Home » Posts tagged 'innovation'
Tag Archives: innovation
Ever tried. Ever failed. No matter. Try again. Fail again. Fail better.
Now here’s a question: how are we to ascertain the ‘success’ of the World Dementia Council?
The work of the World Dementia Council is wide-ranging; it’s not just the aggressive pimping of innovations for dementia.
The four main areas of work are to be as follows.
Four main areas are being pursued in order to tackle the lack of effective treatment and sufficient funding to find a cure:
- Integrated development – Optimising the path of medicines from research through to market by reducing barriers & encouraging regulatory flexibility.
- Finance and incentives – Looking at ways to increase the relatively low investment in funding dementia innovation by exploring new types of funding product.
- Open science – Unleashing the potential of open science for sharing information and knowledge to accelerate progress in developing new treatments and care approaches, and avoiding wasteful duplication of effort.
- Public health/prevention – The Council is also beginning an evidence review into existing research on how risk factors such as diabetes and heart disease relate to dementia, as well as looking into public health messaging on lifestyle and prevention.
There are some occasions when it is blatantly unwise to reward failure. For example, one could argue that senior management of the NHS should not automatically command high salaries, if they are not doing the basic things well, such as listening to their junior staff in their decision making.
But the operational failures of the NHS have been eye watering. Data showed just under 90% of patients were seen within four hours in the seven days up to December 14 2014. Pressures in England’s A&E units have hit record levels, with the lowest percentage of patients seen within four hours since monitoring began in 2010. Major units particularly struggled, with just six out of 140 meeting the target to see 95% within four hours.
Earlier this year, it was reported that NHS organisations have run up a total deficit of nearly £500m in the first three months of this financial year, according to two reports from health sector watchdogs Monitor and the Trust Development Authority. Monitor reported that the NHS had come under “unprecedented pressure” from increased patient demand, at a time when they are still trying to make savings in response to the biggest squeeze on Government health spending in the health service’s history. The Foundation Trust sector, made up of 147 NHS organisations, including 83 acute hospitals, which have historically been more financially stable than the rest of the NHS, has gone into overall deficit for the first time.
One of the phenomena which the NHS seems to be learning from big business is the immorality of high executive pay. The High Pay Centre, a think tank, said shareholders were still backing high executive pay deals despite new powers to vote them down at annual meetings. The pay of the average FTSE 100 chief executive increased from £4.1m to £4.7m last year, said the report. The High Pay Centre’s report says that, without further action, trust in business will be damaged by the perception that an executive “elite” is reaping all the rewards from economic growth.
The famous Samuel Beckett adage is, “Ever tried. Ever failed. No matter. Try again. Fail again. Fail better.” But if the current Government were to fail better over the NHS, they would be presiding over an unfathomable epidemic of A&E trolley queues. The adage also draws into sharp focus what ‘failure’ is for the NHS. Failure for an individual Doctor or nurse might be easier to define, in terms of patient safety. One could argue that the metric of overall whether the NHS and care are safe is too blunt, but a necessary component.
Success in health and care, one can broadly define, should not be measured clinically through the lens of shareholder dividend. And yet this is precisely what we appear to do for private providers of care homes. It has long been felt that the 1945 Attlee ‘post war settlement’ failed both the left and right. It failed the left as it led to growing marketisation and privatisation of public services, and it failed the right as true socialism planning and shared resources went flying out of the window.
Numerous recent governments have tried to triangulate their way out of this problem. But it is clear that this has introduced more new problems than the old problems it purported to solve. Take for example financial failure for failed market entities. In a health service that pretended to be safe, otherwise you would not de-prioritise clinical emergencies, you would be taking out of scope life or death situations. And yet successive recent governments have allowed a situation where a NHS hospital might be acting unlawfully if it received ‘state aid’.
There are also strata of how failure is ‘hidden’ in the modern health and care system. The cuts in social care have been staggering, with the current Government coming up with increasingly convoluted explanations of their vanity project ‘The Better Care Fund’ to explain away a social care system on its knees. A fundamental problem, for example, with not being entirely truthful about the quality of care, running it entirely under market forces, is that you cannot easily tell if a patient with mental health problems gets a ‘bum deal’ in clinical care? Even measuring suicides has not become an uncontroversial measure of lack of success of policy; even though reports of suicides of disabled citizens allegedly brought about in welfare reforms continue to emerge.
It is possibly true that the phrase is better suited to long term conditions in service provision.
Let’s think again about, “Ever tried. Ever failed. No matter. Try again. Fail again. Fail better.”
Innovation, doing traditional things differently to achieve the same or better outcome, should not be the territory necessarily of any political ideology. And it is certainly true that you have to crack a few eggs to make an omelette; in other words, an innovator has to be prepared to put up with a few dead ducks before hitting upon a great idea.
So how do you measure the success of an innovator? This question does merit some scrutiny, as one might then consider whether the performance of a successful innovator ought to be ‘sustainable’. Or whether we should make do with an innovator who has ‘hit it lucky’? But here I feel that there are some fundamental misunderstandings about what innovations are. Innovations aren’t simply inventions. A lot of work has to be put into discovering whether an intended target audience can actually adopt an innovation or not; hence the absurdity of not having a person living well with dementia on the World Dementia Council.
How are we to tell whether the World Dementia Council is any good? For me, one measure is whether they include people they purport to be interested in. By this, I don’t include having a person living with dementia in attendance at a meeting, but a person living with dementia with a portfolio and programme to influence their work. Inevitably one person living well with dementia to represent the millions globally in the world will appear tokenistic, but we’re shockingly not even at that stage. There is no person living well with dementia who has been appointed yet as a regular member of the World Dementia Council, and I certainly don’t want to see this to be situation when Kate Swaffer and Dennis Gillings participate in the same session of the Alzheimer’s Disease International Conference next year.
You can see whether a health system is truly embracing integrated care by certain proxy phenomena arguably, such as whether there is a whole person care tariff incentive in place, whether data are shared, whether there is care coordination, whether there is an ethos of multidisciplinary teams, whether stakeholders embrace shared or distributed leadership, and so on.
You can see the extent to which science is ‘open’ by the degree to which results are shared, including those from drug trials which have been dead ducks; the question is whether Pharma will wish to share this information with the market, as this form of market signalling could be to the detriment of shareholder dividends, even if for the market good. Market forces again. Whenever I see somebody sleeping rough under Waterloo Bridge in London, like the late and great Tony Benn, I think of market forces.
But the one domain which is the most vague is measuring the efficacy of prevention strategies. This, however, could be clearer than the ‘target’ of having a drug cure for dementia by 2025. Forget the usual question about which of the hundred dementias they’re finding and funding a cure for? Nobody’s listening. La la la la la. How will be able to tell the actual prevention strategies are working? This is not asking the same question as whether Governments have in place got operations in place to promote prevention; such as Mediterannean diets or fitness clubs.
For those of certain political spectrum, the development of an illness or disease is due to a failure in responsibility by an individual. We have seen this argument reach torrential proportions in the backlash against the effects of obesity being construed as a disability. Some people are medically morbidly obese, so should they be tarred with same brush over criticism of ‘those fatties who eat too many cream cakes’? The current evidence that the non-modifiable risk factors for Alzheimer’s disease are quite substantial, so even if we somehow eradicated all risk certain individuals would still develop that type of dementia. However, it could well be that some forms of dementia are amenable to healthy living. And if so are those people who are developing certain types of dementia, e.g. vascular dementia, guilty of not trying harder?
2014 has seen the growth of the meme ‘healthy body healthy mind’ as the beneficial effects of diet (including cholesterol), blood pressure control or physical exercise have come to the fore in considering the vascular dementias. This whole discussion, though, potentially poses questions about what sort of health system we want. Parking aside the issue of whether we want a health system which views illness as a punishment for personal indiscretions, and therefore your access to treatment fundamentally dependent on society’s view of retribution, we could consider whether we want a health system where we pool our risk, or whether you are sealed to your insurance premium fate by your particular genetic make up? We keep on being told that the future of medicine in the NHS is through advances in DNA technology. We’ll all one day be able to access details of our genome, even if our local care home for Granny is up shit creek.
So where now for, “Ever tried. Ever failed. No matter. Try again. Fail again. Fail better.”
Lessons do have to be learnt from catastrophes, whichever political term they happen to fall under, whether Harold Shipman or Mid Staffs. But there is a danger of making good policy out of extreme disasters (even if extreme disasters turn out to be ‘isolated events’). Likewise, the risks we take in developing innovations may be utterly dissonant with the need to minimise risk in the acute part of the service. But considering this question enables us to think about what sort of society we want? In the case of my interest, dementia, whether we want to have a World Dementia Council without a sitting member living well with dementia or whether we want to ‘blame’ people for developing dementia?
Money is tight, but the person remains pivotal in dementia care and support
There’s no question that there is a greater number of people who are old needing to be looked after by care and support services in England.
But dementia is not simply a disease of older people, one of the critical messages of “Dementia Friends”.
Indeed, much of the budget goes into the health and care of younger people, as health technologies, say for treating cardiovascular disease through stents, get better.
The reality is there is pressure on service and the workforce simultaneously in dementia, as the Nuffield Trust and Health Foundation have argued in a sophisticated way.
Earlier in this year, in an article for ETHOS Journal “Living well = greater wellbeing”, I argued a joined up approach would now be needed to deliver a better standard of care and support for people living well with dementia.
In 2010, the UK government became among the first countries to officially monitor people’s psychological and environmental wellbeing. Academic research and policy developments have recently converged upon the notion of ‘living well with dementia’, which transcends any political ideology. This means promoting the quality of life of any person with dementia. It views each person as a unique individual and champions his or her involvement in making decisions whenever possible.
England actually leads the way with the ground-breaking ‘first mover’ exploration by academic Tom Kitwood of ‘personhood’ in the late 1980s: “It is a standing or status that is bestowed upon one human being, by others, in the context of relationship and social being. It implies recognition, respect and trust”.
