Home » Posts tagged 'whole person care' (Page 2)
Tag Archives: whole person care
Care at the crossroads. Burnham has something big, and you may be quite pleased to see him
Social care funding is on its knees.
Andy Burnham MP, Shadow Secretary of State for Health, addressed a sympathetic audience at the #NHSConfed2014 yesterday, talking about unlocking resources for general medicine.
We live in crazy times. Newark saw the christening of the Conservative Party as the protest party you should vote if you wanted to STOP UKIP. But let me take you back to an era when the Labour Party had principles (!) In August 1945, Aneurin Bevan was made Minster for Health following the 1945 General Election. The National Health Service (NHS) was one of the major achievements of Clement Attlee’s Labour government. By July 1948, Minister for Health, Aneurin Bevan had helped guide the National Health Service Act through Parliament.
A full day has been allocated to the Opposition health on Monday in parliament in part of their discussions on her Majesty’s Gracious Speech. Simon Stevens – NHS England’s new chief – has asked for solutions for well rehearsed issues, and Andy Burnham is clear that this is no time for another apprentice like Jeremy Hunt. Whilst being upbeat about the future of the health and social care system, he wants to move away from a “malnourished system”, with carers employed on zero hours contracts and less than the minimum wage. Indeed, this is a serious issue which has caused me some considerably anxiety too. A “product of [my] time in Government”, clearly this framework has also benefited from a parliamentary term in opposition.
Burnham crucially identifies not an inefficiency in which money is spent (although the ongoing Nicholson savings rumble on). But he does identify an inefficiency in outcomes (such as the near-inevitable fractured neck of the femur in the leg for a seemingly-trivial cost-saving in not purchasing a grab handrail). Labour, inevitably, though has an uphill battle now. The system appears to encourage the medical model of care, according to Burnham, encourages hospitalisation of people, so it is not simply a question of throwing money at the service. People are more than aware that an ‘unsustainable NHS’ is in a nutshell code for a NHS starved of adequate fundings.
Burnham feels that you can’t half-believe in ‘integration’, and is mollified about the consensus about a need for integration across all main political parties.
“I am really worried that the ‘Better Care Fund‘ might give integration a bad name”, comments Burnham.
People who have watching Burnham’s comments will note how Burnham has openly commented how he feels he has been misled by certain think-tanks in the past. A period of opposition has enabled Burnham conversely to obtain a crisis of insight. And yet he talks about his “precious moment” in order “to build a consensus of shared endeavour, which I intend to use to the full and very carefully.” Intriguingly, he does not wish to ‘foist a grand plan’ on voters after the next general election. This is of course is political speak for his ‘shared agenda’, driving a cultural change by stakeholders within the system. This is precisely what Burnham feels he has achieved through the commission on whole person care by Sir John Oldham.
“Not a medical or a treatment model, but a truly preventative service, that can at last aspire to give people a state of physical, mental and social wellbeing.”
Burnham wants to put a stop to the ‘random set of disconnected meetings with individuals within the service.’
An exercise was carried out at the start of the NHS.
This is the famous leaflet.
Burnham desires a new leaflet from an incoming Labour government to introduce how social care can become under the umbrella of the National Health Service.
“Going forward, you should expect to receive much more support in your home. The NHS will work to assemble one team to look after you covering all the needs you have. We want to build a personal solution that works for you, for your family, and for your carers, because if we get right at the very outset and the very beginning it’s more likely to work for you and give you what you want, and cost us all much less. We want you to have one point of contact for the co-ordination of your care. We know you are fed up with telling the same story to everyone who comes through the door. It’s frustrating for you, and wasteful for us. To get the care that you’re entitled to, when and where you want it, you will have powerful new rights set out in the NHS Constitution such as the right to a single point of contact for the coordination of all of your care and a personalised care plan that you have signed off. But – and there is a big but – to make of all this happen, you will changes in your local NHS, and, in particular, you will changes in your local hospital. We can do a better job of supporting you where you want to be, we won’t need to carry out as much treatment in hospitals, or have as many hospital beds. It is only by allowing the NHS to make this kind of change to move from hospital to home that we will all secure it for the rest of this century.”
Burnham feels that the NHS must be the ‘preferred provider’ and the DGH should be allowed to reinvent itself - building the notion of one team around the person. I personally have formed the opinion: “close smaller hospitals at haste, and repent at leisure“. Critics of marketisation will inevitably point out the blindingly obvious: that even with a NHS preferred provider, there’s still a market, and nothing short of abolition of the purchaser-provider split will remedy the faultlines. There could be a one person tariff or one person budget for a person for a year. It would give an acute trust a much more stable platform, according to Burnham, in contradistinction to the activity based tariff. This does require some rejigging of how we have the proper financial performance management system in place: there should be a drive, I feel, for rewarding behaviours in the system that promote good health rather than rewarding disproportionately the work necessary to deal with failures of good control, such as dialysis, amputations or laser treatment.
Burnham is clearly inspired by the ‘Future Hospitals’ soundings from the Royal Colleges of Physicians, focused on a new generation of generalist doctors working across boundaries of primary and secondary care:
“Since its inception, the NHS has had to adapt to reconcile the changing needs of patients with advances in medical science. Change and the evolution of services is the backbone of the NHS. Hospitals need to meet the requirements of their local population, while providing specialised services to a much larger geographical catchment area.”
Burnham even talks about possibly reviewing the “independent contractor” status of GPs.
Centralised care is mooted for people in life threatening situations. But Burnham has found that barriers to service reconfiguration exist through the current competition régime and market, with integration encouraging in contrast to collaboration, people before profit, and merge “without the nonsense of competition lawyers looking over their shoulders”. Therefore, Burnham repeats his pledge to remove the Health and Social Care Act (2012), which has driven “fragmentation, complexity and greater cost”. Under this construct, section 75 and its associated Regulations is disabling rather than enabling for health policy. There is clearly much work to be done here to make the legislation fit for purpose, as indeed I have discussed previously. Wider dangers are at play, as Burnham well knows, however. Here he is speaking about his opposition to TTIP (the EU-US Free Trade Treaty) which the BBC News did not seed fit to cover despite their Charter requirements for public broadcasting. And here is George Eaton writing about his opposition to TTIP in the New Statesman.
Burnham is clearly, to me, positioning himself to the left, distancing himself from previous Labour administrations. There are clearly budgets in the system somewhere, and while Burnham talks about unified budgets he does not put the emphasis on personal budgets. There is no doubt to me that personal budgets can never be ‘compulsory’, and each person group (e.g. people living with dementia) presents with unique challenges. It’s clear to me that deep down Andy Burnham is still in principle keen on something like the ‘National Care Service’, in preference to any gimmicks from the Cabinet Office. Burnham in the Q/A session with Anita Anand indeed describes how this had been thrown into the long grass at the time of Labour losing the general election in 2010, but how paying for social care in 2014 is as fundamentally unfair as paying for medicine had been pre-NHS according to Burnham. This would take some time to put in place, such as a mechanism for a mandatory insurance system, and a proper care coordinator infrastructure. And these are not without their own controversies. But, with Miliband playing safe one unintended consequence for neoliberal fanatics has been that it has not been possible to impose a strong neoliberal thrust to whole person care; and whatever Miliband’s personal preferences, the pendulum to me is definitely swinging to the left. Burnham talks specifically about a well planned social care system as part of the NHS.
