Home » Posts tagged 'Jeremy Hunt'
Tag Archives: Jeremy Hunt
Does Jeremy Hunt wish to ‘save the NHS’? Most definitely not.
There is nothing more embarrassing than for hardworking clinicians in the NHS and practitioners in social care than to hear of Jeremy Hunt going to New York to lay the groundwork for a transatlantic trade deal or to go to international conferences to preach to others on patient safety. Whether the longest serving Secretary of State for Health chooses to admit or not, and he doesn’t, there is nothing to boast about in 20 hour trolley waits, or people being asked to sit in a toilet or corridor before being given a hospital bed. If the definition of patient safety is that nobody has died unnecessarily yet, then expectations are indeed very low. Indeed, Sir Robert Francis, whom Hunt used to quote all the time, now says another Mid Staffs is “inevitable”.
To be honest, this is the perfect storm which prominent campaigners, including junior doctors, themselves have been warning about. It might seem beyond ludicrous that Jeremy Hunt can shamelessly say that the performance of the NHS is ‘unacceptable’, but as far as he is concerned he is not responsible for the performance of the NHS. And the purpose of the 2012 Health and Social Care Act (2012) was not to promote the highest quality clinical care – symptomatic of that is the fact in the 500 pages of legislation the legislation found time to devote only one clause to patient safety, and that was to abolish the National Patient Safety Agency. The legislation instead was put in place to turbo-boost the transfer of NHS services to the private sector. This is – wait for it – the definition of ‘privatisation’. It also provided legislation for clinical commissioning groups, where is no statutory mandate for clinical skill. These clinical commissioning groups, which are even definite in size of population in law, are merely insurance entities which happen to reside in the public sector, assessing the potential risk of illness in a certain geography. In other words, this highly contentious Act of parliament, on which billions of £ were ultimately spent in a top-down reorganisation that nobody as such voted for, laid down the infrastructure for harmonisation between the public sector and the private sector for the ultimate piecemeal sell off of the NHS.
The ultimate issue that successive governments have had to face for the last three or four decades has been a desire not to go ‘public’ about transferring the NHS to the private sector, so that the NHS simply becomes a badge for the state deliverer of services, not the state provider. In an ideal world, Jeremy Hunt MP does not even want to be involved with anything to do with the NHS. Hunt, and many others of the same ideological ilk, would be perfectly happy for different providers, e.g. Capita, Virgin, G4S, in some corporate plutocracy to run the NHS using the NHS logo if need be.
Jeremy Hunt’s faux disdain at the performance of the NHS is completely understandable, if one realises that Hunt thinks the public will blame the fact the NHS is in the public sector rather than him for the poor performance of the NHS. And, to be fair to him, there are people who ring up local radio phone shows to say that the problems of the NHS are entirely due to mismanagement, the fact that the general public take no responsibility for their own health (a completely irrelevant argument if someone is born with a congenital disease such as heart problem or lung problem). And, furthermore, more in the post-facts milieu, the hope is that nobody can discern fact from fiction. In other words, with the help of a compliant media, the general public can be manipulated into thinking that the root cause of the NHS being overloaded is entirely due to the immigrant population. There is no discussion of non-indigineous doctors or other healthcare professionals in this utopia, just ‘small talk’, albeit dangerous UKIP pillow talk, of an aspiration of Jeremy Hunt to reverse decades of the NHS being propped up by foreign clinicians to train ‘home grown’ doctors. Mainsteaming British Doctors for British patients has never been easier.
But back to the fundamental issue of why I believe Jeremy Hunt does not care about the performance of the NHS is that his thinking rests on three assumptions. And, whilst a sizeable number of people in parliament think the same way as him, the likelihood of a cross-party commission on the NHS will come to the conclusion that some form of privatisation of the NHS, whether in terms of co-payments, vouchers or full blown increase in capacity of private insurance providers, will occur, rubber-stamped by all the political parties (except for some this time). It might, for example, be seductive for irritable, cranky people to ‘charge drunk people for attending A&E’, but think about the actual practical implementation of this policy – by what measure would you define the tipping point from ‘quite tipsy’ to ‘quite drunk’? Is it, for example, either feasible or desirable that healthcare professionals, including GPs, to carry Visa card or passport readers in addition to their numerous other duties?
A number of assumptions can possibly be made about this current Government and recent ones too:
1. There is no distinction between private and public providers in the NHS.
2. The Government believes in a ‘small state’ and low taxation.
3. The NHS is expected to make efficiency savings in keeping with an austerity approach.
That there is no distinction between private and public providers in the NHS is why Jeremy Hunt resents being in a centre of a tsunami about junior doctors’ pay. In an ideal world, he would like there to be complete harmonisation between private and public sectors, so that doctors could come and go as they wish in terms of employment. This is entirely the drive for the 24/7 NHS, which is why Jeremy Hunt is do keen to promote any fake research news coming out of the BMJ to further his ideology. You do not need to be an expert in sophisticated mathematical modelling techniques to realise that if you were to stretch out the already woefully inadequate resources for a 5-day elective service into a 7-day one the consequences on patient safety would be diabolical. What, furthermore, is quite incredible is for the current Department of Health to be so oblivious to the fact there already exists a 7-day emergency service running at full throttle, hence their need to spend valuable resources in making further metrics to measure A&E performance by.
Where junior doctors can come and go as they please, like where consultants can come and go as they please, or where nurses come and go as they please, is a strategy which is the direct opposite to the public sector keeping its workforce loyal, wellbeing promoted and well educated, and being contained budget-wise in terms of salaries. We already know that the agency spend has become out of control, due to poor planning of the Department of Health over many years, and to the weird hybrid private-NHS market we currently have. And all this is to ignore completely that private providers take no responsibility for, financially or otherwise, for the education and training of the workforce the vast majority of which start in the NHS. This is entirely in keeping in why Hunt is so intensely relaxed about applications for nursing training going through the floor after his devastating nursing bursary initiative – Hunt does not ideologically believe the Government should be safeguarding against a minimum body of doctors, nurses or allied health professionals in the workforce. The problem now of course for him now is #Brexit unless it looks like he can poach staff from the Asian subcontinent; but word is spreading fast how bad the working conditions of the English NHS are.
