Home » Posts tagged 'England'
Tag Archives: England
Two Titanic democratic deficits are colliding: Scotland and the NHS
Two huge democratic deficits are about to collide: what the general public feel about the NHS and the action of governments, and also the government of Scotland.
The Health and Social Care Act (2012) did not have a single clause on patient safety. It did not speak to Mid Staffs.
Remember when David Cameron promised ‘no top down reorganisation’?
It did, however, contain a very nifty clause, distinct from the legislation which had preceded it, providing a massive legal threat to those NHS contracts which did not go out to competitive tender in section 76(7).
It was clear that this legal threat was not innocent at all, as previous experience from the Netherlands had been very costly.
I reviewed back in January 2013 that in the Netherlands, a year previously, competition law authorities fined the national GP association £6.4 million for trying to prevent the same situation as has been allowed to develop in Sweden, rural areas unserved by primary care services (reported in the British Medical Journal).
This legal pincer grip continues to have sharp teeth. Earlier this year, it was reported that a complaint by private healthcare operators had been upheld against Blackpool CCG on the basis of ‘insufficient choice’.
A lot of damage has done in the English health policy in the name of competition and choice. The idea was that competition would drive up quality and drive down costs. Because of the nature of the oligopolistic market, as would be predicted, this has not happened.
This competition policy has been aggressively pimped in the academic journals as a ‘success’ for New Labour’s health policy between 1997-2010, and together with the public private initiative and TTIP formed an unholy mess.
The privatisation of social care in England is well known to have been a disaster, an explosive mixture of austerity, outsourcing and privatisation opportunities and poor employment bargaining.
In England yesterday, the current Prime Minister framed low taxes as ‘a moral decision’. Low taxes means, however, theoretically less money you contribute to the running of public services such as the NHS, and more you can spend elsewhere for example on private health insurance.
And it has all being elegantly through: the ability to take your pension as a lump sum encourages the free movement of capital into private industry too.
The SNP have now got a clear lead in the polls, and the tendency has been for this to be under-reported in England, emphasising instead that the Conservatives and Labour are ‘neck and neck’.
Whatever the claim and counterclaim, Scotland made a clear departure from the English pro-privatisation legislation back in 2011, and is set to complete the current phase of devolution with a Scotland Bill to be presented to parliament later this year.
As a Guardian newspaper report in 2011 revealed,
“The rhetoric may be strident, but Scottish Government ministers at least practice what they preach. Across a whole range of areas, public versus private sector, telehealth, pooling health and social care and streamlining management, the devolved government has adopted a markedly different approach for the NHS in Scotland. And although that health service had long been administered separately from that in England, it was the creation of the Scottish Parliament in 1999 that made this increasing divergence politically possible.”
So a critical question becomes would the SNP be willing to vote on non-Scottish issues such as the NHS?
The answer, as of January 2015, appears to be “yes”.
Sturgeon explains:
“On health, for example, we are signalling that we would be prepared to vote on matters of English health because that has a direct impact potential on Scotland’s budget. So, if there was a vote in the House of Commons to repeal the privatisation of the health service that has been seen in England, we would vote for that because that would help to protect Scotland’s budget.”
In exchange, the SNP viewed in public during the referendum campaign that Scottish independence as producing a sustainable financial budget for the NHS, hence the smirks from Sturgeon when Nigel Farage claimed that Scotland gets a relatively good deal from “the Barnet Formula”.
Labour’s policy is for the NHS to be the “preferred provider”, but only in January 2015 the English NHS achieved its “biggest-ever privatisation of its services in a deal worth up to £780m intended to help hospitals tackle the growing backlogs of patients waiting for surgery and tests.”
But this policy does not go as far as the SNP one. For a start, the Labour policy still retains the failed quasi-market and purchaser-provider split.
The anti-austerity arguments run that if you ease off the rate of austerity then you can encourage consumer-led growth, increasing tax revenues, and encouraging a recovering economy.
The direct parallel of this is the austerity-induced ‘efficiency savings‘ in the NHS, an austerity narrative which has seen some English NHS hospitals running unsafe staffing in the aim of balancing budgets, because neoliberal parties do not wish to entertain funding the NHS properly.
The freeze on pay in nurses, therefore, looks ideologically driven, as opposed to using pay to incentivise performance of staff as in any other industry. Also, national policy appears to give the impression that nurses are immune from any recovery in the economy due to this imposed austerity, which is a crying shame.
Of course, the trade off for a more public NHS in England might be Scottish independence, but some feel the most pertinent moral argument is here that Westminster should not be governing over Scotland anyway if has few or no MPs.
Unbelievably, two democratic deficits have collided: one to do with the NHS and one to do with Scotland.
Living better with dementia: a “Year of Care” for dementia?
This is an extract from my book ‘Living better with dementia’ by me (Forewords by Prof Alistair Burns, Kate Swaffer, Chris Mason and Dr Peter Gordon), to be published by Jessica Kinglsey Publishers 2015. It comes from the chapter on whole person care (chapter 10).
Acute medicine is ideally suited to the medical model where you make a diagnosis on the basis of investigations, and then you immediately implement a management plan. There should of course be prompt action on acute situations for people living with dementia, but this is rather different to the usual needs of a person trying to live better with dementia. A person with a long term condition “lives with the condition day by day for their whole life and it is the things they do or don’t do that will make the difference to their quality of life and the long term outcomes they will experience” (Royal College of General Practitioners, 2011).
Shirley Ayres (2014) argues in her article entitled “The long term care revolution: a provocation paper” that “people in later life offer wisdom, experience, perspective and a wide range of skill sets and capacities”, reflecting that that long term institutional care is not the correct setting for them. This argument also holds true, perhaps, for people living well with advanced dementia.
The burning question still remains, as it was in the genesis of the first English dementia strategy, how a framework of post-diagnostic support for people living with dementia could best take place in England. I have already discussed earlier in chapter 10 of my book the policy of ‘whole person care’, and the critical rôle of social care practitioners and clinical nursing specialists in a multidisciplinary approach. It is also worth noting that the “year of care” initiative has seen some crystallisation of the approach for living well. It offers a framework that supports delivery of the Domain 2 of the NHS Outcomes Framework ‘Enhancing quality of life for people with long-term conditions’. Through this, it is hoped that ‘far more people will have developed the knowledge, skills and confidence to manage their own health’, but there are clear implications for the implementation of whole person care, namely, “care which feels more joined-up to the users of services”, and “care [which] centres on the person as a whole, rather than on specific conditions” (Year of Care website, accessed December 2014).
There will always be the criticism that self management, rather than having the prime goal of encouraging health and wellbeing, is meant as a ‘cover’ for essential services being cut. Benefits of “self management” which have previously been proposed are, nonetheless, proposed in Box 1.
—————
Box 1. Benefits of ‘self management’ [Source: Royal College of General Practitioners (Clinical Innovation and Research Centre) (2011) (authors: Nigel Mathers, Sue Roberts, Isabel Hodkinson and Brian Karet) Care Planning: Improving the Lives of People with Long Term Conditions]
When people self care and are supported to do this, they are more likely to:
- experience better health and well-being
- reduce the perceived severity of their symptoms, including pain
- improve medicines compliance
- prevent the need for emergency health and social services
- prevent unnecessary hospital admissions
- have better planned and co-ordinated care
- remain in their own home
- have greater confidence and a sense of control
- have better mental health and less depression
—————
Indeed, this policy agenda has been slowly ‘cooking’ for about year. For example, nearly a decade ago, Department of Health (2005) issued its document “Supporting People and integration with Long Term Conditions – An NHS and Social Care Model to support local innovation: Improving Care Improving Lives” had proposed a number of key priority areas, namely:
- To embed into local health and social care communities an effective, systematic approach to the care and management of patients with a long term condition.
