Home » Economics of healthcare
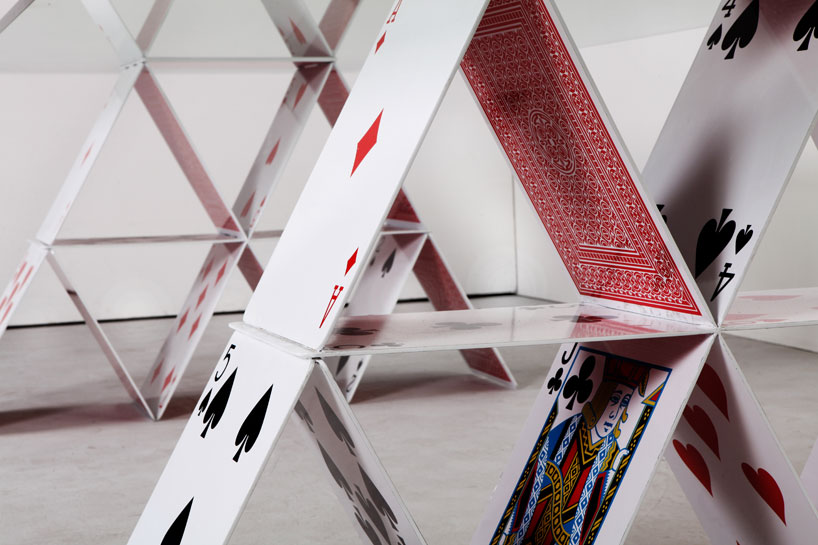
Like a faulty house of cards, the competition rationale for the Health and Social Care has fallen apart
In the beginning….
In the beginning, there was garbage and rhetoric. It sounded nice, but it was intellectually devoid of quality, there was not much competition for ideas even though this WAS bad, and so there was not much choice.
Julian LeGrand back in 2003 talks of the “competition juggernaut”:
Labour has made many mistakes, usually and unsurprisingly given its roots in socialism and central planning, in the direction of too heavy-handed central control. The public service juggernauts are now on a different course, with decentralisation, competition and choice as part of their route maps – and with plenty of resources as fuel. If they fail to arrive at their destination, if our expectations are dashed, there will be real questions over the future of each area of public services: how long can it remain public; how long can it remain a service?
‘Competition fever‘ should have never have got off the ground. The University of York, Economics of Social Care and Health Unit, and Centre for Health Economics once published a study of ‘Hospital competition under fixed prices’ (research paper 80).
The argument that competition improves quality fell apart because of the sheer volume of invalid assumptions, as demonstrated in the following quotation from that document:
The review of the theoretical literature suggests that the plausible argument that greater competition amongst providers facing fixed prices will lead to higher quality rests on strong assumptions which may not hold. The literature shows that more competition increases quality when providers are profit maximisers and marginal cost of treatment is constant. Competition has an ambiguous or negative effect on quality when providers are altruistic, the marginal cost of treatment is increasing and quality is only imperfectly observable. The literature has been largely silent on the relationship between market size, as measured by total population or population density, and quality.
Competition as the failed central plank of the Health and Social Care Act (2012)
The raison d’être of the Health and Social Care Act (2012) is nothing to do with improving clinical care, though that could be a consequence of its three main areas. There is nothing about how patient staffing can be addressed, related to the equally potent issue of patient safety. It has never been entirely clear how the Act came about, but the three planks of policy are laid bare by the impact assessments from the Department of Health (2011) (published here on 19 January 2011). The three main planks of the Bill are firstly to establish the competitive market as the substrate for the National Health Service, to define better the insolvency régime (it is important to clarify how economic entities as autonomous units can be allowed to fail ‘to get them out of the system’), and the machinery needed to regulate the market. I will come to how Monitor has had to come into being to ‘regulate the internal market’, but it is not insignificant that introducing the market is itself a source of waste and inefficiency (such as duplicated transaction costs). Of course, the issue of how to regulate the internal market should be regulated has often been analysed in a substandard manner before by some social scientists, not competition lawyers, but this is now an important policy issue which has been thrust into the limelight.
Central to this argument is that competition promotes innovation. This is indeed cited on page 41 of the “Impact assessment”.