And so Burnham looks genuinely burnt by previous administrations, and, whilst certain key players will want personal budgets and competition to be playing a greater part in policy, it appears to me that the current mood music is for Labour not appearing to promote privatisation of the NHS in any form. The ultimate success of the next Labour administration will be determined by the clout of the Chancellor of Exchequer, whoever that is. It could yet be Ed Balls. For matters such as ‘purse strings’ on the social impact value bond or the private finance initiative, Burnham may have to slog out painful issues with Balls in the way that Aneurin Bevan once did with Ernie Bevin in a previous Labour existence. Burnham’s problem is ensuring continuity with the current system where services have been proactively pimped out to the private sector, but ultimately it is the general public who call the shots. Burnham knows he’s onto something big, and, for once, some people may be quite pleased to see him.
Thanks to Andy Burnham for emphasising “care co-ordinators” which I feel are pivotal to living well with dementia
This morning I had a present for Andy Burnham MP (@andyburnhammp), about to lead the Labour troops into battle for the European elections. The present is of course a copy of my book ‘Living well with dementia’, which is an account of the importance of personhood and the environment for a person living with dementia.
In my article entitled “Living well = greater wellbeing” for the ETHOS Journal (@ETHOSJournal), I highlighted the critical importance of the ‘care coordinator':
“So, if one had unlimited funds, what sort of service could be designed to provide care and support for people with dementia? In my opinion, the answer is a very different one. Ideally, all services, which could include healthcare, housing and legal systems, would adapt quickly and flexibly according to the needs of the individual living with dementia. This would need to be managed by a named, long-term co-ordinator of care and support.”
In reply to my article, Paul Burstow MP commented helpfully:
“The idea of a care navigator able to call on and coordinate all available health and social care, as well as housing support and voluntary sector provision is a persuasive one. It is something that the Richmond Group of charities, among others, have for a long time called for – and it is something I would like to see the Liberal Democrats deliver in the next government. Better managed and coordinated care would be a huge step forward and could make all the difference to dementia sufferers and their often strained carers.”
And Andy gave it much prominence this morning:
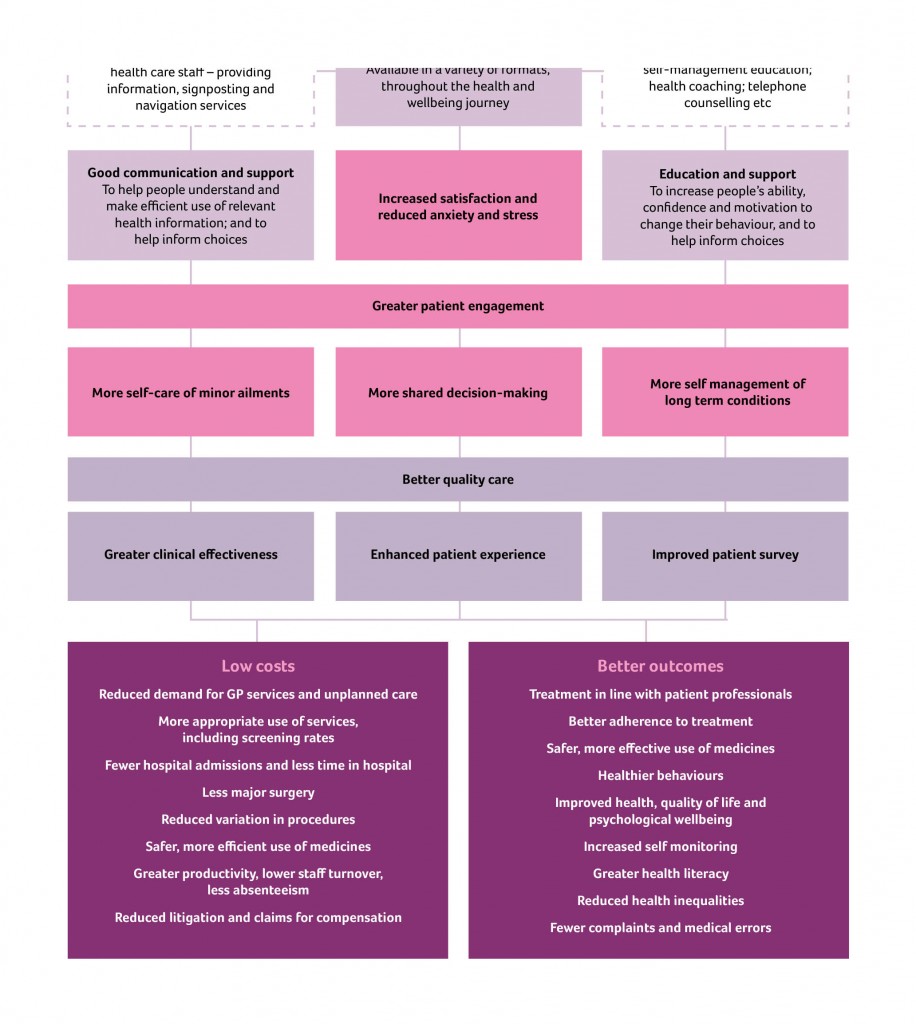
The King’s Fund (@TheKingsFund) has previously looked into co-ordinated care for chronic conditions.
In this framework, a “care co-ordinator” acts as a single point of contact and works with the patient, their carer(s) and the multidisciplinary team to develop a care plan.
Once this has been agreed, the co-ordinators work with the team, the patient, the patient’s family and other care providers to deliver co-ordinated and coherent care. Personal continuity of care is actively encouraged, and the care teams work hard to ensure an immediate response to care needs as they arise.
The care co-ordinator becomes he patient’s advocate in navigating across multiple services and settings ??providing care directly in the home environment.
He or she also ??communicates with the wider network of providers (outside of the core multidisciplinary team) so that information about the patient/carer is shared and any actions required are followed up.
The King’s Fund has previously found that the type of person undertaking the care co-ordination function varied greatly.
Most care co-ordinators had been community or specialist nurses, yet the role has also been taken on by non-clinical ‘link workers’ (in Sandwell) and health and social care co-ordinators (in Torbay).
There also appears to be a continuum from the non-clinical approach – primarily providing personal continuity to service users and acting as their advocate to ensure that care is co-ordinated around their needs – to the clinical approach, in which a case manager would also be able to provide clinical care directly.
This, I feel, is significant, as my book ‘Living well with dementia’ has a very non-medical thrust.
It’s very much a n0n-authoritarian, non-hierarchical approach where each person, including the person living with dementia, has an important part to play.
Influences on someone living well with dementia might include design of a home or ward, assistive technologies, ambient-assisted living, “dementia friendly communities”, for example.
With the introduction of ‘whole person care’, it’s possible that the care co-ordinator for a person living well with dementia might become a reality.
In this construct, Andy Burnham MP, Shadow Secretary of State for Health, is trying to stop the overhospitalisation (and overmedicalisation) of people.
Labour can make political weather on the NHS, but it shouldn’t be thrown off track by gale force winds
Political decisions will always be made, but are unlikely to be representative if certain people don’t wish to be part of the political process.
