Home » Posts tagged 'Francis Report'
Tag Archives: Francis Report
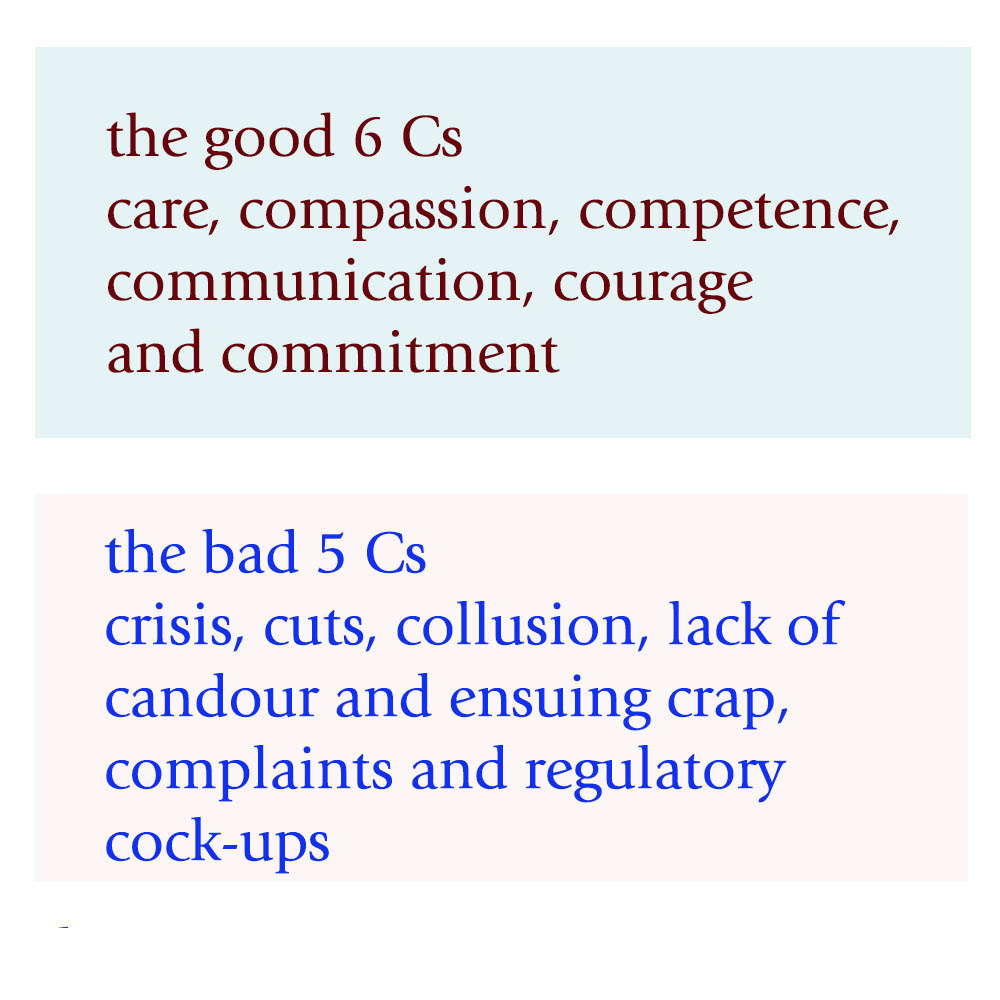
The 11 Cs – can we avoid another Mid Staffs one year after the last Francis Report?
This is the NHS leaflet on the 6Cs here.
Even for the official 6Cs, powerful forces are at play in undermining the acute medical take.
The 6Cs still, though, potentially form the ‘greater good'; that of the ‘ying Cs’.
But it’s how they engage with the 5 other ‘yang Cs’ which will determine whether there’s another Mid Staffs, more than one year on from the last Francis Report.
1. Care
Care is described as a “core business”, perceiving each event with a patient as a transaction which is a potentially billable event.” Caring defines us and our work” indeed is true; as it defines to some extent how people get paid. Unfortunately, the way in which care goes wrong is pretty consistent in the narrative. For example, nurses may be too ‘posh’ to care. In this version, nurses who are too academic are incapable of caring for which there is little published evidence. The other more likely version is that junior nurses are “too rushed to care”. This is understandable, in that if there are ten people still waiting to be clerked in, it can be hard for all professionals to focus on taking a proper history and examination without cutting corners, for examination in completing an accurate neurological examination of the cranial nerves. However, the emergency room often cultivates a feeling of a conveyor belt, with a feeling of “Now serving number 5″. A patient experience is not going to be great if the doctor, nurse or AHP appears rushed in clerking in a patient. The patient feels more like they are in a sheep dip as “continuity of care” between different medical teams suffers.