Ahn (2002) reviews a large number of studies on the link between competition and innovation and concludes that competition encourages innovative activities and has a significant impact on long-term productivity growth:
“Competition has pervasive and long lasting effects on economic performance by affecting economic actors’ incentive structure, by encouraging their innovative activities, and by selecting more efficient ones from less efficient ones over time”.
The myth that competition drives innovation, when COLLABORATION does
However, there is an intrinsic problem in business management: the assumption that competition drives innovation. This bit of missing evidence in the impact assessments totally distorts the raison d’être of the Act itself, and of course there is a separate debate in management as to whether innovation can be detrimental to organisational culture or learning. There is considerable evidence now that collaboration, not competition, can be essential for innovation. This theme is taken up in an interesting article about ‘internal markets’ from Forbes:
Major innovation needs collaboration, not competition. For innovation, internal markets have the same problem as hierarchical bureaucracies. Managers vote their resources for innovations that bolster their current fiefdoms and careers. The safest strategy is to stick to the status quo. Ms. Kimes’ article gives multiple examples where competing managers at Sears looked after their own units at the expense of the interests of the firm as a whole.
Second, innovation isn’t basically an issue of spending. Booz & Company’s annual innovation reports repeatedly state: “Spending more on R&D won’t drive results. The most crucial factors are strategic alignment and a culture that supports innovation.”
Finally, the hope of the internal markets theory is that, by funding a variety of different ideas, the organization will emulate the evolutionary process of natural selection and so the best ideas will survive and prosper. The problem is that once a disruptive idea starts to flourish and becomes more interesting than the normal bread-and-butter work of the organization, it risks becoming a threat to the rest of the organization.
The wheels are coming off the Competition Juggernaut a bit sooner than expected
David Williams at the Health Services Journal only very recently on 16 September 2013 reported that:
NHS England has delayed the publication of its choice and competition framework amid a “paucity of evidence” of the benefit to patients.
Policy director Bill McCarthy made the announcement at a board meeting on Friday, highlighting the issue as a new risk for the central body.
The framework and supporting documents were originally slated for publication in July.
Mr McCarthy said: “We’re having [a discussion] with Monitor around choice and competition, and how best they can be applied in healthcare to improve outcomes for patients, including a better experience.
“That’s taken a bit longer than we hoped.
“We had hoped to be able to put out some guidance early in the summer – I think that probably reflects… it is one of the areas where there is a paucity of evidence.”
“Operation Propper”
Clause “B47” (p.42/3) in the official Impact Assessments from the Department of Health cites one of the key planks of evidence that the Department of Health wishes to use in promoting its competition argument.
“A July 2010 study by health economists Martin Gaynor, Rodrigo Moreno-Serra, and Carol Propper investigated outcomes in the NHS following the introduction of choice in 2006. They conclude as follows: “We find that the effect of competition is to save lives without raising costs. Patients discharged from hospitals located in markets where competition was more feasible were less likely to die, had shorter length of stay and were treated at the same cost”. The study found that there was a larger inflow of patients to better quality hospitals after the 2006 NHS reforms, suggesting that popular providers in health care are able to expand supply.”
There is an even worse justification for the competition dogma later in the Department of Health’s official impact assessments:
B48. A January 2010 study by the London School of Economics also looked at NHS data post- introduction of choice in 2006. The key conclusion is as follows: “Using AMI mortality as a quality indicator, we find that mortality fell more quickly (i.e. quality improved) for patients living in more competitive markets after the introduction of hospital competition in January 2006. Our results suggest that hospital competition in markets with fixed prices can lead to improvements in clinical quality”.
B49. Evidence from the LSE shows that management quality – measured using a new survey tool – is strongly correlated with financial and clinical outcomes such as survival rates from emergency heart attack admissions (AMI). Moreover, the study finds that higher competition (as indicated by a greater number of neighbouring hospitals) is positively correlated with increased management quality.
The general issue received a scathing response from Allyson Pollock, Alison Macfarlane and Ian Greener who could not have put it any clearer.
The major improvements in outcome after acute myocardial infarction can be attributed to improvements in primary prevention in general practice and in hospital care, including the introduction of percutaneous IV angiography. The government’s own cardiac Tzar, Sir Roger Boyle, was sufficiently angered by their claims to respond with withering criticism: “AMI is a medical emergency: patients can’t choose where to have their heart attack or where to be treated!” It is “bizarre to choose a condition where choice by consumer can have virtually no effect”. Patients suffering “severe pain in emergencies clouded by strong analgesia don’t make choices. It’s the ambulance driver who follows the protocol and drives to the nearest heart attack centre”.
