Home » Posts tagged 'decision-making'
Tag Archives: decision-making
I have not set out to build a social movement, but I want to do this for persons with early dementia
I received this message last night.
The thing is, I don’t buy into the profoundly negative imagery of the media, including memes such as “crippling”, “horrific”, “timebomb” and “explosion”.
Whilst some people, and caregivers, are undeniably “suffering”, you can’t expect all people to agree with this particular narrative at all times, I feel.
One of the things I’ll never forget was when my Ph.D. supervisor, Prof John Hodges, received a complaint about me doing neurocognitive assessments in a person with frontal dementia back in 1997.
This type of dementia, commoner in an age group below 60, is characterised by a personality and behavioural change early on, often in the absence of deficits in thinking such as memory or perception. You need an account from someone very close to that person with dementia, as the person himself or herself can have no insight into the changes.
I remember saying to the wife of a young man with this type of dementia, “I would never have guessed that he had a dementia”. This comment had upset her very much, and by that stage I was years into my medical training.
This one event is something I’ve never forgotten in the 16 years subsequently.
I remember I literally didn’t sleep for a week, and I was profoundly upset by this. But it does lie to the heart of some of my reservations about the term ‘dementia friendly communities’. There are some people for whom you would not be able to tell they were living with dementia.
I understand the focus on memory problems in the general media, as this can be a dominant presentation in typical Alzheimer’s disease, the commonest form of dementia. But memory is only one of the cognitive functions we have.
What unites all people with dementia is that the law makes a verdict on whether they are able to make decisions. This is called legal capacity.
Decisions impact on many aspects of life, such as working out how to spend your money, or which treatment to go for in hospital.
And capacity is very topical. Not only is the House of Lords seeking to update the Mental Capacity Act (2005), but also neuroscientists currently want to know what members of the public think about their research on decisions.
This is therefore not about denying compassion or dignity for all persons with dementia. It’s about redressing a power balance, where I feel people who’ve just received a diagnosis of dementia might learn something constructive about dementia, decisions and science of how to influence decisions.
This is profoundly about having a discussion with persons with dementia.
I’ve been on the receiving end of ‘look at my website’ and I find it intensely nauseating. But I wish my website, which I intend to build with funds from a crowdfunding campaign and scientific grant bodies, to allow persons with dementia to think about their own decisions.
It’s well known in the science of decisions for example that some ‘bad’ decisions can be avoided by not following ‘hot impulses’ or following the ‘herd effect’.
So here is my explanatory video:
Whilst I have been urged to make this campaign so that ‘it touches every person with dementia’, I do also want a grown up conversation without dumbing down any of the concepts.
A lot of feedback has concentrated on the ‘social movement’ aspect of it, but I should like to say whilst I say I would like to build one, I really mean it’s important for me personally that this gathers some momentum.
And I think it will from initial feedback from persons with dementia, and even people involved in the NHS and social care.
All too easily dementia policy can have more regard to marketing and tokenism, which lends itself to commissioning ‘tick box’ culture. My campaign is not for them.
And I’ve got a bit of a shock for some people – I am determined to make a big success of it.
@legalaware @theRSAorg amazing idea – we need to do more of this in the nhs
— Pollyanna Jones (@PollyannaJones) April 2, 2014
@legalaware @tommyNtour @dementia_2014 Great video, great idea. Need more openness- dementia isn’t going to go away, so embrace opportunity
— #HelloMyNameis Pip (@pippa_dolittle) April 3, 2014
very proud of friend & colleague @legalaware who has started this important campaign in dementia wellbeing: http://t.co/2y9dmTJkW2 please RT
— James Murray-White (@sky_larking) April 2, 2014
@legalaware I have been trying to convince people the nhs needs it’s own kickstarter platform for a while. Will be great to see if it works
— Pollyanna Jones (@PollyannaJones) April 2, 2014
@legalaware @dementia_2014 looks like a really exciting project.
— Rebecca Wassall (@Bexmoxon) April 8, 2014
My plans for a crowdfunding campaign to empower decisions in people with early dementia
The power of decisions for people living with early dementia
This project is dedicated to all persons living with dementia, carers and caregivers, all other people touched by dementia past present or future, and more.
