Home » Posts tagged 'Health and Social Care Act'
Tag Archives: Health and Social Care Act
We didn’t vote for the Health and Social Care Act, so why should we believe Russell Brand?
Take two people called Russell and Jeremy in a hôtel room in London, and ask one of them to put the world to rights.
Fringe meetings for Labour Party conferences for as long as I can remember have run panel discussions about how we can engage more people in the political process. For virtually of these fringe meetings which I have attended, almost invariably is the fact that political parties introduce policies for which people didn’t vote almost every parliament.
These issues remain dormant on the mainstream media for months on end, and yet continue to enrage people in the social media. Many issues under the umbrella of social justice continue to cause anger and resentment: these include the closure of English law centres, or the NHS reforms. The media continues to be skewed against such issues. For example, the flagship programme on BBC1 every Thursday, “Question Time”, regularly features a candidate from UKIP, a party which as yet has failed to elect a single MP. They have never featured a candidate from the National Health Action Party, and yet the running of the NHS continues to be a totemic issue.
Blaming the media would be like a bad tap-dancer wishing to blame the floor. And yet protest votes are not easily dismissed. Recently, in France, the right-wing National Front has taken the lead in an opinion poll before elections for the European Parliament, in a development that has truly shocked the French political establishment. The survey, which gave Marine Le Pen’s party 24 per cent of the vote, marked the first time that the party founded in 1972 by her father has led before a national election. The centre-right Union for a Popular Movement, which led in the previous equivalent poll, stood at 22 per cent and the Socialists at 19 per cent.
Part of David Cameron’s problem is that the initial friendship towards his Conservative Party was lukewarm to begin with. The intervening years (2010-2013) have seen a Party which just appears ‘out of touch’, which makes Sir Alec Douglas-Home look trendier than a hip-hop artist. But likewise, Russell Brand is not a ubiquitously popular man himself. Whilst some people feel he stands up for their views, irrespective of his reported wealth, others find him narcissistic and nauseating.
Russell Brand is however successful at being famous, and this is a peculiar British trait. He often begins his set by talking about his love for fame: ‘My personality doesn’t work without fame. Without fame, this haircut is just mental illness.’ He has found his way of getting his name in the news, and in the tabloids. His comedy is not even that popular, but at least he has the ear of the British media. The National Health Action Party would have loved ten minutes with Jeremy Paxman, although it’s quite unlikely a ten-minute video with Clive Peedell would become an instantaneous viral hit.
Meanwhile, in a parallel universe, the UK Labour Party almost seems to have re-discovered its mojo. The triangulation of the past appealed to those in Labour who felt they could win simply by appealing to floating Tory voters. But it is a strategy that ran out of steam in 2010, leaving abandoned Blairite commentators to become embittered and self-consumed in a passion of self-destruction, while spitting bullets at Ed Miliband. Labour’s traditional supporters did not come out and vote, while floating voters saw through the cynical vote-grabbing exercises. Labour did not appear particularly ‘socialist’ any more.
Russell Brand didn’t mention the deficit once. Russell Brand did not have to appeal to his fans to say that there will be no return to the days of lavish spending. He did not have to say that he had learnt lessons from the past.
And yet deep-down voters do have excuses, if not reasons, not to vote Labour. There are some people who believe that Ed Miliband will need to identify Labour’s mistakes – the blind eye to a City running wild; an over-reliance on both high finance and a house-price bubble; or being ‘weak on welfare’.
And yet we are in a society which is absurdly superficial. Should Russell Brand have to bite the bullet for riding the crest of this banality? This strange Universe is not just occupied by reality TB stars. Many famous people are famous for being famous. Nicole Kidman is famous for being famous. Arguably, Nicole Kidman famous for divorcing Tom Cruise. At the same time when Russell Brand was selling what he sells best, that is Russell Brand, Cher was on BBC1 on ‘The Graham Norton Show’. And nobody sane can claim that Cher is the world’s best singer.
This does not necessarily mean that Labour should ignore the polls, although Labour will invariably say it ignores the polls when they are bad. From level-pegging to an 11-point lead in 10 days, Labour has plainly had a good conference, in terms of public opinion polling. After a difficult summer, YouGov’s poll put Labour at its highest level, 42%, since June. 30% now said Ed Miliband is doing well as party leader – his best rating since May. When people were asked who would make the best prime minister, Miliband (25%) was now within three points of David Cameron (28%). That was the narrowest gap since Miliband became party leader three years ago.
Ed Miliband is the one who keeps on saying that he wants ‘to tell you a story’. After the recent coverage of Ralph Miliband, paradoxically people appear to have warmed to the narrator as much as the story. In Russell Brand’s case, there is a curious mixture of some people liking the narrator as well as the story.
And yet for all of Russell Brand’s themes, such as global warming, inequality, or dominance of corporatism, for Brand it is simply entertainment. For many viewers, it is simply entertainment. Life is far from entertaining from some who have deeply suffering in this Government. Social injustices, such as in the personal independence payment or Bedroom Tax, have literally taken their casualties, and the myth of ‘the record number in employment’ has been blown out-of-the-water.
Russell Brand can be thanked for his form of escapism. But at the end of the day it is superficial crap, and not the solution to more than thirty years of failed triangulation in UK politics. We didn’t vote for the Health and Social Care Act, so why should we believe Russell Brand?
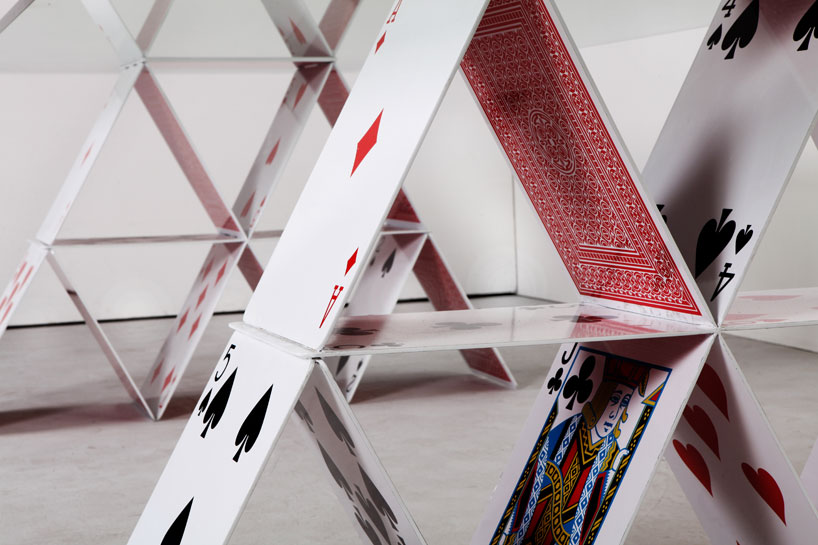
Like a faulty house of cards, the competition rationale for the Health and Social Care has fallen apart
In the beginning….
In the beginning, there was garbage and rhetoric. It sounded nice, but it was intellectually devoid of quality, there was not much competition for ideas even though this WAS bad, and so there was not much choice.
Julian LeGrand back in 2003 talks of the “competition juggernaut”:
Labour has made many mistakes, usually and unsurprisingly given its roots in socialism and central planning, in the direction of too heavy-handed central control. The public service juggernauts are now on a different course, with decentralisation, competition and choice as part of their route maps – and with plenty of resources as fuel. If they fail to arrive at their destination, if our expectations are dashed, there will be real questions over the future of each area of public services: how long can it remain public; how long can it remain a service?
