Home » Posts tagged 'integration'
Tag Archives: integration
Health and social care are ‘better together’, but a new government should still be cautious in delivery
Being cautious does not mean not changing things.
But for any change you have to take the key people with you.
For people who come into contact with the National Health Service or social care, the services are currently too bitty. It’s quite difficult to navigate your way through them.
There are further structural problems with how the service is organised for the NHS.
Ideally, there should be a consensus amongst members of political parties in doing something about the private finance initiative, or moving towards abolition of the purchaser-provider split?
Also, if ‘reconfigurations’ of NHS entities are deemed necessary, great thought should be put into the best clinically-driven as well as health economy method of doing so, involving meaningful engagement with persons and patients.
GPs, the backbone of the NHS, who are essential in providing a ‘proactive’ service for both health and illness, should not have their attention diverted into political attacks denigrating their value or into wondering whether their practices will have to shut.
With the default option now competitive tendering, this has generated a need for people who are savvy at making pitches and knowing the law. This is clearly a push of resources away from frontline care, the deliverers of which are expected to do ‘more for less’.
A brave Government will therefore have to organise better communication between the health and social care systems, and the person or patient.
It will also have to make technical adjustments to the law which currently puts competition law above clinical need (see for example the issue of mergers.)
Previous Governments in England have been great ‘reformers’, for example the Gladstone tenure.
Indeed, this Coalition inflicted a 493 page Act of parliament which had three aims: turbo boost a market, turbo boost getting rid of financially distressed hospitals, and pumping resources into an economic regulator.
This Act of parliament, accompanied by a £2 bn ‘reorganisation’, had nothing to do with patient safety. Indeed, the only clause in the Act acts to abolish the National Patient Safety Agency.
The new Government will have to be brave about funding.
For a Government of socialist flavour, this will mean avoiding at all costs compulsory personal budgets which are the shoo-horn for neoliberalism; and avoiding co-payments, which end up being a tax on the ill.
The focus of the new Government should be offering a pleasurable experience for any person using health and social care services, such that each member of the public is treated as an unique individual.
That individual is not merely a ‘collection of problems’, but has a past, present, and future, and interacts with his or her own social networks, community and environment.
The discussion to be had will at stage have to be a serious one, and there will be a need to engage the mainstream media in such a way that they evidently have had enthusiasm for (over Douglas Caswell, UKIP or Nigel Farage).
So the next Government is likely to introduce integrated or whole person care, but this should be clinically driven. Serious thought should be making each pound of healthcare spending go as far as possible, but ultimately there should be an acknowledgement that you get what you pay for.
And furthermore an ‘unsustainable’ NHS does not merely mean a NHS you wish to starve of adequate funds.
The NHS and social care systems do contain outstanding, hardworking professionals, and with the correct leadership the NHS can continue to be the ‘envy of the world’.
Hundreds of thousands of people are marching to London for September 6th to show just that.
Care at the crossroads. Burnham has something big, and you may be quite pleased to see him
Social care funding is on its knees.
Andy Burnham MP, Shadow Secretary of State for Health, addressed a sympathetic audience at the #NHSConfed2014 yesterday, talking about unlocking resources for general medicine.
We live in crazy times. Newark saw the christening of the Conservative Party as the protest party you should vote if you wanted to STOP UKIP. But let me take you back to an era when the Labour Party had principles (!) In August 1945, Aneurin Bevan was made Minster for Health following the 1945 General Election. The National Health Service (NHS) was one of the major achievements of Clement Attlee’s Labour government. By July 1948, Minister for Health, Aneurin Bevan had helped guide the National Health Service Act through Parliament.
A full day has been allocated to the Opposition health on Monday in parliament in part of their discussions on her Majesty’s Gracious Speech. Simon Stevens – NHS England’s new chief – has asked for solutions for well rehearsed issues, and Andy Burnham is clear that this is no time for another apprentice like Jeremy Hunt. Whilst being upbeat about the future of the health and social care system, he wants to move away from a “malnourished system”, with carers employed on zero hours contracts and less than the minimum wage. Indeed, this is a serious issue which has caused me some considerably anxiety too. A “product of [my] time in Government”, clearly this framework has also benefited from a parliamentary term in opposition.
Burnham crucially identifies not an inefficiency in which money is spent (although the ongoing Nicholson savings rumble on). But he does identify an inefficiency in outcomes (such as the near-inevitable fractured neck of the femur in the leg for a seemingly-trivial cost-saving in not purchasing a grab handrail). Labour, inevitably, though has an uphill battle now. The system appears to encourage the medical model of care, according to Burnham, encourages hospitalisation of people, so it is not simply a question of throwing money at the service. People are more than aware that an ‘unsustainable NHS’ is in a nutshell code for a NHS starved of adequate fundings.
Burnham feels that you can’t half-believe in ‘integration’, and is mollified about the consensus about a need for integration across all main political parties.
“I am really worried that the ‘Better Care Fund‘ might give integration a bad name”, comments Burnham.
People who have watching Burnham’s comments will note how Burnham has openly commented how he feels he has been misled by certain think-tanks in the past. A period of opposition has enabled Burnham conversely to obtain a crisis of insight. And yet he talks about his “precious moment” in order “to build a consensus of shared endeavour, which I intend to use to the full and very carefully.” Intriguingly, he does not wish to ‘foist a grand plan’ on voters after the next general election. This is of course is political speak for his ‘shared agenda’, driving a cultural change by stakeholders within the system. This is precisely what Burnham feels he has achieved through the commission on whole person care by Sir John Oldham.
“Not a medical or a treatment model, but a truly preventative service, that can at last aspire to give people a state of physical, mental and social wellbeing.”
Burnham wants to put a stop to the ‘random set of disconnected meetings with individuals within the service.’
An exercise was carried out at the start of the NHS.
This is the famous leaflet.
Burnham desires a new leaflet from an incoming Labour government to introduce how social care can become under the umbrella of the National Health Service.
“Going forward, you should expect to receive much more support in your home. The NHS will work to assemble one team to look after you covering all the needs you have. We want to build a personal solution that works for you, for your family, and for your carers, because if we get right at the very outset and the very beginning it’s more likely to work for you and give you what you want, and cost us all much less. We want you to have one point of contact for the co-ordination of your care. We know you are fed up with telling the same story to everyone who comes through the door. It’s frustrating for you, and wasteful for us. To get the care that you’re entitled to, when and where you want it, you will have powerful new rights set out in the NHS Constitution such as the right to a single point of contact for the coordination of all of your care and a personalised care plan that you have signed off. But – and there is a big but – to make of all this happen, you will changes in your local NHS, and, in particular, you will changes in your local hospital. We can do a better job of supporting you where you want to be, we won’t need to carry out as much treatment in hospitals, or have as many hospital beds. It is only by allowing the NHS to make this kind of change to move from hospital to home that we will all secure it for the rest of this century.”
Burnham feels that the NHS must be the ‘preferred provider’ and the DGH should be allowed to reinvent itself - building the notion of one team around the person. I personally have formed the opinion: “close smaller hospitals at haste, and repent at leisure“. Critics of marketisation will inevitably point out the blindingly obvious: that even with a NHS preferred provider, there’s still a market, and nothing short of abolition of the purchaser-provider split will remedy the faultlines. There could be a one person tariff or one person budget for a person for a year. It would give an acute trust a much more stable platform, according to Burnham, in contradistinction to the activity based tariff. This does require some rejigging of how we have the proper financial performance management system in place: there should be a drive, I feel, for rewarding behaviours in the system that promote good health rather than rewarding disproportionately the work necessary to deal with failures of good control, such as dialysis, amputations or laser treatment.
Burnham is clearly inspired by the ‘Future Hospitals’ soundings from the Royal Colleges of Physicians, focused on a new generation of generalist doctors working across boundaries of primary and secondary care:
“Since its inception, the NHS has had to adapt to reconcile the changing needs of patients with advances in medical science. Change and the evolution of services is the backbone of the NHS. Hospitals need to meet the requirements of their local population, while providing specialised services to a much larger geographical catchment area.”
Burnham even talks about possibly reviewing the “independent contractor” status of GPs.
