Home » Posts tagged 'stigma'
Tag Archives: stigma
Sticks and stones may break my bones
I had first become interested in the language surrounding dementia in 2014, when I presented a poster on the G8 pitch, at the Alzheimer’s Europe conference in Glasgow.
At that point, I realised that sticks and stones could break my bones, but words could hurt me.
I have long since not attended any national or international conferences, not simply because I found the same topics being discussed in perpetuity, but because I felt the conferences were for an in-house cliques who were far more into massaging their own egos and putting themselves up in flash hotels than the reality of dementia.
But I later returned to the issue of language, in relation to stigma, in my second book on dementia ‘Living better with dementia’ published in 2015 by Jessica Kingsley Publishers. As my own mother lives with me, and as her dementia advances, I’ve genuinely found my own book to be a source of information and support. For example, only last night I was reading up on my own thoughts of the ‘sweet tooth’ in dementia and the neuroscientific evidence for why it occurs. Latterly, I’ve toyed with the idea of writing a cookbook for unpaid carers, living with limited resources including scarce money and time, of people living with dementia. I would love to work with someone who’s interested in this specialist field, such as a nutritionist or dietician, to help me.
I became physically disabled in 2007 after more than a month unconscious on the intensive care unit of a local hospital, where I was invasively monitored for acute meningitis. Although I subsequently read Goffman on stigma about a decade later, I had the misfortune to experience stigma first-hand. The sense of ‘otherness’ is something you experience if you’re in a wheelchair, and a London cab refuses to stop despite the cab having its yellow light on. Of course, I had direct experiences of ‘otherness’ as other medical professionals disowned and excluded me when I needed help the most – both in my alcoholism and in recovery. I am currently doing professional dilemma questions, and the knowledge that senior clinical people I worked with turned a blind eye, or did not know what to do and did not admit it, to my illness still frightens me.
As a result of this, I have a low threshold to calling out ‘otherness’, that is where you define people as different to you, and, more than than that, try to discredit them. This might include supporters of Brexit or not, Jewish or Muslim citizens or not, or even living with a long term condition. I don’t think the key to destigmatising stigma is by segregating people. At worst, this might include the ghettoization of people with dementia or mild cognitive impairment such that they all safely live in the same ‘dementia village’, to all intents and purposes ‘out of sight’ and ‘out of mind’. Care homes used to be criticised, by some, for potentially warehousing individuals if the prescription of chemical or physical restraints was frequently abused, similarly. This is not real integration and inclusion, in other awards appreciating the diversity of individuals, but actually lumping all people together with the same label.
For example, in ‘dementia friendly communities’, we don’t acknowledge individuals have different qualia of cognitive impairments, in memory, language or whatever, at various degrees of severity. We don’t discuss how the social determinants of health impact on the health and wellbeing of people, such as poverty or the shutting of day centres. We just clump all people together as ‘dementia’. This is not a million miles off of creating vast groups comprising unique individuals, such as ‘learning disabilities’ or ‘the elderly’.
Whilst the counter-argument is that identification of these groups of people means that their needs can be serviced, often the opposite is true. Recently, a paper has been published on identifying the most ‘frail’ people so that we can be aware that they are the most intense in resource allocation. But think about this carefully. This can mean that we use the information to discriminate actively against the most vulnerable – ‘equity’ and ‘justice’ are not necessarily compatible ethically.
Above all, I am scared how language is used to legitimise discrimination, ‘otherness’ and to embolden other people’s vulnerabilities and weaknesses.
I did a brief scan of some ‘offending’ words, and I compiled them into a table.
I have been much derided for talking about “assets” and “strengths” as well as “deficits”. For example, one person commenting on a piece I wrote in the Guardian remarked similar to, “We don’t need to worry about this patient lying on the operating theatre table with advanced pancreatic cancer. She has great teeth.”
But I strongly believe that it is not difficult to slip into the patronising ‘does he take sugar mentality?’ I don’t wish to turn the medico-legal concept of ‘paternalism’ into a “dirty word”, but, as for our experiences with individuals with special needs, it is a slippery slope to outright dehumanisation and depersonalisation.
I never really understood what it was like to lose your sight until I went blind in one eye last year – but this was surgically operated upon with success. Likewise, I think many of us think we won’t be the ones who get diagnosed with cancer or dementia. But the law of averages means that some of us will be.
And we should think about how “we” would feel if “other people” talked about “us” like that.
Stigma in dementia poses crucial questions for dementia friendly communities
The literature on stigma is comprehensive.
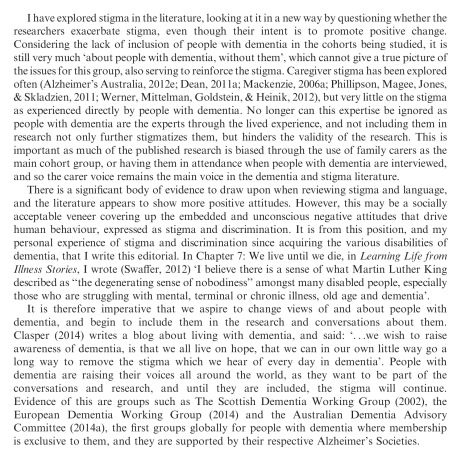
But Kate Swaffer added to it beautifully in the journal ‘Dementia’, with an article today – on open access – entitled “Dementia: Stigma, language and dementia friendly”.
Kate refers to a blogpost by Ken Clasper, a Dementia Friends Champion, which asks, sensibly, what we are trying to achieve with more ‘awareness’.
