Home » Posts tagged 'genomics'
Tag Archives: genomics
“Think like a multinational corporate leader. Act like the chief of the NHS.”
Simon Stevens’ catchphrase is: “Think like a patient, act like a taxpayer.”
In 2013, the US and EU decided to start negotiations on a new free trade agreement, the Transatlantic Trade and Investment Partnership (TTIP).
In a recent piece for the New Statesman, the most notable comments by Andy Burnham MP in George Eaton’s interview concerned TTIP and its implications for the NHS (apart from he was spitting bullets at aspects of HS2).
Many Labour activists and MPs had been concerned, according to George, “at how the deal, officially known as the Transatlantic Trade and Investment Partnership (TTIP), could give permanent legal backing to the competition-based regime introduced by the coalition.”
And here was Andy again at the start of the European elections (not reported by the media who were much more interested in Nigel Farage, Roger Helmer, and their ilk.)
As Benedict Cooper wrote recently on The Staggers for the New Statesman:
“A key part of the TTIP is ‘harmonisation’ between EU and US regulation, especially for regulation in the process of being formulated. In Britain, the coalition government’s Health and Social Care Act has been prepared in the same vein – to ‘harmonise’ the UK with the US health system.
“This will open the floodgates for private healthcare providers that have made dizzying levels of profits from healthcare in the United States, while lobbying furiously against any attempts by President Obama to provide free care for people living in poverty. With the help of the Conservative government and soon the EU, these companies will soon be let loose, freed to do the same in Britain …
… The agreement will provide a legal heavy hand to the corporations seeking to grind down the health service. It will act as a transatlantic bridge between the Health and Social Care Act in the UK, which forces the NHS to compete for contracts, and the private companies in the US eager to take it on for their own gain.”
So fast forward a few months.
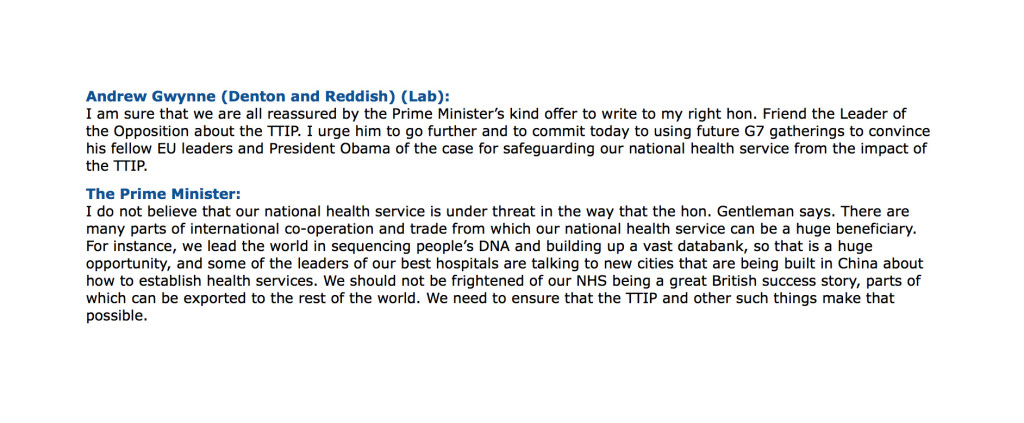
Ed Miliband asked David Cameron today specifically how TTIP would impact on the NHS.
Cameron reported today that there had been five good meetings on progressing it, and continued thus:
“We are pushing very hard and trying to set some deadlines for the work. No specific deadline was agreed, but it was agreed at the G7 that further impetus needed to be given to the talks and, specifically, that domestic politicians needed to answer any specific questions or concerns from non-governmental organisations, or indeed public services, that can sometimes be raised and that do not always, when we look at the detail, bear up to examination.”
And the attack on NGOs continued:
“I do think this is important because all of us in the House feel—I would say instinctively—that free trade agreements will help to boost growth, but we are all going to get a lot of letters from non-governmental organisations and others who have misgivings about particular parts of a free trade agreement. It is really important that we try to address these in detail, and I would rather do that than give an answer across the Dispatch Box.”
So the upshot was Cameron agreed to write to Miliband in detail to provide an update on TTIP and the NHS at last.
And this is not a moment too soon – it’s almost a year to the day since @Debbie_Abrahams asked about this on 19 June 2013 (see here).
Cameron tried also to advance the rather bizarre argument that TTIP would lift people out of poverty, trying to link up in a very Conservative approach to the free trade arrangements and the social determinants of health.