Centralised care is mooted for people in life threatening situations. But Burnham has found that barriers to service reconfiguration exist through the current competition régime and market, with integration encouraging in contrast to collaboration, people before profit, and merge “without the nonsense of competition lawyers looking over their shoulders”. Therefore, Burnham repeats his pledge to remove the Health and Social Care Act (2012), which has driven “fragmentation, complexity and greater cost”. Under this construct, section 75 and its associated Regulations is disabling rather than enabling for health policy. There is clearly much work to be done here to make the legislation fit for purpose, as indeed I have discussed previously. Wider dangers are at play, as Burnham well knows, however. Here he is speaking about his opposition to TTIP (the EU-US Free Trade Treaty) which the BBC News did not seed fit to cover despite their Charter requirements for public broadcasting. And here is George Eaton writing about his opposition to TTIP in the New Statesman.
Burnham is clearly, to me, positioning himself to the left, distancing himself from previous Labour administrations. There are clearly budgets in the system somewhere, and while Burnham talks about unified budgets he does not put the emphasis on personal budgets. There is no doubt to me that personal budgets can never be ‘compulsory’, and each person group (e.g. people living with dementia) presents with unique challenges. It’s clear to me that deep down Andy Burnham is still in principle keen on something like the ‘National Care Service’, in preference to any gimmicks from the Cabinet Office. Burnham in the Q/A session with Anita Anand indeed describes how this had been thrown into the long grass at the time of Labour losing the general election in 2010, but how paying for social care in 2014 is as fundamentally unfair as paying for medicine had been pre-NHS according to Burnham. This would take some time to put in place, such as a mechanism for a mandatory insurance system, and a proper care coordinator infrastructure. And these are not without their own controversies. But, with Miliband playing safe one unintended consequence for neoliberal fanatics has been that it has not been possible to impose a strong neoliberal thrust to whole person care; and whatever Miliband’s personal preferences, the pendulum to me is definitely swinging to the left. Burnham talks specifically about a well planned social care system as part of the NHS.
And so Burnham looks genuinely burnt by previous administrations, and, whilst certain key players will want personal budgets and competition to be playing a greater part in policy, it appears to me that the current mood music is for Labour not appearing to promote privatisation of the NHS in any form. The ultimate success of the next Labour administration will be determined by the clout of the Chancellor of Exchequer, whoever that is. It could yet be Ed Balls. For matters such as ‘purse strings’ on the social impact value bond or the private finance initiative, Burnham may have to slog out painful issues with Balls in the way that Aneurin Bevan once did with Ernie Bevin in a previous Labour existence. Burnham’s problem is ensuring continuity with the current system where services have been proactively pimped out to the private sector, but ultimately it is the general public who call the shots. Burnham knows he’s onto something big, and, for once, some people may be quite pleased to see him.
Will looking for blame in the ‘prime contractor model’ end up like one giant “pass-the-parcel”?
In a previous article of mine, “Outsourcing has become a policy drug, and they need to kick the habit”, I explained how the aspiration to have a smaller State had led to “reform” of the public services where the situation was now far worse.
Public money is being siphoned off into private sector shareholder dividends. Worse still, some performance monitoring of ongoing contracts is terrible. Furthermore, many outsourcing companies are currently embroiled in criminal allegations of one sort of another, mainly fraud.
It does seem a laudable aim to integrate healhcare (including mental health care) and social care. Indeed, by calling it ‘whole person care’, you temporarily get round the comparison to the ‘integrated shared care plans” of the United Staes.
The Health and Social Care Bill initially started life as the tr0jan horse of competitive markets into the NHS. Once this approach under Earl Howe blatantly fell apart, Norman Lamb was left to bring up the policy rear by talking about “integrated care”. However, the problem with integrated care is that it is yet again being launched as a launchpad for private providers to rustle together huge packages across a number of different areas through subcontracting.
Of course, one can argue that it’s great that a private provider can take control of so many different diverse services. But remember when the same argument was used to attack the NHS as ‘outdated’, ‘bloated’ and ‘Stalinist’? Such arguments for economies of scale or promotion of a coherent national health policy were jettisoned in favour of a fetish for introducing the market into the NHS at high speed. Unfortunately this policy has been totally discredited.
On the “prime contractor model”, the eminent health commentator Roy Lilley remarks:
Is this novel contacting or dumping the problem on someone else. Imaging trying to unpick a problem in the pathway. Everyone will blame someone else. This is a giant game of pass the parcel, isn’t it? The prime contractor may be accountable but they will pass the accountability up the line, delays will occur in getting answers. They will become a CCG-lite.
The prime contractor model involves a single organisation subcontracting work to other providers to integrate services across a pathway. A proportion of payments is dependent on the achievement of specific outcomes. Dozens of clinical commissioning groups are already said to be devising “innovative” contracts in which a lead provider receives an outcomes based payment to integrate an entire care pathway. For example, if the £120m deal is finalised, Circle ? which also runs Hinchingbrooke Health Care Trust ? will be financially and clinically accountable to commissioners for the whole pathway. The CCG said this previously involved 20 contracts across primary, secondary and community services. That news came after Bedfordshire CCG was named private company Circle as its preferred bidder to be “prime contractor” for an integrated musculoskeletal service.
Outsourcing companies don’t particularly appear to care what sectors they operate in, whether it’s in the running of healthcare, asylum seeking or probation services. Such an approach therefore lends itself easily to each citizen becoming a number not a name. The idea of us all having a special ‘services mastercard’ is not that far-fetched now, and if one day NHS budgeting is linked up with benefits, we’ll be yet closer to this ‘brave new world’.
In March 2012, G4S won a massive £30 million UK Border Agency contract to house asylum-seekers in the Midlands, the East of England, the North East, Yorkshire and Humberside. Using the “prime contractor model”, which G4S tells investors is “attractive”, the company granted subcontracts to UPM and the charity Migrant Help. And yet, in July 2013, Stephen Small, G4S managing director for Immigration and Borders, and Jeremy Stafford, Serco CEO for the UK and Europe were forced to defend their record before the Home Affairs Committee into the asylum system.
Serco’s evidence to the Committee revealed that in the North West it directly manages homes for asylum seekers through what the chair Keith Vaz described as ‘around twenty subcontractors from Happy Homes Ltd to First Choice Homes and Cosmopolitan Housing’.
Jeremy Stafford of Serco claimed this apparent recipe for housing management disaster was in fact a proven way of outsourcing and privatisation. It is ‘a very effective model and we do that in a number of the services we deliver’, he said.
This confidence in the ‘new delivery model’ of privatisation in the COMPASS contracts seems somewhat misplaced in the context of the JRF evidence. For it reveals that Reliance, the other security company with asylum housing contracts in London, the South West and Wales, sold on the privatised contracts after only two months to Capita and Clearel. The new provider, Clearel, did not fulfil the requirements of the contracts as tendered.
Only this week, the Serco boss quit. Four of the government’s biggest suppliers – G4S, Serco as well as rivals Capita and Atos – have been called to appear before a committee of British lawmakers next month for questioning about the outsourcing sector. Serco, which makes annual revenue of around 4.9 billion pounds, has continued to win deals in its other markets, such as a 335 million pound tie-up to run Dubai’s metro system, though it has encountered some problems abroad.
But back to G4S. There is even some reference to problems in the past on the G4s Welfare to Work website:
G4S Welfare to Work knows that most of the services needed to support workless people into meaningful, progressive employment in the UK already exist. What has been missing is an effective structure for managing and coordinating that provision.
… We are:
…
Operating a unique model for the delivery of welfare-to-work services that learns from mistakes made in previous Prime Contracting models, and builds on what works.
As I have described also in a previous article on this blog, one facet of globalisation is that it has become extremely difficult to regulate the behaviour of multinational corporations involved in healthcare.
G4s has now been ‘accused of “shocking” abuses and of losing control at one of South Africa’s most dangerous prisons‘. The South African government has temporarily taken over the running of Mangaung prison from G4S and launched an official investigation. It comes after inmates claimed they had been subjected to electric shocks and forced injections. G4S says it has seen no evidence of abuse by its employees. However, the BBC has obtained leaked footage filmed inside the high security prison, in which one can hear the click of electrified shields, and shrieking. It also shows a prisoner resisting a medication.
I have previously on this blog described the legal problems with the “prime contractor” model.
