Home » Posts tagged 'Keogh report'
Tag Archives: Keogh report
Keogh: Is the solution to failed outsourcing more failed outsourcing?
Sir Bruce Keogh has published a report on the first stage of his review of urgent and emergency care in England. You can read more about the review as it progresses on NHS Choices.
There are various potential causes of the current A&E problems. One reason might be that many people anecdotally seem to have trouble in getting a ‘routine’ GP appointment.
Labour says the crisis has been made worse by job cuts under this Government — such as the loss of 6,000 nursing posts since the election, and decisions to axe NHS Direct and close walk-in centres.
Sir Bruce says the current system is under “intense, growing and unsustainable pressure”. This is driven by rising demand from a population that is getting older, a confusing and inconsistent array of services outside hospital, and high public trust in the A&E brand.
Invariably, the response, from either those of are of a political inclination, or uneducated about macroeconomics, or both, is that “we cannot afford it”. This is dressed up as “sustainability”, but the actual macroeconomic definition of sustainability is being bastardised for that purpose.
Unite, which has 100,000 members in the health service, said this year that it wanted the “Pay Review Body” to “grasp the nettle” of declining living standards of NHS staff. “The idea behind the flat rate increase is that the rise in the price of a loaf of bread is the same whether you are a trust chief executive or a cleaner. Why should the CEO get a pay increase of more than ten times that of the cleaner, as would be the case if you have a percentage increase,” said Unite head of health Rachael Maskell.
According to one recent report, the boss of a failing NHS trust was awarded a £30,000 pay rise as patients were deprived of fluids and forced to wait in a car park because A&E was full. Karen Jackson, chief executive of Northern Lincolnshire and Goole Hospitals NHS Foundation Trust, is reported to have accepted a 20% increase last year, taking her salary from £140,000 to £170,000.
Even if you refute that the global financial crash was due to failure of the investment banking sector, it’s impossible to deny that the current economic recovery is not being ‘felt’ by many. Indeed, some City law firms have unashamedly reported record revenues in recent years. Many well-known multi-national companies have yet further managed to avoid paying corporation tax in this jurisdiction.
Sir Bruce Keogh has himself admitted that extra money and “outsourcing” of some services to the private sector will be used to attempt to head off an immediate crisis, but will say the whole system of health care needs to be redesigned to meet growing long-term pressures.
This is on top of an estimated £3bn reorganisation of the NHS which the current Government has denied is ‘top down'; in their words, it is a ‘devolving’ reorganisation; similar to how the ‘bedroom tax’ should be a ‘spare room subsidy’ according to the Government and the BBC.
A poet who uses language far better than either the current Coalition or the BBC is Samuel Taylor-Coleridge. One of his poems, “The Rime of the Ancient Mariner”, relates the experiences of a sailor who has returned from a long sea voyage.
The poet uses narrative techniques such as repetition to create a sense of danger, the supernatural, or serenity, depending on the mood in different parts of the poem.
Water, water, every where,
And all the boards did shrink;
Water, water, every where,
Nor any drop to drink.
Like the manner of this poem, the mood of the NHS changes with the repetition of certain language triggers such as ‘sustainability’.
More than £4bn of taxpayer funds was paid out last year to four of Britain’s largest outsourcing contractors – Serco, Capita, Atos and G4s – prompting concerns that controversial firms have become too big to fail, according to the National Audit Office.
But according to the National Audit Office, increasingly powerful outsourcing companies should be forced to open their books on taxpayer-funded contracts, and be subject to fines and bans from future contracts in the event that they are found to have fallen short. The report estimates that the four groups together made worldwide profits of £1.05bn, but paid between £75m and £81m in UK corporation tax. Atos and G4S are thought to have paid no tax at all.
“[This report] raises some big concerns: the quasi-monopolies that have sprung up in some parts of the public sector; the lack of transparency over profits, performance and tax paid; the inhibiting of whistleblowers; the length of contracts that taxpayers are being tied into; and the number of contracts that are not subject to proper competition,” said Margaret Hodge, chair of the public accounts committee, who commissioned the NAO to carry out the study.
As for the NHS, Keogh describes it as ‘complete nonsense’ that his proposals are a ‘downgrading’ or ‘two tier system’. As an example, Keogh says there has been 20% increased survival rate in major trauma by treatment in a specialist treatment on the basis of his 25 designated trauma centres. Keogh’s focus is on major trauma, stroke or heart attack.
This is a perfectly reasonable observation, in the same way that the existence of the tertiary referral medicine centres for clinical medicine, such as the Brompton, the Royal Marsden or Queen Square, for highly specialist medical management of respiratory, palliative and neurological medicine should not be interpreted as the NHS Foundation Trust ‘tier’ offering a second-rate service on rare conditions. Developed after an extensive engagement exercise, the new report proposes a new blueprint for local services across the country that aims to make care more responsive and personal for patients, as well as deliver even better clinical outcomes and enhanced safety.
Keogh advocates a system-wide transformation over the next three to five years, saying this is “the only way to create a sustainable solution and ensure future generations can have peace of mind that, when the unexpected happens, the NHS will still provide a rapid, high quality and responsive service free at the point of need.”
But it is highly significant that this ‘beefed up system’ is building on the rocky foundation for the NHS since May 2010, where the Coalition has ‘liberalised the market’. Far from giving the NHS certainty, the Health and Social Care Act (2012), as had been widely anticipated, has liberated anarchy and chaos.
There are many more private providers delivering profit for their shareholders.
However, the National Health Service has been propelled at high speed into a fragmented, disjointed service with numerous providers not sharing critical information with each other let alone the public.
Only this week, Grahame Morris, Labour MP for Easington, warned yet again about how private providers are able to hide behind the ‘commercial sensitivity’ corporate veil when it comes to freedom of information act requests. This wouldn’t be so significant if it were not for the fact that ‘beefing up’ the NHS 111 system is such a big part of Keogh’s plan.
