Home » Posts tagged 'Big Pharma'
Tag Archives: Big Pharma
Now that Maria Miller’s finally left, it’s time to welcome ‘dementia pharma’ to the last chance saloon
In everyday English, a “last chance saloon” means a situation beyond all rational hope.
After decades of working on drugs for Alzheimer’s disease (AD), the best the industry can manage is some drugs which have some effect on symptoms for a few months, but for which there’s no evidence they delay the progression in the long term.
Big Pharma have maintained this deception uptil the very last minute, indeed uptil the patents ran out.
They know they’re now drinking at “the last chance saloon”.
David Cameron backed Maria Miller, and that failed.
He backed the Big Society, and that failed.
Now he has backed research into dementia-busting medications.
After a 16-month inquiry, a verdict was reached on Maria Miller.
Commissioner Hudson found that Miller should have designated the Wimbledon property as her main residence, that she should have reduced her claims by two-sevenths to take account of her parents’ presence and that she overclaimed for interest on the mortgage by around £45,000.
Nonetheless, there was no indication Miller had done anything unlawful or illegal in her deception.
On the other hand, the Japanese drugs company Takeda was fined a record £3.6bn ($6bn) by a federal court in the United States on 8 April 2014 following claims that it concealed a possible link between the drug pioglitazone and bladder cancer.
The fine is the largest to be imposed on any pharmaceutical company.
Takeda’s US partner Eli Lilly, who marketed and sold pioglitazone in the United States between 1999 and 2006, also received a £1.79bn ($3bn) fine.
The diabetes drug pioglitazone, marketed as Actos in the US, received marketing authorisation in Europe in 2000. Actos is marketed and sold in the United Kingdom by Takeda UK Ltd.
Today we found out that Tamiflu doesn’t work so well after all. Roche, the drug company behind it, withheld vital information on its clinical trials for half a decade, but the Cochrane Collaboration, a global not-for-profit organisation of 14,000 academics, finally obtained all the information.
Putting the evidence together, it has found that Tamiflu has little or no impact on complications of flu infection, such as pneumonia.
The huge scandal, of course, is that scandal Roche broke no law by withholding vital information on how well its drug works.
Elsewhere, standardised tobacco packaging is intended to reduce the appeal of tobacco products by removing advertising and increasing the prominence of health warnings.
This measure has strong support from health professionals, particularly as rates of child uptake of smoking are still unacceptably high.
Tobacco industry misrepresentation of the evidence in order to try to block public health interventions by manipulating policy making and public opinion is now well documented.
On March 2011, the National Health Service’s National Institute for Health and Care Excellence (NICE) concluded that donepezil hydrochloride (trade name Aricept, Pfizer) could be ‘recommended as (an option) for managing mild as well as moderate AD’.
The conclusion was drawn despite reportedly poor cost efficacy3 and opinions that the use of the drug is a ‘desperate measure’.
The NICE decision was based on two meta-analyses (the second was an update of the first) of randomised controlled trials (RCTs) that demonstrated donepezil’s effect on measures of cognition, behaviour, function and global skills.
Of the 19 studies included, 12 were produced by the companies that manufacture and market donepezil. And a recent study has found that the effect size of donepezil on cognition is larger in industry-funded than independent trials and this is not explained by the longer duration of industry-funded trials.
The history of anti-dementia drugs is inglorious. This is significant because every pound spent in flogging this dead horse is a pound denied from current persons living well with dementia.
Tacrine is an oral acetylcholinesterase inhibitor previously used for therapy of Alzheimer disease. Tacrine therapy has been linked to several instances of clinically apparent, acute liver injury.
Because of continuing concerns over safety and availability of other acetylcholinesterase inhibitors, tacrine was withdrawn from use in 2013.
And it is widely reported that current candidate drugs for Alzheimer’s disease are running into problems because of their side effect profile.
Maria Miller may have finally left the ‘last chance saloon’.
But it can’t have escaped Big Pharma, despite ‘the G8 dementia summit’, possibly the largest PR stunt for pharma and research funded by pharma in history, that they are currently drinking there.
The deceptions might be so far be legal.
Maria Miller’s claims might have been hyperbolic; at least she didn’t have a highly staged G8 summit afterwards.
But, as with Maria Miller, the court of public opinion may provide otherwise.
Specialised organisations of persons with dementia and carers are needed to promote the wellbeing agenda
One of the biggest illusions, and this is not a ‘complaint’ about this jurisdiction only, is that large dementia charities represent the views of persons with dementia.
They have a myriad of different influences, and certainly it has become dangerous that they legitimise policy directions from which many persons with dementia and caregivers can become totally disenfranchised.
This leaves persons with dementia two options.
The first option is that they can hope to influence large dementia charities better, but this is an impossible task. They act in organised corporate ways, with much marketing and branding power, so if they decide not to adopt the agenda of persons with dementia and carers it would not be altogether surprising.
The second option is to form strategic alliances with general patient groups, but not all persons with a long term condition are ‘users’ of healthcare services which thus far have typically concentrated on illness rather than health.
The third way, and this is in my opinion the most realistic option is to organise better a national and international network of groups focused on the needs of, and run by, persons with dementia.
There are, however, very impressive carers organisations, and many of their competences and aims align with the person-driven agenda for wellbeing.
The uphill task for those of us pursuing a living well with dementia agenda is truly formidable. Cholinesterase inhibitors, the frontline drugs for treating memory problems in Alzheimer’s disease, have annual sales in the billions, but have very modest effects in the vast majority of patients. They do not reverse or markedly slow down the disease either.