‘Competition fever‘ should have never have got off the ground. The University of York, Economics of Social Care and Health Unit, and Centre for Health Economics once published a study of ‘Hospital competition under fixed prices’ (research paper 80).
The argument that competition improves quality fell apart because of the sheer volume of invalid assumptions, as demonstrated in the following quotation from that document:
The review of the theoretical literature suggests that the plausible argument that greater competition amongst providers facing fixed prices will lead to higher quality rests on strong assumptions which may not hold. The literature shows that more competition increases quality when providers are profit maximisers and marginal cost of treatment is constant. Competition has an ambiguous or negative effect on quality when providers are altruistic, the marginal cost of treatment is increasing and quality is only imperfectly observable. The literature has been largely silent on the relationship between market size, as measured by total population or population density, and quality.
Competition as the failed central plank of the Health and Social Care Act (2012)
The raison d’être of the Health and Social Care Act (2012) is nothing to do with improving clinical care, though that could be a consequence of its three main areas. There is nothing about how patient staffing can be addressed, related to the equally potent issue of patient safety. It has never been entirely clear how the Act came about, but the three planks of policy are laid bare by the impact assessments from the Department of Health (2011) (published here on 19 January 2011). The three main planks of the Bill are firstly to establish the competitive market as the substrate for the National Health Service, to define better the insolvency régime (it is important to clarify how economic entities as autonomous units can be allowed to fail ‘to get them out of the system’), and the machinery needed to regulate the market. I will come to how Monitor has had to come into being to ‘regulate the internal market’, but it is not insignificant that introducing the market is itself a source of waste and inefficiency (such as duplicated transaction costs). Of course, the issue of how to regulate the internal market should be regulated has often been analysed in a substandard manner before by some social scientists, not competition lawyers, but this is now an important policy issue which has been thrust into the limelight.
Central to this argument is that competition promotes innovation. This is indeed cited on page 41 of the “Impact assessment”.
Ahn (2002) reviews a large number of studies on the link between competition and innovation and concludes that competition encourages innovative activities and has a significant impact on long-term productivity growth:
“Competition has pervasive and long lasting effects on economic performance by affecting economic actors’ incentive structure, by encouraging their innovative activities, and by selecting more efficient ones from less efficient ones over time”.
The myth that competition drives innovation, when COLLABORATION does
However, there is an intrinsic problem in business management: the assumption that competition drives innovation. This bit of missing evidence in the impact assessments totally distorts the raison d’être of the Act itself, and of course there is a separate debate in management as to whether innovation can be detrimental to organisational culture or learning. There is considerable evidence now that collaboration, not competition, can be essential for innovation. This theme is taken up in an interesting article about ‘internal markets’ from Forbes:
Major innovation needs collaboration, not competition. For innovation, internal markets have the same problem as hierarchical bureaucracies. Managers vote their resources for innovations that bolster their current fiefdoms and careers. The safest strategy is to stick to the status quo. Ms. Kimes’ article gives multiple examples where competing managers at Sears looked after their own units at the expense of the interests of the firm as a whole.
Second, innovation isn’t basically an issue of spending. Booz & Company’s annual innovation reports repeatedly state: “Spending more on R&D won’t drive results. The most crucial factors are strategic alignment and a culture that supports innovation.”
Finally, the hope of the internal markets theory is that, by funding a variety of different ideas, the organization will emulate the evolutionary process of natural selection and so the best ideas will survive and prosper. The problem is that once a disruptive idea starts to flourish and becomes more interesting than the normal bread-and-butter work of the organization, it risks becoming a threat to the rest of the organization.
The wheels are coming off the Competition Juggernaut a bit sooner than expected
David Williams at the Health Services Journal only very recently on 16 September 2013 reported that:
NHS England has delayed the publication of its choice and competition framework amid a “paucity of evidence” of the benefit to patients.
Policy director Bill McCarthy made the announcement at a board meeting on Friday, highlighting the issue as a new risk for the central body.
The framework and supporting documents were originally slated for publication in July.
Mr McCarthy said: “We’re having [a discussion] with Monitor around choice and competition, and how best they can be applied in healthcare to improve outcomes for patients, including a better experience.
“That’s taken a bit longer than we hoped.
“We had hoped to be able to put out some guidance early in the summer – I think that probably reflects… it is one of the areas where there is a paucity of evidence.”
“Operation Propper”
Clause “B47” (p.42/3) in the official Impact Assessments from the Department of Health cites one of the key planks of evidence that the Department of Health wishes to use in promoting its competition argument.
“A July 2010 study by health economists Martin Gaynor, Rodrigo Moreno-Serra, and Carol Propper investigated outcomes in the NHS following the introduction of choice in 2006. They conclude as follows: “We find that the effect of competition is to save lives without raising costs. Patients discharged from hospitals located in markets where competition was more feasible were less likely to die, had shorter length of stay and were treated at the same cost”. The study found that there was a larger inflow of patients to better quality hospitals after the 2006 NHS reforms, suggesting that popular providers in health care are able to expand supply.”
There is an even worse justification for the competition dogma later in the Department of Health’s official impact assessments:
B48. A January 2010 study by the London School of Economics also looked at NHS data post- introduction of choice in 2006. The key conclusion is as follows: “Using AMI mortality as a quality indicator, we find that mortality fell more quickly (i.e. quality improved) for patients living in more competitive markets after the introduction of hospital competition in January 2006. Our results suggest that hospital competition in markets with fixed prices can lead to improvements in clinical quality”.
B49. Evidence from the LSE shows that management quality – measured using a new survey tool – is strongly correlated with financial and clinical outcomes such as survival rates from emergency heart attack admissions (AMI). Moreover, the study finds that higher competition (as indicated by a greater number of neighbouring hospitals) is positively correlated with increased management quality.
The general issue received a scathing response from Allyson Pollock, Alison Macfarlane and Ian Greener who could not have put it any clearer.
The major improvements in outcome after acute myocardial infarction can be attributed to improvements in primary prevention in general practice and in hospital care, including the introduction of percutaneous IV angiography. The government’s own cardiac Tzar, Sir Roger Boyle, was sufficiently angered by their claims to respond with withering criticism: “AMI is a medical emergency: patients can’t choose where to have their heart attack or where to be treated!” It is “bizarre to choose a condition where choice by consumer can have virtually no effect”. Patients suffering “severe pain in emergencies clouded by strong analgesia don’t make choices. It’s the ambulance driver who follows the protocol and drives to the nearest heart attack centre”.
The intervention that the authors claimed reduced heart attacks and was a proxy for competition was patient choice. In 2006, patients were given choices of hospitals including private for-profit providers for some selected treatments. Less than the half patients surveyed in 2008 even remember being given a choice, and only a tiny proportion made those choices based on data from the NHS choices website. If patient choice was one of the two key elements of competition, it wasn’t prevalent and rather than being derived from the authors’ data, it was assumed.
Crucially, even if patient choice had occurred it does not explain why heart attack mortality rates fell. There is no biological mechanism to explain why having a choice of providers for elective hip and knee operations surgery (including hospitals which did not treat or admit acute MI patients) could affect the overall outcomes from acute myocardial infarction where patients do not exercise choice over where they are treated.
The problem of data dredging is well known; if you repeat an analysis often enough significant statistical associations will appear. But the authors make the cardinal error of not understanding their data and of confusing minor statistical associations with causation. Deaths from acute MI are not a measure of quality of hospital care, rather a measure of access to and quality of cardiology care. At best, what the paper appears to show is not the effect of choice on heart attacks but that if an individual has a heart attack in an area close to a hospital and their GP is near the hospital, then outcomes are better, but such findings are not new.