2. Unfortunately, the Conservatives and Liberal Democrats were able to converge on the ideology behind the Health and Social Care Act 2012 and the mirage that economic competition would drive up clinical quality because of the robustnesss in their belief in the small State. This does not envision the State to be a supportive thing to promote the health and wellbeing of its citizens, including so that they can be healthy enough to be in ‘gainful employment’ and be ‘productive’. This instead pre-supposes that everybody wishes to pay very low taxes, somehow living in a world where public services are still magically working well. But this falsehood is very easy to put in place if the main political parties are able to blame a ‘common enemy’ for all of their problems, e.g. immigrants. Such politicians want to divorce the link between improved public services and paying for them, which is why the Conservatives invest so much effort into depicting the Labour Party as incompetent (whereas the national debt under the 7 years of Conservatives has ballooned way above the previous 13 years of Labour).
Unfortunately, a hypothecated tax for the NHS would necessitate a debate about hypothecated taxes for everything else such as national security or education, and is well known to be yet another ‘zombie policy’ which won’t go away. Finally, whilst the Government gives the impression that the debacle in social care, causing delayed transfers of care from hospitals to care packages in the community, is seen as a ‘local authority’ not national problem, say for example through the ‘precept’ or the Surrey referendum, the impression is reinforced that social care is out of control, and its catastrophic state impacting on the performance of the NHS is nothing which can be reversed essentially.
3. Stephen Dorrell MP already has said that the NHS efficiency savings, first proposed by the management consultants, McKinseys have never successfully been tried before – and indeed many blame this drive for efficiency and for ‘foundation trust’ status to be at the heart of how disasters at Mid Staffs and other Trusts happened. It is a plain fact that if budgets are under enormous strain in providing a skeleton workforce (e.g. one junior doctor to cover all the medical wards in one large teaching hospital AND cover the cardiac arrest bleep), and to pay massive unconscionable private finance initiative payments (a form of a Corporate Wonga), something will have to give. There might be a temptation for such cuts to be hidden by commissioners and managers in mental health, despite all the Twitter infograms and rhetoric about ‘parity of esteem’ – unless of course there happens to be a spike in uncontrollable demand for mental health beds or suicides. So far, all the main English political parties have been very loyal to ‘efficiency savings’ – but this is essentially ‘austerity’, and a political choice for the NHS not an economic one.
If the ultimate aim is to increase transfer of public assets to private entities (the definition of privatisation), keeping the NHS at a low unsafe level of funding reinforces the impression the NHS is ‘unsafe in public hands’. That is why rolling coverage by the BBC of ‘specials’ of a NHS and social care system at breaking point might lead people to blame the public funding of the NHS, not Jeremy Hunt. This is of course fully intended, so that the green light can be given for a blatant privatisation of the NHS.
The correct conclusion, of course, is that the NHS has been chronically underfunded for years, and no Government wishes to admit they want to privatise the NHS as it’s so politically toxic.
Jeremy Hunt’s final speech to the Conservative Party conference on the NHS
This is the text of the speech given by Mr Jeremy Hunt, the Minister who oversees the running of the NHS and care despite having no legal statutory duty for it.
Today I am here to tell the British people that a future Conservative government will have no greater priority than to protect, support and invest in our NHS.
In 1948, the greatest of all Conservatives Winston Churchill supported the then Labour government in its plan to set up a National Health Service. He said ‘disease must be attacked whether it occurs in the poorest or richest man or woman simply on the grounds that it is the enemy.’
That safety net Churchill wanted is our NHS today, supported across the political spectrum.
Last week Labour tried to paint a different picture. They know this government increased the NHS budget despite the financial mess Labour left behind. They know the NHS has more doctors and more nurses than ever before. They know fewer people than ever are waiting long periods for their operations. They know the culture is becoming more caring. But they still seek to trick the public into thinking one party cares for the NHS and the other doesn’t.
Well I have a message for Mr Miliband. It’s not a Labour Health Service or a Conservative Health Service…it is a National Health Service. And when my father was cared for by a district nurse or my wife had our baby this summer or our son goes for his jabs, they aren’t Conservative patients, Labour patients or LibDem patients, they’re NHS patients. When people in this hall volunteer to support the local league of friends or join the board of a hospital we’re not Conservative supporters – we’re NHS supporters. We all support the NHS because the NHS is there for us all.
So don’t turn the National Health Service into a National Political Football and don’t use the NHS to divide us when it’s the fabric that unites our nation.
This morning the Prime Minister announced plans to make it easier for millions of people to get 8 till 8 and weekend appointments with their GPs.
And I want to start today by celebrating that and some of the other successes of our NHS, doing so well despite huge pressure.
Take cancer, our biggest killer. Every family in the country has lost a friend or loved-one to cancer – I lost my own father last year. It is a ruthlessly indiscriminate killer – whether it targets someone who has just retired after a life of hard work or a child with a life stretching out in front of them.
In 2010 this country had amongst the lowest cancer survival rates in Western Europe. So we set up the cancer drugs fund. We’ve transformed cancer diagnosis so the NHS now tests 1000 more people for cancer every single day. And so far this parliament we have treated nearly three quarters of a million more people for cancer than the last one – that’s thousands of lives saved, thousands of families kept together, thousands of tragedies averted. So let’s hear it for our brilliant cancer doctors and nurses.
Or look at dementia, one of the most terrifying conditions of all.
I’ll never forget the courage of man I met with dementia who single handedly stood up to the banks and demanded they gave him an alternative to having to remember a pin number. But it isn’t just your pin number that goes. It’s precious family memories, marriages of many years, relationships with children – all snatched away by cruel tricks of the mind. When we came to office fewer than half of those with dementia got a diagnosis, meaning many missed out on vital medicine or support for their family. We’ve now diagnosed an extra 80,000 people. The Prime Minister hosted a G8 summit to get the drug companies to do more to find a cure. And we’re working with the Alzheimers Society to enroll one million dementia friends to tackle stigma – with half a million signed up so far.
So let’s hear it for GPs, dementia nurses, dementia carers, dementia friends and people with dementia who are changing the way our society tackles this horrible condition.
Or A & E, the critical frontline for the NHS. A young A & E doctor told me how she had cried after seeing a 90 year old man say his goodbyes to a 90 year old woman he’d been married to for over 60 years. For her that was just part of the job. And with a million more people using A & E, the pressures on her and her colleagues are immense.
Sometimes, yes, it’s been tough meeting the target. But despite that we have halved the time people wait to be assessed and are treating nearly 2,000 more people every day within the four hour target compared to 2010. So let’s hear it for our brilliant A & E frontline staff now preparing for a challenging winter.
