem. Indeed, according to Professor Seth Love? Department of Neuropathology, University of Bristol Institute of Clinical Neurosciences, “In most published series, the accuracy of clinical diagnosis of the different diseases that cause dementia is of the order of 70–80%.”
The definitive diagnosis of dementia is achieved post mortem.
Whilst it is laudable that there is a strong drive to improve the diagnosis of rate of dementia in England, it is absolutely imperative that this diagnosis should be reliable. Otherwise the scenario arises where a 85 year-old man who lives on his own, recently widowed, suffering from profound clinical depression can inadvertently get mislabelled as having a dementia, and this diagnosis in itself makes him even more depressed.
In recent years, large corporate-acting charities have been largely responsible for touting the concept of identifying people ‘before they have the disease’, for example overweight people who are likely to develop type II diabetes. Likewise, in dementia, professionals have received massive pressure from non-professionals for finding that ‘pot of gold’ of people who most likely might develop dementia. Despite much obfuscation and smoke and mirrors, it is known reliably now that the ‘mild cognitive impairment’, of ‘minor’ dementia-like symptoms, is not that pot of gold, as many individuals with this condition never go onto develop dementia.
But having a roadside MOT in primary care has been argument popularised by large charities and politicians who have been successfully lobbied by them. Without adequate resources going into service provision or training of people in the service, this approach runs the risk of creating an unprecedented demand for people who are in fact ‘worried well’.
Robert Aronowitz (2009) argues that risk of disease and actually having the disease have become conflated.
“Imagine two women, one who is suffering from breast cancer and the second, “merely” at risk for the disease. The first woman is fifty-eight years old. Two years earlier, she detected a lump in her left breast. After an aspiration biopsy revealed cancerous cells, she had a lumpectomy and removal of lymph nodes in her armpit (none of which contained cancer), followed by a course of local radiation and then six months of chemotherapy. After this acute treatment, she was put on a five-year course of the “anti-estrogen” Tamoxifen. She now closely follows developments in breast cancer. At the moment, she is concerned about whether to start another kind of hormonal therapy after her course of Tamoxifen ends and whether she should begin getting screening breast MRIs and/or more frequent mammography. For these and other questions, she frequently searches the web and attends meetings of breast cancer survivor and advocacy groups.”
“The second woman also is fifty-eight years old. She took birth control pills during her twenties, had her first child at age thirty-four, and, at the urging of her gynecologist, took supplementary estrogen pills starting at age fifty because of menopausal symptoms and to prevent heart disease and osteoporosis. A few years later her doctor told her to stop taking these pills because new medical evidence had conclusively shown that their risks—especially an increased risk of developing breast cancer—outweighed their putative benefits. Since age forty, she has been getting annual mammograms. Four years ago, she had an abnormal mammogram, which led to an aspiration biopsy that did not show cancer. Fearful of developing breast cancer, she is attentive to media reports and periodically browses the Internet for new information on cancer prevention. She has seen direct-to-consumer advertisements for Tamoxifen as a preventive measure for women at high risk of breast cancer. She understands that she has multiple risk factors for breast cancer, such as being middle-aged, being postmenopausal, having had her first child after thirty, having earlier used hormone replacement therapy, and having a history of a benign breast biopsy. She has sought advice from friends, doctors, and breast cancer advocacy groups about whether to take Tamoxifen and/or to find other means of reducing her risk of breast cancer.”
“At present, the first woman does not experience any symptoms of cancer but nonetheless undergoes intensive surveillance, has concerns about the long-term effects of previous treatments, and faces the future with caution. The experience of the second women is not very different. She may well decide to take Tamoxifen to prevent breast cancer. Like the first woman, she undergoes frequent surveillance and faces the future with caution. Both women face an array of similar choices and seek guidance in similar places. They share fears for the future, feelings of randomness and uncertainty, and pressures for self-surveillance. Both seek ways to regain a sense of control and face difficult decisions about preventive treatment and consumption. They are part of a larger breast cancer continuum, both in how scientists understand breast cancer and as a mobilized group for advocacy, fund-raising, and awareness (Klawiter 2002).”
In dementia, people who might be ‘at risk’ are those with strong genetic risk factors, or have a particular constellation of risk factors (hypothetically food intake low in zinc or high in cholesterol etc.) Industries allied to medicine would love to open up new markets by finding these people and offering them treatments early on. However, the drugs currently used to treat Alzheimer’s disease only impact on symptoms for some for a short while, and there is no consistent robust evidence that they slow down the disease course in humans.
In October 2014, I will be presenting data in the Alzheimer’s Europe conference in Glasgow about how precise identification of people most likely to develop dementia will lead those people to have insurance premiums which go through the roof, in a private insurance system, compared to a system where we all pool risk in the National Health Service.
