Home » Posts tagged 'person-centred care'
Tag Archives: person-centred care
Money is tight, but the person remains pivotal in dementia care and support
There’s no question that there is a greater number of people who are old needing to be looked after by care and support services in England.
But dementia is not simply a disease of older people, one of the critical messages of “Dementia Friends”.
Indeed, much of the budget goes into the health and care of younger people, as health technologies, say for treating cardiovascular disease through stents, get better.
The reality is there is pressure on service and the workforce simultaneously in dementia, as the Nuffield Trust and Health Foundation have argued in a sophisticated way.
Earlier in this year, in an article for ETHOS Journal “Living well = greater wellbeing”, I argued a joined up approach would now be needed to deliver a better standard of care and support for people living well with dementia.
In 2010, the UK government became among the first countries to officially monitor people’s psychological and environmental wellbeing. Academic research and policy developments have recently converged upon the notion of ‘living well with dementia’, which transcends any political ideology. This means promoting the quality of life of any person with dementia. It views each person as a unique individual and champions his or her involvement in making decisions whenever possible.
England actually leads the way with the ground-breaking ‘first mover’ exploration by academic Tom Kitwood of ‘personhood’ in the late 1980s: “It is a standing or status that is bestowed upon one human being, by others, in the context of relationship and social being. It implies recognition, respect and trust”.
It’s estimated that there are at least 800,000 people currently living with dementia in the UK. These individuals are likely to come into contact with a number of different people and services in an extensive network including carers (paid and unpaid, including family caregivers), care home staff, transport services, social housing, welfare and benefits and the police to name but a few.
I am, indeed, grateful for Paul Burstow MP’s excellent reply to my article.
The current Government in England has made substantial progress with policy in dementia in my opinion.
The current Care Act (2014) could not be clearer.
In the statutory guidance, the importance of wellbeing is signalled extremely strongly.
It is important for commissioners not to lose sight of this, and not to treat ‘living well with dementia’ not as a slogan but as a reality.
Helping people to live well has been a key aim of the current Government, and I hope future governments, perhaps implementing ‘whole person care’, will retain this strong focus.
Enabling people to live well leads to a fairer society. The value of people living with dementia for society cannot be denied either.
But people in power and influence have a rôle to play.
The Alzheimer’s Society has played its part in addressing stigma and discrimination through its successful ‘Dementia Friends’ campaign. I myself am a “Dementia Friends Champion”, and proud to run my sessions.
One of the key messages in this campaign is that ‘there is more to the person to the dementia’.
This message is currently a critical global one, across many jurisdictions. Here is friend and colleague Kate Swaffer with a huge banner in Australia to the same effect.
And dementia and loneliness already occur together all too often.
The wider community is essential. This is about compassion. It is also about the right people showing the right leadership.
But this should not just simply include household names, although the distress caused by lack of inclusion of people with dementia in high street shops cannot be underestimated.
This community must include all caregivers and professionals.
And central to this recognition of the role of the wider community is a new deal for carers.
As the number of people living with chronic conditions grows rapidly, so does the number of carers. There is a huge army in England currently consisting of selfless individuals giving of themselves to support a loved one.
According to Carers UK, family carers currently save the Government £119 billion every year.
Carers themselves need help.
Carers are invaluable as I discuss here.
And we need to make sure in the next Government that all paid caregivers are given a statutory minimum wage, which could also be a living wage.
We are a society which values footballers more than caregivers for people with dementia. This is simply abhorrent.
I thank the current Government for progress made in this direction, but more has to be done whoever holds office and power next year.
We need collectively to support the Dementia Action Alliance Carers Call to Action. By achieving the shared vision, the aim is to have positive impact on people with dementia and carers and improve their quality of life.
In the Dementia Action Alliance “Carers Call to Action”, carers of people with dementia:
- have recognition of their unique experience – ‘given the character of the illness, people with dementia deserve and need special consideration… that meet their and their caregivers needs’ (World
Alzheimer Report 2013 Journey of Caring are recognised as essential partners in care – valuing their knowledge and the support they provide to enable the person with dementia to live well - have access to expertise in dementia care for personalised information, advice, support and co-ordination of care for the person with dementia
- have assessments and support to identify the on-going and changing needs to maintain their own health and well-being
- have confidence that they are able to access good quality care, support and respite services that are flexible, culturally appropriate, timely and provided by skilled staff for both the carer and the person for whom they care
But we do need some sort of standards, whether aspirational or regulatory, for example?
