Home » Posts tagged 'privacy'
Tag Archives: privacy
Are we actually promoting the NHS ‘choice and control’ with the current caredata arrangements?
In the latest ‘Political Party’ podcast by Matt Forde, an audience member suggests to Stella Creasy MP that wearing a burkha is oppressive and should not be condoned in progressive politics. Stella argued the case that she can see little more progressive than allowing a person to wear what he or she wants.
The motives for why people might wish to ‘opt out’ are varied, but dominant amongst them is a general rejection of commercial companies profiteering about medical data without strict consent. This is not a flippant argument, and even Prof Brian Jarman has indicated to me that he prefers a ‘opt in’ system:
Patients are not fully informed about how their information will be used. For such confidential data they should have to opt in @legalaware
— BrianJarman (@Jarmann) January 28, 2014
If people are properly told the pros and cons they can decide if they want to accept the cons, for the sake of the pros @sib313 @legalaware
— BrianJarman (@Jarmann) January 27, 2014
There are potential benefits, but also risks and if the risks happen they’re irreversible. Hence it’s safer to have opt-in. @legalaware
— BrianJarman (@Jarmann) January 27, 2014
Opting out can be argued as not being overtly political, though – it is protecting your medical confidentiality. People may (also) have political reasons for doing this, but the choice is fundamentally one about your right to a private family life. The government (SoS) has accepted this, and that is why it is your NHS Constitution-al right to opt out – you don’t have to justify it and if you instruct your GP to do it for you, she must.
It’s argued fairly reliably that section 251 of the NHS Act 2006 maps exactly onto Section 60 of the Health and Social Care Act 2001. Section 60 was implemented the following year under Statutory Instrument 2002/1438 The Health Service (Control of Patient Information) Regulations 2002. It is argued that the Health and Social Care Act 2012 did not modify or repeal those provisions of the HSC Act 2001 or the NHS Act 2006, nor did it modify or repeal any related provision of the Data Protection Act 1998. SI 2002/1438 remains in force. However, noteworthy incidents did occur under this prior legislation, see for example this:
Whatever motive you have for arguing against care.data, whether the whole principle of it, the HSCA removing any requirement for consent, the fact that it is identifiable data being uploaded from GP records (i.e. not anonymised or pseudonymised), or that the data will be made available, under section 251, for both research and non-research purposes, to organisations outside of the NHS, etc, the matter remains that the is no control over your data unless you opt-out.
Proponents of the ‘opt out’ therefore propose their two lines of action: either prevent your identifiable data being uploaded (9Nu0) and so effect a block on the release of linked anonymised or pseudonymised (potentially identifiable) data, which otherwise you cannot prevent or control; or block all section 251 releases (9Nu4), whether or not you apply the 9Nu0 code.
The point is, they argue, that you – the patient – cannot pick and choose, when, to whom, or for what purposes your data will be released. You cannot prohibit your data from being released for purposes other than research, or to organisations out with the NHS. This is completely at odds to the ‘choice and control’ agenda so massively advanced in the rest of the NHS. While it has been argued that the arguments against commercial exploitation of these data should have been made clearer beforehand, it’s possibly a case ‘I know we’re going there, but I wouldn’t start from here.’
Compelling arguments have been presented for the collection of population data. It’s argued wee need population data to do prevention and to monitor equity of access and use. It’s an open secret that the current Government is continuing along the track of privatising the NHS; arguably making it all the more important to have good data so we know what is happening. Having more of this data at all starting in the private sector, under this line of argument, is much less transparent, as it’s hidden from freedom of information from the start.
It’s, however, been argued that “the route to data access” has in fact changed. Under Health and Social Care Act (2012), it was intended that either the Secretary of State (SoS) or NHS England (NHSE) could direct HSCIC to make a new database, and – if directed by SoS or NHSE – HSCIC can require GPs (or other care service providers) to upload the data they hold. care.data represents the single largest grab of GP-held patient data in the history of the NHS; the creation of a centralised repository of patient data that has until now (except in specific circumstances, for specific purposes) been under the data controllership of the people with the most direct and continuous trusted relationship with patients. Their GP.