It is hard to know what has caused a decline in political engagement, but politicians not appearing to listen might be a major factor. The social media has empowered a plurality of opinions, which means that it is less easy for politicians to speak with a collective voice on issues. The traditional narrative is that people ultimately care about the economy, as economic competence is the sort of issue which can make or break political parties. However, it’s very likely that residents of Lewisham care about local hospital closures, and hospital campaigns can gain momentum and traction whatever the state of national politics.
Voices of Labour who are interested in social justice, solidarity, equality, equity, solidarity or cooperation are not in fact in a minority, whatever the current state of the Blairite arm of the political party. While think tanks prioritise concepts such as ‘accountability’ and ‘co-production’, authentic voices on the left do not feel that their brand of politics is irrelevant. The question inevitably arises – if the current party is doing what you want to do, why should you stand for election? It is possibly the case that many people will nonetheless vote for Labour, despite reservations on the ‘welfare cap’, because the modern political system does not offer them any realistic choice. ATOS were contracted to do welfare benefits in the last government, and it is likely that some other outsourcing company will assume the mantle.
Labour clearly will state that it is insufficient for political parties to lose elections for others to win them, and they should formulate coherent policies of their own. But likewise nobody will expect Ed Miliband to reveal his hand until much closer to the election. Many people do not come into contact with the NHS when young, although there are many who do, and it is possible that Labour will wish to hone its offering on general health issues as well as the National Health Service. The recent Clegg v Farage debates have highlighted some appetite for single issue politics, when charismatically explored in ‘leaders debates’.
The forthcoming European elections will give a good indicator as to the relevance of the NHS to people’s lives, arguably. The fate of Louise Irvine and Rufus Hound will possibly provide good clues as to whether people in the general public care as much about the NHS as much as NHS campaigners clearly do. The National Health Action Party – NHAP – to be national will need to have coverage throughout the country, but there has always been concern about whether they might realistically gain enough seats to prevent Labour from winning an overall majority. Nonetheless, this Party feels serious that the NHS is a major political issue, and it is a genuine policy issue what they feel they can achieve over and above what a Labour government might. It is possible that that the NHAP might prevent a Labour MP from being elected in Stafford. I met someone recently who was adamant that, with the right resources, NHAP could win in Stafford. Likewise, it’s possible that Clive Peedell could win against David Cameron in Witney, where arguably Labour do not have a realistic chance of winning.
With the second rabbit to come out of George Osborne’s hat in the form of pension reforms, the first being inheritance tax, it’s possible that Labour can’t take the running of the economy as a vote winner in the 2015 general election. Some people still blame Ed Balls as too intimately implicated in the economic policy of the last administration. It is therefore counterintuitive to imagine then that Labour will wish to ignore its potential strengths such as social justice. Despite the concerns over ISTCs and PFI in previous Labour government, and the events running to Mid Staffs, it is still controversial whether people feel strongly enough about Labour’s record not to vote for them. Even hardened Socialists might be keen to contribute to the election of a Labour government than to see the continuation of a Conservative one.
The £2.4 bn top down reorganisation resulting from the Health and Social Care Act (2012) is a major faultline in national policy. Most seasoned pundits are aware of the calamitous effects of competition on national policy, but it is far more likely that members of the general public are unconcerned about ‘section 75′. As sure as night follows day, it’s likely that Labour will oppose privatisation, but the logical conclusion of this is that it supports state ownership. Its inability to call for this publicly speaks volumes. And the people who argue that this country is fundamentally right-wing know they’re being economical with the truth. Unpopular policies from the right have included the astronomic pay of certain investment bankers, the cost of energy bills, the general failures of privatisation policies, perceived attacks on the welfare state, and an enthusiasm to introduce tuition fees in universities denying access-to-education. Whilst Labour is unlikely to voice loudly that ‘capitalism kills’, Labour potentially can make some political weather on the NHS and on health issues such as ‘whole person care’. This will require some strength in the leadership of the Labour Party, but it should not be thrown off course by the equivalent of gale-force winds.
Living well with dementia and the #Oldham review of whole person care
There were of course huge structural problems in the much heralded Oldham report on whole person care was published this week.
It’s officially called ‘One Person, One Team, One System‘.
These structural problems are, not least, to what extent will the NHS be paid for out of general taxation in the long term. The issue is not fudged altogether, in that Oldham calls for a future government to look into this as a priority.
Nonetheless, the Oldham Commission does fudge the issue of how much integrated and social care systems can rely on private not state provision. This is a strange ‘elephant in the room’, given the emphasis of the report on individualised budgets (call them what you will, personal budgets or personal care budgets).
Oldham does however concede helpfully that ‘financial arrangements in the adult social care system are equally fragmented, with complex and overlapping funding and provision arrangements between private and public funding sources, and private and public providers of care. The multitude of private care providers adds to this complexity.’
The need to repeal section 75 Health and Social Care Act is pivotal to all this. In fact, a repeal of the whole Act, as Labour (as Andy Burnham and Ed Miliband have indeed promised), would be helpful. This is, quite simply, because legally integration might offend the competition legal infrastructure established by section 75 and its associated Regulations, and of course sit uneasily with EU competition law.
At the moment, the NHS and social care services are geared up to ‘reacting to events’. And this is reflected in the payment by results mechanism (a reincarnation of ‘activity based costing’).
“Public funding has increasingly focused on those with greatest needs – particularly as rationing of care has become more severe – driven by a reactive, crises oriented approach rather than a focus on early intervention and wellbeing.”
Wellbeing is of course not just the opposite of illbeing, though lessons can be learnt from poor hydration and nutrition, for example, in individuals with advanced dementia.
The Oldham Commission view health and wellbeing boards as a vehicle for collective system leadership for whole person care,” involving the leaders of existing organisations working together to coordinate care and align incentives across their geography.” And therefore it is critically important that they are fluent in what wellbeing is, and how to promote it. This is especially important for dementia, but I would say that wouldn’t I.
Information is obviously vital in decision-making along a path to wellbeing however defined. I, in fact, devote a whole chapter to decision-making in my book ‘Living well with dementia’.
The exact mechanism of integration of voluntary organisations and health and care services to provide a combination of medical and non-medical support as part of the care pathway for older people living with multiple long term conditions needs of course to be put under greater scrutiny.
The ‘deal‘ between the Department of Health and the Alzheimer’s Society in promoting ‘Dementia Friends’ is of course welcome in promoting awareness of dementia. But we do need to be careful that, firstly, other dementia charities do not suffer in a ‘zero sum gain’ manner. Secondly, we need to be doubly sure that charities are not expected to pick up any shortfall in state provided services. Already there’s valid criticism of the way in which private companies can legitimately ‘cherry pick’ services to maximise their shareholder dividend.
Oldham’s group is right to refer to “a strong evidence base now exists to target key risks to health independence and wellbeing in old age.” Clearly there’s a balance to be struck between independence through assistive technologies perhaps of persons living with dementia in their own homes, and social inclusion with other persons face-to-face. Online communities offer great value for persons with dementia nonetheless.
Oldham’s team also helpfully reviews how Preventive aspects of whole person care must therefore pay attention to environmental factors. The emphasis in the Report is on diet, but this is valid too for dementias in the context of vascular dementias. Vascular dementias are common in older age groups, and certainly medical professionals, dieticians and others are keen at considering cholesterol and diet, and their interaction with other factor such as smoking.