And if you scroll down to the end of this tour de force on stigma and dementia, you’ll see exactly why Kate is able to opine with such legitimacy and authority.
I conceded a long time ago – in March 2014, in fact – on this blog that the policy plank of ‘dementia friendly communities’ is an incredibly complex one.
The discussion of stigma seems to be one of perpetuity. We’ve seen numerous attempts at it, including the original work of Goffman (1963) on stigma and ‘spoiled identity’.
It’s been re-incarnated as a Royal College of Psychiatrists campaign on stigma.
This morning there was another bite of the cherry.
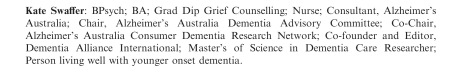
The report, New perspectives and approaches to understanding dementia and stigma, published by the think tank International Longevity Centre UK (ILC-UK) is produced by the MRC, Alzheimer’s Research UK, and Alzheimer’s Society; it was also supported by Pfizer.
I’ve thought how I could possibly respond to Kate. And I can’t, as Kate is in every sense of the word an ‘expert’.
But it did get me thinking.
It got me thinking of the happy times I had with Chris and Jayne last week at the Alzheimer Europe conference in the city of my birth in Glasgow.
‘There’s more to the person than the diagnosis” is one of the key five messages of ‘Dementia Friends’, an initiative from the Alzheimer’s Society predominantly (and Public Health England). This is mirrored in a tweet by Chris from this morning.
Chris is also a “Dementia Friends Champion“, and lives well with dementia.
Last week, I attended a brilliant all-day workshop chaired by Karishma Chandaria, Dementia Friendly Communities manager for the Alzheimer’s Society. The progress which has been made on this policy plank is substantial, and I am certain that the next Government will wish to support this policy initiative in the English for 2015-20.
It is stated clearly in Simon Stevens’ “Five Year Plan” for NHS England.
It is a core thread of the Prime Minister’s Dementia Challenge.
And the ‘coalition of the good’ has seen the dementia friendly communities policy plank develop drawing on work from ‘Innovations in dementia’ and the Joseph Rowntree Foundation.
And to give the Alzheimer’s Society credit, where it is certainly due, there has been launched an open consultation for a British Code of Practice (currently ongoing), to which anybody can contribute.
But this code of practice does, again, have the potential to be very divisive. It might be painful to make dementia friendly communities, such as the large one in Torbay, ‘fit into this box’.
Torbay in many ways is a beacon of innovation for integration between NHS and care. There is genuine “community bind”, with citizens, shopkeepers, transport, police, for example, contributing.
The article on the BBC website about Norman McNamara (January 2012) predates the Prime Minister’s Dementia Challenge, (which started in March 2012.)
Any top down way of making bottom-up social groups ‘conform’ will be hugely problematic in the implementation of this approach to dementia-friendly communities, potentially.
The methodology of dementia friendly communities has to be truly inclusive: it is all or nothing.
I agree with Kate, and like her I wish to avoid protracted circular definitions of ‘stigma’. For me, I recognise stigma when you see it, like how the Supreme Court of the US recognises erotica and pornography as per Jacobellis v Ohio [1964].
It is possibly easier to define stigma by its sequelae, such as avoiding wishing to talk about dementia in polite conversation, or not wishing to see your GP about possible symptoms of a dementia in its early stages, or not wanting to socialise with people with dementia who happen to be in your family.
We know these are real phenomena, as demonstrated, for example, by the loneliness of many people on receiving a diagnosis of possible dementia.
And we know stigma can harbour deep-seated irrational prejudice, like the incorrect notion that dementia is somehow contagious like a ‘superbug’.
Stigma can be exhibited in pretty nasty ways in language: such as “snap out of it” or “victim”.
My discussion of whether people living with dementia are ‘sufferers’ tends to go round and round in circles with people who disagree with me.
Suffice to say, I agree it is possible for a person living with dementia, such as a person who has received a diagnosis of Lewy body dementia and who has to put up with terrible “night terrors” and exhaustion the following day.
I think if you live independently, but with full insight into your symptoms, it can be exasperating. I have never been in that position though, and it would be invidious of me to second-guess.
I think if you are close to someone in the latter stages of dementia, you can suffer.
But I’ve written about this all, indeed on this blog, before here.
The only thing that is new is Peanuts’ cartoon (original citation here).
In that workshop, I also sat through Joy and Tone Watson’s brilliant “Dementia Friends” session. Joy lives with dementia. And their session was brilliant.
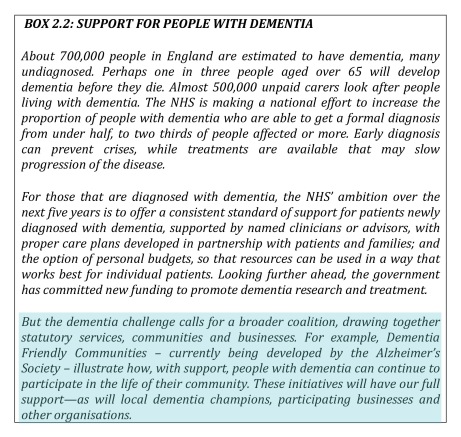
This was the final ‘exhibit’.
I attended a special group session on stigma with Toby Williamson from the Mental Health Foundation during that day. In that session, it was mentioned that ‘rôle models’ of people living well with dementia might help to break down stigma.
Or maybe guidance for the media might help? One cannot help wondering if an article such as in the Daily Mail today might actually put off people from seeking a diagnosis of dementia (completely unintentionally).
But I did bring up something on my mind.
“Stigmata” literally means signs.