2. Compassion
“Compassion is how care is given through relationships based on empathy, respect and dignity.” Again there is some irony in the same management consultants outfit recommending compassion by healthcare professionals, when the same professionals have recommended ‘efficiency savings’. Compassion in the NHS can of course be extremely difficult to deliver from the nurses remaining after there have been staff cuts, and the remaining nurses are having to work twice as fast ‘to beat the clock’, or a target such a “four hour target”.
3. Competence
“Competence means all those in caring roles must have the ability to understand an individual’s health and social needs.” This is of course is motherhood and apple pie stuff. The problem comes if the NHS ‘productivity’ is improved with lateral swapping of job rôles: that some functions are downgraded to other staff. Health care assistants might find themselves doing certain tasks which had been reserved for them. If there’s mission creep, the situation results of receptionists triaging a patient, rather a physician’s assistant doing a venflon. Competence of course cannot be delivered by untrained staff delivering an algorithm, as has been alleged for services such as NHS 111.
4. Communication
Communication is central to successful caring relationships and to effective team working. The overall “no decision about me without me” mantra of course has been made a mockery of, with unilateral variation of nursing and medical contracts (with adjustments to terms and conditions, and pay, of staff by NHS managers without any dialogue.) If you don’t communicate any errors in clinical care to the patient (reflected in the ‘lack of candour’ below), the patient and relatives are bound to leave with an unduly glossy version of events of the acute medical assessment. This can of course bias the outcome in the ‘Friends and Family Test’.
5. Courage
“Courage enables us to do the right thing for the people we care for, to speak up when we have concerns.” Take the situation where your Master (senior nurse) is wishing to implement a target, but you’re the one rushed off your feet with missing drug charts, no investigations ordered, no management plan formed as the patient was shunted out of A&E before the 4 hour bell started ringing? Are you therefore going to be able to speak out safely against your Master when your Master is the one who determines your promotion? If you’re made of strong stuff, and completely fastidious about patient safety, you might decide ‘enough is enough’ by whistleblowing. But the evidence is that whistleblowers still ultimately get ‘punished’ in some form or others.
6. Commitment
“A commitment to our patients and populations should be the cornerstone of what we doctors, nurses, and allied healthcare professions do, especially in the “experience of the patients.””. Of course, if you get a situation where junior staff are so demoralised, by media witch hunting, it could be that people are indeed driven out of the NHS for working for other providers, or even other countries. A commitment to the public sector ethos may have little truck if you’ve got more interest in ‘interoperability’, or ‘switching’, which are of course the buzzwords of introducing ‘competition’ into healthcare systems.
There can be some downright ‘yang Cs’ epitomising danger for the acute medical take and hospital.
7. Crisis
When things get out of hand, some of the more hyperbolic allegations might conceivably happen. With people lose the plot, they are capable of anything. And if the system is too lean, and there’s a road traffic accident or other emergency, or there’s an outbreak of rotavirus amongst staff, there may be insufficient slack in the system to cope.
8. Cuts
Whilst patient campaigners have been right to emphasise that it’s more of a case of safe staffing rather than a magical minimum number, there’s clearly a number of trained staff on any shift below which it’s clearly unsafe for the nurses to deliver good nursing care. Cuts in real terms, even if that’s the same budget (just) for an increased numbers in an elderly population, can of course be a great motivator for producing unstable staffing, as the Keogh 14 demonstrated. That might be especially tempting if ‘financially strained’ NHS FTs are trying to balance their budgets in light of PFI loan repayments.
9. Collusion
This can affect a nurse’s ability to communicate problems with courage, if senior nurses are colluding with certain consultants in meeting targets. This means that medical consultants who are recipient of the non-existent drug charts, non-existent management plans, or non-existent investigation orders can probably take one or two weeks to ‘catch up’, but the ‘length of stay’ gets extended. Frontline staff might take the risks. But senior nurses might collude with the management to deliver ‘efficiency savings’ and promote themselves. That’s not fair is it?
10. Lack of Candour and Ensuing Crap
This target-driven culture of the NHS, and excessive marketing of how wonderful things are, must stop. A lack of honest communication with the patient through candour can lead to patients never knowing when things go wrong. This is a cultural issue, and it may be legislated upon at some point in the future. But without this cultural willingness by clinical staff to tell patients when things have unnecessarily got delayed through the missing drug charts etc., they will only get to know of things going badly wrong.
