Home » Posts tagged 'Alzheimer’s disease'
Tag Archives: Alzheimer’s disease
Meet Norman and Terry: two people living with a dementia in different ways
“Dementia is not just about sitting in a bathroom all day, staring at the walls.”
So speaks Norman McNamara in his recent BBC Devon interview this week.
This may seem like a silly thing to say, but the perception of some of “people living with dementia” can be engulfed with huge assumptions and immense negativity.
The concept of ‘living well with dementia’ has therefore threatened some people’s framing of a person who happens to have one of the hundred or so diagnoses with dementia.
It’s possible memory might not be massively involved for someone who has been diagnosed with a dementia.
Or as “Dementia Friends” put it, “Dementia is not just about memory loss.”
Norman McNamara and Sir Terry Pratchett are people who are testament to this.
“If you made a mistake, would you laugh it off to yourself and say ‘Ha, ha, maybe it’s because I have dementia.””
If somebody else made a mistake, would you laugh at that person and say ‘Ha, ha, maybe it’s because you have dementia.” Definitely not.
There are about a hundred different underlying causes of dementia.
“Dementia” is as helpful a word as “cancer”, embracing a number of different conditions tending to affect different people of different ages, with some similarities in each condition which part of the brain tend to be affected.
These parts of the brain, tending to be affected, means it can be predicted what a person with a medical type of dementia might experience at some stage.
This can be helpful in that the emergence of such symptoms don’t come as much of a shock to the people living with them.
Elaine, his wife, noticed Norman was doing “weird and wonderful things”.
Norman says “my spatial awareness was awful”, and “I was stumbling and falling”.
Norman, furthermore, was putting “red hot tea in the fridge”, and “shower gel, instead of toothpaste, in [my] mouth”.
Dementia with Lewy bodies (DLB) is a type of dementia that shares symptoms with both Alzheimer’s disease and Parkinson’s disease. It may account for around 10 per cent of all cases of dementia. It is not a rare condition.
It is thought to affect an estimated 1.3 million individuals and their families in the United States.
Problems in recognising 3-D objects, “agnosia”, can happen.
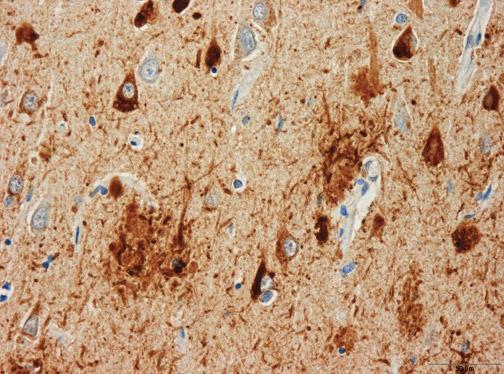
Lewy bodies, named after the doctor who first identified them, are tiny deposits of protein in nerve cells.
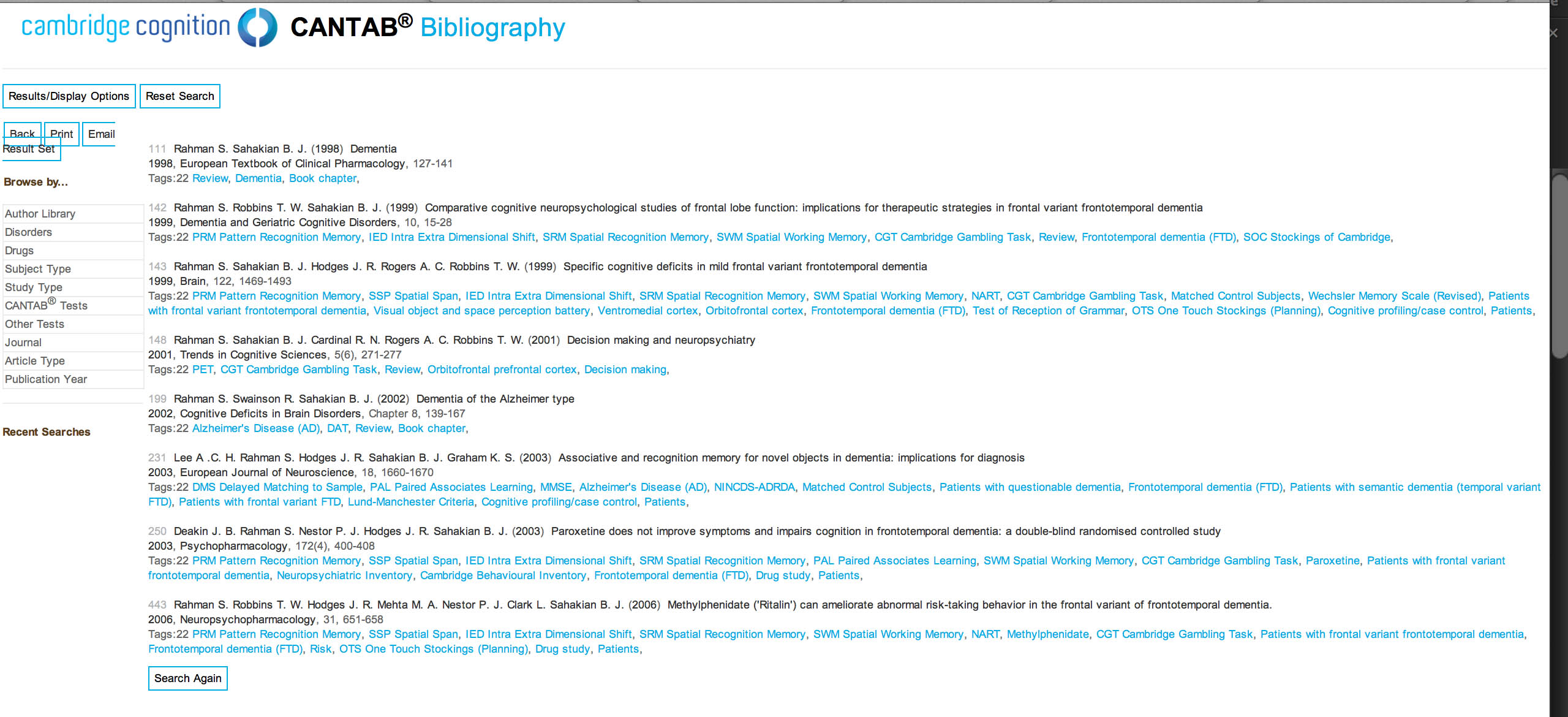
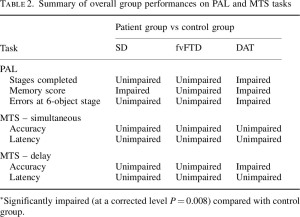
See for example this report in this literature.
“Night terrors” have long been recognised in diffuse lewy Body disease.
“The hallucinations are terrific”
The core features tend to be fluctuating levels of ability to think successfully, with pronounced variations in attention and alertness and recurrent complex visual hallucinations, typically well formed and detailed.
See for example this account.
For Norman, it was ‘prevalent in his family’.
Other than age, there are few risk factors (medical, lifestyle or environmental) which are known to increase a person’s chances of developing DLB.
Most people who develop DLB have no clear family history of the disease. A few families do seem to have genetic mutations which are linked to inherited Lewy body disease, but these mutations are very rare.
The patterns of blood flow can help to confirm an underlying diagnosis (see this helpful review).