Conference our opponents say the NHS is in decline. But according to the independent Commonwealth Fund under this government the NHS became the top-rated healthcare system in the world. Better than America, better than France, better than Germany, better than Australia. And the way they rose to the challenge of Ebola says it all – with 164 NHS volunteers offering to go and help contain the outbreak in West Africa. So let’s hear it for all NHS doctors, nurses, porters, cleaners, caterers, carers and volunteers. You are the best of British and the pride of our nation.
But that doesn’t mean things are perfect. About the first thing I did as Health Secretary was to read the original Francis report about the terrible things that happened at Mid Staffs Hospital between 2005 and 2009. I was utterly horrified. As Francis made clear, system-wide failings meant these problems weren’t limited to one hospital.
One member of the public wrote to me about what happened somewhere else in a letter that was so shocking I asked to meet her.
She said she visited her late husband in hospital at 5 in the morning and found him naked on a deflated mattress, caked in urine and excrement, and curled in a foetal position with a cold air conditioner blowing directly onto his body. She still has nightmares about that visit. Now that story, thankfully, is far from typical of our NHS.
But I vowed that day that if I did nothing else, I would make sure I returned a culture of compassionate care to every corner of our NHS. Because caring is what the NHS stands for, what every doctor and nurse passionately wants, why the NHS was set up – and what a quagmire of targets, goals and plans too often allowed to be squashed.
Supported by a wonderfully committed ministerial team – Freddie Howe, Norman Lamb, Dan Poulter, Jane Ellison and George Freeman – we’re changing things.
We introduced a tough new inspection regime.
Since then our hospitals have hired over 5,000 more nurses to tackle the scandal of short-staffed wards; 5 hospitals – Basildon, North Lincs, George Eliot, Bucks and East Lancashire – have been put into special measures and been turned round; and patients are saying that they are treated with dignity and respect not just at Mid Staffs but across the NHS the highest numbers ever recorded.
Indeed on Friday of last week the CQC announced the first hospital in the country to get an ‘outstanding’ rating, Frimley Park in Camberley. Chief Executive Andrew Morris is so committed he has been there for 25 years and his son even works there as a porter. Well done to Frimley Park.
Now the problems of poor care highlighted by Robert Francis happened under Labour – so I thought Labour would rush to support me in sorting them out. In fact they did the opposite. They said talking about poor care was ‘running down the NHS.’ They even tried to vote down the law setting up a new Chief Inspector of Hospitals.
I’ll tell you what ‘running down the NHS’ is:
- It’s not learning the lessons when a mother is forced to give birth on a toilet seat, as happened in 2007. Ignored by Labour, being sorted out by us.
- It’s making hospitals Foundation Trusts even when their mortality rates are too high. Brushed aside by Labour, being sorted out by us.
- It’s stopping the CQC telling the truth about blood-stained floors in one hospital. Happened under Labour, stopped by us.
It happened in England before and it’s happening in Labour-run Wales today – so don’t you dare talk to us about running down the NHS.
Because for Labour good headlines about the NHS matter more than bad care for patients – and in our NHS nothing matters more than patients and whilst I am running it nothing ever will.
I simply say this to a Labour Party that still refuses to learn the lessons of Mid Staffs, until you do, you are not fit to run our NHS. And if you won’t put patients first we will – and it will be the Conservative Party that completes Nye Bevan’s vision for an NHS that treats every patient with dignity and respect. We will finish the job.
I could go on with my concerns about the culture Labour left behind in our NHS. But I want to look forward and deal with one of the biggest concerns people have about the NHS which is about funding.
Labour talked about putting in more money last week. But securing the NHS budget isn’t about an extra billion here or there. It’s about funding over £100bn, which is what we spend on the NHS every year. And that needs a strong economy. Because it’s very simple: you can’t fund the NHS if you bankrupt the economy. This parliament we’ve actually increased spending on the NHS by more – in real terms – than Labour promised last week. We’ve done it because of David Cameron’s personal commitment to the NHS and difficult decisions taken by George Osborne.
Other countries followed Labour’s advice. They ducked those decisions. They had no plan – and ended up cutting their health budgets. Italy by 3%, Greece by 14%, Portugal by 17%. I don’t want that to happen here.
So never forget we’ve just had the greatest squeeze on finances in NHS history because a Labour government lost control of our national finances. So to anyone worried about investment in the NHS I say this: a Labour government with reckless economic policies is the biggest single danger to funding our NHS. Do not take that risk. Nor should we forget that every penny of NHS funding comes not from the government but out of the pockets of hard working taxpayers. So if we increase spending on the NHS we must also look every one of them in the eye and promise that every penny is being spent wisely. Which means we mustn’t stop new ideas that come from outside the NHS – whether from charities or, yes, the independent sector.
Labour call this privatisation. But using a charity like WhizzKids to supply wheelchairs to disabled children or using Specsavers to speed up the supply of glasses is not privatisation. When the last Labour government used the independent sector to bring down waiting times that wasn’t privatisation either. So stop scaremongering about privatisation that isn’t happening. It nearly cost us Scotland – and we won’t let it poison the debate in England as well. Secure NHS funding backed by a strong economy is the foundation.
But the building blocks to a modern health service are two things that need real cultural change.
Personal care – a real challenge as patients navigate one of the biggest organisations in the world. And personal control – in a world which has too often said the doctor, not the patient, knows best.
I remember when I did a shift in an A & E last year. A 90 year old lady with dementia was brought in by ambulance after a fall in her care home. She was completely motionless. She couldn’t talk. She couldn’t feed herself or even drink a glass of water. What made it worse was that in that A & E we knew next to nothing about her. We didn’t have her medical record. We didn’t know her allergies. We didn’t know if she was normally able to talk or whether it was just because of the fall. To us at that hospital she was not just unknown. She was anonymous. How could we possibly give her the personal care she desperately needed?
The same could happen to any one of half a million over 90s in our society. And it could happen to anyone with long term or mental health conditions, anyone of whom can find themselves anonymously pushed from pillar to post in a system that doesn’t know who they are. But for me the point of the NHS is to make sure all everyone gets truly personal care from people who know about them, know about their condition, know about their care plan – so that what happened in that A & E never happens again.
As a first step that needs the integration of the health and social care systems. And for the first time ever this year it is happening. 150 local authority areas working together with their local NHS on their Better Care plans to pool commissioning, reduce emergency admissions and share medical records all starting from next April – with many of you in this hall involved.