The need
Decisions are crucial to our lives. Every person is unique.
A person’s ability to make decisions is defined legally as his or her “capacity”.
The brain is fascinating. It’s also incredibly complex. Neuroscience is beginning to work out how decision-making is affected in people with early dementia.
We’ve been told by many people who’ve been diagnosed with dementia that they’re interested in how the brain makes decisions.
Dementia can happen to anyone, but we should be motivated as all members in society to encourage people with dementia to live as well as possible.
Every individual with dementia is different. There are about a hundred different types of dementia.
The aim of this project is to build a social movement to empower people living with early dementia to think about decision-making. It’s about explaining the science of decisions in early decision. This is also about inviting people including those with dementia to think about their decision-making in an exciting way, and to participate in ways of influencing them for the better.
Our idea
This project is to design a website for all to enjoy, but including people who’ve been newly diagnosed with dementia.
This will provide exciting videos about why decisions are so pivotal in understanding dementia. We hope to produce exciting creative films to explore this topic by asking a professional filmmaker, James Murray-White, with a known interest in dementia and a proven record in film making.
We will design our website is so that they can understand the science of what a dementia is and how it affects decisions. It’ll also have an interactive blog.
The website will build on the RSA’s “Social Brain” findings in “Steer” (2010), but will also make use of cutting-edge research such as Daniel Kahneman’s “Thinking fast and slow”.
People with the earliest stages of dementia can think about their decisions.
People will know about it through my Twitter (@legalaware). We’ll also set up a special new Twitter account to promote the project.
The future
People with dementia can also tell neuroscientists what they feel they should be researching, and tell lawyers what they think about “capacity”.
They can get directly involved in policy making without any middle men, in keeping with the RSA’s philosophy and values.
With being empowered to make better decisions, people with early dementia can also lead communities. They would be not just be “involved” in communities which are “friendly” to them.
We’re also hoping that as the project establishes itself it will provide a core offering in NHS packages for people living well with dementia, a key national policy priority.
Who’s behind it?
Our team consists of three people.
1. Dr Shibley Rahman FRSA – academic in dementia, with book chapters, a book, original research papers and keen blogger on dementia http://www.livingwelldementia.org
2. Dr Marian Naidoo FRSA – dementia specialist in dementia-friendly communities
3. Kate Swaffer – a person living with dementia in Adelaide, Australia; Chair, Dementia Advisory Committee at Alzheimer’s Australia; Volunteer; a powerful advocate for people living with dementia, whose blog already has a powerful international outreach.
Rewards
Please support this project.
We are trying to raise £2500.
The ‘rewards’ for participating are awesome.
Backers will get
1. For up to 50 people: £5 or more
A special name mention/shout-out on the website,
2. For up to 30 people: Pledge £15 or more
a special limited edition e-book by the authors explaining decisions, the science of how decisions are affected in early dementia, and what all people might do to influence their decision-making
3. For up to 30 people: Pledge £15 or more
a special limited edition attractive mug so that you can demonstrate your personal involvement with this project; price includes postage and packing
4. For up to 30 people: Pledge £20 or more
a special limited edition attractive T-shirt so that you can demonstrate your personal involvement with this project; price includes postage and packing.
5. For up to 30 people: Pledge £25 or more
a special limited edition attractive tote bag so that you can demonstrate your personal involvement with this project; price includes postage and packing
6. For up to 30 people: Access to special privileged areas of the website for £40 or more pledges
- we are offering access through a special username and password unlimited access to certain protected parts of the website
- there will be special information sheets about the science of decisions and early dementia, and how they can be influenced; with special access to other resources such as videos or blog articles.
- this may be especially of interest to NHS commissioners.
6. For up to 20 people: Mentions in my new book ‘Living better with dementia’ for £30 or more pledges
I have already written a well-received book on ‘Living well with dementia’ which has very good reviews. I am offering exclusively mentions for up to 20 people involved in this project special mentions in my follow-up book ‘Living better with dementia’.