- To reduce the reliance on secondary care services and increase the provision of care in a primary, community or home environment.
- Patients with long term conditions need high-quality care personalised to meet their individual requirements.
This follows on from an elegant analysis from one of Derek Wanless’ numerous reports, this time “Securing our Future Health: Taking a Long-Term View” from 2002. This one envisages one scenario for the future involving full public engagement.
Wanless (2002) describes this as,
“levels of public engagement in relation to their health are high. Life expectancy increases go beyond current forecasts, health status improves dramatically and people are confident in the health system and demand high quality care. The health service is responsive with high rates of technology uptake, particularly in relation to disease prevention. Use of resources is more efficient.”
(Derek Wanless, Public Enquiry Unit (2002))
It has become increasingly acknowledged that under this approach, the “care plan” is pivotal. The care plan “should set out the patient’s agreed health objectives and care needs, including what the individual can contribute towards their own self care, and what each professional and agency will do to help them meet these. It will include preventive and health promotion actions (such as avoiding accidents, reducing infection or nutrition).” (Department of Health, 2005).
In a pamphlet from the King’s Fund (2013), entitled “Delivering better services for people with long-term conditions”, the authors, Angela Coulter, Sue Roberts and Anna Dixon describe a co-ordinated service delivery model – the ‘house of care’ – that incorporates learning from a number of sites in England that have been working to achieve these goals.
They describe that the “house of care” model differs from others in two important ways:
- it encompasses all people with long-term conditions, not just those with a single disease or in high-risk groups;
- and it assumes an active role for patients, with collaborative personalised care planning at its heart.
This model is a system innovation, as applied to dementia, as it proposes a shift in power from professionals to persons living with dementia play an active part in determining their own care and support needs. Such an approach, it is hoped, would respect autonomy dignity, promote independence and offer maximum choice and control for need help from the health and care systems. The philosophy of “whole person care” moves the NHS towards an integrated health and care system, which is concerned about individuals during health as well as disease, a critical time when the coordination between the NHS and social care could not possibly be worse.
Self care is about individuals, families and communities taking responsibility for their own health and wellbeing. It includes actions people take in order to stay fit and maintain good physical and mental health, meet their social and psychological needs, prevent illness or accidents and care more effectively for minor ailments and long term conditions.
Both dementia and diabetes mellitus can be viewed as disabilities, and each may be a co-morbidity of the other. Sinclair and colleagues (2014) have outlined the key steps in an integrated care pathway for both elements of this clinical relationship, produced guidance on identifying each condition, dealt with the potentially risky issue of hypoglycaemia, and have outlined important competencies required of healthcare workers in both medical/diabetes and mental health settings to enhance clinical care. In the overall construct, people living with a long term condition, disability or a minor illness, as well as carers, can benefit enormously from being supported to self care.
The ‘Common Core Principles to Support Self Care’ aim to help health and social care services give people control over, and responsibility for, their own health and well-being, working in partnership with health and social care professionals (Skills for Care/Skills for Health, 2007) Seven principles have been elaborated. These are shown in Box 2 below.
—————
Box 2. Seven principles to support ‘self care’ [Source: Skills for Care/Skills for Health (2007)“Common core principles to support self care: a guide to support implementation” http://www.skillsforcare.org.uk/document-library/skills/self-care/commoncoreprinciples.pdf]
- Ensure individuals are able to make informed choices to manage their self care needs
- Communicate effectively to enable individuals to assess their needs, and develop and gain confidence to self care
- Support and enable individuals to access appropriate information to manage their self care needs
- Support and enable individuals to develop skills in self care
- Support and enable individuals to use technology to support self care
- Advise individuals how to access support networks and participate in the planning, development and evaluation of services
- Support and enable risk management and risk taking to maximise independence and choice.
—————
The “NICE quality standard for supporting people to live well with dementia: information for the public” is intended to support people to live well with dementia. It sets out how high-quality social care services should be organised and what high-quality social care should include, so that the best support can be offered to people with dementia using social care services in England (NICE, 2013). This has provided a very useful yardstick against which services which purport to improve the quality of life of people with dementia can be judged.
It is, further, reported that the ‘Year of Care’ (YOC) programme was successful in implementing the key features of care planning in diabetes, for example. The YOC Programme has two components, according to ‘Diabetes UK’ (2011). Firstly, it enhances the routine biomedical surveillance and ‘QOF review’ with a collaborative consultation, based on shared decision making and self management support, via care planning; and then it ensures there is a choice of local services people need to support the actions they want to take to improve their health, wellbeing and health outcomes.
People are involved in the care of their diabetes in quite a new way and enjoying it. People are setting personal goals and action plans relevant to their everyday life; take up of education programmes has improved and in very disadvantaged populations, poor attendance rates, biomedical outcomes and service use are also improving.
(Royal College of General Practitioners, 2011)
It is likely that the health and care sectors will seek to engineer the ‘best’ solutions on offer for post diagnostic support, within a framework of ‘whole person care’.
Such solutions might include ‘dementia advisers’, ‘clinical nursing specialists’, or ‘a year of care’. The solutions most appropriate for “living better with dementia” might be drawn, for example, from best practice in other long term conditions, such as diabetes or cancer. The quality of local commissioning, undoubtedly, is going to be pivotal in this. It will be a sensitive policy balance to make the argument that responsibilities of the State are not shunted across to the third sector in an unaccountable or unorthodox manner. But many will argue that there is valid and crucial role for the third sector to play. Actually, the policy imperative for this could not be clearer – many persons living well with dementia report not expecting to see a professional until the end of life phase, having seen one for the initial diagnosis. This is clearly not on if policy truly wishes to promote living better with dementia in England.
References
Department of Health (2005) “Supporting People and integration with Long Term Conditions – An NHS and Social Care Model to support local innovation: Improving Care Improving Lives”, accessed 6 December 2014,available at: http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/Browsable/DH_4965951
Diabetes (UK) “Year of Care: Report of findings from the pilot programme” (date June 2011), accessed 6 December 2014,available at: http://www.diabetes.org.uk/upload/Professionals/Year%20of%20Care/YOC_Report.pdf
Innovate UK (2014) The long term care revolution: a provocation paper. (author Shirley Ayres), accessed 6 December 2014,available at: https://connect.innovateuk.org/documents/15494238/0/LTCRprovocationPaper.pdf/45cf1947-c477-4f21-913e-4eb3f9061aa0
King’s Fund (2013) (authors: Angela Coulter, Sue Roberts and Anna Dixon, October 13) “Delivering better services for people with long-term conditions”, accessed 6 December 2014,available at: http://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/delivering-better-services-for-people-with-long-term-conditions.pdf
NICE quality standard 30 April 2013 NICE quality standard for supporting people to live well with dementia: information for the public, accessed 6 December 2014,available at: https://www.nice.org.uk/guidance/qs30
“Policy: A Year of Care”, accessed 6 December 2014,available at: http://www.yearofcare.co.uk/policy-0
Public Enquiry Unit (2002) “Securing our Future Health: Taking a Long-Term View. Final Report” (author Derek Wanless), accessed 6 December 2014, available at: http://si.easp.es/derechosciudadania/wp-content/uploads/2009/10/4.Informe-Wanless.pdf
Royal College of General Practitioners (Clinical Innovation and Research Centre) (2011) (authors: Nigel Mathers, Sue Roberts, Isabel Hodkinson and Brian Karet) Care Planning: Improving the Lives of People with Long Term Conditions, accessed 6 December 2014, available at: http://www.impressresp.com/index.php?option=com_docman&task=doc_view&gid=75&Itemid=70
Sinclair AJ, Hillson R, Bayer AJ; National Expert Working Group. Diabetes and dementia in older people: a Best Clinical Practice Statement by a multidisciplinary National Expert Working Group. Diabet Med. 2014 Sep;31(9):1024-31. doi: 10.1111/dme.12467.