It’s estimated that there are at least 800,000 people currently living with dementia in the UK. These individuals are likely to come into contact with a number of different people and services in an extensive network including carers (paid and unpaid, including family caregivers), care home staff, transport services, social housing, welfare and benefits and the police to name but a few.
I am, indeed, grateful for Paul Burstow MP’s excellent reply to my article.
The current Government in England has made substantial progress with policy in dementia in my opinion.
The current Care Act (2014) could not be clearer.
In the statutory guidance, the importance of wellbeing is signalled extremely strongly.
It is important for commissioners not to lose sight of this, and not to treat ‘living well with dementia’ not as a slogan but as a reality.
Helping people to live well has been a key aim of the current Government, and I hope future governments, perhaps implementing ‘whole person care’, will retain this strong focus.
Enabling people to live well leads to a fairer society. The value of people living with dementia for society cannot be denied either.
But people in power and influence have a rôle to play.
The Alzheimer’s Society has played its part in addressing stigma and discrimination through its successful ‘Dementia Friends’ campaign. I myself am a “Dementia Friends Champion”, and proud to run my sessions.
One of the key messages in this campaign is that ‘there is more to the person to the dementia’.
This message is currently a critical global one, across many jurisdictions. Here is friend and colleague Kate Swaffer with a huge banner in Australia to the same effect.
And dementia and loneliness already occur together all too often.
The wider community is essential. This is about compassion. It is also about the right people showing the right leadership.
But this should not just simply include household names, although the distress caused by lack of inclusion of people with dementia in high street shops cannot be underestimated.
This community must include all caregivers and professionals.
And central to this recognition of the role of the wider community is a new deal for carers.
As the number of people living with chronic conditions grows rapidly, so does the number of carers. There is a huge army in England currently consisting of selfless individuals giving of themselves to support a loved one.
According to Carers UK, family carers currently save the Government £119 billion every year.
Carers themselves need help.
Carers are invaluable as I discuss here.
And we need to make sure in the next Government that all paid caregivers are given a statutory minimum wage, which could also be a living wage.
We are a society which values footballers more than caregivers for people with dementia. This is simply abhorrent.
I thank the current Government for progress made in this direction, but more has to be done whoever holds office and power next year.
We need collectively to support the Dementia Action Alliance Carers Call to Action. By achieving the shared vision, the aim is to have positive impact on people with dementia and carers and improve their quality of life.
In the Dementia Action Alliance “Carers Call to Action”, carers of people with dementia:
- have recognition of their unique experience – ‘given the character of the illness, people with dementia deserve and need special consideration… that meet their and their caregivers needs’ (World
Alzheimer Report 2013 Journey of Caring are recognised as essential partners in care – valuing their knowledge and the support they provide to enable the person with dementia to live well - have access to expertise in dementia care for personalised information, advice, support and co-ordination of care for the person with dementia
- have assessments and support to identify the on-going and changing needs to maintain their own health and well-being
- have confidence that they are able to access good quality care, support and respite services that are flexible, culturally appropriate, timely and provided by skilled staff for both the carer and the person for whom they care
But we do need some sort of standards, whether aspirational or regulatory, for example?
This situation had become known to Norman Lamb by February 2013:
In light of the recent Stafford Hospital Scandal, an independent review was carried out, underlining irregularities in staff training. According to today’s BBC report, as of March 2015, UK care staff and assistants in care homes, hospitals, and private homes are to be required to complete a training certificate within 12 weeks of starting a new position.
The current UK stance is that there is no minimum standard of training. With over 1million care workers in the country, it came as alarming news to Care Minister, Norman Lamb, to discover that these untrained workers were completing skilled tasks normally undertaken by medical professionals such as taking bloods. He confirmed the responsibility for the certificate would “…rest with employers and I think that’s where the training responsibility should lie.”
I expect the next Government will wish to think about a register for paid carers to help the fight against neglectful care which can tragically happen. It can be hard to achieve a successful prosecution of ‘wilful neglect’, but likewise carers need to be able to do their job with dignity and without fear.
The broad consensus has been for some time “that the principles of person-centred care underpin good practice in the field of dementia care”. Their principles assert:
- the human value of people with dementia, regardless of age or cognitive impairment, and those who care for them
- the individuality of people with dementia, with their unique personality and life experiences among the influences on their response to the dementia
- the importance of the perspective of the person with dementia
- the importance of relationships and interactions with others to the person with dementia, and their potential for promoting well-being.
In a presentation called “Developing nursing in dementia care” in May 2014 influential expert Rachel Thompson outlined a “Commitment to the care of people with dementia in hospital settings”, calling for increase in specialist nurse roles –building evidence and supporting leaders.
I believe strongly this need has not gone away. Indeed, it is stronger than ever.
Thompson there mentions the SPACE principles to support good dementia care
Staff who are skilled and have time to care.
Partnership working with carers.
Assessment and early identification of dementia.
Care plans which are person centred and individualised.
Environments that are dementia-friendly.
The financial case for ‘Admiral nurses’, an innovation from Dementia UK, is compelling; see for example the recent report from the University of Southampton Centre for Innovation and Leadership in the Health Sciences.
As is the case from the academic and clinical nursing literature on the importance of proactive case management in avoiding admissions to hospital care.
Claims that nine in ten care homes and hospitals fail to provide the proper treatment are indeed astonishing. That particular Care Quality Commission review found widespread neglect, lack of care, poor training and failings in communication.
In the same way there can be enormous disparity between a ‘bad’ and ‘good’ care home, there can be a subtle difference between a ‘very good’ and a ‘superb’ care home.
We, one day, need to be able to celebrate the ‘outstanding’ in care homes: for example, person-centred activities or environment generally might make all the difference?
The next Government, whoever it is, will need to have the confidence to implement an organic, stakeholder-driven systemic innovation in dementia.
I have long felt that the health and care services need more than a minimum ‘protected funding’. As Roy Lilley, experienced health commentator, remarks, ‘more effort can be put into weighing the pig than actually fattening it’.
This is the danger we run if we do not place adequate resources into service provision and training.
However, even within these domains, I believe that innovation has, potentially, an important and responsible part to play (as indeed I argued in the Health Services Journal this year).
There is no question that money is tight.
But we need also to have a minimum in frontline services to maintain an adequate standard of care, as indeed is supposed to be enforced from the regulation of all clinical professions.
It is easy to jump on a ‘person-centre care’ bandwagon, but all too easily this can turn into selling courses and products for person-centred care.
Putting the person at the heart of how you behave with a person with dementia does not need to cost money. Tom Kitwood articulated it brilliantly.
But, whatever the budget constraints of the health and care and future, I believe personhood should be pivotal for living well with dementia.
This should include the whole person.
If we involve people living with dementia in the design of research and services, I feel, a lot of my concerns will be addressed. The ‘Dementia Without Walls’ project from the Joseph Rowntree Foundation, in collaboration with other stakeholders, has truly been outstanding, for example.
I am grateful to the current Government for taking us a long way down the journey. But we’ve only just begun.
Lots of small gains will see our shared vision for living better with dementia shine through
When I asked Charmaine Hardy (@charbhardy) if she would mind if I could dedicate my next book, ‘Living better with dementia’ to her, I was actually petrified.
Obviously, Charmaine had every right to say ‘no’. You see, I met Charmaine through Beth on Twitter, and I saw the three letters ‘PPA’ in Charmaine’s Twitter profile. Charmaine’s Twitter timeline is simply buzzing with activity. It’s hard not to fall in love with Charmaine’s focused devotion everywhere, nor with how much she adores her family. This passion, despite daily Charmaine working extremely hard, itself generates energy. People are attracted to Charmaine, as she never complains however tough times get. She thinks of ways to go forwards, not backwards, even when she had trouble with her roses recently. She basically creates a lot of good energy for all of us. As Charmaine’s Twitter profile clearly states, “I’m a carer to a husband with PPA dementia.”
Things are not right with the external world though. We have millions of family unpaid caregivers rushing around all the time, trying to do their best. Seeing these relationships in action, as indeed Rachel Niblock and Louise Langham must do at the Dementia Carers’ Call to Action (@DAACarers), must be a fascinating experience. There’s a real sense of shared purpose, often sadly against the “system”.
Contrary to popular opinion, perhaps, I have a strong respect for the hierarchy I find myself in. I have asked Prof Alistair Burns (@ABurns1907), a very senior academic in old age psychiatry, to write one of my Forewords. He also happens to be England’s lead for dementia, but I hope to produce my book as a work of balanced scholarship, which does not tread on any policy toes.
But underlying my book is a highly energised social network (@legalaware), based on my 14000 followers on Twitter. My timeline is curation of knowledge in action, in real time as my #tweep community actively share knowledge on a second-by-second basis. There’s a real change of us breaking down the barriers, and changing things for the better. Sure, some things of course don’t go to plan, but with innovation you’re allowed to crack a few eggs to make an omelette. I have enormous pleasure in that in this network people on the whole feel connected and with this power might produce a big change for the better.
My new book is indeed called ‘Living better with dementia: champions challenging the boundaries‘ – and I feel Kate Swaffer (@KateSwaffer) and Chris Roberts (@mason4233) are doing just that. They continually explain, reasonably and pleasantly, how the system could be much improved from their perspectives of living well with dementia, such that we could end up with a ‘level playing field’. And of course the fact we know what each is up to, for example pub quizzes or plane flights, means that we end up being incredibly proud even if we have the smallest of wins.
My proposed contents of this book are as follows: here.
I am not going to write a single-silo book on living better with dementia, however much the medics would like that.