I have said before, and I will say it again. Especially since these contracts can be of such a long duration (for example, ten years), it is absolutely essential there are rigorous mechanisms for ongoing and continuous monitoring of performance. This way commissioners can spot easily and early on when providers are running into difficulties.
The English law gives a complex message on whether a private provider can still take the money and run, even if it doesn’t fulfill part of its side of the bargain in a contract.
Take for example the case of Sumpter v Hedges [1898] 1 QB 673 in the English Court of Appeal.
This was a matter where the plaintiff was contracted to erect certain buildings on the grounds of the defendant for a lump sum of 565 pounds, but the plaintiff was only able to do part of the work to a value of 333 pounds, with the defendant subsequently completing the rest of the work. As a result, the plaintiff sued on quantum meruit (as much as he or she has earned) appealing from the judgment of the trial judge who awarded the plaintiff for the value of the materials used, but nothing in respect to the work done.
The Court of Appeal upheld the trial judge’s decision and held that the plaintiff could not recover from the defendant in respect to the work done as part of quantum meruit due to the fact that the contract was for a lump sum, and there was no evidence that an agreement for part performance was formed.
While spinners are giving themselves multiple orgasms over ‘transparency and disclosure’ in the new Jerusalem of the NHS, it appears that “the fair playing field” of private and public health providers regarding basic patient safety is a complete fiasco.
Grahame Morris MP recently reviewed the gravity situation on the influential “Our NHS” website:
While public services are being outsourced to the private sector, especially in the NHS, Freedom of Information responsibilities are not following the public pound. Private health care companies can hide behind a cloak of commercial confidentiality when barely transparent contracts are awarded.
At the start of the bidding process private providers already receive a competitive advantage due to unequal disclosure requirements.
Private companies are free to use the Freedom of Information Act to gain detailed knowledge of a public sector provider, which can then be used to undercut or outbid the same public body when the contract is put out for tender.
NHS bodies must answer Freedom of Information requests relating to costs, performance and staffing. Yet a private provider has no similar duty of disclosure despite the fact they could have treated private patients for many years.
Once a contract is awarded, there is little that can be done if a private provider refuses to supply details to allow commissioning bodies to answer Freedom of Information requests. As they are not subject to Freedom of Information laws, the Information Commissioner has no power to investigate private contractors. They cannot serve notices for an investigation, and neither can they take enforcement action if a contractor destroys information or fails to comply with a request.
As a result of the decision in Sumpter and other similar decisions, the common law had subsequently recognised some exceptions to the general rule other than that performance of a contract must be exact and complete according to the terms. Furthermore, there is nothing preventing parties to a contractual relationship to vary or discharge the agreement, and can do so in a few ways.
One such way is “mutual discharge”, where both parties agree to release one another from what was agreed upon before either party has performed any of the acts promised. Another way is “release by one party”, where one party has completed their contractual promise, and agrees to release the other party from further performance of the contract.
Anyway, the “pass the parcel” analogy may not be entirely accurate.
It more be of the case that someone is holding a highly explosive bomb eight years into a ten year “prime contractor model” contract when it suddenly blows up.
And you can bet your bottom dollar that the Secretary of State for Health will definitely not be to blame.
What’s best for a person isn’t necessarily what’s best for a hospital
It is pretty clear that the NHS as currently engineered puts Foundation Trusts on an elevated platform. Hospitals, being paid on the basis of activity involved for any one patient, can act for a sink for funding, when the health of any particular person is not easily matched to the aggregate level of activity for that person in a hospital.
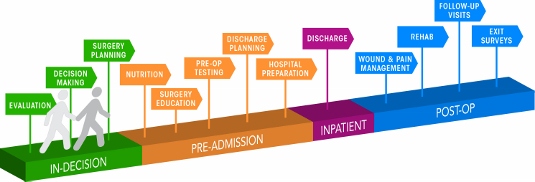
The problem with ‘money following the patient‘ is it depends on whether you view it to be a success or failure that more money is spent on you the more ill you become. When a patient is admitted for an acute medical emergency in England, the care pathway can be pretty unambiguous. Most reasonable doctors on hearing about a history of cough, sputum and temperature, for a person with new breathing difficulties, on seeing the appropriate chest x-ray, would embark on a management of pneumonia; depending on the hospital, the course of antibiotics would be pretty standard from i.v. to oral, and the person would end up being discharged.
However, ‘activity based costing‘ and ‘payment by results‘ for hospital totally ignore the health of a person outside hospital. And if a healthcare model is to shift with time to ‘whole person care‘, what happens to a person outside of hospital is going to become increasingly important. If a person is better ‘controlled‘ for diabetes in the community, it is hoped that emergency admissions, such as for the diabetic ketocacidotic coma, can be avoided; or for example if a person is able to monitor their breathing peak flow in the community and notice the warning signs (such as a change in the colour of sputum), an acute exacerbation of chronic obstructive pulmonary disease may be headed off at the pass.
Medicine is not an exact art or science, and the approach of ‘payment-by-results’, of a managerial accounting approach of activity-based costing, is at total odds to how decisions are actually made. Even in complex economics, within the last decade or so, the idea of “bounded rationality” has conceded that in decision-making, rationality of individuals is limited by the information they have, the cognitive limitations of their minds, and the finite amount of time they have to make a decision. Many ‘decision makers’ are not in fact perfectly rational, and it is likely that even the best doctors will differ in exact details for management of a patient in hospital for any given set of circumstances.
In health care, value is defined as the patient health outcomes achieved per pound spent. Value should be the pre-eminent goal in the health care system, because it is what ultimately matters for patients. Value encompasses many of the other goals already embraced in health care, such as quality, safety, patient centeredness, and cost containment, and integrates them.
However, despite the overarching significance of value in health care, it has not been the central focus.
The failures to adopt value as the central goal in health care and to measure value are arguably the most serious failures of the medical community.
Health care delivery involves numerous organisational units, ranging from hospitals, to departments and divisions, to physicians’ practices, to units providing single services. The fundamental failing has been not to acknowledge how all these units interact in the “patient journey”.
In health care, needs for specialty care are determined by the patient’s medical condition. A medical condition is an interrelated set of patient medical circumstances — such as breast cancer, diabetes, inflammatory bowel disease, asthma, or congestive heart failure — that is best addressed in an integrated way. Therefore, a patient can be ‘plugged into the system’, as Mr X attending the specialist cystic fibrosis clinic at a local hospital. However, it is equally true to say that there are many patients with many different conditions, which interact either in disease process or treatment. And there are people who may later develop a medical illness who are perfectly well at any one ti,e.
For primary and preventive care, value could be measured for defined patient groups with similar needs. Patient populations requiring different bundles of primary and preventive care services might include, for example, healthy children, healthy adults, patients with a single chronic disease, frail elderly people, and patients with multiple chronic conditions. Each patient group has unique needs and requires inherently different primary care services which are best delivered by different teams, and potentially in different settings and facilities. However, life is clearly not so simple, and the beauty about the National Health Service is that it does not consider a person as the sum of his individual insurance packages.
Care for a medical condition (or a patient population) usually involves multiple specialties and numerous interventions. The most important thing here is that value for the patient is created not by any one particular intervention or specialty, but by the combined efforts of all of them. (he specialties involved in care for a medical condition may vary among patient populations. Rather than “focused factories” concentrating on narrow sets of interventions, we need integrated practice units accountable for the total care for a medical condition and its complications. To give as an example, optimal glucose control for diabetes in the community could possibly mean fewer referrals to the specialist eye clinic for the condition of diabetic retinopathy, an eye manifestation of diabetes, or to the vascular surgeon for a gangrenous toe requiring amputation.
A major barrier to delivering this care will be a fragmented, outsourced or privatised, NHS. In care for a medical condition, then, value for the patient is created by providers’ combined efforts over the full cycle of care — not at any one point in time or in a short episode of care. The only way to accurately measure value, then, is to track individual patient outcomes and costs longitudinally over the full care cycle. And this will be difficult the more care providers there are for any one patient.