Therefore, one of the conclusions is that, “Whole person care should not only include joining up services …”
It is inescapable that whole person care should include ‘joined up services’. Data sharing different disciplines, despite the concerns about #caredata, needs to involve a more effective dialogue with the general public, one expects.
The report also picks up on a number of other important issues.
One is the possible interaction with benefits. People with disabilities, for example, are right to wonder if benefits might be taken away if the system drives towards ‘whole person care’. On the other hand, it does not perhaps make intuitive sense for the care and benefits situation to work in isolation?
This is of course an intense political quagmire, given ATOS’ role in both the GP extraction scheme and the implementation of the much criticised disability and employment benefits.
Also, it turns out that 70% of people over 75 live with a major long term condition and a quarter live with two or more. Many persons living with dementia also live with otherconditions.
Furthermore, the Report notes that, “in all groups in society, housing has a large impact on people’s health and wellbeing.” As perhaps care embraces personhood in the true meaning of Kitwood or otherwise, the influences of other people in society, such as housing or the criminal justice system to name but a few, may become apparent.
But what the State is by that stage is anyone’s guess. In the meantime, the Oldham Report is fully consistent with my book ‘Living well with dementia’.
I had expected this to be the case. In fact, there’s a paragraph on whole person care in my book.
Can the English NHS enter a ‘period of calm’ if it wishes to introduce integrated care?
Sir David Nicholson, KCB, CBE, is Chief Executive of NHS England.
In 2010 Nicholson jokingly described NHS reform plans, the implementation of the Health and Social Care Act (2012), as the biggest change management programme in the world – the only one “so large that you can actually see it from space.”
Andy Burnham MP gave a speech to The King’s Fund on 24 January 2013, entitled “‘Whole-Person Care’ A One Nation approach to health and care for the 21st Century”.
And the Conservative Party, with Jeremy Hunt MP as Secretary of State for Health, have been eyeing up ‘integration‘ too.
So, like many areas of policy such as the private finance initiative, personal budgets or ‘efficiency savings’, there might be considerable consensus amongst the main political parties about implementing a further transformational change in the English NHS.
In that famous King’s Fund speech, Burnham comments, “Second, our fragile NHS has no capacity for further top-down reorganisation, having been ground down by the current round. I know that any changes must be delivered through the organisations and structures we inherit in 2015. ”
This is coupled with, “While we retain the organisations, we will repeal the Health and Social Care Act 2012 and the rules of the market.”
The Health and Social Care Act (2012) as a legislative instrument, whatever the political bluster, had three main legislative aims.
It aimed to implement competitive tendering in procurement as the default option, thus expediting transfer of resources from the public sector to the private sector; it beefed up the powers of the economic regulator (“Monitor”) for this “market”; and it produced a preliminary mechanism for the managed decline of financially unviable entities in the NHS.
Therefore repealing the Act can be argued as a necessary and proportionate move for taking out the ‘competition jet engines’ of the NHS “market”.
Experience from a number of jurisdictions provides that the legal challenges in allowing integration (and bundling) within the framework of competition law are formidable.
There is a clinical case for integrated care, in allowing more co-ordinated care of the person across various disciplines, for example medical, psychiatric or social, for both health and disease.
If community services are ‘wired up’ with hospital services, provided that community services are not starved of money at the same time as hospital services, there is a good rationale in that the health of certain people, followed closely in the community, might not freefall so badly that they require admission to a medical admissions unit.
There is also a financial argument that integrated or whole person care might work, but clearly no political party will wish to prioritise this ahead of quality of clinical care, particularly given the current tinderbox of cuts in medical and social care.
But whichever way you look at it, ‘whole person’ care involves a huge cultural change; this has repercussions for how all professions conduct themselves in their care, especially with regards to community care, and has consequences for training of staff in NHS England.
And it is impossible to think that, whichever political party ultimately becomes responsible for introducing a whole person or integrated care approach, it won’t cost money.
For example, setting up the infrastructure for data sharing, whether clinical or for the purposes of unified budgets, has a long history of being expensive.
Estimates of the cost of the reorganisation just gone are a bit confused, but they tend to range between £2.5 and £3 bn.
The risk of turbulence can be, to some extent, mitigated against by known people at the helm, such as Andy Burnham or Liz Kendall, but the last thing the general public will wish is another period of massive upheaval.
It can be argued that these changes are ‘a good idea’, and it’s only a question of explaining the benefits to the general public, but, following the Health and Social Care Act and caredata, the track record of this current Government is nothing to write home about.
Twitter: @legalaware
‘Whole person care’ needs a bit of tinkering and strong leadership
In a now very famous article, “The genius of a tinkerer: the secret of innovation is combining odds and ends”, Steve Johnson describes how innovation must be allowed to succeed in face of regulatory barriers.
“The premise that innovation prospers when ideas can serendipitously connect and recombine with other ideas may seem logical enough, but the strange fact is that a great deal of the past two centuries of legal and folk wisdom about innovation has pursued the exact opposite argument, building walls between ideas”
“Ironically, those walls have been erected with the explicit aim of encouraging innovation. They go by many names: intellectual property, trade secrets, proprietary technology, top-secret R&D labs. But they share a founding assumption: that in the long run, innovation will increase if you put restrictions on the spread of new ideas, because those restrictions will allow the creators to collect large financial rewards from their inventions. And those rewards will then attract other innovators to follow in their path.”
Bundling of goods can offend competition law, so that’s why legislators in a number of jurisdictions are nervous about ‘integrated care’.
In the past, Microsoft has accused of abusing Windows’ dominant status in the desktop operating system market to give Internet Explorer a major advantage in the browser wars.
Microsoft argued bundling Internet Explorer with Windows was just innovation, and it was no longer meaningful to think of Internet Explorer and Windows as separate things, but European authorities disagreed.
There’s no doubt that ultimately ‘whole person care’ will be some form of “person centred care”, where the healthcare needs (as per medical and psychiatric domains currently) are met.
But it is this idea of treating every person as an individual, with a focus on his or her needs in relation to the rest of the community which is the most challenging aspect of whole person care.
Joining up medical and social care with an ‘unified care record’ has never been attempted nationally, but it makes intuitive sense that care information from one institution should be made available to another.
Far too many investigations are needlessly repeated on successive admissions of the same patient, which is exhausting for the person involved. It would make far more sense to have a bank of results of investigations for persons, say who are frail, who are at risk of repeated admissions to acute hospitals in this country.
And this can’t be brought in with the usual haphazard ‘there is no alternative’ and ‘a pause for consultation’ if things go wrong. The introduction of the Health and Social Care Act (2012) and the CareData makes one nervous that lightning will strike a third time.
Labour has had long enough to think about what could go wrong.
Care professions might feel themselves ill-prepared in person-centred care. A range of training needs, from seasoned physicians to seasoned occupational therapists, will have to get themselves oriented towards the notion of a ‘whole person’. This might involve getting to grips with what a person can do as well as what they can’t do.
The BMA will need to be on board, as well as the Royal Colleges. Doctors, nurses, and all allied health professionals will have to double declutch from the view of people as problem lists, and get themselves into a gear about their patients as individuals who happen to be well or ill at the time.