I feel that getting in lost in a definition of wellbeing, and how we measure it, is not the way to win the argument, although clearly relevant to how commissioning for integrated care might happen in future, say through value-based commissioning.
I feel arguments based on cause and effect will be more compelling (and easily supported by supporting evidence). That is, memory reminiscence techniques, improving the design of homes and wards, and introduction of innovations such as the ‘Dementia Dog’, which clearly have had a beneficial outcome for many, are options worth pursuing.
The ’cause’ of attracting monies for high quality research, acting as a foundation for pharmacological interventions, is a very worthy one. As someone who has published in this arena in international journals, I certainly don’t have any weird ideological objection to such work.
But we have to acknowledge, albeit reluctantly, that the world is changing, and whether some of us like it or not becoming more “consumer-driven”.
Citizens have become consumers with status proportional to purchasing power, and there’s now a fine line between data gathering of your personal lifestyle preferences through the ‘recreational’ social media and direct targetted marketing of things to improve your health or prevent illness.
The ultimate prize for industry is to determine government policy, but smaller organisations cannot compete against the large corporations, many of which contribute generously to political organisations too.
Where wellbeing campaigners lobbying may not succeed on economic power, their organising ability might succeed on the basis of facts and logic, in seeking out a constructive alternative to the existing policy, practice, or product.
It is often said that the basic rule of pressuring targets is that politicians react to publicity that reflects on their character, bureaucrats react to disrupting their provision of services and programmes, and corporations react to loss of their product’s reputation.
Wellbeing is an agenda for which politicians could have, and have had, much affinity.
If regulations are to be implemented, it’s often possible, hijack or “capture” the regulatory process. This can become easy if the regulatory process is biased towards a medical model of dementia, e.g. the General Medical Council and NICE, rather than social care institutions which are tacitly not given parity.
A committed opponent, who for the most part we’re not interested in reaching because debate with this individual tends to harden his or her position. Big Pharma, the General Medical Council, NICE and large dementia charities are clearly not targets to promote the wellbeing agenda.
The focus in parliament, through the All Party Parliamentary Group, and to some extent helped by powerful allies in the charity and corporate sector, has been relentlessly medical too.
Prof Felicia Huppert, to which my book is dedicated, ran a Royal Society meeting on wellbeing. There is no doubt that this was very succcessful, but we have never had a corollary in parliament.
A legislative hearing, however, gives the lawmakers the opportunity to hear all sides of an issue and to ask questions and challenge witnesses in a relatively brief span of time.
In 1991, the author Michael Frayn wrote a book, A Landing on the Sun, about a British prime minister who tasked his advisers with looking into happiness and what the government could do to promote it. The prize proved elusive, the adviser went mad and died.
Even in November 2010, speaking at the Google Zeitgeist Europe conference, David Cameron suggested, “Wellbeing can’t be measured by money or traded in markets.”
“It’s about the beauty of our surroundings, the quality of our culture and, above all, the strength of our relationships. Improving our society’s sense of wellbeing is, I believe, the central political challenge of our times.”
And this agenda has not sprung out of nowhere.
Aristotle talked about “eudaimonia” – happiness as human flourishing and purpose to life – rather than the modern hedonistic concept. John Maynard Keynes talked about the “art of life” in 1930, and in 1968 Bobby Kennedy told a student audience in Kansas: “We cannot measure national spirit by the Dow Jones average, nor national achievement by the gross domestic product.”
Tacrine was the prototypical cholinesterase inhibitor for the treatment of Alzheimer’s disease. William K Summers received a patent for this use (US Patent No. 4,816,456). Studies found that it may have a small beneficial effect on cognition and other clinical measures, though study data was limited. and the clinical relevance of these findings was unclear.
Tacrine was ultimately discontinued in the US. Unfortunately, it is associated with transaminase elevation in up to 50% of patients. The mechanism of tacrine-induced liver damage is not fully understood, but earlier studies have suggested that genetic factors may play a role.
And now leading Big Pharma companies are involved in an ‘arms race’ to get their drugs to market, and they have powerful allies in large dementia charities worldwide.
Both the AstraZeneca and Merck medicines work by blocking an enzyme called beta secretase that is involved in production of beta-amyloid, a protein that creates brain plaques considered a major cause of Alzheimer’s disease.
Such oral drugs are known as BACE inhibitors and are viewed as a promising new approach to fighting the memory-robbing condition.
BACE inhibitor drugs have taken centre stage after an injectable class of medicines targeting beta-amyloid plaque failed or fell short in trials conducted by Pfizer and Eli Lilly.
Not all experts accept that reducing beta-amyloid is the key to defeating Alzheimer’s, however, and the safety of the new BACE drugs has also been a subject of concern after Lilly pulled the plug on its product due to liver toxicity.
Unlike heart disease and cancer, no major advancements have been seen in Alzheimer’s drug research since the first treatment was approved in 1993 by U.S. regulators.
Of course, the push away from the relative failure of the drug industry should not be the only reason to pursue living well with dementia.
Being disciplined and organising specialist groups to represent only the needs of persons with dementia, both nationally and internationally, will be the only way to promote living well with dementia in the current environment.
They need to ‘capture’ research grant processes, such that we know what psychological interventions work too. They need to ‘capture’ service provision design.
A problem has been the cosiness between the large charities and the Pharma agenda. It is virtually impossible now to detect and act upon material conflicts of interest.
It’s not impossible that the sheer numbers of interested people can act as one large external radical for change. A new organisation, Dementia Alliance International, holds already substantial promise for advocacy for people living with dementia. There is also monumental size of influence of ‘the Carers’ Call to Action’ from the Dementia Action Alliance in this jurisdiction. And size is power.