Skills for Care/Skills for Health (2007) “Common core principles to support self care: a guide to support implementation”, accessed 6 December 2014,available at: http://www.skillsforcare.org.uk/document-library/skills/self-care/commoncoreprinciples.pdf
What happens after a diagnosis of dementia? My quick survey.
There’s been a lot of diagnosis on improving the diagnosis rates for dementia in primary care as a result of the Prime Minister’s Dementia Challenge.
This survey which you can take only once asks seven quick questions.
Each scenario is separate.
Choose the best option out of the choices given.
You can only choose one answer. There is no “correct” answer.
The questionnaire does not abruptly end. You need to scroll down to see beyond question 1.
Create your free online surveys with SurveyMonkey , the world’s leading questionnaire tool.
Trivialising dementia – too much inappropriate rocking of the boat?
When I wrote my highly successful book, “Living well with dementia”, using the phrase deliberately from the 2009 English dementia strategy document for England, I never knew the phrase was being bastardised so much for often very trivial initiatives in dementia.
On the other hand, I had huge delight in seeing its immediate relevance to a carers’ support group I went to last week.
I feel deeply hurt that the serious issues in my book, such as advocacy for mental capacity, the presentation of the cognitive neurology of the dementias, or the use of ambient-assisted technology have not been widely discussed amongst the wider community.
In that, I feel the book has failed.
I welcome proposals for the next Government to maximise money into actual service, and to re-establish health funding in line with other comparator countries.
Commissioning in dementia is now not based on what is best for the person for the person with dementia, but what is best for your Twitter commissioner friends.
I look forward to the Health and Wellbeing Boards playing a pivotal rôle in establishing some sort of normality for what commissioning in living well with dementia might be as a value-based outcome.
The strangehold of “shiny”, “off the shelf” “innovative packages”, in the drive for the current Government to ‘liberalise’ the financial market in dementia has acted for a cover for disturbing, unacceptable cuts in dementia service provision in the last few years.
I remember ‘boat rocking’ the first time around from the elegant work of Prof Debra Meyerson.
I do not wish to promote frontline professionals, many of whom have spent seven years at least at medical school or in their nursing training, to become lambs to the slaughter in the modern NHS and social care.
Keeping it real, we know that real frontline professionals in medicine and social care, even if they are not in a downright toxic environment requiring whistleblowing, can find it dangerous being risk appetitive.
Indeed, being risk appetitive, while great for innovation and leadership, can literally be deadly for patient safety.
The next Government has enough on its hands with enforcing care home standards and sanctioning for offences against the national minimum wage for paid carers as it is.
We have to think for a second for the vast army of paid workers in the NHS, as well as the rather well paid people who like their shiny new boxes, I feel.
The schism between the social media and what is happening at service level I think is most alarming, and perhaps symptomatic about how the health and social care services have begun to work in reality.
All too often, I am having first hand experience of busy frontline nurses being dragged in front of entrepreneurs in their local dementia economy to hear shills beginning, “I don’t have first hand experience of caring in dementia, but…”, before the hard sell.
This is tragically being reflected on the world stage too, though I do anticipate that the G7 legacy event from Japan which is looking carefully at their experience with care and support post diagnosis, next year, will be brilliant.
It is important for leaders in dementia to have authenticity.
I have severe doubts and misgivings about what gives the World Dementia Envoy the appropriate background and training in dementia for him to be in this important post.
It is all too easy for ‘thought leaders’ in corporate-like medical charities to have no formal qualifications or training in medicine, nursing, or social care, and opine nonetheless about weighty issues to do with policy.
I am concerned that the global ‘dementia friendly communities’ policy plank appears to have been straightjacketed through one charity in England, when it is patently obvious that various other charities such as the Joseph Rowntree Foundation have made a powerful contribution.
The media have largely not engaged in a discussion about living well with dementia, but engaged simply with Dementia Friends or a story arising out of that.
I am alarmed about the lack of plurality in the dementia research sector.
I think the All Party Parliamentary Group (“APPG”) for dementia have done some valuable work, but their lack of momentum on specialist nurses including Admiral nurses, spearheaded by the charity Dementia UK, seriously offends me.
I am sick of how the notion of ‘involvement’ of people with dementia has been abused in service provision mostly, although I am encouraged very much by initiatives such as from DEEP and Innovations in Dementia.
I think there have been genuine improvements in engaging people with dementia in research, through a body of work faithfully peer-reviewed in the Dementia Journal looking at heavy issues such as the meaning of real consent.
I am now going to draw the line of tokenistic involvement of people with dementia to front projects without any meaningful inclusion.
And in fairness, this tokenistic involvement is, I am aware, happening in various jurisdictions, not just England.
All too often, “co-production” has become code for ‘exploitation’ rather than ‘active partnership’.
The prevalence of dementia is actually falling in England, it is now thought.
The ‘dementia challenge’ was our challenge to making sure that we adequately safeguarded against people rent seeking from dementia since 2012.
In that, I think we have spectacularly failed.
I am overall very encouraged, however, with the success of the huge amount of work which has been done, including from the highly influential Alzheimer’s Society, and from the communitarian activism of “The Purple Angels”.
All this ‘radicalism’ has taken on a rather ugly, conformist twang.
Now is though time to ‘take stock’, as Baroness Sally Greengross, the current chair of the APPG on dementia, herself advised, as the new England dementia strategy is being drafted ahead of the completion of the current one in March 2015.
The Scottish referendum was, predictably, a disaster for Westminster’s historic view of the NHS
Scotland’s decision on its future, everyone knows, was as much a referendum on the past performance of the Westminster governments to date. In human resources, a guiding principle is that a candidate is likely to behave in future as he or she has down in the past, unless there are exceptional circumstances.
Andy Burnham MP was quoted himself many times as warning against the creeping privatisation of the National Health Service in England. While the ‘No’ campaign consistently explained the Westminster government had protected the NHS budget, it was widely known that the statistical authority has rebuked David Cameron for stating incorrectly that NHS spending has increased in recent years.
The ‘no’ campaign nonetheless did put up a valiant fight, with exceptional campaigners Clare Lally and Johanna Baxter, for example. These campaigners, against some formidable abuse, tried to explain why the leverage of being united with England was especially important for Scotland to withstand future economic pressures resiliently, and why it was in fact intensely patriotic to keep Scotland as part of the United Kingdom.
Whatever Andy Burnham promises as the Shadow Secretary of State for Health, it is a fact that the efficiency savings in the NHS and the private finance initiative loan repayments have put enormous pressure on the operations on the service. Managers, who all too often behave in a divorced way to frontline clinicians, do not appear easily accountable for poor staff shortages impacting on clinical patient safety.
The efficiency savings operate on the assumptions that nobody wants to pay any tax to fund the NHS properly, and that the economy is not growing. Labour, whilst rightly drawing attention to how the ‘cost of living crisis’ is damaging the wellbeing of people, cannot easily claim that people are so unwilling to fund the NHS properly. Nor can they easily dismiss that the GDP of the UK might now be improving.
The resulting democratic deficit which has happened in Scotland is therefore an extreme serious one. Whilst it is the perception that New Labour and the Conservatives, at least, have paid more attention to their friends in the City of London rather than their workforce, there has been a lack of trust between voters and the mainstream parties. Today, UNITE decided it would go on strike. Labour has not yet given a clear indication of what intends to do about the private finance initiative.