But dementia can be, like other disabilities, quite invisible.
Somebody might have insidious change in personality and behaviour, noticed by somebody closest to him or her, with no obvious changes in cognition (nor indeed in investigations).
I showed this in my paper published in Brain in 1999, currently also in the Oxford Textbook of Medicine.
The condition I refer to is in fact one of the more prevalent causes of dementia in the younger age group, called the “behavioural variant of frontotemporal dementia“.
If the signs are ‘visible’, then you are obliged legally to make reasonable adjustments for any disability. In England, this includes dementia under the guidance to the Equality Act (2010).
As Toby Williamson says, if you’re obliged to build a ramp for somebody in a wheelchair for a place of work, there’s an equal obligation to produce adequate signage for people who have navigation problems as a result of a dementia such as dementia of the Alzheimer’s type.
There are reams and reams of evidence on equality and the built environment (for example the Design Council or Commission for Architecture and the Built Environment).
I personally think it’s brilliant you can go into certain shops, and the customer-facing staff will, potentially, be able to recognise if a person does need time and space to pay for items.
This is also been tackled in the Scottish jurisdiction through Alzheimer Scotland.
Also, corporate lawyers should be advising large employers about the scope for unfair dismissal claims by people dismissed as they are about to arrive at a diagnosis of dementia (particularly young onset dementia).
The timeline is roughly this. Somebody has health problems – he or she is invited to leave and given a pay off – these health problems turn out to be a diagnosis of probable dementia – by this time the dismissal is not unfair.
I feel confident the ‘dementia friendly communities’ policy strand in England, and across other jurisdictions, is here to stay. I share, though, Kate’s concerns that about the relative ease with which this policy has lifted off, say, compared to how one might feel about ‘gay friendly communities’ or ‘black friendly communities’. One has to be extremely careful about any policy plank which alerts people to divisions, “them against us”.
This is what I know best as the “don’t think of elephants phenomenon” and then you think of elephants.
This policy, anyway, currently has huge momentum. Marc Wortmann is currently Executive Director of Alzheimer’s Disease International (ADI), the organisation providing a global voice for dementia and the founder of World Alzheimer’s Month. Wortmann has been instrumental in propelling dementia friendly communities to the foreground of world policy.
But, in firing up ‘dementia friendly communities’ (a term which I think is sub-optimal’), v 2.0, there is plenty of time to get it right.
The Dementia Alliance International is not a convenient marketing tool for dementia salesmen
The following is the draft of an extract from my chapter “Stigma, citizenship and living better with dementia” in “Living better with dementia: how champions can break down the barriers”, by Shibley Rahman with Forewords by Prof Alistair Burns, Kate Swaffer and Chris Roberts.
The really important question therefore is: how can people living with dementia lead? A really important steer for this came from the Joseph Rowntree Foundation in a report by Toby Williamson called “A stronger collective voice for people with dementia” (October 2012). The Dementia Engagement and Empowerment Project (DEEP) was a project which aimed to explore, support, promote and celebrate groups and projects led by or actively involving people with dementia across the UK that were influencing services and policies, affecting the lives of people with dementia. DEEP was a one year project which finished in Summer 2012. One of their key recommendations was that national and local organisations providing services or working with people with dementia need to develop and implement involvement plans, allocating resources to develop new groups, link groups together and help them share resources. Furthermore, it was recommended that researchers and research networks need to involve groups of people with dementia in helping to identify research topics, advise on research findings and undertake research on topics identified as important by people with dementia. Thankfully, this work has now been extended as part of the Joseph Rowntree Foundation’s work “Dementia Without Walls”, with various stakeholders also involved.
Ruth Bartlett erself found that keeping a diary has the potential to be used much more widely in patients living with dementia. In her opinion, the main advantage of this method is that unlike interviews, the diarist, rather than the researcher, is ultimately in control of how and when data are collected (e.g. Bartlett, 2011). Bartlett argues that diaries encourage participants to record thoughts and feelings as and when they occur and wherever they feel most comfortable; it therefore has the potential to compensate for short-term memory problems associated with dementia, plus it could help to minimise ‘respondent burden’ traditionally associated with interview based studies involving people with dementia (Cottrell and Schulz, 1993, p. 209). Bartlett has further suggested that people living well with dementia are willing, able to campaign, and presenting this at national and international conferences.
Dementia Alliance International (DAI) is the first global group, of, by and for people with dementia, where membership is comprised exclusively of people with dementia. Dementia Advocacy and Support Network International (DASNI) was the first organisation set up in 2001 by people with dementia; however their membership was not exclusive to people with dementia. There subsequently saw a sprinkling of groups at national levels, the Scottish Dementia Working Group (2002), the European Dementia Working Group (2012) and the Australian Dementia Working Committee (2013) were set up with membership of people with dementia, supported by their national Alzheimer’s organisations.
DAI was therefore established in January 2014 to promote education and awareness about dementia, in order to eradicate stigma and discrimination, and to improve the quality of the lives of people with dementia. DAI advocates for the voice and needs of people with dementia, and provides a global forum, aiming to unite all people with dementia around the world to stand up and speak out.