This needs strong leadership, not people proficient at counting beans such that the combined sum total of a PFI loan interest payments and budget for staff doesn’t send a Trust into deficit.
Nor does it mean hitting a 4 hour target, but missing the point as a Trust does many needless admissions as they haven’t in reality fulfilled their basic admissions assessment fully.
For too long, politicians have been stuck in the groove of ‘efficiency savings’, ‘PFI’, ‘four hour waits’, and become totally disinterested in presenting a person-oriented service which looks after people when they are well as well as when they’re ill.
Once ‘whole person care’ finds its feet, with strong leadership and evident peer-support, we can think about how health is dependent on other parts of society working properly, such as housing and transport.
Technology, if this means that a GP could immediately know what a hospital physician has prescribed in real time in an acute admission, could then be worth every penny.
For the last few years, the discussion has centred around alternative ways of paying for healthcare instead of thinking how best to offer professional care to patients and persons.
The fact that this discussion has been led by non-clinicians is patently obvious to any clinician.
Technology also has the ability to predict, say in thirty years, which of the population is most likely to develop Alzheimer’s disease. Do you really want one of your fellow countrymen to have health insurance premiums at sky high because of having been born with this genetic make-up?
A lot of our problems, like the need for compassion, have been as a result of the 6Cs battling head-on with a 7th C – “cuts”. It’s impossible for our workforce to perform well if they haven’t got the correct tools for the job.
Above all, whole person care needs strong leadership, not just management. And if we get it right the NHS will be less focused on what it’s exporting, but more focused on stuff of real importance.
Ed Miliband at the 2014 Hugo Young lecture: Labour can’t sell its vision on the NHS because it doesn’t have one
One of the most famous criticisms of Gordon Brown that he was less concerned about the manner in which he delivered the argument, so long as he was ‘right’.
Tony Blair realised that Gordon Brown was ‘to the left’ of him quite early on.
In 2001, Blair and Brown had a tussle over ‘top up fees’ in higher education. Brown was against them, and Blair was in favour of them. There was a concern that this might lose Labour seats.
Fast forward onto 2014, and Ed Miliband presents disabled people being in control of their budgets. Of course, the idea of personal budgets has been progressing steadily for the last few years. But austerity presents a new opportunity for the personal budget: always presented as a method of empowering persons and patients with choice, it now gives the Labour Party, and a possible Liberal Democrat partner, a chance to mix up health and social care budgets. The beauty of this is that with the opportunity of top-pay payments in health, previously called ‘copayments’, slimming the State is sold as choice.
This has been briefed as being an aspect of Ed Miliband’s Hugo Young Speech to be given this evening.
The Clement Attlee government, in implementing the National Health Service, was accused of always having to combine ‘a vision’ with sheer improvisation.
Ed Miliband’s outlook on the NHS, while clearly obsessing in general about the interaction between the States and market in a curiously academic way, is now threatening to be full of improvisation, but no vision.
Andy Burnham MP is doing as much as he can do in selling Labour as ‘the party of the NHS’, and opposing competition, privatisation and hospital closures. But there’s curiously a complete lack of vision of what is going to take its place, apart from a rather nebulous concept known as ‘whole person care’.
Tony Blair often boasted about how people’s satisfaction of the NHS could often have nothing to do with political ideology. For example, how long you have to wait in A&E is surely something which should not depend on your political make-up?
Quite ironically, the theme of ‘abuse of power’ is common to both the left and right of political ideology, as is well known to ardent followers of E.P. Thompson and Edmund Burke respectively.
Even Churchill commented at the height of reaction to Bevan’s “vermin speech” that the Conservatives “might be vermin”, but did support the NHS.
The Labour perspective is full of inherent contradictions. This was for example seen in all its glory when Ed Miliband triumphed in the notion of ‘One Nation’, while launching quite an unpleasant attack on the Conservatives. One Nation is not, of course, completely possible while different devolved NHS systems are running in England, Wales and Scotland.
Ed Miliband’s populist left speech this evening manages to identify the “pantomime villains” of the outsourcing companies, without explaining why it might matter who delivers the NHS services?
Tony Blair always boasted how his great work on the public sector combined ‘reforms’ with ‘investment’.
But making money is not an ideology. Introducing neoliberal budgets, but saying it’s not individual consumerism, is laughable.
There’s clearly going to be some resentment from the general public to see hardworking taxpayers’ money invested in public services only for these to be privatised at some later date (e.g. HS2, Royal Mail).
When Blair proudly said he wished to see the NHS as a business, it’s an ideology of sorts; but in the same way you might wish to see education as a business, or war as a business, or prostitution as a business.
Blair of course disingeniously couples with this the idea that he wants to see the NHS as more ‘innovative’. This is of course is to assume that socialism can never deliver innovation, which is an unworkable concept because of the emphasis which socialism places on solidarity, cooperation and collaboration.
It’s all very well combining Arthur Daley with Citizen Smith producing ‘power to the people with cheque books’.
But the idea of accountability in the NHS is an utterly fraudulent one. Local people have absolutely no power on budget sheets of PFI hospitals being engulfed with regular interest payments, such that safe staffing levels cannot be enforced.
Local people have no power when it comes to a complaints system in the NHS which does not action any complaints.
The major problem is that Labour can’t sell its vision. That’s because it doesn’t have one. To execute its agenda, maybe a Labour-Liberal Coalition might in fact be the best thing for it.
Is doing “more with less” in dementia becoming “a lot more with virtually nothing”?
The “doing more with less” mantra of course very popular as a solution to the impending doom of having to treat the old fatties with a burgeoning technology budget. Re-engineering the health system has become a hobby of thinktankers, in the best spirit of the blind watchmaker. But policy wonks are still unable to escape from the fact that the NHS is not a widget factory. The management school of Frederick Taylor is totally unfit for purpose in considering outcomes rather than outputs. As national policy moves steathily towards promoting wellbeing, particularly in long term conditions, the question becomes, “what is a good outcome for a person with dementia?” Econometrics, and people in big corporates, will immediately point to costs, such as the financial cost of ‘unplanned admissions’. However, the “tide is turning” on all that. People are becoming interested in empowering people with dementia to lead fulfilling lives, building on what they can do. It is however inherently undermined by people wishing to abuse the system, such as large companies returning massive shareholder value and paying their staff pittance on zero-hours contracts. Everyone also knows the system only can survive through the large army of unpaid family caregivers.
At a time when Don Berwick was in fact Donald M Berwick president of the “Institute for Healthcare Improvement”, before he became ‘even more famous’, he published, “Measuring NHS productivity: How much health for the pound, not how many events for the pound” in the BMJ on Saturday 30 April 2005. Berwick reported that the ONS had recently concluded that NHS productivity had declined by 3-8% (depending on the method of calculation) between 1995 and 2003. This had led Berwick cheekily to ask, and most pertinently to ask, ““Production of what?” is the key question here. If we ask the wrong question the answer may lead us to the wrong policy conclusion.”
Berwick noticed that the method used thus far was fundamentally flawed.