But truly personal care means more than joining up health and social care. It means personal, responsive care from your GP too.
Last year I manned the phones in a busy London GP practice. The doctors there worked very hard. But what was frustrating was having to tell nearly every caller there were no appointments available for two to three weeks.
We urgently need to make it easier for busy, working people to get an appointment. That means more GPs, so I can today confirm plans to train and retain an extra 5,000 GPs.
But it also means new ways of working. Last year we announced plans for 7.5 million patients to get weekend and 8 till 8 appointments. Today we have also announced we are rolling that out to millions more – meaning this service will be available for a quarter of the whole population. And going even further, I commit that at the end of the next parliament a Conservative government will make sure every NHS patient across the whole country will be able to get weekend and 8 till 8 GP appointments.
But personal care isn’t just about a convenient appointment. It means talking to a doctor who knows about you and your condition.
Astonishingly in 2004 Labour abolished the requirement for every patient to have their own, named, personal GP. At a stroke, many patients were told they no longer had their own GP, but were merely attached to a surgery. And GPs were told they were no longer personally responsible for patients. If you have a chronic condition or complex needs, continuity of care is absolutely vital. You don’t want to have to explain everything about yourself over and over again – and you want a doctor who takes ongoing responsibility for sorting things out – not just that day but every day.
So last year I changed that back for over 75s by insisting they get a GP named on their medical record and responsible for their care. Today I can go further and announce that in the new GP contract for 2015 every single person in England will go back to having a family doctor named on their record and responsible for their care.
Personal care for every NHS patient – delivered by this government. People want personal care. But in the 21st century they want something else. Not just personal care but personal control. People with diabetes, or a heart condition, or recovering from a stroke say the best person to take control of your care is not actually your doctor – it’s you. And right now we make that far too hard. We don’t give people enough information.
So this summer we became the first country in the world to publish detailed information about safety, waiting times, patient experience and food for every major hospital. And on the new MyNHS website we’ll go further.
But it isn’t just information about your local hospital you want, it’s information about you. So today I can confirm that by April next year, every patient in England will be able to access their own medical record online – the first country in the world to take this huge step. It means you will no longer have to pay to access your medical record. You’ll be able to see it and show it to anyone you choose. You’ll find it easier to do detailed research about your condition and easier to challenge decisions. Because the boss is not the doctor – it’s you. Nothing about me without me. Personal control of your health delivered by this government.
Conference my vision is simple. We in this party have always believed passionately we should honour our debt to previous generations. So I want Britain to be the best country in the world to grow old in. I want us to enjoy the fruits of prosperity, yes, but never forget the people before us who’ve worked hard to make that possible. Never forget that all our success, all our strength, all our wealth as a country is but a hollow dream if at the end of it we are not able to give all our citizens the healthcare and support they need in old age. Never forget that it’s not a choice between a strong economy or a strong NHS. You need both and only one party – this party – can deliver both. A strong NHS. A strong economy. From a Conservative party proudly rebuilding a strong country. Personal care. Personal control. For patients treated with dignity, compassion and respect. Delivered by our party. For our NHS. For our country.
Thank you.
Could the “social impact bond” help to improve services in dementia care?
This blogpost first appeared on the ‘Living well with dementia’ blog yesterday.
It’s impossible to ignore the occasional spate of reports of ‘care home scandals’, including Winterbourne View and Orchid View.
Whilst a direction of travel might be to advance people living ‘successfully’ as long as possible independently, there’ll be some people for whom a care home might be appropriate. There are particular aims of policy designed to support living well with dementia, such as combating loneliness and providing meaningful leisure activities, which can possibly be achieved through high quality care homes.
It’s pretty often that you hear of social care being “on its knees”, due to drastic chronic underfunding. A concern about attracting investment from the private sector is that this will help to accelerate the lack of financial resource allocation from the State. And yet this is the opposite to the argument of resources ‘leeching’ out of the public sector into the private sector.
In terms of the ‘business model’, there are concerns that, to maximise shareholder dividend, staff will not be incentivised to ‘care well’, if they are barely meeting the requirements of the national minimum wage. Whilst the employer emphasises ‘flexibility’ of zero hours contracts, for many such contracts are symbolic of a lack of commitment for sustained employment by the employer.
So the idea of bonds being used to prop up dementia care, currently one of the three big arms of the Prime Minister’s Dementia Challenge, has gained some momentum, for example here. Bonds are effectively “IOUs“, and concerns remain for them as in the private finance initiative – such as who actually benefits, the prolonged threat of penalty for not being able to meet your loan repayments, the issue of who decides the outcomes by which performance will be assessed, and who actually manages or controls the enterprise.
Social Impact Bonds (SIBs) are depicted as “a way of enabling innovation, creating flexible contracts around social outcomes and providing linked investment“. But for some, they are a vehicle for enabling ‘privatisation by stealth’.
The current Labour opposition officially is trying to distance itself from any mechanisms promoting the privatisation of the NHS, and yet it is known Chris Ham and Norman Lamb wish to publish a report imminently on the possible use of SIBs in policy under the auspices of the King’s Fund.
This is the title slide of Hazel Blears’ presentation for the Alzheimer’s Show on Friday.
And here is a section of her talk.
[apologies for the sound quality]
Hazel has a strong personal attachment to campaigning on dementia, and is particularly interested and influential in the direction of travel, not least in her rôle as Vice Chair of the All Party Parliamentary Group on dementia, a cross party group made up of MPs and Peers with an interest in dementia.
Andy Burnham MP, Shadow Secretary of State for Health, has made it clear that it is his firm and settled intention to repeal the Health and Social Care Act (2012). The current Prime Minister’s Dementia Challenge is to come to an end officially in March 2015.
Dementia UK set up some time ago its innovative ‘Admiral Nurses’ scheme, to provide specialist nurses who could help people with dementia and family carers to improve the quality of life of people with dementia and family carers.
Burnham has also let it be known that he intends to subsume social care within the NHS under the construct of ‘whole person care’. Whichever various formulations of ‘whole person care’ you look at, you tend to find a ‘care coordinator’ somewhere. The exact job description of the care coordinator, nor indeed which specialisms might be best suited to accomplish this rôle, is somewhat unclear presently.
But it is all too common to hear of people being diagnosed with dementia being ‘lost in the system’, sometimes for years without follow up.