But I don’t really feel that it should be a competition. The risk, nonetheless, of totally ignoring persons with dementia, their friends, family, or carers, is that the more you ignore them, they more they’ll come back.
Or as Labi Saffre said, “”The higher you build your barriers, the taller I become.”
The “dementia prevalence calculator”: for a person to access a timely diagnosis, or for private markets to access the person?
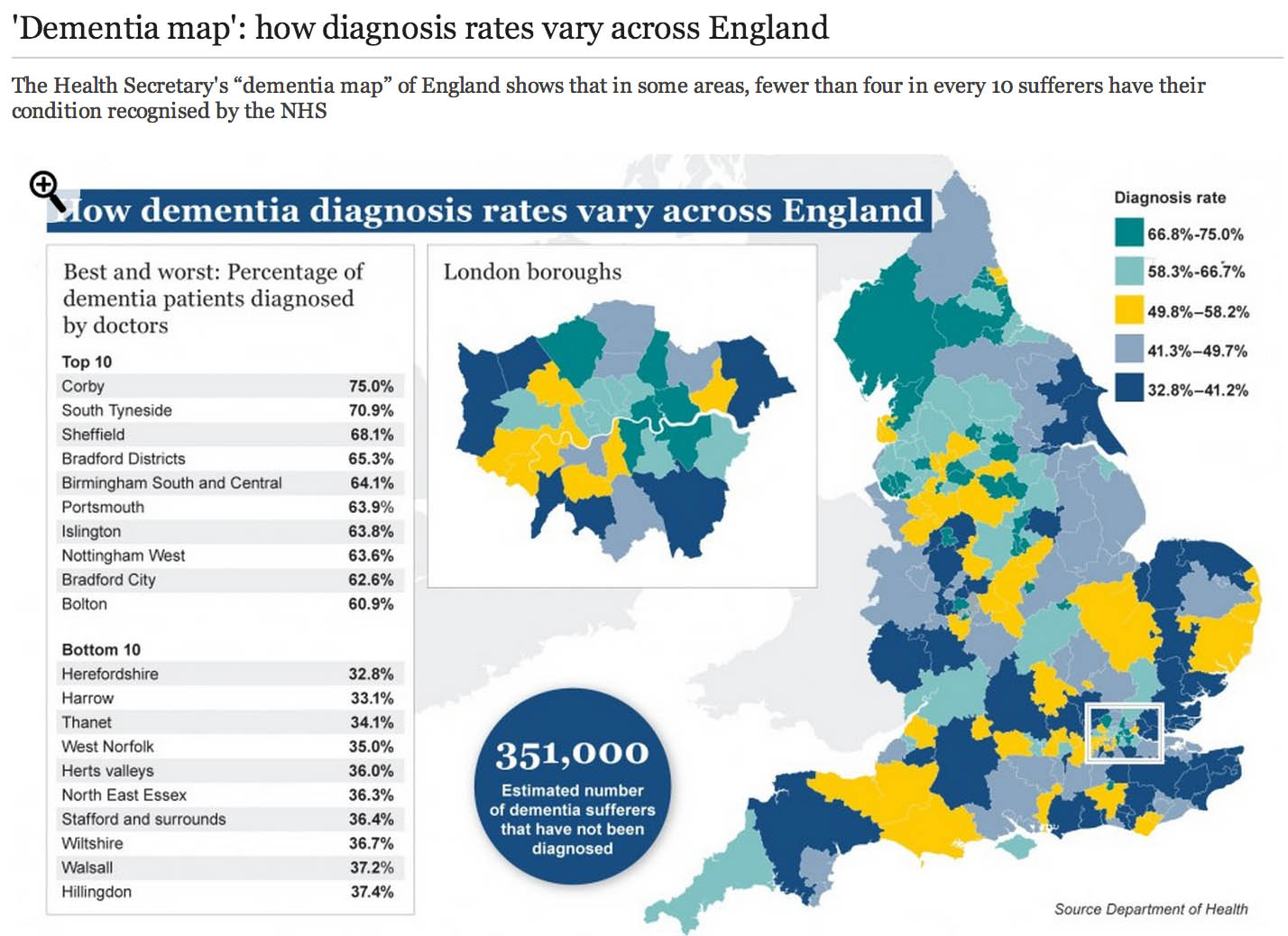
The market philosophy has gripped the NHS by the jugular through policy developments from successive governments. It is argued that all health care systems in the world have to design effective allocative mechanisms for the available “scarce health care resources”. The “dementia prevalence calculator” tool also enables health and care communities to: calculate local dementia diagnosis rates, forecast local dementia prevalence, view trajectories and set “ambitions” (aka targets) for improvement in diagnosis rates and compare diagnosis rates with other localities. Its main problem has been that it has been crowbarred in through various side windows, except nobody knows why public health experts didn’t call for this calculator to come in through a front door. One can now view and compare diagnosis rates on the “Ambition Map”, and link to the “Knowledge Portal” to access a wealth of resources to improve dementia diagnosis rates, and diagnosis pathways. All of this will have taken time, effort and money to set up, so the question of whether it’s worth it, given ‘scarce resources’, is clearly in the public interest. Here is one such example of the Department of Health’s attempts and their partners to disseminate information about “the dementia map”.
So what’s the point of these data? Burns concedes that estimating the number of people who have dementia is important for both local planning and national guidance. Burns freely admits too there have been problems in the past:
“Most current estimates of dementia prevalence (the number of people affected by the disorder) and incidence (the number of people developing it over a defined period, usually one year) are based on studies dating back to the 1980s.”