“it does not assess improvement in the mix of these so called outputs, such as when innovations in care allow patients to be treated successfully in outpatient settings rather than in the hospital. To its credit, the ONS notes carefully that “the output estimates do not capture quality change.” Its interpreters need to show equal caution.”
Berwick concluded,
“The people of the UK should be not asking, “How many events for the pound?” but rather, “How much health for the pound?” At least, that is what they should ask if they desire an NHS that can keep them healthy and safe at an affordable price for as long as is feasible.”
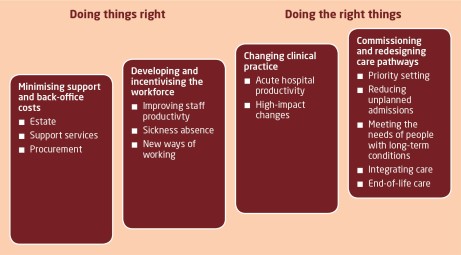
Wind on five years, and John Appleby, Chris Ham, Candace Imison and Mark Jennings gave birth to “Improving NHS productivity: More with the same not more of the same” from the King’s Fund on 21st July 2010. You can view it from here, if you wish. Efficiency, in true Frederick Taylor, was the name of the game again.
“As the evidence brought together here shows, there is huge scope for using existing expenditure more efficiently, in relation to both support and back-office costs, and particularly variations in clinical practice and redesigning care pathways. It should be noted that the actual sums identified as potential savings may have already been partly achieved by the programmes listed, and so the figures should be interpreted as an indication of the scale of potential savings rather than an absolute figure.”
Of course, the language of efficiency is totally laughable in the private sector with finding profit in repeated work and unnecessarily transactions. As the NHS lives in denial that its budget is not being squeezed, as £20bn is returned to the Treasury from “efficiency savings”, pursuing efficiency has been ‘a means to an end’, and, together with the zest for austerity, perpetuates the notion that NHS needs to dramatically cut budgets, reduce systematically services for patients and sack staff.
In his 2008/9 Annual Report, Sir David Nicholson prepared the NHS to plan ‘on the assumption that we will need to release unprecedented levels of efficiency savings between 2011 and 2014 – between £15 billion and £20 billion across the service over the three years’. These figures were based on analysis by the Department of Health, which assumed zero real growth from 2011/12 to 2013/14 in actual funding for the NHS in England. Given the state of the handling of the economy by the current Government, this was in fact quite a good assumption. It set this against spending that would be required to meet – as Nicholson reported (Health Select Committee 2010) – demographic changes, upward trends in historic demand for care, additional costs of guidance from NICE, changes in workforce and pay, and the costs of implementing government a £2.4bn non-“top down reorganisation” policy. Hence, the resultant ‘gap’ between actual and required funding of between £15 billion and £20 billion by 2013/14. Talking optimistically that is..
For dementia, there are other factors at play. With unified integrated budgets, or “whole person care”, it might be difficult to identify where the cutbacks are, as the figures merge into a morasse of confusion. Slimming the State might give a blank cheque under such a construct completely to annihilate social care. And against this background “self-care” – helping patients to better manage their own condition – has been promoted as being effective in reducing emergency admissions, including the use of care planning. At worst, “self care” is a figment of the Big Society which is a turkey which never flew.
So in that report from the Kings Fund various leadership and management devices are identified in relation to a productivity squeeze, of relevance to “the funding gap”:
A practical example of the benefits of integration along the pathway of care can be seen in Torbay, where health and social care integration has had a measurable impact on the use of hospitals. Torbay has established five integrated health and social care teams for older people, organised in localities aligned with general practices. Health and social care co-ordinators liaise with users and families and with other members of the team in arranging the care and support that is needed. Budgets are pooled and can be used by team members to commission whatever care is needed.
And – if productivity for dementia is extremely difficult to quantify, especially if you’re doing “more with less”, what about the general economy? According to NEF, recent estimates of productivity have told a familiar story: output per hour worked fell by 0.3% over the middle part of 2013. This means whatever economic growth occurred over the last year was not the result of people working better, or more efficiently. It was the result of an increase in the total number of hours worked. Productivity, over the whole year, barely improved. Roll over Taylor.
Labour productivity, the amount of economic output each worker generates per hour, fell sharply in the recession and has remained very weak. Employers hung on to workers when output fell and hired more people when the economy was stagnant. Productivity levels have remained relatively unchanged since the beginning of 2008. The difference between this and the three previous recessions is stark. And that is “the productivity puzzle”. ONS research has concluded that there is no single factor that provides an explanation, but identifies several that may have contributed.
Of particular scrutiny from economists has been something which has been enigmatically called “the changing nature of the workforce”. Firms have less need to fire people if pay rises are modest or if they are willing to work fewer hours. It is called “labour hoarding”, where employers hang on to more workers than they need in a downturn, so that when there is a recovery they can respond quickly, without incurring the costs of hiring and training new people. In a paper published published by the Institute for Fiscal Studies, researchers found many factors affecting productivity. They foud little evidence that the overall fall has been caused by labour hoarding, the demise of financial services or changes in workforce composition. Instead, we conclude that the key contributing factors are likely to be low real wages, low business investment and a misallocation of capital. But there’s always been one particularly attractive theory: “flexible” labour markets have been proved to be very effective in delivering part-time and temporary work, at low cost to employers. This is where market forces can lead to exploitation.
A “zero-hour contract” is a contract of employment used in the UK which, while meeting the terms of the Employment Rights Act 1996 by providing a written statement of the terms and conditions of employment, contains provisions which create an ‘on call’ arrangement between employer and employee. It does not oblige the employer to provide work for the employee.The employee agrees to be available for work as and when required, so that no particular number of hours or times of work are specified. The employee is expected to be on call and receives compensation only for hours worked. And they are popular – one survey suggests that up to 5.5m people are now working on a zero hours basis. Meanwhile, underemployment – those who would like to work more hours, but cannot – is at record levels. When faced with collapsing markets in the recession, employers – rather than reducing the number of people in work – effectively cut wages and hours of those working.
Doesn’t this sound perfect for addressing the NHS funding gap in dementia?
Reviewed by Roger Kline, several reports have made clear that recent changes in employment practices are undermining safe and effective care outside hospitals. In particular, according to Skills for Care, 307,000 social care workers are now employed on zero-hours contracts under which staff have no guaranteed hours (or income) and travel time is unpaid. This accounts for one in five of all professionals in this sector and the numbers are growing rapidly. Also, it is argued that “personalisation” has led to a growth of a section of the homecare workforce with virtually no employment rights at all – often on quasi self-employed terms – as well as raising serious questions about support, quality, training and supervision. All parties have been keen to pursue personal health budgets. It may be a coincidence that all parties agree on the need for the “efficiency savings”.
So the parties are largely singing from the same hymn sheet, and it is hard to know whether the think tanks have led to a discussion which airbrushes zero-hours contracts and unpaid family caregivers in dementia. In discussions of integrated care from think tanks, albeit in various guises such as “Making best use of the Better Care Fund” from the King’s Fund or “Whole person care” from the Fabian Society, there is a distinct unease about talking about the army of unpaid family caregivers, without whom many agree the care system would collapse, or those low-paid carers on zero-hours contracts. Converging evidence from the macroscopic picture of our economy, in the form of the ‘productivity puzzle’, and the landscape of social care for dementia paints in fact quite a grim picture of legitimising a solution to “the funding gap”.