HSCIC is an Executive Non Departmental Public Body (ENDPB) set up under HSCA 2012 in April 2013. NHS England, the re-named NHS Commissioning Board, was established on 1 October 2012 as an executive non-departmental public body under HSCA 2012. Therefore, to suggest that the government has ‘little control’ over these arm’s-length bodies is being somewhat flimsy in argument – they were both established and mandated to implement government strategy and re-structure the NHS. There are also problems with the “greater good” argument; being paternalistic, the opposition to caredata spread bears similarity to the successful opposition to ID cards. This argument presumes that patients will benefit individually, when – and it ignores the fact that it is neither necessary or proportionate –and may be unlawful under HRA/ECHR – to take a person’s most sensitive and private information without (a) asking their permission first, and (b) telling them what it will be used for, and by who. Nobody is above the law, critically.
The fact is that the data gathered may increment the data available to research but that in its current form, care.data may actually not be that useful – it includes no historical data, for starters. And all this of course ignores the fact that care.data (and the CES that is derived from linking it to HES, etc.) will be used for things other than research, by people and companies other than researchers. That is the linchpin of the criticism. Finally, the Care Bill 2013-14 – just about to leave Committee in the Commons – will amend Section 251, moving responsibility for confidentiality from a Minister (tweets by Ben Goldacre here and here).
Anyway, the implementation of this has been completely chaotic, as I described briefly here on this Socialist Health Association blog. What now happens is anyone’s guess.
The author should like to thank Prof Ross Anderson, Chair of Security Engineering at the Computer Laboratory of the University of Cambridge, Phil Booth and Dr Neil Bhatia for help with this article.
Don’t you think it’s very odd a Conservative PM should nationalise something? What is the real issue about patient records?
Even Google gave up on their central database for health information called “Google Health”. Whilst few things are as certain as death and taxes, it is fairly certain that there is big money in big data. Lord Shutt of Greetland, Chair of the Joseph Rowntree Reform Trust Ltd. warned, in a foreword on a recent report on “the database state”, that the problem is huge, and as a society we must face up to formidable challenges. There has always been a tough balance in the law between balancing individual rights of privacy and freedom, with the State’s rights of national policy of health and security, for example. Whatever ideological position the Liberal Democrats eventually settle on, it is striking that a Conservative Prime Minister should actually advocate nationalising something.
It is unsurprising that Big Pharma would have welcomed the move. Andrew Witty, the chief executive of GlaxoSmithKline, stated to the Sunday Telegraph he welcomed the data-sharing initiative: “Any action the government takes to improve the environment in this country for life science across these activities is welcome.” The Autumn Statement (2011) had indeed signposted this. It might seem paradoxical that the Department of Health at this time wishes to embark on an initiative to make the NHS “paperless”, at a time when a reorganisation, estimated at £3bn, is currently underway. Patient data, essential for individual patient security, confidentiality and consent, are “rich pickings” for the private healthcare industry, which have not collectively paid to collect this information nor invest in the IT infrastructure of the NHS, but the ethical concerns are enormous. Personalised medicine, dependent on real-time patient information, is “the next big thing” emergency in the pharmaceutical industry, currently keeping stocks of companies very healthy. However, the professional code for Doctors, from the General Medical Council (“GMC”) is very clear on the regulation of patient confidentiality and privacy: this is contained within “Confidentiality” (2009), and clearly guides doctors on the conflicting balance between confidentiality and disclosure.
There are interesting reasons why the operational roll-out of the National Patient Record failed in 2006-7. It is now reported that all prescriptions, diagnoses, operations and test results will be uploaded on to central computers by the end of next year, and, by 2018, all NHS organisations will be expected to be able to share this information with other hospitals, GPs, ambulances and health trusts. Mr Hunt hopes local councils will sign up to similar systems, along with private care homes. As with the overall direction of travel of the NHS towards an insurance system where private companies pay “a greater part”, this blurring of the need for patient consent has been insidious.