In a way, the decision for Scotland was in fact very simple. It was about making a firm decision on separating from England, rather than subjecting Scotland to another eighteen years festering with Devo Max prior to another vote. But of course, we all know it was far from simple. Whatever one’s views about Johanna Lamont or Alex Salmond, the answer of many voters is a response to David Cameron’s original question, “We can’t go on like this.” Gordon Brown’s uttered the famous words yesterday, “And proud that with the powers of the Parliament we can guarantee that the National Health Service will be in public hands, universal, free at the point of need, as long and as ever as the people of Scotland want it.”
But will the general public believe Westminster any more?
It is clear that the Westminster governments totally underestimated the passion and drive of the ‘Yes’ campaign. If Gandhi had been subject to rolling news, one wonders how the Indian independence would have turned out. But the gut feeling of many ‘Yes’ campaigners was a blatant abreaction to lies and misinformation by people who were supposed to be acting in their best interests.
Predictably, Big Business were all mobilised to depict the #iScotApocalypse #ProjectFear scenario. Unfortunately, it had Westminster’s fingerprints all over it. The Westminster delegates, including Danny Alexander, George Osborne and David Cameron, looked utterly unconvincing in raising a populist case. And the media as per usual totally screwed up the reality of the economic contribution to the rest of the UK, which is quite a formidable one albeit not as strong as London and the South East.
When Margaret Thatcher reached Downing Street in 1979, she said, “And I would just like to remember some words of St. Francis of Assisi which I think are really just particularly apt at the moment. ‘Where there is discord, may we bring harmony. Where there is error, may we bring truth. Where there is doubt, may we bring faith. And where there is despair, may we bring hope’ … and to all the British people—howsoever they voted—may I say this. Now that the Election is over, may we get together and strive to serve and strengthen the country of which we’re so proud to be a part.”
England currently is deeply divided, between rich and poor, between employed and unemployed, and, as a result of the ‘welfare reforms’, between able bodied and physically disabled. September 18th was a chance for Scotland to have a ‘clean break’.
The question is, however, will Scotland go Alex Salmond’s way?
Living well with corporate capture. What’s the future of the English dementia strategy?
“Citizens have become consumers with status proportional to purchasing power, and former public spaces have been enclosed and transformed into private malls for shopping as recreation or “therapy.” Step by step, private companies, dedicated to enriching their owners, take over the core functions of the state. This process, which has profound implications for health policy, is promoted by politicians proclaiming an “ideology” of shrinking the state to the absolute minimum. These politicians envisage replacing almost all public service provision through outsourcing and other forms of privatisation such as “right to provide” management buyouts. This ambition extends far beyond health and social care, reaching even to policing and the armed forces.”
And so write Jennifer Mindell, Lucy Reynolds and Martin McKee recently about ‘corporate capture’ in the British Medical Journal.
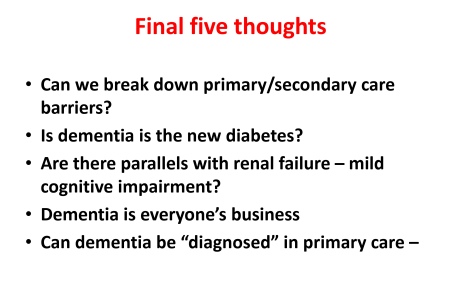
Alistair Burns, England’s clinical lead on dementia, recently concluded a presentation on the clinical network for London with the following slide:
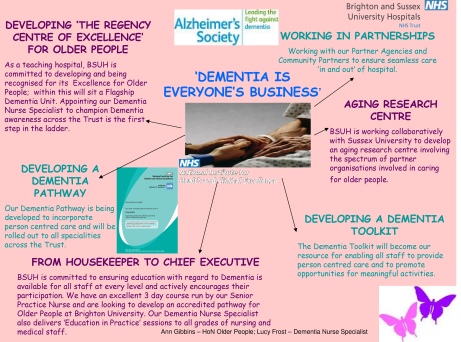
Alistair clearly does not mean ‘Dementia is everyone’s business’ in the “corporate capture” sense. Instead, he is presumably drawing attention to initiatives such as Brighton and Sussex Medical School’s initiative to promote dementia awareness at all levels of an organisation (and society).
The comparison with diabetes is for me interesting in that I think of living well with diabetes, post diagnosis, as conceptually similar to living well with dementia, in the sense that living well with a long term condition is a way of life. And with good control, it’s possible for some people to avoid hospital, becoming patients, when care in the community would be preferred for a number of clinical reasons.
Where I feel the comparison falls flat is that I do not think that it is possible to measure outcomes for living well with dementia easily. Sure, I have writen on metrics used to measure living well with dementia, drawing on the work of Sube Banerjee, Alistair’s predecessor.
It might be possible to correlate good control with a blood test value such as the HBA1c, and it steers the reward mechanism of the NHS for rewarding clinicians for failure of management (e.g. laser treatment in the eye, foot amputation, renal dialysis), but the comparison needs some clinical expertise to be pulled off properly.
The issue of breaking down ‘barriers’ between primary and secondary care is an urgent issue, and ‘whole person care’ or ‘integrated care’ may or may not help to facilitate that.
But the question of who gives the correct diagnosis of dementia, or even verifies it, won’t go away.
Having done Dementia Friends myself, a Public Health Initiative delivered by the Alzheimer’s Society, I feel the initiative is extremely well executed from an operational level. I think it’s pushing it for a member of the public to think that an old and doddering lady crossing the lady might have dementia and requires help, as medicalising ageing into dementia is a dangerous route to take.
The £2.4 million programme is funded by the Social Fund and the Department of Health.
There are a number of important clinical points here.
People with dementia need to be followed up across a period of time for a diagnosis of dementia to be reliably made, and ‘in the right hands’, i.e. of a specialist dementia service.
Some people have ‘mild cognitive impairment’ instead, and will never progress to dementia.
There are 149,186 dementia friends currently. This number is rapidly increasing. The goal is one million.
Furthermore, there are many people given a diagnosis of dementia while alive who never have it post mortem. And the diagnosis can only be definitively made post mortem.
Seth Love’s brilliant research (and he is an ‘Ambassador’ to the Alzheimer’s BRACE charity) is a testament to this.
This policy plank for me will also go back to the issue of whether policy is putting sufficient resources into the diagnostic process and beyond. Stories of people being landed with a diagnosis out of nowhere and given not much further information than an information pack are all too common. A well designed system would have counselling before the diagnosis, during the diagnosis, and after the diagnosis.
Ideally, an appointed advisor would then see to continuity of care, allowing persons with dementia to be able to feel confident about telling their diagnosis to friends and/or family. The advisor would ideally then give impartial advice on social determinants of health, such as housing or education.
But all this requires money and skill. There is no quick fix.
The areas of action for the Prime Minister’s Dementia Challenge are: dementia friendly communities, health and care and improving research.