The intervention that the authors claimed reduced heart attacks and was a proxy for competition was patient choice. In 2006, patients were given choices of hospitals including private for-profit providers for some selected treatments. Less than the half patients surveyed in 2008 even remember being given a choice, and only a tiny proportion made those choices based on data from the NHS choices website. If patient choice was one of the two key elements of competition, it wasn’t prevalent and rather than being derived from the authors’ data, it was assumed.
Crucially, even if patient choice had occurred it does not explain why heart attack mortality rates fell. There is no biological mechanism to explain why having a choice of providers for elective hip and knee operations surgery (including hospitals which did not treat or admit acute MI patients) could affect the overall outcomes from acute myocardial infarction where patients do not exercise choice over where they are treated.
The problem of data dredging is well known; if you repeat an analysis often enough significant statistical associations will appear. But the authors make the cardinal error of not understanding their data and of confusing minor statistical associations with causation. Deaths from acute MI are not a measure of quality of hospital care, rather a measure of access to and quality of cardiology care. At best, what the paper appears to show is not the effect of choice on heart attacks but that if an individual has a heart attack in an area close to a hospital and their GP is near the hospital, then outcomes are better, but such findings are not new.
Going for their central criticism, in the same article, they explained:
The drip feed of pro-competition studies from Zack Cooper at LSE raises serious questions for the academic community and the public about what constitutes bad science and what to do about its politicisation. Recently, on 21 February in the columns of the FT, Cooper and colleague Julian Le Grand warded off serious scientific criticisms of the studies with an ad hominem attack, categorising those in favour of competition as empiricists and those whose work is critical of markets in health care as intuitivists. In so doing they sweep aside decades of careful economic theory and evidence which shows why markets do not work in health services and distract the reader from the facts that their work is ungrounded and far from empirical. Their repeated claims that competition in the NHS saves lives and improves quality and productivity have no scientific basis.
A litigation factory?
Of course the £3bn Health and Social Care Act (2012) which have no mechanisms of helping with clinical staffing or patient safety, in the drive for business efficiencies, have become a bonanza for private companies to which work has been outsourced, and a boon for the commercial and corporate law firms which are now nurturing them. The NHS of course has trouble in meeting the formidable legal bill against the private providers, as well as staff it has made redundant due to this top-down reorganisation.
I have long argued that the commissioning (‘competition and choice’) process through section 75 Health and Social Care Act (2012) would soon turn sour, for example in the original blogpost I did for the Socialist Health Association in January 2013 here. Crispin Dowler recently reported early tensions on 11 September 2013 in the Health Services Journal:
A number of private providers are likely to take complaints to the NHS’s new competition regulator Monitor over the next three years, the chief executive officer of Ramsay Health Care UK warned last week.
Jill Watts, whose organisation was ranked the largest private provider of NHS funded acute care in the most recent study by market analysts Laing and Buisson, said she could “almost guarantee” there would be challenges to come.
She told a Westminster Health Forum conference that the April switchover to clinical commissioning groups under the government’s health reforms had not produced uniform changes in commissioners’ attitudes to the private sector.
“In one part of the country, where we had almost adversarial relationships and they didn’t want to use us at all, they’re very keen to work with us now,” she said.
The New Labour Legacy, competition, performance and “the target culture”
Competition was intimately wound up in the target-driven agenda. NHS hospitals would have to meet targets to jump through regulatory hoops to become NHS Foundation Trusts. As long as finances stacked up, patient safety appears to have suffered in some Trusts under Labour’s watch. Whilst the evidence for competition being beneficial in the NHS market is weak, it has remained with us in policy like a bad smell. Julian LeGrand could have not put better how idiotic this policy really was.
The problem is indeed partly money – a historical legacy of underspending in all areas of public services. But, as John Hutton says, it isn’t only that. There is also a legacy of poor performance: of failing to use what resources there are effectively and efficiently. This is a lesson that six years in power have taught New Labour. The Government has tried and is trying a wide variety of techniques to lever up performance: publishing league tables on comparative performance, encouraging private sector involvement, offering independence to high fliers, stimulating competition and choice. But one of its favourite instruments has been targetry: the setting of targets with heavy penalties for failing to meet them. Many in government are convinced that this is the way to go.