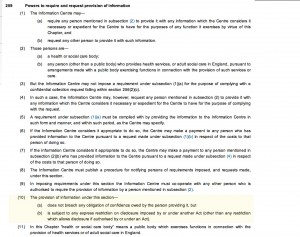
Section 251 of the NHS Act 2006 (originally enacted under Section 60 of the Health and Social Care Act 2001), allows the common law duty of confidentiality to be set aside in specific circumstances where anonymised information is not sufficient and where patient consent is not practicable. For example a research study may require access to patient identifiable data to allow linkages between different datasets where the cohort is too large for consent. This would require time limited access to identifiable information where gaining consent from a large retrospective cohort would not be feasible and would require more identifiable data than would be necessary for linkage purposes. However, section 10 of the Data Protection Act (1988) currently allows a right for an individual to prevent damage or distress by data processing. This is indeed conveniently “triggered” by section 259(10) of the Health and Social Care Act (2010), i.e. “[the provision] is subject to any express restriction on disclosure imposed by or under another Act (other than any restriction which allows disclosure if authorised by or under an Act”:
The Secondary Uses Service (SUS) Programme supports the NHS and its partners by providing a single source of comprehensive data for planning, commissioning, management, research, audit, public health and “payment-by-results”, a reimbursement mechanism for acute care payments. It is critical to know whether patients their right to opt out of the SUS database. It should not be the case that NHS patients are denied hospital care if they do not agree to my records being sent to SUS. Steve Nowottny in his “Editor’s Blog” for Pulse, a newspaper circulated to GPs, on 8 January 2013 outlined some important very recent developments:
“That year, Pulse ran a ‘Common Sense on IT’ campaign which highlighted a series of concerns over the consent and confidentiality safeguards in the new system.
“GPs wanted patients to have to give explicit rather than merely implied consent before records were created. Plans to use data within the records for research purposes without explicit consent had Catholic and Muslim leaders up in arms, because they feared the research could be purposes contrary to their faiths, such as abortion or stem cell research.
We revealed that celebrities, politicians and other patients whose information is regarded as sensitive would be exempted from the automatic creation of a Summary Care Record, raising questions about the system’s security. And we reported that patients who did not initially choose to opt out of the Summary Care Record would be unable to have their records subsequently deleted.
At the time, it felt as though the stories, while interesting and concerning, were somewhat theoretical. The Summary Care Record’s deployment to date had been patchy and it was far from certain it would continue. In the meantime, fewer than 1% of patients had bothered to opt out. (Now, with nearly 22 million records created and more than 41 million patients contacted, the figure stands at 1.34%).
But the news today that 4,201 patients had Summary Care Records created without them giving even implied consent – and that they will not be able to have them deleted – reignites the whole debate. Suddenly ‘what if’ scenarios have become reality.”
Tim Kelsey is the NCB’s National Director for Patients and Information – his stated aims are to put transparency and public participation at the centre of a transformation of customer service in the NHS. In a recent lecture, he quoted George Soros who said “our social institutions are imperfect, they should be open to improvement [and that] requires transparency and data“. On-line banking and e-ticketing demonstrate the power of open access to personal data in a safe, secure way – for some reason, heath data is deemed more personal that finance and travel arrangements. Data.gov.uk is an example of his vision for the future – the UK has so much medical data, not only about patients but also genomics and other bioinformatics disciplines. The law currently gives the NCB power to mandate more data flows – TK targets April 2014 to get outcomes-based data flows from primary and secondary care – once achieved, next step is to embrace social and specialist care. So, once the data is “freely available”, it can be made available for public participation – he is investing in a course called ‘Code for Health’, a 3 day course to learn how to develop apps. Data is essential from April 2013, there will be push for on-line interaction with GPs, to realise nationally the benefits seen in pilot areas.
So why should commissioners need access to “personal identifiable data”. It is considered that these may be “good reasons”:
- integrated care and monitoring services including outcomes & experience requires linkages across sources
- commissioning the right services for the right people requires the validation that patients belong to CCGs and have received the correct treatments
- aspects of service planning and monitoring on geographic data basis require postcodes for certain type of analysis
- understanding population and monitoring inequalities
- target support for patients and population groups at highest risk requires data from several sources linked together
- specialist commissioning is commissioned outside local areas and can require wider discussions about individual patients and their associated costs
- ensuring appropriate clinical service delivery and process requires access to records
To enable commissioning, ‘personal identifiable data’ including NHS no, DOB, Postcode data needs to flow to “data management integration centres” (“DMICs”). The DMICs need to have similar powers and controls to the Health and Social Care Act information centres to process data In order for processing of PID at DMICs to be undertaken legally, a change in legislation will be required; it is considered that legislative changes can not be achieved by April 2013, and that the new Caldicott is report expected around Jan/Feb 2013. Meanwhile, DMICs need to be operational in April 2013.