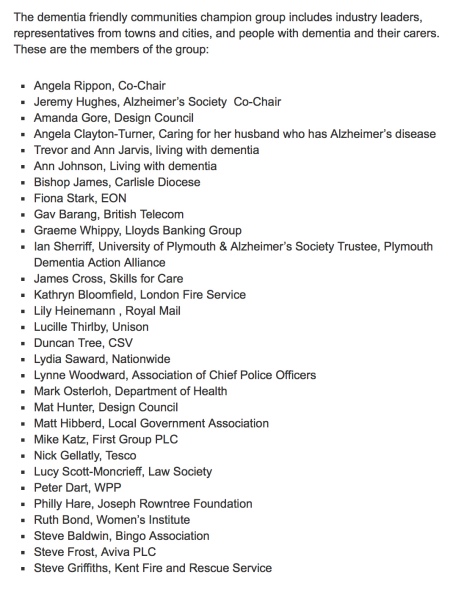
The term ‘dementia friendly communities’ is intrinsically difficult, for reasons I have previously tried to introduce. A concern must be the ideology behind the introduction of this policy in this jurisdiction. The emphasis has been very much on making businesses ‘business friendly’, which is of a plausible raison d’être in itself. This, arguably, is reflected in the list of chief stakeholders of the dementia friendly communities champion group.
It happens to fit very nicely with the Big Society and the ‘Nudge’ narrative of the current government. But it sits uneasy with the idea that it is in fact a manifestation of a small state which bears little responsibility apart from overseeing at an arm’s length a free market.
And meanwhile, the care system in England is on its knees. Stories of drastic underfunding of the care system are extremely common now.
An army of millions of unpaid family carers are left propping up a system which barely works. There appears to be little interest in guiding these people, with psychological, financial and/or legal burdens of their own, to reassure them that all their hard work is delivering an extraordinary level of person-centred care.
But this for me was an inevitable consequence of ‘corporate capture’. The G8 World Dementia Council does not have any representatives of people with dementia or carers.
That is why ‘Living well with dementia’ is an important research strand, and hopefully one which Prof Martin Rossor and colleagues at NIHR for dementia research will give due attention to in due course. But all too readily research into innovations, ambient assisted living, design of the ward, dementia friendly communities, assistive technology, and advocacy play second fiddle to the endless song of Big Pharma, touting how a ‘cure’ for dementia is just around the corner. Yet again.
So what’s the solution?
The answer lies, I feel, in what happens in the next year and beyond.
The Prime Minister’s challenge on dementia was developed as a successor to the National Dementia Strategy, with the challenge of delivering major improvements in dementia care, support and research. It runs until March 2015.
Preparatory work to produce a successor to the Challenge from the Department of Health (of England) is now underway in order that all the stakeholders can fully understand progress so far and identify those areas where more needs to be done.
The Department of Health have therefore commissioned an independent assessment of progress on dementia since 2009.
There are a number of other important pieces of work that are underway, which will provide information and evidence about progress and gaps. For example the All Party Parliamentary Group on Dementia chaired by The Baroness Sally Greengross OBE are producing a report focused on the National Dementia Strategy, and the Alzheimer’s Society has commissioned Deloitte to assess progress and in the autumn will be publishing new prevalence data.
Indeed the corporate entity known as Deloitte Access Australia (a different set of management consultants in the private sector) produced in September 2011 a report on prevalence of dementia estimates in Australia.
Deloitte themselves have an impressive, varied output regarding dementia.
But of course they are not interested in dementia solely. “Deloitte” is the brand under which tens of thousands of dedicated professionals in independent firms throughout the world collaborate to provide audit, consulting, financial advisory, risk management, tax, and related services to select clients.
Apparently, once all this work has been concluded a decision will be made on the focus and aims of the successor to the PM’s challenge.
The current Coalition government has been much criticised in parts of the non-mainstream media for the representation of corporate private interests in the Health and Social Care Act (2012).
I believe people who are interested in dementia, including persons with dementia, caseworkers and academics, should make their opinions known to the APPG in a structured articulate way in time. I think not much will be achieved through the pages of the medical newspapers.
And only time will tell whether the new dementia strategy will emerge in time before the next general election in England, to be held on May 7th 2015.
It could be a case of: all change please.
This blogpost first appeared on the ‘Living well with dementia’ blog.
Living well with corporate capture. What is the future of the Prime Minister’s Dementia Challenge?
“Citizens have become consumers with status proportional to purchasing power, and former public spaces have been enclosed and transformed into private malls for shopping as recreation or “therapy.” Step by step, private companies, dedicated to enriching their owners, take over the core functions of the state. This process, which has profound implications for health policy, is promoted by politicians proclaiming an “ideology” of shrinking the state to the absolute minimum. These politicians envisage replacing almost all public service provision through outsourcing and other forms of privatisation such as “right to provide” management buyouts. This ambition extends far beyond health and social care, reaching even to policing and the armed forces.”
And so write Jennifer Mindell, Lucy Reynolds and Martin McKee recently about ‘corporate capture’ in the British Medical Journal.
Alistair Burns, England’s clinical lead on dementia, recently concluded a presentation on the clinical network for London with the following slide:
Alistair clearly does not mean ‘Dementia is everyone’s business’ in the “corporate capture” sense. Instead, he is presumably drawing attention to initiatives such as Brighton and Sussex Medical School’s initiative to promote dementia awareness at all levels of an organisation (and society).
The comparison with diabetes is for me interesting in that I think of living well with diabetes, post diagnosis, as conceptually similar to living well with dementia, in the sense that living well with a long term condition is a way of life. And with good control, it’s possible for some people to avoid hospital, becoming patients, when care in the community would be preferred for a number of clinical reasons. Where I feel the comparison falls flat is that I do not think that it is possible to measure outcomes for living well with dementia easily. Sure, I have writen on metrics used to measure living well with dementia, drawing on the work of Sube Banerjee, Alistair’s predecessor. It might be possible to correlate good control with a blood test value such as the HBA1c, and it steers the reward mechanism of the NHS for rewarding clinicians for failure of management (e.g. laser treatment in the eye, foot amputation, renal dialysis), but the comparison needs some clinical expertise to be pulled off properly. The issue of breaking down ‘barriers’ between primary and secondary care is an urgent issue, and ‘whole person care’ or ‘integrated care’ may or may not help to facilitate that. But a future government must not get too enmeshed in sloganising if it means forgetting basic requirements of foot soldiers on the ground, such as specialist dementia nurses including Dementia UK’s ‘Admiral nurses’.
But the question of who gives the correct diagnosis of dementia, or even verifies it, won’t go away.
Having done Dementia Friends myself, a Public Health England the Alzheimer’s Society joint initiative, I feel the initiative is extremely well executed from an operational level. I think it’s pushing it for a member of the public to think that an old and doddering lady crossing the lady might have dementia and requires help, as medicalising ageing into dementia is a dangerous route to take. The £2.4 million programme is funded by the Social Fund and the Department of Health. Public Health England are planning to undertake an evaluation of the Dementia Friends Campaign launched on 7 May 2014, which will include tracking data and prevention message testing.
There are a number of important clinical points here. There are crucial questions as to whether persons themselves with a possible diagnosis, friends and/or families themselves want a diagnosis of dementia. A diagnosis of dementia in anyone’s book is a life-changing event. The concerns of the medical profession have been effectively rehearsed. Notwithstanding, the ambition that, by 2015, two thirds of the estimated number of people with dementia should have a diagnosis, with appropriate post diagnostic support has been agreed with NHS England. To support GPs and other primary care staff, a Dementia Roadmap web-based tool has been commissioned by the Department of Health from the Royal College of General Practitioners. The roadmap has now been officially launched, and will provide a framework that local areas can use to provide local information about dementia from health, social care and the third sector to assist primary care staff to more effectively support patients, families and carers from the time of diagnosis and beyond. Feedback from relevant stakeholders will be most interesting.