NHS 111 was launched in a limited number of regions in March 2013 ahead of a planned national launch in April 2013. This initial launch was widely reported to be a failure. Prior to the launch the British Medical Association – affectionately referred to by the BBC as “The Doctors’ Union” – had sufficient concern to write to the Secretary of State for Health requesting that the launch be postponed. On its introduction, the service was unable to cope with demand; technical failures and inadequate staffing levels led to severe delays in response (up to 5 hours), resulting in high levels of use of alternative services such as ambulances and emergency departments. The public sector trade union UNISON had also recommended delaying the full launch.
The service has run by different organisations in different parts of the country, with private companies, local ambulance services and NHS Direct, which used to operate the national non-emergency phone line, all taking on contracts last year. The problems led to the planned launch date being abandoned in South West England, London and Midlands (England). In Worcestershire, the service was suspended one month after its launch in order to prevent patient safety being compromised. The 111 non-emergency service has faced criticism since a trial was launched in parts of England last month. Some callers said they had struggled to get through or left on hold for hours.
Andy Burnham, Labour’s shadow health secretary, at the time accused the Government of destroying NHS Direct, “a trusted, national service” in an “act of vandalism”. “It has been broken up into 46 cut-price contracts,” he said. “Computers have replaced nurses and too often the computer says ‘go to A&E’.”
Clare Gerada, also at the time, said that the introduction of 111 had “destabilised” a system that was functioning well under NHS Direct and called for non-emergency phone services to be operated in closer collaboration with local GP services.
“The big problem about 111 is of course money,” she said. “It was the lowest bidders on the whole that won the contracts… If you pay £7 a call versus £20 a call you don’t have to be an economist to see that something’s going to be sacrificed. What’s sacrificed is clinical acumen.”
Keogh is keen to put a different gloss on the situation now. He admits that people wish to talk to clinician if they are worried, rather than an “unqualified call handler”. He says that this is possible ‘but we need to put the infomatics in place’. 40% of patients need reassurance, according to Keogh. Keogh then argues that, if there is a concern, an ambulance can be called up, or a GP appointment can be arranged.
However, for this system to work, people offering out-of-hours services will not just be dealing with a third degree burn in the absence of any previous medical history at all. There will be patients with long-term conditions like diabetes, asthma and chronic heart disease, who might not have to use A&E services so frequently if they were supported to manage their health more effectively.
Some of these patients will be ‘fat filers’, where it’s impossible to know what a medical presentation might be without access to complex medical notes; e.g. a cold in a profoundly immunosuppressed individual is an altogether different affair to a cold in a healthy individual. Likewise, individuals with specific social care needs will need to be recognised in any out-of-hours service.
The aim of ‘beefing up’, as Keogh puts it, the ‘National Health Service’ was to make it a coherent service across all disciplines, with clinicians – as well as top CEOs – adequately resourced out of general taxation.
As it is, it is pouring more money into people who have not delivered the goods thus far.
The solution to failed outsourcing cannot be more failed outsourcing. As one interesting article in ‘Computer Weekly’ explained recently, the “NHS 111 chaos is a warning to organisations outsourcing”.
The report has also made a case for improved training and investment in community and ambulance services, so that paramedics provide more help at the scene of an incident, with nurses and care workers dispatched to offer support in the home, so fewer patients are taken to hospital. This can work extremely well, provided that resources are allocated to such services first, and there is a proven improvement in quality (which seems very likely.)
And if somebody tells you it’s all about sustainability – tell them there’s water water everywhere, and there’s not a drop to drink as this recent event provoked.
To deny the need for safe nursing staffing levels is to defend the indefensible
 Later today, a review of patient safety in the NHS by an acclaimed US expert, Don Berwick, is expected to recommend minimum staffing levels for hospitals, a “zero harm culture“, regulation of health care assistants (HCAs), and a “legal duty of candour ” for NHS entities and/or staff within them to admit their mistakes. The Berwick review will be published around 11 am for journalists and ‘interested parties’, and 3.30 pm for everyone else, it is anticipated. A “zero harm culture” is a reasonable policy goal, but there has to be a safe number of pilots and cabin crew to make the plane fly safely, and you have to check there’s enough fuel in the tank.
Later today, a review of patient safety in the NHS by an acclaimed US expert, Don Berwick, is expected to recommend minimum staffing levels for hospitals, a “zero harm culture“, regulation of health care assistants (HCAs), and a “legal duty of candour ” for NHS entities and/or staff within them to admit their mistakes. The Berwick review will be published around 11 am for journalists and ‘interested parties’, and 3.30 pm for everyone else, it is anticipated. A “zero harm culture” is a reasonable policy goal, but there has to be a safe number of pilots and cabin crew to make the plane fly safely, and you have to check there’s enough fuel in the tank.
On the publication of the recent Francis report, David Cameron said:
“The Government has so far resisted calls to introduce mandatory staff ratios for hospitals in the wake of the Mid Staffordshire scandal arguing that it would not necessarily improve patient care and could lead to organisations seeking to achieve staffing levels only at the minimum level.”
One of the most horrific things I have watched in the last few months is the undignified spectacle of campaigners ‘at each other’s throats’, discussing the issue of patient safety. Forgetting for a moment the well known indecency of the Care Quality Commission having given clinical departments a ‘clean bill of health’ before a disaster happened, the way in which some campaigners have avoided the need for a safe nursing staff level has truly offended me. In part, this is due to the fact that some campaigners are blatantly political. However, this has been to conflate an objective discussion of patient safety with a need for party loyalty which has completely not discussed the need for safe nursing levels. Any senior nurse or Sister will tell you about the ‘How many registered experienced nurses do I have on duty for this shift?” test question before nurses start their 2 pm – 9 pm shift, for example. Cutting nursing numbers makes the atmosphere for the nurses who are left turn from providing quality care for which they have trained to do into a method of ‘firefighting’, with an attitude of ‘I hope nothing goes wrong on my watch.” It is all very well for management consultants from outside of the profession to bleat on about ‘compassion’, and indeed this is low hanging fruit given the almost ubiquitous desire for compassion from the caring services, and an under-resourced service will have its consequences. The usual criticism of this argument is ‘there’s no excuse for lack of compassion’, but indeed in a well resourced National Health Service, this should not even be an issue. But it is – particularly as NHS Trusts locally implement ‘McKinsey efficiency savings’. It is easy to demonstrate financial solvency in the balance sheet, but it is possibly easier for Trusts to hide substandard care in both mortality and morbidity, which is why there is such a need for accurate data without the horrific shroud-waving we have seen in recent weeks.