A “care coordinator” might help to boost access to the following services: emotional support, enable short breaks for people with dementia and anyone in a caring role, promote nutritious meals, ensure medications are given on time, ensure the correct medications have been subscribed (for example avoiding antipsychotic medications in individuals who might be unsuited to these), advice about suitable housing (including downsizing), ensure all physical commodities are properly medically managed; and so the list goes on.
I feel it’s pretty likely there’ll be a ‘first mover advantage‘ effect for any entity which takes up this coordination rôle in dementia care. But the tension between this and the Opposition’s policy is palpable: one cannot talk of this entity being ‘the first to enter the market’, as many wish (and expect) Labour to abolish the internal market in health care.
Such a coordinating entity could well be a recipient of a SIB – but is this like the PFI of social care? PFI by and large has an incredibly negative press amongst members of the general public.
But on the other hand, is it vindictive to prevent a social enterprise from pitching from such a service? If that entity has the technical ‘know how’ to run operations nationally competently and at a reasonable price, would that be preferable to the State running such services when projects such as NHS IT and universal credit have not gone terribly well?
In our jurisdiction, private companies can hide easily being a corporate veil, and are for example currently not readily accountable through freedom of information legislation. This is despite numerous requests to Jeremy Hunt in parliament about parity in disclosure requirements from both private and public providers.
And the track record of some outsourcing companies in the private sector, it is said, has been terrible.
Jeremy Hunt and Norman Lamb are currently in control of NHS and care policy, but there might be a fundamental change in direction from the next Government.
Or there might not be.
Could the “social impact bond” help to improve services in dementia care?
It’s impossible to ignore the occasional spate of reports of ‘care home scandals’, including Winterbourne View and Orchid View.
Whilst a direction of travel might be to advance people living ‘successfully’ as long as possible independently, there’ll be some people for whom a care home might be appropriate. There are particular aims of policy designed to support living well with dementia, such as combating loneliness and providing meaningful leisure activities, which can possibly be achieved through high quality care homes.
It’s pretty often that you hear of social care being “on its knees”, due to drastic chronic underfunding. A concern about attracting investment from the private sector is that this will help to accelerate the lack of financial resource allocation from the State. And yet this is the opposite to the argument of resources ‘leeching’ out of the public sector into the private sector.
In terms of the ‘business model’, there are concerns that, to maximise shareholder dividend, staff will not be incentivised to ‘care well’, if they are barely meeting the requirements of the national minimum wage. Whilst the employer emphasises ‘flexibility’ of zero hours contracts, for many such contracts are symbolic of a lack of commitment for sustained employment by the employer.
So the idea of bonds being used to prop up dementia care, currently one of the three big arms of the Prime Minister’s Dementia Challenge, has gained some momentum, for example here. Bonds are effectively “IOUs“, and concerns remain for them as in the private finance initiative – such as who actually benefits, the prolonged threat of penalty for not being able to meet your loan repayments, the issue of who decides the outcomes by which performance will be assessed, and who actually manages or controls the enterprise.
Social Impact Bonds (SIBs) are depicted as “a way of enabling innovation, creating flexible contracts around social outcomes and providing linked investment“. But for some, they are a vehicle for enabling ‘privatisation by stealth’.
The current Labour opposition officially is trying to distance itself from any mechanisms promoting the privatisation of the NHS, and yet it is known Chris Ham and Norman Lamb wish to publish a report imminently on the possible use of SIBs in policy under the auspices of the King’s Fund.
This is the title slide of Hazel Blears’ presentation for the Alzheimer’s Show on Friday.
And here is a section of her talk.
[apologies for the sound quality]
Hazel has a strong personal attachment to campaigning on dementia, and is particularly interested and influential in the direction of travel, not least in her rôle as Vice Chair of the All Party Parliamentary Group on dementia, a cross party group made up of MPs and Peers with an interest in dementia.
Andy Burnham MP, Shadow Secretary of State for Health, has made it clear that it is his firm and settled intention to repeal the Health and Social Care Act (2012). The current Prime Minister’s Dementia Challenge is to come to an end officially in March 2015.
Dementia UK set up some time ago its innovative ‘Admiral Nurses’ scheme, to provide specialist nurses who could help people with dementia and family carers to improve the quality of life of people with dementia and family carers.
Burnham has also let it be known that he intends to subsume social care within the NHS under the construct of ‘whole person care’. Whichever various formulations of ‘whole person care’ you look at, you tend to find a ‘care coordinator’ somewhere. The exact job description of the care coordinator, nor indeed which specialisms might be best suited to accomplish this rôle, is somewhat unclear presently.
But it is all too common to hear of people being diagnosed with dementia being ‘lost in the system’, sometimes for years without follow up.
A “care coordinator” might help to boost access to the following services: emotional support, enable short breaks for people with dementia and anyone in a caring role, promote nutritious meals, ensure medications are given on time, ensure the correct medications have been subscribed (for example avoiding antipsychotic medications in individuals who might be unsuited to these), advice about suitable housing (including downsizing), ensure all physical commodities are properly medically managed; and so the list goes on.
I feel it’s pretty likely there’ll be a ‘first mover advantage‘ effect for any entity which takes up this coordination rôle in dementia care. But the tension between this and the Opposition’s policy is palpable: one cannot talk of this entity being ‘the first to enter the market’, as many wish (and expect) Labour to abolish the internal market in health care.
Such a coordinating entity could well be a recipient of a SIB – but is this like the PFI of social care? PFI by and large has an incredibly negative press amongst members of the general public.
But on the other hand, is it vindictive to prevent a social enterprise from pitching from such a service? If that entity has the technical ‘know how’ to run operations nationally competently and at a reasonable price, would that be preferable to the State running such services when projects such as NHS IT and universal credit have not gone terribly well?
In our jurisdiction, private companies can hide easily being a corporate veil, and are for example currently not readily accountable through freedom of information legislation. This is despite numerous requests to Jeremy Hunt in parliament about parity in disclosure requirements from both private and public providers.
And the track record of some outsourcing companies in the private sector, it is said, has been terrible.
Jeremy Hunt and Norman Lamb are currently in control of NHS and care policy, but there might be a fundamental change in direction from the next Government.
Or there might not be.
A person newly diagnosed with dementia has a question for primary care, and primary care should know the answer
Picture this.
It’s a busy GP morning surgery in London.
A patient in his 50s, newly diagnosed with Alzheimer’s disease, a condition which causes a progressive decline in structure and function of the brain, has a simple question off his GP.
“Now that I know that I have Alzheimer’s disease, how best can I look after my condition?”
A change in emphasis of the NHS towards proactive care is now long overdue.