People with dementia need to be followed up across a period of time for a diagnosis of dementia to be reliably made, and ‘in the right hands’, i.e. of a specialist dementia service. Whilst NHS England are working with those areas with the longest waits, with the aim of ensuring that anyone with suspected dementia will not have an excessive wait for a timely assessment, there has to be monitoring of who does that timely assessment and whether it produces an accurate result. At an extreme example, clinical diagnoses of rarer dementias, particularly younger onset, can only be done effectively by senior physicians with reference to two clinical histories, two clinical examinations, neuroimaging (e.g. CT, MRI, or even fMRI or SPECT), lumbar puncture/cerebrospinal fluid (if not contraindicated), cognitive psychology, EEG, or even – extremely rarely – a brain biopsy. But this would be to propose an Aunt Sally argument – many possible cases of dementia can be tackled by primary care with appropriate testing perhaps in the future, and certainly adequate resources will need to be put into primary care for training of the workforce. Or else, it is literally a ‘something for nothing’ approach. Some people have ‘mild cognitive impairment’ instead, and will never progress to dementia.There are 149,186 dementia friends currently. This number is rapidly increasing. The goal is one million.Furthermore, there are many people given a diagnosis of dementia while alive who never have it post mortem. And the diagnosis can only be definitively made post mortem. Seth Love’s brilliant research (and he is an ‘Ambassador’ to the Alzheimer’s BRACE charity) is a testament to this. Anyway, NHS England and the Department of Health are working with the Royal College of Psychiatrists to encourage more Memory Services to become accredited.
And when is screening not officially screening? This continues to require definition in England’s policy. The original Wilson and Jungner (1968) principles have appear to have become muffled in translation. The CQUIN has led to over 4,000 referrals a month, but this will only contribute to improving diagnosis rates for dementia if this is not producing a tidal wave of false positives. For quarter 3 2013/14, 83% of admitted patients were initially assessed for potential dementia. Of those assessed and found as potentially having dementia, 89% were further assessed. And of those diagnosed as potentially having dementia, 86% were referred on to specialist services. But we do need the final figure. This policy plank for me will also go back to the issue of whether policy is putting sufficient resources into the diagnostic process and beyond. Stories of people being landed with a diagnosis out of nowhere and given not much further information than an information pack are all too common. A well designed system would have counselling before the diagnosis, during the diagnosis, and after the diagnosis.
Ideally, an appointed advisor would then see to continuity of care, allowing persons with dementia to be able to feel confident about telling their diagnosis to friends and/or family. The advisor would ideally then give impartial advice on social determinants of health, such as housing or education. Policy may be slowly moving in this direction. In April 2014 NHS England published a new Dementia Directed Enhanced Service (DES) for take up by GPs to reward practices for facilitating timely diagnosis and support for people with dementia. Patients who have a diagnosis of dementia will be offered an extended appointment to develop a care plan. The care planning discussion will focus on their physical and mental health and social needs, which will include referral and signposting to local support services. From 10 signatories in March 2012, to date, there are now 173 organisations representing nearly 3,000 care services committed to delivering high quality, personalised care to people with dementia and their carers.
But all this requires money and skill. There is no quick fix.
The areas of action for the Prime Minister’s Dementia Challenge are: dementia friendly communities, health and care and improving research.
In November 2012, The Secretary of State for Health announced a £50 million dementia-friendly environments capital investment fund to support the NHS and social care to create dementia-friendly environments. The term ‘dementia friendly communities’ is intrinsically difficult, for reasons I have previously tried to introduce. A concern must be the ideology behind the introduction of this policy in this jurisdiction. The emphasis has been very much on making businesses ‘business friendly’, which is of a plausible raison d’être in itself. This, arguably, is reflected in the list of chief stakeholders of the dementia friendly communities champion group.
It happens to fit very nicely with the Big Society and the ‘Nudge’ narrative of the current government. But it sits uneasy with the idea that it is in fact a manifestation of a small state which bears little responsibility apart from overseeing at an arm’s length a free market. The critical test is whether this policy plank might have improved NHS care. 42 NHS and 74 Social Care National pilot schemes were approved in June 2013 as national pilots. Most of the projects have now been completed, and they will be evaluated by a team of researchers at Loughborough University over the coming months. The evaluation will provide knowledge and evidence about those aspects of the physical care environment which can be used to provide improved care provision for people with dementia, their families and carers. But the policy has had some very exciting successes: for example the ‘Sporting Memories Network’, an approach based on the neural re-activation of sporting autobiographical memories, recently scooped top prize for national initiative in the Alzheimer’s Society Dementia Friendly Communities Awards 2014.
And meanwhile, the care system in England is on its knees. Stories of drastic underfunding of the care system are extremely common now. An army of millions of unpaid family carers are left propping up a system which barely works. There appears to be little interest in guiding these people, with psychological, financial and/or legal burdens of their own, to reassure them that all their hard work is delivering an extraordinary level of person-centred care.
But this for me was an inevitable consequence of ‘corporate capture’. The G8 World Dementia Council does not have any representatives of people with dementia or carers.
That is why ‘Living well with dementia’ is an important research strand, and hopefully one which Prof Martin Rossor and colleagues at NIHR for dementia research will give due attention to in due course. But all too readily research into innovations, ambient assisted living, design of the ward, dementia friendly communities, assistive technology, and advocacy play second fiddle to the endless song of Big Pharma, touting how a ‘cure’ for dementia is just around the corner. Yet again.
So what’s the solution?
The answer lies, I feel, in particularly what happens in the next year and beyond.
The Prime Minister’s challenge on dementia was developed as a successor to the National Dementia Strategy, with the challenge of delivering major improvements in dementia care, support and research. It runs until March 2015. Preparatory work to produce a successor to the Challenge from the Department of Health (of England) is now underway in order that all the stakeholders can fully understand progress so far and identify those areas where more needs to be done. The Department of Health have therefore commissioned an independent assessment of progress on dementia since 2009.
There are a number of other important pieces of work that are underway, which will provide information and evidence about progress and gaps. For example, according to the Department of Health, the All Party Parliamentary Group on Dementia chaired by The Baroness Sally Greengross OBE are producing a report focused on the National Dementia Strategy, and the Alzheimer’s Society has commissioned Deloitte to assess progress and in the autumn will be publishing new prevalence data. Indeed the corporate entity known as Deloitte Access Australia (a different set of management consultants in the private sector) produced in September 2011 a report on prevalence of dementia estimates in Australia. Deloitte themselves have an impressive, varied output regarding dementia. But of course they are not interested in dementia solely. “Deloitte” is the brand under which tens of thousands of dedicated professionals in independent firms throughout the world collaborate to provide audit, consulting, financial advisory, risk management, tax, and related services to select clients.
But also it appears that the Alzheimer’s Society, working with NHS England, has commissioned the London School of Economics to undertake a review into the accuracy of dementia prevalence data. The updated data is expected to be published in Autumn 2014. Apparently, once all this work has been concluded a decision will be made on the focus and aims of the successor to the PM’s challenge.
The current Coalition government has been much criticised in parts of the non-mainstream media for the representation of corporate private interests in the Health and Social Care Act (2012).
I believe people who are interested in dementia, including persons with dementia, caseworkers and academics, should make their opinions known to the APPG in a structured articulate way in time. I think not much will be achieved through the pages of the medical newspapers. And only time will tell whether the new dementia strategy will emerge in time before the next general election in England, to be held on May 7th 2015. However, even the most ardent critics will ultimately. The present Government should be congratulated for having made such a massive effort in educating the country about dementia, which is a necessary first step towards overcoming stigma and discrimination. The Alzheimer’s Society has impressively delivered its part of it, it appears, but future policy will benefit from much more ‘aggressive inclusion’ of other larger stakeholders (e.g. the Joseph Rowntree Foundation, Dementia UK) and smaller stakeholders.
It could be a case of: all change please. But a huge amount has been done.
