Home » NHS Management (Page 2)
Integrated care – there’s an app for that! A hypothetical case study.
Innovation and integrated care
Andrew Neil reminded us this morning on ‘The Sunday Politics’ that there are currently around 4 million individuals who don’t have access to the internet. Prof Michael Porter, chair of strategy at the Harvard Business School, has for a long time reminded us that sectors which have competitive advantage are not necessarily those which are cutting-edge technologically, but his colleague Prof Clay Christensen, chair of innovation at the same institution, has been seminal in introducing the concept of ‘disruptive innovation’. An introduction to this area is here. The central theory of Christensen’s work is the dichotomy of sustaining and disruptive innovation. A sustaining innovation hardly results in the downfall of established companies because it improves the performance of existing products along the dimensions that mainstream customers value. Disruptive innovation, on the other hand, will often have characteristics that traditional customer segments may not want, at least initially. Such innovations will appear as cheaper, simpler and even with inferior quality if compared to existing products, but some marginal or new segment will value it. (more…)
‘Fixing the broken delivery system: the case for change” – Dean’s lecture series, City University
Prof Stanton Newman, Dean of School of Health Sciences at City University, introduced Prof Chris Ham this evening. Chris Ham is of course extremely well known as the Chief Executive of the King’s Fund.
He is also engaged directly in clinical work and holds a regular clinic at University College Hospital mainly with referrals from medical and surgical colleagues in the hospital and also from primary care.He is the Principal Investigator on the Whole Systems Demonstrator Project funded by the Department of Health to evaluate the role of assistive technologies in health and social care. The studies in this programme constitute the largest randomized controlled trials on the role and impact of telehealth and telecare devices. The whole system demonstrator project is a comprehensive evaluation of these devices to inform policy. In addition his group is conducting research on the role of them portable devices in diabetes and web-based applications to improve the management of chronic conditions.
The biography of Prof Ham appears here:
Chris Ham took up his post as Chief Executive of The King’s Fund in April 2010.
He has been Professor of Health Policy and Management at the University of Birmingham, England since 1992. From 2000 to 2004 he was seconded to the Department of Health, where he was Director of the Strategy Unit, working with ministers on NHS reform. Chris is the author of 20 books and numerous articles about health policy and management. Chris was awarded an honorary doctorate by the University of Kent in 2012.
Chris has advised the WHO and the World Bank and has served as a consultant to governments in a number of countries. He is an honorary fellow of the Royal College of Physicians of London and of the Royal College of General Practitioners, an honorary professor at the London School of Hygiene and Tropical Medicine, a companion of the Institute of Healthcare Management, and a visiting professor at the University of Surrey.
Chris was a governor and then a non-executive director of the Heart of England NHS Foundation Trust between 2007 and 2010. He has also served as a governor of the Canadian Health Services Research Foundation and the Health Foundation.
In 2004 he was awarded a CBE for his services to the National Health Service.
Rather than privatisation being the main challenge, Ham believes that inertia is the main challenge. Ham and colleagues will be producing constructive comments on how change can happen on scale and at pace. The King’s Fund is ‘the middle ground’ between theory and practice, but in an applied practical capacity. ‘This interest gets me out of bed in the morning, to improve health and healthcare’.
Chris Ham’s presentation
There are four burning platforms, not an inappropriate metaphor for health and social care.
The first burning platform is money. There are important differences in the four country, with no growth. Given the state of the economy, it could be a decade for austerity for public services including the NHS. We’ve had seven years of ‘feast’, perhaps followed by seven years of ‘famine’. After eighteen months, the situation is reasonably good. The pay freeze has helped to maintain a surplus. At a local level, there are growing financial pressures. An increasing number of organisations find themselves in deficit, struggling. The number of organisations struggle will increase.
After 18 months, it will be a test to ensure standards of patient care are maintained. John Appleby published a report on ‘Improving NHS productivity: more with the same not more of the same’. Prof David Nicholson has sought £20 bn “efficiency savings”. Everybody has to play a part in ‘Nicholson Challenge’, and this can be approached through an inverted triangle. Key decisions are made in the clinical microsystems, e.g. GPs, nurses, AHPs; prescribing, referrals, length of stay of patients, etc. It is the sum of these clinical decisions that will account for £10 bn of how the health budget is spent. Every clinical team has to eliminate waste, freeing up money for investment.