Also, in this particular ‘type of dementia’, it can be helpful for medical physicians to avoid certain medications (which people with this condition can do very badly with). So therefore while personhood is important here an understanding of medicine is also helpful in avoiding doing harm to a person living with dementia.
However, Norman has been tirelessly campaigning: he, for example, describes how hundreds of businesses in the Torbay-area of Devon have signed up for ‘dementia awareness.”
And, as Norman says, “When you’ve met one person with dementia, you’ve met one person with dementia.”
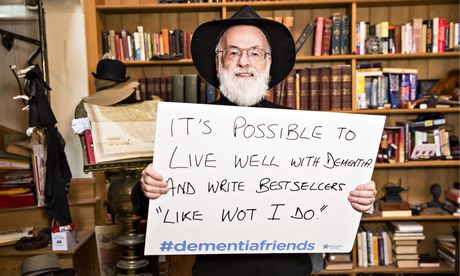
Sir Terry Pratchett is another person living with dementia.
Sir Terry Pratchett described on Tuesday 13th May 2014 the following phenomenon bhe had noticed:
“That nagging voice in their head willing them to understand the difference between a 5p piece and £1 and yet their brain refusing to help them. Or they might lose patience with friends or family, struggling to follow conversations.”
“Astereognosis” is a feature of ‘posterior cortical atrophy’ (“PCA”).
A good review on the condition of PCA is here.
Sir Terry Pratchett has written a personal reflection on society’s response to dementia and his own experience of Alzheimer’s to launch a new blog for Alzheimer’s Research UK: http://www.dementiablog.org
Sir Terry became a patron of Alzheimer’s Research UK in 2008, shortly after announcing his diagnosis with posterior cortical atrophy, a rare variant of Alzheimer’s disease affecting vision.
He went on to make a personal donation of $1 million to the charity, and has subsequently campaigned for greater research funding, including delivering a major petition to No.10 and countless media appearances.
In his inaugural post for the blog, Sir Terry Pratchett writes: “There isn’t one kind of dementia. There aren’t a dozen kinds. There are hundreds of thousands. Each person who lives with one of these diseases will be affected in uniquely destructive ways. I, for one, am the only person suffering from Terry Pratchett’s posterior cortical atrophy which, for some unknown reason, still leaves me able to write – with the help of my computer and friend – bestselling novels.”
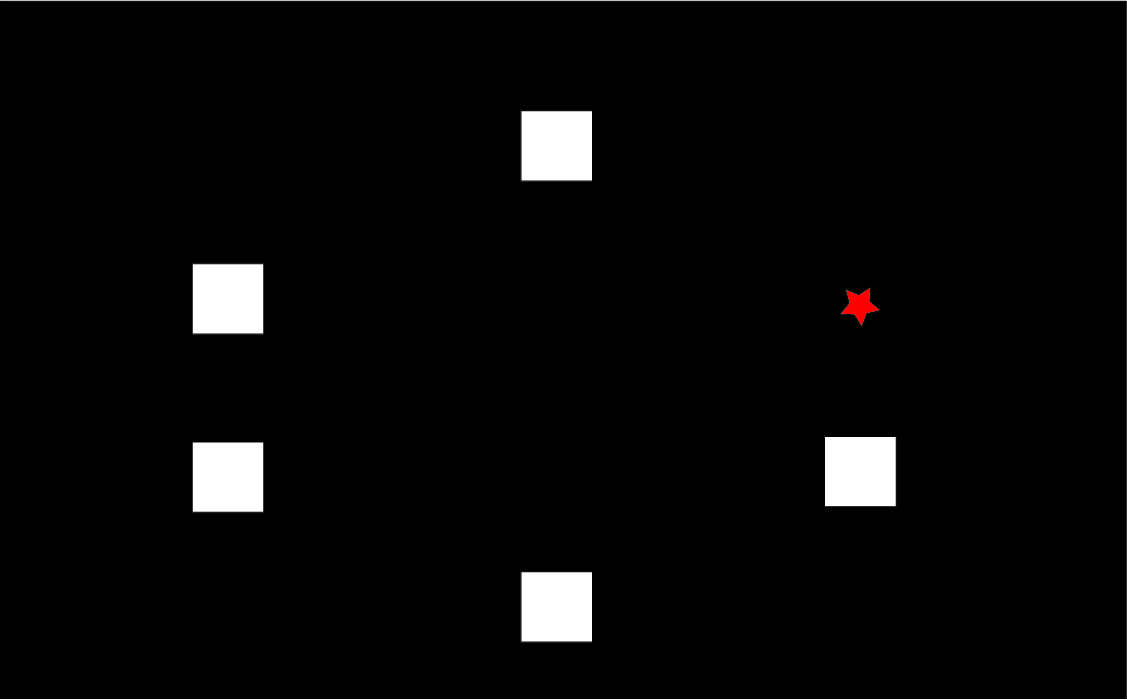
Posterior cortical atrophy (PCA) refers to gradual and progressive degeneration of the outer layer of the brain (the cortex) in the part of the brain located in the back of the head (posterior).
The symptoms of PCA can vary from one person to the next and can change as the condition progresses. The most common symptoms are consistent with damage to the posterior cortex of the brain, an area responsible for processing visual information.
Consistent with this neurological damage are slowly developing difficulties with visual tasks such as reading a line of text, judging distances, and distinguishing between moving objects and stationary objects.
Other issues might be an inability to perceive more than one object at a time, disorientation, and difficulty maneuvering, identifying, and using tools or common objects.
Some persons experience difficulty performing mathematical calculations or spelling, and many people with PCA experience anxiety, possibly because they know something is wrong. In the early stages of PCA, most people do not have markedly reduced memory, but memory can be affected in later stages.
Astereognosis (or tactile agnosia if only one hand is affected) is the inability to identify an object by active touch of the hands without other sensory input.
An individual with astereognosis is unable to identify objects by handling them, despite intact sensation. With the absence of vision (i.e. eyes closed), an individual with astereognosis is unable to identify what is placed in their hand. As opposed to agnosia, when the object is observed visually, one should be able to successfully identify the object.
Living well with dementia means different things to different people.
Pratchett further writes:
“For me, living with posterior cortical atrophy began when I noticed the precision of my touch-typing getting progressively worse and my spelling starting to slip. For an author, what could be worse? And so I sought help, and will always be the loud and proud type to speak my mind and admit I’m having trouble. But there are many people with dementia too worried about failing with simple tasks in public to even step out of the house. I believe this is because simple displays of kindness often elude the best of us in these manic modern days of ours.”
As we better understand what dementia is, our response as a society can be more sophisticated. I’ve found one of the most potent factors for encouraging stigma and discrimination is in fact total ignorance.
Both Norman and Terry demonstrate wonderfully: it’s not what a person cannot do, it’s what they CAN DO, that counts.
This is ‘degree level’ “Dementia Friends” stuff, but I hope you found it interesting.
The difficulties of the delayed diagnosis for dementia in primary care
If a surgery appointment is booked for someone over 65, a ‘participating GP’, might be incentivised to ask about memory problems in a patient at risk of dementia due to heart disease, stroke or diabetes.
There is a concern that some people are missing out on a timely diagnosis of dementia.
It is claimed that some people go undiagnosed for around ten years even, and a large proportion of persons with dementia have never received a formal diagnosis of a dementia.