Going for their central criticism, in the same article, they explained:
The drip feed of pro-competition studies from Zack Cooper at LSE raises serious questions for the academic community and the public about what constitutes bad science and what to do about its politicisation. Recently, on 21 February in the columns of the FT, Cooper and colleague Julian Le Grand warded off serious scientific criticisms of the studies with an ad hominem attack, categorising those in favour of competition as empiricists and those whose work is critical of markets in health care as intuitivists. In so doing they sweep aside decades of careful economic theory and evidence which shows why markets do not work in health services and distract the reader from the facts that their work is ungrounded and far from empirical. Their repeated claims that competition in the NHS saves lives and improves quality and productivity have no scientific basis.
A litigation factory?
Of course the £3bn Health and Social Care Act (2012) which have no mechanisms of helping with clinical staffing or patient safety, in the drive for business efficiencies, have become a bonanza for private companies to which work has been outsourced, and a boon for the commercial and corporate law firms which are now nurturing them. The NHS of course has trouble in meeting the formidable legal bill against the private providers, as well as staff it has made redundant due to this top-down reorganisation.
I have long argued that the commissioning (‘competition and choice’) process through section 75 Health and Social Care Act (2012) would soon turn sour, for example in the original blogpost I did for the Socialist Health Association in January 2013 here. Crispin Dowler recently reported early tensions on 11 September 2013 in the Health Services Journal:
A number of private providers are likely to take complaints to the NHS’s new competition regulator Monitor over the next three years, the chief executive officer of Ramsay Health Care UK warned last week.
Jill Watts, whose organisation was ranked the largest private provider of NHS funded acute care in the most recent study by market analysts Laing and Buisson, said she could “almost guarantee” there would be challenges to come.
She told a Westminster Health Forum conference that the April switchover to clinical commissioning groups under the government’s health reforms had not produced uniform changes in commissioners’ attitudes to the private sector.
“In one part of the country, where we had almost adversarial relationships and they didn’t want to use us at all, they’re very keen to work with us now,” she said.
The New Labour Legacy, competition, performance and “the target culture”
Competition was intimately wound up in the target-driven agenda. NHS hospitals would have to meet targets to jump through regulatory hoops to become NHS Foundation Trusts. As long as finances stacked up, patient safety appears to have suffered in some Trusts under Labour’s watch. Whilst the evidence for competition being beneficial in the NHS market is weak, it has remained with us in policy like a bad smell. Julian LeGrand could have not put better how idiotic this policy really was.
The problem is indeed partly money – a historical legacy of underspending in all areas of public services. But, as John Hutton says, it isn’t only that. There is also a legacy of poor performance: of failing to use what resources there are effectively and efficiently. This is a lesson that six years in power have taught New Labour. The Government has tried and is trying a wide variety of techniques to lever up performance: publishing league tables on comparative performance, encouraging private sector involvement, offering independence to high fliers, stimulating competition and choice. But one of its favourite instruments has been targetry: the setting of targets with heavy penalties for failing to meet them. Many in government are convinced that this is the way to go.
Competitive tendering is no longer the solution; it is very much the problem
As part of the “Big Society”, medics and lawyers have now been offended over competitive tendering. Competitive tendering is no longer the solution; it is very much the problem.
Yesterday, it was the lawyers’ turn. The Bar Standards Board (“BSB”) yesterday extended (10 May 2013) the first registration deadline for the Quality Assurance Scheme for Advocates in the face of a threatened mass boycott by barristers. The Solicitors Regulation Authority is expected to follow. In a statement yesterday, the BSB said the deadline will be extended from 10 January to 9 March 2014 ‘to ensure the criminal bar will have more time to consider the consequences of government changes to legal aid before registering’. The end of the first registration period will now be after the Ministry of Justice publishes its final response to its consultation on price-competitive tendering. The SRA board is expected to approve a similar extension later shortly.
A group of leading academics, including Prof. Richard Moorhead from University College London, indeed wrote yesterday,
“As academics engaged for many years in criminal justice research, we write to express our grave concern about the potentially devastating and irreversible consequences if the government’s plans to cut criminal legal aid and introduce a system of tendering based on price are introduced. Despite the claim by Chris Grayling, the minister of justice, that ‘access to justice should not be determined by your ability to pay’, this is precisely what these planned changes will achieve. This is not about ‘fat cat lawyers’ or the tiny minority of cases that attract very high fees. As we know from the experiences of people like Christopher Jefferies, anyone can find themself arrested for the most serious of crimes. No one is immune from the prospect of arrest and prosecution.”
Previously, it had been the medics’ turn. That did not deter Earl Howe in collaboration with people who clearly did not understand the legislation like Shirley Williams in competition with the medical Royal Colleges, Labour Peers and BMA. The Royal College of Physicians set out their oppositions to competitive tendering articulated their position last month:
Competitive tendering is often considered to promote competition, provide transparency and give all suppliers the opportunity to win business. It may be that price tags are driven down, but most reasonable professionals would actually ask, “At what cost?” Competitive tendering, rather, has a number of well known criticisms.
When making significant purchases, frank and open communication between potential supplier and customer is crucial. Competitive tendering is not conducive to open communication; in fact, it often discourages deep dialogue because in many cases all discussions between a bidder and the purchaser must be made available to all other bidders. Hence, Bidder A may avoid asking certain questions because the questions or answers may help other bidders by revealing Bidder A’s approaches, features, and the like. At the moment, there is a policy drive away from competition towards collaboration, innovation and ‘creating shared value’. Dr. Deming also writing in Out of the Crisis, “There is a bear-trap in the purchase of goods and services on the basis of price tag that people don’t talk about. To run the game of cost plus in industry a supplier offers a bid so low that he is almost sure to get the business. He gets it. The customer discovers that an engineering change is vital. The supplier is extremely obliging, but discovers that this change will double the cost of the items……the vendor comes out ahead.” This is called the cost-plus phenomenon.
Competitive tendering furthermore encourages the use of cheaper resources for delivering products and services. A supplier forced to play the competitive tendering game may come under pressure to keep costs down to ensure he gets a satisfactory profit margin. One way a supplier can lower costs is by using cheaper labour and/or materials. If the cheaper labour and materials are poor quality, the procurer will often end up with inferior, poor quality product or service. However, warranty and other claims may result –raising the price of the true, overall cost. Another area where suppliers may be tempted to lower costs is safety standards. This current administration is particularly keen on outsourcing, and sub-contractors may cut corners and creating safety risks. This is obviously on great concern where patient safety in the NHS has recently been criticised, after the Francis Inquiry over Mid Staffs NHS Foundation Trust. Furthermore, then government agencies, and indeed, private companies use competitive tendering it can take several years to choose a successful bidder, creating a very slow system. The result is the customer can wait incredibly long periods for product or service that may be required quickly. Finally, insufficient profit margin to allow for investment in research and development, new technology or equipment. Already, in the U.S., private “health maintenance organisations” spend as little as possible on national education and training of their workforce.
So the evidence is there. But, as the Queen’s Speech this week demonstrated on minimum alcohol pricing and cigarette packaging, this Government does not believe in evidence-based policy anyway. In the drive for efficiency, with a focus on price and cost in supply chains, the legal and medical professions have had policies imposed on them which totally ignores value. This is not only value in the product, but value in the people making the product. One only needs to refer to the (albeit extreme) example of a worker being retrieved from the rubble of that factory in Bangladesh to realise that working conditions are extremely important. This is all the more hideous since the policies behind the Legal Aid, Sentencing and Punishment of Offenders Act (2012) and the Health and Social Care Act (2012) were not in any of the party manifestos (sic) of the U.K. in 2010.