Although outcomes and costs should be measured for the care of each medical condition or primary care patient population, current organisational structure and information systems make it challenging to measure (and deliver) value. Thus, most providers fail to do so. Providers tend to measure only the portion of an intervention or care cycle that they directly control or what is easily measured, rather than what matters for outcomes. For example, current measures often cover a single department (too narrow to be relevant to patients) or outcomes for a hospital as a whole, such as infection rates (too broad to be relevant to patients). Or providers measure what is billed, even though current reimbursement is for individual services or short episodes.
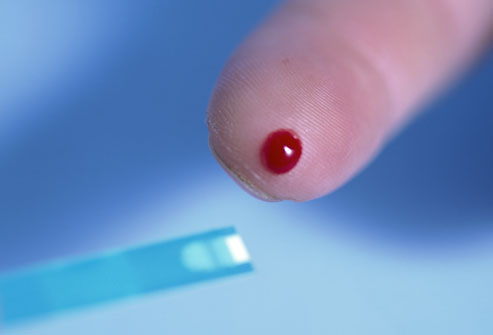
A way to get round this problem is to consider “indicators” which are are biological measures in patients that are predictors of outcomes, such as glycated hemoglobin levels (“HBA1c”) measuring blood-sugar control in patients with diabetes. Indicators can be highly correlated with actual outcomes over time, such as the incidence of acute episodes and complications. A HbA1c can be a good indicator of the compliance of an individual with diabetes with his or her medication or diet.
Indicators also have the advantage of being measurable earlier and potentially more easily than actual outcomes, which may be revealed only over time.
This is where over-focus on the wrong measure can be unhelpful. The launch of the ‘friends and family test’, which has seen an explosion of innovative technologies being sold to NHS Foundation Trusts over all the land, may be an important means of ensuring patient safety. Or it may not. We don’t know, as the data on this doesn’t exist.
However, patient satisfaction has multiple meanings in value measurement, with greatly different significance for value. It can refer to satisfaction with care processes. This is the focus of most patient surveys, which cover hospitality, amenities, friendliness, and other aspects of the service experience. Though the service experience can be important to good outcomes, it is not itself a health outcome. The risk of such an approach is that focusing measurement solely on friendliness, convenience, and amenities, rather than outcomes, can distract providers and patients from value improvement.
Value measurement in health care today in the English NHS is rather limited, and highly imperfect. Most physicians lack critical information such as their own rates of hospital readmissions, or data on when their patients returned to work. Not only is outcome data lacking, but understanding of the true costs of care is virtually absent. Most physicians do not know the full costs of caring for their patients — the information needed for real efficiency improvement.
In the recent target-driven culture of the English NHS, senior physicians are well aware of how length-of-stay has been gamed so there has been a ‘quick in and quick out’ mentality, seeing readmission rates for certain patients with cardiovascular or cerebrovascular disease sky-high.
At worst, what could have been a properly managed non-ST-elevation acute coronary syndrome ultimately ends up being a full-blown heart attack. Or what could have been a minor transient ischaemic attack ends up being a full-blown haemorrhagic stroke, causing a patient to be in a wheelchair and numerous healthcare teams looking after him or her.
Today, measurement focuses overwhelmingly on care processes. Processes are sometimes confused or confounded not only with outcomes, but with structural measures as well. Radiologists focus on the accuracy of reading a scan, for example, rather than whether the scan contributed to better outcomes or efficiency in subsequent care. Cancer specialists are trained to focus solely on survival rates, overlooking crucial functional measures in which major improvements vital to the patient are possible.
Cost is among the most pressing issues in health care, and serious efforts to control costs have been under way for decades. At one level, there are endless cost data at all levels of the system. However, as an ongoing project with Robert Kaplan makes clear, we actually know very little about cost from the perspective of examining the value delivered for patients.
Understanding of cost in health care delivery suffers from two major problems. The first is a cost-aggregation problem. Today, health care organisations measure and accumulate costs for departments, physician specialties, discrete service areas, and line items (e.g. supplies or drugs). As with outcome measurement, this practice reflects the way that care delivery is currently organised and billed for. Today each unit or department is typically seen as a separate revenue or cost centre. Proper cost measurement is challenging because of the fragmentation of entities involved in care.
To understand costs properly, they must be aggregated around the patient rather than for discrete services, just as is the case with outcomes. It is the total costs of providing care for the patient’s medical condition (or bundle of primary and preventive care services), not the cost of any individual service or intervention, that matters for value. If all the costs involved in a patient’s care for a medical condition — inpatient, outpatient, rehabilitation, physiotherapy, dietician, occupational therapy, diagnostic services, pharmacy, physician services, equipment, facilities — are brought together, it is then finally possible to compare the costs with the outcomes achieved.
Proper cost aggregation around the patient will allow us to distinguish charges and costs, understand the components of cost, and reveal the sources of cost differences.
Today, most physicians and provider organisations do not even know the total cost of caring for a particular patient or group of patients over the full cycle of care. There has been no reason to know, and Doctors resent turning their profession of medicine into one of bean-counting.
In aggregating costs around patients and medical conditions, we quickly arrive at the second problem: “the cost-allocation problem“. Many, even most, of the costs of health care delivery are shared costs, involving shared resources such as physicians, staff, facilities, equipment, and overhead functions involved in care for multiple patients. Even costs that are directly attributable to a patient, such as drugs or supplies, often involve shared resources, such as units involved in inventory management, handling, and set-up (e.g., the pharmacy). Today, these costs are normally calculated as the average cost over all patients for an intervention or department, such as an hourly charge for the operating room. However, individual patients with different conditions and circumstances can utilize the capacity of such shared resources quite differently.
The NHS in England has latterly become obsessed by its “funding gap”. Much health care is delivered in over-resourced facilities. Routine care, for example, is delivered in expensive hospital settings. Expensive space and equipment is underutilised, because facilities are often idle and much equipment is present but rarely used. Skilled physicians and staff spend much of their time on activities that do not make good use of their expertise and training. It is not uncommon for junior doctors to end up spending hours in a hospital taking blood, putting in catheters, or putting in venflons.
It is likely that ‘payment-by-results’ will at some stage have to go. Reimbursement should cover a period that matches the care cycle. For chronic conditions, bundled payments should cover total care for extended periods of a year or more. Aligning reimbursement with value in this way rewards providers for efficiency in achieving good outcomes while creating accountability for substandard care.
Improvements in outcomes and cost measurement will greatly ease the shift to bundled reimbursement and produce a major benefit in terms of value improvement. Current organisational structures, practice standards, and reimbursement create obstacles to value measurement, but there are promising efforts under way to overcome them.
The “payment-by-results” model is a complete anethema to how decisions are made in the real world. Prospect theory is a behavioral economic theory that describes the way people choose between probabilistic alternatives that involve risk, where the probabilities of outcomes are known. The theory states that people make decisions based on the potential value of losses and gains rather than the final outcome, and that people evaluate these losses and gains using certain heuristics. The model is descriptive: it tries to model real-life choices, rather than optimal decisions. The theory was developed by Daniel Kahneman, a professor at Princeton University’s Department of Psychology, who won the Nobel Prize for economics in 2002.
It is a pity that the payment-by-results ideology has been so overwhelming, perhaps powerfully pushed for by the accountants and management consultants wishing to drive ‘efficiency’ in the NHS, taking the media with them on this escapade. However, it is poorly aligned to how healthcare, psychiatric care and social care professionals make decisions in the real world.
Critics will correctly argue that value is notoriously difficult to measure, and might be virtually impossible to measure across a ‘care cycle’. Indeed the original criticism of the Kaplan and Cooper (1992) account of ‘activity based costing’ warned against organisations allocating excessive resources to collecting information which they are then able to make use of properly.
We are quickly coming to an age where it is going to be a ‘good outcome’ to keep a frail patient out of hospital through high quality care in the community through integrated teams. By that stage, the ideological shift from cost to value will have needed to have taken place, and funding models will have to reflect more the drive towards value and ultimate clinical outcome.
“Co-epetition” – how collaborative competition might ultimately benefit the patient
The debate about competition is polar. Either you’re a believer or not.
Yet competition can co-exist with collaboration. Also, in theory, integration or bundling could even be seen as ‘anti-competitive behaviour’.