Lessons need to be learnt for the NHS from failure of competition in imperfect markets
 There are two ways of trying to understand the human body in medicine. One is to understand its anatomy and physiology in normal health, which gives you a definition of its structure and functions. Another approach is to understand what goes wrong in pathology and why. Both approaches give valid complementary information. The problem with singing the praises of the market is that it assumes that there is ‘perfect competition’, and that the relationship between supply and demand can be predicted accurately. There are very many reasons why markets do not obey this perfect competition. In fact, perfect competition is virtually unheard of. Many of us believe that the NHS does not meet the definition of a market anyway, but my article here is to try to explain to health policy works, many of whom are quasi-economists, how the failures of competition are patently clear in the current investigation of this market by the Competition Commission.
There are two ways of trying to understand the human body in medicine. One is to understand its anatomy and physiology in normal health, which gives you a definition of its structure and functions. Another approach is to understand what goes wrong in pathology and why. Both approaches give valid complementary information. The problem with singing the praises of the market is that it assumes that there is ‘perfect competition’, and that the relationship between supply and demand can be predicted accurately. There are very many reasons why markets do not obey this perfect competition. In fact, perfect competition is virtually unheard of. Many of us believe that the NHS does not meet the definition of a market anyway, but my article here is to try to explain to health policy works, many of whom are quasi-economists, how the failures of competition are patently clear in the current investigation of this market by the Competition Commission.
There are two highly influential ideas which have been applied in the NHS. One is from Professor Michael Porter and his “five forces of competition”, which provides a useful construct about how competitive factors interact in the market to determine a company’s competitive advantage. (Porter also has another strong theme called ‘strategy and society’, which is more to do with corporate social responsibility, which many believe to be the substrate of Ed Miliband’s ‘responsible capitalism’ theme). The second idea is that of “disruptive innovation”, also from Harvard Business School, first advanced by Professor Clayton Christensen.
The “Five Forces” model of competition assumes that there are five important forces that determine competitive power in a business situation.
These are:
- Supplier power: How easy it is for suppliers to drive up prices? This is driven by the number of suppliers of each key input, the uniqueness of their product or service, their strength and control over you, the cost of switching from one to another, and so on. The fewer the supplier choices you have, and the more you need suppliers’ help, the more powerful your suppliers are.
- Buyer power: How easy it is for buyers to drive prices down? Again, this is driven by the number of buyers, the importance of each individual buyer to your business, the cost to them of switching from your products and services to those of someone else, and so on. If you deal with few, powerful buyers, then they are often able to dictate terms to you.
- Competitive rivalry: The number and capability of your competitors are important here. If you have many competitors, and they offer equally attractive products and services, then buyers will go elsewhere if they don’t get a good deal from the supplier. On the other hand, if a supplier produces an offering no-one else can do, that supplier will have considerable ‘competitive power’.
- Threat of substitution: This is affected by the ability of your competitors to find a different way of doing what you do – hence the growing importance of innovation in English health care policy. If substitution is easy and substitution is viable, then this weakens your power.
- Threat of new entry: Power is also affected by the ability of people to enter your market. If it costs little in time or money to enter your market and compete effectively, if there are few economies of scale in place, or if you have little protection for your key technologies, then new competitors can quickly enter your market and weaken your position. If you have strong and durable barriers to entry, then you can preserve a favorable position and take fair advantage of it. Monitor has of course been very keen to lower the barriers-to-entry so that ‘any qualified provider’ can compete with the NHS for contracts.
The Competition Commission ‘Issues Statement’ from February 2013 adopts the structural analysis of Porter, without saying so. The privately-funded healthcare sector is a relatively small part of the wider UK healthcare sector, most of which is funded via each nation’s respective public health- care systems. Certain treatments, including elective cosmetic surgery and standard maternity treatments, were not included. The five largest hospital operators account for approximately 70 per cent of privately- funded healthcare revenues in the UK.Almost 80 per cent of UK patients using privately-funded healthcare services are funded by insurance. The other 20 per cent are ‘self-pay’ patients. These healthcare services are also used by overseas patients, particularly in London. The four largest private medical insurers account for approximately 87 per cent of insurance premium revenue with the two largest alone accounting for 65 per cent.