This situation had become known to Norman Lamb by February 2013:
In light of the recent Stafford Hospital Scandal, an independent review was carried out, underlining irregularities in staff training. According to today’s BBC report, as of March 2015, UK care staff and assistants in care homes, hospitals, and private homes are to be required to complete a training certificate within 12 weeks of starting a new position.
The current UK stance is that there is no minimum standard of training. With over 1million care workers in the country, it came as alarming news to Care Minister, Norman Lamb, to discover that these untrained workers were completing skilled tasks normally undertaken by medical professionals such as taking bloods. He confirmed the responsibility for the certificate would “…rest with employers and I think that’s where the training responsibility should lie.”
I expect the next Government will wish to think about a register for paid carers to help the fight against neglectful care which can tragically happen. It can be hard to achieve a successful prosecution of ‘wilful neglect’, but likewise carers need to be able to do their job with dignity and without fear.
The broad consensus has been for some time “that the principles of person-centred care underpin good practice in the field of dementia care”. Their principles assert:
- the human value of people with dementia, regardless of age or cognitive impairment, and those who care for them
- the individuality of people with dementia, with their unique personality and life experiences among the influences on their response to the dementia
- the importance of the perspective of the person with dementia
- the importance of relationships and interactions with others to the person with dementia, and their potential for promoting well-being.
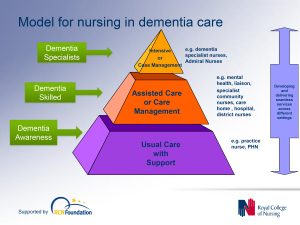
In a presentation called “Developing nursing in dementia care” in May 2014 influential expert Rachel Thompson outlined a “Commitment to the care of people with dementia in hospital settings”, calling for increase in specialist nurse roles –building evidence and supporting leaders.
I believe strongly this need has not gone away. Indeed, it is stronger than ever.
Thompson there mentions the SPACE principles to support good dementia care
Staff who are skilled and have time to care.
Partnership working with carers.
Assessment and early identification of dementia.
Care plans which are person centred and individualised.
Environments that are dementia-friendly.
The financial case for ‘Admiral nurses’, an innovation from Dementia UK, is compelling; see for example the recent report from the University of Southampton Centre for Innovation and Leadership in the Health Sciences.
As is the case from the academic and clinical nursing literature on the importance of proactive case management in avoiding admissions to hospital care.
Claims that nine in ten care homes and hospitals fail to provide the proper treatment are indeed astonishing. That particular Care Quality Commission review found widespread neglect, lack of care, poor training and failings in communication.
In the same way there can be enormous disparity between a ‘bad’ and ‘good’ care home, there can be a subtle difference between a ‘very good’ and a ‘superb’ care home.
We, one day, need to be able to celebrate the ‘outstanding’ in care homes: for example, person-centred activities or environment generally might make all the difference?
The next Government, whoever it is, will need to have the confidence to implement an organic, stakeholder-driven systemic innovation in dementia.
I have long felt that the health and care services need more than a minimum ‘protected funding’. As Roy Lilley, experienced health commentator, remarks, ‘more effort can be put into weighing the pig than actually fattening it’.
This is the danger we run if we do not place adequate resources into service provision and training.
However, even within these domains, I believe that innovation has, potentially, an important and responsible part to play (as indeed I argued in the Health Services Journal this year).
There is no question that money is tight.
But we need also to have a minimum in frontline services to maintain an adequate standard of care, as indeed is supposed to be enforced from the regulation of all clinical professions.
It is easy to jump on a ‘person-centre care’ bandwagon, but all too easily this can turn into selling courses and products for person-centred care.
Putting the person at the heart of how you behave with a person with dementia does not need to cost money. Tom Kitwood articulated it brilliantly.
But, whatever the budget constraints of the health and care and future, I believe personhood should be pivotal for living well with dementia.