GPs were asked about the best ways of introducing efficiency savings. There is a lot of apparent agreement between GPs and hospital doctors; better coordination of care, and increased collaboration, between GPs and other services. At the time they were working on ‘Clinical and service integration: the route to improved outcomes” by Natasha Curry and Chris Ham. Getting clinical teams collaborating, and getting care for elderly people more joined-up. The means-to-the-end is better value for the resources being committed, and this paper aims to provide the evidence base from various research studies and countries, to demonstrate evidence and experience towards greater integration. The evidence is seen as ‘good enough’ to justify greater integration.
The second burning platform: the Health and Social Care Act 2012.
What does this mean?
- Massive organisational change
- Loss of experienced managers
- Increased complexity
- A focus on structures and not services
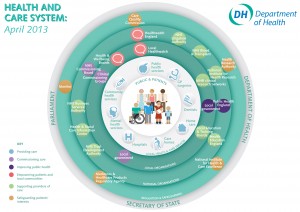
The simplified streamline map of the Department of Health (April 2013)
What does this mean?
Thatcher, Blair and Milburn started on this journey. Next chapter is the extension of choice and competition, with a bigger role for GP-led commissioning through 212 Clinical Commission Groups in England. There will be a new NHS Commissioning Board will have a major influence and its role viz a viz CCGs will be criticial. Provider reform/failure is well underway. Several healthcare providers are in financial difficulties. In South London Trust, a trust is bankrupt, and has been subject to administration. Peterborough Foundation NHS Trust has been in financial difficulty. The public will be worried about whether the hospital, GP, community nurse, are still there, and therefore whether failure is small but increasing.
The key document from the King’s Fund and the Institute of Government is Nick Timmins, “Never again?”. Timmins had unprecedented access to people involved in the genesis of the Act, a ‘who done it’ of health policy. A new team is appointed at the beginning of September. This does not signal a major change in the direction of reform. More emphasis will be placed on presentation and communication of the government’s plans. The big political challenges are about service reconfigurations, especially in hospitals.
The third burning platform is the Francis Report. There will be a delay. It will be produced very early in January 2013, bringing quality back onto the agenda. Supervisory bodies, and the role of CQCs and Monitors, in Mid Staffs NHS Foundation Trust will be scrutinised, considering systematic failures. This report will add ‘fuel to the fire’.
The government has put into place a mechanism for safeguarding quality in the NHS (National Quality Board 2010).
There are three lines of defence. The first line of defence should be the front line teams delivering care. The second line should be organisational leadership at the board level; are they talking about finance, or taking patient safety and quality-of-care seriously? The third line should be regulators and others. Organisational leadership and culture at all levels and staff engagement are critical. A focus on regulation could be erroneous, Ham believes. CQC must bear its share of responsibility, under David Bearn. You have to be realistic about what a regulator can do, and what a regulator cannot do. The experience and credibility of people who go on visits will have to be scrutinised. This will project on the King’s Fund RADAR early in the new year.
The fourth burning platform is the most important, and critically important. It is about future of services, coming from real and welcome improvements in the NHS. We have moved from very long waiting times in the NHS. NHS performance has improved greatly. Despite this, the model for health and care delivery is outmoded. We are really feeling the effects of overinvesting in hospitals and care homes, but tolerated average improvements in general practice, but been slow in technology and innovation uptake. There is a fundamental clinical, compelling, case as to how these services are provided in future.
- Report published at the beginning of September produces a foundation, hopefully. The UK has the second highest rate of mortality amenable to health care among16 high income nations, despite recent falls in death rates (Nolte and McKee, 2011). 10,000 lives would be saved each year, if England achieved survival rates at the level of the Euopean best.
- As many as 1,500 children a year might not die if the UK performed as well as Sweden, in relation to illnesses that rely on first-cass care, such as asthma and pneumonia.
- There is excess mortality in hospitals at weekends (Dr Foster Intelligence, 2011), and in London alone there would be a minimum of 500 fewer deaths a year, if the weekend mortality rate were the same as the weekday rate.
- More than half of 100 acute hospitals inspected by Care Quality Commission in 2011 were non-compliant with standards of dignity and nutrition for older people, or were found to be cause of concern (Care Quality Commission, 2011).
We have a lot of work to do: the report published by the King’s Fund is “Transforming the delivery of health and social care: the case for fundamrntal change”. It is interesting to compare the data to international data, in the form of ‘Commonwealth Fund International Ranking’. Netherland ranked first, and the UK came 2nd. Ten years ago, the rankings would be near the bottom. Long, healthy, productive lives comes 6th out of 7th (Nolte and McKee, 2011), and patient-centred care we come out bottom.