“Drop in centres”. Definitely “one to watch” in the new English dementia strategy.
Access to any sort of dementia service has become the focus of scrutiny in the English dementia strategy.
For example, NHS Bristol and Bristol City Council Health and Social Care have produced a strategy document entitled ‘Living well with dementia in Bristol’ to run 2011-2015. They helpfully provide the following table on page 32.
There is considerable interest in how much ‘support’ can be provided by the NHS and social care providers, and how much can be provided by charities and other voluntary entities.
A major faultline in policy is how the third sector can lower the barriers to entry for ‘other providers’ for dementia awareness, other than the usual suspects. There is a growing momentum that any awareness is to be welcomed, wherever it comes from, but ultimately this awareness should not be for knowledge for its own sake, but should be an application to encourage inclusivity.
And all services can be a bit rushed, especially any services, medical or legal, where the end point of funding is activity-based. But conversely what people with dementia and those closest to them, whether in an official caring rôle or otherwise, invariably mention is the need for time and patience.
“Drop-in centres” have attracted much interest of late.
They offer emotional support, companionship and practical advice to people, including individuals with dementia who wish to live well independently in the community.
They’re generally run by voluntary organisations, local councils and day centres. Drop-in centre sessions usually run for a few hours at a time, one or more times a week.
The volunteers at drop-in centres are generally there to listen and provide support to those who come along, as well as to encourage people to make friends and take part in activities that interest them. Activities are especially promoted in the NICE Quality Standard 30, a strategy document which has as its aim supporting people to live well with dementia. Activities can include things like games and quizzes, arts and crafts, exercise and relaxation classes. There might also be TV, computer and internet facilities. Some drop-in centres offer educational and life-skills workshops, on topics such as developing confidence.
Individuals who use drop-in centres often have opportunities to help make decisions about how the centre is run even, and decision-making, choice and control have become key planks of dementia whichever political party is in office.
The overall aim is to provide a friendly, relaxed and unthreatening atmosphere.
Drop-in centres support people with a very wide range of needs, including older people, young people, people with learning disabilities, deaf or blind people, refugees and asylum seekers, or People facing specific health conditions such as cancer
Many drop-in centres are also open to carers, which may include families and friends of people who have these kinds of support needs. Many people in some sort of ‘caring rôle’ do not consider themselves ‘carers’, numerous successive studies find.
Drinks and snacks are often available at drop-in centres and some also offer hot meals. Some centres can help arrange transport for people who find public transport difficult to use.
And ‘drop in’ approaches might be particularly positive for people living with dementia. Often people living with dementia find the diagnosis stigmatising, but invariably people living with dementia on receiving a diagnosis still wish to live life to the full.
There are lots of services available for people living in the community who would like companionship or support during the daytime. Day centres open for longer hours than drop-in centres and offer support to older people and adults with disabilities or mental health problems. There are lunch clubs for older people too. If you feel lonely or cut off from others in the community, or can’t leave your home very often, then you might like to benefit from “companion and befriender services” arranged through the drop-in mechanism.
‘Drop in centres’ have developed a momentum of their own in England. For example, Age UK Shropshire Telford & Wrekin have opened five Diamond Drop In Centres to support local people with dementia and memory difficulties, their families, carers and friends. Previously it was reported that carers in Faversham have access to a drop in centre in their own locality. This Kingsfield team had created the drop-in service to offer support and information for both their residents’ relatives and people in the local community who are caring for someone with dementia.
Norman McNamara, Founder of Purple Angels, announced this morning that there might be plans to launch a drop in centre in Exeter. Norman admitted to being ‘quite tearful’ at having organised a previous ‘Day Lewis – Purple Angel’ drop in centre, particularly of the busy nature of the location. But it is well known that Norman McNamara has achieved an enormous amount through a remarkable amount of personal determination, as he lives with a type of dementia called diffuse Lewy Body type. This all is a noteworthy development of a campaign which ‘thinks global acts local’. Their ‘global’ website is here.
Now it turns out that “Barchester” is in full support of the Purple Angel campaign. Norman had started this campaign in Torbay – an area with a solid reputation as a retirement destination. He began by generating awareness about dementia with local businesses and soon his iconic Purple Angel stickers started appearing in shop windows around the district to show solidarity and understanding of living with dementia
Many hope that ‘drop in centres’ will feature in the new English dementia strategy 2014-9.
An innovative programme to encourage extensive knowledge sharing: the HE KSS/BSMS Primary Care Dementia Fellowship Programme
The HE KSS/BSMS (Health Education Kent Surrey and Sussex / Brighton and Sussex Medical School) have launched the “Primary Care Dementia Fellowship Programme”.
This is a programme for GPs, practice nurses and staff, and community nurses in Kent, Surrey and Sussex.
(Health Education Kent Surrey and Sussex will provide the funding to release Fellows to attend a regional skills development programme that will run from March to September 2014.
The Fellows will join with doctors and nurses from Kent, Surrey and Sussex (KSS) to build the knowledge and skills needed for them to create better dementia services in KSS.
Prof Sube Banerjee and Breda Flaherty of Brighton and Sussex Medical School (BSMS) are leading this initiative based on their successful experience in the NHS London Deanery.
It appears that the main aim is to build a network of Fellows who can act as ‘change catalysts’ (my words not theirs), to spread best contemporaneous practice in dementia care.
It’s important as dementia is one of the top five strategic priorities in the KSS Skills Development Strategy.
Modules will be led by Banerjee and Flaherty, with contributions from clinical experts in dementia; colleagues in social care; people in the care home sector; NGOs; persons living with dementia and carers; specialists in service development; commissioners and researchers.
I believe that such a course will have considerable competitive advantage in being totally disruptive in how traditional training for juniors in dementia is conducted.
The value is clearly in the collaborative ties between members of the network. By lowering the cultural barriers in this way, the team at Sussex have something very special here.
The set-up is perfect for boundary-less knowledge sharing, and this is enormously value as we all get to grips with what the priorities in local and national policy in dementia might be.
There are three modules running from March to June: good practice in dementia assessment and care, good practice in dementia, and changing practice.
These are followed by a ‘Next Steps’ conference and a period of evaluation and research.
Such an approach might become paradigmatic for future learning in the NHS in dementia.
The real influencers of English dementia policy aside from #G8dementia
In a rather strange Stakhanovite way, certain health magazines are strangely obsessed with the fetish of the ‘top 100′. I am as such not a great advocate of, “Everybody has won, and all must have prizes.” immortalised by Chapter 3 of Lewis Carroll’s Alice’s Adventures in Wonderland, but as someone who has devoted all of his entire life to dementia academia I do find somewhat curious (to put it politely) the judgments of those outside the dementia field about who are most influential to other people outside the academic dementia field, in their “world of dementia”. However, corporates need ‘symbols’ of their ‘success’ to attract inward attention and investment, so I’ll simply leave them to their own pathetic whims.
The issue of who “influences” a given network is currently of huge interest in modern ‘actor network theory’ (ANT). ANT was first developed at the Centre de Sociologie de l’Innovation of the École nationale supérieure des mines de Paris in the early 1980s by staff and visitors. Network thinking has contributed a number of important insights about social power. Perhaps most importantly, the network approach emphasises that power is inherently relational. An individual does not have power in the abstract, they have power because they can dominate others.
Network analysts often describe the way that an “actor” is embedded in a relational network as imposing constraints on the actor, and offering the actor opportunities. Actors that face fewer constraints, and have more opportunities than others are in “favourable structural positions”. Having a favoured position means that an actor may extract better bargains in exchanges, have greater influence, and that the actor will be a focus for deference and attention from those in less favoured positions. However, a key deference is that the people mentioned below do not consider themselves as requiring deference or attention. Their devotion to the living with the dementias is crystal clear. There can of course be “inhibitors”. We all know who they are: they actively stifle the activities of some members of the community.