11. Complaints and Regulatory Cock-ups.
If things go badly wrong, they may generate complaints. These complaints may as such not matter if the system completely ignores complaints. For example, there has been only one successful judicial review against the PHSO since 1967. The recent review of the complaints process for NHS England has revealed how faulty the process is. There has been criticism of the clinical regulators in their ability to enforce patient safety too, particularly in light of Mid Staffs.
As you can see, the system is delicately balanced.
If transparency is the best disinfectant, it’s time to reveal the other five Cs for a start?
The most important thing of course may be Culture, the 12th C. If the culture is toxic, as happened in Mid Staffs, it may be hard to analyse the problem in terms of its root causes.
Isn’t it time to admit failure in ‘regulating cultures’?
It is alleged that a problem with socialists is that, at the end of the day, they all eventually run out of somebody else’s money. Perhaps more validly, it might be proposed that the problem with all politicians is that they all run of other people to blame?
It is almost as if politicians form in their minds a checklist of people they wish to nark off systematically when they get into government: candidates might include lawyers, Doctors, bankers, nurses, disabled citizens, to name but a few.
Politicians are able to use the law as a weapon. That’s because they write it. The law progressively has been reluctant to decide on moral or ethical issues, but altercations have occurred over potentially inflammable issues such as ‘the bedroom tax’. Normative ethics takes on a more practical task, which is to arrive at moral standards that regulate right and wrong conduct.
There has always been a tension between the law and ethics. As an example, to prove an offence in the English criminal law, you have to prove beyond reasonable doubt an intention rather than a motive, for example that a person intended to burn someone’s house down, rather than why he had intended so. Normative ethics involve articulating the good habits that we should acquire, the duties that we should follow, or the consequences of our behaviour on others. The ultimate ‘normative principle’ is that we should do to others what we would want others to do to us.
Parliament is about to get its knickers in a twist once again over the thorny issue of press regulation. However, there is a sense of history repeating itself. A few centuries ago, “Areopagitica” was published on 23 November 1644, at the height of the English Civil War. It is titled after Areopagitikos (Greek: ?????????????), a speech written by the Athenian orator Isocrates in the 5th century BC. (The Areopagus is a hill in Athens, the site of real and legendary tribunals, and was the name of a council whose power Isocrates hoped to restore).
“Areopagitica” was distributed via pamphlet, defying the same publication censorship it argued vehemently against. As a Protestant, Milton had supported the Presbyterians in Parliament, but in this work he argued forcefully against the Licensing Order of 1643, in which Parliament required authors to have a license approved by the government before their work could be published.
Milton then argued that Parliament’s licensing order will fail in its purpose to suppress scandalous, seditious, and libellous books: “This order of licensing conduces nothing to the end for which it was framed.” Milton objects, arguing that the licensing order is too sweeping, because even the Bible itself had been historically limited to readers for containing offensive descriptions of blasphemy and wicked men.
England has for a long time experienced problems with moving goalposts in the law, and indeed the judicial solutions sought have varied with the questions being asked. Lord Justice Leveson acknowledged that the “world wide web” was a medium subject to no central authority and that British websites were competing against foreign news organisations, particularly in America, which were part of no regulatory system.
Leveson once nevertheless proposed that newspapers should still face more regulation than the internet because parents can ‘to some extent’ control what their children see online, while they could not control what they see on a newsagent or supermarket shelf.
‘It is clear that the enforcement of law and regulation online is problematic,’ said Lord Justice Leveson at the end of his year-long inquiry into press ethics.