This should include the whole person.
If we involve people living with dementia in the design of research and services, I feel, a lot of my concerns will be addressed. The ‘Dementia Without Walls’ project from the Joseph Rowntree Foundation, in collaboration with other stakeholders, has truly been outstanding, for example.
I am grateful to the current Government for taking us a long way down the journey. But we’ve only just begun.
Meeting other people living with posterior cortical atrophy
A dementia is not a natural part of ageing.
Dementia is caused by diseases of the brain.
It’s not just about losing your memory.
It’s possible to live well with dementia.
There’s more to a person than the dementia.
Sue Stephen, one of the founding members of the Dementia Alliance International (DAI), spoke about how she came to be diagnosed with PCA.
This is one of the latest additions on their blog, which I strongly recommend. The DAI is an unique group of individuals with a strong sense of solidarity, who live with one of the various types of dementia.
“I had been noticing myself for the last few years that I was having visual issues… very bad glaring.. when I tried to read..”
She put it down to stress, but she still went ‘to get [my] eyes tested.’
And this went on for a few years. Interestingly, she reports this delay in diagnosis as rather typical for many people finding a diagnosis of PCA.
Tests for dementia of the Alzheimer type, typically initially shown up by problems in short term learning and memory, were negative.
When she was eventually given a diagnosis, she was told, “That’s it. There’s nothing I can do. Here’s a prescription for Aricept. See you in six months.”
But she described being shocked, and she had no idea what PCA is/was.
“I lost all certainty in my life. How do I make decisions in my life?”
She then sat on her month doing ‘research’, but reported ‘three wonderful things’ which came out of her research.
She found a list of symptoms which matched what she had been experiencing. “That was really good”. This enabled her to see her GP who then went referred her onto more suitable specific tests, confirming the diagnosis.
That’s one of the slight paradoxes about the way we approach a fellow citizen of ours living with a dementia. Nobody wants to be defined by any medical conditions they live with. They do not wish (rightly) to consider themselves as a collection of diagnoses.
But it is often reported by people living with conditions how it can be both a blessing to know what might happen but also a burden to know something might happen, with this information resulting from a clinical diagnosis.
She then reported discovering the work of Sir Terry Pratchett, who is living well with PCA, still writing books.
A third thing which she reports is finding a group of people on Facebook of people with posterior cortical atrophy. It’s a closed group where people can share in private “scenarios”.
“I could see in the future what symptoms might be. I look at symptoms, and I think if this happened to me, what could I do now to help?”
Stephen reports sharing these stories really helped.
Terry Pratchett went to see other people living with posterior cortical atrophy in 2010, a form of dementia.
Pratchett is an example of an individual who has shown that it is possible to live well with dementia.
Pratchett admitted he was apprehensive about the meeting, as he said it was like ‘seeing into the future’.
One person in the meeting, “Anything coming through the postbox, I can’t read. Susan has to do everything from cutting my nails to putting my shoes on. This disease.. or whatever you call it, changes your perspective.”
“It didn’t happen – it evolved.”
Pratchett though admitted despite his fears he enjoyed the meeting.
“I can see why people enjoy meeting up”
He had dinner with Graham Doggett, who is an 70 year-old author, and academic who has written books about quantum chemistry, and his wife.
“Susan is the gardener. If I help her, I can never find the wretched branches in the air to prune. They disappear.”
“I was doing computing since 1959. That’s gone.”
“I used to play piano up to grade 7. Gone.”
“Reading, writing, gone gone”.
When the term ‘living well with dementia’, one of the main disclaimers on that is that the person living with one of the dementias will have their life before to compare their experience to.
And this is bound to impact upon one’s own personal perception of living with dementia. Unless you bother to find out about the past of a person, in relation to his environment, you will not be able to understand his or her world.
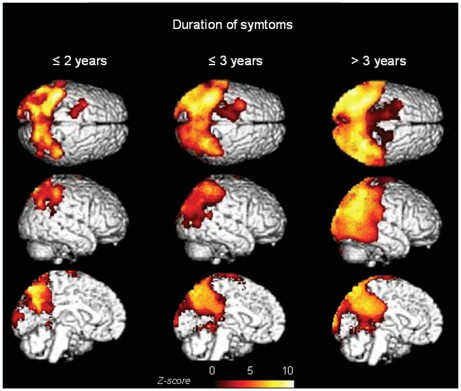
The symptoms of PCA can vary from one person to the next and can change as the condition progresses.