In the last few years, the voices of people with dementia around the world have become stronger, with leaders including Richard Taylor, Janet Pitts and Kate Swaffer. More recently a number of people with dementia have been discussing things globally, finally giving birth to DAI, to ensure issues such as social isolation, discrimination, stigma and exclusion are addressed. Their members wished to build a group consolidating the vast global networks of people with dementia now speaking and collaborating with each other over the Internet through blogs, Twitter, Pinterest, Facebook and other social media. The modern internet now offers incredible opportunities for organising social movements. too large or too difficult for a single person to undertake. In typical crowdsourcing applications, large numbers of people add to the global value of content, measurements, or solutions by individually making small contributions. Such a system can succeed if it attracts a large enough group of motivated participants,such as Wikipedia, Flickr and YouTube. These successful crowdsourcing systems have a broad enough appeal to attract a large community of contributors, giving true credibility to the idea that the whole is more than the sum of its constituent parts. And initial experience of people living well with dementia and the social media has led to interest in a related activity called ‘friendsourcing’. Friendsourcing attempts to synthesise social information in a social context: it is the “use of motivations and incentives over a user’s social network to collect information or produce a desired outcome, using as a guide what members of the network themselves consider to be important” (Bernstein et al., 2010).
But the notion that dementia is a cognitive or behavioural disability puts the debate into an altogether different stratosphere. Instead of aspirational ‘dementia friendly communities’, a title which itself is open to abuse by politicians, other leaders and charities, the narrative then becomes treating persons with dementia for whom policies cannot serve to their detriment. That is unlawful, under indirect discrimination in various legal jurisdictions. That is therefore an enforceable right. But why is there a feeling that things have not improved much despite various global initiatives.
Batsch and Mittleman (2012) in their ADI World Alzheimer Report, “Overcoming the stigma of dementia” remark that:
“Government and non-government organisations in some countries have?been working tirelessly to pass laws aimed at eliminating discriminatory practices such as making people with dementia eligible for disability schemes. Regional organisations within countries have worked with local governments to improve access to services and delay entry to residential care, most of the time by trying to reduce stigma amongst family carers and health and social service professionals through increased education and regulations.”
Beard and colleagues (2009) offer practical suggestions for how a volte face in thinking could come about:
“Study participants reported various ‘rough spots’ along the path of dementia and their strategies for circumventing them. There were personal, interactional, and environmental factors that caused them difficulties. Strategies included concrete activities, emotional responses, and environmental adaptations. Respondents used cognitive aids, made various modifications, garnered assistance from others, and practiced ‘acceptance’ to deal with persistent problems. Barriers resulted from the disease itself as well as personal obstacles and pressures from others. Participants clearly demonstrated that their lives were meaningful and could be further enriched through advocacy, a positive attitude, and physical, mental, and social engagement. These data show persons with dementia performing the emotional work of illness management, incorporating related contingencies into everyday life, and reframing their own biographies. As they creatively adapted and constructed meaning, order, and selves that were valued, respondents demonstrated agency by actively accommodating dementia into their lives rather than allowing it to be imposed upon them by structural forces.”
The highly intriguing aspect now is that even the narrative of ‘involvement’ is being reframed. This was indeed warned about by Beresford (2002) who suggested service user involvement has emerged out of two different rationales for participation – one consumerist, the other democratic. The former claims that greater efficiency, efficacy and effectiveness will result from appropriately-placed service user feedback mechanisms. The latter, democratic approach, often framed in a rights discourse, views user participation as a form of self advocacy. The history of mental health activism can be dated far further back, to 1620, when inmates at the Bedlam asylum petitioned for their rights (Weinstein, 2010). That the DAI finds itself having attracted the attention of large charities, Big Pharma and social enterprises promoting living well with dementia is not altogether surprising therefore, even despite its relatively young existence.
References
Bartlett, R. (November 2011) Realities Toolkit #18: Using diaries in research with people with dementia.
Batsch, N. L., Mittelman, M. S. (2012) World Alzheimer’s report. Overcoming the stigma of dementia. Executive summary. London, UK: Alzheimer’s Disease International.
Beresford, P. (2002) ‘User Involvement in Research and Evaluation: Liberation or Regulation? Social Policy & Society, vol. 1(2), pp. 95-105.
Cottrell, V., Shulz, R. (1993) The perspective of the patient with Alzheimer’s disease: A neglected dimension of dementia research, The Gerontologist, 33 (2), 205-211.
Weinstein, J. (2010) Mental Health, Service User Involvement and Recovery, London: Jessica Kingsley.
My personal experience of an introductory day to ‘Dementia Friends’ Champions
OK it’s not heaven on earth – but Kentish Town London does have some merits I suppose.
To say that I am passionate about the dementia policy in England is an understatement.
Throwing forward, I believe living well with dementia is a crucial policy plank (here’s my article in ‘ETHOS journal’), for which service provision needs a turbo boost through innovation (here’s my article co-written in Health Services Journal).
“Dementia Friends” in reality means rocking up in a venue somewhere near you for about 45 minutes to learn something about the dementias.
Once you sign up on their website, the experience is also backed up by an useful non-public website containing details of training, pre-training materials, and help on how to promote sessions. You can also provide on that website precise details of any ‘Dementia Friends’ information sessions that you run in due course.
I had known of this initiative mainly through Twitter, where I am very active. I find the twitter thread of @DementiaFriends interesting.
Even I’ve been known to get involved in a bit of mass hysteria myself:
I possibly signed up despite of the substantial interest in the media and social media, what psychoanalysts might call an “abreaction”. There’s a large part of me which feels that I do not need 45 minutes on dementia, having studied it for my much of my final undergraduate year at Cambridge, done my Ph.D., written papers such as this (one of which even appears in the current chapter on dementia in the Oxford Textbook of Medicine), written book chapters on it (which as this one which appears in a well known book on younger onset dementia), and even written a book on living well with dementia.
But Prof Alistair Burns is a Dementia Friend – and he’s the clinical lead for dementia in England.