It can’t simply be a question of the “numbers”, “stupid”. It is methodologically tricky to make cross-comparisons between hospitals, especially across a number of different jurisdictions with varying emphasis on private healthcare provision. Differences may be caused not by the staffing level of nurses per se, but by other unmeasured factors associated with higher levels of staffing by registered nurses or other unmeasured characteristics of the hospitals’ nursing workforce, such as proven competence in that particular specialty. The level of staffing by nurses is an incomplete measure of the quality of nursing care in hospitals. Other factors, such as effective communication between nurses and physicians and a positive work environment, have been found to influence patients’ outcomes. For example, the quality of “hand over” in nurses from shift to shift may have a bearing on whether clinical issues are picked up upon, e.g. a particular patient is getting ‘sicker’ and requires more frequent clinical observations; or simply that a patient’s CT scan of the thorax has been postponed for a fourth day in a row?
Politicians generally are not clinicians putting aside for a moment the rather rare cases of Dr Dan Poulter or Lord David Owen, and so can, generally, only be blamed for things which fall under their jurisdiction (or things which do not fall under their jurisdiction, as Justice Silber explained to the Secretary of State last week.) The Government has been criticised for presiding over cuts to nursing posts at a time of increasing concern over patient safety in NHS hospitals. Nearly 5,000 nursing places have been cut since the Coalition took power in 2010, with 800 lost in April this year alone. While NHS England plan to recruit more than 4,100 new nurses next year – a 2 percent increase – the health sector’s own economic regulator, Monitor, said last month that the recruitment drive was a “short-term fix” and will be followed by a further 4 per cent cut to nursing posts over 2014-15 and 2015-16. It has been argued that each ward is different, with a different case mix and layout, and staffing levels should therefore be locally determined. It has also been argued that if authorities set a local staffing levels the “floor” will soon become the “ceiling” and it will not be long before all hospitals plummet towards the bargain basement. This is where who provides the healthcare service does become relevant, in contradistinction to the Tony Blair dictum, which I have previously discussed on this blog. A private healthcare provider, even a NHS Trust which is funded through the PFI initiative, is able to hide staffing employment data on the grounds that this information is “commercially sensitive”.
The Nursing Times “Speak out safely” campaign has also been at the forefront of calling for a culture where the concerns of staff are valued and taken seriously. Also, the “Safe Staffing Alliance“, which includes the Royal College of Nursing, Unison, the Patients’ Association and the directors of nursing at a number of English hospitals, has campaigned for national minimum staffing levels since its foundation last year. The “Safe Staffing Alliance” is made up of NHS directors of nursing, senior healthcare academics, leaders of professional organisations and the Patients Associatiobm and oints to the current variation in staffing levels. Recent research by King’s College London shows that in some NHS hospitals registered nurses will provide care to an average of five named patients during a shift, while in other hospitals nurses have up to 11 patients to care for. Research has found considerable variation between and within hospitals even when specialty and patient dependency are taken into account.
- Registered nurse staffing levels vary considerably in English hospitals. In some National Health Service (NHS) hospitals registered nurses will provide care to an average of five named patients during a shift, whilst in other hospitals nurses have up to 11 patients to care for. Whilst a degree of variation in staffing between units is expected and necessary because of differences in patient needs and the type of care provided, research has found considerable variation between and within hospitals even when speciality and patient dependency are controlled for.
- Some wards can be well-staffed while other wards are dangerously understaffed. When the numbers are added up across a hospital the overall staffing levels can appear to be adequate. Planning safe nurse staffing levels is a recognised problem in many countries, including the US, Belgium, China, Korea and the UK. Care Quality Commission reports consistently warn that quality and staffing vary considerably within NHS hospitals.
- Neglected care (or care not done because of time pressures) is correlated to low registered nurse staffing levels on a ward. There are more errors in care, failure to rescue increases, and care is more likely to be ‘left undone’ when there are fewer registered nurses on a ward.
- Understaffing has cost implications for hospitals. Emergency admissions are higher where there are fewer registered nurses and nurses are likely to suffer more injuries and stress, exacerbating staffing problems and costs.
- Some specialties – such as older people’s care – typically suffer lower staffing levels and more dilute skill-mix. 50% of the nursing workforce caring for older people is made up of care assistants who are not trained nurses.
From “Registered Nurse staffing levels and patient outcomes: Overview of research evidence” published by the NNRU, King’s College London February 2013.
Even Robert Francis QC revisited the explosive issue of staffing levels last week:
However, during a public appearance last week, Mr Francis said he had seen evidence from the Safe Staffing Alliance – a confederation of nursing and patient groups set up earlier this year – that had convinced him the issue should be revisited.
Mr Francis stated: “It’s evidence… [that] ought to be considered with regard to whether there is some sort of benchmark, which at least is a bit like a mortality rates – an alarm bell which should require at least questions to be asked about whether it is possible for a service to be safe.”
He stressed the level should not be viewed as “the adequate level of staffing, but the level below which you cannot be safe”.
The ‘hospital standardised mortality ratio‘ as the warning trigger is for mortality, so clearly pretty distal in the chain of events, very blatantly. Francis has called for simple effective measures which are simple, meaningful, and for breaches against which can be sanctioned. His discussion of this issue of objective findings of poor staffing levels, in this context, is about 55 minutes in when you play this video:
Benchmarking can be a useful tool, but if used at an aggregated trust level it can mask underlying risks. Many directors of nursing have witnessed turnaround teams who suggest staffing can be reduced, on the basis of a comparative overall trust nurse-to-bed ratio. However, the recently published Keogh mortality report identified low nursing levels in many of the trusts they investigated (see my previous blogpost). The tragedy is that minimum safe staffing levels were recommended six months ago by Robert Francis in the report on Mid Staffs. However, the Government is yet to introduce a national standard for nurse to patient ratios, despite constant warnings from medical professionals.