At this point, the patient, in a busy office job in Clapham, has some worsening problems with his short term memory, but has no other outward features of his disease.
His social interactions are otherwise normal.
A GP thus far might have been tempted to reach for her prescription pad.
A small slug of donepezil – to be prescribed by someone – after all might produce some benefit in memory and attention in the short term, but the GP warns her patient that the drug will not ultimately slow down progression consistent with NICE guidelines.
It’s clear to me that primary care must have a decent answer to this common question.
Living well is a philosophy of life. It is not achieved through the magic bullet of a pill.
This means that that the GP’s patient, while the dementia may not have advanced much in the years to come, can know what adaptations or assistive technologies might be available.
A GP will have to be confident in her knowledge of the dementias. This is an operational issue for NHS England to sort out.
He might become aware of how his own house can best be designed. Disorientation, due to problems in spatial memory and/or attention, can be a prominent feature of early Alzheimer’s disease. So there are positive things a person with dementia might be able to do, say regarding signage, in his own home.
This might be further reflected in the environment of any hospital setting which the patient may later encounter.
Training for the current GP is likely to differ somewhat from the training of the GP in future.
I think the compulsory stints in hospital will have to go to make way for training that reflects a GP being able to identify the needs of the person newly diagnosed with dementia in the community.
People will need to receive a more holistic level of support, with all their physical, mental and social needs taken into account, rather than being treated separately for each condition.
Therefore the patient becomes a person – not a collection of medical problem lists to be treated with different drugs.
Instead of people being pushed from pillar to post within the system, repeating information and investigations countless times, services will need to be much better organised around the beliefs, concerns, expectations or needs of the person.
There are operational ways of doing this. A great way to do this would be to appoint a named professional to coordinate their care and same day telephone consultations if needed. Political parties may differ on how they might deliver this, but the idea – and it is a very powerful one – is substantially the same.
One can easily appreciate that people want to set goals for their care and to be supported to understand the care proposed for them.
But think about that GP’s patient newly diagnosed with dementia.
It turns out he wants to focus on keeping well and maintaining his own particular independence and dignity.
He wants to stay close to his families and friends.
He wants to play an active part in his community.
Even if a person is diagnosed with exactly the same condition or disability as someone else, what that means for those two people can be very different.
Once you’ve met one person with dementia, you’ve done exactly that: you happen to have met one person with dementia.
Care and support plans should truly reflect the full range of individuals’ needs and goals, bringing together the knowledge and expertise of both the professional and the person. It’s going to be, further, important to be aware of those individuals’ relationships with the rest of the community and society. People are always stronger together.
And technology should’t be necessarily feared.
Hopefully a future NHS which is comprehensive, universal and free at the point of need will be able to cope, especially as technology gets more sophisticated, and cheaper.
Improvements in information and technology could support people to take control their own care, providing people with easier access to their own medical information, online booking of appointments and ordering repeat prescriptions.
That GP could herself be supported to enable this, working with other services including district nurses and other community nurses.
And note that this person with dementia is not particularly old.
The ability of the GP to be able to answer that question on how best her patient can lead his life cannot be a reflection of the so-called ‘burden’ of older people on society.
Times are definitely changing.
Primary care is undergoing a silent transformation allowing people to live well with dementia.
And note one thing.
I never told you once which party the patient voted for, and who is currently in Government at the time of this scenario.
Bring it on, I say.
“The latest stage of the Secretary of State’s political smear campaign”
 Yesterday’s exchanges were particularly acrimonious between Andy Burnham MP, Shadow Secretary of State for Health, and Mr Jeremy Hunt. Here’s one short excerpt reported in Hansard:
Yesterday’s exchanges were particularly acrimonious between Andy Burnham MP, Shadow Secretary of State for Health, and Mr Jeremy Hunt. Here’s one short excerpt reported in Hansard:
“Andy Burnham rose—
Mr Hunt: No, I am going to make some progress. Today he had a chance to show that he had learned how wrong—
Andy Burnham: On a point of order, Mr Speaker. Is it in order for the Secretary of State to misrepresent the views of the previous Government and previous Ministers, and refuse to take interventions? He has just said that I refused to change and strengthen the regulation system of hospitals in England—that is factually incorrect. I brought forward a new system for the registration of all hospitals in England in autumn 2009, on the back of recommendations from the CQC. Again, he should get his facts straight at that Dispatch Box.”
However, it had started badly,
“Andy Burnham: How can it be appropriate to introduce a debate on such fundamentally important issues as the way we care for older people with such narrow, petty, partisan, point scoring efforts?“
Burnham then got totally exasperated.
“Andy Burnham:The Bill began as a response to the Dilnot report and a reform of social care, but has since taken in major new measures on the NHS. It deals with issues that matter greatly to millions—issues to which that very thin speech we have just heard did not do justice. Worse, it was an inappropriate attempt to turn an occasion such as this into the latest stage of the Secretary of State’s political smear campaign. I refuse to sink to his level, and instead will deal with the important issues before the House today. For clarity, I will take the issues separately—social care, then health…”
Machine politics by incremental soundbite is not a way for Jeremy Hunt to manage the NHS
 Jeremy Hunt’s tenure at the Department of Health has so far been pretty inglorious.
Jeremy Hunt’s tenure at the Department of Health has so far been pretty inglorious.
Hunt tweeted on December 13 2013, “Shocking Labour not supporting measures in Care Bill that will prevent another Mid Staffs. Have they learned nothing?”
The Care Bill is however intensely complicated. The Government plans to widen the powers of trust special administrators face opposition both within and outside Parliament. There can, of course, be grounds for hospital reconfigurations where this improves the quality of patient care, however it is essential that this takes place with proper regard to due process.
And yet Jeremy Hunt has allowed himself to be completely at the mercy of health services journalists, some of whom are not particularly bright and who have little understanding of the English law. Specialist registrars in medicine, the rank below a Consultant, can only wonder whether they wish to become a NHS consultant working in such demanding conditions.
It is clear that the Secretary of State for Health, too, cannot have that clear an understanding of the current law, as he has now lost in the second and third highest courts in England and Wales.
However, by courting certain people, Jeremy Hunt has ensured that he cannot be attacked by key personnel in the clinical regulators.
The NHS would be nowhere without the opinions and views of patient campaigners, particularly in the discussion over reconfigurations. The quality of their work continues to be astounding. The news about the Mid Staffs Trusts reconfigurations is expected shortly.