7. For up to 30 people: Invitations to a special workshop afternoon for £30 or more pledges
In our special-invite only workshops, we’ll be presenting the science of decisions, and be discussing how these are affected in early dementia, and what we know from the science about what can be done to influence them.
8. Recognition as a sponsor – pledges of £100 or more
We’ll proudly recognise your contribution on our website for a year and in our promotion of this initiative, which could include in NHS commissioning rounds.
The future
A chance to shape policy through NHS strategic commissioning decisions.
Risks and challenges
We feel that this is an incredibly exciting project, concentrating on what people with early dementia can do, rather than what they cannot do.
The main risk is that our website, described above, fails to explain the importance of decisions in early dementia. We hope as well experienced authors we’ll do a very good job of it though.
But we hope the resources will have been written in a way that is easily accessible, and inclusive by experts with considerable experience in this area.
We will instruct a proficient designer of websites, with a proven track record, to make the website for us.
Our project is all about people working together.
That brings challenges to make sure enough people feel engaged, but our experience from our involvement in social media (e.g. @legalaware with 11000 followers), interested people love being engaged.
We have put our time and effort into these projects because we believe in people getting involved – with each other, with their community, with making things better.
FAQ
The RSA’s curated area on Kickstarter selects the best new ideas to help tackle social problems that its 27,000 Fellows are looking to deliver. I’m an RSA Fellow and have been selected to be a part of this. ?Visit www.kickstarter.com/pages/rsa to see more RSA-backed projects and find out more about the RSA.
Thank you.
Why I’m on a mission to explain the science of decisions to people living with mild dementia
As a person who is physically disabled, and who has a speech impediment due to a meningitis from 2007, I am more than aware of how people can talk down to you in a patronising way.
It’s why I am very sensitive about language: for example, even with the best intentions in the world, “dementia friendly communities” conjures up an intense feeling of ‘them against us’.
It’s really important to not do anything which can cause a detriment to any group of people.
If you happen to be living with a condition which could cause you to have difficulties, this is especially important.
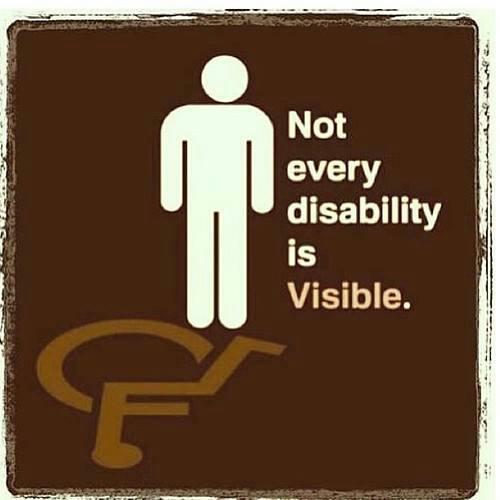
A “dementia” might be a disability under the Equality Act, and the person you’re speaking to might not obviously to you be living with a disability – it’s a ‘so-called invisibility’.
But – I’m deadly serious this. People shouldn’t be judged on what they can’t do. We all have failings of some sort. People should be encouraged for what they can do whenever possible. I don’t, likewise, consider the need for policy to embark on ‘non-pharmacological interventions’ as if what I’m talking about is second fiddle: living well with dementia is a complete philosophy for me.
In any other disability, you’d make reasonable adjustments. I see the need to explain how decisions are made to people with dementia as absolutely no different, both under the Equality Act (2010) and morally for a socially justice-oriented nation.
The excitement about how ‘decisions’ are made was recently described in the book by Prof Daniel Kahneman, “Thinking fast and slow”.
How we hold information for long enough to weigh up the pros and cons fascinates me.
Kahnemann, and others, feel that there are two systems.
System 1 is fast; it’s intuitive, associative, metaphorical, automatic, impressionistic, and it can’t be switched off. Its operations involve no sense of intentional control, but it’s the “secret author of many of the choices and judgments you make”. System 2, on the other hand, is slow, deliberate, effortful. Its operations require attention. (To set it going now, ask yourself the question “What is 13 x 27?”
Kahneman is a hero of mine as in 2002 he was awarded the Nobel Prize for economics, but he is essentially a cognitive psychologist.