A further worry is that certain people with much lesser degrees of memory impairment will be plugged into the dementia care pathways, according to Dr John Cosgrove.
At worst, this policy, where individuals are said to be ‘ambushed’ in the video above, may put people from going to see their GPs about other problems.
The risk factors, heart disease, stroke or diabetes, are not known to be risk factors for many types of dementia, although they are certainly treatable risk factors for the ‘vascular dementias’.
There is a concern about what then happens to those people who then receive a possible diagnosis of dementia.
It is known that many of these individuals do not actually want further investigations. In fact, for some, they will not even turn out to have a dementia at all.
A probable diagnosis of dementia is certainly ‘life changing’, and it can mean that a person has access to support services.
But a full work-up of a dementia, ideally, needs more than a quick chat over memory problems.
In one type of dementia, frontal dementia, common in the younger age group (that is, below the age of sixty), memory problems are not even prominent. This type of dementia is characterised by an insidious change in behaviour and personality, often noticed first by those closest to the person with that type of dementia.
And dementia is not the cause of all memory problems: depression in the older age group is an important cause of memory problems.
It is not entirely clear what the medical model offers for dementia; many of the drugs for memory have modest effect if that in Alzheimer’s disease, the commonest form of dementia worldwide.
In fact, Prof Sube Banerjee last week in the Brighton and Sussex Medical School as the new Chair of Dementia there voiced concerns about the relative ineffectiveness that antidepressants can have in dementia; this comes on top of previous concerns that antipsychotics may be relatively contraindicated in some patients particularly, and might even lower the objective quality of life of an individual with dementia.
It’s impossible also to ignore the effects that a diagnosis of dementia might potentially have on the ability of a person to drive a motor vehicle.
And a diagnosis of dementia might put pressure on well informed people concerning financial considerations through ‘lasting power of attorney’.
One wonders how the drive for diagnosis in primary care can enable a balanced discussion of all these powerful issues, against the background of this government policy to improve diagnosis rates of dementia.
At the tail end of Cathy Jones‘ excellent Channel 5 report, the lack of adequate funding of social care is raised.
Further details of Dr Cosgrove’s concerns are described clearly in this blogpost.
This policy as it stands could do much more damage than good,with many unintended consequences arising from false diagnoses.
But there are pressures at play which might give this policy a sustainable momentum for the timebeing.
Blurred lines in English dementia policy – privatisation in all but name
In case you don’t like the soundtrack, here are the slides.
To some extent, Europe resolved our dispute about whether we should aspire to an ‘early diagnosis’, or ‘timely diagnosis’ for dementia. The overall consensus from the European ALCOVE project was that a diagnosis should be timely, in keeping with the needs of the person with a dementia, his friends, his family or his carers.
This was an extremely helpful move in English policy, although the road had not been that clear.
One blurred line in the public was how dementia so massively became conflated with all memory problems in the elderly. Whilst it was argued that the memory problems in Alzheimer’s disease should no longer be passed off as ageing (and indeed there are strong cultural pressures elsewhere for calling dementia ageing), there was some concern from GPs that older people thought their memory problems were dementia because of the widespread media campaign. Many of these individuals were later to arrive at a diagnosis of minor cognitive impairment, underactive thyroid, or depression. Given that there are hundreds of different causes of dementia which can affect any part of the brain and brainstem (though they all tend to start off in different areas), it’s not altogether surprising that some of the dementias don’t present with memory problems at all.
The drive to make the diagnosis is almost certainly going to be affected by the policy from NHS England to achieve ‘ambitions’ for increasing dementia diagnosis rates. The evidence from the MRC study at Cambridge has demonstrated that this prevalence has in fact been falling over some decades, so there is serious concern that a drive to increase dementia rates will lead to a large number of false diagnoses in 2014. This is definitely one to watch, as a false diagnosis can lead to very serious harmful repercussions. Nonetheless, the number of people who have a MMSE in the region of 10-15 on initial diagnosis is, arguably, staggering, and blatant lack of diagnoses of more obvious presentations of diagnosis most people would agree is unacceptable.
The spotlight in G8, and certainly the presence of corporates there, will lead to increased scrutiny of those people who financially have much to gain from an early diagnosis. An early diagnosis may indeed lead to someone ‘accessing care’, even that care results from a personal health budget with treatments which are not proven clinically from the evidence. The direction of this particular plan depends how far individualised consumer choice is pushed in the name of personalisation. Genetics, neuropsychologists, and pharmaceutical private sector companies wishing to monitor the modest effects of their drugs on substances in the brain all stand to capitalise on dementia in 2014, much of which out of the NHS tax-funded budget. This of course is privatisation of the NHS dementia policy in all but name. One thing this Government has learnt though is how to make a privatisation of health policy appear popular.
Despite corners being cut, and the drive to do ‘more for less’, it will be quite impossible to avoid making a correct diagnosis in individuals thought to have a dementia in the right hands. A full work-up, though the dementia of the Alzheimer type, is the most common necessitates a history of the individual, a history from a friend, an examination (e.g. twitching could be associated with the motor neurone disease variant found in one of the frontotemporal dementias), brain scan (CT/MRI/PET), brain waves (EEG), brain fluid (cerebrospinal fluid), bedside psychology, formal cognitive psychological assessment, and even in some rarely a brain biopsy (for example for variant Creutzfeld-Jacob or a cerebral inflammatory vasculitis).
Analysis by paralysis is clearly not desirable either, but the sticking point, and a blurred line, is how England wishes to combine increasing diagnostic rates; and making resources available for post-diagnosis support; making resources available for the diagnosis process itself including counselling if advised. As the name itself ‘dementia’ changes to ‘neurocognitive impairment’ under the diagnostic manual DSM in 2015, the number of people ‘with the label’ is likely to increase, and this will be ‘good news’ for people who can capitalise on dementia. The label itself ‘neurocognitive impairment’ itself introduces a level of blur to the diagnosis of dementia itself.
The general direction of travel has been an acceleration of privatisation of dementia efforts, but this to be fair is entirely in keeping with the general direction of the Health and Social Care Act (2012). A major question for 2014 is whether this horse has now truly bolted?
Why I wrote ‘Living well with dementia’
“Living well with dementia: the importance of the person and the environment for wellbeing” is my book to be published in the UK on January 14th 2014. I have written it on my own, but I have drawn on the published work a number of Professors working in the field of dementia have sent me. I hope the advantage of having an overview of their research programmes has been to put together with one voice where exactly this approach might be heading using the most contemporary published papers. I am enormously grateful that these busy Professors were able to supply me with their recent papers.
I was asked by my publishers to provide pointers about what a “marketing strategy” for this book might be. I can honestly say that, having given considerable time to thinking about this issue, I have no intention of pursuing a conventional promotion of my book. I don’t intend to do nothing, but I can confidently say that this book will be widely read. I have no intention of flogging it to commissioners, who will have their own understanding of what health or wellbeing is in the modern construct of NHS England’s policy.
I do, however, have every intention of addressing what I think is a major shortfall in the medical profession in their approach to dementia. Their emphasis has been, where done well, the exact diagnosis of dementia through an accurate history and examination of a patient, with appropriate investigations to boot (such as a CT scan, MRI, lumbar puncture, EEG or cognitive psychology). The combined efforts of Big Pharma and medics have produced limited medications for the symptomatic treatment of memory and attention in some dementias, but it would simply be a lie to say that they have a big effect in the majority of patients, or that they reverse the underlying the disease process consistently and robustly.