A similar issue has arisen with NHS consultant cover.
If Jeremy Hunt wants a NHS Consultant to do 24 hours for example, he presumably will have to pay another NHS Consultant to act ‘as cover’ for the next 24 hour period. Otherwise, this will offend ‘patient safety’ so beloved of many who had themselves not prevented a Mid Staffs previously.
If Jeremy Hunt wants NHS Consultants to be there seven days a week, he will presumably also pay for the formidable army of dieticians, occupational therapists, physiotherapists, speech and language therapists, nurses, healthcare allied professionals, ward clerks, and so it goes on, too. The costing figures estimating what this might cost have been virtually non-existent so far.
If Jeremy Hunt wants a NHS Consultant to do the work instead of Specialist Registrars, he must ensure that they are adequately trained and revalidated on specialist procedures such as insertion of a central line, chest drain or pacing wires, and pay for this.
Otherwise, Jeremy Hunt is all talk and no action.
It’s been long known that Tony Blair wished the civil service to be more ‘innovative’ and not act like technicians. The deprofessionalisation which the NHS finds itself now is a genuine problem.
If private providers really want ‘an equal playing field’, is it not reasonable to request private providers such as Circle, Serco or Virgin to pay for Specialist Registrar training posts in their ‘NHS hospitals’? They are, after all, using the NHS logo.
Otherwise, despite the brand loyalty, the time possibly has to come where the ‘National Health Service’ gets rebranded as a ‘whole person care service’ (or similar). The NHS is unrecognisable to how it used to be recently, and the legitimised use of the NHS logo is simply causing confusion from members of the public. This is unless of course politicians can unit on re-framing the NHS away from a pseudomarket, but as a service which is comprehensive, universal, and free-at-the-point of need.
As it is, we’re left with Jeremy Hunt and some health services journalists, and the clinical regulators, trying to move policy incrementally by soundbite, often by completely ignoring the professionals who matter: the doctors, nurses and allied health professionals. They should spend less time managing the media, and more time managing the NHS.
It’s all gimmicks, gimmicks, gimmicks.
Jeremy Hunt’s message on dementia should have been ‘screened’ for damaging myths
My presumption is that I wish to be extremely positive about HM Government’s own volition about leading the G8 with the subject of dementia.
Also, the “Prime Minister’s Dementia Challenge”, which sets out a roadmap for dementia for this year and next, has been a success which I much admire.
David Cameron and Jeremy Hunt, and their team, must rightly be applauded.
However, some accidental problems with the latest message appear to have crept in unfortunately.
The article in the Telegraph says that, “Health Secretary Jeremy Hunt says it is “utterly shocking” that only half of people suffering from dementia are being formally diagnosed.”
You can watch the video here.
Recently in English policy a skirmish over screening has been temporarily staved off by certain stakeholders avoiding ‘the S word’.
They have decided to plump for the ‘C-word instead’.
“Case-finding”
But in fairness Jeremy Hunt MP, Secretary of State for Health, in the actual “piece to camera” does not use the word “suffering”.
This is particularly ironic as Hunt later says, “”We’ve got to overcome the stigma.”
A major thrust of dementia must be to destigmatise dementia, by emphasise the myriad of things which can be done to help individuals living with dementia, like improvements of the house and the outside environment, non-statutory advocacy or dementia friendly communities.
Hunt’s attempts to overcome the stigma are, unfortunately, somewhat mitigated by his claim that,
“Dementia is a really horrible condition.”
Hunt mentions that “This is not surprisingly because memory is an intrinsic part of all of this.”
The meme that memory problems are synonymous with dementia remains a persistent toxic misrepresentation.
Not all memory problems are dementia (depression can cause profound memory problems.)
Not all dementia presents with memory problems. One of the most common forms of dementia in the age group below 60 is the behavioural variant of frontotemporal dementia.
This presents typically with an insidious change in behaviour and personality, often not noticed by the person himself or herself (but noticed by somebody close by.)
Even some of such individuals can present with plum-normal brain scans.
This small fact would aggravate hugely physics experts to sit on dementia clinical steering groups perhaps, if they knew.
A number of parliamentarians have recently emphasised the need for prevention.
This is indeed a worthy claim.
“You can change your lifestyle to help to stave off the diagnosis.”
However the evidence for this claim is extremely scant.
Non-clinicians in policy must not give false hope to members of society.
This is extremely irresponsible.
Hunt continues, “GPs have been reluctant to give a diagnosis as they’ve thought that ‘nothing is really going to happen'”
There has been in recent years a language depicting war, between GPs and persons with a possible diagnosis of dementia.
There is a very damaging myth, perpetuated by some influential people in the third sector, that GPs are actively withholding a dementia diagnosis in some people.
This claim undermines the credibility and probity of medical professionals, but GPs are relatively defenceless against such a slur.
Hunt says, “If people are worried, come and talk to your GP.”
A moral dementia policy is giving correct support including non-pharmacological interventions to support people living with dementia, as well as support for carers who often experience significant pressures in caring themselves.
People need to be accurately diagnosed with dementia. A wrong ‘label’ of dementia, for a person with no dementia, can do much harm.
Nonetheless, the idea of identifying correctly new people with dementia such that they can be given the right support is a commendable one.
It’s essential though that we do not enmesh this with this policy goal becoming targets, and clinicians being thrown off track by perverse incentives which are not directly beneficial to patients of the NHS.
Joke of the week goes to the Telegraph for “Return of the Family Doctors”
This is an extract from a brilliant article by Matthew Norman this week entitled, “A proper GP can be a pain in the wallet”.
It even made tonight’s #WTPS (“What the papers say”) on BBC Radio 4.
Reactions to Jeremy Hunt’s “nominated Doctor” for over 75s have been generally underwhelming.
Some have even mooted whether the lack of nominated doctor for people with numerous comorbidities, and 75 years or under, may even be an offence of age discrimination under the Equality Act (2010).
Should Doctors and Nurses act as surrogate immigration officials?
 Anyone can get very ill at any time.
Anyone can get very ill at any time.
This issue is also about recognising mutual obligations and responsibilities, and looking after all our futures.
Would you like to be a British citizen abroad in France and being refused treatment?
Nonetheless, the British media has been relentless in presenting the ‘dogwhistle’ politics of immigration, rather than having an open, honest or complete debate about the NHS privatisation enacted by this Government.