Competitive tendering is no longer the solution; it is very much the problem.
Competitive tendering is no longer the solution; it is very much the problem.
As part of the “Big Society”, medics and lawyers have now been offended over competitive tendering. Competitive tendering is no longer the solution; it is very much the problem.
Yesterday, it was the lawyers’ turn. The Bar Standards Board (“BSB”) yesterday extended (10 May 2013) the first registration deadline for the Quality Assurance Scheme for Advocates in the face of a threatened mass boycott by barristers. The Solicitors Regulation Authority is expected to follow. In a statement yesterday, the BSB said the deadline will be extended from 10 January to 9 March 2014 ‘to ensure the criminal bar will have more time to consider the consequences of government changes to legal aid before registering’. The end of the first registration period will now be after the Ministry of Justice publishes its final response to its consultation on price-competitive tendering. The SRA board is expected to approve a similar extension shortly.
A group of leading academics, including Prof. Richard Moorhead from University College London, indeed wrote yesterday,
“As academics engaged for many years in criminal justice research, we write to express our grave concern about the potentially devastating and irreversible consequences if the government’s plans to cut criminal legal aid and introduce a system of tendering based on price are introduced. Despite the claim by Chris Grayling, the minister of justice, that ‘access to justice should not be determined by your ability to pay’, this is precisely what these planned changes will achieve. This is not about ‘fat cat lawyers’ or the tiny minority of cases that attract very high fees. As we know from the experiences of people like Christopher Jefferies, anyone can find themself arrested for the most serious of crimes. No one is immune from the prospect of arrest and prosecution.”
Previously, it had been the medics’ turn. That did not deter Earl Howe in collaboration with people who clearly did not understand the legislation like Shirley Williams in competition with the medical Royal Colleges, Labour Peers and BMA. The Royal College of Physicians set out their oppositions to competitive tendering articulated their position last month:
Competitive tendering is often considered to promote competition, provide transparency and give all suppliers the opportunity to win business. It may be that price tags are driven down, but most reasonable professionals would actually ask, “At what cost?” Competitive tendering, rather, has a number of well known criticisms.
When making significant purchases, frank and open communication between potential supplier and customer is crucial. Competitive tendering is not conducive to open communication; in fact, it often discourages deep dialogue because in many cases all discussions between a bidder and the purchaser must be made available to all other bidders. Hence, Bidder A may avoid asking certain questions because the questions or answers may help other bidders by revealing Bidder A’s approaches, features, and the like. At the moment, there is a policy drive away from competition towards collaboration, innovation and ‘creating shared value’. Dr. Deming also writing in Out of the Crisis, “There is a bear-trap in the purchase of goods and services on the basis of price tag that people don’t talk about. To run the game of cost plus in industry a supplier offers a bid so low that he is almost sure to get the business. He gets it. The customer discovers that an engineering change is vital. The supplier is extremely obliging, but discovers that this change will double the cost of the items……the vendor comes out ahead.” This is called the cost-plus phenomenon.
Competitive tendering furthermore encourages the use of cheaper resources for delivering products and services. A supplier forced to play the competitive tendering game may come under pressure to keep costs down to ensure he gets a satisfactory profit margin. One way a supplier can lower costs is by using cheaper labour and/or materials. If the cheaper labour and materials are poor quality, the procurer will often end up with inferior, poor quality product or service. However, warranty and other claims may result –raising the price of the true, overall cost. Another area where suppliers may be tempted to lower costs is safety standards. This current administration is particularly keen on outsourcing, and sub-contractors may cut corners and creating safety risks. This is obviously on great concern where patient safety in the NHS has recently been criticised, after the Francis Inquiry over Mid Staffs NHS Foundation Trust. Furthermore, then government agencies, and indeed, private companies use competitive tendering it can take several years to choose a successful bidder, creating a very slow system. The result is the customer can wait incredibly long periods for product or service that may be required quickly. Finally, insufficient profit margin to allow for investment in research and development, new technology or equipment. Already, in the U.S., private “health maintenance organisations” spend as little as possible on national education and training of their workforce.
So the evidence is there. But, as the Queen’s Speech this week demonstrated on minimum alcohol pricing and cigarette packaging, this Government does not believe in evidence-based policy anyway. In the drive for efficiency, with a focus on price and cost in supply chains, the legal and medical professions have had policies imposed on them which totally ignores value. This is not only value in the product, but value in the people making the product. One only needs to refer to the (albeit extreme) example of a worker being retrieved from the rubble of that factory in Bangladesh to realise that working conditions are extremely important. This is all the more hideous since the policies behind the Legal Aid, Sentencing and Punishment of Offenders Act (2012) and the Health and Social Care Act (2012) were not in any of the party manifestos (sic) of the U.K. in 2010.
Competitive tendering is no longer the solution; it is very much the problem.
How is parliamentary procedure being followed to take the previous statutory instrument on NHS procurement out-of-action?
A Statutory Instrument is used when an Act of Parliament passed after 1947 confers a power to make, confirm or approve delegated legislation on: the Queen and states that it is to be exercisable by Order in Council; or a Minister of the Crown and states that it is to be exercisable by Statutory Instrument. 1.15 pm last Tuesday (5 March 2013) saw Andy Burnham MP, the Shadow Secretary of State for Health, go head-to-head with Norman Lamb (The Minister of State, Department of Health). Lamb was invited to comment on the regulations on procurement, patient choice and competition under section 75 of the Health and Social Care Act 2012.
The discussion is reported in Hansard.
Lamb describes an intention to ‘amend’ the legislation
Lamb explains:
“Concerns have been raised that Monitor would use the regulations to force commissioners to tender competitively. However, I recognise that the wording of the regulations has created uncertainty, so we will amend them to put this beyond doubt.”
The problem is that this statutory instrument would have become law automatically on 1 April 2013, and still promises to do so in the absence of anything else happening. The safest way to get this statutory instrument out-of-action is to ‘annul’ the law, rather than having the statutory instrument still in force but awaiting amendment. Experts are uncertain the extent to which statutory instruments can be so easily amended, while in force.
Most Statutory Instruments (SIs) are subject to one of two forms of control by Parliament, depending on what is specified in the parent Act.
Fatal motion
There is a constitutional convention that the House of Lords does not vote against delegated legislation. However, Andy Burnham has said the exceptional nature of the Section 75 regulations, which force all NHS services out to tender, meant he needed to table a ‘fatal’ motion in the second Chamber. Indeed, Lord Hunt later tweeted that this fatal chamber had forced a rethink on the original Regulations:
The main effect of delegated legislation being made by Statutory Instrument is that it is effective as soon as it is made, numbered, catalogued, printed, made available for sale, and published on the internet. This ensures that the public has easy access to the new laws. This statutory instrument (SI 2013/057:The National Health Service (Procurement, Patient Choice and Competition) Regulations 2013) is still available in its original form, with no declaration of its imminent amendment or annulment, on the official legislation website here.
The “Prayer”
The more common form of control is the ‘negative resolution procedure’. This requires that either the Instrument is laid before Parliament in draft, and can be made once 40 days (excluding any time during which Parliament is dissolved or prorogued, or during which both Houses are adjourned for more than four days) have passed unless either House passes a resolution disapproving it, or the Instrument is laid before Parliament after it is made (but before it comes into force), but will be revoked if either House passes a resolution annulling it within 40 days.