In 2001, I was awarded a PhD from Cambridge for my thesis in decision-making in frontal dementia. I was the first person in the world to demonstrate on a task of decision-making that people with frontal dementia are prone to make risky decisions, despite having very high scores on standard neuropsychological tests and having full legal capacity.
Now, one coma later following my meningitis, I have done my postgraduate studies in law, and I have become fascinated by the rather arbitrary way in which our law has developed the notion of mental capacity, based on our ability to make decisions.
People with dementia can lose their ability to make decisions, so decision-making is a fundamental part of their life. As neuroscience and law straddle my life, I should like to make it my personal mission to explain the science of decision-making to people with full capacity, and who happen to have a diagnosis of dementia.
I am all in favour of a world sympathetic to the needs of people living with dementia, but this requires from us as a society much greater literacy in what the symptoms and signs of dementia are. I am not convinced we’re anywhere near that.
In the meantime, I think we can aim to put some other people in the driving seat, and they rarely get put in the driving seat: yes, that’s right, it’s time to engage people with mild dementia in the scientific debate about how decisions are made.
Chris Roberts’ plan to set up a dementia café: persons with dementia driving decision-making
There’s been a persistent concern amongst many academics and amongst many persons with dementia themselves that persons with dementia are not at the heart of decision-making in dementia-friendly communities.
The notion of ‘no dementia about me without me’ has not been rigorously applied to dementia-friendly communities, with directors of strategy in corporates seeking to consider how to make their organisations dementia-friendly as part of a corporate social responsibility or marketing strategy.
Such directors are obviously fluent in how to present such a strategy as elegant marketing, to secure competitive advantage, to make money, so it makes absolute sense for them.
It also makes sense for the Department of Health and the Alzheimer’s Society, who are seeing through the policy of ‘Dementia Friends’ through a sustainable financial arrangement, to see this policy plank politically flourish. With every single newspaper article on dementia now mentioning ‘Dementia Friends’, it is hard to see how this campaign cannot succeed.
Norman McNamara, an individual campaigning successfully and living with dementia of Lewy Body type, reported yesterday on Facebook local success around the Brixham community area.
Chris Roberts, another person in his 50s living with a dementia, also mooted the idea of setting up cafés himself.
“Since being diagnosed, i’ve noticed that there isn’t a lot for people in the mild to moderate stage. There are dementia cafes of course, but these seem to suit carers more than the people with dementia, we just sit there smiling when looked at while our carers and spouses chat away to each other, sharing there experiences and so on.”
“There are 100s of thousands of us in the same positition with nowhere to go or nowhere to be left! We could popin for an hour or for the day. We could practically run the place our selves, some where we could chat and share, watch tv, play cards, draw , we would arrange our own activities not led by someone who thinks they know what we want!”
“Yes we can live with dementia, yes we could even live well ! Yes we could live even better !”
The “living well with dementia” philosophy is all about enabling people to pursue what they can do rather what they cannot do. There’s a chapter on activities in my thesis on living well with dementia, reflecting the fact that activities are not only promoted in the current National Dementia Strategy but also in NICE Quality Standard 30 ‘Supporting people living with dementia’.
The National Dementia Strategy makes reference to such activities being ‘purposeful‘:
And this gets away from the concept of persons with dementia sitting around calmly doing knitting when they might have been, for example, proficient motorcycle bikers:
When one criticises that persons with dementia are often not at the heart of decision-making, these days I get a standard reply saying, ‘we always take serious note of the opinions of people with dementia; in fact there are two representatives on our board.’
Yet personal feedback which I receive is that persons with dementia resent this “tokenism”.
Having persons with dementia at the heart of decision-making I feel is important in the campaign to overcome stigma and discrimination against persons living with dementia. Persons with dementia running businesses of their own dispels the notion that persons with dementia are incapable of doing anything at all.
As a Fellow of the RSA, I intend to apply for a RSA Catalyst grant, as well as to the Wellcome Trust (who funded my own Ph.D. in decision-making in dementia fewer than 15 years ago now), to investigate collective decision by people in earlier stages of living with dementia to see how they in fact shape their community.