For many of us in the network, dementia is not a ‘day job’. This shared vision is not about creating havoc. It’s simply that we wish the days of the giving the diagnosis of dementia as ‘It’s bad news. it’s dementia. See you in six months’, as outnumbered. That’s as far as the destruction goes. We want to work with people, many of whom I used to know quite well a decade ago, who felt it was ‘job done’ when you diagnosed successfully one of the dementias from seeing the army of test results. I would like the medics and other professionals not to kill themselves over our urge for change, and work with us who believe in what we’re doing too.
Whenever I chat with Kate and Chris, often with a GPS tracker myself in the form of Facebook chat, I am struck by their strong sense of equity, fairness and justice. And I get this from Charmaine too. The issue for us is not wholly and solely focused on how a particular drug might revolutionise someone’s life with dementia. The call for action is to acknowledge friends and families need full help too, and that people living with dementia wish to get the best out of what they can do (rather than what they cannot do) being content with themselves and their environment. We’re looking at different things, but I feel it’s the right time to explain clearly the compelling message we believe in now.
These values of course take us to an emotional place, but one which leads us to want to do something about it. For me, it’s a big project writing a massive book on the various contemporary policy strands, but one where I’ve had much encouragement from various close friends. For me, the National Health Service kept me alive in a six week coma, taught me how to walk and talk again, when I contracted meningitis in 2007. As I am physically disabled, and as my own Ph.D. was discovering an innovative way of diagnosing a type of frontotemporal dementia at Cambridge in the late 1990s, I have a strong sense of wishing to support people living with dementia; especially since, I suspect, many of my friends living well with dementia will have experienced stigma and discrimination at some time in their lives.
I understand why medics of all ranks will find it easier to deal with what they are used to – the prescription pad – in the context of dementia. But I do also know that many professionals, despite some politicians and some of the public press, are excellent at communicating with people, so will want to improve the quality of lives of people who’ve received a diagnosis. We need to listen and understand their needs, and build a new system – including the service and research – around them. I personally ‘wouldn’t start from here’, but this sadly can be said for much for my life. Every tweet on dementia is a small but important gain for me in the meantime. Each and every one of us have to think, ultimately, what we’ve tried to do successfully with our lives.
Suggested reading
Read anything you can by @HelenBevan, the Chief Transformation Officer for the NHS.
Her work will put this blogpost in the context of NHS ‘change’.
Our new white paper is finally out! “The new era of thinking & practice in change & transformation”. Download at http://t.co/83ZFUO1z99
— Helen Bevan (@helenbevan) July 5, 2014
Does a policy of ‘Dementia Dogs’ unfairly indirectly discriminate against Cats?
Under our law, a mental health condition is considered a disability if it has a “long-term” effect on your “normal day-to-day activity”. This is defined under the Equality Act 2010.
Your condition is ‘long term’ if it lasts, or is likely to last, 12 months.
‘Normal day-to-day activity’ is defined as something you do regularly in a normal day. For example – using a computer, working set times or interacting with people.
There are many different types of mental health condition which can lead to a disability, including dementia. This Act makes it unlawful for service providers to unreasonably discriminate against disabled people. Since the Act was introduced, things have improved for many people with disabilities.
Traditionally, services that discriminate unfairly against disabled people face the wrath not only of the law, but of new generations of disabled people prepared, encouraged and empowered to fight for their rights.
Living well with dementia is therefore not just a societal aspiration. It is a legal necessity.
However, we know that the rights of people with dementia can seem to disappear after the diagnosis. This can happen in small ways. For example people in authority including health and social care professionals may only consult a carer and may make assumptions about what people with dementia want.
This occurs when an organisation (for example, the University, or a member of staff at the University) makes a decision, or puts in place a particular policy or practice, which, on the face of it appears to treat everyone equally, but which actually, in practice, leads to people from a protected group being treated less favourably than other people. This is unless the person applying the provision can justify it as a proportionate means of achieving a legitimate aim.
On a less serious note, does a policy of ‘Dementia Dogs’ unfairly indirectly discriminate against Cats?
Comparing the intelligence of animals of different species is difficult although there are certain tests and problem sets that have proved to be useful. Making the tests equivalent, however, has proved difficult. Dogs are designed to be more efficient runners while cats have better ability at manipulating things with their paws. Thus a test that involved pulling strings or operating levers would tend to favor a cat, while a test involving moving from place to place, where speed is a measure of performance, would favor a dog.
Charles Darwin claimed, “Intelligence is based on how efficient a species became at doing the things they need to survive,” and one might argue that by this definition all species that stay healthy, remain numerous and avoid extinction are equally intelligent.
In the late 1970’s the psychologist Harry J. Jerison developed an alternative measure that he called the Encephalisation Quotient or EQ. It is a mathematically sophisticated comparison of the actual brain weight of an animal compared to the expected brain mass for that animal’s body size. This compensates for the fact that bigger animals tend to have bigger brains and basically shifts the question to one of whether the animal has a larger or smaller brain size than what we would expect for an animal with its body mass.
Based on the encephalisation quotient, the brightest animals on the planet are humans, followed great apes, porpoises, and elephants. The dog is close behind elephants in its EQ. Descending down the list we find cats lower than dogs, followed by horses, sheep, mice, rats and rabbits.
However, a real surprise occurs in some recent data provided by Suzanne Shultz and Robin Dunbar at Oxford University.
They wondered about whether there had been evolutionary changes in the Encephalisation Index. For example, when we domesticate animals, especially a companion animal like a dog, we are placing new demands upon it. Some of these demands are social in nature, such as understanding human communication gestures and words. Dogs are subjected to more of this pressure than are cats. Thus it might be expected that dogs would show a greater rise in their EQ than cats.
This was indeed verified by the Oxford researchers using 511 different samples ranging from extinct species only available as fossils, up through current living examples. Thus it appears that based on their EQ dogs are becoming progressively more intelligent over time while cats have remained at much the same level of mental ability that they had when we first domesticated them. This means that not only are dogs smarter than cats, but the gap between the species is increasing over time.
At the risk of starting another argument, these data may explain why we never hear about such things as a “seeing eye cat,” “police cat” or “search and rescue cat.”
Dementia Dog, one of the five innovative solutions developed through the Living Well with Dementia Design Challenge, is a service providing assistance dogs to people with dementia, helping them lead more fulfilled, independent and stress-free lives.
A sense of routine can often break down for people with dementia. Dogs can be trained to live to a consistent routine. Ultimately, each dog will be trained with the person with dementia and their carer so all three can operate as a team.
In certain cases, functional effects dementia causes can be diverse: forgetting to eat, drink or sleep can increase disorientation, medication can be forgotten and confusion can heighten anxiety about the outside world, increasing isolation. This is a factor to consider for caregivers too.
The dogs are taught to support existing patterns of waking, sleeping and eating for people with dementia.
Through responding to sound alerts they can also help with regular hydration, medication and toilet use.
The social and emotional benefits are potentially huge. Just by being able to get out more independently, in certain cases, the person with dementia can widen his or her circle of support.
If the policy of ‘Dementia Dogs’ does unfairly discriminate against ‘Dementia Cats’ on the grounds of equality, it can be argued that this is legally justified on the grounds of cats having a lower emotional intelligence than dogs.
This would need to be supported by suitable corroborative evidence, such as survey results.
Of cats and dogs aren’t humans, so the Equality Act (2010) doesn’t apply to them.
So I do apologise for wasting your time – but the first bit of this blogpost was important, I humbly submit.
Should dementia charities trademark their campaign logos?
The idea of all charities being fluffy and nice is long gone.
One or two have eyewatering incomes which stick in your throat somewhat. They are fully corporate in behaviour, and have access to the same tools used by other corporates (including corporate lawyers).
On the other hand, some dementia activists have ploughed on regardless.
Norman McNamara posted in his Facebook group for people interested in dementia today news of a communication which he’d received.
This was from Jeremy Hughes, CEO of the Alzheimer’s Society, about how the Torbay Ostrich could be shown side-by-side with the Alzheimer’s Society “Forget-me-not” symbol.
In it together?
To make up for this potentially irritating situation, however, Norman has massive goodwill from persons with dementia and their friends.
The idea of dementia communities is not new.
The Torbay Dementia Action Alliance ‘Purple Angel’ is below:
Clearly the “Purple Angel” looks nothing like the “Forget me not” visually.
And adding to the confusion is the issue that the ‘forget-me-not’ is apparently the emblem of members of the Freemasons community, so that they can recognise each other.
See for example this recent e-Bay item.
All of this is incredibly important legally, when you analyse how the law works for infringement of a trademark works under the Trade Marks Act (1994). The relevant clauses are s.10(2)(a) and s.10(2)(b).
The concept of friendship in dementia can be deciphered from a number of different sources in fact.
For example, the concept is a natural extension of the “connected communities” idea of the RSA. This is a programme that explores ‘social network’ approaches to social and economic challenges and opportunities.
They concentrate on understanding and mobilising ‘real world’ face to face networks of support and exchange between citizens, small informal groups, public sector and third sector agencies, and private sector businesses.
Supportive communities are well known in Japan. For example, Fureai kippu (in Japanese ?????? :Caring Relationship Tickets) is a Japanese currency created in 1995 by the Sawayaka Welfare Foundation so that people could earn credits helping seniors in their community.
The basic unit of account is an hour of service to an elderly person. Sometimes seniors help each other and earn the credits, other times family members in other communities earn credits and transfer them to their parents who live elsewhere.
In Japan, there’s a strong ethos of befriending, and English policy has emulated that. Imitation is the best form of flattery, but not when it comes to intellectual property law.
There’s also WHO. The WHO Global Network of Age-friendly Cities and Communities was established to foster the exchange of experience and mutual learning between cities and communities worldwide.
Any city or community that is committed to creating inclusive and accessible urban environments to benefit their ageing populations is welcome to join.
The Joseph Rowntreee Foundation initiative “York Dementia Without Walls” project looked into what’s needed to make York a good place to live for people with dementia and their carers.