The most common symptoms are consistent with damage to the part of the brain at the back of the head, an area responsible for processing visual information.
Consistent with this process are slowly developing difficulties illustrating its slow and progressive nature due to a disease of the brain.
Now you’re even able to follow it using sophisticated ‘imaging’ of the brain.
These difficulties include visual tasks such as reading a line of text, judging distances, and distinguishing between moving objects and stationary objects.
Other symptoms include an inability to perceive more than one object at a time, disorientation, and difficulty maoneuvering, identifying, and using tools or common objects.
Some people can experience hallucinations.
Yet further symptoms can include difficulty performing mathematical calculations or spelling, and many people with PCA experience anxiety, possibly because they know something is wrong.
In the early stages of PCA, most people do not have markedly reduced memory, but memory can be affected in later stages.
This illustrates how this particular dementia is not just about memory.
Age of onset is typically 50-65, demonstrating why dementia is not simply about ageing.
Both Stephen and Pratchett demonstrate by a country mile while there are more to people than their dementias.
If you’d like to find more about dementia, you can do a short 45 minute session close to where you live in England (and now in other parts of the UK). The initiative is run by the Alzheimer’s Society, but is a Public Health England initiative. To find out more about this initiative called “Dementia Friends”, please go to their website.
There’s more to this initiative than the badge you’ll receive in the process, but this initiative is all about improving understanding in the general population about the dementias. I hope you will wish to learn more.
People with PCA are are at risk of being let down by ‘traditional dementia support groups’.
That is partly because they are younger and face different challenges, and partly because the activities offered in day centres puzzles, large-font books—are visual and thus actively unhelpful for people with PCA.
PCA is not new to the research community.
Already in 1902, the Czech psychiatrist Arnold Pick mentioned a woman’s inability to see and grab a lit candle held in front of her face in his essay “Ueber eine eigenthuemliche sehstoerung senile dementer,” Jahrbuecher f. Psychiatrie u. Neurol., see excerpt.
Several attempts at defining criteria for diagnosis exist.
The neurologist Frank Benson at the University of California, Los Angeles, coined the term while describing the pattern of symptoms in five patients (Benson et al., 1988).
Later, Mario Mendez, also of University of California and San Francisco proposed clinical diagnostic criteria arguing that PCA is its own syndrome, not simply Alzheimer’s disease with visual symptoms (Mendez et al., 2002).
The English dementia strategy is mindful of the needs to develop communities supportive of the needs of people living with PCA, of the need for high quality research research into PCA, and to think how people living with PCA can be best supported professionally and personally.
‘Whole person care’ needs a bit of tinkering and strong leadership
In a now very famous article, “The genius of a tinkerer: the secret of innovation is combining odds and ends”, Steve Johnson describes how innovation must be allowed to succeed in face of regulatory barriers.
“The premise that innovation prospers when ideas can serendipitously connect and recombine with other ideas may seem logical enough, but the strange fact is that a great deal of the past two centuries of legal and folk wisdom about innovation has pursued the exact opposite argument, building walls between ideas”
“Ironically, those walls have been erected with the explicit aim of encouraging innovation. They go by many names: intellectual property, trade secrets, proprietary technology, top-secret R&D labs. But they share a founding assumption: that in the long run, innovation will increase if you put restrictions on the spread of new ideas, because those restrictions will allow the creators to collect large financial rewards from their inventions. And those rewards will then attract other innovators to follow in their path.”
Bundling of goods can offend competition law, so that’s why legislators in a number of jurisdictions are nervous about ‘integrated care’.
In the past, Microsoft has accused of abusing Windows’ dominant status in the desktop operating system market to give Internet Explorer a major advantage in the browser wars.
Microsoft argued bundling Internet Explorer with Windows was just innovation, and it was no longer meaningful to think of Internet Explorer and Windows as separate things, but European authorities disagreed.