David Cameron has stated explicitly his intention for social care to head towards a private insurance system. As stated in the transcript of the interview with Andrew Marr,
“Well the point that was being made earlier on the sofa by Nick Watt, this is a massive problem – that you know more and more people suffering from dementia and other conditions where they go into long-term care and there are catastrophic costs that lead them to have to sell their homes to pay for that care – it’s right to try and put in place a cap which will then open up an enormous insurance market, so people can insure against that sort of catastrophic loss.”
A longrunning conundrum about where there is such intense interest in ‘raising awareness of dementia’. The idea of having GPs and physicians ‘diagnose’ dementia on the basis of a screening test, without it being called ‘screening’ in name, has not been backed up with the appropriate resource allocation for dementia care elsewhere in the system, including adequate training for junior doctors and nurses crucially involved in actual dementia care. Is this and integration of care an entirely virtuous sociological problem? Integration of care at first sight seems to involve primarily avoidance of reduplication of operations, and better ‘coordinated’ care between health and social care and funding. This is not an unworthy ambition at all. It is well known that the endpoint of the Pirie and Butler “Health of Nations” blueprint for NHS privatisation has a greater rôle for the private insurance market as the endpoint, so it makes complete sense to have a fully integrated IT system which private insurers and the Big Pharma can tap into. Lawyers will, of course, be cognisant about the added beauty of integration of clinical and financial information. One of the biggest banes of insurance markets is information asymmetry, making calculation of risk and potential payouts difficult. Insurers will argue that calculation of risk is only possible with precise information, and as I described earlier, clinical commissioning groups are merely “statutory insurance schemes”. It is a long-held belief that private insurers refuse to pay off given the slightest lack of compliance in terms and conditions, but private insurers provide that this mechanism needs to exist to protect them making unnecessary payouts. Failure to disclose medical conditions is an excellent way for private insurers to get out of “paying up”, otherwise known as rescission.
So, given all the above, you can see why the current Government wish to progress with this particular approach to private medical data. The private insurance market and Big Pharma stand to benefit massively, and their lobbying is much more sophisticated than lobbying from GPs, physicians or members of the public. The drive towards all nurses having #ipad3s and all TTOs from Foundation Doctors being sent by broadband to nursing homes may seem utterly virtuous, but there are more significant drivers to this agenda beyond reasonable doubt.
Where now for a law of privacy in England and Wales?
The row over court privacy rulings has come to a head in the past few days – as politicians used parliamentary privilege to name Ryan Giggs as the footballer at the centre of one injunction, and to reveal details of another injunction concerning former RBS boss Sir Fred Goodwin. However, the High Court has rejected attempts to overturn the injunction concerning Ryan Giggs – despite his name being published following MP John Hemming’s intervention in Parliament.
David Cameron has said privacy rulings affecting newspapers were “unsustainable” and unfair on the press and the law had to “catch up with how people consume media today” . He has apparently written to Mr Whittingdale and the chairman of the justice select committee, Lib Dem MP Sir Alan Beith, to ask them to suggest members for a new joint committee of MPs and peers, to consider the issue more carefully.
There are currently at least four possible “ways forward” for the new law of privacy which has been developed by the courts over the past decade and which has, at least from the point of view of sections of the media, been very controversial. These are as follows.
(1) Active steps could be taken to abolish the law of privacy and return to the pre-Human Rights Act position.
(2) The current “judge made” law of privacy could be replaced by a new “statutory tort” of invasion of privacy.
(3) A special “privacy regime” for the media could be established under a statutory regulator.
(4) “Primum non nocere” – the law of privacy could be left to develop in the current way – by the judges on the basis of the Article 8 and Article 10 case law.
Each of these possibilities gives rise to different issues and potential difficulties.