But that’s the medical model, and certainly the ambition for a ‘cure’ is a laudable one. I found the recent G8 dementia summit inspiring, but a bit of a distraction from providing properly funded solutions for people currently living with one of the hundreds of dementias. Many of us in the academic community have had healthy collaborations for some time; see for example one of the Forewords to my book by Prof Facundo Manes, Chair of Research of the World Federation of Neurology (Dementia and aphasia). To say it was a ‘front’ for Big Pharma would be unnecessarily aggressive, but it has been openly admitted in the media that a purpose of the summit was to assist ‘an ailing industry’.
I think to emphasise what might be done for future patients of dementia would be to fail to maximise the living of people with dementia NOW. By this, I mean a correct and timely diagnosis of an individual, the suggestion of appropriate assistive technologies and innovations, appropriate leisure activities, and the proper design of a positive environment (whether that be a ward, a house or external environment).
My book is strongly footed in current research, but I openly admit that research does not have all the answers. I should like there to be a strong emphasis also in non-pharmacological approaches, such as the benefits of life story and reminiscence, art or dancing. Lack of current research certainly does not make these approaches automatically invalid, particularly when you consider the real reports of people with dementia who have reported benefit.
The main reason is that I do not wish to organise attendance in a series of workshops or conferences about dementia is that I do not wish to be perceived as selling a book. I am more than happy to talk about the work if anyone should so desire. A number of my friends are very well-known newspaper journalists, and I deliberately have not approached any of them as I consider this might be taking advantage of my friendship. I haven’t approached dementia campaigners, or other dementia charities, as I don’t wish to get involved in some sort of competition for other people’s attention. I haven’t sought the ‘celebrity backing’ of some senior practitioners in dementia, although Prof John Hodges (a world expert particularly in the frontotemporal dementias) kindly wrote one of my Forewords. If people wish to discuss the issues in a collaborative manner to take English policy further, I’d be delighted.
At the centre of this book is what an individual with dementia CAN do rather what they cannot do. If you’re looking for a cogent report into the medical deficits of people with dementia, you’ll be sorely disappointed. I spent about 10 years of medical training at undergraduate and postgraduate levels, without having heard of personhood or Tom Kitwood’s work once. I think this a travesty. As a person who is physically disabled himself, the need to understand the whole person is of massive personal significance to me. I think that, beyond doubt, future training of anyone in the caring professions, including medicine, will have to start with understanding the whole person, rather than seeing a patient with a series of problems to be cured or symptomatically addressed.
No academic, practitioner, or charity can have a monopoly of ideas, which is why I hope my book will be sincerely treated with an open mind. People have different motivations for why they get involved in dementia; for example, a corporate wishing to be part of a ‘dementia friendly community’ through a charity might have a different guiding principle to an academic at a University wishing to research from scratch some of the fundamental principles of a dementia friendly community. Despite all the “big players”, nobody can match up to THAT individual who happens to be living with dementia; that person is entitled to the utmost dignity and respect, as brilliantly expressed by Sally Marciano in her powerful Foreword.
I am hoping very much to meet up with some personal friends that I’ve met in the #dementiachallengers community on January 18th 2014, and this is as close as I’ll get to the book launch. But I hope you will find the book readable. I don’t feel that there’s any other book currently available which bridges these two totemic topics (dementia and wellbeing); but I hope there are other good reasons for reading it!
Related articles
- Need for Dementia Caregivers Grows as Boomers Age (abcnews.go.com)
- A cure for dementia could be found within twelve years, David Cameron has said (telegraph.co.uk)
- Simple Steps Could Keep People With Dementia at Home Longer: Study (nackpets.wordpress.com)
The G8 dementia Summit: the comparison with the botched NHS reforms is striking
This week, to great fanfare, the G8 hosted its summit on dementia. Indeed, that the G8 were discussing a single condition was indeed remarkable. That they were joining forces to consider working together on this inspired hope.
What was unforgiveable was the sheer volume of myths about dementia which were pedalled though by the media. Prof Alistair Burns to his credit gave an answer in an interview by Emily Maitlis explaining how dementia prevalence rates appeared to be falling, in response to the backdrop set up by media memes such as ‘timebomb’. Many were left extremely angry on account of the lack of balance, completely distorting the picture such that any idea of someone ‘living well with dementia’ became a rarity.
What was not expected was a sanitisation of advanced dementia, but even there there was not a discussion of end of life care. In fact, there generally was no discussion of a minimum safe level of health and social care in any of the countries. The media pushed hard ‘a cure for dementia by 2025′, which major Alzheimer’s societies had signed up to. The claim is complete and utter rubbish, as there are over a hundred different types of dementia; the public were unashamedly being sold a pup.
The English health system, the National Health Service, has an obsession with ‘efficiency’. So much so it will happily fork out to pay one for one junior doctor covering all the general medical hospital every night for a week, and that junior doctor doesn’t stop all night. Sometimes that junior doctor will be expected to cover the wards too. Cover by nurses can be equally ‘lean’ during the weekends too.
The obsession with measuring ‘I want good care’ and regulation is akin to a teacher who has forgotten to teach but can set regular assessments. When the system is set up to run everything with much less doing a lot more, it’s possible something has got to give. And this is of course precisely what happened at Mid Staffs.
And yet out of the blue there appeared a 493 page document ultimately called the Health and Social Care Act (2012) which had nothing to do with this most important point about patient safety. There is not even a single clause to do with patient safety (unless you include the clause abolishing the National Patient Safety Agency). The medical Royal Colleges were not involved. The BMA was not involved. And yet the Act of parliament, outsourcing and privatising the NHS, is just what the Corporate ordered.
This is what is known in the (business) trade as an ‘opportunity cost’ where money and efforts could have been better spent elsewhere. In this particular case, despite a promise of ‘no top reorganisation’, there was a £3bn reorganisation.
When attending a medical ward, you have to go to the sick patient first. You have to prioritise. If there had to be an unannounced reform of the NHS, outsourcing it was not the priority. The latest survey even shows that the public don’t especially like private providers doing NHS work.
Likewise, the priority for dementia care should have been investment in the social capital of caring. Too often carers are embattled with the biological, financial and legal considerations of caring. Many carers are themselves on zero-hours contracts. The G8 dementia summit was a great opportunity to confront that.
It didn’t. Instead, with alarming synchrony, the G8 leaders came together to sing off the corporate script. Vivienne Parry with effortless ease choreographed a seemingly spontaneous discussion about well rehearsed arguments for the need for ‘big data’, global data sharing, genomics, and personalised medicine, for much of the day. Prevention was of course discussed, but this is of course intimately wound up with the collection of information about the person, and the use of that other pet subject, biomarkers.
And more research is not better research, in the same way bigger information is not better information. If research monies are diverted into data analysis, genomics and personalised medicine, these monies will be diverted away from research into caring for example. One wonders whither the ‘cure for dementia’ will actually go, unless they have another fifteen years to look at slowing the progression of Alzheimer’s disease. The evidence that cholinesterase inhibitors, a class of drugs used to treat symptomatically memory and attention problems in Alzheimer’s disease, has a beneficial effect on slowing disease progression is as low as it possibly can be after nearly 20 years of expensive research in this area.