There’s no doubt that ultimately ‘whole person care’ will be some form of “person centred care”, where the healthcare needs (as per medical and psychiatric domains currently) are met.
But it is this idea of treating every person as an individual, with a focus on his or her needs in relation to the rest of the community which is the most challenging aspect of whole person care.
Joining up medical and social care with an ‘unified care record’ has never been attempted nationally, but it makes intuitive sense that care information from one institution should be made available to another.
Far too many investigations are needlessly repeated on successive admissions of the same patient, which is exhausting for the person involved. It would make far more sense to have a bank of results of investigations for persons, say who are frail, who are at risk of repeated admissions to acute hospitals in this country.
And this can’t be brought in with the usual haphazard ‘there is no alternative’ and ‘a pause for consultation’ if things go wrong. The introduction of the Health and Social Care Act (2012) and the CareData makes one nervous that lightning will strike a third time.
Labour has had long enough to think about what could go wrong.
Care professions might feel themselves ill-prepared in person-centred care. A range of training needs, from seasoned physicians to seasoned occupational therapists, will have to get themselves oriented towards the notion of a ‘whole person’. This might involve getting to grips with what a person can do as well as what they can’t do.
The BMA will need to be on board, as well as the Royal Colleges. Doctors, nurses, and all allied health professionals will have to double declutch from the view of people as problem lists, and get themselves into a gear about their patients as individuals who happen to be well or ill at the time.
This needs strong leadership, not people proficient at counting beans such that the combined sum total of a PFI loan interest payments and budget for staff doesn’t send a Trust into deficit.
Nor does it mean hitting a 4 hour target, but missing the point as a Trust does many needless admissions as they haven’t in reality fulfilled their basic admissions assessment fully.
For too long, politicians have been stuck in the groove of ‘efficiency savings’, ‘PFI’, ‘four hour waits’, and become totally disinterested in presenting a person-oriented service which looks after people when they are well as well as when they’re ill.
Once ‘whole person care’ finds its feet, with strong leadership and evident peer-support, we can think about how health is dependent on other parts of society working properly, such as housing and transport.
Technology, if this means that a GP could immediately know what a hospital physician has prescribed in real time in an acute admission, could then be worth every penny.
For the last few years, the discussion has centred around alternative ways of paying for healthcare instead of thinking how best to offer professional care to patients and persons.
The fact that this discussion has been led by non-clinicians is patently obvious to any clinician.
Technology also has the ability to predict, say in thirty years, which of the population is most likely to develop Alzheimer’s disease. Do you really want one of your fellow countrymen to have health insurance premiums at sky high because of having been born with this genetic make-up?
A lot of our problems, like the need for compassion, have been as a result of the 6Cs battling head-on with a 7th C – “cuts”. It’s impossible for our workforce to perform well if they haven’t got the correct tools for the job.
Above all, whole person care needs strong leadership, not just management. And if we get it right the NHS will be less focused on what it’s exporting, but more focused on stuff of real importance.
Are individuals living with dementia “recipients” of care?
Language is very important. Only this week, the media was stuffed full of talk of dementia being a ‘horrible disease’, and people ‘suffering’.
A recent Telegraph article cited, “Health Secretary Jeremy Hunt says it is “utterly shocking” that only half of people suffering from dementia are being formally diagnosed.”
Society has a certain image of dementia. It really is no use denying that this image is horribly negative, and feeding on this fear can be low-hanging fruit for raising funds through charity.
In this scheme of thinking, those with the dementia are only viewed through the prism of their illness, and this is often reduced to the image of its last and most tragic phases.
It is as if as soon as a diagnosis of a progressive dementia is made, the person in question, it is perceived by the rest of society, automatically becomes incapable of taking any autonomous decisions, loses his/her personality and identity and immediately needs to be cared for.
In reality, however, this illness can develop quite slowly: between the moment when it is diagnosed and the terminal phase, there may be years of development. Moreover, people living with the illness can rarely have the opportunity to express their thoughts and feelings about it: there is communication about them, but only rarely with them. The individual sadly disappears behind the blanket label of an illness.
The term “suffering”, however, sounds negative, and does not support the concept of “personhood”, and certainly does not fit with a philosophy of “hope” and “wellness”.