They found that dementia-friendly communities can better support people in the early stages of their illness, maintaining confidence and boosting their ability to manage everyday life.
As part of this project, the team also worked with groups of people with dementia to create a dementia-friendly summary of the research.
Thus it can be easily argued that the concept of dementia friendship is generic.
This applies not only to words that begin life as generic terms, but also to words that begin life as brand names but are appropriated by consumers as another word for the types of goods/services they were coined to brand.
This is what happened to the terms “escalator,” “cellophane,” and “aspirin,” which were originally created to serve as marks, but which became so widely used to refer simply to that type of good (any elevated moving stairway, any plastic wrap, any acetylsalicylic acid painkiller) that they lost their ability to brand.
But here, the concept of dementia friendship is already widespread in global policy.
The Alzheimer’s Society have protected their visual mark for “Dementia Friends” on the trademark register for the IPO, as trademark UK00002640312. It is protected under various categories. This is across various classes.
A trademark in English law was traditionally used as a “badge of origin”: a mark or sign that would tell purchasers exactly who had made the particular product they were about to buy.
Today, the largest companies in the world value the goodwill that’s embodied in their names in the hundreds of millions of pounds.
Trademarks distinguish the goods or services of one trader from those provided by its competitors: e.g. a smartphone from Samsung compared to a similar one from Apple.
The overzealous use of registering trademarks is demonstrated well in the recent furore over the word ‘candy’ Gamemakers have mounted a protest against King.com after it trademarked the word “candy”.
The company trademarked the word in Europe in a bid to protect its best-selling Candy Crush Saga game. The Candy Jam webpage said the protest was in response to King.com’s action to defend its trademark.
The Candy Jam page accused King.com of being a “bully” and said the issue had now become one of “freedom and creativity”.
Here, trademarking logos for campaigns is wandering into dangerous territory, when most dementia campaigners wish to promote the concept of friendly communities. However, it is reasonable that any society should wish to act against a competitor producing confusing very similar merchandise.
Nonetheless, at an extreme, protecting the trademark, in this case represented by a commercial and corporate firm known to have a penchant for competition law in contemporary NHS legislation by the current Coalition, might be seen as a tad corporate and bullish.
Here there is an intriguing possibility of a “Goliath” medical charity exerting its right one day to take a “David” medical charity to court over an innocuous mix-up where a smaller charity, without good legal resources, setting up its own dementia friends scheme with a confusingly similar logo.
Whilst a trademark protects innovation in English law like other jurisdictions, it is also a monopolistic right which exerts an anti-competitive effect.
This is actually a formidable legal policy issue, known to Barack Obama and Abraham Lincoln.
If it shows ‘mission creep’ in the form of large charities ‘competing’ in the third sector with the help of the commercial law, that’s arguably a problem.
In theory, the Freemasons could wish to argue in court that their motif, being more longstanding, is being infringed by the Alzheimer’s Society symbol.
I am not aware that the Freemasons hold a registered trademark for the “forget-me-not” symbol. If they don’t, they are open to take a claim in the common law of tort of passing off.
However, this motif also exists on the Trade Marks Register (and several similar others.)
And as it is a prior motif by Landsforeningen LEV, it would be up to Landsforeningen to argue it was sufficiently similar. They would have the right to raise an objection as the Alzheimer’s Society registered their ‘dementia friends’ trademark after their ‘forget-me-not’ symbol.
The Alzheimer’s Society would only have to argue that theirs is sufficiently different because of the words “Dementia Friends”, it’s for a different sector entirely, and in a different colour. And they could easily produce survey data to demonstrate there had been no confusion, one speculates.
But the colour combo is unfortunate!
But you see what I mean?
It gets unnecessarily corporate, complicated and potentially costly to go down this route.
At worst, this registration of a trademark sends a powerful message to any other smaller dementia charities wishing to promote the concept of friends, in a move not dissimilar to pre-emptive “cybersquatting” for a domain name.
A danger here comes down to what you mean by ‘badge of orgin’.
People may think that the Alzheimer’s Society is the sole origin of the idea of friends in dementia, where as I’ve described it comes from a number of sources which have acted rather in parallel, or in a collaborative manner.
On the other hand, it is perfectly reasonable for the Alzheimer’s Society to wish to protect strongly their emblem, in case a competitor tries to copy it in such a way a member of the public might get confused with that precise initiative in which the Alzheimer’s Society have presumably invested quite a lot of time, money and effort.
But we are perhaps taking a leaf now out of the US “competition” book, which caused the market in the NHS in England to be turbo-boosted through the ill-fated “section 75″ and associated Regulations.
In the U.S. non-profit sector, there has been a growing problem with the phenomenon of ‘brandjacking’.
A guest blogpost here describes how the Christmas SPIRIT Foundation accidentally discovered an industry competitor “had created a copycat ripoff of our TweetUp4Troops effort to generate support for the Foundation’s Trees for Troops program”.
Indeed, in the article, the author describes:
“To engage more consumers in the program and to generate financial support for Trees for Troops, the Foundation created and organized TweetUp4Troops events to be held during Veterans Day Week (Nov 7-14). As part of the campaign, the Foundation created a TweetUp4Troops group site, web site and Twitter handle.”
Charities are able to register a trademark, particularly if they have the funds,a visually attractive emblem such that any infringer can take be taken to court, for an injunction or damages (for example).
But is this actually how we want charities to operate, the income source of which includes people who have given up money to further a cause very personal to them?
It is sad that certain charities are tending to work in increasingly corporate ways, with a good understanding of the application of the commercial and corporate law, to secure competitive advantage in an intensely difficult market.
The Alzheimer’s Society clearly has a head start in marketing their ‘Dementia Friends’ initiative, through their badges which can be worn by MPs in parliament.
It also has a very powerful strategic partnership with the Department of Health in promoting the Prime Minister’s Dementia Challenge.
While there is clearly a need for the Alzheimer’s Society to protect their brand in ‘Dementia Friends’, there is a difficult balance to be enforced to make sure that this does not impede smaller entrants to the market of fundraising.
This is especially critical given how difficult is has been for smaller charities and community interest groups involved in dementia to keep going, despite of or because of the Prime Minister’s Challenge.
[Many thanks to C.R. for a discussion of the meanings of an emblem discussed in this blogpost.]
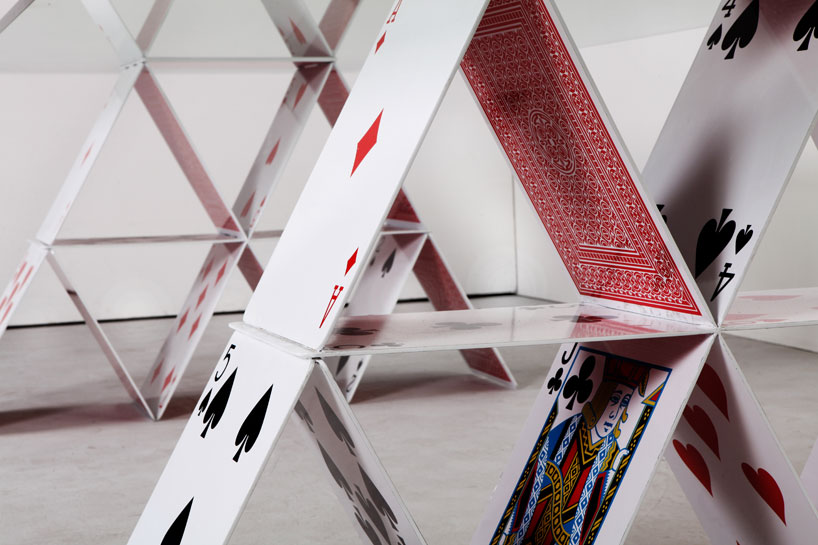
Like a faulty house of cards, the competition rationale for the Health and Social Care has fallen apart
In the beginning….
In the beginning, there was garbage and rhetoric. It sounded nice, but it was intellectually devoid of quality, there was not much competition for ideas even though this WAS bad, and so there was not much choice.
Julian LeGrand back in 2003 talks of the “competition juggernaut”:
Labour has made many mistakes, usually and unsurprisingly given its roots in socialism and central planning, in the direction of too heavy-handed central control. The public service juggernauts are now on a different course, with decentralisation, competition and choice as part of their route maps – and with plenty of resources as fuel. If they fail to arrive at their destination, if our expectations are dashed, there will be real questions over the future of each area of public services: how long can it remain public; how long can it remain a service?
‘Competition fever‘ should have never have got off the ground. The University of York, Economics of Social Care and Health Unit, and Centre for Health Economics once published a study of ‘Hospital competition under fixed prices’ (research paper 80).
The argument that competition improves quality fell apart because of the sheer volume of invalid assumptions, as demonstrated in the following quotation from that document:
The review of the theoretical literature suggests that the plausible argument that greater competition amongst providers facing fixed prices will lead to higher quality rests on strong assumptions which may not hold. The literature shows that more competition increases quality when providers are profit maximisers and marginal cost of treatment is constant. Competition has an ambiguous or negative effect on quality when providers are altruistic, the marginal cost of treatment is increasing and quality is only imperfectly observable. The literature has been largely silent on the relationship between market size, as measured by total population or population density, and quality.
Competition as the failed central plank of the Health and Social Care Act (2012)
The raison d’être of the Health and Social Care Act (2012) is nothing to do with improving clinical care, though that could be a consequence of its three main areas. There is nothing about how patient staffing can be addressed, related to the equally potent issue of patient safety. It has never been entirely clear how the Act came about, but the three planks of policy are laid bare by the impact assessments from the Department of Health (2011) (published here on 19 January 2011). The three main planks of the Bill are firstly to establish the competitive market as the substrate for the National Health Service, to define better the insolvency régime (it is important to clarify how economic entities as autonomous units can be allowed to fail ‘to get them out of the system’), and the machinery needed to regulate the market. I will come to how Monitor has had to come into being to ‘regulate the internal market’, but it is not insignificant that introducing the market is itself a source of waste and inefficiency (such as duplicated transaction costs). Of course, the issue of how to regulate the internal market should be regulated has often been analysed in a substandard manner before by some social scientists, not competition lawyers, but this is now an important policy issue which has been thrust into the limelight.