I went out of curiosity to see how Public Health England had joined forces with the Alzheimer’s Society. I must admit that I am intensely loyal to the whole third sector for dementias, including other charities such as the Joseph Rowntree Foundation, Young Dementia UK, Alzheimer’s BRACE, and Dementia UK.
I have my own particular agendas, such as a proper care system for England, with the provision of specialist nurses such as Admiral Nurses. I think some of the English policy is intensely complicated, best reserved for those who know what they’re talking about – especially people currently living with dementia and all carers including unpaid caregivers.
I personally think the name ‘dementia friendly communities‘ is ill conceived, but the ethos of having inclusive communities, well designed environments and ways of making life easier for people with certain thinking problems (such as memory aids, good signage) highly attractive. It would be unfair in my view for this construct to be engulfed in cynicism, when the fundamental idea is likely to be a meritorious one.
But I don’t think Dementia Friends competes with any of that, and one must be mindful of the gap society had of awareness of dementia.
This gap is still enormous.
And the aim is for people – not just Pharma – to be interested in dementia. These are real people with their own lives, not merely ‘potential subjects for drug trials’ (worthy that the cause of finding an effective symptomatic treatment or even cure might be potentially). But these are people living in the now – take for example the Dementia Alliance International, persons with dementia with beliefs, concerns and expectations of their own like the rest of us.
Only at London Olympia at the “Alzheimer’s Show” [and it is very well I am not a fan of such events which I have previously called "trade shows"], the other week, I presented at London Olympia for my ‘Meet the author session’, arranged on the kind invitation of various people to whom I remain very grateful.
At “The Alzheimer’s Show”, I met within the space of ten minutes a lady newly diagnosed with vascular dementia who did not intend to tell anyone of her diagnosis, and one person married to someone with probable dementia of the Alzheimer type who did not even tell his friends for three years.
It’s a rather badly articulated slogan but the saying ‘no decision made about me without me’ I think is particularly important for dementia.
These are two real (without warning) discussion points from the floor.
“Are people with dementia actually involved with any of the sessions?”
Yes: in fact my pal Chris Roberts (@mason4233) in Wales delivers his Dementia Friends sessions word-perfect for 45 minutes, without telling his audience that he himself lives well with dementia until the very end. Chris tells me this dispels, visibly, preconceived prejudices from his audience members. Chris blogs regularly on his blog, and has written for the ‘Dementia Friends’ blog.
“Why should people with dementia be given special elevated status compared to any other medical condition?”
It’s a difficult one. Some people believe that with dementias people will easily ‘snap out of it’ ‘if they pull themselves together’. This is completely at odds with one of the learning points that dementia is chronic and progressive. And of course people in the real world – viz CCG commissioners – have to decide how much they wish to prioritise dementia ahead of, instead of, etc. other medical conditions such as schizophrenia. But people living with dementia can present with known problems such as forgetting their pin number, and therefore it’s not actually a case about giving people with dementia an ‘elevated status’, but getting them up as individuals to be expected from anyone. Although it’s motherhood and apple pie, it’s very difficult to find, whatever the motive, the intention of dementia friendly high street banking fundamentally objectionable.
Dementia Friends Champions become rehearsed in the programme at one-day sessions across England. What happens is that you watch videos on their website, sign up for a day (where you get to take part in a Dementia Friends session) and then attend the session somewhere close to where you live habitually.
The sessions are run all over England at regular frequency. You sign up for a session, then you get an email quickly afterwards. You go to the meeting.
My meeting started on time. I am physically disabled, so I was grateful for easy access to the venue in Voluntary Action Camden (I could use the lift).
One of the things some of us mean-minded people pick holes in is whether the venue itself might be dementia-friendly. TICK.
I thought so.
The group dynamics worked really well.
My group consisted of interesting people, all ‘realistic’ in their expectations of shifting the Titanic of messaging of negative memes in the media. Many of my group were particularly interested in social equity, fairness and justice, reading between the lines.
I particularly enjoyed speaking with one delegate who is a NHS consultant in psychiatry. We went through pleasant niceties of what he was examined on in his professional membership exams (in his case the difference between schizophrenia and drug-induced psychosis). But he was great to chat to during the day.
I bored him to death with my example of persons with dementia putting numerous teaspoons of sugar in their cups of tea, on rare occasions, due to ‘utilisation behaviour’, a particular predilection for sweet foods since the onset of dementia, or cognitive estimates problem, a very niche area of cognitive neuropsychology for both of us. But this was simply in an activity on making tea where such private chit-chat was irrelevant; the actual session as delivered, on how to make a cup of tea, was far superior than the two hour version I did in a workshop for my MBA in that well known method known to managers: “process mapping“.
The whole day was presented by Hannah Piekarski (@HannahPiekarski), Regional Volunteering Support Officer for the London and South East region for “Dementia Friends.
I’ve sat through more presentations than you’ve had hot dinners, but the standard of the presentation was excellent. Although the presenter clearly had a corpus of statements to make, the presentation was not contrived at all, and the audience had plenty of opportunity to ask questions at points during the day. The presenter evidently knew what she was doing, and was a very good representative of the Dementia Friends programme. She gave her own ‘Dementia Friends’ session which the group of about twenty found faultless.
Hannah even ran a session after the lunch break on what makes a BAD presentation.
Here are my scrappy notes which I took – and please don’t take this to be representative of the actual discussion of what makes a bad presentation which we had in our group.
I SO wish some of my lecturers (including Readers and Professors) had been to Hannah’s session on generic skills in presentations. Whatever you do after ‘Dementia Friends Champions’ day, there’s no doubt that such a session is really useful across various sectors including law and medicine.