A motion to annul a Statutory Instrument is known as a ‘prayer’ and uses the following wording:
- That an humble address be presented to Her Majesty praying that the [name of Statutory Instrument] be annulled.
Any member of either House can put down a motion that an Instrument should be annulled, although in the Commons unless the motion is signed by a large number of Members, or is moved by the official Opposition, it is unlikely to be debated, and in the Lords they are seldom actually voted upon.
Indeed, this is exactly what happened. Ed Miliband submitted EDM 1104 on 26 February 2013, which currently – at the time of writing – has 183 signatures – with the exact wording:
“That an humble Address be presented to Her Majesty, praying that the National Health Service (Procurement, Patient Choice and Competition) Regulations 2013 (S.I., 2013, No. 257), dated 11 February 2013, a copy of which was laid before this House on 13 February, be annulled.”
The purpose of “amending” the legislation
Lamb later provides in his answer:
“Concerns have also been raised that competition would be allowed to trump integration and co-operation. The Future Forum recognised that competition and integration are not mutually exclusive. Competition, as the Government made clear during the passage of the Bill, can only be a means to improve services for patients—not an end in itself. What is important is what is in patients’ best interests. Where there is co-operation and integration, there would be nothing in the regulations to prevent this. Integration is a key tool that commissioners are under a duty to use to improve services for patients. We will amend the regulations to make that point absolutely clear.”
How the Government “amends” the legislation is clearly pivotal here. Integration is another “buzzword” in the privatisation ammunition. Colin Leys wrote in 2011:
“In the emerging vision of the Department of Health, however, integrated care has always been associated with the drive to enlarge private sector provision, and the Kaiser [Permanente] connection emphasised this. The competitive culture attached to integrated care in the Kaiser model, coupled with the keen interest of private providers in all integrated care initiatives, were constants, and put their stamp on official thinking about the future NHS market.”
A possible reason for why this emphasis on competition has failed is that in other markets, such as utilities, rail and telecoms, there is a strong case that competition has not driven down cost at all, because of shareholder dividend primacy. Another good reason for people in favour of the private market to discourage competition is that competition might even inhibit a drive to integration, and integration is strongly promoted by private providers (and, incidentally, New Labour).
What does the Act itself say about ‘annulling’ statutory instruments?
According to s. 304(3), “Subject to subsections (4) to (6), a statutory instrument containing regulations under this Act, or an order by the Secretary of State or the Privy Council under this Act, is subject to annulment in pursuance of a resolution of either House of Parliament.” So, at the moment, we are clearly in limbo, with parliament yet to pass a EDM, and new redrafted Regulations yet to appear. However, it is still a very dangerous situation, as the original set of Regulations is still yet to be enacted on 1 April 2013.
Why David Cameron's "lurch to the right" must not be above the law
Like John Hirst, the former prisoner who studied law and put the UK on-the-spot about the proportionality of imposing a total ban on prisoners using the vote, David Cameron is not above the law. In a question on fox hunting once in Prime Minister’s Questions, Cameron voluntarily offered the information that he had not done anything unlawful; this was a stupid strategic error, as nobody had accused him of having done anything unlawful. The ‘rule of law’ holds the supremacy of the law, everyone is equal in front of the law, and nobody is above the law.
David Cameron does make the law however for the time-being. He can effectively do what he wants: hence the famous aphorism of parliamentary supremacy of Sir Leslie Stephen ((1832–1904), “If a legislature decided that all blue-eyed babies should be murdered, the preservation of blue-eyed babies would be illegal; but legislators must go mad before they could pass such a law, and subjects be idiotic before they could submit to it.” [The Science of Ethics, p. 145 (1882).]
Eastleigh was a tragedy for Cameron. Having set things up nicely on how his party would offer a referendum on Europe in 2015, which kept the Tory Euroskeptics happy for the time-being, the UKIP backlash was fully active last Thursday. Whilst UKIP does not have a single MP yet, they still threaten the Conservatives with the power to deny them an overall majority. And yet, David Cameron knows that he cannot unilaterally have special terms for the UK’s membership of Europe. Sure, directives can be applied by our Government according to parliament’s wishes, but if he wants anything more he will have to leave Europe. He is not above the law, but he could repeal the European Communities Act (though it would be difficult for him to do so). Even if David Cameron decides that he wishes to tear up the Human Rights Act, he will still have to submit human rights allegations to Strasbourg unless he decides not to become a signatory to the European Convention of Human Rights. Louise Mensch has described that the Human Rights Act itself is faulty, whereas most learned experts feel that the implementation of its analysis could be improved, and we are better off doing the proverbial in the tent than outside it. Leaving the European Convention of Human Rights denies us any moral authority on commenting on the human rights of other jurisdictions, and sets out a very dangerous signal in terms of reputation on our attitude towards inalienable human rights as per Delhi for example.
The more insightful conclusion is that David Cameron is desperate. He was initially tolerated as Prime Minister, but generally even this has deteriorated to being positively loathed by people within his party and outside of it. His Coalition, for example, has legislated for the Health and Social Care Act, which contains one clause section 259(10), which in conjunction with the Data Protection Act and Human Rights Act, is an area where the European Court of Human Rights could easily find the approach of GPs to data confidentiality unlawful; this could be determined one day in a test case similar to S and Marper v UK. It is helpful indeed that lawyers are able to act on poor legislation, as indeed they recently had to do with Iain Duncan-Smith’s mandatory work placement schemes (in the case of Cait Reilly). However, it is the democratic deficit, that laws appear to come from nowhere (and certainly not contained in any party manifesti at the time of the 2010 general election), which is most worrying. It is not so much a case of this Coalition ‘running out of things to do'; it is rather a case of this Coalition ‘running out of things to destroy’.
Unpacking the legacy of this Coalition is going to be extremely painful. George Osborne’s “badge of honour”, the triple A rating, was humiliatingly stripped off the Government, as Moody’s caste judgement on their deficit reduction plan. Construction performance hit a 41 month low this morning. Anyone with the most rudimentary understanding of economics will appreciate that the Coalition terminating ‘Building Schools for the Future’, and other key infrastructure projects, put the brakes on the economy which had been recovering in May 2010. Add to this an increase in 2.5% in the VAT rate, encouraged by corporate CEOs writing letters to the Times, and murder of consumer spending, and you can easily understand how corporate interests saw the UK’s economy being sent down the river. But it’s ok because we don’t have a functional BBC. The BBC, which is not covered by the Freedom of Information Act, is not obliged to explain its ‘creative authority’ for why its journalists never explain why the deficit exploded in 2009 due to a £1 tn recapitalisation of the banks. It does not need to explain either on the basis of its creative licence either why it barely mentioned the activities of the NHA Party in Eastleigh, or why the criticisms of the 2012 Health and Social Care Act (and the concomitant statutory instrument 2012/057) evade scrutiny. However, the reality is that the UK has been trashed like a Bullingdon restaurant party; whether this is the scrapping of the education support allowance, the implementation of tuition fees, the shutting of libraries, the poor regulation which allows ‘value’ horsemeat to be fed in school dinners, the privatisation of the NHS, the triple dip recession, rioting in the streets, or otherwise, the UK at the moment is a disgrace compared to what it could and should be. David Cameron’s “lurch to the right” will not get round that – his only way to get above the law is to rewrite it fast. The other way to get above the law is to annihilate access-to-justice, and by stopping access to the European Court of Human Rights, or any high street mechanism of achieving justice (for example, high street law centres or citizen advice bureaux). No comment.