A key issue for this investigation is the way in which the privately-funded healthcare sector is affected by the conduct of, and interaction with, the private medical insurers (PMIs).Defining the market in itself is difficult. Local aspects may arise because patients may prefer not to travel far to hospitals or because there may be limits on patients’ ability to travel (eg limited geographic coverage by the insurer or GPs referring primarily to local consultants). On the other hand, patients may be willing to travel different distances depending on the type of treatment (eg patients may be willing to travel further for treatments for more serious conditions). There also seems to be differences in the type of ‘product’ being offered; for example, oncology (cancer management) is offered by a lower proportion of general private hospitals.
The analysis nicely falls into the factors described by Porter, as follows:
Supplier power:
Many PMIs expressed concerns that HCA hospitals in London have market power. There are a substantial number of private hospitals in London, and London private hospitals differ from those in the rest of the UK in that they offer different sets of specialties, some hospitals are very specialised and their patients may work in London but reside further away. Their analysis identified some ‘hospitals of potential concern’ in London but it may not fully capture the extent of any competition problems in London. Consultant market power may be caused by several factors, some specific to the location in which the consultant works and others reflecting the way in which privately-funded healthcare services are purchased.
These factors include:
(a) a limited number of consultants in a particular local area for specific treatments or specialties;
(b) the way that referrals are made and consultants selected; we note that the pro- cess of choosing anaesthetists for a patient differs from that for other consultants and typically involves less input from the patient and/or GP; and
(c) joint setting of prices by some consultant groups.Buyer power:
This theory of harm hypothesises that insurers may possess buyer power in relation to consultants.The Competition Commission have stated that if insurers are suppressing consultant fees to a level below those which would prevail in a competitive market, this could lead to a reduction in the quality of service provided by consultants to patients and affect the incentives to innovate. They also considered that insurer conduct may distort competition between consultants when caps on the reimbursement of fees are applied to some consultants (eg newer or junior consultants) and not to others (eg more experienced ones).
Threat of substitution:
There are real problems with the substitution arguments. Private hospitals may be able to change the treatments they supply if they supply a range of different treatments and may be able quickly to change how they operate. Supply-side substitution by consultants is likely to be more limited than supply-side substitution by private hospitals. In the absence of demand-side substitution, treatments (or specialties) that should be defined as separate markets may be aggregated into clusters of treatments (or specialties).
Threat of new entry:
These are complicated. For example, one source of a ‘barriers to entry’ could be that of customers into privately-funded healthcare resulting from bargaining between insurers and hospital chains. This theory of harm hypothesises that bargaining between PMIs and hospital chains creates barriers to new local entrants. In particular, it may result in contractual terms that disincentivize PMIs from recognizing new entrants. This bargaining pattern may lead to a hospital operator placing pressure on PMIs to continue to recognize all the hospital operator’s hospitals and not to recognize hospitals of new entrants. High fixed costs of hospitals make it attractive for hospital groups to offer ‘volume for discount’ deals to PMIs, if by doing so they can secure business from the insurer that they would not otherwise receive.
However, the Porter analysis is notorious for its poor comprehension of anti-trust of anti-competitive regulation across a number of jurisdictions. That’s why the Competition Commission is unable to address competitive rivalry at all – this is still extremely disappointing for a statutory legal authority for the regulation of competition, and provides for ultimately a weak, incomplete analysis whatever is finally returned. The analysis is traditionally attacked from the perspective that the conclusions from Porter’s analysis, originally achieved from the automobile industry, do not easily extrapolate. Whilst there have been attempts at applying Porter to the internet or telecoms in general, there is a real paucity of data looking at the application of Porter either in private healthcare markets. Therefore, one can only be immensely frightened to consider how such an analysis can be properly applied to the NHS, which can described as a ‘hybrid market’ at best (avoiding the flawed term ‘quasimarket’); it is beyond the scope of this article to consider how it may not be possible to consider the current NHS as an example of market socialism.
The political lesson here is that privatisation of the utilities under the Conservative governments has been an unmitigated disaster from the perspective of the UK citizen. From the viewpoint of a company director or shareholder in a privatised utility, it is of course a ‘cash cow’ as there is no competitive rivalry. The competition authorities have immense difficulty in regulating this market, such that prices continue to go up under the pretense of ‘returning investment’ to the infrastructure. This argument cannot be easily applied to the NHS, as the Health and Social Care Act (2012) has totally demolished the ‘national’ nature of the NHS, delivering a highly fragmented service which is beginning to bear a resemblance to the disasters of the privatised railways industry in England.