It’s become clear that a huge “democratic deficit” has engulfed the English dementia policy. The problem for Prof Alistair Burns, who is a genuinely a nice and well-meaning man, is that he can become indundated with various complaints from academics and practitioners. An example is the G8 dementia summit which was presented as a ‘once in a lifetime opportunity’ to talk about dementia. What did, however, happen was that it became a ‘once in a lifetime opportunity’ for various myths to be propagated by the media, using highly charged words such as ‘shocking’, ‘devestating’, ‘crippling’, ‘horrible’, ‘horrific’, portraying the notion that people now on receiving a diagnosis of dementia are just counting their hours until their death. It, likewise, cannot be overstated that the drugs for memory or attention simply do not have a huge effect in the vast majority of patients, and certainly after about fifteen years of published studies on these “cholinesterase inhibitors”, the evidence that they slow down the rate of loss in critical parts of the brain is not terrific. Academics in dementia are currently collaborating across geographical boundaries, so the idea of there now being suddenly a world collaboration is FALSE. A cure for a single dementia is FALSE as there are hundreds of different causes of dementia. Dementia charities of course can mobilise individuals with dementia to contribute in pan-global drug trials in what has been euphemistically been called ‘co-production’, discovering new drugs based on the basis of personal DNA genomic information. Looking at your genetic make-up might tell a practitioner or drug-company your risk of subsequently developing dementia, and so it goes on. The issue is not subjecting the designers of English dementia policy with time-consuming vexatious ‘attacks'; it is hopefully that we can all have an open, transparent discussion of some of the ‘unintended consequences’ of the English dementia policy currently in progress.
In March 2012 the Prime Minister, David Cameron, published his challenge on dementia which set out an ambitious programme of work to push further and faster in delivering major improvements in dementia care and research by 2015, building on the National Dementia Strategy (published on 3 February 2009). Central to the challenge is the requirement that from April 2013, there needs to be a quantified ambition for diagnosis rates across the country, underpinned by robust and affordable local plans (NHS Mandate). This is of course so remarkable in itself in the State having such a strangehold on policy which should in theory be devolved as locally as possible to experts and professionals. A painfully obvious point to those who have done a medical degree is that there will be variation in some rates of particular dementias across the country anyway. For example, in some populations with a predominantly Asian immigrant population with certain risk factors, they might be at high risk of vascular dementias. As it happens, near Warsaw in Poland is thought to have a high prevalence of dementia due to copper overload due to a genetic cluster of an inherited copper metabolism problem called Wilson’s disease. But presumably certain dementia charities and certain politicians want you ‘to get angry’ at those GPs who are underdiagnosing dementia, because they are somehow colluding in keeping this information away from you. This is by the way against their professional code, but you cannot expect people without a medical background who are quite senior in charities or politics to know that necessarily.
I have found that having lack of ability to have a balanced debate (due to enormous information asymmetries) has been quite dispiriting, and clearly hampered by the virtual lack of published research papers in the medical professional literature. Hopefully, the University of Stirling will be able to diminish this ‘research gap’, now that they have been awarded a major grant to investigate this issue properly with no vested interests. This is the only paper on Medline from 1996 if you search for the term “dementia prevalence calculator”. And there is no doubt that the claims of some of the drugs used to treat early dementia in the NHS have been overinflated. Luckily, largely thanks to the work of Glenis Willmott MEP who has been leading negotiations as the European Parliament’s rapporteur on the clinical trials regulation, pharmaceutical companies and academic researchers will be obliged to upload the results of all their European clinical trials to a publicly accessible database, if a deal reached this week is approved, according to a recent report. Indeed, Pharma have got it right about “openness”, but not in the sense of using regulation to allay fears about patient privacy and confidentiality – Big Pharma need to share with the general public their results, and their particular motives and intentions for dementia policy especially if the descriptions are otherwise not easily forthcoming.
I openly admit to being extremely disappointed at one particular plank of English dementia policy: the “dementia prevalence calculator”. It’s incredibly easy to get hold of the marketing shills for CCGs about how they can overcome “the diagnosis gap” for the reported lack of diagnosis of dementia; but there again, the discussion of how there are hundreds of different types of dementia in different age groups is not forthcoming, together with a less than candid explanation of how risk factors for dementia might be tackled. For something so fundamental to English dementia policy, it was deeply distressing to see Prof Carol Brayne’s question on where the Prime Minister saw his “Challenge” progressing on dementia to be passed ‘down the line’ like a rugby ball going backwards with effortless ease first to Mr Jeremy Hunt and then with Dr Margaret Chan. To get a decent grasp on why there has been such a drive to improve dementia rates, you have to go across the Atlantic and research terms such as “needs based resource allocations” in health maintenance organizations (sic). These papers are written entirely from the business model perspective, so do not have any intention of wishing to address remotely the professional concerns of senior clinicians in dementia.
Like all 500 pages of the Health and Social Care Act (2012), there was no open discussion of the need to “turbo boost” the outsourcing of NHS contracts to the private sector. Likewise, meaningful discussion of the perils of ‘case finding’ and ‘screening’ in dementia have largely been throttled at source (though Dr Martin Brunet has been raising awareness of the perils of incentivising GPs to up their rates of dementia diagnosis through ‘case finding’ in primary care, of course drawing attention to the hugely stigmatising “false diagnoses of dementia”). Nonetheless, through the combined efforts of the European ALCOVE project (including Prof Burns and Dr Karim Saad), it’s been successfully argued that,
“Dementia happens to people, living in their families and their communities. It does not happen just to their brains. When people have worrying symptoms they want health care professionals who can spot the signs, take their concerns seriously, diagnose the problem accurately, so they can get the most up to date treatment and advice.”