My blogposts on Section 75 Health and Social Care Act and NHS England Procurement Regulations (SI 2013/057)
Since 7 January 2013, I have written a number of blogposts detailing the legal and policy implications of the Health and Social Care Act and the statutory instrument 2012/057.
These are on the “Legal Aware” blog.
Main article:
SI 2012/057:
The legal issues in the statutory instrument (2013, No. 257) on NHS procurement in England
Possible letter to send to the Clerk of the Committee
VERY IMPORTANT. Tomorrow is the last day to the write to the Clerk about SI 257
Lord Owen’s Bill:
History:
This one on stakeholder reaction is published on the ‘Socialist Health Association’ (independently authored) blog:
Rainbow coalition warns about section 75 NHS Regulations
Possible letter to send to the Clerk of the Committee
To: seclegscrutiny@parliament.uk
The Lords Secondary Legislation Scrutiny Committee
Dear Sir,
Secondary legislation under Section 75 of the Health and Social Care Act 2012
I notice that the Lords’ Secondary Legislation Scrutiny Committee will be discussing the regulations laid by the Government under Section 75 of the new NHS Act 1 at their meeting on 5 March.
I write to request that the Committee send these regulations for reconsideration. The reason is that there is a significant disjunction between the public statements of ministers and the content of the regulations.
Ministers said:
- Andrew Lansley MP: “There is absolutely nothing in the Bill that promotes or permits the transfer of NHS activities to the private sector.” (13/3/12, Hansard )
- Andrew Lansley MP, 12.02.12, letter to Clinical Commissioning Groups: “I know many of you have read that you will be forced to fragment services, or put them out to tender. This is absolutely not the case. It is a fundamental principle of the Bill that you as commissioners, not the Secretary of State and not regulators – should decide when and how competition should be used to serve your patients interests..”
- Simon Burns MP: “…it will be for commissioners to decide which services to tender…to avoid any doubt—it is not the Government’s intention that under clause 67 [now section 75] that regulations would impose compulsory competitive tendering requirements on commissioners, or for Monitor to have powers to impose such requirements.” (12/7/11, Hansard, c442 )
- Lord Howe: “Clinicians will be free to commission services in the way they consider best. We intend to make it clear that commissioners will have a full range of options and that they will be under no legal obligation to create new markets….” (6/3/12, Hansard )
- Nick Clegg: “That’s why I have been absolutely clear: there will be no privatisation of the NHS. The NHS has always benefited from a mix of providers, from the private sector, charities and social enterprises, and that should continue… It’s not the same as turning this treasured public service into a competition-driven, dog-eat-dog market where the NHS is flogged off to the highest bidder.” 26/5/11
The regulations
The regulations break these promises by creating requirements for virtually all commissioning done by the National Commissioning Board (NCB) and Clinical Commissioning Groups (CCGs) to be carried out through competitive markets regardless of the will of local people. They contain legal powers for Monitor to enforce the privatisation spontaneously or at the request of private companies which lost bids.
They would also make it impossible to fulfil some of the key thrust of the Francis report recommendations.
According to David Lock QC, the regulations as a whole have the effect of closing down the current option of an in-house commissioning process, even if local people wish it. This option has been taken in a number of cases, including since the passage of the Act . Ministers have confirmed that at the present time such arrangements are legal and would not give rise to challenge under EU Procurement law .
Regulation 5 – awarding a contract without competition can, effectively, only be done in an ‘emergency’, a much narrower restriction than suggested in the parliamentary debate.
Regulation 10 makes whatever Monitor judges to be an “unnecessary” restriction of competition, illegal. It thus effectively closes down the current option of one state body (i.e. the NHS Commissioning Board or a Clinical Commissioning Group) merely making a new arrangement (not contract) with another – i.e. an NHS Trust.
Regulation 12 forces commissioners to use the market to meet waiting time considerations, in contravention of assurances offered to CCGs during the passage of the Act when they were told they would have discretion and could also consider quality issues. This regulation also ignores the summary of the DH’s own consultation which highlighted that waiting time considerations should not be used to override quality considerations.
Part 3 Regulations 13-17, covering Monitor’s powers
The sweeping (and time unlimited) statutory powers given to Monitor enable it to decide when the CCG has breached regulations (Regulation 14), to end any arrangements the CCG has come to and to impose their own (Regulation 15) – including the criteria governing selection of suppliers, and more fundamentally, the decision about whether to use competitive methods like tendering and AQP at all. Under these regulations Monitor will have sweeping statutory power to enforce (as yet unseen) guidance, whereas the current guidance is not legally binding.
In summary, therefore, there is a contradiction between the intention of the Act as expressed by ministers and the consequences of the regulations.
The regulations need to be reconsidered and rewritten.
Yours faithfully,
Integrated care – there's an app for that! A hypothetical case study.
Innovation and integrated care
Andrew Neil reminded us this morning on ‘The Sunday Politics’ that there are currently around 4 million individuals who don’t have access to the internet. Prof Michael Porter, chair of strategy at the Harvard Business School, has for a long time reminded us that sectors which have competitive advantage are not necessarily those which are cutting-edge technologically, but his colleague Prof Clay Christensen, chair of innovation at the same institution, has been seminal in introducing the concept of ‘disruptive innovation’. An introduction to this area is here. The central theory of Christensen’s work is the dichotomy of sustaining and disruptive innovation. A sustaining innovation hardly results in the downfall of established companies because it improves the performance of existing products along the dimensions that mainstream customers value. Disruptive innovation, on the other hand, will often have characteristics that traditional customer segments may not want, at least initially. Such innovations will appear as cheaper, simpler and even with inferior quality if compared to existing products, but some marginal or new segment will value it.
A consortium, led by Frontier Economics, and including The King’s Fund, The Nuffield Trust and Ernst & Young, was appointed by Monitor to consider issues relating to the delivery of integrated care. Their report is here. Under the Health and Social Care Act Monitor has a duty to “enable” integrated healthcare and integrated health and social care. “Integrated care” is a concept that has been defined in many different ways. A recent review of the literature on integrated care by Armitage et al. (2009) revealed some 175 definitions and concepts. There is now a clear consensus that successful integrated care is primarily about patient experience, although all dimensions of quality and cost-effectiveness are relevant. A definition of integrated care that combines the experiential dimension with that of cost and quality means there are potential benefits from integrated care for current and future service users, the public, providers and commissioners. This means that a working definition of integrated care may be around the smoothness with which a patient or their representatives or carers can navigate the NHS and social care systems in order to meet their needs.