A trick will be ultimately to find a way in which integration of services cannot offend competition law. As an useful starting point, Curry and Ham (2010) suggest that there are three levels of integration, the top of which is a “a macro-level or systems-level integration”, in which a single organisation or network takes full clinical and fiscal responsibility for the spectrum of health services for a defined population, Underneath is a “meso-level integration of services” for patients with particular conditions, which encompasses a continuum of care for a subset of patients with those conditions.
Ultimately, clinical commissioning groups, whatever expertise they precisely consist of, will need to source services which promote highest quality and best choice for its patients. And yet the law has to reconcile one of its fundamental rules (that everyone is innocent unless otherwise proven guilty), and the law should not penalise people wishing to work together if it is for the benefit of the patient. One is reminded of Diogenes of Sinope (412-323 B.C.) who was seen roaming about Athens with a lantern in broad daylight and looking for an honest man but never finding one.
“Co-epetition” can mean a ‘joint dominance’ of suppliers of health services, provided their activity does not abuse that dominance or distort the market. There are good reasons in business management why certain parties might choose to coordinate their commercial conduct to benefit patients, such as in bundling. Despite certain conflicting interests, they also share strong common values and are exposed to common risks. Such synergies in competences is well known to be essential for building cohesive organisational entities, and in forcing strategic alliances even if there is formal relationship at all.
Unfortunately, joint or collective dominance has been traditionally treated by the Competition Authorities as equivalent to oligopolistic dominance. The concept of joint dominance has been developed under both Article 102 of the Treaty on the functioning of EU. There is some consensus among National Health Service (NHS) researchers, managers and clinical leaders that increased integration within the health system will enable the NHS to respond better to the growing burden of chronic illnesses. In “real markets”, the prohibition laid down in Article 102 TFEU has been justified by the consideration that harm should not be caused to the consumer, either directly or indirectly by undermining the effective competition. However, healthcare is not a “real market”. Unlike the other concepts, co-opetition (blend of cooperation and competition) focuses on both cooperation and competition at the same time.
Basic principles of co-opetitive structures have been described in game theory, a scientific field that received more attention with the book “Theory of Games and Economic Behavior” in 1944 and the works of John Forbes Nash on non-cooperative games. It is also applied in the fields of political science and economics and even universally [works of V. Frank Asaro, J.D.: Universal Co-opetition, 2011, and The Tortoise Shell Code, novel, 2012]. Although several people have been credited with inventing the term co-opetition, including Sam Albert, Microsoft’s John Lauer, and Ray Noorda, Novell’s founder, its principles and practices were fully articulated originally in the 1996 book, “Co-opetition”, by Harvard and Yale business professors, Adam M. Brandenburger and Barry J. Nalebuff.
One sincerely hopes that NHS management will be able to cope with the pace of this debate too. Competitors with such management ability will likely forge a co-opetitive relationship. When two companies compete fiercely in a market, they likely perceive each other as an enemy to defeat, and have less willingness to collaborate, even if they have complementary skills and resources. One day, the best minds in the world will probably ‘have a go’ at producing a coherent construct of this for the NHS quasimarket.
“Co-epetition” provides, furthermore, a mechanism for English health policy to revisit yet again the notion of “public private partnerships” which first probably became really sexy about a decad ago at the heart of the government’s attempts “to revive Britain’s public services”. A decade later, Cameron is still lingering with this particular revival. The problem with how this is sold is that many have rightly rubbished the idea that the private sector is necessarily more “efficient”, an ab initio basic assumption, The private sector, both accidentally and sometimes quite deliberately, introduces needless reduplication and waste, evidenced by the cost of wastage in the US health market. However, the “dream” is that, in trying to bring the public and private sector together, the government hopes that the management skills and financial acumen of the business community will create better value for money for taxpayers.
Globally, diabetes is the second biggest therapeutic “market segment”, behind oncology, in terms of revenues generated. IMS Institute of Healthcare Informatics forecasts that the global diabetic segment will grow to $48-53 billion by 2016. In India, it is already the fastest growing segment. Diabetes medicines currently fall into two broad categories — tablets and injectable insulin. While domestic players are market leaders in the conventional oral drugs segment (market share of 80 per cent), multinational corporations (17 percent) are fast catching up with patent-protected new generation oral drugs. The anti-diabetes market has been consistently growing well above the pharmaceutical market for the past few years. It is possible to see the future in this crowded market in a coupled business strategy that involves in-licensing one or more compounds (new products from multi-national corporations), while continuing with time tested, less expensive (own) products for the mass market.
If the NHS should wish work together with private providers in provision of integrated bundles of healthcare, and the feeling is mutual in a way which clearly promotes patient choice, assuming that all parties see a rôle for the private sector in the NHS, the legislative framework should be re-engineered immediately to reflect that. This should a pivotal task for Monitor to turn its attention to.
Whatever the precise approach taken to “co-epetition”, the current legislative guidance will need to much better defined to ensure that any form of integration does not offend the anti-competitive environment.
The author is extremely grateful for the rich conversations he has had with Dr Na’eem Ahmed who is the first person to the author’s knowledge to acknowledge the potential value of this mode of provider dynamics for the NHS.
Introducing collaboration into a competitive market: a perfect storm of NHS “bundling”?
 Andy Burnham MP, Shadow Secretary of State for Health, announced at the Labour Party Annual Conference 2012, on 3 April 2012:
Andy Burnham MP, Shadow Secretary of State for Health, announced at the Labour Party Annual Conference 2012, on 3 April 2012:
However how to bring about a collaborative NHS is a formidable ask from a NHS which has just become geared up to private competition. To give an example, “bundles” in the NHS have been used, particularly by the Liberal Democrats and a beleaguered Earl Howe, to argue a case for ‘integrated care’ which has a whole plethora of meanings to healthcare experts. “Pure bundling” refers to a situation where products A and B can only be purchased together. This is the case, for example, when buying a business class ticket on the Eurostar, which includes a meal. Transport and meal can only be purchased together. “Mixed bundling” is where A and B can be purchased separately but purchasing them together is cheaper (there can be more than two products). This is what the Commission also refers to as “commercial tying”.
Allegations of anti-competitive bundling were significant parts of the antitrust cases against Microsoft in the United States and the European Union. Article 102 TFEU and s. 18 Competition Act provide a list of example behaviours that can constitute an abuse for these purposes and they are almost identical. The precise problem is making the conclusion of contracts subject to acceptance by the other parties of supplementary obligations which, by their nature or according to commercial usage, have no connection with the contracts. For example, on 24 March 2004 Microsoft decision (IP/04/382), the Commission found that the bundling of Windows Media Player as a compulsory product to take (for free) when customers bought Windows 98 or Windows XP was an abuse of a dominant position. The reasoning was based on the fact that suppliers of competing products to Windows Media Player were being pushed out of the market. In addition to a large fine, the Commission ordered Microsoft to make the operating systems available without Windows Media Player within 90 days.
“Bundling” is a key aspect of “A fair playing field for the benefit of NHS patients” published by Monitor in February 2013.
According to Monitor,
“Commissioning a range of services from a single provider through “one block contract” contract will sometimes be the best way to secure efficient, effective and coordinated care. In such cases, commissioners must be able to determine the appropriate price for the bundled set of services. In other circumstances, bundling may exclude smaller providers who are well placed to provide one element of the service bundle.
Getting bundling decisions right is critical to delivering integrated care to patients. Our evidence suggests that the current NHS pricing system may be a barrier to make the best bundling decisions, particularly in relation to community and mental health services. Improving the pricing system entails developing standardised currencies (descriptions of what is being purchased for a given price) and better data on providers’ costs.”
In an excellent document called “The Health and Social Care Bill: Where next?” from the Nuffield Trust in May 2011, this tension between collaboration and competition had been revisited.
The authors wrote then,
“Ideally [they] should build on the Vertical Agreements Block Exemption provisions in EU competition law within Article 101 (which covers restrictive agreements) that applies to agreements entered into by two or more organisations operating at different levels along the production chain. Almost all such agreements are exempted provided that the market share of the parties is less than 30 per cent. The rules should also build on the experience of US regulators in proactively establishing examples of permitted models of competition and collaboration in so-called ‘safe harbours’, especially if the market share was greater than 30 per cent.”