The way the NHS has latterly been structured as a market also reinforces this customer-supplier master-servile relationship. Dementia care is a ‘service’ you can pay for, with or without a personal health budget.
The dominant notion itself that the need of people with dementia to socialise should be met by “services” is disempowering, for the concept of service incorporates the notions of “providers” and “recipients”; of the “helpers” and “the helped”, of “us” and them”.
These notions further perpetuate the stigmatising assumption that people with dementia are only able to participate in relationships as “receivers”, and that relating to them is a problem for those who do not have the disease: they further advance the widespread perception that people with dementia are, essentially, a “burden” on their families and society.
This term “burden” can perhaps help validate the ‘burden’ some caregivers experience, but should not be assumed and should be avoided when speaking in generalities such as public presentations.
This language and terminology are in desperate need of change, and the prevailing perception of people past the first stages of dementia as just receivers of care, and users of services, needs drastic reframing.
The truth is that, as the symptoms of the disease progress, people with dementia can still play an active role in society, if provided with support, and this support can very often be provided by fellow citizens, rather than by professionals paid to deliver a service.
The purpose of person-centred language is to recognise the impact of language on thoughts and actions, to ensure language does not diminish the uniqueness and intrinsic value of each person.
Personhood is pivotal. This is the standing or status that is bestowed upon one human being by others in the context of relationship and social being. It implies recognition, respect and trust.
The aim is to create the positive conditions where the person can live without stigma; where people are treated with warmth and authenticity, listened to without judgment and are given opportunity for self-expression.
There are, however, ways to ‘reframe’ this debate.
Framing is a fast developing concept, as much in communication sciences as in other disciplines. This is partly due to the fact that it is a rather flexible approach that lends itself to many applications.
When there is a question relating to knowing how a particular subject is presented, in the media for instance, framing immediately springs to mind.
Instead of painting the illness as a homogenous and unchanging totality, it would be preferable to place the accent on its progressive and developmental nature.
One can put the accent on continuing to be a real person despite the decline due to the illness: acknowledge the personality, the identity and the life journey of those with a progressive dementia.
One can also develop empowerment and social inclusion with people with a progressive dementia. Such individuals are more than passive and dependent consumers of help and care services. They have resources that should be mobilized. The principle of inclusion implies that society is composed of all its citizens. However, this needs competent leadership.
Let those who living with dementia speak. It will provide others with one of the most powerful counter-examples in relation to the current dominant image, which often makes the individual disappear behind his/her illness.
Let your respect for those living with the dementia be obvious in what you have to say.
It is useful also never to forget that people with Alzheimer’s disease also have their own life story, their own personality and character. This is because their long-term memories are relatively preserved, due to a phenomenon first characterised by the French neurologist Ribot in the 1880s. Enable these aspects to be expressed too.
Those who disseminate messages, especially via texts designed to influence people, may deliberately choose a frame that the reader is supposed to pick up and appropriate so as to henceforth view reality in this way.
Given that frames form part of any culture, many of them are common to both the sender and the recipient of a given message.
The question of whether framing is a conscious process remains open to discussion: how far will the writer of a given text deliberately choose a frame that serves his own interests?
As we approach the G8 leading on the subject of what is important in dementia diagnosis, research and care, it is all the more important that we frame the discussion properly.
There are so many stakeholders in English dementia policy, it can be quite uncertain know where the current dementia policy has come from.
David Cameron has often argued that ‘it is not where you’ve come from, it’s where you’re going to’. If one of the goals is destigmatising dementia in society, how we articulate the present debate today is vital to our progress tomorrow.
This means not talking about ‘horrible’ and ‘suffering’ in a way as to encourage ‘moral panic’.
This means treating people with dementia, living at all stages with any particular condition, with the dignity they deserve; this will enormously help carers too.
The English dementia policy: some personal thoughts
The last few years have seen a much welcome progression, for the better, for dementia policy in England. This has been the result of the previous Government, under which “Living well with dementia: the National Dementia Strategy” was published in 2009, and the current Government, in which the Prime Minister’s Dementia Challenge in 2012 was introduced.