According to the International Longevity Centre – UK, the current (non-integrated) health and social care system has several failures. They include:
- Lack of ‘ownership’ for the patient and her problems, so that information gets lost as she navigates the system
- Lack of involvement by the user/patient in the management and strategy of care
- Poor communication with the user/patient as well as between health and social care providers
- Treating service users for one condition without recognising other needs or conditions, thereby undermining the overall effectiveness of treatment
- Decisions made in the social care setting affect the impact of health care treatment, and vice versa
At the heart of this new model of care is the need to better integrate services between providers around the individual needs of patients and service users. As The King’s Fund’s review of the evidence for integrated care concluded, significant benefits might potentially arise from the integration of services (Curry and Ham 2010), particularly when these are targeted at those client groups for whom care is currently poorly co-ordinated. In the NHS, integrated care could be particularly important in meeting the needs of people with chronic diseases like diabetes and chronic obstructive pulmonary disease; frail older people who may have several chronic diseases and be in contact with a range of health and social care professionals; and people using specialist services – for example, those involved in respiratory, cardiac and cancer care – where networks linking hospitals that provide these services have contributed to improved outcomes. In some cases integration may even entail bringing together responsibility for commissioning and provision. This form of integration is important because it allows clinicians to use budgets either to provide services more directly or to commission these services from others through ‘make or buy’ decisions. The critical ingredients of integrated care are considered to be: defining the right populations, aligning the right financial incentives to support a variety of diverse healthcare providers (but primarily to ensure the highest quality in patient overall experience), improved accountability for better performance in a more coherent outcome of coordinated care, judicious use of information technology and other knowledge management resources, effective leadership, a collaborative (and competitive where appropriate) culture, patient engagement, and better and more appropriate use of resources according to multi-disciplinary relevance.
In this hypothetical innovation described below, patients, members of CCGs, and healthcare providers have access to a smartphone app called “Integrated care”.
Who is the end user?
A problem with integrated care is that it is likely that the same organisational structures would still exist – albeit with key agents, such as health care provider organisations, healthcare professionals including doctors, clinical commissioning groups representatives, and so on, but a better way of looking at this innovation is where all participants are members of a continuous ‘network’ of innovation; this would help to diminish perception of there being a hierarchy in healthcare, which is a source of considerable inertia in the current English NHS. A version of the app could be available to clinical commissioning group members, or directly to the patient, and of course data are shared with healthcare providers.
The advantage about giving the app directly to the patient would be that the patient himself or herself makes a decision about the care, based on up-to-date information about cost and quality of care (it would be necessary to ensure that accurate data are submitted). The main procedural problem is deciding how much money each person has to play with in a personalised budget – would it be higher or indeed without limit for an individual with multidisciplinary needs or lives a long way from their place of treatment? Indeed, should the budgets be limitless, or should there be some form of rationing in keeping with the finite resources provided by the English economy? Notwithstanding these massive issues, this app would be more in keeping of what the general public understands by “money following the patient”.
Rationale for an app
This app could be based around diseases or conditions, such as dementia, systemic lupus erythematosus, and diabetes, which very often affect more than one bodily system, or more than discipline (for example nurses, doctors, dieticians, physiotherapists, SALT experts). The Department of Health initiated a two-year national programme of pilots to investigate the impact of providing integrated care. The national programme consisted of 16 specific initiatives, including: structured care for dementia, end-of-life care, older people at risk of admissions, long term conditions, chronic obstructive pulmonary disease, care for diabetes, and substance misuse.
The Kings Fund/Nuffield Trust Report has emphasised the potential value of an innovation-approach to this problem. They felt a need to allow innovations in integrated care time to embed locally, requiring longer planning cycles. For this innovation change to succeed, providers should be allowed to take on financial risks and innovate as approaches to integrated care often work best when some of the responsibilities for commissioning services are given to those who deliver care. They also set out a more nuanced interpretation of patient choice. Patient choice should be intrinsic to the provision of integrated care, however, it could also be a barrier to integrated care.
It would be hard to see such an app being truly automated, in that it would be inconceivable to think of an individual making a decision about integrated care without help of an appropriate expert. However, having an app supported on the cloud has its advantages. Notwithstanding the usual privacy and security issues (which exist even with online shopping with supermarkets), resources could be scaled according to the needs of the population, and the transfer of information freely across all parts of the network would be virtually instantaneous.
Barriers to integration which the app would seek to overcome:
- Quality of IT and communication system: having separate information systems with different formats for clinical documents and without a common access to service users’ information makes integrated care more difficult (i.e. inter-operability); apps are commonplace on a variety of media including Apple iphones and Google Android phones, and for example different operating systems?
- Risk aversion: health professionals often work under heavy responsibilities and may be over-cautious e.g. when transferring their patients to another organisation, or collaborating with other providers; using an app might itself might be symbolic of embracing a different cultural approach to the more cumbersome (and slower) paper handling of integrative healthcare administration?
- Service users choosing alternative providers: service users have freedom of choice regarding their elected place of care. However, this freedom can create deviations from the planned pathway of care and may cut across attempts to provide integrated care. Regulation has a critical rôle here, if the definition of ‘any qualified provider’ allows as many regulated healthcare providers to enter into a competitive market.
There are still problems that the app would have difficulty in overcoming, namely:
- Governance: it may be unclear who has ultimate clinical and/or organisational responsibility should anything go wrong. That may make individuals reluctant to discharge patients from their care into that of another clinician.
- Clinical practice: differences in how to treat patients between different institutions can mean a lack of consensus and unwillingness to transfer patients from one part of the system to another.
- Cultural differences: driven by some of the issues above but even also by management style, extent of delegation of authority, clarity over objectives and other factors that might affect willingness to share information, resources and service users.
Nonetheless, there are possible advantages of the app:
- Having structured relationships between service providers and with patients – co-location, case management, multidisciplinary teams and assigning patients to a particular primary health care provider
- Using structured arrangements for coordinating service provision between providers – coordinated or joint consultation, shared assessments, and arrangements for priority access to another service
- Using systems to support care coordination – care plans, shared decision support, patient-held or shared records, shared information or communication systems, and a register of patients
- Improving communication between service providers – electronic transfer of data could be facilitated through instant messaging, or audio/video conferencing (like Skype)
- Providing support for patients – access to the most-up-to-date information about the condition, and healthcare providers.
Advantages of integrated care
Integrated Care should improve quality of health care. Quality can have several dimensions and interpretations. However, according to the evidence that we have reviewed, integrated care should improve quality based on four types of benefits:
- Patient experience: according to the NHS Confederation, improving patient experience as a whole is complex. It involves looking at every aspect of how care is delivered, including how the patient comes into contact with the ‘health system’ in the first place.
- Clinical outcome: based on Frommer et al. (1992), a clinical outcome is the “change in the health of an individual, group of people or population which is attributable to an intervention or series of interventions”. It could include lower admission and readmission rates, shorter hospital stay, reduction in the use of hospital beds, shorter recovery periods, etc.
- Patient safety: the Department of Health’s report on patient safety states that healthcare relies on a range of complex interactions between people, skills, technologies and drugs. Sometimes things can – and do – go wrong. While progress has been made, patient safety is not always given the same priority or status as other major issues such as reducing waiting times, implementing national service frameworks and achieving financial balance.
- Cost efficiency: reducing the overall cost of health-related concerns is complicated by defining the scope of such concerns and the extent to which prevention, actual treatment and post-treatment recovery, rehabilitation and re-integration and ongoing support are included in the calculation of costs.
The author is well aware that there are many operational and strategic issues with the implementation of such an app, but the purpose of this article is simply to introduce some basic concepts of integrated healthcare.
An ethos of collaboration is essential for the NHS to succeed
As a result of the Health and Social Care Act, the number of private healthcare providers have been allowed to increase under the figleaf of a well reputed brand, the NHS, but now allowing maximisation of shareholder dividend for private companies. The failure in regulation of the energy utilities should be a cautionary tale regarding how the new NHS is to be regulated, especially since the rule book for the NHS, Monitor, is heavily based on the rulebook for the utilities. The dogma that competition drives quality, promoted by Julian LeGrand and others, has been totally toxic in a coherent debate, and demonstrates a fundamental lack of an understanding of how health professionals in the NHS actually function. People in the NHS are very willing to work with each other, making referrals for the general benefit of the holistic care of the patient, without having to worry about personalised budgets or financial conflicts of interest. It is disgraceful that healthcare thinktanks have been allowed to peddle a language of competition, without giving due credit to the language of collaboration, which is at the heart of much contemporary management, including notably innovation.