This has led lawyers and philosophers to consider how we might be able to ‘collaborate in a competitive market’. David Boaz concludes that ‘collaboration is as much part of capitalism as competition.” As for the immediate problem of how bundling might be promoted in the implementation of the Health and Social Care Act, Earl Howe on 24 April 2013 seemed to appreciate that “unbundling” might lead to fragmentation, providing that,
“It is interesting that some stakeholders have raised concerns about unbundling leading to fragmentation, while others are concerned about the effects of bundling too many services together. In practice, it is for clinically led commissioners to take decisions on whether or not services should be bundled in the best interests of patients. That is their job, and these regulations do nothing to require them to bundle or unbundle, as I have said.”
But the guidance from Earl Howe and Monitor has not been that forthcoming about how integrated services through mechanisms such as bundling can be introduced so as to not offend EU competition law, given that the primary effect of the introduction of the Health and Social Care Act will be, as widely warned against, to introduce a fragmented privatised market into NHS services.
The “Tony Blair dictum” (revisited)
Labour themselves perhaps wished to “open up” the NHS to more private sector involvement, even if they did not “introduce” the private market approach to the NHS: it is felt by many that was successfully achieved in the 1980s under the previous Thatcher administration. More recently, the details of “independent sector treatment centres”, and criticisms about their relative inefficiency, introduced under the previous Labour administration are well known.
A Future Fair For All?
Indeed, Labour’s 2010 general election manifesto promised:
“We will support an active role for the independent sector working alongside the NHS in the provision of care, particularly where they bring innovation – such as in end-oflife care and cancer services, and increase capacity”
and further promised that:
“patients requiring elective care will have the right, in law, to choose from any provider who meets NHS standards of quality at NHS costs.”
The “Tony Blair Dictum”
The “Tony Blair dictum” essentially is that it doesn’t matter who provides care, so long as it is free to the patient. It approaches the perspective of a ‘reasonable member of the general public’ as somebody who does not particularly care how much his or her own personal healthcare services is costing the taxpayer “or increasing the deficit”. It is therefore quite a Thatcherite view of an individual, rather than a view held by a socialist.
This is an extract from a speech given by Rt Hon Tony Blair MP, The Prime Minister to a meeting of The New Health Network Clinician Forum on Tuesday 18th April 2006:
“…
Therefore thirdly, patients are being given a choice of NHS provider. So if they have to wait too long at one hospital or are dissatisfied with the standard of care, they can go elsewhere. This choice is already available in the private sector. Now it will be available in the NHS.
Fourth, there will be new independent providers encouraged in the NHS, of which the ITC’s are the first wave. Now this is being opened up to diagnostics, where the major bottlenecks often occur. In addition, where GP lists are full and areas are underprovided, new providers will, for the first time ever, be allowed to come in and provide GP services.
As a consequence of these reforms, there is then structural change to Strategic Health Authorities and PCTs, to streamline them so that they fit the purpose of a less centralised system and to focus them on helping the effective commissioning of care
The result of all of this is to try to create an NHS where there is not a market in the sense that consumer choice is based on an individual user’s wealth; but where there is the opportunity, on an equal basis, for users to choose and exercise power over the system that provides the service. It signals the move from a “get what you’re given” service where the patient falls into line with what the service decides; to one that is more a “get what you want” service moulded around the decisions of the patient. It rewards the producers well; but insists in return that it is the user that comes first. It mirrors the change from mass production to a customised service in the private sector.”
Sean Worth only this week at the RSA used this patient choice argument to justify the enactment of new legislation, “putting patients’ voices in control” and “public’s choices driving policies, not politicians in backroom deals.”
The overall intellectual property legislative framework for branding for “independent sector treatment centres” in this regard is very interesting. In English law, branding is protected by registered trademarks, such that goodwill to and the reputation of the organisation is protected. The branding is meant to be “shop window” of an organisation, and represents the “badge of origin”. In the NHS’ case, co-branding private providers’ suppliers brands with the NHS logo sets out a rather confusing message about the exact origin of NHS services which have been made available by private suppliers. It cannot be the case the “ethos” of private suppliers is the same as that of the NHS, in that private limited companies exist in law for the directors to maximise shareholder dividend.
In this particular context, the branding advice is very specific, for instance:
Remember: you cannot use the NHS logo on any materials which are not directly related to the provision of your NHS services. For all marketing materials that are co-branded with the NHS logo, you must use theNHS typefaces and colour palette.Your marketing materials must also support the NHS brand values and communication principles.
“I can’t believe it’s not the NHS”
Therefore, it seems that, at face value, the Coalition like the previous administration is allowing the patient to ‘shop around’ for the NHS services, and these NHS services are being made available.
THERE ARE MASSIVE ECONOMIC PROBLEMS WITH THE TONY BLAIR DICTUM, RECYCLED BY SEAN WORTH ABOVE.
Fundamental difficulties still arise from this type of scenario, and they’re all to do with information. Tim Kelsey and Paul Nuki might argue that “the more information the better”, but there are still significant policy issues here.
If the information cost of services is made available to the patient, then the accusation will come that patients are ultimately choosing their services on the basis of low cost not high quality; and furthermore the patient will simply get confused in trying to reconcile this with clinical advice from his or her own GP; and thirdly there is potentially a conflict-of-interest anyway between the Doctor and his/her patient about clinical need and cost.
If this information is not made available to the patient, then it is perfectly possible that a single provider can decide to become known for a certain procedure such as day case hernias, which just happens to be “low cost and high volume”. and this is where the problem of “cherry picking” comes in. It is perfectly possible for the private provider then to make a huge profit from such procedures, unknown to the taxpayer who is ultimately paying for these, as long as these private providers are awarded contracts (by submitting slick pitches on the basis of “integrated care” or “best value”). Tthe private provider is of course very happy because it can return a massive shareholder dividend to its investors, and in the long term the costs of running the NHS get much larger.
This is precisely what has happened in all other privatised industries, such as gas, electricity, telecoms, water, leading to a fragmented service, offering homogenous products where there is massive supplier strength in a crowded market (an “oligopoly”), where in fact there is little real competition. The idea of choice, in shopping in a supermarket or even in a patient choosing a NHS standard service, is fine IF the market is not distorted. Instead, an ability of a NHS patient to shop around will then be an artifact of how crowded the market is, and how much a clinical commissioning group will justify clinical decisions with the risk of facing expensive litigation suits in domestic and EU courts of law (which Monitor cannot protect them from, now that the NHS section 75 Regulations have finally been drafted officially.)
There is a huge problem with all of this. The biggest danger still remains about how, if left to its own devices, the market can steer to becoming contracted, which is why it is hardly surprising that the statutory duty of the Secretary of State to provide comprehensive healthcare has been removed, even if what remains strictly speaking remains “free-at-the-point-of-use”. That’s why politicians have become very adept at separating “universal” or “comprehensive”, from the “free-at-the-point-of-use” strands.
Therefore this little tub of “I can’t believe it’s not the NHS” may not be as innocuous as it first appears. The issue is of course the extent to which parliament wishes to throw the NHS to the private sector. However, this Government have made it very clear that their statutory instruments lock the NHS into a private competitive market unless in extreme conditions, paving the way for the destruction of the infrastructure of the NHS, as Oliver Letwin’s alleged remark, “The NHS will not exist any more”, can tragically become true.
Thank you very much for valuable comments on previous drafts of this article.
Is the future ‘integration’?
This is an excerpt from an interview with Andy Burnham MP, MP for Leigh and Shadow Secretary of State of Health, last year at the Labour Party Conference 2012.
This is statement by Earl Howe last week (5 March 2013):
The Parliamentary Under-Secretary of State, Department of Health (Earl Howe): My Lords, I shall now repeat as a Statement the answer to an Urgent Question given in another place by my honourable friend the Minister for care services earlier today on the National Health Service (Procurement, Patient Choice and Competition) Regulations 2013. The Statement is as follows:
“I know that the right honourable gentleman and others have raised concerns about the effect of the regulations, and I would like to address these. First, however, I would like to make it absolutely clear that the regulations must be fully in line with the assurances given to this House during the passage of the Health and Social Care Bill.
The former Secretary of State said to clinical commissioning groups in 2012 that,
“commissioners, and not the secretary of state, and not the regulators, should decide when and how competition should be used to serve patient interests”.
This absolutely must be the case. I made it clear in health Questions last week that we would review the regulations to ensure that this is the case and that they are not open to any misinterpretation.