This solution implemented has not in fact “doing more with less”. It’s been “doing a lot with virtually nothing”. And whatever your precise definition of ‘productivity’ for these workers, it is clear that many are at breaking point themselves under consider psychological and financial pressures themselves. Shame on no-one for discussing this with the general public.
Exploitation of carers should not be the solution for solving “the funding gap”.
Whole person care: disability still remains an exciting context for this policy
Of all the issues facing society, there is possibly not one medical issue which affects more systems in the body more? Alcohol misuse or abuse is a risk factor for various pathologies of the gut (e.g. liver cirrhosis, pancreatic cancer), for the mind and brain (e.g. alcoholic dementia, depression), the nerves (e.g. peripheral neuropathy), and it can exacerbate skin conditions (e.g. porphyria cutanea carda). It is also a massive societal issue as the work of Prof David Nutt on harm has shown. Alcohol abuse is also a risk factor for disability, as referred to in this description on the WHO website:
The harmful use of alcohol is a global problem which compromises both individual and social development.
It results in 2.5 million deaths each year. Alcohol is the world’s third largest risk factor for premature mortality, disability and loss of health; it is the leading risk factor in the Western Pacific and the Americas and the second largest in Europe. Alcohol is associated with many serious social and developmental issues, including violence, child neglect and abuse, and absenteeism in the workplace. It also causes harm far beyond the physical and psychological health of the drinker. It harms the well-being and health of people around the drinker. An intoxicated person can harm others or put them at risk of traffic accidents or violent behaviour, or negatively affect co-workers, relatives, friends or strangers. Thus, the impact of the harmful use of alcohol reaches deep into society.
In many ways, the various effects of alcohol on the health and social care service is an interesting policy consideration to seeing how ‘whole person care’ might work in future for the NHS. The problems with the ‘health maintance organisation’ and an approach driven by privatisation are well known across the pond, for other multi-system conditions such as diabetes and rheumatoid disease. If a future health system is ‘fit for the future’, it will need to overcome these problems, and “whole person care” possibly could not have come at a more helpful time for policy here in England and Wales.
Much heat has gone into the ‘pressures’ facing the NHS, with the limelight having been hogged by Sir David Nicholson and his ‘efficiency challenges’ and the “the funding gap”. While such discussions, mainly centred around the ageing society and the increased costs of privatisation can become rather repetitive and definitely tiring, the NHS is arguably facing its most challenging period since it was created in 1948. While much of the focus has been on the government’s reforms in England, there are a host of other factors that make the coming years crucial. Demands on the national service, ideally comprehensive and universal and free at the point of need, are rising, as are costs. The McKinsey analysis unhelpfully does not factor in all the sources of income of a national economy; it seems almost to assume that appreciable growth will not be an issue for the UK economy, and there is an absolute veto on voters wishing to fund a NHS adequately. This of course is a fault of the analysis of the current government, but “living within our means” has been a worthy factor of all political parties here in England and Wales. One of the great success stories of the past century has been the almost continuous rise in life expectancy. Since the NHS was set up life spans have increased by a dozen years for both men and women – and this trend is predicted to continue. This also means that people with medical conditions are living longer, and it possibly has been striking how disability and ageing have become ‘medicalised’ in recent years in policy strands driven by non-medics.
A massively tiring slogan has been ‘the need to think differently’, misused by some to justify ‘cutbacks’ in the name of ‘sustainability’. Liam Byrne and Jenny Macklin recently wrote a very powerful article on how best to empower disabled citizens ‘to fulfil their potential’. There is undoubtedly a need for “assessments that work”, but it is a simple fact at the moment, hundreds of thousands of the assessments are wrong. Years are wasted in court, where eventually 40% of appeals around employment and support assessments are won, and some disabled citizens have experienced huge mental distress and anguish (thus indirectly adding to the ‘demands’ on the NHS). Like the bedroom tax, the ideological onslaught perceived by disabled citizens, as per the “bedroom tax” (or more correctly described as “the spare room subsidy”), it is a “false economy”. As Bryne and Macklin describe, “it is a monumental waste of money – £74m, according to evidence provided to the public accounts committee by Disability Rights UK. We spend £900m on Atos. We’re about to spend £540m on Atos and Capita.”
In their very helpful article, they further describe:
It’s time to end the labyrinth. We’ll be looking at how we take the radical ideas of “whole person care”, developed by Andy Burnham, to bring services and benefits together to support disabled people in a new way. And we’re delighted that in Britain, Sir Bert Massie, a great pioneer of disability rights, will be working alongside us to make sure ideas are co produced with disabled people every step of the way. Labour will be publishing a green paper on the idea next summer. It’ll be far stronger for the advice from down under.
According to a news report from Australia, on 3 July 2013, Minister for Ageing and Disability Services Andrew Constance released the “Living Life My Way Framework” which will guide the expansion of opportunities for people to exercise choice and control over their supports as NSW transitions to the National Disability Insurance Scheme (NDIS). People with disability currently receiving disability services who are interested in moving into an individualised funding arrangement in a policy strand mirroring the drive towards personal health budgets I have recently discussed elsewhere. The framework is based on the findings from the extensive Living Life My Way consultations held across NSW during 2011 and 2012. The NSW Government is committed to a service system that increases choice and control for people with disability. For this reason, NSW became the first Australian state to agree to a fully funded NDIS in which we’ll contribute $3.1 billion a year from 2018/19, with the Commonwealth to invest $3.3 billion. As in Australia, here in England and Wales a common cause of disability is stroke, and therefore thinking about how all the services ‘link up’ with each other is going to be essential. For many needs of a patient who has suffered a stroke, there may be care needs, such as speech and language, physiotherapy, social care and dietary, which may not be in the direct specialist knowledge and experience of the hospital physician (or General Practitioner).
Dementia and disability will be considerable policy planks in the NHS in the forthcoming decades, and of course they impact on other important policy considerations for England and Wales such as frailty. In Chapter 7, “Bringing the person back” by Richard Massie in “Together: A vision for whole person care for a 21st century health and care service“, a policy discussion document for the Fabian Society published earlier this year, Massie writes as follows:
“A third of people using care services are working- age disabled adults, and in many areas they take up half of the local budget. With whole person care, Labour could be on the cusp of creating a care system fit for disabled people in the 21st century. But only if some big questions are answered, not least how a health system free at the point of access can be merged with a care system so dependent on eligibility and assessment.
Disabled people across the country were smiling to themselves as Andy Burnham took the stage and spoke of his vision for ‘whole person care’. Smiling because his vision was strong, positive and put disabled people at the heart of health and social care reform. But also because they know how difficult it will be to turn this sentiment into practice.
Burnham’s vision is of active people in control of their health and support, collaborating with the state to achieve better outcomes. Seeing people in the round and increas- ing choice and control are core tenets of the disability and independent living movements. Needing to manage a health condition like MS or diabetes, needing support to wash because you lack manual dexterity, or needing specialist support to communicate with people in your community because you are deafblind should not be limiting, but be the cornerstone of independence. Providing good care and support can enable people to take part in family life, get involved in their local community and go to work.”