It has now been belatedly admitted that there need to move beyond fragmented care to an integrated approach in which patients receive high-quality co-ordinated services. There is of course a useful rôle for competition, but it has to be acknowledged that healthcare professionals all try to provide the optimal medical care for their patient in the NHS, irrespective of cost, as this is literally a life-death sector, unlike production of a widget. The implication is that competition itself need not be a barrier to collaboration provided that the risks of the wrong kind of competition are addressed. Porter and Teisberg’s argument is related to the analysis of Christensen and colleagues (Christensen et al 2009), who see the solution to the problems of health care in the United States as lying in competition between integrated systems. And when the United States coughs we of course sneeze.
In 2011, the Kings Fund produced a pamphlet entitled, “Where next for the NHS reforms? The Case for Integrated Care”. This was before the inevitable enactment of the Health and Social Care Act (2012). This pamphlet was nonetheless useful in articulating that there are many barriers to the implementation of integrated care, including organisational complexity, divisions between GPs and specialists, perverse financial incentives, and the absence of a single electronic medical record available throughout the NHS. The Kings Fund at that time argued that enhanced primary care involves an action to reduce variations in the quality of primary care and to provide additional services that help to keep people out of hospital. This required a network of primary care providers that promote and maintain continuity of care with local people and act as hubs not only for the provision of generalist care but also for access to diagnostics and chronic disease management. This was of course before a wholesale shift in the ownership and outsourcing of the functions of the NHS had taken place, and what exists now is nothing short of a mess.
It is all too easy to produce politics-based evidence for contemporary healthcare in the NHS, but it is perhaps worth taking note of disasters from abroad. Martin Painter, writing in The Australian Journal of Public Administration in 2008, was one of the first to point out the dangers of privatisising the State, discussing Vietnam and China. In Vietnam and China, decentralisation is a by-product, both by default and design, of the transition to a state-managed market economy. A dual process of horizontal and vertical decentralisation was occurring simultaneously in both the economic and political arena, with an increasingly high level of de facto political/fiscal decentralisation, much of it occurring by default as local governing units try to meet rising demand for services. This is accompanied by the marketisation and socialisation of services such as education and health. Accompanying both of these processes is a trend towards greater ‘autonomisation’ of service delivery units, including the emergence of new ‘para-state’ entities. This could be seen akin to the enthusiasm demonstrated by New Labour for the NHS Foundation Trust, and the Francis Report (2013) promises to provide useful insights into the definition of this new model army of autonomous units. Most of these decentralisation processes were recognised to be the by-product of marketisation, rather than part of a process of deliberate state restructuring in pursuit of ideals of decentralised government. The cumulative effects include a significant fragmentation of the state, a high potential for informalisation and corruption, and a growing set of performance accountability problems in the delivery of public services.
With fragmentation, in addition to a lack of coherent national policy, brings a culture of mistrust which is toxic for any organisation, let alone economic sequelae (discussed later in this article.) According to the Deloitte LLP 2010 “Ethics & Workplace Survey,” when asked what factors contributed to their plans to seek new 9-to-5 work environments, 48 percent of employees cited a “loss of trust,” 46 percent said a “lack of transparency in communications,” and 40 percent noted “unfair treatment or unethical behavior by employers.” Hospitals are among the most complex types of hierarchical social organisations. Collaboration within and across hospital departments can improve efficiency, effectiveness and the quality of services, but competition for resources, professional differences and hierarchical management practices hinder innovation. However, coordinating activities across functional and interorganisational boundaries is difficult. Conflicting goals and competition for scarce resources diminish trust and the willingness of decision makers across the value chain to work together. Several researchers have identified collaboration as a means of reducing various different types of conflict both between and within organisations, in the private sector. Importantly, the “dynamic-capabilities” approach highlights two realities that underlie a firm’s opportunity to exploit collaboration. First, the word “dynamic” implies the ability to rapidly change a firm’s resource base in response to a changing environment. Second, by definition, a capability is “the firm’s ability to integrate, build, and reconfigure internal and external competencies”. The literature consistently employs terms such as “coordinate,” “combine,” and “integrate” to describe the process of capability development. These core concepts suggest the need to work effectively across organisational boundaries. Thus, decision makers should consider the orientations and strategic conflict literatures as they seek to achieve inimitable advantage via a dynamic collaboration capability.
The aim of collaboration is to produce “synergy”, that is, outcomes that are only possible by working with others. However, effective collaborative functioning is hard to achieve, because various institutions, departments and professionals have different aims, traditions, styles of working and mandates. Overcoming differences to forge productive collaboration is a key challenge to the implementation of innovative health promotion. Collaboration is a multifaceted concept with many synonyms. One person’s ‘teamwork’ can be another person’s ‘alliance’ or ‘collaboration’. Kickbusch and Quick (1998) define health promotion partnerships as the bringing together of “a set of factors for the common goal of improving the health of populations based on mutually agreed roles and principles”. Straus (2002) sees collaboration as problem solving and consensus building. Cooperation and collaboration between organisation units is also risky, and marked by uncertainty regarding a partner’s skills, goals, and reliability, as well as the pair’s ability to work together. This can be cast as an issue of incomplete information, and the most obvious way to reduce uncertainty is to improve the information used in choosing a partner. There are two possible sources: experience and other firms. Past experiences with another unit will both improve abilities to cooperate and yield information about that firm. Successful collaboration involves common knowledge, shared routines, similar ways of thinking, and tacit knowledge, all of which can be built through repeated cooperation. In addition, it also creates trust, both in terms of motives and in terms of competencies. As a consequence, there is inertia in partnership formation, and stability in network structures: firms will, all else being equal, prefer partners with whom they have worked in the past.
A problem is that collaboration may require investment from the NHS, which is justified if the partners realise valued aims that could not have been realised by the partners working in isolation. However, it may also be that one or more partners consider at least part of their investment of time, effort and money to be wasted – resulting in antagony, which is the opposite of synergy. While some waste is perhaps inevitable (‘that meeting was a complete waste of our time!’), when the waste is judged excessive, collaboration may fall in danger of crumbling before aims are achieved. This is among the reasons that many collaborations cease functioning before they have achieved their aims. However, recent experience is that public health networks can produce economies of scale, enable shared expertise, increase capacity and support professional development across all three domains of public health – health improvement, health protection and health care. Networks potentially fit well with current moves across local government towards cross-authority collaboration. Future plans need to ensure that the work of existing public health networks is not lost. Within local government, public health networks will offer new opportunities for collaboration, including shared services, intelligence and analysis and cross-authority public health commissioning.
A lot of time inevitably has been lost in a package of unelected reforms costing around £2bn so far, and will continue to be lost if the Health and Social Care Act (2012) is repealed. However, Andy Burnham has promised to move forward by allowing existant structures to do ‘different things’. Either way, Part 3 of the Act is definitely to be reversed under Burnham’s plans, and it seems as if Burnham wants to re-engineer the NHS such that private companies do not participate in ‘economic undertakings’ in such a way that EU competition law is triggered. This, I feel, would be a valuable time for Andy Burnham to admit that, while there is a rôle for competition, there is also a value role for collaboration and solidarity, through which other organisational competencies could be embedded such that key aspects are promoted like innovation or leadership. No experience goes to waste.