The right honourable gentleman himself gave guidance to primary care trusts, which made it clear, in 2010-and again I quote:
“Where there is only one capable provider for a particular bundle of services or the objective of the procurement is to secure services to meet an immediate interim clinical need there will be a case for Single Tender Action (ie uncontested procurement). By definition, an immediate”-
“scenario will be exceptional and likely to only … arise on clinical safety grounds or, for example, where existing services have been suspended following intervention by the Care Quality Commission”.
The next bit is very important:
“A decision to procure through a single tender action should always take account of the potential to secure better value by investing in a competitive process, as long as this is justified by the scale and importance of the opportunity (ie it has to be worth it)”.
As we committed in the Government’s response to the Future Forum report, we want to ensure that the regulations simply continue this approach. However, I fully recognise that the wording of the regulations has inadvertently created confusion and generated significant concerns about their effect. I have therefore listened to people’s concerns and my department is acting quickly to improve the drafting so that there can be no doubt that the regulations go no further than the previous set of Principles and Rules, inherited from the previous Labour Government. As we also committed in response to the Future Forum’s report, the Co-operation and Competition Panel has been transferred to Monitor and this will ensure consistency in the application of the rules.
Concerns have been raised that commissioners would need to tender all services. This is not our intention and we will amend the regulations to remove any doubt that this is the case and to clarify that the position remains the same as at present-and as stated in the former Secretary of State’s letters in 2012. Concerns have been raised that Monitor would use the regulations to force commissioners to competitively tender. However, I recognise that the wording of the regulations has created uncertainty and we will therefore amend them to put this beyond doubt.
Concerns have also been raised that competition would be allowed to trump integration and co-operation. The Future Forum recognised that competition and integration are not mutually exclusive. Competition, as the Government made clear during the passage of the Bill, can only be a means to improving services for patients, not an end in itself. What is important is what is in patients’ best interests. Where this is co-operation and integration there would be nothing in the regulations to prevent this. Integration is a key tool that commissioners are under a duty to use to improve services for patients. We will amend the regulations to make this point absolutely clear”.
Statutory instrument SI 2013/057 on NHS procurement in England: amendment or annulment?
A Statutory Instrument is used when an Act of Parliament passed after 1947 confers a power to make, confirm or approve delegated legislation on: the Queen and states that it is to be exercisable by Order in Council; or a Minister of the Crown and states that it is to be exercisable by Statutory Instrument. 1.15 pm last Tuesday (5 March 2013) saw Andy Burnham MP, the Shadow Secretary of State for Health, go head-to-head with Norman Lamb (The Minister of State, Department of Health). Lamb was invited to comment on the regulations on procurement, patient choice and competition under section 75 of the Health and Social Care Act 2012.
The discussion is reported in Hansard.
Lamb describes an intention to ‘amend’ the legislation
Lamb explains:
“Concerns have been raised that Monitor would use the regulations to force commissioners to tender competitively. However, I recognise that the wording of the regulations has created uncertainty, so we will amend them to put this beyond doubt.”
The problem is that this statutory instrument would have become law automatically on 1 April 2013, and still promises to do so in the absence of anything else happening. The safest way to get this statutory instrument out-of-action is to ‘annul’ the law, rather than having the statutory instrument still in force but awaiting amendment. Experts are uncertain the extent to which statutory instruments can be so easily amended, while in force.
Most Statutory Instruments (SIs) are subject to one of two forms of control by Parliament, depending on what is specified in the parent Act.
Fatal motion
There is a constitutional convention that the House of Lords does not vote against delegated legislation. However, Andy Burnham has said the exceptional nature of the Section 75 regulations, which force all NHS services out to tender, meant he needed to table a ‘fatal’ motion in the second Chamber. Indeed, Lord Hunt later tweeted that this fatal chamber had forced a rethink on the original Regulations:
The main effect of delegated legislation being made by Statutory Instrument is that it is effective as soon as it is made, numbered, catalogued, printed, made available for sale, and published on the internet. This ensures that the public has easy access to the new laws. This statutory instrument (SI 2013/057:The National Health Service (Procurement, Patient Choice and Competition) Regulations 2013) is still available in its original form, with no declaration of its imminent amendment or annulment, on the official legislation website here.
The “Prayer”
The more common form of control is the ‘negative resolution procedure’. This requires that either the Instrument is laid before Parliament in draft, and can be made once 40 days (excluding any time during which Parliament is dissolved or prorogued, or during which both Houses are adjourned for more than four days) have passed unless either House passes a resolution disapproving it, or the Instrument is laid before Parliament after it is made (but before it comes into force), but will be revoked if either House passes a resolution annulling it within 40 days.
A motion to annul a Statutory Instrument is known as a ‘prayer’ and uses the following wording:
- That an humble address be presented to Her Majesty praying that the [name of Statutory Instrument] be annulled.
Any member of either House can put down a motion that an Instrument should be annulled, although in the Commons unless the motion is signed by a large number of Members, or is moved by the official Opposition, it is unlikely to be debated, and in the Lords they are seldom actually voted upon.
Indeed, this is exactly what happened. Ed Miliband submitted EDM 1104 on 26 February 2013, which currently – at the time of writing – has 183 signatures – with the exact wording:
“That an humble Address be presented to Her Majesty, praying that the National Health Service (Procurement, Patient Choice and Competition) Regulations 2013 (S.I., 2013, No. 257), dated 11 February 2013, a copy of which was laid before this House on 13 February, be annulled.”
The purpose of “amending” the legislation
Lamb later provides in his answer:
“Concerns have also been raised that competition would be allowed to trump integration and co-operation. The Future Forum recognised that competition and integration are not mutually exclusive. Competition, as the Government made clear during the passage of the Bill, can only be a means to improve services for patients—not an end in itself. What is important is what is in patients’ best interests. Where there is co-operation and integration, there would be nothing in the regulations to prevent this. Integration is a key tool that commissioners are under a duty to use to improve services for patients. We will amend the regulations to make that point absolutely clear.”
How the Government “amends” the legislation is clearly pivotal here. Integration is another “buzzword” in the privatisation ammunition. Colin Leys wrote in 2011:
“In the emerging vision of the Department of Health, however, integrated care has always been associated with the drive to enlarge private sector provision, and the Kaiser [Permanente] connection emphasised this. The competitive culture attached to integrated care in the Kaiser model, coupled with the keen interest of private providers in all integrated care initiatives, were constants, and put their stamp on official thinking about the future NHS market.”
A possible reason for why this emphasis on competition has failed is that in other markets, such as utilities, rail and telecoms, there is a strong case that competition has not driven down cost at all, because of shareholder dividend primacy. Another good reason for people in favour of the private market to discourage competition is that competition might even inhibit a drive to integration, and integration is strongly promoted by private providers (and, incidentally, New Labour).
What does the Act itself say about ‘annulling’ statutory instruments?
According to s. 304(3), “Subject to subsections (4) to (6), a statutory instrument containing regulations under this Act, or an order by the Secretary of State or the Privy Council under this Act, is subject to annulment in pursuance of a resolution of either House of Parliament.” So, at the moment, we are clearly in limbo, with parliament yet to pass a EDM, and new redrafted Regulations yet to appear. However, it is still a very dangerous situation, as the original set of Regulations is still yet to be enacted on 1 April 2013.
Don’t you think it’s very odd a Conservative PM should nationalise something? What is the real issue about patient records?
Even Google gave up on their central database for health information called “Google Health”. Whilst few things are as certain as death and taxes, it is fairly certain that there is big money in big data. Lord Shutt of Greetland, Chair of the Joseph Rowntree Reform Trust Ltd. warned, in a foreword on a recent report on “the database state”, that the problem is huge, and as a society we must face up to formidable challenges. There has always been a tough balance in the law between balancing individual rights of privacy and freedom, with the State’s rights of national policy of health and security, for example. Whatever ideological position the Liberal Democrats eventually settle on, it is striking that a Conservative Prime Minister should actually advocate nationalising something.