This is a helpful slide from Prof Dawn Brooker’s presentation for the UK Dementia Congress Conference 2013 entitled, “Benchmarking against ALCOVE recommendations for timely diagnosis in dementia”:
This discussion embarrassingly even led to Prof Burns trying to find Dr Brunet at his practice for a frank chat about the policy, but Martin unfortunately was away that day.
Of course, if you’re going to introduce a policy to ‘up the dementia rate’, it possibly will run into problems given that the actual prevalence of dementia has appeared to be falling. The first UK Cognitive Function and Ageing Study (CFAS), known as the Medical Research Council (MRC) CFAS, began in 1989. One of a suite of European prevalence and incidence studies (forming the EURODEM collaboration), it was designed to test for geographical differences within the UK, across populations with widely varying characteristics, including vascular health. The study published by Matthews and colleagues (2013) in the Lancet confirmed that later-born populations have a lower risk of prevalent dementia than those born earlier in the past century. The general prevalence of dementia (overall numbers of people) in the population might be subject to change. Factors that might increase prevalence include: rising prevalence of risk factors, such as physical inactivity, obesity, and diabetes; increasing numbers of individuals living beyond 80 years with a shift in distribution of age at death; persistent inequalities in health across the lifecourse; and increased survival after stroke and with heart disease. By contrast, factors that might decrease prevalence include successful primary prevention of heart disease, accounting for half the substantial decrease in vascular mortality, and increased early life education, which is associated with reduced risk of dementia. Where possibly primary care will have the greatest impact will be in tackling the risk factors they do anyway for cardiovascular disease, i.e. better diabetic control, tackling cholesterol, smoking, ‘poor diet’, or high blood pressure. This in itself is not a valid reason to avoid improving diagnosis rates of dementia (especially these are treatable risk factors for vascular dementias.)
Health maintenance organizations (HMOs) have been argued by their supporters as a “cost-effective’ way to provide health care. In the United States, in allocating resources in the HMO, the rationing of preventive services appears to be one of the principal questions where the potential benefits (i. e., efficacy) of a service are considered in relation to costs of healthcare. The direct counterpart of the HMO in English health policy, following the enactment of the Health and Social Care Act (2012), is the “clinical commissioning group”, which act as state insurance schemes for pooling risk in population samples.
Just because there’s no effective treatment, there’s still a business case to be made for ‘opening up new markets’ of persons with dementia. For example in the NHS Outcomes Framework 2013/4 domain CB_A9 covers an estimated diagnosis rate for people with dementia, with an aim of “improving the ability of people living with dementia to cope with symptoms, and access treatment, care and support.“. The rationale is therefore stated as:
“A diagnosis enables people living with dementia, and their carers/families to access treatment, care and support, and to plan in advance in order to cope with the impact of the disease. A diagnosis enables primary and secondary health and care services to anticipate needs, and with people living with dementia, plan and deliver personalised care plans and integrated services, thereby improving outcomes.”
According to articulation of neo-liberal ideology, the main justification of the reforms is to make resource allocation “more efficient, more innovative and more responsive to consumers’ preferences” than centrally integrated health systems (Ven 1996, p. 655). The effect of this change in philosophy is the introduction of activity-based resource allocation and funding as a system of paying hospitals and other health care providers on the basis of the work they perform rather than previously applied defined budgets based en bloc global contractual considerations. This new system relies on cost-and-volume and cost-per-case contractual relationships, in which payments are closely linked with the services offered, and clearly the information from “dementia prevalence calculators” is useful here. Conceptually, “dementia prevalence calculators” have been presented on equity grounds, i.e. tackling the inequity of a postcode-lottery diagnosis of dementia. However, this makes a fundamental assumption that there cannot be geographical variations in the prevalence of dementia. I repeat the point – any practising physician would know that this assumption is entirely erroneous, as vascular dementia prevalence rates for cardiopaths for diabetic hypertensive individuals in Tower Hamlets in a ghee-laden diet might be hypothesised to be quite high? The actual drive for the ‘dementia prevalence calculator’ is to open up new active markets, in a form of ‘payment of results’. According to Gay and Kronedfeld (1990), the gradual evolvement of an activity based resource allocation can be traced to the United States, where from 1983 most reimbursement for health care providers had been based upon the Diagnosis-Related Group (DRG) where patients within different categories were classified as clinically similar and were expected to use the same level of hospital resources.
Having a ‘care plan’ for dementia is potentially advantageous in that it can provide harmonisation with private insurance systems. The ‘Kaiser Permanente Care Management’ program contains guidelines and recommendations on how dementia care should be provided to Kaiser enrollees. The new program is an informational resource only and is not a substitute for clinical judgment based on the individual needs of patients. The program includes nine “key principles” on diagnosing and caring for patients with dementia and support for their caregivers. These principles include early identification and diagnosis, connecting caregivers to vital community resources, developing a care plan, and monitoring and adjusting medication use. With the introduction of “whole person care” (or similar models of integrated care in the next government), it is likely health and social care will be taken down a “final common pathway” of the ‘personal budget’ or ‘individualised’ budget (see this article for a recent discussion of some of the key themes from the English healthcare thinktanks). The commercialisation of care, under the guise of control and budgets, is, in fact, of course a complete anethema to genuine principles of professional person-centred care. And merging a universal system which has lots of highly personal data (NHS) with one that is heavily conditional (benefits) has all kinds of risks. In the long run it could make it still easier to restrict access to healthcare on the basis of economic status or behaviour.