The biggest problem with the fact that the new NHS is not a real ‘market’ is that in an oligopoly, a market with few players, the participants can easily bump up prices when they are not really competing with each other anyway. They either are offering the same product at the same inflated price (e.g. a ‘standard hernia operation’), or they can easily cherrypick what services they wish to provide at high volume and low cost to maximise their shareholder profitability. As the Secretary of State no longer has a duty for the NHS to offer a universal national health service, this is no longer an issue legally.
We can argue until the cows come home about the efficacy of the current political coalition in the UK, but the problems of ‘forming coalitions’ is well known in the legal academic press and increasingly so in the business press. For example, in an excellent paper called “Michael Porter’s Missing Chapter: The Risk of Antitrust Violations” from Fried and Oviatt in February 1989, the authors describe that:
“Porter also proposes forming coalitions to raise entry barriers, although he does not provide any detail or exam- ples of what he means. Statutory prohibitions on conspiracies and combinations show that antitrustlaw takes a dim view of coalitions formed to raise entry barriers unnecessarily. In addition to the cases previously discussed involving coalitions, organizations (sic) in many industries have attempted to form “associations” for the purpose of limiting competi- tion in a trade by limiting access to suppliers. Diamond dealers, kosher butchers, and golf club manufacturers have all been ordered at one time or another to stop this behavior. Much more prominent is a Supreme Court case that dealt with the garment industry.^s Fashion Originator’s Guild of America, Inc, (EOGA) was an association of designs, manufacturers, and distributors of women’s clothes. The manufarturers in FOGA controlled over 60% of the high- price segment of the market, FOGA members were upset because after original clothes designed by FOGA members entered the retail market, competitors would copy the designs and sell identical garments. To combat this “style piracy” guild members refused to sell to any retailer who sold copied fashions. The Court ruled that in so doing FOGA was in violation of antitrust laws.”
One suspects that if the UK competition authorities, such as Monitor, OFT and Competition Commission, fails to regulate properly even the private healthcare market, they are going to have a pretty disastrous time with the NHS at general. But the people who wished to introduce the market in the NHS in the first place should have thought about. None of us, as such, voted for it.
Monitor has much work to do to produce a cogent analysis of pricing in healthcare
Monitor is in its infancy, but, pardon the pun, I would like to describe an example of childbirth to explain the mountain of problems that the new privatised NHS is yet to experience. Consider this a steep learning-curve that not many of us voted for at the last election.
“The new NHS provider licence: consultation document” was issued by Monitor on 31 July 2012 with a deadline for responses determined as 23 October 2012. According to section 5.1 of this Document on pricing,
“One of Monitor’s new functions will be to set prices for health care services funded by the NHS.Accurate pricing is essential to ensure that providers are paid appropriately for services they provide to patients. Accurate pricing information helps GPs, commissioners and providers to plan and budget for health care services to meet people’s needs. Pricing can also be used to encourage providers to improve the quality of services for patients, and to increase the efficiency with which services are provided. If providers are not properly reimbursed, this can reduce the quality and efficiency of care they offer and may, in some circumstances, threaten the sustainability of their services.”
Pricing is pivotal in markets, and will obviously therefore be expected to the subject of considerable scrutiny by competition regulatory authorities. In future, Monitor will be responsible, in partnership with the NHS Commissioning Board, for setting prices for NHS services.Indeed, according to a statement produced on 20 June 2012,
“The Health and Social Care Act 2012 makes changes to the way health care is regulated in order to strengthen the way patients’ interests are promoted and protected. Monitor’s role will change significantly as we take on a number of new responsibilities. We will become the sector regulator for health care, which means that we will regulate all providers of NHS-funded services in England, except those that are exempt under secondary legislation.”
Take for example the cost to the taxpayer of a provider delivering a baby – not the antenatal or postnatal packages, but the cost of the actual labour and peri-partum process (“the package”). Like any other “product” in the market, a supplier will have to price its product carefully, to ensure that it offers a competitive price, but especially to ensure it does not price itself out of the market by being too costly. The price of “the package” might be determined through a number of different ways.
- Premium pricing (also called prestige pricing) is the strategy of consistently pricing at, or near, the high end of the possible price range to help attract status-conscious consumers. People might buy a premium priced product because they believe the high price is an indication of good quality.