Abolition of the Law of Privacy
The law of privacy has been developed by the judges as part of the common law and the common law can be replaced by statute. The new law of privacy has been developed as a result of duty placed on the courts to act compatibly with convention rights imposed by section 6 of the Human Rights Act However, these steps would, in turn, risk placing the United Kingdom in breach of its positive obligations under Article 8 of the European Convention on Human Rights to protect privacy against media intrusion. This would, in turn, lead to adverse findings in Strasbourg and place the United Kingdom under an obligation in international law to re-introduce a law of privacy. In order to escape from this obligation it might be necessary to denounce the Convention and withdraw from the Council of Europe. As adherence to the Convention is a condition of EU membership it would also be necessary to leave the EU. of the law of privacy is not practical.
A Statutory Tort
The second possibility is the introduction of a statutory tort – a course favoured by a number of official inquiries bodies in the 1990s and the early 2000s – presents no such practical difficulties. The advantages of a new statutory tort are that it would enable clearer boundaries to be defined (although some flexibility would, of course, have to be retained). It would also give the privacy law the democratic legitimacy which the new judge made law of privacy is said to lack. This approach has been taken in a number of different common law jurisdictions. Statutory torts of privacy have been introduced in four provinces of Canada.
The Australian Law Commission has recommended the introduction of a statutory cause of action for a serious invasion of privacy containing a non-exhaustive list of the types of invasion which fall within the cause of action. It was suggested that in order to establish liability a claim would have to show:
(a) A reasonable expectation of privacy; and
(b) The act or conduct complained of is highly offensive to a reasonable person of ordinary sensibilities (See Australian Law Reform Commission, Report 108, May 2008, Recommendations 74-1 and 74-2, p.2584).
The Hong Kong Law Reform Commission proposed the introduction of a tort of invasion of privacy in the following terms:
“any person who, without justification, intrudes upon the solitude or seclusion of another or into his private affairs or concerns in circumstances where the latter has a reasonable expectation of privacy should be liable under the law of tort if the intrusion is seriously offensive or objectionable to a reasonable person.” (HKLRC Report, Civil Liability for Invasion of Privacy, 9 December 2004).
A statutory tort of this form would be unlikely to cause difficulties with Article 8 and the Convention. The United Kingdom’s positive obligation would be discharged by its introduction. The Article 8 rights of private parties would be protected by means of civil claims under this tort.
It is envisaged that the introduction of such a law would improve the ‘rule of law’, by enhancing access to justice. Currently, it is said that the present furore over superinjunctions is one in the eye for some London firms of celebrity lawyers, who have made large sums out of their new tools of “reputation management”. As a pioneer of privacy injunctions – Schillings obtained a trendsetting order in 2004 for model Naomi Campbell – the firm has not been short of new clients or referrals from media advisers. It insists it acts only on clients’ instructions and even after John Terry’s injunction was overturned last year, the firm suffered no decline in celebrities seeking gagging orders. In both the Giggs and Trafigura cases, the injunctions were destroyed by a combination of old and new forces. British politicians using the ancient powers of parliamentary privilege, combined with thousands of tweeters, often sitting at foreign-based computers and invulnerable to orders of British judges.
A Statutory Regulator
The third option – the establishment of a statutory regulator – is potentially the most radical. Such a regulator could take a wide variety of forms. The most cautious would simply be to replace the PCC with a statutory body – “OFPRESS” – performing functions similar to those performed by OFCOM in relation to the broadcast media. This may or may not command greater public confidence but would not, of itself, affect the application of the new law of privacy to the press.
Primum non nocere
The most straightforward approach is, of course, do nothing. In other words, let the judges continue the development of the law of privacy on the basis of Articles 8 and 10. This course has the advantage of requiring no Parliamentary time or difficult drafting. It is nevertheless unsatisfactory because it means that the issues arising will not be the subject of proper public debate.
As Carl Gardner notes on his blog (http://www.headoflegal.com/),
“There’s nothing wrong with the privacy law Parliament enacted in the Human Rights Act 1998, and which the judges are loyally applying – except that redtop newspapers want to breach and destroy it in their own commercial interests, and that many internet users have allowed themselves to be persuaded to flout it by a one-sided, self-serving and ill-informed media onslaught. I find it astonishing that, against the background of the News of The World phone hacking scandal, so many people swallow the claim that it’s judges who are out of control. As Alastair Campbell has implied in what he’s tweeted, what’s happened today is no victory for free speech, but for the worst of British journalism.”