While GPs and the public are clearly none-the-wiser about the goal of upping the diagnosis rates, already work is being done on the barriers and solutions for implementation of personal health budgets in dementia. Claire Goodchild’s report for the Mental Health Foundation from October 2011 still makes for interesting reading. Goodchild argues that, “individualised, tailored support and care that a personal budget can facilitate can have enormous benefits to a person with dementia“. The irony is of course that Big Pharma may not actually end up the big beneficiaries of this drive, unless they can make their medications relevant to individuals with dementia in this brave new world. While the G8 conference was an effective pitch for personalised medicines for Big Pharma, relatively little attention was given to psychological therapies or carers, aside from ‘dementia friendly communities’ which bring competitive advantage to the included corporates (and benefits for persons with dementia too). Personal budgets are all about choice and control; it is unlikely that a person with dementia will be unaware of the personal spending decisions that he or she can make to improve wellbeing (deferred to a carer where that person does not have capacity); but other valid interventions do include the assistive technologies and innovations which curiously did also make a mention in the G8 dementia.
Therefore, at first blush, it might look a bit random having a ‘dementia prevalence calculator’ and then all the shennanigans of the G8 dementia summit, but whilst the English government cannot as such make dementia ‘wealth creating’, it can do its best to open up new markets. It hasn’t been an accident that the question, “Have you had problems with your memory?”, has been suggested for those ‘health MOTs‘ which private healthcare would love to get off the ground. And the big beauty of this plan when NHS budgets are looking to do ‘more with less’ or implement ‘efficiency savings’ (or cuts to frontline care, more accurately) is that the NHS budget itself won’t ‘take the hit‘. It is hoped that with the implementation of whole person care budgets somebody will be able to ‘top up’ payments for care (e.g. “co-payments”), and the patient (or customer) will now pay for care providers in the private sector too. Do the treatments actually have to be proven to work? Absolutely not, if the experience in personal health budgets is anything to go by, but that’s not the point. As David Cameron might say, “Oh come on.. please do keep up!”
Further reading
Gay E.G. and Kronedfeld J.J. (1990). “Regulation, retrenchment – the DRG experience: problems from changing reimbursement practice”. Social Science and Medicine. 31 (10), pp. 1103-1118.
Ven, W.P.M.M., van de. (1996). “Market-oriented health care reforms: trends and future options”. Social Science and Medicine. 43 (5), pp. 655-666.
Why I wrote ‘Living well with dementia’
“Living well with dementia: the importance of the person and the environment for wellbeing” is my book to be published in the UK on January 14th 2014. I have written it on my own, but I have drawn on the published work a number of Professors working in the field of dementia have sent me. I hope the advantage of having an overview of their research programmes has been to put together with one voice where exactly this approach might be heading using the most contemporary published papers. I am enormously grateful that these busy Professors were able to supply me with their recent papers.
I was asked by my publishers to provide pointers about what a “marketing strategy” for this book might be. I can honestly say that, having given considerable time to thinking about this issue, I have no intention of pursuing a conventional promotion of my book. I don’t intend to do nothing, but I can confidently say that this book will be widely read. I have no intention of flogging it to commissioners, who will have their own understanding of what health or wellbeing is in the modern construct of NHS England’s policy.
I do, however, have every intention of addressing what I think is a major shortfall in the medical profession in their approach to dementia. Their emphasis has been, where done well, the exact diagnosis of dementia through an accurate history and examination of a patient, with appropriate investigations to boot (such as a CT scan, MRI, lumbar puncture, EEG or cognitive psychology). The combined efforts of Big Pharma and medics have produced limited medications for the symptomatic treatment of memory and attention in some dementias, but it would simply be a lie to say that they have a big effect in the majority of patients, or that they reverse the underlying the disease process consistently and robustly.
But that’s the medical model, and certainly the ambition for a ‘cure’ is a laudable one. I found the recent G8 dementia summit inspiring, but a bit of a distraction from providing properly funded solutions for people currently living with one of the hundreds of dementias. Many of us in the academic community have had healthy collaborations for some time; see for example one of the Forewords to my book by Prof Facundo Manes, Chair of Research of the World Federation of Neurology (Dementia and aphasia). To say it was a ‘front’ for Big Pharma would be unnecessarily aggressive, but it has been openly admitted in the media that a purpose of the summit was to assist ‘an ailing industry’.
I think to emphasise what might be done for future patients of dementia would be to fail to maximise the living of people with dementia NOW. By this, I mean a correct and timely diagnosis of an individual, the suggestion of appropriate assistive technologies and innovations, appropriate leisure activities, and the proper design of a positive environment (whether that be a ward, a house or external environment).
My book is strongly footed in current research, but I openly admit that research does not have all the answers. I should like there to be a strong emphasis also in non-pharmacological approaches, such as the benefits of life story and reminiscence, art or dancing. Lack of current research certainly does not make these approaches automatically invalid, particularly when you consider the real reports of people with dementia who have reported benefit.
The main reason is that I do not wish to organise attendance in a series of workshops or conferences about dementia is that I do not wish to be perceived as selling a book. I am more than happy to talk about the work if anyone should so desire. A number of my friends are very well-known newspaper journalists, and I deliberately have not approached any of them as I consider this might be taking advantage of my friendship. I haven’t approached dementia campaigners, or other dementia charities, as I don’t wish to get involved in some sort of competition for other people’s attention. I haven’t sought the ‘celebrity backing’ of some senior practitioners in dementia, although Prof John Hodges (a world expert particularly in the frontotemporal dementias) kindly wrote one of my Forewords. If people wish to discuss the issues in a collaborative manner to take English policy further, I’d be delighted.