Central to this argument is that competition promotes innovation. This is indeed cited on page 41 of the “Impact assessment”.
Ahn (2002) reviews a large number of studies on the link between competition and innovation and concludes that competition encourages innovative activities and has a significant impact on long-term productivity growth:
“Competition has pervasive and long lasting effects on economic performance by affecting economic actors’ incentive structure, by encouraging their innovative activities, and by selecting more efficient ones from less efficient ones over time”.
The myth that competition drives innovation, when COLLABORATION does
However, there is an intrinsic problem in business management: the assumption that competition drives innovation. This bit of missing evidence in the impact assessments totally distorts the raison d’être of the Act itself, and of course there is a separate debate in management as to whether innovation can be detrimental to organisational culture or learning. There is considerable evidence now that collaboration, not competition, can be essential for innovation. This theme is taken up in an interesting article about ‘internal markets’ from Forbes:
Major innovation needs collaboration, not competition. For innovation, internal markets have the same problem as hierarchical bureaucracies. Managers vote their resources for innovations that bolster their current fiefdoms and careers. The safest strategy is to stick to the status quo. Ms. Kimes’ article gives multiple examples where competing managers at Sears looked after their own units at the expense of the interests of the firm as a whole.
Second, innovation isn’t basically an issue of spending. Booz & Company’s annual innovation reports repeatedly state: “Spending more on R&D won’t drive results. The most crucial factors are strategic alignment and a culture that supports innovation.”
Finally, the hope of the internal markets theory is that, by funding a variety of different ideas, the organization will emulate the evolutionary process of natural selection and so the best ideas will survive and prosper. The problem is that once a disruptive idea starts to flourish and becomes more interesting than the normal bread-and-butter work of the organization, it risks becoming a threat to the rest of the organization.
The wheels are coming off the Competition Juggernaut a bit sooner than expected
David Williams at the Health Services Journal only very recently on 16 September 2013 reported that:
NHS England has delayed the publication of its choice and competition framework amid a “paucity of evidence” of the benefit to patients.
Policy director Bill McCarthy made the announcement at a board meeting on Friday, highlighting the issue as a new risk for the central body.
The framework and supporting documents were originally slated for publication in July.
Mr McCarthy said: “We’re having [a discussion] with Monitor around choice and competition, and how best they can be applied in healthcare to improve outcomes for patients, including a better experience.
“That’s taken a bit longer than we hoped.
“We had hoped to be able to put out some guidance early in the summer – I think that probably reflects… it is one of the areas where there is a paucity of evidence.”
“Operation Propper”
Clause “B47” (p.42/3) in the official Impact Assessments from the Department of Health cites one of the key planks of evidence that the Department of Health wishes to use in promoting its competition argument.
“A July 2010 study by health economists Martin Gaynor, Rodrigo Moreno-Serra, and Carol Propper investigated outcomes in the NHS following the introduction of choice in 2006. They conclude as follows: “We find that the effect of competition is to save lives without raising costs. Patients discharged from hospitals located in markets where competition was more feasible were less likely to die, had shorter length of stay and were treated at the same cost”. The study found that there was a larger inflow of patients to better quality hospitals after the 2006 NHS reforms, suggesting that popular providers in health care are able to expand supply.”
There is an even worse justification for the competition dogma later in the Department of Health’s official impact assessments:
B48. A January 2010 study by the London School of Economics also looked at NHS data post- introduction of choice in 2006. The key conclusion is as follows: “Using AMI mortality as a quality indicator, we find that mortality fell more quickly (i.e. quality improved) for patients living in more competitive markets after the introduction of hospital competition in January 2006. Our results suggest that hospital competition in markets with fixed prices can lead to improvements in clinical quality”.
B49. Evidence from the LSE shows that management quality – measured using a new survey tool – is strongly correlated with financial and clinical outcomes such as survival rates from emergency heart attack admissions (AMI). Moreover, the study finds that higher competition (as indicated by a greater number of neighbouring hospitals) is positively correlated with increased management quality.
The general issue received a scathing response from Allyson Pollock, Alison Macfarlane and Ian Greener who could not have put it any clearer.
The major improvements in outcome after acute myocardial infarction can be attributed to improvements in primary prevention in general practice and in hospital care, including the introduction of percutaneous IV angiography. The government’s own cardiac Tzar, Sir Roger Boyle, was sufficiently angered by their claims to respond with withering criticism: “AMI is a medical emergency: patients can’t choose where to have their heart attack or where to be treated!” It is “bizarre to choose a condition where choice by consumer can have virtually no effect”. Patients suffering “severe pain in emergencies clouded by strong analgesia don’t make choices. It’s the ambulance driver who follows the protocol and drives to the nearest heart attack centre”.
The intervention that the authors claimed reduced heart attacks and was a proxy for competition was patient choice. In 2006, patients were given choices of hospitals including private for-profit providers for some selected treatments. Less than the half patients surveyed in 2008 even remember being given a choice, and only a tiny proportion made those choices based on data from the NHS choices website. If patient choice was one of the two key elements of competition, it wasn’t prevalent and rather than being derived from the authors’ data, it was assumed.
Crucially, even if patient choice had occurred it does not explain why heart attack mortality rates fell. There is no biological mechanism to explain why having a choice of providers for elective hip and knee operations surgery (including hospitals which did not treat or admit acute MI patients) could affect the overall outcomes from acute myocardial infarction where patients do not exercise choice over where they are treated.
The problem of data dredging is well known; if you repeat an analysis often enough significant statistical associations will appear. But the authors make the cardinal error of not understanding their data and of confusing minor statistical associations with causation. Deaths from acute MI are not a measure of quality of hospital care, rather a measure of access to and quality of cardiology care. At best, what the paper appears to show is not the effect of choice on heart attacks but that if an individual has a heart attack in an area close to a hospital and their GP is near the hospital, then outcomes are better, but such findings are not new.
Going for their central criticism, in the same article, they explained:
The drip feed of pro-competition studies from Zack Cooper at LSE raises serious questions for the academic community and the public about what constitutes bad science and what to do about its politicisation. Recently, on 21 February in the columns of the FT, Cooper and colleague Julian Le Grand warded off serious scientific criticisms of the studies with an ad hominem attack, categorising those in favour of competition as empiricists and those whose work is critical of markets in health care as intuitivists. In so doing they sweep aside decades of careful economic theory and evidence which shows why markets do not work in health services and distract the reader from the facts that their work is ungrounded and far from empirical. Their repeated claims that competition in the NHS saves lives and improves quality and productivity have no scientific basis.
A litigation factory?
Of course the £3bn Health and Social Care Act (2012) which have no mechanisms of helping with clinical staffing or patient safety, in the drive for business efficiencies, have become a bonanza for private companies to which work has been outsourced, and a boon for the commercial and corporate law firms which are now nurturing them. The NHS of course has trouble in meeting the formidable legal bill against the private providers, as well as staff it has made redundant due to this top-down reorganisation.
I have long argued that the commissioning (‘competition and choice’) process through section 75 Health and Social Care Act (2012) would soon turn sour, for example in the original blogpost I did for the Socialist Health Association in January 2013 here. Crispin Dowler recently reported early tensions on 11 September 2013 in the Health Services Journal:
A number of private providers are likely to take complaints to the NHS’s new competition regulator Monitor over the next three years, the chief executive officer of Ramsay Health Care UK warned last week.
Jill Watts, whose organisation was ranked the largest private provider of NHS funded acute care in the most recent study by market analysts Laing and Buisson, said she could “almost guarantee” there would be challenges to come.
She told a Westminster Health Forum conference that the April switchover to clinical commissioning groups under the government’s health reforms had not produced uniform changes in commissioners’ attitudes to the private sector.
“In one part of the country, where we had almost adversarial relationships and they didn’t want to use us at all, they’re very keen to work with us now,” she said.
The New Labour Legacy, competition, performance and “the target culture”
Competition was intimately wound up in the target-driven agenda. NHS hospitals would have to meet targets to jump through regulatory hoops to become NHS Foundation Trusts. As long as finances stacked up, patient safety appears to have suffered in some Trusts under Labour’s watch. Whilst the evidence for competition being beneficial in the NHS market is weak, it has remained with us in policy like a bad smell. Julian LeGrand could have not put better how idiotic this policy really was.
The problem is indeed partly money – a historical legacy of underspending in all areas of public services. But, as John Hutton says, it isn’t only that. There is also a legacy of poor performance: of failing to use what resources there are effectively and efficiently. This is a lesson that six years in power have taught New Labour. The Government has tried and is trying a wide variety of techniques to lever up performance: publishing league tables on comparative performance, encouraging private sector involvement, offering independence to high fliers, stimulating competition and choice. But one of its favourite instruments has been targetry: the setting of targets with heavy penalties for failing to meet them. Many in government are convinced that this is the way to go.
Preface to my book: “Living well with dementia: where the person meets the environment”
Introduction
According to the Department of Health’s “Improving care for people with dementia” (2013), there are around 800,000 people with dementia in the UK, and the disease costs the economy £23 billion a year. By 2040, the number of people affected is expected to double – and the costs are likely to treble. There is no doubt therefore about the scale of the problem, and it needs the finest minds in showing leadership on how to enable individuals with dementia to live better, and indeed live well. The Prime Minister’s Challenge on dementia (“Challenge”) (2012) set out a renewed ambition to go further and faster, building on progress made through the National Dementia Strategy, so that people with dementia, their carers and families get the services and support they need. This Challenge wished to address in particular certain issues, such as the observation that the number of people with dementia is increasing, that currently the diagnosis rates are thought to be low, and there is sadly a lack of awareness and skills needed to support people with dementia and their carers. Whilst it is possibly difficult to find a ‘miracle cure’ for dementia, it is a reasonable aspiration for individuals with dementia (and their immediates) to have as best a quality-of-life as possible, and it is not necessarily the case that subtle but significant improvements in quality-of-life will “cost the earth”.