The most helpful exchange, perhaps however, was between Andrew Gwynne and the Prime Minister this afternoon:
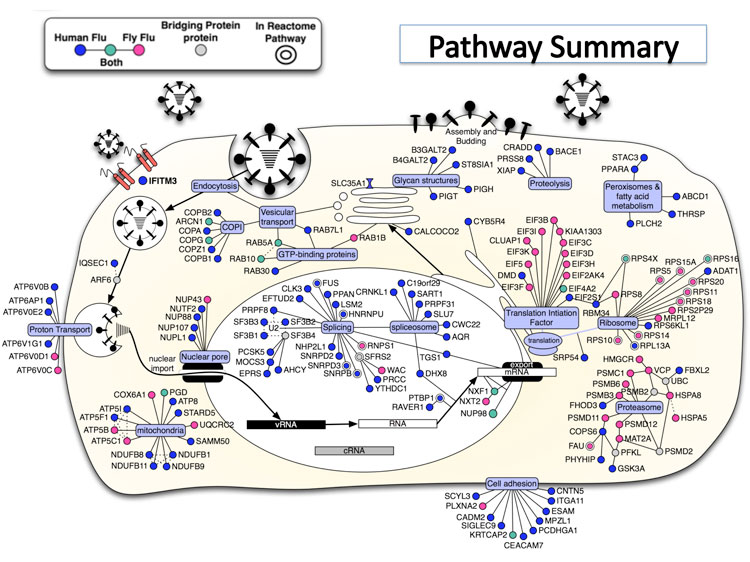
From the late 1980s, a narrative surrounding the ethics and economics of human gene patents has been taking shape into a ‘perfect storm’.
The discussion included impact of gene patents on basic and clinical research, on health care delivery, and on the ability of public health care systems to provide equitable access when faced with costly patented genetic diagnostic tests.
Scientists at institutions around the world discovered and sequenced a series of genes linked to breast and ovarian cancer in the early 1990s.
Mutations in these genes prevent the body from producing tumor suppressing proteins, which in turn increases an individual’s risk of contracting breast or ovarian cancer.
A key discovery, for example, was that individuals with these mutations have a cumulative lifetime risk of ~40–85% of developing breast cancer and ~16–40% chance of developing ovarian cancer, compared with 12.7% and 1.4% risk for the general population of developing breast or ovarian cancer, respectively.
So with these cutting edge findings in research, ‘translationary’ laboratories developed diagnostic tests for these mutations, which opened up the possibility of preventive management for breast and ovarian cancer, including prophylactic surgery and the use of certain medications.
There are countless other examples.
There also has been talk about doing a genomic screen with a view to identifying genetic risk factors for the dementias.
And Simon Stevens lovebombed the idea last week at the NHS Confederation:
“First, personalisation. A decade and a half on from the Human Genome Project, we’re still in the early days of the clinical payoff. But as biology becomes an information science, we’re going to see the wholesale reclassification of disease aetiologies. As we’re discovering with cancer, what we once thought of as a single condition may be dozens of distinct conditions. So common diseases may in fact be extended families of quite rare diseases. That’ll require much greater stratification in individualised diagnosis and treatment. From carpet-bombing to precision targeting. From one-size-fits many, to one-size-fits-one.”
So a more appropriate catchphrase for Simon Stevens might be:
“Think like a multinational corporate leader. Act like the chief of the NHS.”
One concern has been that TTIP powers would jeopardise well entrenched national laws and regulations.
Frances O’Grady of the UK’s Trade Union Congress for example, is publicly concerned that deregulation and bolstering of corporate rights could mean an accelerated privatisation of the UK’s National Health Service.
“The clauses [of ISDS] could thwart attempts by a future government to bring our health service back towards public ownership”.
A “socialist planned economy” combines public ownership and management of the means of production with centralised state planning, and can refer to a broad range of economic systems from the centralised Soviet-style command economy to participatory planning via workplace democracy.
In a centrally-planned economy, decisions regarding the quantity of goods and services to be produced as well as the allocation of output (distribution of goods and services) are planned in advanced by a planning agency.
According to Linda Kaucher, quoted in the New Statesman:
“[The Health and Social Care Act] effectively enforces competitive tendering, and thus privatisation and liberalisation i.e. opening to transnational bidders – a shift to US-style profit-prioritised health provision.”
“The TTIP ensures that the Health and Social Care Act has influence beyond UK borders. It gives the act international legal backing and sets the whole shift to privatisation in stone because once it is made law, it will be irreversible. Investor State Dispute Settlement (ISDS) laws, fundamentals of the agreement, allow corporations legal protection for their profits regardless of patient care performance, with the power to sue any public sector organisation or government that threatens their interest.”
“Once these ISDS tools are in place, lucrative contracts will be underwritten, even where a private provider is failing patients and the CCG wants a contract cancelled. In this case, the provider will be able to sue a CCG for future loss of earnings, thanks to the agreement, causing the loss of vast sums of taxpayer money on legal and administrative costs.”
Given also Andy Burnham’s reported opposition to TTIP, it would be absolutely ludicrous for the Socialist Health Association to adopt any position other than to oppose the parts of TTIP which are clearly to the detriment of the NHS. This situation, I feel, has arisen because “leaders” who’ve never set foot on a ward in a clinical capacity have little understanding of the social capital of its workforce: doctors, nurses, healthcare assistants, and all allied health professionals. It will be painful for members of the Socialist Health Association if they wish to collude knowingly with this non-socialist agenda. This is all the more telling as the Socialist Health Association seem bizarrely silent concerning the pay freeze for much of the nursing workforce.