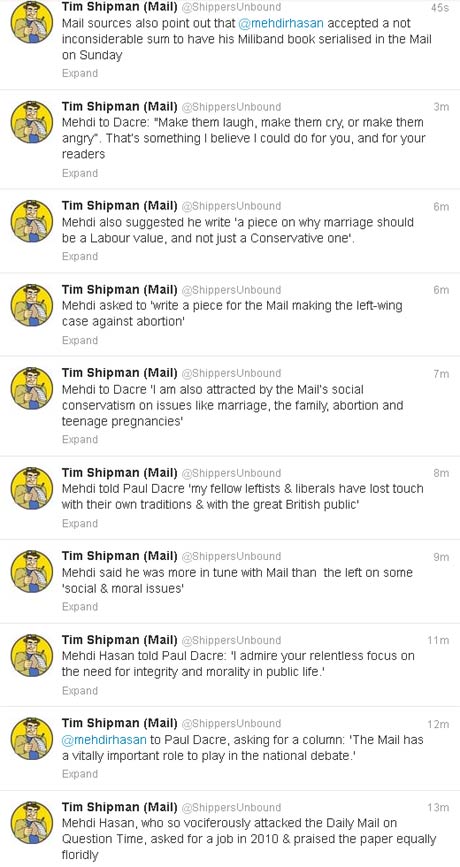
An attempt at ‘regulating culture’ was dismissed in the Leveson Report largely through arguing that the offences were substantially already ‘covered’, such as trespass of the person or phone hacking. And yet it is the case that there are ‘victims of phone hacking’ who feel that we are unlikely to be much further forward than we were before spending millions on an investigation into journalistic practices. In recent discussions this week, eyebrows have been raised at the suggestion that Ed Miliband could write to senior members in the Mail-on-Sunday empire to suggest that the culture in their newspapers is awry, and to ask them to do something about it. It could be argued it is none of Miliband’s business, except that Miliband would probably prefer the Mail to write favourably about him. Such flexibility in judgments might be on a par with Mehdi Hasan changing his writing style and target audience within a few years, as the recent Twitterstorm demonstrates.
The medical and nursing professions have latterly urged for an approach which is not overzealously punitive. There have been very few sanctions for regulatory offences in Mid Staffs or Morecambe Bay, for example.
Robert Francis QC still identified that an institutional culture which put the “business of the system ahead of patients” is to blame for the failings surrounding Mid Staffordshire Foundation Trust. Announcing the publication of his three volume report into the Mid Staffordshire Foundation Trust public inquiry, Mr Francis described what happened as a “total system failure”.
Francis argued the NHS culture during the 2005-2009 period considered by the inquiry as one that “too often didn’t consider properly the impact on patients of decisions”. However, he said the problems could not “be cured by finding scapegoats or [through] reorganisation” of the NHS but by a “real change in culture”. However, having identified the problem, solutions for cultural ‘failure’ in the NHS have not particularly been forthcoming.
There are promising reports of ‘cultural change’ in the NHS, for example at Mid Staffs and Salford, but some aggrieved relatives of patients still have a feeling that ‘justice has not been done’. There has been no magic bullet from the legislature over concerns about bad practice in the NHS, and it is unlikely that any are immediately forthcoming. There is little doubt, however, that parliament improving the law on safe staffing or how whistleblowers can raise issues in the public interest safely might be constructive steps forward. There therefore exists how the law might conceivably ‘improve’ the culture, and one suspects that this change in culture will have to permeate throughout the entire organisation to be effective. That is, fundamentally, people are not punished for speaking out safely, and, whilst legitimate employers’ interests will have to be protected, the protection for employees will have to be necessary and proportionate equally under such a framework.
Journalism and the NHS are not isolated examples, however, Newly released reports into the failures of management at several major banks – HBOS, Barclays, and JP Morgan among them – show that some of the worst losses had roots deeper than the 2008 credit crisis. It is said that a toxic internal culture and poor management, not the subprime mortgage collapse, caused billion-dollar losses at some of the world’s largest banks
In an argument akin to that used to argue that there is no need to regulate the journalism industry, the banking industry have long maintained that a strong feeling of internal competition can be healthy for profitability, but problems such as abject fraud and misselling of financial products are already illegal.
The situation is therefore a nonsense one. There is a failed culture, ranging across several diverse disciplines, of politicians wishing to use regulation to correct failed cultures. Cultures of an organisation, even with the best will in the world, can only be changed from within, even if the public, vicariously through politicians, wish to impose moral and ethical standards from outside.
Whichever way you wish to frame the argument, it might appear ‘we cannot go on like this.’ It is a pathology which straddles across all the major political parties, and yet all the parties wish to claim that they have identified a poor culture.
Their lack of perception about what to do with these problems is perhaps further evidence that the political class is not fit for the job.
Toxic cultures, NHS Trusts and the Francis Report.
Robert Francis has an incredibly difficult task. It is difficult for people who have not qualified in medicine, even managers and leaders of healthcare think tanks, to understand how this situation has arisen. Being a senior lawyer, his approach will necessarily involve “the law is not enough”. The NHS is currently a “political football”, but the overriding objective must be one of patient safety. Whatever your views about managers following financial targets religiously, and regulatory authorities pursuing their own targets sometimes with equal passion, it is hard to escape from the desire for a national framework for patient safety. This is at a time indeed when it is proposed that the National Health and Patient Safety Agency should be abolished, which indeed has oversight of medical devices and equipment. Indeed, one of the findings of the Francis Inquiry is that essential medical equipment was not always available or working. A general problem with the approach of the Health and Social Care Act (2012) has been the abolition of ‘national’ elements, such as abolition of the Health Protection Authority.