It is unsurprising that Big Pharma would have welcomed the move. Andrew Witty, the chief executive of GlaxoSmithKline, stated to the Sunday Telegraph he welcomed the data-sharing initiative: “Any action the government takes to improve the environment in this country for life science across these activities is welcome.” The Autumn Statement (2011) had indeed signposted this. It might seem paradoxical that the Department of Health at this time wishes to embark on an initiative to make the NHS “paperless”, at a time when a reorganisation, estimated at £3bn, is currently underway. Patient data, essential for individual patient security, confidentiality and consent, are “rich pickings” for the private healthcare industry, which have not collectively paid to collect this information nor invest in the IT infrastructure of the NHS, but the ethical concerns are enormous. Personalised medicine, dependent on real-time patient information, is “the next big thing” emergency in the pharmaceutical industry, currently keeping stocks of companies very healthy. However, the professional code for Doctors, from the General Medical Council (“GMC”) is very clear on the regulation of patient confidentiality and privacy: this is contained within “Confidentiality” (2009), and clearly guides doctors on the conflicting balance between confidentiality and disclosure.
There are interesting reasons why the operational roll-out of the National Patient Record failed in 2006-7. It is now reported that all prescriptions, diagnoses, operations and test results will be uploaded on to central computers by the end of next year, and, by 2018, all NHS organisations will be expected to be able to share this information with other hospitals, GPs, ambulances and health trusts. Mr Hunt hopes local councils will sign up to similar systems, along with private care homes. As with the overall direction of travel of the NHS towards an insurance system where private companies pay “a greater part”, this blurring of the need for patient consent has been insidious.
Section 251 of the NHS Act 2006 (originally enacted under Section 60 of the Health and Social Care Act 2001), allows the common law duty of confidentiality to be set aside in specific circumstances where anonymised information is not sufficient and where patient consent is not practicable. For example a research study may require access to patient identifiable data to allow linkages between different datasets where the cohort is too large for consent. This would require time limited access to identifiable information where gaining consent from a large retrospective cohort would not be feasible and would require more identifiable data than would be necessary for linkage purposes. However, section 10 of the Data Protection Act (1988) currently allows a right for an individual to prevent damage or distress by data processing. This is indeed conveniently “triggered” by section 259(10) of the Health and Social Care Act (2010), i.e. “[the provision] is subject to any express restriction on disclosure imposed by or under another Act (other than any restriction which allows disclosure if authorised by or under an Act”:
The Secondary Uses Service (SUS) Programme supports the NHS and its partners by providing a single source of comprehensive data for planning, commissioning, management, research, audit, public health and “payment-by-results”, a reimbursement mechanism for acute care payments. It is critical to know whether patients their right to opt out of the SUS database. It should not be the case that NHS patients are denied hospital care if they do not agree to my records being sent to SUS. Steve Nowottny in his “Editor’s Blog” for Pulse, a newspaper circulated to GPs, on 8 January 2013 outlined some important very recent developments:
“That year, Pulse ran a ‘Common Sense on IT’ campaign which highlighted a series of concerns over the consent and confidentiality safeguards in the new system.
“GPs wanted patients to have to give explicit rather than merely implied consent before records were created. Plans to use data within the records for research purposes without explicit consent had Catholic and Muslim leaders up in arms, because they feared the research could be purposes contrary to their faiths, such as abortion or stem cell research.
We revealed that celebrities, politicians and other patients whose information is regarded as sensitive would be exempted from the automatic creation of a Summary Care Record, raising questions about the system’s security. And we reported that patients who did not initially choose to opt out of the Summary Care Record would be unable to have their records subsequently deleted.
At the time, it felt as though the stories, while interesting and concerning, were somewhat theoretical. The Summary Care Record’s deployment to date had been patchy and it was far from certain it would continue. In the meantime, fewer than 1% of patients had bothered to opt out. (Now, with nearly 22 million records created and more than 41 million patients contacted, the figure stands at 1.34%).
But the news today that 4,201 patients had Summary Care Records created without them giving even implied consent – and that they will not be able to have them deleted – reignites the whole debate. Suddenly ‘what if’ scenarios have become reality.”
Tim Kelsey is the NCB’s National Director for Patients and Information – his stated aims are to put transparency and public participation at the centre of a transformation of customer service in the NHS. In a recent lecture, he quoted George Soros who said “our social institutions are imperfect, they should be open to improvement [and that] requires transparency and data“. On-line banking and e-ticketing demonstrate the power of open access to personal data in a safe, secure way – for some reason, heath data is deemed more personal that finance and travel arrangements. Data.gov.uk is an example of his vision for the future – the UK has so much medical data, not only about patients but also genomics and other bioinformatics disciplines. The law currently gives the NCB power to mandate more data flows – TK targets April 2014 to get outcomes-based data flows from primary and secondary care – once achieved, next step is to embrace social and specialist care. So, once the data is “freely available”, it can be made available for public participation – he is investing in a course called ‘Code for Health’, a 3 day course to learn how to develop apps. Data is essential from April 2013, there will be push for on-line interaction with GPs, to realise nationally the benefits seen in pilot areas.
So why should commissioners need access to “personal identifiable data”. It is considered that these may be “good reasons”:
- integrated care and monitoring services including outcomes & experience requires linkages across sources
- commissioning the right services for the right people requires the validation that patients belong to CCGs and have received the correct treatments
- aspects of service planning and monitoring on geographic data basis require postcodes for certain type of analysis
- understanding population and monitoring inequalities
- target support for patients and population groups at highest risk requires data from several sources linked together
- specialist commissioning is commissioned outside local areas and can require wider discussions about individual patients and their associated costs
- ensuring appropriate clinical service delivery and process requires access to records
To enable commissioning, ‘personal identifiable data’ including NHS no, DOB, Postcode data needs to flow to “data management integration centres” (“DMICs”). The DMICs need to have similar powers and controls to the Health and Social Care Act information centres to process data In order for processing of PID at DMICs to be undertaken legally, a change in legislation will be required; it is considered that legislative changes can not be achieved by April 2013, and that the new Caldicott is report expected around Jan/Feb 2013. Meanwhile, DMICs need to be operational in April 2013.
David Cameron has stated explicitly his intention for social care to head towards a private insurance system. As stated in the transcript of the interview with Andrew Marr,
“Well the point that was being made earlier on the sofa by Nick Watt, this is a massive problem – that you know more and more people suffering from dementia and other conditions where they go into long-term care and there are catastrophic costs that lead them to have to sell their homes to pay for that care – it’s right to try and put in place a cap which will then open up an enormous insurance market, so people can insure against that sort of catastrophic loss.”
A longrunning conundrum about where there is such intense interest in ‘raising awareness of dementia’. The idea of having GPs and physicians ‘diagnose’ dementia on the basis of a screening test, without it being called ‘screening’ in name, has not been backed up with the appropriate resource allocation for dementia care elsewhere in the system, including adequate training for junior doctors and nurses crucially involved in actual dementia care. Is this and integration of care an entirely virtuous sociological problem? Integration of care at first sight seems to involve primarily avoidance of reduplication of operations, and better ‘coordinated’ care between health and social care and funding. This is not an unworthy ambition at all. It is well known that the endpoint of the Pirie and Butler “Health of Nations” blueprint for NHS privatisation has a greater rôle for the private insurance market as the endpoint, so it makes complete sense to have a fully integrated IT system which private insurers and the Big Pharma can tap into. Lawyers will, of course, be cognisant about the added beauty of integration of clinical and financial information. One of the biggest banes of insurance markets is information asymmetry, making calculation of risk and potential payouts difficult. Insurers will argue that calculation of risk is only possible with precise information, and as I described earlier, clinical commissioning groups are merely “statutory insurance schemes”. It is a long-held belief that private insurers refuse to pay off given the slightest lack of compliance in terms and conditions, but private insurers provide that this mechanism needs to exist to protect them making unnecessary payouts. Failure to disclose medical conditions is an excellent way for private insurers to get out of “paying up”, otherwise known as rescission.
So, given all the above, you can see why the current Government wish to progress with this particular approach to private medical data. The private insurance market and Big Pharma stand to benefit massively, and their lobbying is much more sophisticated than lobbying from GPs, physicians or members of the public. The drive towards all nurses having #ipad3s and all TTOs from Foundation Doctors being sent by broadband to nursing homes may seem utterly virtuous, but there are more significant drivers to this agenda beyond reasonable doubt.