I blogged on this study originally here.
The direction of travel for dementia with influences from private industry is a malign one. It consists of actively seeking out people are who are yet to develop dementia at the risk of completely ignoring the needs of the current cohort of people trying to live well with dementia. The pharmaceutical companies have been spectacular in the minimisation of failures over the last few decades in therapeutic treatment of dementia, and the current case finding approach in the English national health service has the potential to produce as much distress as much benefit.
But people have been warning about major fault lines in our dementia policy, correctly, for some time. See, for example, the excellent work by Margaret McCartney and Martin Brunet.
We can’t go on like this. Identifying people who “might” have dementia is simply not good enough. A properly funded National Health Service, where we are all “in it together”, where the concerns of professionals are listened to as well as the spokesmen of the new ‘dementia economy’, is a necessary start. Besides, the service for post-diagnostic support for those individuals who have been correctly identified as having a dementia needs to be far better resourced and organised so that people don’t feel they are being sent from pillar to post.
Have Big Pharma undermined the case for screening through their grip on dementia policy?
Certain General Practitioners are ‘on heat’ as they take great delight in identifying that dementia does not meet current screening criteria, but they are missing their targets of creating maximum fuss but totally missing the point. In their narrow world, they define “benefit” as a treatment such as a magic bullet. “Benefit”, I believe even under the Wilson and Jungner (1968) construct, can mean something much wider, and ultimately the authors give a very big sense of this being for the benefit of the person or patient not the benefit of the physician. We simply have a lack of evidence base for living well with dementia, due to charities which focus on cure, care and prevention. Without this evidence, we cannot say, any of us, however big or small in the medical establishment or outside, that there’s “no benefit”. Carts and horses spring to mind. This is a good case of medical hierarchy being utterly irrelevant to ‘who is right’, and more importantly ‘what is right’ for the person trying to live well with dementia after his or her diagnosis.
There’s no doubt about it. There’s been an intense policy drive to encourage people with memory problems ‘to present themselves’ for early diagnosis, and various devices have been used to encourage this, including participating in drug research (hence the extreme media publicity for a ‘drive for a cure’). Screening for dementia is a pot of gold for the ‘dementia health economy’, even more so than “Dementia Friends”, as it produces a new market for people who might be eligible for a drug treatment that ‘stops dementia in its tracks’ one day. But some of the confusion has come from the extent to which the screening criteria embraces early symptomatic persons as well as completely asymptomatic ones, and official guidelines, derived from Wilson and Jungner (1968), are not solely for early symptomatic people. But the irony is that the relentless focus on the medical model, without resources going into demonstrating the efficacy of wellbeing interventions as a way of ameliorating morbidity in dementias, including Alzheimer’s Disease, may be ultimately stopping the screening criteria being met, denying access of Big Pharma to this pot of gold. But the way in which Big Pharma has a stranglehold on big charities and research programmes, epitomised by the recent G8 dementia summit in Lancaster House frontloading personalised medicine, could be entirely to blame.
Various intellectual frameworks have, for example, been proposed for the screening of dementia in primary care outside of this jurisdiction. For example, this scheme appeared in the following paper.
The UK NSC policy on Alzheimer’s Disease screening in adults is in fact clear. A systematic population screening programme is not recommended. The National Screening Committee criteria for appraising the viability, effectiveness and appropriateness of a screening programme are based on the criteria developed by Wilson and Jungner in 1968 and address the condition, the test, the treatment and the screening programme. The need to refine them in the genomic age is illustrated in this statement from WHO in 2008. I have no intention of discussing the usual issues of screening/early detection, such as the distress caused by a false diagnosis, described elegantly elsewhere.
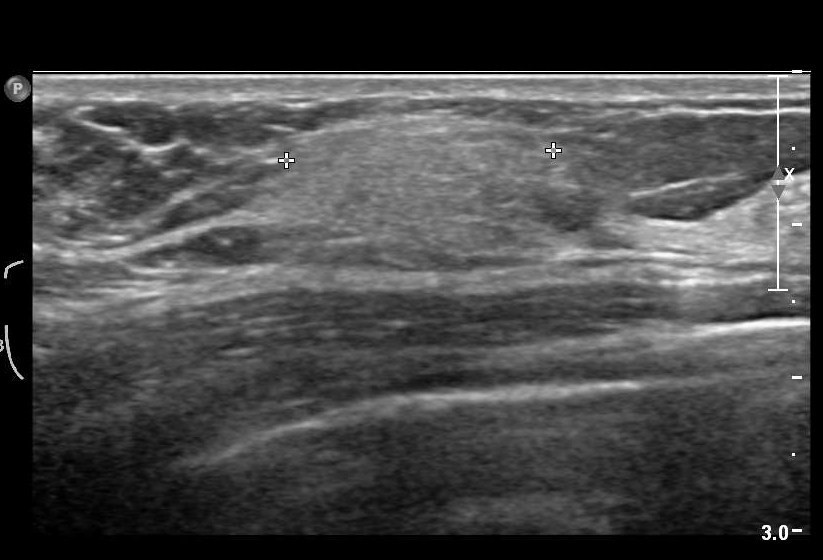
There is no doubt that the drives for screening at all under standard criteria suffer from a lack of inexpensive test which is sufficiently sensitive and specific – but this might be a temporary situation, and might be ultimately resolved one day with the correct ‘mix’ of questions, say in testing a wide range of neurocognitive functions. What is clearly untenable is sticking a large needle into the backs of all people who might be at risk of developing dementia to collect cerebrospinal fluid for biomarkers, or doing expensive MRI scans on everyone (notwithstanding the known limitations of brain scans in making the dementia diagnosis.)