Another campaign has been set up to lobby government to introduce a mandatory minimum staffing ratio of four patients to each registered nurse. It is reported in Nursing Times that:
Members of the 4:1 Campaign said they were “acutely aware of the pressures experienced by staff everyday through understaffing and the negative consequences this has on direct patient care and experience”.
“We believe a mandatory minimum staffing ratio of 4:1 should be introduced by the government to ensure that patients are cared for safely and effectively,” they state in a letter to Nursing Times.
“Research articulating the link between high patient-nurse ratios and poor patient health outcomes is strong and the experience of 1:4 ratios from California and the Australian state of Victoria demonstrate the immense benefits to patients and hospital staff where mandatory staffing ratios have been implemented.”
Further research in this jurisdiction is needed to refine the measurement of the nursing case mix on the basis of discharge data, and to elucidate the factors influencing the staffing levels of nurses and the mix of nursing personnel in hospitals. Given the evidence that such staffing levels are associated with adverse outcomes, as well as the current and projected shortages of hospital-based registered nurses, systems could be developed for the routine monitoring of hospital outcomes that are sensitive to levels of staffing by nurses. Beyond monitoring, hospital administrators, accrediting agencies, insurers, and regulators should take action to ensure that an adequate nursing staff is available to protect patients and to improve the quality of care. The professional regulatory bodies, such as the General Medical Council and the Nursing Midwifery Council, have not found themselves deliberating on wider matters of insufficient resource allocation, unless they happened to be effected by clinicians holding professional registration. Other clinical regulatory bodies might be more effective in regulating this particular domain, which clearly impacts upon the ‘quality’ of clinical care.
 Since earlier this year, UNISON, the UK’s largest health union, has been challenging the government over its refusal to implement what is potentially an important recommendation in the Francis Report – the introduction of minimum staff to patient ratios. Most professionals believe that this simple intervention would provide safer, more caring environment for all. That call had been backed by a new survey from the union of more than 1,500 nurses, midwives and healthcare assistants, which shows that 45% of respondents are looking after eight or more patients on their shift. Research shows that looking after this number increases the risk of patient harm. While in political circles, we have heard a lot from the hedge funds and private equity funds about liberalising the economic activity in the NHS, it would be timely to take careful note of the frontline staff regarding what they will help them to deliver safe and compassionate care.
Since earlier this year, UNISON, the UK’s largest health union, has been challenging the government over its refusal to implement what is potentially an important recommendation in the Francis Report – the introduction of minimum staff to patient ratios. Most professionals believe that this simple intervention would provide safer, more caring environment for all. That call had been backed by a new survey from the union of more than 1,500 nurses, midwives and healthcare assistants, which shows that 45% of respondents are looking after eight or more patients on their shift. Research shows that looking after this number increases the risk of patient harm. While in political circles, we have heard a lot from the hedge funds and private equity funds about liberalising the economic activity in the NHS, it would be timely to take careful note of the frontline staff regarding what they will help them to deliver safe and compassionate care.
Remember them?
Where was the Big Society last week in the parliamentary discussion of the Keogh report?
The Big Society was the flagship policy idea of the 2010 UK Conservative Party general election manifesto. It now forms part of the legislative programme of the Conservative through the Liberal Democrat Coalition Agreement. Its stated aim was to create a climate that empowers local people and communities, building a “Big Society” that will take power away from politicians and give it to people.The idea was launched in the 2010 Conservative manifesto and described by The Times as “an impressive attempt to reframe the role of government and unleash entrepreneurial spirit”. The plans include setting up a Big Society Bank and introducing a national citizen service. The stated priorities were to give communities more powers (localism and devolution), encourage people to take an active role in their communities (volunteerism), transfer power from central to local government, support co-ops, mutuals, charities and social enterprises, and publish government data (open/transparent government).
The Big Society remains as vague now, as it did then. Localism has clearly been a frustration of ‘communities taking action’. Both the ‘Save Trafford A&E’ and ‘Save Lewisham A&E’ have been on the receiving end of an argument which urges the need for responsible reconfiguration of NHS services.Whilst campaigners in both situations have urged the need for recognition of their own services, the constant rebuttal has been that in any policy formulation or consultation there are bound to be dissenting views particularly if the sample size of respondents is high. Many people will share the frustration of those who had been encouraged by mechanisms such as the Localism Act (2011), in wider local issues.
There has been a big drive also to encourage ‘social value’ in public services, manifest in the Public Services (Social Value) Act 2012. The fundamental idea behind ‘social value’ is that it is a way of thinking about how scarce resources are allocated and used. It involves looking beyond the price of each individual contract and looking at what the collective benefit to a community is when a public body chooses to award a contract. Social enterprises are businesses that exist primarily for a social or environmental purpose. They use business to tackle social problems, improve people’s life chances, and protect the environment. Healthwatch England has referred to “The NHS Bodies and Local Authorities (Partnership Arrangements, Care Trusts, Public Health and Local Healthwatch) Regulations 2012″.
In relation to the section covering political campaigning, their view is that,
“section 36(2) ensures local Healthwatch has the necessary freedom to undertake campaigning and policy work related to its core activities and believe to do otherwise would be distracting. We do however, appreciate how there could be some confusion due to the nature of the wording in the section.”