That the hospital assumes voluntarily a duty-of-care for its patient once the patient presents himself is a given in English law, but this fact is essential to establish that there has been a breach of duty-of-care legally later down the line. In the increasingly corporate nature of the NHS following the Health and Social Care Act, there is of course a mild irony that there is more than a stench of corporate scandals in the aftermath which is about to explode in English healthcare. Patients’ families feel that they have been failed, and this is a disgrace.
ENRON was a corporate scandal of equally monumental proportions, as explained here:
Mid Staffs NHS Foundation Trust was poor at identifying when things went wrong and managing risk. Some serious errors happened more than once and the trust had high levels of complaints compared with other trusts.
The starting point must be whether the current law is good enough. We have systems in place where complaints can be made against doctors, nurses, midwives and hospitals through the GMC, MWC and CQC respectively, further to local resolution. In fact, it is still noteworthy that many junior and senior doctors are not that cognisant of the local and national complaint mechanisms at all, and the mechanisms used for risk mitigation. There is a sense that the existing regulatory framework is failing patients, and public trust and confidence in medical and nursing, and this might be related to Prof Jarman’s suggestion of an imbalance between clinicians and managers in the NHS.
The Francis Inquiry heard a cornucopia of evidence about a diverse range of clinical patient safety issues, and indeed where early warnings were made but ignored. Prof Brian Jarman incredibly managed to encapsulate many of the single issues in a single tweet this morning:
Any list of failings makes grim reading. There are clear management failures. For example, assessing the priority of care for patients in accident and emergency (A&E) was routinely conducted by unqualified receptionists. There was often no experienced surgeon in the hospital after 9pm, with one recently qualified doctor responsible for covering all surgical patients and admitting up to 20 patients a night. A follower on my own Twitter thread who is in fact him/herself a junior, stated this morning to me that this problem had not gone away:
However, it is unclear what there may be about NHS culture where clinicians do not feel they are able to “whistle blow” about concerns. The “culture of fear” has been described previously, and was alive-and-well on my Twitter this morning:
Experience from other sectors and other jurisdictions is that the law clearly may not be protective towards employees who have genuine concerns which are in the “public interest”, and whose concerns are thereby suppressed in a “culture of bullying“. This breach of freedom of expression is indeed unlawful as a breach of human rights, and toxic leaders in other sectors are able to get away with this, in meeting their targets (in the case of ENRON increased profitability), “project a vision”, and exhibit “actions that “intimidate, demoralize (sic), demean and marginalize (sic)” others. Typically, employees are characterised as being of a vulnerable nature, and you can see how the NHS would be a great place for a toxic culture to thrive, as junior doctors and nurses are concerned about their appraisals and assessments for personal career success. “Projecting a vision” for a toxic hospital manager might mean performing well on efficiency targets, which of course might be the mandate of the government at the time, even if patient safety goes down the pan. Managers simply move onto a different job, and often do not have to deal even with the reputational damage of their decisions. Efficiency savings of course might be secured by “job cuts” (another follower):
Another issue which is clearly that such few patients were given the drug warfarin to help prevent blood clots despite deep vein thrombosis being a major cause of death in patients following surgery. This is a fault in decision-making of doctors and nurses, as the early and late complications of any surgery are pass/fail topics of final professional exams. Another professional failing in regulation of the nurses is that nurses lacked training, including in some cases how to read cardiac monitors, which were sometimes turned off, or how to use intravenous pumps. This meant patients did not always get the correct medication. The extent to which managers ignored this issue is suggestive of wilful blindness. A collusion in failure between management and surgical teams is the finding that delays in operations were commonplace, especially for trauma patients at weekends; surgery might be delayed for four days in a row during which time patients would receive “nil by mouth” for most of the day.