Jeremy Hunt MP says today:
Having a universal health service free at the point of use rightly makes us the envy of the world, but we must make sure the system is fair to the hardworking British taxpayers who fund it.
This current Government, it has been argued, has been extremely divisive, setting off able-bodied people against disabled citizens, employed people against unemployed, and so it goes on.
The ludicrous farce of this latest announcement, of cracking down on “health tourism”, is that similar announcements have been made before. In the meantime, Hunt has been forced to apologise for a tweet when faced with legal action, and there has been talk of an impending crisis in acute medicine.
Today’s announcement will again see Ministers facing renewed claims that GP surgeries are being turned into “border posts”.
In its three years in power the government has a poor record on announcing policies that sound good but prove to be completely unworkable
(shadow health minister Liz Kendall, previously)
The Chair of the Royal College of General Practitioners, Prof Clare Gerada, has previously warned that:
“GPs must not be a new ‘border agency’ in policing access to the NHS. While the health system must not be abused and we must bring an end to health tourism, it is important that we do not overestimate the problem and that GPs are not placed in the invidious position of being the new border agency.”
Today, the Department of Health is publishing the first comprehensive study of how widely migrants use the NHS. These independent findings show the major financial costs and disruption for staff which result from a system which will be substantially reformed in the interests of British taxpayers. Just because they are ‘independent’ findings does not necessarily mean they are very accurate, as any observer of the “output” of the OBR will tell you.
Previous estimates of the cost to the NHS have varied, but this latest attempt research reveals the cost may be significantly higher than all earlier figures.
To tackle this issue and deter abuse of the system, the #omnishambles Government is proposing the following now:-
- introducing a simpler registration process to help identify earlier those patients who should be charged.
- looking at new incentives so that hospitals report that they have treated someone from the EEA to enable the Government to recover the costs of care from their home country.
- introducing a new health surcharge in the Immigration Bill to generate income for the Government (but it is unlikely this money will go into frontline patient care, as indeed the £2.4bn “efficiency savings” have not been returned either);
- appointing Sir Keith Pearson as an independent adviser on visitor and migrant cost recovery;
- identifying a more efficient system of claiming back costs by establishing “a cost recovery unit”, headed by a Director of Cost Recovery;
Andy Burnham MP, Labour’s Shadow Health Secretary, responding to Jeremy Hunt’s announcement on overseas visitors’ and migrants’ use of the NHS, said:
We are in favour of improving the recovery of costs from people with no entitlement to NHS treatment. But it’s hard not to conclude that this announcement is more about spin than substance. The Government’s own report undermines their headline-grabbing figures, admitting they are based on old and incomplete data. Instead of grand-standing, the Government need to focus on delivering practical changes. Labour would not support changes that make doctors and nurses surrogate immigration officials.
For a video of Andy Burnham MP responding to this latest report, please go here.
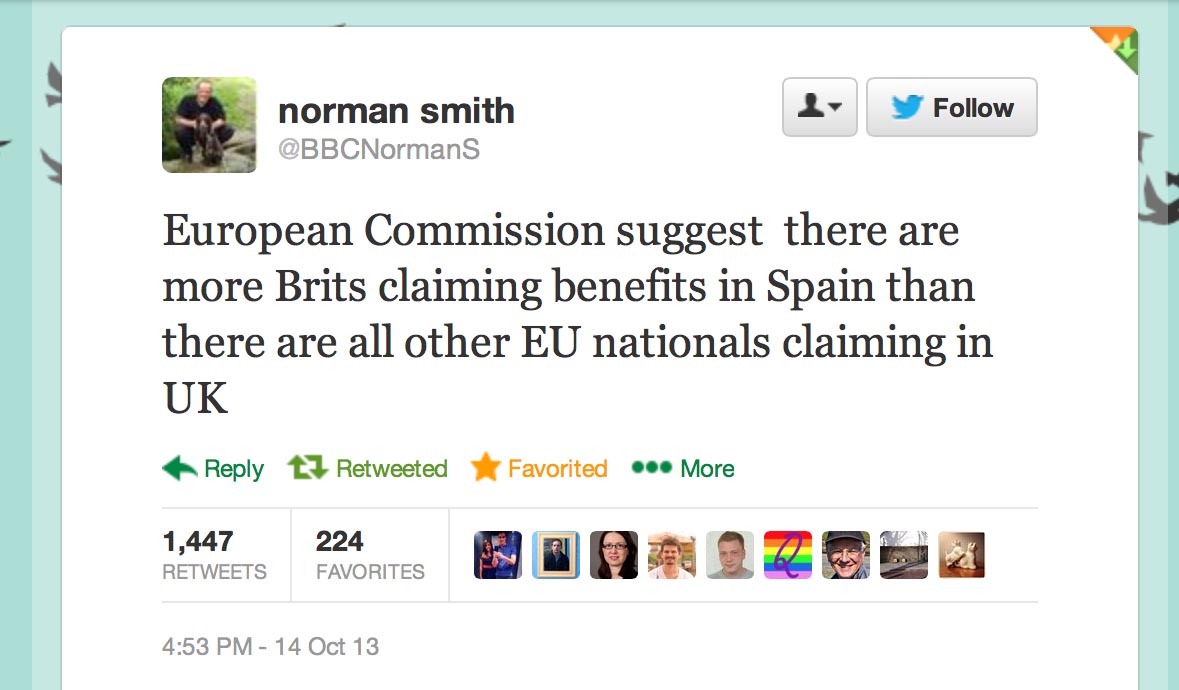
Furthermore, it appears that what Hunt won’t say about migrants is that British expatriates might make much heavier use of the NHS than any other visitors (and accordingly they should pay.)
A recent report by the European Commission concluded that so-called benefits tourism was “neither widespread nor systematic”.
As for most countries, residency not nationality primarily determines eligibility for healthcare treatment.
With the Conservative Party finding themselves ‘squeezed’ by UKIP in the run-up to the European elections, this could provide an useful smokescreen for the disaster in acute care which the Conservatives have somehow single-handedly generated.
However, the “benefits tourism” narrative of the Conservatives and UKIP was dealt a heavy blow by the emergence of this information, which the BBC’s Norman Smith tweeted earlier last week:
 Last week’s announcement by Jeremy Hunt on loneliness was panned in a widespread manner by many professionals.
Last week’s announcement by Jeremy Hunt on loneliness was panned in a widespread manner by many professionals.
Maybe for the Conservatives there is ‘no such thing as Society’ after all?
Overseas visitors and migrant use of the NHS: extent and costs