Another issue is how failing Trusts have been allow to provide poor care for members of the general public. Accusations have been made of a poor ‘culture of care’, and this issue has become political with accusation-and-counteraccusation. Patient groups are vital in representing the views of patients accurately. I know, because I was resuscitated after a cardiac arrest and successfully kept alive for six weeks in a coma at the Royal Free Hampstead. However, more than a decade ago, I studied my basic medical degree at Cambridge and Ph.D. also in early onset dementia there. The concern is that Trusts are not being altogether transparent in their metrics about care. However, I personally think patient groups to do this responsibly should be free to campaign on behalf of patients for poor care, but without turning the public against all hard-working doctors and nurses. My experience was that junior doctors and nurses feel terrible about episodes of poor care, so they definitely wish to work with the patient groups. This is not at all a ‘them against us’ issue, but the language of ‘service user’ and ‘they’re providing a service we pay for’ have not helped in this narrative, perhaps together with a concept that clinicians ‘carry out orders to maintain managerial targets’. This concept is particularly toxic, as it might appear at first blush consistent with a growing trend towards the deprofessionalisation of medical Doctors and nurses. Patient groups do an extremely worthwhile rôle, and I have the highest regard for them.
This is why it is all the more important I feel that these issues about the NHS can be held in future in a dignified and balanced manner, without further talk of Hunt ‘politicising the NHS’ or an ‘active smear campaign against Andy Burnham’. Patient groups need to be carefully about their involvement in the media, otherwise they can easily become politicised. The academic issue of whether HSMRs are reliable has become politicised, although the academic debate about HSMR is safely ringfenced in the academic journals such as the British Medical Journal. The limitations of the claims of ‘excess deaths’ or ‘needless deaths’ always needed to be done carefully, and it was left to Sir Bruce Keogh himself and media sources not particularly known for their Conservative loyalty, such as the Guardian or New Statesman, to defuse the panic which had set in following irresponsible reporting of the Keogh mortality report at the weekend.
Political campaigning is defined by the Charity Commission is as follows:
Campaigning: We use this word to refer to awareness-raising and to efforts to educate or involve the public by mobilising their support on a particular issue, or to influence or change public attitudes. We also use it to refer to campaigning activity which aims to ensure that existing laws are observed. We distinguish this from an activity which involves trying to secure support for, or oppose, a change in the law or in the policy or decisions of central government, local authorities or other public bodies, whether in this country or abroad, and which we refer to in this guidance as ‘political activity’.
Further details are given as follows:
“Political activity, as defined in this guidance, must only be undertaken by a charity in the context of supporting the delivery of its charitable purposes. We use this term to refer to activity by a charity which is aimed at securing, or opposing, any change in the law or in the policy or decisions of central government, local authorities or other public bodies, whether in this country or abroad. It includes activity to preserve an existing piece of legislation, where a charity opposes it being repealed or amended.”
It would seem therefore that the definition of ‘political activity’ is not the same as the “rough and tumble” of politics seen in House of Commons debates, nor even on Twitter. However, it is really hard to know what ‘changes in the law’ might follow from Keogh or the Francis Report. This in part, one must to be admitted, needs clear definition what an appropriate ‘outcome’ might be. If the aspiration is “safe staffing”, serious consideration should be put into how enforceable this is, how it could be measured. and what sanctions might follow from an offence regarding it. A clear problem is that stakeholders will always have different views, particularly if there are more of them, and resolving conflicting views is especially difficult. This is all the more significant if you hope a ‘motherhood and mother pie’ approach in keeping with that ‘flagship policy’ of the Big Society. It is clear that some patient groups, indeed the Government, oppose a flat ‘minimum staffing level’ for perfectly rational reasons:
Christina McAnea, UNISON head of health, said this week:
We are pleased that the Keogh Review, as the Francis Report before it, has recognised the relationship between quality care and safe staffing levels. UNISON has been campaigning for safe staffing levels and the right skills mix on wards for many years. This includes in the evenings and at weekends – there is clear evidence that out of hours cover isn’t safe. It is time for the government to start listening and take action by committing to minimum staffing levels. They must also listen to staff and patients who are the best barometer of an organisation.
Spending pressures mean that health workers are losing their jobs. Financial pressures are building up in the NHS just as the demand for healthcare and its cost is rising – trusts are being asked to make obscene savings. Undoubtedly, this will hit standards of patient care hard, and is the direct consequences of decisions made by the government – not by hardworking NHS staff.”
Whilst one clearly not make everyone happy all of the time, it is fortunate that there are so many brilliant stakeholders who ultimately want the best of patients in the NHS. The purpose of the English law is obviously not to get in the way of all the people participating in English health policy at this particularly sensitive time. Politicians can help too by not turning people against other people, and members of the public can help too by not doing the same.
Safe staffing, Keogh and the Nursing Times “Speak out safely” campaign
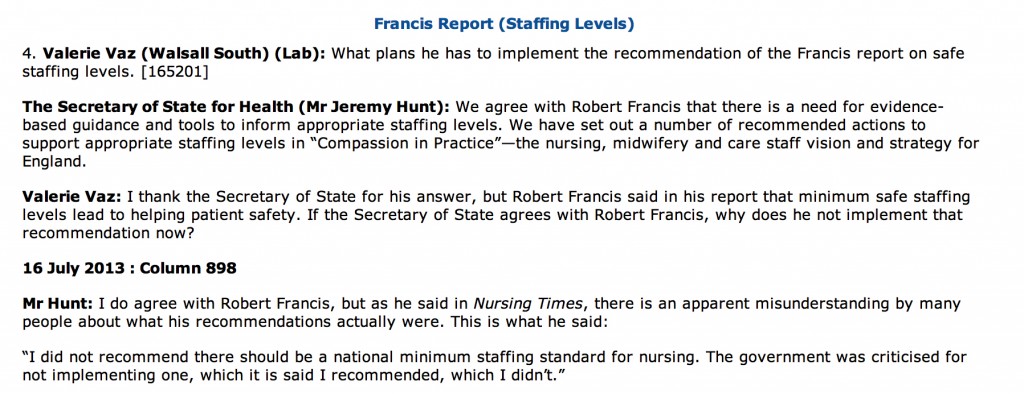
Despite clear differences in opinion about what has happened in the past, patient groups, Andy Burnham, Jeremy Hunt, the Unions, bloggers, experts, other patients, whistleblowers, and relatives at face value appear to want the same thing: a safe NHS where you do not go into hospital as a risky event in itself. The issue of safe staffing in nursing has become the totemic pervasive core issue of secondary care safety, and no amount of parliamentary time one suspects will ever do proper justice to it. In reply to a question from Valerie Vaz, who is herself on the Health Select Committee, Jeremy Hunt immediately quoted the Nursing Times and the Francis Report (from Tuesday 16 July 2013):
The aim of the Nursing Times’ Speak Out Safely (SOS) campaign is to help bring about an NHS that is not only honest and transparent but also actively encourages staff to raise the alarm and protects them when they do so.