Dementia is a condition which lends itself to the ‘whole person’, ‘integrated’ approach. It is not an unusual for an individual with dementia to be involved with people from the medical profession, including GPs, neurologists, geriatricians; allied health professionals, including nurses, health care assistants, physiotherapists, speech and language specialists, nutritionists or dieticians, and occupational therapists; and people in other professionals, such as ‘dementia advocates’ and lawyers. I think a lot can be done to help individuals with dementia ‘to live well'; in fact I have just finished a big book on it and you can read drafts of the introduction and conclusion here.
It is obviously critical that clinicians, especially the people likeliest to make the initial provisional diagnosis, should be in the ‘driving seat’, but it is also very important that patients, carers, family members, or other advocates are in that driving seat too. I feel this especially now, given that there is so much information available from people directly involved in with patients (such as @bethyb1886 or @whoseshoes or @dragonmisery) This patient journey is inevitably long, and to call it a ‘rollercoaster ride‘ would be a true understatement. That is why language is remarkably important, and that people with some knowledge of medicine get involved in articulating this debate. Not everyone with power and influence in dementia has a detailed knowledge of it, sadly.
I am very honoured to have my paper on the behavioural variant of frontotemporal dementia to be included as one of a handful of references in the current Oxford Textbook of Medicine. You can view this chapter, provided you do not use it for commercial gain (!), here.
I should like to direct you to the current draft of a video by Prof Alistair Burns, Chair of Psychiatry at the University of Manchester, who is the current National Clinical Lead for Dementia. You can contact him over any aspects of dementia policy on his Twitter, @ABurns1907. I strongly support Prof Burns, and here is his kind Tweet to me about my work. I agree with Prof Burns that once individuals can be given face-to-face a correct diagnosis of dementia this allows them to plan for the future, and to access appropriate services. The problem obviously comes from how clinicians arrive at that diagnosis.
I am not a clinician, although I studied medicine at Cambridge and did my PhD on dementia there too, but having written a number of reviews, book chapters, original papers, and now a book on dementia, I am deeply involved with the dementia world. I am still invited to international conferences, and I personally do not have any financial vested interests (e.g. funding, I do not work for a charity, hospital, or university, etc.) That is why I hope I can be frank about this. Clinicians will be mindful of the tragedy of telling somebody he or she has dementia or when he or she hasn’t, but needs help for severe anxiety, depression, underactive thyroid, or whatever. But likewise, we are faced with reports of a substantial underdiagnosis of dementia, for which a number of reasons could be postulated. Asking questions such as “How good is your memory?” may be a good basic initial question, but clinicians will be mindful that this test will suffer from poor specificity – there could be a lot of false positives due to other conditions.
At the end of the day, a mechanism such as ‘payment-by-results’ can only work if used responsibly, and does not create an environment for ‘perverse incentives’ where Trusts will be more inclined to claim for people with a ‘label’ of dementia when they actually do not have the condition at all. A double tragedy would be if these individuals had poor access to care which Prof Burns admits is “patchy”. In my own paper, with over 300 citations, on frontal dementia, seven out of eight patients had very good memory, and yet had a reliable diagnosis of early frontal dementia. Prof Burns rightly argues the term ‘timely’ should be used in preference to ‘early’ dementia, but still some influential stakeholders are using the term ‘early’ annoyingly. On the other hand, I wholeheartedly agree that the term ‘timely’ is much more fitting with the “person-centred care” approach, made popular in a widespread way by Tom Kitwood.
I am still really enthused about the substantial progress which has been made in English dementia policy. I enclose Prof Burns’ latest update (draft), and the video I recorded yesterday at my law school, for completion.
Prof Alistair Burns, National Clinical Lead for Dementia
Me (nobody) in reply
Avoiding the rollercoaster: a policy for dementia must be responsible
The last few years have seen a much welcome progression, for the better, for dementia policy in England. This has been the result of the previous Government, under which “Living well with dementia: the National Dementia Strategy” was published in 2009, and the current Government, in which the Prime Minister’s Dementia Challenge in 2012 was introduced.