- Cost-plus pricing is the simplest pricing method. The firm calculates the cost of producing the product and adds on a percentage (profit) to that price to give the selling price. This method although simple has two flaws; it takes no account of demand and there is no way of determining if potential customers will purchase the product at the calculated price. You only need to consider the complexity of doing the calculation for the package”, e.g. will the provider use cheap epipdural needs for the anaesthesia, will a foundation year doctor (who is cheaper) perform most of the medicine compared to a specialist registrar (who is more expensive, but more experienced, especially in dealing with medical emergencies).
- Value-based pricing – a price based on the value the product has for the customer and not on its costs of production or any other factor.. The relevant issue is how much would you be prepared to have provider A deliver your baby? This is a subjective issue, not easy to predict.
The problem with premium pricing is that providers can collude lawfully to set their prices as high as possible between them. Price fixing is illegal under Article 101 TFEU of the European Union:
Article 101
(ex Article 81 TEC)
1. The following shall be prohibited as incompatible with the internal market: all agreements between undertakings, decisions by associations of undertakings and concerted practices which may affect trade between Member States and which have as their object or effect the prevention, restriction or distortion of competition within the internal market, and in particular those which:
(a) directly or indirectly fix purchase or selling prices or any other trading conditions;
(b) limit or control production, markets, technical development, or investment;
(c) share markets or sources of supply;
(d) apply dissimilar conditions to equivalent transactions with other trading parties, thereby placing them at a competitive disadvantage;
(e) make the conclusion of contracts subject to acceptance by the other parties of supplementary obligations which, by their nature or according to commercial usage, have no connection with the subject of such contracts.
2. Any agreements or decisions prohibited pursuant to this Article shall be automatically void.
3. The provisions of paragraph 1 may, however, be declared inapplicable in the case of:
– any agreement or category of agreements between undertakings,
– any decision or category of decisions by associations of undertakings,
– any concerted practice or category of concerted practices,
which contributes to improving the production or distribution of goods or to promoting technical or economic progress, while allowing consumers a fair share of the resulting benefit, and which does not:
(a) impose on the undertakings concerned restrictions which are not indispensable to the attainment of these objectives;
(b) afford such undertakings the possibility of eliminating competition in respect of a substantial part of the products in question.
It has been incredibly hard to prove price-fixing, but numerous examples exist.
For example, the Daily Mail recently reported price-fixing at the petrol pumps:
“Motorists are being ripped off by profiteering oil companies and speculators, MPs suggested yesterday.They demanded an inquiry into allegations of price-fixing at the pumps, and called for the Government to replace its planned fuel duty rise with a windfall tax on oil company profits.
And last year they reported on the price-fixing of milk:
“Supermarkets and dairy firms have been fined almost £50million over price rigging on milk and cheese that cost families £270million. The collusion put up the price of milk by 2p a litre – 1.2p a pint – and added 10p to the cost of a 500g block of cheese. The punishment was announced by the Office of Fair Trading, following an investigation triggered by whistle blowers at the Arla dairy company. First revealed by the OFT in 2007, the ‘Great Milk Robbery’ took place in 2002 and 2003. But only now has a fine of £49.51million been handed down.”
For Monitor, regulating this will be a mammoth task. Private health providers have much scope for setting between them the most profitable way of delivering the patient’s baby, and it is a great market to be in: the country will never be short of a need for providers of safe deliveries of babies. Whilst other metrics might be important to the clinician, such as mortality or morbidity (infection rates), it could be that private providers are distinguished most themselves by the least cost to a GP practice. Or, it could be that people are genuinely fickle about not caring about who picks up the tab, but the preferred private provider might provide “extra frills”, like en-suite TV with 80 channels.
The problematic issue is what happens if an unconventional problem comes out-of-the-blue. The mother might experience a rare type of headache, such as trigeminal autonomic neuralgia, and there is effectively no “patient choice” involved, save for the GP having to refer the patient to a specialist unit like Great Ormond Street Hospital. You will notice here that the quality of patient choice is nothing to do with the innovation of the private health provider, nor indeed how “competitive” the market of private providers of childbirth is: it is entirely to do with the skill of the clinician in making a rare diagnosis, and having the astuteness of having a specialist unit such as Great Ormond Street Hospital deal with it safely, whatever the cost. You must note that I give this example of TAN at GOSH completely at random, and any similarity to a real-life scenario is of course completely unintentional.