They want:
- The government to introduce a statutory duty of candour compelling health professionals and managers to be open about care failings
- Trusts to add specific protection for staff raising concerns to their whistleblowing policies
- The government to undertake a wholesale review of the Public Interest Disclosure Act, to ensure whistleblowers are fully protected.
A very impressive gamut of organisations have supported the “Nursing Times Speak Out Safely” campaign, including Cure the NHS, the Florence Nightingale Foundation, the Foundation of Nursing Studies, Mencap Whistleblowing Hotline, Patients First, Public Concern at Work, Queen’s Nursing Institute, Royal College of Nursing, Unite (including the Community Practitioners and Health Visitors Association and Mental Health Nurses Association), and WeNurses. Also, for example, according to the Royal College of Midwives, maternity staff must be able to publicly raise concerns about the safety of mother and babies without fear of reprisal from their employers, according to the Royal College of Midwives. This college has been the latest organisation to support the Speak Out Safely campaign. They are calling for the creation of an open and transparent NHS, where staff can raise concerns knowing they will be handled appropriately and without fear of bullying.
The pledge of the Speak Out Safely campaign of Nottingham University Hospitals NHS Trust is a pretty typical example of the way in which this campaign has successfully reached out to all people who have the focused aspiration of patient safety.
“This trust supports the Nursing Times Speak Out Safely campaign. This means we encourage any staff member who has a genuine patient safety concern to raise this within the organisation at the earliest opportunity.
Patient safety is our prime concern and our staff are often best placed to identify where care may be falling below the standard our patients deserve. In order to ensure our high standards continue to be met, we want every member of our staff to feel able to raise concerns with their line manager, or another member of the management team. We want everyone in the organisation to feel able to highlight wrongdoing or poor practice when they see it and confident that their concerns will be addressed in a constructive way.
We promise that where staff identify a genuine patient safety concern, we shall not treat them with prejudice and they will not suffer any detriment to their career. Instead, we will support them, fully investigate and, if appropriate, act on their concern. We will also give them feedback about how we have responded to the issue they have raised, as soon as possible.
It is not disloyal to colleagues to raise concerns; it is a duty to our patients. Misconduct or malpractice should never be tolerated, while mistakes and poor practice may reveal a colleague needs more training or support, or that we need to change systems or processes. Your concerns will be dealt with in an open and supportive manner because we rely on you to ensure we deliver a safe service and ensure patient safety is not put at risk. We also want this organisation to have the confidence to admit to mistakes and to use them as learning opportunities.
Whether you are a permanent employee, an agency or temporary staff member, or a volunteer, please speak up when you feel something is wrong. We want you to be able to Speak Out Safely.”
The Keogh report is in its entirety is an apolitical report, and is very constructive. It identifies problems which Keogh’s team (which currently consists of some brilliantly talented Clinical Fellows) have a realistic chance of tackling. Despite criticisms that Hunt has turned up the ‘political heat’ on this issue, there is a feeling that Labour and Andy Burnham MP should either ‘put up or shut up’. If you park aside the mudslinging over the 13,000 ‘needless deaths’ from irresponsible journalism from parts of the media, the current Department of Health has surely begrudgingly have to be given some credit for instigating appropriate responses such as the Keogh review, and a Chief Inspector of Hospitals. There has been a real effort to clear up the methodology of estimating mortality figures, and while methodology issues will persist, an approach which fully involves and acknowledges the views of patients, whatever their political affiliations, is the only way forward.
As an immediate response to the terms of reference to protect patients from harm, Keogh thrust high up the importance of instigating changes to staffing levels and deployment; and dealing with backlogs of complaints from patients. Keogh identified a basic deficiency in effective performance management in the 14 NHS Trusts under investigation, and these basic performance management techniques are now commonplace in successful corporates. These constitute understanding issues around the trust’s workforce and its strategy to deal with issues within the workforce (for instance staffing ratios, sickness rates, use of agency staff, appraisal rates and current vacancies) as well as listening to the views of staff; Keogh laid down a number of “ambitions”. In ambition 6, Keogh argued that nurse staffing levels and skill mix should appropriately reflect the caseload and the severity of illness of the patients they are caring for and be transparently reported by trust boards.
The review teams especially found a recurrent theme of inadequate numbers of nursing staff in a number of ward areas, particularly out of hours – at night and at the weekend. This was compounded by an over-reliance on unregistered staff and temporary staff, with restrictions often in place on the clinical tasks temporary staff could undertake. There were particular issues with poor staffing levels on night shifts and at weekends. There were also problems in some hospitals associated with extensive use of locum cover for doctors.This observation is interesting as at the end of day an over-reliance on agency staff in both private and public sector from a performance management perspective will guarantee the NHS not getting the best out of its staff, and will further impede hospital CEOs from meeting their ‘efficiency targets’. As set out in the “Compassion in Practice”, Directors of Nursing in NHS organisations should use evidence-based tools to determine appropriate staffing levels for all clinical areas on a shift-by-shift basis. This means that a statutory minimum may be the inappropriate sledgehammer for an important nut. It is proposed that boards should sign off and publish evidence-based staffing levels at least every six months, providing assurance about the impact on quality of care and patient experience. The National Quality Board will shortly publish a ‘How to’ guide on getting staffing right for nursing. Whilst it is easy to argue against a national minimum number for nurses, as one can easily argue that it might encourage a race-to-the-bottom with managers gaming the system such that they only provide the minimum to run their Trust, most people, irrespective of the strong-held and important views of professionals within the nursing profession, believe that running a service with too few nurses is simply too risk for the remaining nurses. At times of high demand, Trusts need to be adaptable and flexible enough to cope, as anyone who has been involved in acute care in national emergencies has been involved (“critical incidents”).