The G8 summit, like the Health and Social Care Act, was ‘corporate capture’ at its best, so if you’re angry, well done, that is the appropriate emotional reaction! If you were wondering if you’d accidentally missed the discussion of carers and how they would be involved until 2025, don’t worry, you hadn’t. They weren’t there.
The #G8Dementia Summit: a lack of cure for dementia, and tough on the causes of the lack of cure
The setting for today’s #G8Dementia Summit was in Lancaster House, London.
Many thanks to Beth Britton, Ambassador for Alzheimer’s BRACE and campaigner, Anna Hepburn at the Department of Health, and Dr Peter Gordon, Consultant and expert in dementia, for helping understand, with the excellent livestream from the Department of Health, what challenges might be in store for global dementia policy in the near future.
My account is @dementia_2014
The final G8 Summit Communique is here.
The G8 Summit Declaration is here.
There’s a bit of a problem with global dementia policy.
The patients, carers, families, businesses, corporate investors, charities, media, academics (including researchers) politicians, all appear to have different opinions, depending on who you speak to.
Peter Dunlop, a man with dementia of Alzheimer type, received a standing ovation after his speech. He had explained his reactions on receiving a diagnosis, and how has tried to continue enjoying life. He had been a Consultant Obstetrician and Gynaecologist.
Peter Dunlop: “I continue to enjoy life and fishing” – Moving testimony that a good life with #dementia is possible! #G8dementia
— Alzheimer Europe (@AlzheimerEurope) December 11, 2013
Peter Dunlop had a standing ovation from #G8dementia – NEVER underestimate the power of the lived experience of dementia
— Beth Britton (@bethyb1886) December 11, 2013
The people with dementia who appeared did indeed remind the audience, including Big Pharma, why they were there at all.
Trevor Jarvis talks about person-centered care and need for doctors to fully understand the disease. What an eloquent gentleman. #G8dementia
— Romina Oliverio (@RominaOliverio) December 11, 2013
And that there was more to life than medications:
AE Chair Heike von Lützau-Hohlbein highlights role of self-help movement and successful advocacy work #G8dementia
— Alzheimer Europe (@AlzheimerEurope) December 11, 2013
And this was sort-of touched on even by the Prime Minister:
‘Today is about three things: realism, determination and hope.’ @David_Cameron #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
And personhood was not completely lost on David Cameron MP:
‘… this is about allowing people to live well with dementia, and with dignity’ @David_Cameron #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
And this was indeed music to the ears of people like me, and countless of persons with dementia, their carers, friends and relatives, for example:
Cameron: It’s not just about finding a cure, it’s also about helping people with dementia to lead more fulfilling lives. #G8dementia
— DeNDRoN (@nihrdendron) December 11, 2013
Elephant in the room according to @marcwort is the number of people with #dementia in developing countries #G8dementia
— Alzheimer Europe (@AlzheimerEurope) December 11, 2013
And the carers were listening carefully too..!
listening for David Cameron to tell us some good news for those living with dementia now #G8dementia
— Dementia Skills (@Dementiaskills) December 11, 2013
There was some concern aired that the volunteers and charities would been seen as a valid alternative for a properly supported health and social care system. Whilst everyone agreed that ‘dementia friends’ and ‘dementia friendly communities’ were worthy causes, everyone also agreed that these should not replace actual care.
Please don’t defer the responsibility to volunteers and charities – health and social care need to step up #G8dementia #DAACC2A
— DAA Carers Action (@DAAcarers) December 11, 2013
Part of the aim of today was to foster of culture of diminishing stigma. And yet the media had been full of words such as ‘cruel disease’, ‘robs you of your mind’, ‘horrific’. So the politicians seem conflicted between this utter armageddon and wishing to destigmatise dementia, with generally pitiful results.
Some of the language in the last 24 hours has indeed been truly diabolical. I took a break to watch the main news item on the BBC, and Fergus Walsh was heading up the main item on dementia with extremely terrifying language.
#G8dementia I was going to keep track of how many times the word “Fight” was used today. I have long since lost count! #militarymetaphors
— Peter Gordon (@PeterDLROW) December 11, 2013
But the Summit kept on reverting to the ‘real world’, pretty regularly though.
A pervasive theme, brought up by many health ministers and other interested parties, was how dementia carers themselves needed supported. Dr Margaret Chan even later in the day spoke about a new online resource for carers, which would be fantastic.
“Dementia carers also need our support.” Dr Chan @WHO #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
‘We’re going to develop an online resource to help carers.” Dr Margaret Chan @WHO #G8dementia This is indeed brilliant news.
— Living Well Dementia (@dementia_2014) December 11, 2013
An aspect of why this situation had arisen was not really explained. Prof Martin Rossor, Honorary Consultant for the Dementia and Cognitive Disorders unit at Queen Square, described the dementia issue as ‘a wicked problem’ on the BBC “You and Yours”. However, Dr Margaret Chan from WHO was much more blunt.
“This is yet another case of market failure.” Dr Margaret Chan @WHO #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
Big Pharma had failed to ‘come up with the goods’, despite decades of trying.
Dr Chan: In terms of a cure (for #dementia), or even treatments that can modify the disorder or slow its progression, we are empty-handed
— WHO (@WHO) December 11, 2013
But few speakers were in any doubt about the societal impact of dementia, though much of the media resorted to scare tactics as usual in their messaging.
London-G8HealthMinisters on dementia. One of the most important challenges for ageing societies.Huge human,social and economic impact.#OECD
— Yves Leterme (@YLeterme) December 10, 2013
The speakers on the whole did not wish to discuss how care for people could be reconfigured. The disconnect between the health and social care systems is clearly a concern in English policy. And indeed this was even raised.
Integrated approach for the delivery of services bridging health and social care is needed, says @yleterme #G8dementia
— Alzheimer Europe (@AlzheimerEurope) December 11, 2013
All was not lost regarding wellbeing.
Hazel Blears, Labour MP for Salford, explained how her mother was living with dementia, so it was vital that policy should do everything it could do to help people live with dementia.
“We need to find the evidence for non-pharmacological interventions as well.” @HazelBlearsMP #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
I met the Salford Institute for Dementia, a brand new Twitter account, for the first time this afternoon, which was in fact one of the highlights of my day.
Salford Institute for Dementia launched to use research to improve the lives of people with dementia #G8dementia http://t.co/BgDw3X9Xw9
— Inst for Dementia (@InstforDementia) December 11, 2013
Although not pole position compared to ‘cures’ and ‘disease modifying drugs’, it was clear that the #G8summit were keen to support assistive technology, telecare and telemedicine. This could be in part due to the generous research grants from various jurisdictions for innovation, or it could be a genuine drive to improve the wellbeing of persons living with dementia.
‘Homecare is arguably one of the best means of care because of quality of life – we should all think of innovative ways to keep ppl at home’
— Anna Hepburn (@AnnaHepburnDH) December 11, 2013
At just before lunchtime, I suddenly “twigged it”.
I must admit I was angry at myself for having been “slow on the uptake”.
I now understand what this ‘data sharing’ drive is about. It’s for DNA genomic collaboration to develop personalised treatment. #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
As it was, the discussion appeared to swing periodically between two ends of an extreme during the course of the day. At one end, the discussion was about ‘big data’ and ‘open data’ sharing.
Vivienne Parry , then said how she preferred the term ‘safe data’ to ‘open data’, but Twitter was at that point awash with queries as to whether a rose by any other name would smell as sweet?