At the centre of this book is what an individual with dementia CAN do rather what they cannot do. If you’re looking for a cogent report into the medical deficits of people with dementia, you’ll be sorely disappointed. I spent about 10 years of medical training at undergraduate and postgraduate levels, without having heard of personhood or Tom Kitwood’s work once. I think this a travesty. As a person who is physically disabled himself, the need to understand the whole person is of massive personal significance to me. I think that, beyond doubt, future training of anyone in the caring professions, including medicine, will have to start with understanding the whole person, rather than seeing a patient with a series of problems to be cured or symptomatically addressed.
No academic, practitioner, or charity can have a monopoly of ideas, which is why I hope my book will be sincerely treated with an open mind. People have different motivations for why they get involved in dementia; for example, a corporate wishing to be part of a ‘dementia friendly community’ through a charity might have a different guiding principle to an academic at a University wishing to research from scratch some of the fundamental principles of a dementia friendly community. Despite all the “big players”, nobody can match up to THAT individual who happens to be living with dementia; that person is entitled to the utmost dignity and respect, as brilliantly expressed by Sally Marciano in her powerful Foreword.
I am hoping very much to meet up with some personal friends that I’ve met in the #dementiachallengers community on January 18th 2014, and this is as close as I’ll get to the book launch. But I hope you will find the book readable. I don’t feel that there’s any other book currently available which bridges these two totemic topics (dementia and wellbeing); but I hope there are other good reasons for reading it!
Related articles
- Need for Dementia Caregivers Grows as Boomers Age (abcnews.go.com)
- A cure for dementia could be found within twelve years, David Cameron has said (telegraph.co.uk)
- Simple Steps Could Keep People With Dementia at Home Longer: Study (nackpets.wordpress.com)
"Cui bono" again – who exactly stands to gain from the NHS IT initiative?
Even Google gave up on their central database for health information called “Google Health“. Whilst few things are as certain as death and taxes, it is fairly certain that there is big money in big data. Lord Shutt of Greetland, Chair of the Joseph Rowntree Reform Trust Ltd. warned, in a foreword on a recent report on “the database state“, that the problem is huge, and as a society we must face up to formidable challenges. There has always been a tough balance in the law between balancing individual rights of privacy and freedom, with the State’s rights of national policy of health and security, for example. Whatever ideological position the Liberal Democrats eventually settle on, it is striking that a Conservative Prime Minister should actually advocate nationalising something.
It is unsurprising that Big Pharma would have welcomed the move. Andrew Witty, the chief executive of GlaxoSmithKline, stated to the Sunday Telegraph he welcomed the data-sharing initiative: “Any action the government takes to improve the environment in this country for life science across these activities is welcome.” The Autumn Statement (2011) had indeed signposted this. It might seem paradoxical that the Department of Health at this time wishes to embark on an initiative to make the NHS “paperless”, at a time when a reorganisation, estimated at £3bn, is currently underway. Patient data, essential for individual patient security, confidentiality and consent, are “rich pickings” for the private healthcare industry, which have not collectively paid to collect this information nor invest in the IT infrastructure of the NHS, but the ethical concerns are enormous. Personalised medicine, dependent on real-time patient information, is “the next big thing” emergency in the pharmaceutical industry, currently keeping stocks of companies very healthy. However, the professional code for Doctors, from the General Medical Council (“GMC”) is very clear on the regulation of patient confidentiality and privacy: this is contained within “Confidentiality” (2009), and clearly guides doctors on the conflicting balance between confidentiality and disclosure.

There are interesting reasons why the operational roll-out of the National Patient Record failed in 2006-7. It is now reported that all prescriptions, diagnoses, operations and test results will be uploaded on to central computers by the end of next year, and, by 2018, all NHS organisations will be expected to be able to share this information with other hospitals, GPs, ambulances and health trusts. Jeremy Hunt hopes local councils will sign up to similar systems, along with private care homes. As with the overall direction of travel of the NHS towards an insurance system where private companies pay “a greater part”, this blurring of the need for patient consent has been insidious.
Section 251 of the NHS Act 2006 (originally enacted under Section 60 of the Health and Social Care Act 2001), allows the common law duty of confidentiality to be set aside in specific circumstances where anonymised information is not sufficient and where patient consent is not practicable. For example a research study may require access to patient identifiable data to allow linkages between different datasets where the cohort is too large for consent. This would require time limited access to identifiable information where gaining consent from a large retrospective cohort would not be feasible and would require more identifiable data than would be necessary for linkage purposes. However, section 10 of the Data Protection Act (1988) currently allows a right for an individual to prevent damage or distress by data processing. This is indeed conveniently “triggered” by section 259(10) of the Health and Social Care Act (2010), i.e. “[the provision] is subject to any express restriction on disclosure imposed by or under another Act (other than any restriction which allows disclosure if authorised by or under an Act”:
The Secondary Uses Service (SUS) Programme supports the NHS and its partners by providing a single source of comprehensive data for planning, commissioning, management, research, audit, public health and “payment-by-results”, a reimbursement mechanism for acute care payments. It is critical to know whether patients maintain a right to opt out of the SUS database. It should not be the case that NHS patients are denied hospital care if they do not agree to my records being sent to SUS. Steve Nowottny in his “Editor’s Blog” for Pulse, a newspaper circulated to GPs, on 8 January 2013 outlined some important very recent developments:
“That year, Pulse ran a ‘Common Sense on IT’ campaign which highlighted a series of concerns over the consent and confidentiality safeguards in the new system.
“GPs wanted patients to have to give explicit rather than merely implied consent before records were created. Plans to use data within the records for research purposes without explicit consent had Catholic and Muslim leaders up in arms, because they feared the research could be purposes contrary to their faiths, such as abortion or stem cell research.