Staffing was a recurrent pathology in the 14 Trusts under investigation. In Basildon and Thurrock University Hospitals NHS Foundation Trust, it was argued that the Trust needs to review current staffing levels for nursing and medical staff. In Buckinghamshire NHS Trust, the panel had a concern over staffing levels of senior grades, in particular out of hours. In Colchester Hospital University NHS Foundation Trust, it was found that staffing in some high risk wards needs urgent review. For the Dudley Group NHS Foundation Trust, inadequate qualified nurse staffing levels were identified on some wards, including two large wards which needed to be reviewed in light of concerns raised by the panel. For North Lincolnshire and Goole NHS Foundation Trust, there were concerns over the staffing of key elements of acute care, including recruitment of staff and maintenance of adequate staffing levels and skill mix on the wards. In North Cumbria University Hospital NHS Trust, inadequate staffing levels was identified, as well as an over-reliance on locum cover in some areas of the Trust.
For East Lancashire NHS Trust, the review team considered that staffing levels were low for medical and nursing staff when compared to national standards. Registrar cover and medical staffing in the emergency department was considered poor (this is medical ‘code’ for an overreliance on juniors at Foundation level), and levels of midwifery staff were considered poor too. Certain clinical concerns raised by staff have not been addressed, including known high mortality at the weekends. Whilst some of these actions will take longer to address entirely, assurance in respect of patient flows in A&E and concerns over staffing in the midwifery unit had already been sought by the CQC. For Medway NHS Foundation Trust, a top priority was made of teviewing staffing and skill mix to ensure safe care and improve patient experience, emphasising yet again that there might be false security to be derived from just looking at the overall number. For Sherwood Forest Hospitals NHS Foundation Trust, significant concerns around staffing levels at both King’s Mill Hospital and Newark Hospital and around the nursing skill mix, with trained to untrained nurse ratios considered low, at 50:50 on the general wards. Finally, for United Lincolnshire Hospitals NHS Trust, inadequate staffing levels and poor workforce planning particularly out of hours were discovered; concern over the low level of registered nursing staff on shifts in some wards during the unnannounced visit out of hours was escalated to CQC. Further investigation is underway.
This is a matter for all the political parties to get to the bottom of urgently. Party affiliations and tribal politics threaten real substantial progress in this area for all those who work in this area. This is not the time for energised disputes about political leadership in organisations. This is most certainly a time for action. Both the Francis report into the failures of care at Mid Staffs, and The Keogh Review into high hospital mortality rates, highlight how important the right skills mix and sufficient numbers of staff are to providing top quality care. Having the right staff cover is increasingly important out of hours – at evenings and weekends. With all political parties urging a need to work ‘harder and smarter’, or generally under the rubric of working more ‘efficiently’, this is a harsh climate, due to shrinking budgets as the cost of healthcare rises, and because of demands for £20 billion of so-called efficiency savings. Of course, the public are not involved in a genuine public debate at the moment which does not depict the ageing population as a budgetary ‘burden’ on the society, instead pumping in a carefree way billions into the HS2 project with its unclear business case. Billions more have been wasted on a chaotic, unnecessary top down reorganisation of the NHS; the National Audit Office has latterly criticised for the Government for going ‘over-budget’ on these bureaucratic reforms. Frontline staff are obviously rightly angry that this is money that they feel this is money that could and should have gone towards actually caring for patients.
The tragedy is that it really feels as if the NHS has never known, or unlearnt at great speed, basic performance management. One can argue until the cows come home how in this managerial-heavy approach to the NHS such management is extremely poorly done in such a way the CIPD would feel ashamed at possibly. The NHS will deserve to have problems in recruiting the best managers for the NHS so long as the climate of performance management, perhaps affected by an obsession for targets, remains deeply unappealing. It is recognised that good performance management helps everyone in the organisation to know hat the organisation is trying to achieve, their role in helping the business achieve its goals, the skill and competencies they need to fulfil; their role, the standards of performance required, how they can develop their performance and contribute to development of the organisation, how they are doing, and when there are performance problems and what to do about them. The general consensus is that, if employees are engaged in their work they are more likely to be doing their best for the organisation. An engaged employee is someone who:
The actual reality is that currently spending pressures mean that many health workers, sadly, are losing their jobs. Financial pressures are building up in the NHS just as the demand for healthcare and its cost is rising – trusts are being asked to make unconscionable savings. Trusts such as Barts Healthcare are in severe trouble, and the contribution of the failed policy of PFI is a massive scandal in itself. This perfect storm will hit standards of patient care hard, and is the direct consequences of decisions made by various recent governments – not by hardworking NHS staff. The only thing which is set up to work in the Act, apart from outsourcing (section 75) and raising massively the private cap (section 164(1)(2A)) of the Health and Social Care Act 2012 is the legal precision of the various failure or insolvency regimes. In any other sector, this would fall under wrongful or fraudulent trading. Except, it’s the NHS. It does economic activity in a very special way. As the shift in economic and political power shifts from a state well-funded comprehensive healthcare system to a fragmented disorganised piecemeal private integrated system in the next few decades, patient safety must take priority even if not a top priority seemingly in business plans. Initiatives such as the Nursing Times ‘Speak out Safely’ campaign is one of those vital ‘checks and balances’ to ensure that the NHS is working with and for patients and not against them. This means the NHS valuing staff as a top priority, as social capital is the most important thing in any organisation.