You don’t really have to take notes as it’s all fundamentally in their well laid out handbook.
The day was run with the purpose of not giving you tedious crap on how to run a session. But it was furnished with many useful pointers. For example, I learnt of possible venues such as a local library, church halls, and community centres.
Actually, I have in mind to ask Shahban Aziz, CEO of BPP Students, Prof Peter Crisp (Professor of Law at BPP Law School) and Prof Carl Lygo (also Professor of Law at BPP Law School) whether I might run dementia friend sessions at this law school which I attended for my pre-solicitor training. I’ve always had a bit of a discomfort that lawyers are not really given any introduction to dealing with people with dementia, other than professional regulatory considerations or in direct dealings with the law such as mental capacity? I think it’d be great if law students had a basic working knowledge of what dementias are.
It was nice for me to get out of my flat, and meet a range of people. These people ranged from other people in the third sector, for example the Dementia Action Alliance. They bothered to provide free coffee all day, and a free lunch.
And when I tweeted that on my @legalaware Twitter account from my mobile phone in the lunch break (you’re told to turn your mobiles off for the day), I received this smartarse (#lol) remark from one of my 12000 followers immediately.
You’re given a guidebook. You’re not coerced in any way into becoming a Dementia Friend or Dementia Friend Champion. You’re told specifically having done Dementia Friends you can do whatever point of action you wish, even if that includes supporting another charity other than the Alzheimer’s Society.
You are told that the point of the current dementia strategy in England in no way is intended to be political. In support of that claim is that the current strategy has overwhelming cross-party support.
The sessions include information about dementia and how it affects people, as well as the practical things that can be done to help people with dementia live well in their community.
I was given resources to answer people’s questions about dementia and suggest sources of further information and support.
After completing the course Dementia Friends Champions can access resources and tools to help set up and run sessions for people who sign up as Dementia Friends.
These resources include exercises, quiz sheets, bingo sheets, book club ideas and reading suggestions. You’re made very familiar with the content of ‘Dementia Friends’ as they helpfully provide ALL the material on the website when you sign up. They don’t hold any of it back. The point is you go away and run the whole session as ‘Dementia Friends’. Having seen how the 45 minutes works, I have no burning desire to change any of it.
Having said that, there are one or two things I would do differently, hypothetically. The format makes it very clear the presenter is not an expert in dementia or counsellor. I think this actually helps in that an expert possibly could write an hour long essay on each of the five statements for finals, and get truly bogged down in “paralysis by analysis”.
One of the possible features of the ‘Dementia Friends’ session is comparing dementia to a bookcase. This is a well described metaphor, first proposed by Gemma Jones. I have indeed used it to propose a scheme of explaining ‘sporting memories’, an initiative which recently won the Alzheimer’s Society Dementia Friendly Communities national initiatives awards.
Here’s my pal Tony Jameson-Allen picking up his gong.
There’s a bit in the explanation of the bookcase analogy that gets quite technical in fact.
With the presenter of the session having said that he or she is not an expert in dementia or counsellor, it seems counter-intuitive to me that there is an explanation of the organisation of memory using two highly technical locations in the brain, the hippocampus and amygdala. But things like that are not a ‘deal maker’ or ‘deal breaker’ for me. There’s an excellent video of a presentation of the bookcase analogy by Natalie Rodriguez floating around, in fact, but we were all encouraged to be explain the analogy ‘live’ in our sessions, ‘rather than playing the DVD’.
I have absolutely no problem with the material being pre-scripted. I used to supervise neuroscience and experimental psychology for various colleges at Cambridge between 1997 and 2000 inclusive, and, whilst the guidance for teaching that was not as intense, it’s fair for me to mention that supervisors knew exactly what they had to cover for their students to achieve at least an upper second in finals.
Dementia Friends Champions, like me, are then be encouraged to run Dementia Friends sessions at lunch clubs, educational institutions and other community groups, but it could also include ideas such as arranging a meeting to talk with a small group of friends.
I intend to run five sessions to achieve about 100 further dementia friends. I conceptually find targets anywhere quite odious, and see exactly where this ambition has come from (Japan). On the other hand, nobody is a clairvoyant. The fact the number exists at all (aiming for March 2015) is a testament that this programme is being taken seriously. Had the number been set at 400, then we would all have said ‘job done’ some time ago.
I am actually, rather, amazed that somebody somewhere has signed off for a national programme to invite ordinary members of the public to attend free of charge a day on delivering the Dementia Friends programme, with nice company, and of course that free coffee and lunch.
I am also amazed that the actual substrate of the information sessions for ‘Dementia Friends’ is being offered to the member of the public free of charge, and it effectively has been paid for by Government.
The operational delivery of ‘Dementia Friends Champions’ day was totally faultless from start to finish. Even though I have nothing to do with their output, the Alzheimer’s Society here in England have done a brilliant job with it.
And finally I’ve tended to query whether it can be a genuine ‘social movement’ which so much resource allocation.
But people are genuinely interested in the programme, as these tweets to me demonstrate, I feel:
Look.
There are all sorts of things which do irritate me such as the issue that any dementia awareness should observe boundaries. For example, there are also many global ‘Purple Angels’ motivated by the leadership of Norman McNamara (@norrms), himself living with dementia of diffuse Lewy Body Type.
Here’s their brand new website. Norman is a very good friend of mine, so I’m bound to be loyal to him.