There are many laboratories around the world which publish widely in the world on cognitive and behavioural neurology: how people think, and the brain processes involved. Of the off top of my head, I can think of Prof Bruce Miller at the University of California and San Francisco, Prof Martin Rossor at the National Hospital for Neurology and Neurosurgery and University of London (UK), Prof Facundo Manes at Favorolo Hospital, Argentina, Prof David Neary at the University of Manchester (UK), and Prof John Hodges of NeuRA, Australia.
There are of course people in fields to do with living well, for example defining wellbeing, measuring wellbeing, assistive technology, ambient assisted living, design of the home, design of the ward, and design of the built environment. Research in all these areas in English dementia policy is currently extremely important. I would go so far as to say that the people successfully working in, and publishing on, these areas around the world are much more important than the health ministers and corporate representatives who spoke at the ‘G8 dementia’ conference last week.
One person who does deserve a special mention though, even though all must have possibly have prizes, is Beth Britton. Beth’s interview captured attention at last week’s #G8dementia, and rightly so. Beth’s father had vascular dementia for 19 years. It began when Beth was around 12 years old, and would go on to dominate Beth’s life in her teens and twenties. Her father, whom she clearly adores, went for ten years without a diagnosis and he then spent none years in three different care homes. He passed away in April 2012, aged 85.
Norman McNamara from Devon was diagnosed with dementia a few years ago when he was just 50. After his diagnosis, Norman, from Torquay, began blogging online about his experiences and during a phone call with a friend he had the idea of organising the first Dementia Awareness Day on 17 September 2011. Norman particularly is really helpful in offering insights about what it’s like to ‘live with dementia’. In his recent blogpost, for example, he talks about how he doesn’t wish to be seen as being on some ‘journey’. He talks poignantly about how he is ‘living with’ dementia, not ‘dying from’ dementia, stating correctly that we are all in fact dying if one took this approach.
Kim Pennock, from Thornton-le-Dale, gave up her part-time job at Beck Isle Museum to help care for her mother who has the dementia of the Alzheimer type. Kim has become one of only 50 worldwide ambassadors for a pioneering new project to make communities safer for people with dementia. When her mother was first diagnosed, Kim said the family found it almost impossible to find the information and help they needed. Conversely, Lee set up the incredible ‘Dementia Challengers’ website to help people with dementia and the carers the right info they need to help them to live well.
In Australia, Kate Swaffer is committed to meaningful dialogue with a wide range of stakeholders about the critical issues impacting a person living with a diagnosis of dementia and their loved ones. When a person with dementia ‘comes out’ about their diagnosis, and openly admits they are living with the symptoms of, and diagnosis of dementia, there are a number of reactions and responses. Kate is one of the world’s most powerful advocates for dementia and the elderly, living well with a diagnosis of dementia; and she describes herself on Twitter (@KateSwaffer) as an “author, poet, blogger, and always trying to be a nice person”.
Back in the UK, Fiona Phillips speaks directly from her first hand experience as her mother had Alzheimer’s until her death in May 2006 and her father, who was diagnosed with the disease shortly afterwards, died in February 2012. In January 2009, Fiona presented Mum, Dad, Alzheimer’s and Me, an incredibly moving “Dispatches” documentary on Channel 4, featuring Fiona talking candidly about her struggles caring for both her parents during their respective illnesses and investigating the difficulties faced by people with the dementia of the Alzheimer type, and their families to get adequate care and support. Fiona has written a book “Before I Forget”, about her relationship with her parents and their dementia.
There are certain people who do understand particular areas of dementia policy and education. Lucy Jane Marsters is one such example, being a specialist nurse. Gill Phillips has also been pivotal in raising awarneness, generally, of the significant to personal-centred approaches in questioning quite deeply entrenched assumptions. There are also some brilliant people in innovations, such as Mike Clark, Prof Andrew Sixsmith and Prof Roger Orpwood in telemedicine and telehealth. Activities and healthy living communities are also extremely important; despite challenges in funding, like many in the dementia world, Simona Florio has been utterly resolute in supporting members of the excellent Healthy Living Club in Stockwell.
For years, magnificent Scot Tommy Whitelaw travelled the world running global merchandising operations for the Spice Girls, Kylie and U2. However, over the past few years he had become a fulltime carer my late mum, Joan, who had vascular dementia. His motivation as a carer came from the love he had for his own mum, and his experience has shown me just how tough it is to live with dementia and how many struggles it can bring. For the last year, he has been collecting carer’s life stories to raise awareness. Tommy is now working on The Dementia Carers Voices project with the Health and Social Care Alliance which will build on my ‘Tommy on Tour’ campaign by engaging with carers, collecting their life stories and raise awareness amongst health and social care professionals on both dementia and caring.
Caring for someone with dementia clearly infuses some with an incredible passion for the subject which you simply is hard to match. Sally Marciano has talked openly about supporting her mum supporting her father who later died of a dementia. She has talked openly about how the system didn’t work properly, but is very constructive about raising awareness and educational skills in the healthcare sector.
In March 2013, filmmakers and scientists come together at an event to increase the public understanding of dementia. A series of short films about dementia was presented by James Murray-White, will precede a discussion with researchers from the University of Bristol and other institutions supported by “Alzheimers BRACE”, a local charity that funds research into Alzheimer’s disease and other forms of dementia. James’ activities include being a freelance writer, journalist, reviewer, and filmmaker. James was in fact featured in last week’s #G8dementia media coverage.
Sarah Reed’s mother had Alzheimer’s disease for ten years. As a result of this, she became passionate about the quality of life of older people, especially those with dementia.?? She left a design career to found “Many Happy Returns” in order to innovate, research and develop evidence-based products to connect young and old, especially those with dementia, more meaningfully. Her goal has to change the experience of dementia for those who have it for the better, by persuading care organisations and carers everywhere that good care counts for nothing without good communication – and then helping them to deliver it.
And of course there are some brilliant influencers in the world of medicine who don’t simply regurgitate the copy fed to them. Dr Peter Gordon has produced a number of original films and articles about the ethics of the diagnosis, particularly the need for a ‘timely’ rather ‘early’ diagnosis, and potential conflicts of interest between the medical profession and the pharmaceutical industry. Dr Martin Brunet has likewise become massively influential in articulating the debate, especially, from the medical profession’s perspective of a policy ‘target’ to increase diagnosis rates. While Martin’s work is not easy, his perspective and substantial experience as a GP is invaluable, particularly in redressing other people’s motives which can too easily be too motivated by surplus and profit.
And, of course, a top influencer, even though ‘all shall have prizes’, is Prof Alistair Burns. Alistair is the clinical lead for dementia in England, and has a highly influential position in NHS England. Alistair clearly has a number of different stakeholders with which he needs to have a fair legitimate discussion about English policy. He has nonetheless steered the policy through rather turbulent times. As a senior academic and person within higher education, and someone who clearly has a very ‘human perspective’ too, his contribution to English dementia policy has been much valued and much appreciated.
Actually, I’m being totally ingenious. Most of us are actually one big happy family in the network I’m in. We have our disagreements, but we value each other. We don’t inhibit one another (which is what can go wrong with networks). For a list of #dementiachallengers, please go to the list in the top right corner of this blog. You’ll see for example Charmaine Hardy, who cares for, and adores, her husband who has a very rare form of dementia called primary progressive aphasia. Though having a well deserved break for once in Norway, for once, you can catch her on Twitter!