I am hoping that this will be in the context of their ongoing research work with the RSA Social Brain project, and I am hoping to hear from other Fellows about their work there, shortly. I will be putting my grant in with various people who are genuinely interested in this project.
Preface to my book: “Living well with dementia: where the person meets the environment”
Introduction
According to the Department of Health’s “Improving care for people with dementia” (2013), there are around 800,000 people with dementia in the UK, and the disease costs the economy £23 billion a year. By 2040, the number of people affected is expected to double – and the costs are likely to treble. There is no doubt therefore about the scale of the problem, and it needs the finest minds in showing leadership on how to enable individuals with dementia to live better, and indeed live well. The Prime Minister’s Challenge on dementia (“Challenge”) (2012) set out a renewed ambition to go further and faster, building on progress made through the National Dementia Strategy, so that people with dementia, their carers and families get the services and support they need. This Challenge wished to address in particular certain issues, such as the observation that the number of people with dementia is increasing, that currently the diagnosis rates are thought to be low, and there is sadly a lack of awareness and skills needed to support people with dementia and their carers. Whilst it is possibly difficult to find a ‘miracle cure’ for dementia, it is a reasonable aspiration for individuals with dementia (and their immediates) to have as best a quality-of-life as possible, and it is not necessarily the case that subtle but significant improvements in quality-of-life will “cost the earth”.
It is intended that this book should not just of interest in the UK, as the problems in healthcare are relevant to all jurisdictions. Thinking about how society should respond does pose some jurisdiction-specific issues; for example, this book refers to legislation in the UK such as the Equality Act (2010) or the Mental Capacity Act (2005), or regulations in health and safety relevant to building design in the UK. However, a consideration of the global issues in public health leads one quickly to appreciate the complexity of the economic case for improving wellbeing in individuals in dementia and their immediates, and that there are many people who are genuinely interested. Whilst indeed there has been a lead through the Prime Minister’s Dementia Challenge (2012), it is clear that previous administrations in England have latterly decided to prioritise dementia as a public health priority (for example, the National Dementia Strategy, “Living well with dementia” (2009)).
The ‘ecosystem’ of interested parties is large, and it is striking that there are so many passionate ‘#dementiachallengers’ on Twitter daily for example who are always a source of contemporary information, enthusiasm and innovation. There are currently huge advances being made in research and policy, and it is only possible through dementia communities ‘working together’ to keep abreast of them all. For that reason, this book has necessarily had to include electronic references, and I have tried to maintain links as correct as up-to-date at the time of publication. However, please feel free to look for any related information anywhere, and please do not use this book as an authoritative source of information to rely on necessarily. This book is intended simply as an introduction to a vibrant field, and certainly please be guided by healthcare professionals regarding individual care. The text of this book provides general principles, which I hope you might find interesting.
NICE quality standard 30 on ‘supporting people to live well with dementia’
In April 2013, NICE published its quality standard 30 on ‘supporting people to live well with dementia’. This quality standard was intended to cover the care and support of people with dementia. It applies to all social care settings and services working with and caring for people with dementia.
NICE quality standards are supposed to describe high-priority areas for quality improvement in a defined care or service area. Each standard consists of a prioritised set of specific, concise and measurable statements. NICE quality standards draw on existing guidance, which provide an underpinning, comprehensive set of recommendations, and are designed to support the measurement of improvement.
The areas covered in this ‘quality standard’ includes:
Statement 1. People worried about possible dementia in themselves or someone they know can discuss their concerns, and the options of seeking a diagnosis, with someone with knowledge and expertise.
Statement 2. People with dementia, with the involvement of their carers, have choice and control in decisions affecting their care and support.
Statement 3. People with dementia participate, with the involvement of their carers, in a review of their needs and preferences when their circumstances change
Statement 4. People with dementia are enabled, with the involvement of their carers, to take part in leisure activities during their day based on individual interest and choice.
Statement 5. People with dementia are enabled, with the involvement of their carers, to maintain and develop relationships.
Statement 6. People with dementia are enabled, with the involvement of their carers, to access services that help maintain their physical and mental health and wellbeing.