A significant stumbling block is that there should be evidence from high quality Randomised Controlled Trials that the screening programme is effective in reducing mortality or morbidity. Clearly, drugs in reducing mortality for Alzheimer’s disease, which is only one type of dementia, have been lacking. The conclusion that there have been no randomised controlled trials to show that a screening programme for Alzheimer’s disease would be effective in reducing mortality or morbidity. But in fairness there has NEVER been a drive to collect a robust body of information on the long term effects on living well with dementia from an early diagnosis of dementia. Nobody has wished to fund it. The data are lacking. Decades and millions at least have been chucked into the aim that the drugs which ‘don’t work’ (and in fact can have dreadful side effects).
It is interesting that the stumbling block is not the lack of pre-symptomatic stage, though interestingly the National Screening Committee never make reference to mild cognitive impairment, which people who do not understand the evidence incorrectly refer to as ‘pre-dementia’. It is argued, for example, that during the pre-symptomatic period there is a gradual loss of axons and neurons in the brain and at a certain threshold the first symptoms, typically impaired memory for events and facts appear.
And it’s a useful context to think about the ethos in which the Wilson and Jungner criteria should be applied? Wilson and Junger themselves used the term ‘principles’ for ‘ease of description rather than from dogma’. It is unlikely that any screening programme will be able to fulfil all of these criteria to everyone’s satisfaction in any case. The question therefore arises as to whether each criterion has equal merit, or whether there is a hierarchy of importance using this construct. Wilson and Junger felt that ‘of all the criteria that a screening test should fulfil, the ability to treat the condition adequately, when discovered, is perhaps the most important’.
And the build up of these criteria emphasise the clinical method, although the literature in reviewing data results as a desktop exercise is massive. Jungner and Wilson themselves state:
“The medical history is very important, and can be obtained by appro- priate questionaries. It has been reported from many investigations that the medical history and the physician’s physical examination make the greatest contribution to the diagnosis. However, most of the diagnoses are then known before the screening procedures. How much medical value is afforded by the notation of earlier known disease remains to be seen. Obviously, the information is most useful the first time an examination is undertaken. The history is of immense value and the advantage of questionaries is great.”
Jungner and Wilson refer to their review of relevant papers in the 1950s, and their criticisms of case-finding in the absence of seeing the big picture are well known from close reading of their paper.
They cite:
“Some of the chief points made in these papers were:
(1) Case-finding by multiple screening is a technique well suited to public health departments, whose role is changing.
(2) Provision for diagnosis, follow-up and treatment is vitally impor- tant; without it case-finding must inevitably fall into disrepute.
(3) Tests must be validated before they are applied to case-finding; harm may result to public health agencies’ relationships with the public (not to mention the direct harm to the public), and with the medical profession, from large numbers of fruitless referrals for diagnosis.”
Putting all your eggs in the investigations basket has been a discredited approach in the past in neurology. In one particular review of studies, 82% percent (54/66) of investigators reported discovering incidental findings, such as arteriovenous malformations, brain tumours, and developmental abnormalities. Auhors of that particular paper (J. Magn. Reson. Imaging 2004;20:743–747) proposed that guidelines for minimum and optimum standards for detecting and communicating incidental findings on brain MRI research are needed.
So is it viable to do backdoor collection of data to identify cases? Wilson and Jungner indeed describe this failed approach in diabetes detection, according to Joslin and colleagues this work goes back to 1909, when Barringer had reported the findings on over 70 000 persons examined for life insurance purposes. Wilson and Jungner themselves noted that, “Despite all this work it is still difficult to evaluate the results in terms of benefit to the populations screened. Some of the criteria for case-finding discussed above remain unsatisfied.”