In a different jurisdiction – Australia – a close friend of mine, Kate Swaffer (@KateSwaffer), blogs daily on her busy life living with dementia, which includes being an advocate, travelling, cuisine (Kate is very experienced in sophisticated cooking), a background in healthcare, a student at the University of Wollongong, and what’s it like to live with dementia after being given the diagnosis. Her blog is here.
Chris, Norrms and Kate are all quite different – like the rest of the population – getting on with their lives. And as the very famous adage goes, once you’ve met one person living with dementia, you’ve done exactly done. You’ve met only one person with dementia.
And there’s clearly a huge amount to be done. Also at the Alzheimer Show one carer reported a person with dementia being ‘lost to the system’, completely unknown to anyone for care for three years.
I had a huge volume of concerns about this initiative, and I’m no pushover as far as being ‘in with the in-gang’ is concerned. But I strongly recommend you park your misgivings and go there wanting to be a part of a “change”.
I went on the day after the passing away of the incredible Dr Maya Angelou.
As she said, “If you don’t like something, change it. If you can’t change it, change your attitude.”
If you’re an unpleasant person, a week of ‘dementia awareness’ will make no difference
There’ll be a third of people roughly who’ll hate whatever you do.
There’ll be a third of people roughly who’ll love whatever you do.
There’ll be a third of people roughly who’ll be completely indifferent.
This is advice my father gave to me shortly before he died. In society, there will always be a hardcore group of selfish bastards.
Many people who develop long term conditions in adulthood report how people whom they had considered ‘friends’ suddenly desert them.
They say ‘sayonara’ when times get tough. They are not there for you when it matters.
Sadly, in the real world, with all the best will in the world from policy-makers, there will very many people for whom this becomes an extremely negative experience on receiving a diagnosis of dementia from a clinician.
The shock of receiving that diagnosis can be profound, leading almost for the recipient of the diagnosis to enter the first stage of the Kubler-Ross ‘five stages of grief': denial.
And of course doctors can come to the wrong conclusions especially if the information is slightly incorrect: so in an ideal world, every first diagnosis would be confirmed through a specialist look at the supporting evidence including perhaps further tests.
There has never been a definitive statement that there has been a concomitant increase in resources for services for specialist dementia services for this national policy in increasing dementia diagnostic rates. This is one issue which the All Party Parliamentary Group for dementia under The Baroness Greengross should examine urgently, I feel.
Unfortunately, if ‘friends’ of yours suddenly leave you in droves, you will end up lonely, even if you yourself are a pleasant person.
“I have never felt so lonely” is a very common saying to hear a person living well with dementia saying, even in this age of ‘Dementia Friends’.
So, there’s the rub, schemes such as ‘Dementia Friends’ will make certain people collect a badge for making themselves feel better about having done something superficially for dementia, and think ‘job done’.
But it’s the action which follows which matters. This might include contributing to a dementia charity, with a very small proportion of revenue ultimately going towards research into living well with dementia.
The original Japanese ‘befriending’ scheme meant exactly that. The aim was to ‘befriend’ a person living with dementia, to break down the usual taboos.
So it is not altogether surprising that, if society still shows stigma and discrimination towards people living with dementia, there are some people who might recognise symptoms but prefer to keep schtum.
Keeping schtum might be delaying to see the Doctor, or delaying doing something about the diagnosis, such as having it confirmed elsewhere or telling close friends about it.
In the cost-benefit analysis, telling people about the diagnosis might be accompanied about fears of losing your driving licence (as indeed a person from South London living with vascular dementia told me three days ago at the Alzheimer’s Show). Or it could be accompanied by fears about job prospects. Or it could be accompanied by fears shopping or using a bank.
Whilst I disagree with the name, you can sympathise with the general good intentions of ‘dementia friendly communities’. And perhaps award ceremonies which celebrate good practice, if they break down discrimination and stigma, might help.
Seeing people living well with dementia might help turn around negative perceptions of certain people. This might include Norman McNamara’s infectious ‘Run for the Sun’, the winner in the 2014 Riviera Fringe Festival Anthem Competition. Or it could include Sir Terry Pratchett continuing to produce successful books whilst living with a diagnosis of a type of dementia called posterior cortical atrophy.
But one is immediately cautious about embarking on a route where people living with dementia need to prove they are successful to prove their worth. This is reminiscent of some people from ethnic minorities who had to prove themselves academically and professionally to be accepted. At one extreme, for example, should be welcoming immigrants into this country only if they can contribute something economically to this country? Nigel Farage has often spoken about the engineer from New Zealand being discriminated against compared to perhaps an artisan from a country such as Latvia.
But it is clearly going to be difficult to change direction of a huge ocean liner. One week’s ‘Dementia Awareness’ is necessary but insufficient, possibly. People’s basic knowledge about dementia could be improved with some basic facts – e.g. that it is not part of normal ageing, many people live well with dementia, dementia is not just about memory – as per the ‘Dementia Friends’ campaign from Public Health England delivered by the Alzheimer’s Society.
However, people with dementia often report that they need to be given time and for others to be patient from both professionals and non-professionals. People with dementia often report being rushed in settings ranging from supermarket aisles to acute hospitals. Such a sentiment of feeling rushed more often than not gets tagged onto a feeling of being a burden, and can become profoundly depressing.
When professional shills for raising money into dementia get accompanied by ‘cost’ rather than ‘value’, and when public perception of some in society about people living with dementia can be low, the situation can get worse rather than better.
When we use terms such as ‘dementia friendly communities’, it can engender a feeling of ‘them against us’, and people with dementia become ‘somebody else’s problem’.
Of course, many people are not so pathetic, and such negative generalisations may not be justified with recent successes in raising awareness such as G8dementia or ‘Dementia Friends’.