A possible future model of care might therefore have:
- Enhancing the role of patients and users in the care team (chronic diseases, long term conditions, expert patient programme)
- Changing professional routes
- Rethinking the location of care (too much reliance on nursing homes and care homes, too much focus on acute trusts)
- Using new information and communication technologies
- Harnessing the potential of new medical technologies (?better use of smartphones)
- Making intelligent use of data and information
The report deliberately does not spell out details.
“Fixing the broken system” would therefore consist of:
- Fundamental and rapid changes is needed
- More consistent standards of primary care
- Primary care working at scale through networks
- Integrated out of hospital care working 24/7
- Acute hospitals working in collaboration and with reduced role over time.
- The home as the hub of care with range of supported housing options (older people would prefer to be in the own homes, and telecare might be more important in future).
In an article dramatically titled ‘closing one in three hospitals would improve patient care’, the Guardian described:
Shutting a third of hospitals would improve quality of care and should be part of changes to the NHS that would let patients see their GP or have surgery at the weekend, a leading doctor has claimed. A dramatic centralisation of services would benefit patients by putting larger numbers of doctors in fewer places, with the inconvenience for the sick and their loved ones of having to travel further outweighed by better treatment, according to Professor Tim Evans of the Royal College of Physicians (RCP).
This is of course much of what the King’s Fund has been said before. But there has only been limited progress in effecting change this time round at scale and at pace. The issues are urgent.
Tackling the challenge of inertia
Potential strategies might include:
- Opening up the market to new providers, with new and better business models. Competition should be a tactic not a strategy.
- Existing providers to support staff to innovate. A lot of change should not come from outside, but from within.
- Decommissioning outmoded models of care
- Recognising the key role of clinical and managerial leaders, taking on politicians and vested interests.
- Risk taking needs support from politicians. We will not make progress unless there is a degree of innovation.
Selected references
Care Quality Commission (2011). Dignity and Nutrition: Inspection programme. Newcastle upon Tyne: CQC.
Dr Foster Intelligence (2011). Inside your hospital. Dr Foster Hospital Guide. 2001–2011.
Nolte E, McKee M (2011). ‘Variations in amenable mortality – trends in 16 high-income nations’. Health Policy, vol 103 no 1, pp 47–52.
When is a mutual not a mutual? When it’s a public limited company
Circle Holdings Plc is a public limited company in law, and the media characterisation of Circle as a “mutual” is at best disingenious, at worst misleading.
Mutual or public limited company?
A Guardian article recently explained the issue well. Circle appears classified as a “mutual” by the current government because 51% of the company is owned by investors, with the rest given over to workers. Co-operatives are businesses owned and run by, and for, their members. Whether the members are customers, employees or residents, they have an equal say in what the business does and a share in the profits. As a minimum, 75% of the co-op should be owned by the members – if not 100% – with democratic control.
Strictly speaking, a “mutual” exists with the purpose of raising funds from its membership or customers (collectively called its members), which can then be used to provide common services to all members of the organisation or society. A mutual is therefore owned by, and run for the benefit of, its members – it has no external shareholders to pay in the form of dividends, and as such does not usually seek to maximise and make large profits or capital gains. Critically, mutuals exist for the members to benefit from the services they provide and often do not pay income tax.
Circle chief executive Ali Parsa, in the language of mutuals, talks about “surpluses” not profits when talking on Newsnight, but talks about profits and dividends (this company is allowed to pay out dividends legally when it has distributable profits) to his shareholders in the annual reports.
The public of course would much prefer to hear about the ‘social enterprise’ ‘mutual’ end of Circle, rather than the public limited company end of it, with its share price here, and its financial reports here. When I was at medical school, a Professor of Medicine taught me about how to make a diagnosis: “If it looks like a duck, and quacks like a duck, it probably is a duck”. There’s a similar adage that a clip-clop noise outside of your house is probably a horse not a zebra.
In my view, it’s not a mutual – Circle overall is fundamentally a public limited company.
Shibley is a member of Labour, and a member of the Socialist Health Association. He has postgraduate degrees in medicine, natural sciences, law and business.
Dai Powel HCT Group’s Chief Executive takes a similar view of Circle
Circle’s financial strategy