The Health and Social Care (2012) was not about patient safety: implications for the Keogh report
The Health and the Social Care Act (2012) is a massive tome. It actually reads, for lawyers who are well acquainted with such statutory instruments, like a huge patchwork quilt of commercial and corporate law strands. While voluminous, at 473 pages, it has two critical clauses. The first is section 75, and its concomitant now famous Regulations, which provides the statutory basis for procurement contracts in the NHS to be put up for price competitive tendering as the default option, thus fixing the NHS in a competitive market of an economic activity. This is of course the mechanism for outsourcing NHS services into the private sector, and indeed the vast majority of contracts have now been won by the private sector. This was widely predicted, as the private sector have skills and resources to make slicker bids, irrespective of the bid they ultimately deliver, to transfer a much higher proportion of “NHS services” into the profit-making private sector. All of this costs the NHS more money sadly, as while it may not matter to you ‘who provides your services’, you’re in trouble if the private provider goes bust, and you’re not paying for anything at anywhere near cost-price because of the mark-up for profit. This section 75 clause acts in tandem with section 164(1)(2A) which allows any NHS hospital to receive up to 50% of its income from private sources. Thus the Act, and the £2.4 NHS “reforms”, have been a bonanza for the private sector, and disastrous from the perspective of a state-provider of universal, comprehensive healthcare.
Patient safety is in fact only mentioned once in the Act, in clause 281. That is in reference to the abolition of the National Patient Safety Agency. The National Reporting and Learning System which was hosted by NPSA has a two year stint at Imperial College Hospital NHS Trust, while a tender process is scoped and developed by the Board. NPSA’s responsibilities concerning patient safety will transfer to the NHS England.
The Health and Social Care Act 2012 (c. 7) is an Act of the Parliament of the United Kingdom. It is the most extensive reorganisation of the structure of the National Health Service in England to date. It proposes to abolish NHS primary care trusts (PCTs) and Strategic Health Authorities (SHAs). The Act’s proposals were not discussed during the 2010 general election campaign and were not contained in the 20 May 2010 Conservative – Liberal Democrat coalition agreement, which declared an intention to “stop the top-down reorganisations of the NHS that have got in the way of patient care”. However, within two months a white paper outlined what the Daily Telegraph called the “biggest revolution in the NHS since its foundation”. The white paper, Equity and Excellence: Liberating the NHS, was followed in December 2010 by an implementation plan in the form of Liberating the NHS: legislative framework and next steps. The bill was introduced into the House of Commons on 19 January 2011, and received its second reading, a vote to approve the general principles of the Bill, by 321-235, a majority of 86, on 31 January 2011.
The British Medical Association opposed the bill, and held its first emergency meeting in 19 years, which asked the government to withdraw the bill and reconsider the reforms. A later motion of no confidence in Lansley by attendees at the Royal College of Nursing Conference in 2011, however, succeeded, with 96% voting in favour of the motion. Nurses have consistently been opposed to the the “efficiency savings” measures being undertaken across the NHS, with many raising concerns of their material impact on frontline medical services. “People will die”, Richard Horton, editor of The Lancet, warned in March 2012, as he predicted “unprecedented chaos” as a result of the reforms, with a leaked draft risk-assessment showing that emergencies would be less well managed and the increased use of the private sector would drive up costs.
The Bill is now Law, and where are the measures to deal with this longrunning problem of patient safety, particularly in the acute setting? There are none. The media was sent into overdrive in portraying the NHS has a “death machine”, despite the best attempts of nurses and Doctors to run the service under difficult conditions. The publication of the damning Keogh Report (“Report”), which spelt out the failings of 14 hospital trusts which did not quote “13,000 “needless deaths” since 2005″, is despite exhaustive pre-briefing to the media. The Report depicts a situation in certain trusts where patient safety is poor, with no reference to what action has been taken by the Government and their civil service to remedy this since the General Election in May 2010, which the Conservatives lost. Sir Bruce Keogh, the NHS’s Medical Director, will describe how each hospital let its patients down through poor care, medical errors and failures in management, but the Report is as if the clinical regulatory bodies do not exist, the General Medical Council, the Nursing and Midwifery Council and the Care Quality Commission. How they have escaped blame for this reported ‘scandal’ is incredible, although one suspects the media will catch up with them eventually. It might be that the media for whatever reason known to them do not feel the clinical regulators are in “the firing line”, despite being supposed to be responsible for patient safety, in the same way that lawyers are not responsible for the global financial crisis despite being supposed to regulated on the safety of financial instruments.
From a management point of view, the Keogh Report serves a function for convincing the public of a need to take patient safety extremely seriously. However, to sell the Keogh Report as “Do you now see the need for the NHS reforms?” maybe hitting a target but missing a crucial point. The NHS reforms are all to do with outsourcing and eventual privatisation of the NHS. They are nothing to do with patient safety, as even right-wing think tanks and their spokesmen have previously conceded in public. In fact, it is worse than that. The £2.4 reorganisation which nobody voted for, but which private healthcare companies extensively lobbied for, was a reckless missed opportunity to put resources into something other than frontline care, and the opportunity cost of this piece of legislation will continue to haunt the general public for many years. Unfortunately, the media and the members of the Establishment, some members of which have tenuous links with the institutional shareholders in private healthcare companies, will be more than aware of this hard fact. The Conservatives are desperate to pin every conceivable woe of the NHS on Andy Burnham, and every interview which Burnham now does must feel like “Groundhog Day” for him. He has nothing much more in his defense. Meanwhile, the Conservatives are exasperated that they have been unable to get the Burnham scalp, but there are as yet unresolved issues about what Government departments have done about NHS complaints in the last three years since May 2010. The bottom line is that the Health and Social Care Act is nothing to do with patient safety: even safety campaigners in the NHS know this, and they know of the even worse battle now facing them, of a fragmented privatised NHS which is even harder to regulate from that point of view. The NHS reforms, and more specifically the Health and Social Care Act which underpins them, have nothing to do with patient safety. More disturbingly, the Keogh report, when eventually published, will not stop ‘another Francis’, and it is entirely the Government’s fault we are in this stupid ridiculous position.