Statement 7. People with dementia live in housing that meets their specific needs.
Statement 8. People with dementia have opportunities, with the involvement of their carers, to participate in and influence the design, planning, evaluation and delivery of services.
Statement 9. People with dementia are enabled, with the involvement of their carers, to access independent advocacy services.
Statement 10. People with dementia are enabled, with the involvement of their carers, to maintain and develop their involvement in and contribution to their community.
Overview
The aim of this book was not to provide a prescriptive text for this quality standard. I hope the book will be useful for a ‘diverse audience’, in other words anyone interested in the diagnosis, investigation or management of dementia, with especial emphasis on improving wellbeing; such interested people might particularly include the general public, psychologists, innovation specialists,, psychiatrists, neurologists, geriatricians, general medical physicians, nurses, public health physicians, medical students, engineers, economists, psychologists, commissioners and hospital managers. It is therefore extremely hard to find all this information ‘in one place’, and it is hoped that this book will help to provide a much needed overview and to build bridges between different ‘silos’ of thinking.
The approach of the National Dementia Strategy: Living well with dementia (from the Department of Health) (2009) devotes the whole of its chapter 5 to the issue of living well with dementia. In the preceding chapter to this Strategy, chapter 4on ‘early diagnosis’, the approach described is obviously inclusive:
“From our consultation, and based on a successful DH pilot and the DH cost- effectiveness case, it appears that new specialist services need to be commissioned to deliver good-quality early diagnosis and intervention. Such services would need to provide a simple single focus for referrals from primary care, and would work locally to stimulate understanding of dementia and referrals to the service. They would provide an inclusive service, working for people of all ages and from all ethnic backgrounds.”
A ‘timely diagnosis’ is only of benefit, it is felt if there is a ‘useful’ intervention in dementia: this is described in chapter 4 has having three essential components: making the diagnosis well, breaking the news of the diagnosis well to the individual with dementia and their immediates, and providing directly appropriate treatment, information, care and support for such individuals. This timely book is part of a drive to dispel the notion that ‘nothing can be done’ in the context of management of dementia, even if current pharmacological therapies might have limited efficacy. The book is an overview of the field, describing what ‘wellbeing’ actually means, and why it is important in the context of national policy. The book quickly establishes the importance of the ‘person’ in discussing dementia care, including independence, leisure and other activities, and, in the final stages, end-of-life care, which is a discussion which should not be avoided. No individual with dementia should be abandoned in relation to his or her environment, and indeed there is much evidence to support the idea that the environment can be optimised to improve the wellbeing of an individual with dementia and his/her immediates. Considerations include home and ward design, the use of assistive technologies and telecare, and the ‘built environment’. A constructive interaction of an individual with his or her environment is clearly vital, and this includes understanding communication issues, how to champion the rights of an individual living well with dementia through independent advocacy, and the way in which ‘dementia friendly communities’ can be supported.
Contents
- Introduction
- What is “living well with dementia”?
- Measuring living well with dementia
- Socio-economic arguments for promoting living well with dementia
- A public health perspective on living well in dementia, and the debate over screening
- The relevance of the person for living well with dementia
- Leisure activities and living well with dementia
- Maintaining wellbeing in end-of-life care for living well with dementia
- Living well with specific types of dementia: a cognitive neurology perspective
- General activities which encourage wellbeing.
- Decision-making and an introduction to advocacy in living well with dementia
- Communication and living well with dementia
- Home and ward design to promote living well with dementia
- Assistive technology and living well with dementia
- Ambient-assisted living well with dementia
- The importance of built environments for living well with dementia
- Dementia-friendly communities and living well with dementia
- Conclusion
Chapter synopses
It is possible to read each chapter in this book independently, and indeed each chapter is independently referenced.