We revealed that celebrities, politicians and other patients whose information is regarded as sensitive would be exempted from the automatic creation of a Summary Care Record, raising questions about the system’s security. And we reported that patients who did not initially choose to opt out of the Summary Care Record would be unable to have their records subsequently deleted.
At the time, it felt as though the stories, while interesting and concerning, were somewhat theoretical. The Summary Care Record’s deployment to date had been patchy and it was far from certain it would continue. In the meantime, fewer than 1% of patients had bothered to opt out. (Now, with nearly 22 million records created and more than 41 million patients contacted, the figure stands at 1.34%).
But the news today that 4,201 patients had Summary Care Records created without them giving even implied consent – and that they will not be able to have them deleted – reignites the whole debate. Suddenly ‘what if’ scenarios have become reality.”
Tim Kelsey is the NCB’s National Director for Patients and Information – his stated aims are to put transparency and public participation at the centre of a transformation of customer service in the NHS. In a recent lecture, he quoted George Soros who said “our social institutions are imperfect, they should be open to improvement [and that] requires transparency and data“. On-line banking and e-ticketing demonstrate the power of open access to personal data in a safe, secure way – for some reason, heath data is deemed more personal that finance and travel arrangements. Data.gov.uk is an example of his vision for the future – the UK has so much medical data, not only about patients but also genomics and other bioinformatics disciplines. The law currently gives the NCB power to mandate more data flows – Kelsey apparently targets April 2014 to get outcomes-based data flows from primary and secondary care – once achieved, next step is to embrace social and specialist care. So, once the data is “freely available”, it can be made available for public participation – he is investing in a course called ‘Code for Health’, a 3 day course to learn how to develop apps. Data are essential from April 2013, there will be push for on-line interaction with GPs, to realise nationally the benefits seen in pilot areas.
So why should commissioners need access to “personal identifiable data”? It is considered that these may be “good reasons”:
- integrated care and monitoring services including outcomes and experience requires linkages across sources
- commissioning the right services for the right people requires the validation that patients belong to CCGs and have received the correct treatments
- aspects of service planning and monitoring on geographic data basis require postcodes for certain type of analysis
- understanding population and monitoring inequalities
- target support for patients and population groups at highest risk requires data from several sources linked together
- specialist commissioning is commissioned outside local areas and can require wider discussions about individual patients and their associated costs
- ensuring appropriate clinical service delivery and process requires access to records
To enable commissioning, ‘personal identifiable data’ including NHS no, DOB, Postcode data needs to flow to “data management integration centres” (“DMICs”). The DMICs need to have similar powers and controls to the Health and Social Care Act information centres to process data In order for processing of PID at DMICs to be undertaken legally, a change in legislation will be required; it is considered that legislative changes can not be achieved by April 2013, and that the new Caldicott is report expected around Jan/Feb 2013. Meanwhile, DMICs need to be operational in April 2013.
David Cameron has stated explicitly his intention for social care to head towards a private insurance system. As stated in the transcript of the interview with Andrew Marr,
“Well the point that was being made earlier on the sofa by Nick Watt, this is a massive problem – that you know more and more people suffering from dementia and other conditions where they go into long-term care and there are catastrophic costs that lead them to have to sell their homes to pay for that care – it’s right to try and put in place a cap which will then open up an enormous insurance market, so people can insure against that sort of catastrophic loss.”
A longrunning conundrum about where there is such intense interest in ‘raising awareness of dementia’. The idea of having GPs and physicians ‘diagnose’ dementia on the basis of a screening test, without it being called ‘screening’ in name, has not been backed up with the appropriate resource allocation for dementia care elsewhere in the system, including adequate training for junior doctors and nurses crucially involved in actual dementia care. Is this and integration of care an entirely virtuous sociological problem? Integration of care at first sight seems to involve primarily avoidance of reduplication of operations, and better ‘coordinated’ care between health and social care and funding. This is not an unworthy ambition at all. It is well known that the endpoint of the Pirie and Butler “Health of Nations” blueprint for NHS privatisation has a greater rôle for the private insurance market as the endpoint, so it makes complete sense to have a fully integrated IT system which private insurers and the Big Pharma can tap into. Lawyers will, of course, be cognisant about the added beauty of integration of clinical and financial information. One of the biggest banes of insurance markets is information asymmetry, making calculation of risk and potential payouts difficult. Insurers will argue that calculation of risk is only possible with precise information, and as I described earlier, clinical commissioning groups are merely “statutory insurance schemes”. It is a long-held belief that private insurers refuse to pay off given the slightest lack of compliance in terms and conditions, but private insurers provide that this mechanism needs to exist to protect them making unnecessary payouts. Failure to disclose medical conditions is an excellent way for private insurers to get out of “paying up”, otherwise known as rescission. Of course, this could be taking the “conspiracy theory” far too far, and these concerns about the use of “big data” otherwise than for a “public good” may be totally unfounded.
You can, nonetheless, mount an argument why the current Government wish to progress with this particular approach to private medical data. The private insurance market and Big Pharma stand to benefit massively, and their lobbying is much more sophisticated than lobbying from GPs, physicians or members of the public. The drive towards all nurses having #ipad3s and all TTOs from Foundation Doctors being sent by broadband to nursing homes may seem utterly virtuous, but there are more significant drivers to this agenda beyond reasonable doubt. On the other hand, it’s simply that healthcare policy is in fact improving for the benefit of patients.
Extremely grateful to the work of Prof Ross Anderson, Chair of Computer Security at Cambridge University, and Phil Booth @EinsteinsAttic on Twitter with whom I have had many rewarding and insightful Twitter conversations with @helliewm.