You’d be forgiven for thinking that the reform of health and social care was only about our ageing society, so fre- quently are debates only framed as a crisis facing older people. It’s true that there are examples of older people being shockingly treated in our NHS, left undignified in care homes and kept in hospital too long because support isn’t available in their community. Their care crisis rightly needs to be a national priority, but so does the care crisis facing disabled adults. The care crisis is as real for them as older people, and cases like the neglect and abuse of patients by staff at Winterbourne View need to be a wake-up call to decision makers on the need to focus on disability too.
A third of people using care services are working-age disabled adults, and in many areas they take up half of the local budget. Furthermore, the number of disabled adults needing care and support is increasing. In 2010/2011, 1.1 million disabled people relied on the social care system, but by 2020 we anticipate that the number of people in need of care will have risen to 1.3 million. Traditionally this group may not be regarded with as much electoral attraction as the ‘grey vote’, but social care reform that does not have the needs of disabled people at its heart is sure to fail.”
There have been endless discussions about what “integrated care” might mean, further to simply “joined up” or “more co-ordinated care”. A minority still remain convinced that “integrated care”, and in particular individualised personal health budgets is the ‘Trojan horse’ for privatisation of the NHS, akin to the shared care hospital models which are currently active in the US. However, thinking about the needs of two groups of society, people with dementia and people with disability, presents a formidable challenge for how a caring society can look after an individual and perhaps recognise the beliefs, concerns and expectations of that individual. It also poses fundamental questions of what our NHS is there to do. It has long been argued that the emphasis of the NHS should be wrenched away politically and economically from the NHS Foundation Trusts for more shared clinical decision-making in the community. Individuals with dementia or disability do not particularly wish themselves to be considered as a ‘burden on society’, however that debate is framed by society. They do not wish to be seen as ‘ill’ either, although some individuals will succumb to illnesses, on account of their dementia or disability. This is all about a society which is inclusive, and may be in keeping with Labour’s “One Nation” more than people might currently realise.
Benn, Bevan and Burnham: continuity of care?
One of the lasting legacies of the introduction of the Andrew Lansley Health and Social Care Act (2012) is that it was a massive betrayal of trust. It explicitly did not appear in the Conservative manifesto. It was clearly a Lansley ‘vanity project’ which cost billions to implement.
While the purpose of this Act was promoted in a number of different marketing ways, the Act, nearing five hundred pages, is in fact incredibly simple.
It sets up a market based on competitive tenders. It sets up a beefed up economic regulator. It sets up the climate for ‘liquidation camps’ that only Frederich Hayek could have been truly proud of.
That was basically not a vision that most people had for the NHS in these demanding times.
With not a single clause on patient safety, save for abolition of the National Patient Safety Agency, it was clearly not drafted to prevent another Mid Staffs.
With this level of mistrust, there are people who think integrated care is a shoehorn for a private insurance system.
And yet paradoxically the latest NHS reforms seems to have taken a lot of wind out of the sails of a move towards an insurance-based system as proposed by Reform a few years ago. Whilst Kaiser Permanente seems to still quite chummy with certain think tanks, it’s clear the voters in majority want a properly funded national health service funded out of taxation.
Against this backdrop, care of older people is possibly not what anyone would want it to be currently.
Labour has indeed a long legacy in the NHS history, but is clearly now looking to the future. It is argued that ‘whole person care’ can complete Bevan’s vision, uniting the NHS with social care. This would mean one service looking after the whole person – physical, mental and social. Indeed Andy Burnham at this year’s Party conference recalled the “spirit of 45″. This vision would be symbolic for beginning to bring to a close the marketisation and privatisation of the health service.
Labour have pledged to repeal the Health and Social Care Act 2012, which is fragmenting the service.
And yet a decade ago the Health and Social Care (Community Health and Standards) Act 2003 Commencement (No. 1) Order 2003 was the most controversial piece of legislation to come out of the then government’s 10 year strategy for the NHS in England. This piece of legislation, which abolished government control of NHS trusts by turning them into competing independent corporations called foundation trusts, was a major policy reversal. The concern then was it could lead to considerable local variation in services and endangers one of the NHS’s founding principles–to provide equal care for equal need.
Beep, beep – this vehicle is reversing.
Labour has set up an independent commission under Sir John Oldham to examine how health and social care can be integrated. Ed Miliband feels that this is is the biggest challenge in the history of the NHS. This in part addresses the gap between NHS and care demand which is expected in coming years, and current funding.
There is absolutely no doubt that integration is being damaged by the government’s “free market ideology”, a point freely conceded by the corporate competition lawyers.
The great attraction of the Whole-Person approach, with the NHS taking responsibility for coordination, is that it can be in a position to raise the standards and horizons of social care, lifting it out of today’s cut-price, minimum wage business.
It is clear from Tony Benn’s brief interview with Emma Crosby that Benn has concerns. Benn in his latest diaries, “Autumn blaze of sunshine”, talks of various medical issues which have caused him to come into contact with the caring professions. Benn most obviously feels that valuing care workers has not been a priority of English society by any stretch of the imagination. Benn most obviously wants this to be addressed in some form in a future Labour government.
There has been much said about valuing social workers, but the profession of social care work have been equally vocal about voicing their hard-felt concerns. It is possible that social care careers could be more valued and young people able to progress as part of an integrated Whole-Person workforce. This is yet to be seen.
So an NHS providing all care – physical, mental and social – could be held to account by powerful “patient rights”.
The approach, unlike the Health and Social Care Act (with the exception of the surgeons), has been welcomed by professionals in the Royal Colleges. For example, the Royal College of Psychiatrists has argued that ‘a parity approach’ should enable NHS and local authority health and social care services to provide a holistic, ‘whole person’ response to each individual, whatever their needs. They have also argued that this should ensure that all publicly funded services, including those provided by private organisations, give people’s mental health equal status to their physical health needs.
Central to this approach is the fact that there is a strong relationship between mental health and physical health, and that this influence works in both directions. Poor mental health is associated with a greater risk of physical health problems, and poor physical health is associated with a greater risk of mental health problems. Mental health affects physical health and vice versa.
And it’s clear that ‘whole person care’ is not some weird science fiction. A number of local authorities have already signed up to become “whole person care innovation councils” in a programme led by Labour’s shadow health secretary Andy Burnham. The councils are already taking the first steps towards turning into reality Mr Burnham’s vision of a single health and social care service. Under these Labour plans more care will be provided directly in people’s homes, there will be a greater focus on prevention and better co-ordination between different branches of the system.
In the 21st Century, the challenge is to organise services around the needs of patients, rather than patients around the needs of services. That means teams of doctors, nurses, social workers and therapists all working together. This ideally means care being arranged by a single person who you know – ending the frustration of families being passed around between different organisations and having to repeat the same information over and over again.
This seems to be the sort of thing which Tony Benn would like too.
But it is a marked shift in gear. It means a greater focus on preventing people getting ill and more care being provided directly in people’s homes so they avoid unnecessary hospital visits. Keeping frail individuals out of hospital will clearly be one of the ‘next big things’ in English health policy, whoever is in government after May 7th 2015.
It will be quite a culture shock to move the NHS from an organisation being pump-primed for global multi-national expansion. But the NHS has been through worse changes. This one might actually be useful.