Dementia is a condition which lends itself to the ‘whole person’, ‘integrated’ approach. It is not an unusual for an individual with dementia to be involved with people from the medical profession, including GPs, neurologists, geriatricians; allied health professionals, including nurses, health care assistants, physiotherapists, speech and language specialists, nutritionists or dieticians, and occupational therapists; and people in other professionals, such as ‘dementia advocates’ and lawyers. I think a lot can be done to help individuals with dementia ‘to live well'; in fact I have just finished a big book on it and you can read drafts of the introduction and conclusion here.
It is critical obviously that clinicians, especially the people likeliest to make the initial provisional diagnosis, should be in the ‘driving seat’, but it is also very important that patients, carers, family members, or other advocates are in that driving seat too. I feel this especially now, given that there is so much information available from people directly involved in with patients (such as @bethyb1886 or @whoseshoes or @dragonmisery) This patient journey is inevitably long, and to call it a ‘rollercoaster ride‘ would be a true understatement. That is why language is remarkably important, and that people with some knowledge of medicine get involved in articulating this debate. Not everyone with power and influence in dementia has a detailed knowledge of it, sadly.
I am very honoured to have my paper on the behavioural variant of frontotemporal dementia to be included as one of a handful of references in the current Oxford Textbook of Medicine. You can view this chapter, provided you do not use it for commercial gain (!), here.
I should like to direct you to the current draft of a video by Prof Alistair Burns, Chair of Psychiatry at the University of Manchester, who is the current National Clinical Lead for Dementia. You can contact him over any aspects of dementia policy on his Twitter, @ABurns1907. I strongly support Prof Burns, and here is his kind Tweet to me about my work. I agree with Prof Burns that once individuals can be given face-to-face a correct diagnosis of dementia this allows them to plan for the future, and to access appropriate services. The problem obviously comes from how clinicians arrive at that diagnosis.
I am not a clinician, although I studied medicine at Cambridge and did my PhD on dementia there too, but having written a number of reviews, book chapters, original papers, and now a book on dementia, I am deeply involved with the dementia world. I am still invited to international conferences, and I personally do not have any financial vested interests (e.g. funding, I do not work for a charity, hospital, or university, etc.) That is why I hope I can be frank about this. Clinicians will be mindful of the tragedy of telling somebody he or she has dementia or when he or she hasn’t, but needs help for severe anxiety, depression, underactive thyroid, or whatever. But likewise, we are faced with reports of a substantial underdiagnosis of dementia, for which a number of reasons could be postulated. Asking questions such as “How good is your memory?” may be a good basic initial question, but clinicians will be mindful that this test will suffer from poor specificity – there could be a lot of false positives due to other conditions.
At the end of the day, a mechanism such as ‘payment-by-results’ can only work if used responsibly, and does not create an environment for ‘perverse incentives’ where Trusts will be more inclined to claim for people with a ‘label’ of dementia when they actually do not have the condition at all. A double tragedy would be if these individuals had poor access to care which Prof Burns admits is “patchy”. In my own paper, with over 300 citations, on frontal dementia, seven out of eight patients had very good memory, and yet had a reliable diagnosis of early frontal dementia. Prof Burns rightly argues the term ‘timely’ should be used in preference to ‘early’ dementia, but still some influential stakeholders are using the term ‘early’ annoyingly. On the other hand, I wholeheartedly agree that the term ‘timely’ is much more fitting with the “person-centred care” approach, made popular in a widespread way by Tom Kitwood.
I am still really enthused about the substantial progress which has been made in English dementia policy. I enclose Prof Burns’ latest update (draft), and the video I recorded yesterday at my law school, for completion.
Prof Alistair Burns, National Clinical Lead for Dementia
Me (nobody) in reply
Andy Burnham’s “whole-person care” could be visionary, or it could be “motherhood and apple pie”
“Whole-Person Care” was at the heart of the proposal at the heart of Labour’s health and care policy review, formally launched yesterday, and presents a formidable task: a new “Burnham Challenge”?
It is described as follows:
“Whole-Person Care is a vision for a truly integrated service not just battling disease and infirmity but able to aspire to give all people a complete state of physical, mental and social well-being. A people-centred service which starts with people’s lives, their hopes and dreams, and builds out from there, strengthening and extending the NHS in the 21st century not whittling it away.” (more…)