Chapter 2 is an introduction to the whole book. Introduces the concept of what is like to ‘live well with dementia’. Investigating wellbeing has broadened the scope of previously overly narrow approaches to healthcare, in measuring outcomes. This chapter also introduces the idea that it is grossly unfair to consider ‘dementia’ as an unitary diagnosis, as in fact the term is a portmanteau of hundreds of different conditions at least. There has been a growing trend that ‘dementia’ and ‘memory problems’ are entirely synonymous, and this has added unnecessary noise to the debate. Dementia care is currently done in a number of different settings, and assisted living may be of increasing relevance in a drive to encourage individuals to live well independently with dementia.
Chapter 3 presents the formidable challenges of how ‘living well’ might be measured in general. There are issues about how quality of life measures change as a dementia progresses, what the relationship might be between wellbeing and physical health, and how wellbeing in dementia should be measured accurately at all.
Chapter 4 looks at the current socio-economic arguments for promoting a wellbeing approach in dementia. There are a number of converging cases for considering wellbeing, such as the economic case, the ethical case and a case based on social equality. While resources are limited, serious considerations have to be made as to which interventions are truly cost-effective, including of course the assistive technologies.
Chapter 5 presents the background for dementia as a public health issue in the UK. There is also a very active debate as to whether one should ‘screen’ for dementia. A core aim of the National Dementia Strategy (1999) is therefore to ensure that effective services for early diagnosis and intervention are available for all on a nationwide basis. It is argued, in this Strategy, that “the evidence available also points strongly to the value of early diagnosis and intervention to improve quality of life and to delay or prevent unnecessary admissions into care homes.”
Chapter 6 considers how and why being a ‘person’ has become so central to living well with dementia in academic and practitioner circles. In a way, the approach of ‘person-centred care’ is a historic one, but it has been a consistent strand of English health policy developing into contemporaneous views of integrated and whole-person care. This chapter also introduces ‘personhood’, and the approach of ‘dementia care approach’.
Chapter 7 addresses the specific rôle of leisure activities for an individual with dementia. Leisure activities are generally considered for many to be beneficial for the mental and physical wellbeing of individuals with dementia, and there are specific problems to be addressed such as the reported levels of relative inactivity in care homes.
Chapter 8 details how wellbeing is relevant also to end-of-life in dementia. This chapter considers the importance of support for carers, for the wellbeing of individuals with dementia and their carers. This chapter considers where optimal care could be given for individuals with dementia, the contribution of medication, but how it is vital to address specific issues in advanced dementia which have a direct impact on wellbeing (such as pain control).
Chapter 9 identifies that it is in fact it is impossible to consider dementia as a unitary diagnosis, and that specific forms of dementia can present their own formidable demands and issues. This chapter considers in detail how and why memory problems can be a presenting feature of dementia of the Alzheimer type, and the implications for interventions in wayfinding which could rationally improve wellbeing in such patients. The chapter also includes recent elegant work about the neural networks which are hypothesised to be important in behavioural variant frontotemporal dementia, and how this “social context network model” fundamentally affects our notion of wellbeing in such individuals.
Chapter 10 introduces ‘general activities which encourage wellbeing’, in a first chapter on the possibility of “assistive technologies” in enabling individuals with dementia to live well. Certain memories can be particularly potent in the dementia of the Alzheimer Type, and, whilst the ‘jury is possibly out’ on the validity of reminiscence therapy, the chapter discusses the possible benefits of the CIRCA project on the wellbeing of individuals with dementia. Other activities are also considered; how they may help wellbeing, such as dancing, exercise, and music.
Chapter 11 takes up an important theme in living well with dementia; that is empowering the invididual to make decisions, the law relating to capacity, and how independent advocacy services have a beneficial rôle to play. Independent dementia advocacy is a critical area of a statement in NICE QS30, and this chapter reviews types of advocacy (and its relevance to wellbeing and person-centred care), the current mental capacity legislation, and the crucial importance of diversity and equality in policy.
Chapter 12 explains why good communication is so crucial in the setting of individuals living well with, but not simply restricted to healthcare professionals. This not only appears to be in terms of providing information about the condition locally, but also face-to-face communication with people living well with dementia. This chapter looks in detail at both verbal and non-verbal methods of communication, with a view to raising awareness of their impact on living well with dementia.