It is intended that this book should not just of interest in the UK, as the problems in healthcare are relevant to all jurisdictions. Thinking about how society should respond does pose some jurisdiction-specific issues; for example, this book refers to legislation in the UK such as the Equality Act (2010) or the Mental Capacity Act (2005), or regulations in health and safety relevant to building design in the UK. However, a consideration of the global issues in public health leads one quickly to appreciate the complexity of the economic case for improving wellbeing in individuals in dementia and their immediates, and that there are many people who are genuinely interested. Whilst indeed there has been a lead through the Prime Minister’s Dementia Challenge (2012), it is clear that previous administrations in England have latterly decided to prioritise dementia as a public health priority (for example, the National Dementia Strategy, “Living well with dementia” (2009)).
The ‘ecosystem’ of interested parties is large, and it is striking that there are so many passionate ‘#dementiachallengers’ on Twitter daily for example who are always a source of contemporary information, enthusiasm and innovation. There are currently huge advances being made in research and policy, and it is only possible through dementia communities ‘working together’ to keep abreast of them all. For that reason, this book has necessarily had to include electronic references, and I have tried to maintain links as correct as up-to-date at the time of publication. However, please feel free to look for any related information anywhere, and please do not use this book as an authoritative source of information to rely on necessarily. This book is intended simply as an introduction to a vibrant field, and certainly please be guided by healthcare professionals regarding individual care. The text of this book provides general principles, which I hope you might find interesting.
NICE quality standard 30 on ‘supporting people to live well with dementia’
In April 2013, NICE published its quality standard 30 on ‘supporting people to live well with dementia’. This quality standard was intended to cover the care and support of people with dementia. It applies to all social care settings and services working with and caring for people with dementia.
NICE quality standards are supposed to describe high-priority areas for quality improvement in a defined care or service area. Each standard consists of a prioritised set of specific, concise and measurable statements. NICE quality standards draw on existing guidance, which provide an underpinning, comprehensive set of recommendations, and are designed to support the measurement of improvement.
The areas covered in this ‘quality standard’ includes:
Statement 1. People worried about possible dementia in themselves or someone they know can discuss their concerns, and the options of seeking a diagnosis, with someone with knowledge and expertise.
Statement 2. People with dementia, with the involvement of their carers, have choice and control in decisions affecting their care and support.
Statement 3. People with dementia participate, with the involvement of their carers, in a review of their needs and preferences when their circumstances change
Statement 4. People with dementia are enabled, with the involvement of their carers, to take part in leisure activities during their day based on individual interest and choice.
Statement 5. People with dementia are enabled, with the involvement of their carers, to maintain and develop relationships.
Statement 6. People with dementia are enabled, with the involvement of their carers, to access services that help maintain their physical and mental health and wellbeing.
Statement 7. People with dementia live in housing that meets their specific needs.
Statement 8. People with dementia have opportunities, with the involvement of their carers, to participate in and influence the design, planning, evaluation and delivery of services.
Statement 9. People with dementia are enabled, with the involvement of their carers, to access independent advocacy services.
Statement 10. People with dementia are enabled, with the involvement of their carers, to maintain and develop their involvement in and contribution to their community.
Overview
The aim of this book was not to provide a prescriptive text for this quality standard. I hope the book will be useful for a ‘diverse audience’, in other words anyone interested in the diagnosis, investigation or management of dementia, with especial emphasis on improving wellbeing; such interested people might particularly include the general public, psychologists, innovation specialists,, psychiatrists, neurologists, geriatricians, general medical physicians, nurses, public health physicians, medical students, engineers, economists, psychologists, commissioners and hospital managers. It is therefore extremely hard to find all this information ‘in one place’, and it is hoped that this book will help to provide a much needed overview and to build bridges between different ‘silos’ of thinking.
The approach of the National Dementia Strategy: Living well with dementia (from the Department of Health) (2009) devotes the whole of its chapter 5 to the issue of living well with dementia. In the preceding chapter to this Strategy, chapter 4on ‘early diagnosis’, the approach described is obviously inclusive:
“From our consultation, and based on a successful DH pilot and the DH cost- effectiveness case, it appears that new specialist services need to be commissioned to deliver good-quality early diagnosis and intervention. Such services would need to provide a simple single focus for referrals from primary care, and would work locally to stimulate understanding of dementia and referrals to the service. They would provide an inclusive service, working for people of all ages and from all ethnic backgrounds.”
A ‘timely diagnosis’ is only of benefit, it is felt if there is a ‘useful’ intervention in dementia: this is described in chapter 4 has having three essential components: making the diagnosis well, breaking the news of the diagnosis well to the individual with dementia and their immediates, and providing directly appropriate treatment, information, care and support for such individuals. This timely book is part of a drive to dispel the notion that ‘nothing can be done’ in the context of management of dementia, even if current pharmacological therapies might have limited efficacy. The book is an overview of the field, describing what ‘wellbeing’ actually means, and why it is important in the context of national policy. The book quickly establishes the importance of the ‘person’ in discussing dementia care, including independence, leisure and other activities, and, in the final stages, end-of-life care, which is a discussion which should not be avoided. No individual with dementia should be abandoned in relation to his or her environment, and indeed there is much evidence to support the idea that the environment can be optimised to improve the wellbeing of an individual with dementia and his/her immediates. Considerations include home and ward design, the use of assistive technologies and telecare, and the ‘built environment’. A constructive interaction of an individual with his or her environment is clearly vital, and this includes understanding communication issues, how to champion the rights of an individual living well with dementia through independent advocacy, and the way in which ‘dementia friendly communities’ can be supported.
Contents
- Introduction
- What is “living well with dementia”?
- Measuring living well with dementia
- Socio-economic arguments for promoting living well with dementia
- A public health perspective on living well in dementia, and the debate over screening
- The relevance of the person for living well with dementia
- Leisure activities and living well with dementia
- Maintaining wellbeing in end-of-life care for living well with dementia
- Living well with specific types of dementia: a cognitive neurology perspective
- General activities which encourage wellbeing.
- Decision-making and an introduction to advocacy in living well with dementia
- Communication and living well with dementia
- Home and ward design to promote living well with dementia
- Assistive technology and living well with dementia
- Ambient-assisted living well with dementia
- The importance of built environments for living well with dementia
- Dementia-friendly communities and living well with dementia
- Conclusion
Chapter synopses
It is possible to read each chapter in this book independently, and indeed each chapter is independently referenced.
Chapter 2 is an introduction to the whole book. Introduces the concept of what is like to ‘live well with dementia’. Investigating wellbeing has broadened the scope of previously overly narrow approaches to healthcare, in measuring outcomes. This chapter also introduces the idea that it is grossly unfair to consider ‘dementia’ as an unitary diagnosis, as in fact the term is a portmanteau of hundreds of different conditions at least. There has been a growing trend that ‘dementia’ and ‘memory problems’ are entirely synonymous, and this has added unnecessary noise to the debate. Dementia care is currently done in a number of different settings, and assisted living may be of increasing relevance in a drive to encourage individuals to live well independently with dementia.
Chapter 3 presents the formidable challenges of how ‘living well’ might be measured in general. There are issues about how quality of life measures change as a dementia progresses, what the relationship might be between wellbeing and physical health, and how wellbeing in dementia should be measured accurately at all.
Chapter 4 looks at the current socio-economic arguments for promoting a wellbeing approach in dementia. There are a number of converging cases for considering wellbeing, such as the economic case, the ethical case and a case based on social equality. While resources are limited, serious considerations have to be made as to which interventions are truly cost-effective, including of course the assistive technologies.
Chapter 5 presents the background for dementia as a public health issue in the UK. There is also a very active debate as to whether one should ‘screen’ for dementia. A core aim of the National Dementia Strategy (1999) is therefore to ensure that effective services for early diagnosis and intervention are available for all on a nationwide basis. It is argued, in this Strategy, that “the evidence available also points strongly to the value of early diagnosis and intervention to improve quality of life and to delay or prevent unnecessary admissions into care homes.”
Chapter 6 considers how and why being a ‘person’ has become so central to living well with dementia in academic and practitioner circles. In a way, the approach of ‘person-centred care’ is a historic one, but it has been a consistent strand of English health policy developing into contemporaneous views of integrated and whole-person care. This chapter also introduces ‘personhood’, and the approach of ‘dementia care approach’.
Chapter 7 addresses the specific rôle of leisure activities for an individual with dementia. Leisure activities are generally considered for many to be beneficial for the mental and physical wellbeing of individuals with dementia, and there are specific problems to be addressed such as the reported levels of relative inactivity in care homes.
Chapter 8 details how wellbeing is relevant also to end-of-life in dementia. This chapter considers the importance of support for carers, for the wellbeing of individuals with dementia and their carers. This chapter considers where optimal care could be given for individuals with dementia, the contribution of medication, but how it is vital to address specific issues in advanced dementia which have a direct impact on wellbeing (such as pain control).
Chapter 9 identifies that it is in fact it is impossible to consider dementia as a unitary diagnosis, and that specific forms of dementia can present their own formidable demands and issues. This chapter considers in detail how and why memory problems can be a presenting feature of dementia of the Alzheimer type, and the implications for interventions in wayfinding which could rationally improve wellbeing in such patients. The chapter also includes recent elegant work about the neural networks which are hypothesised to be important in behavioural variant frontotemporal dementia, and how this “social context network model” fundamentally affects our notion of wellbeing in such individuals.