But we do need to worry as a society if things have not fundamentally changed as a society in perception and identity of people living with dementia. Some people still refuse steadfastly to believe there are some people living well with dementia. It could be the case that people actively avoid talking about the ‘D’ word in much the same way they once avoided the ‘C’ word, and this is reflected in the comparative lack of funds raised for dementia and cancer respectively.
‘Dementia Awareness Week’ is running here from 18-24 May 2012.
If one more person can become a bit more understanding about living with dementia, there are plenty of reasons to be cheerful?
Please support us on Facebook this week.
Deep breaths..
Are individuals living with dementia “recipients” of care?
Language is very important. Only this week, the media was stuffed full of talk of dementia being a ‘horrible disease’, and people ‘suffering’.
A recent Telegraph article cited, “Health Secretary Jeremy Hunt says it is “utterly shocking” that only half of people suffering from dementia are being formally diagnosed.”
Society has a certain image of dementia. It really is no use denying that this image is horribly negative, and feeding on this fear can be low-hanging fruit for raising funds through charity.
In this scheme of thinking, those with the dementia are only viewed through the prism of their illness, and this is often reduced to the image of its last and most tragic phases.
It is as if as soon as a diagnosis of a progressive dementia is made, the person in question, it is perceived by the rest of society, automatically becomes incapable of taking any autonomous decisions, loses his/her personality and identity and immediately needs to be cared for.
In reality, however, this illness can develop quite slowly: between the moment when it is diagnosed and the terminal phase, there may be years of development. Moreover, people living with the illness can rarely have the opportunity to express their thoughts and feelings about it: there is communication about them, but only rarely with them. The individual sadly disappears behind the blanket label of an illness.
The term “suffering”, however, sounds negative, and does not support the concept of “personhood”, and certainly does not fit with a philosophy of “hope” and “wellness”.
The way the NHS has latterly been structured as a market also reinforces this customer-supplier master-servile relationship. Dementia care is a ‘service’ you can pay for, with or without a personal health budget.
The dominant notion itself that the need of people with dementia to socialise should be met by “services” is disempowering, for the concept of service incorporates the notions of “providers” and “recipients”; of the “helpers” and “the helped”, of “us” and them”.
These notions further perpetuate the stigmatising assumption that people with dementia are only able to participate in relationships as “receivers”, and that relating to them is a problem for those who do not have the disease: they further advance the widespread perception that people with dementia are, essentially, a “burden” on their families and society.
This term “burden” can perhaps help validate the ‘burden’ some caregivers experience, but should not be assumed and should be avoided when speaking in generalities such as public presentations.
This language and terminology are in desperate need of change, and the prevailing perception of people past the first stages of dementia as just receivers of care, and users of services, needs drastic reframing.
The truth is that, as the symptoms of the disease progress, people with dementia can still play an active role in society, if provided with support, and this support can very often be provided by fellow citizens, rather than by professionals paid to deliver a service.
The purpose of person-centred language is to recognise the impact of language on thoughts and actions, to ensure language does not diminish the uniqueness and intrinsic value of each person.
Personhood is pivotal. This is the standing or status that is bestowed upon one human being by others in the context of relationship and social being. It implies recognition, respect and trust.
The aim is to create the positive conditions where the person can live without stigma; where people are treated with warmth and authenticity, listened to without judgment and are given opportunity for self-expression.
There are, however, ways to ‘reframe’ this debate.
Framing is a fast developing concept, as much in communication sciences as in other disciplines. This is partly due to the fact that it is a rather flexible approach that lends itself to many applications.
When there is a question relating to knowing how a particular subject is presented, in the media for instance, framing immediately springs to mind.
Instead of painting the illness as a homogenous and unchanging totality, it would be preferable to place the accent on its progressive and developmental nature.
One can put the accent on continuing to be a real person despite the decline due to the illness: acknowledge the personality, the identity and the life journey of those with a progressive dementia.
One can also develop empowerment and social inclusion with people with a progressive dementia. Such individuals are more than passive and dependent consumers of help and care services. They have resources that should be mobilized. The principle of inclusion implies that society is composed of all its citizens. However, this needs competent leadership.
Let those who living with dementia speak. It will provide others with one of the most powerful counter-examples in relation to the current dominant image, which often makes the individual disappear behind his/her illness.
Let your respect for those living with the dementia be obvious in what you have to say.
It is useful also never to forget that people with Alzheimer’s disease also have their own life story, their own personality and character. This is because their long-term memories are relatively preserved, due to a phenomenon first characterised by the French neurologist Ribot in the 1880s. Enable these aspects to be expressed too.
Those who disseminate messages, especially via texts designed to influence people, may deliberately choose a frame that the reader is supposed to pick up and appropriate so as to henceforth view reality in this way.
Given that frames form part of any culture, many of them are common to both the sender and the recipient of a given message.
The question of whether framing is a conscious process remains open to discussion: how far will the writer of a given text deliberately choose a frame that serves his own interests?
As we approach the G8 leading on the subject of what is important in dementia diagnosis, research and care, it is all the more important that we frame the discussion properly.
There are so many stakeholders in English dementia policy, it can be quite uncertain know where the current dementia policy has come from.
David Cameron has often argued that ‘it is not where you’ve come from, it’s where you’re going to’. If one of the goals is destigmatising dementia in society, how we articulate the present debate today is vital to our progress tomorrow.
This means not talking about ‘horrible’ and ‘suffering’ in a way as to encourage ‘moral panic’.
This means treating people with dementia, living at all stages with any particular condition, with the dignity they deserve; this will enormously help carers too.