Chapter 13 analyses the importance of home and ward design for improving wellbeing in dementia. ‘Therapeutic design’ is a central philosophy of good design, and this chapter has as its focus a number of different setting. General principles are described as how to wellbeing can be improved through careful design of certain parts of the house (such as balconies, bathrooms, bedrooms, living rooms and dining rooms), and considers the neuroscience of sensory considerations at play (for example in lighting and vision, and sound and hearing.)
Chapter 14 is the first of two chapters on ‘assistive technologies’ in dementia, providing an overview of this important area for living well with dementia. This chapter explains what ‘assistive technology’ is, what its potential limitations are, the INDEPENDENT project, the importance of “telehealth” (and important ethical considerations), and the design of ‘smart homes’.
Chapter 15 is the second of two chapters on ‘assistive technologies’ in dementia, looking specifically at an approach called ‘ambient-assisted living’ (AAL). The rationale behind the use of AAL in improving wellbeing is explained, as well as the general issue of how to encourage adoption of innovations in an older population. Detailed examples of specific AAL projects in improving wellbeing are described including SOPRANO, COACH and NOCTURNAL.
Chapter 16 introduces the general emphasis on the ‘built environment’ setting, and how inclusivity still drives this area of work in living well with dementia. Ageing presents its own challenges including opportunities and threats, but this chapter focuses on the remarkable initiatives which have recently taken place in improving the outside environment for individuals with dementia. The chapter details the I’DGO project, and highlights the especial importance of inclusive design for furthering wellbeing in dementia outside environments.
Chapter 17 considers how an individual with dementia lives as part of the rest of a community and society, and policy initiatives which have sought to address this. The discussion is unexpectedly problematic about a need to define what a ‘community’ might be, but the chapter includes domestic and international approaches to the ‘dementia-friendly community’, including the RSA’s “Connected Communities” and WHO’s “age-friendly communities” initiatives. As a central policy plank which is thought to be critical for developing wellbeing in individuals with dementia and their immediates, this chapter considers why dementia-friendly communities are worth encouraging at all, why there is a societal need to involve individuals with dementia in their communities, what aspects individuals with dementia wish from such communities (including the “Four Cornerstones” model), and the benefits of “resilient communities”.
Further information
You are advised to look at specialty websites which are devoted to all the dementias (such as medical charities), which often have useful information factsheets and booklets. Also, the Department of Health and their ‘Dementia Challenge’ website is an impressive source of information. You are also advised to consult https://www.evidence.nhs.uk which has access to a number of useful contemporaneous clinical evidence sources. Online medical journals are also an excellent source of peer-reviewed research, such as the BMJ, the Lancet, and the New England Journal of Medicine.
Looking to the future
There are, of course, no “right answers” to many issues, and a wise person is a person who knows where to find relevant information. However, the sense of optimism and goodwill is a genuine one in UK health policy, regarding dementia. Whilst there will often be difficult debates regarding dementia such as “How willing should a GP be to make a diagnosis of dementia when a patient has only gone to see his GP because of a sore throat?” or “Should we look to research a drug which can immunise people against dementia?”, the fact there are so many bright people in the UK working in areas relating to dementia is a real credit to English health policy as it faces formidable challenges of its own.
References
Department of Health (2009). Living well with dementia: A National Dementia Strategy: Putting people first. London: Her Majesty’s Stationery Office. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/168221/dh_094052.pdf.
Department of Health (2013) The Dementia Challenge. London: Her Majesty’s Stationery Office. Available at: http://dementiachallenge.dh.gov.uk
Department of Health (2013) Improving care for people with dementia. London: Her Majesty’s Stationery Office. Available at: https://www.gov.uk/government/policies/improving-care-for-people-with-dementia
Department of Health (2012) The Prime Minister’s “Dementia Challenge”: Delivering major improvements in dementia care and research by 2015. London: Her Majesty’s Stationery Office. Available at: https://www.gov.uk/government/policies/improving-care-for-people-with-dementia
National Institute for Clinical Excellence (2013). Supporting people to live well with dementia (QS30). Available at: http://guidance.nice.org.uk/QS30.
UK government. Mental Capacity Act (2005) http://www.legislation.gov.uk/ukpga/2005/9/contents