@vivienneparry has hit the nail on the head; ‘unsafe’ data sharing could be perceived as reducing risk for corporate investors. #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
People conceded the need for persons and patients voluntarily to contribute to these data sets, and for international organisations such as WHO to attempt to formulate standardised harmonised templates for these data. At the other end, people were very keen to talk about genetic information, presumably DNA, being the subject of DNA genomics data scrutiny at a personal level.
Also, the discussion itself swung from personal tales (such as Beth Britton’s) to a discussion of looking at societal information as to what sorts of data clusters might show ‘susceptibility’ in their genetic information decades before the onset of clinical dementia. Big data, like 3D printers, has been identified as ‘the next big thing’ by corporates, and it’s no wonder really that big data should of interest to big Pharma corporates.
Having failed spectacularly to have produced a cure or disease-modifying drugs across a number of decades, Pharma are left with two avenues. One is that they look at the individual response to therapy of drugs at a single case level using radio-active binding studies (radio-ligand binding studies), and monitor any slowing of build-up of abnormal protein in the brain as a response to treatment. How much this actually benefits the patient is another thing.
Or Big Pharma can build up huge databases across a number of continents with patient data. Researchers consider this to be in the public interest, but patients are clearly concerned about the data privacy implications.
Here, it was clear that Big Pharma could form powerful allies with the charities (which also acted as patient groups):
“Data sharing is absolutely essential to make the advances needed across the world.” Harry Johns, Alzheimer’s Association #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
And of course this agenda was very much helped by Sir Mark Walport being so enthusiastic about data sharing. Having been at the Wellcome Trust, his views on data sharing were already well known though.
“There are concerns about ‘Big Data’ around the world.” Sir Mark Walport CSO #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
If it were that regulators could allow data sharing more easily, justified presumably on public policy grounds such that freedom of information was more important than data protection according to the legal doctrine of proportionality, this plan could then considerably less risky for corporate investors wishing to invest in Big Pharma.
Andrea Ponti from JP Morgan gave this extremely interesting perspective, which is interesting given the well known phenomena of ‘corporate capture’ of health policy, and ‘rent seeking behaviours’ of corporates.
The G8 have a great opportunity to altering the risk and return ratios, important for investors.” Andrea Ponti @jpmorganfunds #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
It has been argued that waiting for valid consent from the patients would take too long, so presumed consent is more of a practical option. However, this ethically is an extremely tricky argument. The Pharma representatives were very keen to emphasise the ‘free flow’ of data, and the need to ‘harmonise regulation'; but they will be aware that this will requiring relaxing of the laws of more than one country.
And so, during the course of the day, the agenda of Big Pharma became clear. They intended to be tough on the lack of cure for dementia, and tough on the causes of that cure. Some might say, that, as certain anti-dementia drugs come to the end of their patents (and evergreening is not an option), they have suddenly converged on this idea to tackle dementia, as it is a source of profitability to enhance shareholder dividend. They now need new business models to make it succeed (and various charities and research programmes which benefit from this corporate citizenry might be able to make it work too.)
“We have introduced approaches which encourage personalisation and individualisation of care.” Madame Marisol Touraine #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
But during the course of the day those ‘pesky’ tweets about person-centred care kept on coming…
As #G8Dementia summit about to start – see the person not the diagnosis with @SCIE_socialcare award winning film http://t.co/PJ58m6xWB9
— Andrea Sutcliffe (@Crouchendtiger7) December 11, 2013
Some of the tales were truly heart-breaking.
“I lost friends. Well I say friends. If they can’t cope with a diagnosis of dementia, they’re not really friends.” @BethyB1886 #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
But I was happy because Beth was happy at the reception of her film. She is so utterly passionate, and totally authentic, about the importance of her father who had dementia. It was a privilege for us to see how well the film had been received by all there at the #G8summit.
Our montage film, featuring people with dementia & carers (inc me), well received at #G8dementia
— Beth Britton (@bethyb1886) December 11, 2013
And those pesky tweets kept on coming…!
Watch our award winning #SocialCareTV film ‘Getting to know the person with #dementia‘: http://t.co/tivbpYkb8Z
— SCIE (@SCIE_socialcare) December 11, 2013
But indeed there was a lot to be positive about, as research monies if well spent could provide a cure or disease-modifying drugs. Big Pharma and the researchers know that they are not only trying to tackle the big one, the dementia of the Alzheimer type, but also other types such as the vascular dementias, frontotemporal dementias and diffuse Lewy body disease.
EU announces Horizon 2020 call dementia & neurodegenerative disease in 2014/2015 €1.2 billion #G8dementia @isgtw @martinrossor
— DeNDRoN (@nihrdendron) December 11, 2013
Beth’s input today was invaluable.
“I would really like to make a plea, on behalf of the delegates, for non-pharmacological interventions. Thank you.” @BethyB1886 #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
And Dr Peter Gordon loved it!
@bethyb1886 and @HazelBlearsMP well said, both of you. We need balance in our approach. Your voices matter so much #foryourfolk
— Peter Gordon (@PeterDLROW) December 11, 2013
But the best comment of the day must certainly go to Dr Margaret Chan, a V sign to those obsessed with Big Data spreadsheets and molecular biologists looking at their Petri dishes:
‘We’re going to develop person-centred care, not talk about people as collections of organs or diseases’ Dr Margaret Chan @WHO #G8dementia
— Living Well Dementia (@dementia_2014) December 11, 2013
In summary…
It smelt like a corporate agenda.
It looked like a corporate agenda.
It sounded like a corporate agenda.
And guess what?
All the ingredients of ‘corporate capture’ were in attendance: big data, personalised medicine, genomics, data sharing. They’d have managed a full house had the world leaders found a use for 3D printers in all of this.
Related articles
- The G8 Dementia Summit cannot just be about “Pharma-friendly communities” (livingwelldementia.org)
- All stick and no carrot? How much diagnosis, but how much actual care, of dementia? (livingwelldementia.org)
- The #G8Dementia Summit – hopefully a chance for real campaigners, not an international trade fair (livingwelldementia.org)
- Dementia cure ‘within our grasp’, says David Cameron (standard.co.uk)
Is a new sophisticated brain scan desirable to diagnose dementia?
Wouldn’t it be lovely Prime Minister, David Cameron MP, could announce a breakthrough which nails the problem of the diagnosis of Alzheimer’s disease?
The definitive diagnosis of dementia of the Alzheimer type (DAT) comes post mortem (though in practice various techniques while the patient is alive can be used to tell whether a patient has a type of dementia).
The full armoury of tests includes thinking tests or cognitive neuropsychology, a sample of the fluid from the spine (cerebrospinal fluid), the clinical history and examination of the patient, brain waves (the EEG), or even (rarely) a brain biopsy; that’s even before considering types of scan, like the ‘CT scan’, the ‘MRI scan’, or ‘functional scan’.
The trick of the clinician, varying with levels of expertise, is to make the diagnosis reliably such that a person living with dementia might be able to ‘access’ appropriate care in the system; and those without dementia aren’t given an incorrect label of ‘dementia’.
DAT is one of the hundreds of causes of dementia (although most of the media use ‘Alzheimer’s Disease’ and dementia unhelpfully synonymously.)
Amyloid build-up and the diagnosis
There has been a popular idea that the build up of a substance called amyloid which builds up in the brain might hold the clue to early diagnosis of Alzheimer’s Disease.