Chapter 10 introduces ‘general activities which encourage wellbeing’, in a first chapter on the possibility of “assistive technologies” in enabling individuals with dementia to live well. Certain memories can be particularly potent in the dementia of the Alzheimer Type, and, whilst the ‘jury is possibly out’ on the validity of reminiscence therapy, the chapter discusses the possible benefits of the CIRCA project on the wellbeing of individuals with dementia. Other activities are also considered; how they may help wellbeing, such as dancing, exercise, and music.
Chapter 11 takes up an important theme in living well with dementia; that is empowering the invididual to make decisions, the law relating to capacity, and how independent advocacy services have a beneficial rôle to play. Independent dementia advocacy is a critical area of a statement in NICE QS30, and this chapter reviews types of advocacy (and its relevance to wellbeing and person-centred care), the current mental capacity legislation, and the crucial importance of diversity and equality in policy.
Chapter 12 explains why good communication is so crucial in the setting of individuals living well with, but not simply restricted to healthcare professionals. This not only appears to be in terms of providing information about the condition locally, but also face-to-face communication with people living well with dementia. This chapter looks in detail at both verbal and non-verbal methods of communication, with a view to raising awareness of their impact on living well with dementia.
Chapter 13 analyses the importance of home and ward design for improving wellbeing in dementia. ‘Therapeutic design’ is a central philosophy of good design, and this chapter has as its focus a number of different setting. General principles are described as how to wellbeing can be improved through careful design of certain parts of the house (such as balconies, bathrooms, bedrooms, living rooms and dining rooms), and considers the neuroscience of sensory considerations at play (for example in lighting and vision, and sound and hearing.)
Chapter 14 is the first of two chapters on ‘assistive technologies’ in dementia, providing an overview of this important area for living well with dementia. This chapter explains what ‘assistive technology’ is, what its potential limitations are, the INDEPENDENT project, the importance of “telehealth” (and important ethical considerations), and the design of ‘smart homes’.
Chapter 15 is the second of two chapters on ‘assistive technologies’ in dementia, looking specifically at an approach called ‘ambient-assisted living’ (AAL). The rationale behind the use of AAL in improving wellbeing is explained, as well as the general issue of how to encourage adoption of innovations in an older population. Detailed examples of specific AAL projects in improving wellbeing are described including SOPRANO, COACH and NOCTURNAL.
Chapter 16 introduces the general emphasis on the ‘built environment’ setting, and how inclusivity still drives this area of work in living well with dementia. Ageing presents its own challenges including opportunities and threats, but this chapter focuses on the remarkable initiatives which have recently taken place in improving the outside environment for individuals with dementia. The chapter details the I’DGO project, and highlights the especial importance of inclusive design for furthering wellbeing in dementia outside environments.
Chapter 17 considers how an individual with dementia lives as part of the rest of a community and society, and policy initiatives which have sought to address this. The discussion is unexpectedly problematic about a need to define what a ‘community’ might be, but the chapter includes domestic and international approaches to the ‘dementia-friendly community’, including the RSA’s “Connected Communities” and WHO’s “age-friendly communities” initiatives. As a central policy plank which is thought to be critical for developing wellbeing in individuals with dementia and their immediates, this chapter considers why dementia-friendly communities are worth encouraging at all, why there is a societal need to involve individuals with dementia in their communities, what aspects individuals with dementia wish from such communities (including the “Four Cornerstones” model), and the benefits of “resilient communities”.
Further information
You are advised to look at specialty websites which are devoted to all the dementias (such as medical charities), which often have useful information factsheets and booklets. Also, the Department of Health and their ‘Dementia Challenge’ website is an impressive source of information. You are also advised to consult https://www.evidence.nhs.uk which has access to a number of useful contemporaneous clinical evidence sources. Online medical journals are also an excellent source of peer-reviewed research, such as the BMJ, the Lancet, and the New England Journal of Medicine.
Looking to the future
There are, of course, no “right answers” to many issues, and a wise person is a person who knows where to find relevant information. However, the sense of optimism and goodwill is a genuine one in UK health policy, regarding dementia. Whilst there will often be difficult debates regarding dementia such as “How willing should a GP be to make a diagnosis of dementia when a patient has only gone to see his GP because of a sore throat?” or “Should we look to research a drug which can immunise people against dementia?”, the fact there are so many bright people in the UK working in areas relating to dementia is a real credit to English health policy as it faces formidable challenges of its own.
References
Department of Health (2009). Living well with dementia: A National Dementia Strategy: Putting people first. London: Her Majesty’s Stationery Office. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/168221/dh_094052.pdf.
Department of Health (2013) The Dementia Challenge. London: Her Majesty’s Stationery Office. Available at: http://dementiachallenge.dh.gov.uk
Department of Health (2013) Improving care for people with dementia. London: Her Majesty’s Stationery Office. Available at: https://www.gov.uk/government/policies/improving-care-for-people-with-dementia
Department of Health (2012) The Prime Minister’s “Dementia Challenge”: Delivering major improvements in dementia care and research by 2015. London: Her Majesty’s Stationery Office. Available at: https://www.gov.uk/government/policies/improving-care-for-people-with-dementia
National Institute for Clinical Excellence (2013). Supporting people to live well with dementia (QS30). Available at: http://guidance.nice.org.uk/QS30.
UK government. Mental Capacity Act (2005) http://www.legislation.gov.uk/ukpga/2005/9/contents
"Lincoln" at the #Oscars: innovation, a story of charismatic leadership and MEN2B
There are many aspects of Abraham Lincoln which interest me, not least his attributes of leadership, his contribution and interest in innovation, and his possible underlying diagnosis.
Abraham Lincoln is a model for a charismatic leader, having been well-known to be a great story-teller, as explained here:
“Watching the superb film “Lincoln” by Steven Spielberg, I discovered a very important fact about our 16thPresident that I wasn’t really aware of. He was a great storyteller. I knew he was strong in his speechmaking (having memorized the Gettysburg Address in Grade School, along with countless other youngsters), but I didn’t know how skillfully he used the power of story to lead and inspire, to defuse tension and to stir an audience. He was an expert in using powerful language, imagery and humor to get across key points, to open listeners’ ears to another point of view, and to convey practical advice and wisdom that people then wanted and needed to retell themselves. He didn’t force his messages on his audience, he let in unfold in their own imaginations.”
Lincoln was apparently also a great inventor, and many consider him to be the “father of innovation” in the United States. As an attorney, he represented railroads. During the Civil War, he haunted the telegraph office (which provided the instant-messaging of its day) for the latest news from the front and was actively involved in directing troops. He encouraged weapons development and even tested some new rifles himself on the White House lawn. Patent No. 6469, a device for buoying vessels over shoals, makes Abraham Lincoln the only U.S. president to hold a patent. From The New Atlantis, it is described that:
“As a young man, Lincoln had spent some time on riverboats, transporting farm produce and other cargo down the Mississippi River to New Orleans. In 1848, then-Congressman Lincoln was a passenger on a boat in shallow Illinois waters when a passing boat ran into a sandbar. He watched as the captain ordered his crew to place anything that would float—especially empty barrels and boxes—under the sides of the boat for buoyancy. That incident was the direct inspiration for Lincoln’s invention: “buoyant air chambers” made of “water-proof fabric”; they could be inflated and deflated as needed to help keep a boat afloat.”
Although Lincoln was a weapons aficionado, perhaps his greatest contribution to the war effort was his use of the telegraph. Tom Wheeler, author of Mr. Lincoln’s T-Mails: The Untold Story of How Abraham Lincoln Used the Telegraph to Win the Civil War, notes that Lincoln had not even seen a telegraph in operation until 1857. That was twenty-two years before the invention of the light bulb, a time when electricity was a vague scientific concept and sending signals through wires “mind boggling.” Lincoln was fascinated and quizzed the operator about how the telegraph worked. “If he were alive today, we’d call him an early adopter,” says Wheeler.
There has been a longstanding controversy about what the clinical diagnosis of Abraham Lincoln was. The nature and cause of President Abraham Lincoln’s unusual physical features have long been debated, with the greatest attention, recently, directed at two monogenic disorders of the transforming growth factor ? system: Marfan syndrome and multiple endocrine neoplasia type 2B (“MEN 2B”). MEN 2B typically manifests before a child is ten years old. Affected individuals tend to be tall and lanky, with an elongated face and protruding, blubbery lips. Benign tumors can develop in the mouth, eyes, and submucosa of almost all organs in the first decade of life. Medullary thyroid cancer almost always occurs, sometimes in infancy, and is often aggressive. Cancer of the adrenal glands, phaeochromocytomas (sic), occurs in 50% of cases.
Recent work has examined newly discovered phenotypical information about Lincoln’s biological mother, Nancy Hanks Lincoln, and concluded that (a) Lincoln’s mother was skeletally marfanoid, (b) the President and his mother were highly concordant for the presence of numerous facial features found in various transforming growth factor ? disorders, and (c) Lincoln’s mother, like her son, had hypotonic skeletal muscles, resulting in myopathic facies and ‘pseudodepression’. These conclusions establish that mother and son had the same monogenic autosomal dominant marfanoid disorder. A description of Nancy Hanks Lincoln as coarse-featured, and a little-known statement that a wasting disease contributed to her death at age 34, lends support to the multiple endocrine neoplasia type 2B hypothesis.
A Californian cardiologist John G. Sotos of Palo Alto came up with the idea that the 16th American president suffered from a mutation named MEN 2B that could be easily tracked down through DNA analysis of the gene RET on chromosome 10. MEN 2B (multiple endocrine neoplasia type 2B) leads in 100 % of the cases to thyroid cancer and 50 % of the patients also develop adrenal gland cancer and could explain Lincol’s great height and other conditions.
Anyway, I wish Daniel Day-Lewis well in his nomination for Best Actor for “Lincoln” this morning. I bet my life he wins.