And so the NHS strategy is beginning to take shape – parallel worlds of grassroots clinical service delivery (the unprofitable bit which costs money), and the more lucrative bit (where the State can use patient data taken from the general public on the basis of presumed con set to develop diagnostic tests and treatments, with the help of investment from venture capitalists and large charities, to export to the rest of the world under free trade agreements).
It is time for the Socialist Health Association to work out who exactly they represent?
TTIP makes intellectual asset stripping look like taking candy from a baby.
And the jury is out on Simon Stevens and the think tanks, many people will also say. But this is possibly a lost cause.
So we wait with baited breath for Ed Miliband’s reaction to David Cameron’s note about TTIP. Hopefully they will not simply agree to this agenda, ever increasing the democratic deficit.
On international collaborative data sharing and dementia. Surely “it’s good to talk”?
Plans to harvest private data from patients’ NHS files are causing a ‘crisis of public confidence’, the Royal College of GPs said this week. The professional body said it was ‘very worried’ that the public had not been properly informed about the scheme, which is due to begin this spring. Conversely, NHS managers and public health experts say the data will be used for important research and to show up poor care – and that all the data will be made anonymous. But other experts, in information security, say patients will be identifiable from their data – which will be passed on to private companies including insurance firms, and the professional regulatory code for ethics puts valid informed consent as of prime importance. A growing number of GPs oppose the care.data scheme, and say their patients will refuse to give them information for fear it will be harvested.
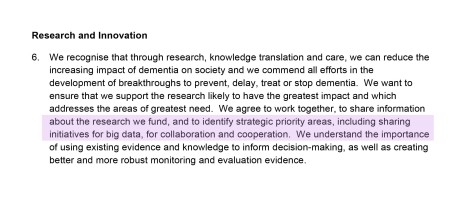
In the actual Communiqué from the G8 dementia Conference, the drive of sharing of “Big Data” was formally acknowledged. In the actual webinar, there was in fact screening of a session by corporate investors on the need to minimise risk from their investments to have the regulatory framework in place to avoid concerns over international data sharing.
Indeed, BT have taken active interest in dementia.
This eye catching headline is from the BT website: :
:
This report cites that, “the goal of finding a treatment to cure or halt dementia by 2025 is “within our grasp”, Prime Minister David Cameron has said, as he announced a doubling in UK funding for research into the disease.”
“The London conference is expected to agree to a package of measures on international information-sharing and collaboration in research. ”
These concerns include data privacy and security, and curiously do not feature above.
But the report does not even mention BT’s own Paul Litchfield, who presented even in the G8 Summit.
Last year, leaders from MedRed and BT were invited by the White House Office of Science and Technology Policy to unveil their new collaboration, the MedRed BT Health Cloud (MBHC), at “Data to Knowledge to Action: Building New Partnerships,” an event held at the Ronald Reagan Building 1300 Pennsylvania Ave NW in Washington, DC, on November 12, 2013.
MBHC is a multiyear, transatlantic effort to make available one of the largest open health data repositories in the world. It has been recognized by the Obama Administration as a high-impact collaboration that supports the Big Data Research and Development Initiative.
Designed to meet the converging needs of the life sciences and healthcare industries, the MedRed BT Health Cloud seeks to enhance integration of U.S. public data sets, such as adverse event reporting data from the U.S. Food and Drug Administration and recently released Medicare data from the Centers for Medicare and Medicaid Services, with data from the UK’s NHS and ‘other healthcare systems’.
Data currently available through the system includes several years of deidentified population health data from England, Scotland and Wales, as well as hundreds of other U.K. and data sources. It features data such as physician encounters, acute care interventions, pharmacy history, and health outcomes data.
It is argued that integration of this data with U.S. data and the addition of advanced analytics hold great potential to help speed the development of products and practices that will advance healthcare and improve the health and well-being of people around the world.
The drive for collaboration in data sharing to find a cure for dementia, most agree, is a worthy policy concern, but so is the current lack of openness in clinical data sharing which has brought about an overwhelming feeling of avoidable mistrust in the public.
The ultimate goal is the use of genomic DNA information for the development of personalised medicine.
A study testing all the DNA in the genome of cancer cells, the first of its kind reported on 7 Februrdy 2014, has identified individuals that may benefit from new treatments currently being tested in clinical trials.
Metastatic cancer – cancer that has spread from the region of the body where it first started, to other areas – is generally regarded as being incurable. In 2013, 39,620 women died from metastatic breast cancer in the US.
Progress in developing effective new chemotherapy or hormonal therapies for metastatic cancer has been slow, though there have been developments in therapies targeting specific genetic mutations in breast cancer.
We’ve all been shown Facebook adverts containing highly focused suggestions for purchases known on our known habits.
McKinseys have high hopes for the future of Big Data, indeed.
“Patients are identified to enroll in clinical trials based on more sources—for example, social media—than doctors’ visits. Furthermore, the criteria for including patients in a trial could take significantly more factors (for instance, genetic information) into account to target specific populations, thereby enabling trials that are smaller, shorter, less expensive, and more powerful.”
Of course, widespread internet access is an essential part of this technological revolution.
As regards BT, data sharing and dementia, surely it’s “good to talk” with the public who are, after all, central stakeholders?
Somebody had better tell Sid.