So this lack of intelligent thinking from the medical profession has come full circle many years after the original Wilson and Jungner paper. General Practitioners increasingly now recognise the importance and benefits of a timely and explicitly disclosed dementia diagnosis. But it’s argued that there are many barriers to diagnosis at both the physician and patient level. Barriers at the physician level include time constraints, insufficient knowledge and skills to diagnose dementia, therapeutic nihilism and fear to harm the patient.
But it’s impossible to skirt around the basic ‘rules’ of medical ethics, much as non-clinicians in the dementia economy might like to. These include respect for autonomy, beneficence, non-maleficience and justice. And doing things without a patient’s consent, if they have mental capacity, is ethically offensive and legally could constitute assault or battery. This issue has been seen in coeliac disease previously, reported in a paper about a decade ago (Gut. Jul 2003; 52(7): 1070–1071):
“Although the investigational process for population screening and case finding may be the same, there is an important ethical difference between them. If a patient seeks medical help then the physician is attempting to diagnose the underlying condition (for example: patients with CD who present with symptoms of irritable bowel syndrome). This would be classified as case finding and clearly it is the patient who has initiated the consultation and in some sense is consenting for investigation. Conversely, individuals (who are not patients) found to have CD through screening programmes, may have considered themselves as “well” and it is the physician or healthcare system that is identifying them as potentially ill.”
And these ethical concerns appeared originally in the mid 1980s with HIV testing. HIV is used as the “poster boy” in the drive for a cure for dementia, but it’s worth remembering the history of this situation too. Prior to an effective treatment, ethical concerns centred on the right of patients not to be tested, since an HIV diagnosis provided few medical benefits and posed serious risks of stigma and discrimination. The 3Cs were identified of “counselling, voluntary informed consent and confidentially”. But with the availability of ART drugs, there was accumulating evidence that ART can prevent transmission of HIV, strengthened public health arguments for scaling up testing. This led to a reformulation of guidelines, such as “Testing the gateway to prevention, treatment and care” when in 2007 WHO recommended PITC (provider?initiated counselling and testing)
Nevertheless, the primary care setting in England provides unique opportunities for timely diagnosis of dementia. It has just been reported that GPs will be given more leeway to use their clinical judgement in deciding when to offer dementia assessments under a revamp of the specifications for the controversial dementia case finding DES. Under the agreed changes, GPs will still be required to offer the assessments to the same ‘at-risk’ groups of patients on their list, but only if the GP feels it is ‘clinically appropriate’ and ‘clinical evidence supports it’. At-risk groups again include patients aged 60 and over with vascular disease or diabetes, those over 40 with Down’s syndrome, other patients over 50 with learning disabilities and patients with neurodegenerative disease.
And, this is broadly consistent with approaches from other jurisdictions. Case finding remains the preferred approach to identifying patients with dementia and Alzheimer disease, according Australian experts, after a US advisory body found insufficient evidence to support universal screening for cognitive impairment in older patients.
Professor Dimity Pond, professor of general practice at the University of Newcastle, agreed that there was insufficient evidence for screening. Professor Pond said further a false-positive diagnosis could also cause a lot of distress to the patient and their family. “It’s a huge diagnosis to be made — it causes their family to worry about the need to start activating power of attorney, selling the house and putting them in a nursing home.”
Wilson and Junger themselves do not, however, specify whether patients, a third party, or society as a whole, should prioritise importance, and the utilitarian part of this economics discussion is lacking in temporal and geographical jurisdiction (in the same way that G8 hopes to meet its objectives likewise). J.S. Mill, in his celebrated essay “On Liberty”, argues that ‘there is no one so fit to conduct business, or to determine how or by whom it shall be conducted, as those who are personally interested in it’. But it is in reality difficult for an individual patient to be objective as to whether his/her health problem is more important than that of another patient or whether he/she deserves scarce resources in preference to others: it is impossible for an individual patient to make that comparison because of patient confidentiality, for example.
And policy makers need to be able to justify why memory problems are sufficient to trigger a particular care pathway, when a cough does not necessarily trigger full investigations for emphysema, or a headache does not trigger necessarily a full work-up for a brain tumour. The general rule for a ‘care pathway’ is “treating the right patient right at the right time and in the right way.”
I feel a fixation on ‘benefit’ as defined through the prism of the Pharma part of the health economy has led to a wilful neglect for wanting to find any beneficial outcomes in wellbeing from a timely diagnosis, such as improved design of the home, design of the built environments, and access to advocacy. But ultimately, regardless of the health economy and the lack of proper scrutiny of the issue, it is persons with dementia and their caregivers who I feel are suffering most, at the hands of the large charities and Big Pharma. GPs and medics are simply unable to say there’s “no benefit” for finding cases of dementia, whether it is screening or not, if the evidence base on living well with dementia is simply absent. Try to put the horse before the cart next time.