In recent years, the emphasis has swung to ‘timely diagnosis’, with the national clinical lead for dementia, Prof Alistair Burns, emphasising that the diagnosis should be made at a time appropriate for the person himself or herself.
A ‘quick fix’ in a test for DAT seems very attractive, but it’s important to remember that the dementia of the Alzheimer type is only one (but the most common) cause of dementia across all age groups.
How to use the test in a safe way
The way in which this diagnosis could be made has also come under scrutiny. A method which uses a radioactive label to which at how much label can bind to abnormal amyloid in the brain, to be practical, should not be excessively time-consuming to administer. It also should not be prohibitively expensive.
Also critically, it should be reliable. In other words, it shouldn’t show up ‘positives’ in otherwise well people, who never go onto develop dementia. A critical problem is that there are many causes of memory loss in older people, including of course depression.
To make things even more complicated, there is a very interesting group of people whose thinking and memory are normal, even late in life, yet their brains are full of amyloid beta plaques that appear to be identical to what’s seen in dementia of the Alzheimer type. How this can occur is an important clinical research question.
Hard plaques made of a protein called amyloid beta are always present in the brain of a person diagnosed with the dementia of the Alzheimer type. But the simple presence of plaques does not always result in impaired thinking and memory. In other words, the plaques are necessary – but not sufficient – to cause DAT.
Is it the type of amyloid which matters?
Earlier this year a paper was published in the prestigious journal in the US (Esparza TJ, Zhao H, Cirrito JR, Cairns NJ, Bateman RJ, Holtzman DM, Brody DL. (2013) Amyloid-? oligomerization in Alzheimer dementia versus high-pathology controls. Ann Neurol. 73(1):104-19. doi: 10.1002/ana.23748. Epub 2012 Dec 7.)
An important clue may come from still come from a form of amyloid beta, but not necessarily in the form of plaques. Instead, smaller molecules of amyloid beta appear more closely correlated with whether a person develops symptoms of dementia; these are called “amyloid beta oligomers“.
Earlier this year, this group developed a way of measuring these amyloid beta oligomers in minute quantities, without binding to similar things.
These amyloid beta oligomers were detected in samples of brain from patients with DAT and nondemented patients with amyloid plaque pathology. However, amyloid beta oligomer concentrations in samples from patients with DAT were tightly correlated with amyloid plaque coverage (correlation very high), but this relationship was weaker in those from nondemented patients (correlation very low) despite equivalent amyloid plaque pathology.
The results raise the intriguing hypothesis that the linkage between plaques and oligomers may be a key pathophysiological event underlying DAT.
This test would be clearly potentially profitable for people who have developed this test, and the critical issue is whether if you scan real patients whether the amount of radioactive binding will reliably distinguish between people with dementia and those without.
Would a new brain scan be helpful?
Looking for amyloid in people who might be developing dementia has been a story going on for ages. The Telegraph newspaper reports a “breakthrough” in a scan, but the description is that of plaques (leading to the possibility of people having lots of plaques found on imaging who later never develop dementia):
“The scan was developed by scientists in London. The test involves giving a patient exhibiting signs of dementia a small amount of a radioactive substance, which will allow amyloid plaques to show up in a brain scan.
The presence of the plaques in the brain is one of the main signs of Alzheimer’s, although it does not make the disease inevitable, so doctors using the test would be sure of giving a patient the all-clear only if the plaques were absent.
It is the first time doctors have been able to detect the plaques while a patient is alive.”
The desire ‘to catch Alzheimer’s early’ – and the actual pitfalls
A major issue is going to be which people should be put forward for such an imaging technique; there has been intense scrutiny of whether bedside tests can reliably tell the difference between people who have a ‘mild cognitive deficit’ and those who have dementia.
A political drive, almost in total parallel led by the current UK and US governments, to “screen” older people for minor memory changes could potentially be leading to unnecessary investigation and potentially harmful treatment for what is arguably an inevitable consequence of ageing. There are no drugs that prevent the progression of dementia according to human studies, or are effective in patients with mild cognitive impairment, raising concerns that once patients are labelled with mild cognitive deficits as a “pre-disease” for dementia, they may try untested therapies and run the risk of adverse effects.
The idea itself that there is a “pre-disease” stage before the full-blown course of the dementia of Alzheimer type is itself erroneous, if one actually bothers to look at the published neuroscientific evidence. A mild cognitive impairment (“MCI”) is a clinical diagnosis in which deficits in cognitive function are evident but not of sufficient severity to warrant a diagnosis of dementia (Nelson and O’Connor, 2008).
However, the evidence of progression of MCI (mild cognitive impairment) to DAT is currently weak. This has been much to the frustration of some researchers where it had been hoped for years that this could be used to identify DAT at an early stage. It might be attractive to think that MCI is a preclinical form of dementia of Alzheimer Type, but unfortunately the evidence is not there to back this claim up at present: only approximately 5-10% and most people with MCI will not progress to dementia even after ten years of follow-up (Mitchell and Shiri-Feshki, 2009).
It’s the post-diagnosis support anyway…
Either way, there should still be adequate post-diagnosis support, which is a problem which simply won’t go away.
Therefore, this result of a ‘breakthrough’, for one of the more common causes of dementia, has to be sufficiently exciting for the drug companies to have a ‘return on investment’ who have developed them.
However, in a week which has seen increasing scrutiny as to whether pharmaceutical-based approaches have been a waste of dawn, particular interest will be paid as to whether this is in fact yet another “false dawn”.
Other references
Mitchell, A.J., and Shiri-Feshki, M. (2009) Rate of progression of mild cognitive impairment to dementia -meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand, 119(4), pp. 252-65.
Nelson, A.P., and O’Connor, M.G. (2008) Mild cognitive impairment: a neuropsychological perspective, CNS Spectr, 13(1), pp. 56-64.
Related articles
- NHS scan to rule out Alzheimer’s (telegraph.co.uk)
- How Brain Scans Might Change the Way Doctors Diagnose Alzheimer s (scientificamerican.com)
- Hardening of Arteries Linked to Plaques in Brain (fightaging.org)
The G8 Dementia Summit cannot just be about “Pharma-friendly communities”, but must be about people
A ‘cure for dementia’ would be wonderful.
The phrase is, of course, as meaningless as a ‘cure for cancer’, but equally trips off the tongue for corporate fundraising purposes. Like there are many different forms of cancer, like breast, ovary or bone, there are many different forms of dementia, like Alzheimer’s, frontotemporal or HIV.
It’s clear not everyone is going to be a winner from the G8 Dementia Summit promotional package. The write-ups of the dementia research strategy have included ‘the usual suspects’ from “Pharma-friendly communities”, with a token sop to research for wellbeing.
The G8 Dementia Summit is an extremely good way of promoting dementia as a worthy public health issue. Many passionate campaigners will indeed take to the stage to explain, often in very personal terms, why dementia is an incredibly important issue for them. It has become extraordinarily difficult not to know somebody who, in one way or another, is touched by dementia.
The complex nature of dementia has forced policy makers and national governments to invest the financial resources available in three main areas: first, medical research to find a cure for the disease or at least ways to prevent it; second, pharmacological care; and finally, support for caregivers, such as information, training, psychological assistance, etc. Arguably though, none of the three areas, however, have the ‘real’ person at the centre of their interest.