What does Ed Miliband really think?
Steve Richards, political columnist for the Independent, recently produced a fascinating portrayal of Ed Miliband. If you missed the programme, you can listen to it here on the BBC website.
I have always felt that David Cameron is in office, but not in power. He failed to win the General Election, despite widespread media backing and a deeply unpopular final Labour administration. More significantly, I feel that David Cameron is a manager, and not a leader; and a very poor one at that. This production, “What does Ed Miliband think?”, is in my opinion a very timely radio documentary by Steve Richards, as Ed Miliband takes stock of his first two years as leader of the Opposition and leader of the UK Labour Party. In recruitment, the philosophy is that you choose an employee based on his or her known interests and competences, as a ‘predictor’ of future success in that job.
Steve Richards early on cites the ‘responsible capitalism’ of the Labour Conference of 2011. I remember that speech, but I didn’t take away the prominent soundbite of ‘predator capitalism’. I was midway through a MBA at the time, and the territory of ‘responsible capitalism’ had already been known to me. The concept of a responsible corporate citizen is a very important one here in the UK, and in the US, and has a formidable academic history. I think part of the reason it was so badly received by commentators was that some phrases in the speech might have been imprecise, but also because the background to this theme had already been poorly known. I think it was brave of Ed Miliband to bring up the big argument of why it is insufficient simply for company directors to maximise shareholder dividend, ignoring the sentiments of the general public (including even consumers).
Ed Miliband is quizzed bluntly by Steve Richards about rail franchising. The complaint about the lack of policy detail is appropriately confronted by Richards, and is one that I know vexes many other members of Labour. There is a detailed policy review underway, but areas where Miliband wishes to appear to distance himself from New Labour are clearly identified. This in marketing terms is about producing a ‘unique selling proposition’, with the majority of Labour geeks (rightly) balk at. Here, it is perhaps relevant what Ed Miliband is not, rather than what he is. What he isn’t is a ‘PR man’, a criticism which Ed Miliband indeed threw at David Cameron last week in Prime Minister’s Questions. Ed Miliband is taking his own to produce a coherent political philosophy, whilst clear to disengage himself from the New Labour ‘brand’. This, I suspect, will be a popular move, even it has been previously described as bordering on populist. When I first met Ed Miliband at his final hustings at Haverstock Hill, I remember asking himself about inequality. He was genuinely very disappointed about Labour’s record on inequality, and has amused to hear my observation that neither the word ‘inequality’ nor ‘poverty’ featured in the index of Tony Blair’s “The Journey”.
The personal friendship with Lord Wood is an interesting one, as the portrayal previously had been of a rather ‘geeky loner’ who had been dwarfed by the academic shadow of his father, Ralph. Indeed, Ed Miliband clearly has elegantly articulated reservations about globalisation and institution themes of Blue Labour. However, it is the argument which Richards then assumes is one which I find intriguing. Miliband is compared to Thatcher (during the opposition years), and Miliband talks about a parallel of how he wishes to ‘rise to the challenge’. Again, I feel that this is where a knowledge of the management and leadership literature really helps. What Miliband is describing is ‘charismatic leadership’, of a figure which the public picks out as a candidate to steer them through a time of political, social, and economic turmoil. Charles Moore’s criticism that there is no goal, such as attacking the power of the trade unions or getting inflation down, is perhaps valid. These are very early days though. Ed Miliband’s “get out of jail” card has recently, ‘we cannot predict what the economy will be like in three years time”, which is indeed true when you consider that we may shortly be entering a “triple dip”. It could be that Ed Miliband does find an easily identifiable issue, such as boosting the constructive industry to provide new housing, or breaking up oligopolies such as banks or utilities such that greater value is returned to the consumer as well as the shareholder.
The lack of policy details, thus far, is one that continues to trouble Labour activists. The ‘opaque’ process, it is described, means that there could be “unexploded bombs”, which might explode accidentally near the time of the General Election. I agree there is a clear direction of travel, in that Ed Miliband wishes to avoid a strangehold of the markets; before the next election, there does need to have a clear narrative of public sector services. However, the £2bn reorganisation of the NHS is currently ‘work in process’, and therefore it is difficult to pre-empt how best to respond, when not all of the key statutory instruments, such as the Regulations for section 75 Health and Social Care Act, have not been “laid” before parliament. Both Ed Miliband and Andy Burnham have provided that they cannot possibly do another “top-down reorganisation”, but will instead ask existing structures to do different things, such as less competition and more collaboration. I think this is a practical approach to be admired. I also feel that freedom to produce policy possibilities in private is an excellent way to encourage creativity. In innovation management, it is a well known finding that many duds are produced before a golden egg is delivered; at this time, Ed Miliband is right to encourage innovation and creativity in policy making.
Last year’s Conference speech, 2012, was very well received, but Philip Collins and Neil O’Brien highlight that some issues were simply unaddressed, for example the deficit. In a sense the moment has ‘passed’ in that the public seem to have made their opinion up that the Conservatives are more trustworthy on the economy, despite the fact that Labour ran a deficit comparable to Ken Clarke and Norman Lamont prior to the global financial crisis. Instead of banging its head against a wall repeatedly, Labour may be better off on concentrating on a vision that the country can believe in, and other details will fall into place. Steve Richards’ discussion deliberately did not discuss other factors affecting the ‘mood music’, such as Nick Clegg and the Liberal Democrats, or UKIP, and it is possible that other big topics, such as the Eurozone, could affect Ed Miliband’s path of travel.
In summary, Steve Richards’ latest radio documentary is an interesting, even very entertaining, discussion of the current problems, opportunities and challenges facing Ed Miliband at the moment. I don’t have a political background by education whatsoever, but certainly a management training in marketing, innovation and leadership does make sense of various issues which Ed Miliband has to tackle. In as much as they are “facts”, the “facts” are currently that no party has ever been successful at increasing its share of the vote after winning an election, and one-term oppositions are vanishingly rare. However, how the current Coalition came to power is indeed unusual, as is how Ed Miliband became Leader of the Labour Party ‘against the odds’. Ed Miliband’s progress in many ways thus far has been unusual, and I suspect, as before, many things will simply fall into place for him. I really enjoyed this documentary.
I will be supporting the BPP Student Engagement team for the BPP Innovation Award
The BPP Students Association is quite new, but is growing very fast, and has the following aims:
- An independent voice for BPP UC students and to work closely with the institution to put students at the heart of everything BPP UC does;
- Information, support and guidance to students about their academic and personal life during their programme of study;
- Academic, cultural, social and professional enrichment through the development of clubs/societies/events/initiatives;
- Awareness and enhancement of students’ employability.
I will be supporting the BPP Student Engagement team for the BPP Innovation Award, not least because Olivia, Clare and Laila have always been extremely kind, helpful and thoughtful to me, as I go about my business with my BPP Legal Awareness Society, but because innovation matters hugely to me. Dr Vidal Kumar taught me innovation as a special elective over several autumnal months in the building next to the Gherkin, at BPP Business School. As it happens, I came top in the year in it with 72% (the pass mark was 50%). I remember the task well – it was all about network theory of innovation, a hugely explosive formulation of how innovation works. Innovation is a really important topic in business management. BPP Business School will be formally conferring my MBA degree on Wednesday 21 February 2012, and I was the first in my cohort to pass the entire exam at one go earlier this year.
The student engagement team behind the nominated best innovation comprises Olivia (based in London), Clare (based in Manchester) and Laila (based in London) but, each, in fact, travel all over to meet with BPP students, organising student societies and empowering students through the “Student Voice” process to contribute to the development of BPP. They are always at the end-of-the-phone, or contactable by email.
You can easily search for the BPP students collaboration through the internet:
They have designed their own website which features short videos from centres, created by students as a guide to each of BPP’s centres. You can find it here. This video provides a general overview, however.
Their unique BPP Students interactive website, representing the BPP Students Association, provides information about clubs and societies in general, discounts from local and national businesses (including those discovered by students on a weekly basis), there are student association’s organised social events (including fairs, balls, nights-out), and help with finding accommodation guides (including rooms, hotels, and halls, and fairs where you can meet people face-to-face). You can run for various rôles in “Student Voice”, where you can run for any number of positions of responsibility, or even write for one of two publications “Business Brief” and “Legal Incite”. Their Facebook page currently has over 1000 likes.
The whole point about an innovation is that it is more than an invention – the interaction with the adopter is what makes it unique. The adopter in this case is a BPP student, and the innovation has to be simple, accessible and useable enough to allow ready ‘diffusion’ to the end user. The whole success of an innovation depends upon its uptake.
Here you can see their uptake has been very successful:
That was from a Leeds student. This is from a Birmingham student.
This is from a Swindon student.
And finally, from where I started off, a BPP Business Student:
Furthermore, in this case, the success of the innovation is that it is all about building a collaborative network where the whole is greater than the sum of the individual parts. Through meaningful interaction between members of the network (and interestingly there is no hierarchy which can scupper such communications within (infra) a large organisation), links can be made between diverse areas of the network (e.g. a direct communication between a student, lecturer and professor) which would be hard to achieve otherwise. Building up such networks is a powerful way for any organisation to live in a dynamic way, and the organisation can take on a vibrant culture and learning of its own. In this way, students can directly contribute to their courses which they’re studying, and genuinely feel a part of it. I am a huge believer in inclusivity and accessibility, so this for me is very important. And finally – it is genuinely disruptive. In my day (I was a student at Cambridge in the 1990s originally where I did my undergraduate, Masters and graduate degree), we had cumbersome committees, with lots of pen-pushing, but where you didn’t get much done. I’m sure those still exist, with people taking minutes, etc., but this is a much more innovative way of doing things. The Government wished higher educational facilities to put students “at the heart of the system” in their White Paper published last year, and this for me is a perfect way for BPP to demonstrate innovative excellence in doing so.