There is also now way that the media can get away with their marginalising of carers for a ‘cure’. Carers face considerable pressures, as they are forced to understand at shotgun notice the biologicial, personal, legal and financial consequences of the dementia. Apart of anything else, many carers, often employed by large private companies, are paid less than a living wage on a ‘zero-hour contract’. Unsurprisingly, how we prioritise the value of care rather than the dividend of a shareholder in a large pharmaceutical company is an important debate to be had.
The cultural stereotype of dementia across various countries is indeed noteworthy. The picture of dementia emerging from these socially-constructed discourses is, at worst, that of a body without a mind, of a hollow shell: that is, a picture in which the dementia “obliterates” the subject, and calls for constant care either by the family members – informal caregivers – or by formal caregivers, at home or in nursing home facilities. This is a powerful pitch by dementia charities, but stigmatises massively those individuals wishing to lead normal lives with more mild forms of dementia.
The stigma is in fact deeply entrenched. The Merriam-Webster Online Dictionary of 2004 defines dementia first as “mental deterioration of organic or functional origin.” Although a generalization [sic], it seems innocuous and close to what is intended by physicians. However, on further reading almost every dictionary refers to its derivation from Latin, meaning madness or out of one’s mind. This debate has, nonetheless, recently hit a new level with the discussion of whether the word ‘dementia’ should be dropped altogether.
‘Minor or major neurocognitive deficits’ as an alternative term has its supporters and critics.
Norman McNamara, well known campaigner for dementia awareness, has even asked on his Facebook page whether dementia “should come under a mental health banner” (reported here).
Kitwood produced a ‘sea change’ in thinking for placing the individual with dementia at the centre of all discourses about it. Within this social-psychological approach to dementia of the Alzheimer type, Kitwood ?’s concept of personhood emerges. Personhood is defined as ‘a status or standing bestowed upon one human being, by others, in the context of social relationship and social being. It implies recognition, respect and trust’.
Dementia is not an unitary construct. It does not only affect the old. And yet ‘messaging’ of dementia consistently has an unpleasant streak of ageism. According to Richard Titmuss, “Viewed historically, it is difficult to understand why the gradual emergence in Britain of a more balanced age structure should be regarded as a “problem of ageing”.”
Ageist stereotypes in Western culture, from the classical period to the present, have gained strength in a social environment in which ageing is perceived as a problem and portrayed negatively. The general connotations of being old – ill, disabled, with failed memory, senile, sad, lonely, grouchy, sexless, boring, lacking vitality, in decline, unable to learn and unproductive. Stereotypes are powerful, as they spread through cultural productions, media, and policies, hence perpetuating them in the social structure, and empowering collective ideologies by marginalising those belonging to the stereotyped group.
That the G8 dementia summit should have such a naked Pharma bent is of course no big surprise. Sales of the five dementia drugs were just shy of $3 billion in 2007. Donepezil and memantine accounted
for 85% of those sales; tacrine had fallen out of use because of its high adverse effect profile. The memory-boosting drugs, whilst expensive, are generally thought to have very modest effects; and there is no evidence in humans that they slow the rate of progression thus far.
However, the effects of medical labels are always mixed.
Medical labels may operate as instruments of empowerment and social recognition that allow individuals to legitimise their grievances in their own and others’ eyes; they may also operate as instruments of professional expansion, social control, and corporate dominance, serving to pathologise normal functioning, unduly reinforce gender norms.
The danger, observed by some, is that the work of medical researchers has transformed what for years was seen as a rare medical condition into a “major killer” and threat to the wellbeing of predominantly the elderly and their caregivers.
This transformation was critical to the consolidation of a movement born from the grievances of sufferers of a range of cognitive, behavioral and personality impairments and their caretakers, because it gave these impair- ments a biomedical definition, thus creating an “entity” deemed modifiable through the application of biomedical science.
The experience of the USA is interesting. As dementia advocacy grew, so did coincidentally the small government ideology of the Reagan years. (A similar phenomenon is happening here with the UK Coalition administration, though perhaps a ‘small state’ should be more accurately described as an ‘outsourced state’). The Omnibus Budget Reconciliation Act of 1980 was the legislative vehicle for the implementation of this ideology, which reduced social services at the same time that it appeared to respond to the “crisis” and public grievances. The Act gave broad authority to the states to restrict Medicaid program eligibility, reduce the number and type of covered services, and limit payments to hospitals.
These reductions in federal support for health and social services occurred at a time when states and cities were experiencing the combined effects of a lagging economy and of various spending limitations imposed by the passage of tax-limiting measures such as Proposition 13 in California and Proposition 2 1?2 in Massachusetts.
Yet another element leading to the triumph of “cure” over “care” was a largely idealised notion of “nuclear family” family functions, which grained ground during this time of political and cultural conservatism, and legitimised an inequitable societal workload falling on women in the provision of long-term care.
Clearly, caregiving, a resource-intensive activity falling predominately on women, is neither “budgetable” nor appreciated at the policy level. So again, rather paradoxically, not only did the heart-rending testimony of caregivers to Congressional committees advocating for more support fail to lead to more formal services and relief of women’s workload, it also legitimised the biomedical framework that deviates public support away from caregivers, as it feeds the hope for effective treatments or a cure for dementia that presumably will derail the “explosive” future costs of caring.
Ironically, here in the UK, the website of the “Dementia Advocacy Network” gets taken down at the end of next month. It is in fact the last week of its hardworking manager, Jan Kendall. This Network was invaluable in offering non-statutory guidance for advocacy, in keeping with statement 9 of the recently published NICE quality standard. This statement on independent advocacy.
Jan Kendall’s experience is sadly not unique. There has been a starvation of funds as many entities in the third sector have found it difficult to cope. The situation in the charity sector is remarkably similar to how City firms have experienced maintained revenues, while high street law firms have been forced to shut down.
The narrative from “Pharma-friendly communities” in the media threatens to drown out what is actually happening on the ground. It is recently reported that budget cuts forced a record 220,000 dementia sufferers to turn to hospital A&E units for help last year.
There is, of course, nothing to stop Big Pharma or large dementia charities to act as good ‘corporate citizens’ , in keeping with the views of Professor Michael Porter at Harvard Business School, in helping to fund frontline care.
But the danger is that this ‘drive for a cure’ represents yet another attack on the running of a universal healthcare system, which should be in principle funded through a fair and equitable general taxation.
Julian Tudor-Hart unsurprisingly puts it perfectly.
“Volume, costs and content of medical care depend on demand, which depends on professional and public expectations. The UK National Health Service (NHS) removed price barriers to access, and depressed expectations became an important factor in cost control. In USA, professional control of care business inflated expectations, and consequent costs. Managed care in the NHS failed to rationalise care because managers seem even less trustworthy than clinicians as arbiters of rational expectations in contexts of permanent underfunding. Development of rational expectations depends on restored trust, mutual and managerial respect for the expertise of both clinicians and patients, and transcendence of the provider-consumer model for value production in medical care.”
This is, contrast, is EXACTLY what person-centred care should be aiming to achieve: allowing people to live well with dementia. The ability of drugs to help people to live well with dementia currently is relatively poor. But Beth’s experience should indeed be about inspiring people who care about dementia. Thanks also enormously to the Department of Health for their efforts in this direction.
Enormous thanks to Dr John Rumbold, Dr Jonathon Tomlinson and Prof Julia Simard for indirect help with this article.