Whether this toxic culture was isolated and unique to Mid Staffs, akin to how corporate failures were rather specialist in ENRON, is a question of importance. What is clear that there has been a fundamental mismatch between the status and perception of healthcare entities where certain individuals have “gamed” the situation. Alarmingly it has also been reported that the University Hospitals of Morecambe Bay NHS Foundation Trust have also had a spate of failures in in maternity, A&E and general medical services. The Sarbanes-Oxley Act (2002) was enacted in the US in response to a number of high-profile accounting scandals. In English law, the Financial Markets and Services Act (2010), even during Labour’s “failure of regulation” was drafted to fill a void in financial regulation. There is now a clear drive for someone to take control, in a manner of crisis leadership in response to natural disasters. Any lack of leadership, including an ability to diagnose the crisis at hand and respond in a timely and appropriate fashion, against the backdrop of a £2bn reorganisation of the NHS, are likely to constitute “barriers-to-improvement” in the NHS.
This issue is far too important for the NHS to become a case for privatisation. It is a test of the mettle of politicians to be able to cope with this. They may have to legislate on this issue, but David Cameron has shown that he is resistant to legislate even after equally lengthy reports (such as the Leveson Inquiry). It is likely that a National Patient Safety Act which puts on a statutory footing a statutory duty for all patients treated in the NHS, even if they are seen by private contractors using the NHS logo, may be entitled to a formal statutory footing. The footing could be to avoid “failure” where “failure” is avoiding harm (non-maleficence). Company lawyers will note the irony of this being analogous to s.172 Companies Act (2006) obliging company directors to promote the “success” of a company, where “success” is defined in a limited way in improving shareholder dividend and profitability under existing common law.
The law needs to restore public trust and confidence in the nursing and healthcare professions, and the management upon which they depend. The problem is that the GMC and other regulatory bodies have limited sanctions, and the law has a limited repertoir including clinical negligence and corporate manslaughter with limited scope. At the end of the day, however, this is not a question about politics or the legal and medical professions, it is very much about real people.
The advantage of putting this on the statute books once-and-for-all is that it would send out a powerful signal that actions of clinical and management that meet targets but fail in patient safety have imposable sanctions. After America’s most high-profile corporate fraud trial, Mr Lay, the ENRON former chief executive was found guilty on 25 May on all six fraud and conspiracy charges that he faced. Many relatives and patients feel that what happened at Stafford was much worse as it affected real people rather than £££. However, the Sarbanes-Oxley Act made auditors culpable, and the actions of managers are no less important.
This is not actually about Jeremy Hunt. Warning: this is about to get very messy. That Mid Staffs is not isolated strongly suggests that an ability of managers and leaders in Trusts to game the system while failing significantly in patient safety, and the national policy which produced this merits attention, meaning also that urgent legislation is necessary to stem these foci of toxicity. A possible conclusion, but presumption of innocence is vital in English law, from Robert Francis, and he is indeed an eminent QC in regulatory law, is that certain managers were complicit in clinical negligence at their Trusts to improve managerial ratings, having rock bottom regard for actual clinical safety. This represents a form of wilful blindness (and Francis as an eminent regulatory QC may make that crucial link), and there is an element of denial and lack of insight by the clinical regulatory authorities in dealing with this issue, if at all, promptly to secure trust from relatives in the medical profession. The legal profession has a chance now to remedy that, but only if the legislature enable this. But this will be difficult.
A failure of leadership and management: toxic cultures, ENRON and the Francis Report
 Robert Francis has an incredibly difficult task. It is difficult for people who have not qualified, even managers and leaders of healthcare think tanks, to understand how this situation has arisen. Being a senior lawyer, his approach will necessarily involve “the law is not enough”. The NHS is currently a “political football”, but the overriding objective must be one of patient safety. Whatever your views about managers following financial targets religiously, and regulatory authorities pursuing their own targets sometimes with equal passion, it is hard to escape from the desire for a national framework for patient safety. This is at a time indeed when it is proposed that the National Health and Patient Safety Agency should be abolished, which indeed has oversight of medical devices and equipment. Indeed, one of the findings of the Francis Inquiry is that essential medical equipment was not always available or working. A general problem with the approach of the Health and Social Care Act (2012) has been the abolition of ‘national’ elements, such as abolition of the Health Protection Authority. (more…)
Robert Francis has an incredibly difficult task. It is difficult for people who have not qualified, even managers and leaders of healthcare think tanks, to understand how this situation has arisen. Being a senior lawyer, his approach will necessarily involve “the law is not enough”. The NHS is currently a “political football”, but the overriding objective must be one of patient safety. Whatever your views about managers following financial targets religiously, and regulatory authorities pursuing their own targets sometimes with equal passion, it is hard to escape from the desire for a national framework for patient safety. This is at a time indeed when it is proposed that the National Health and Patient Safety Agency should be abolished, which indeed has oversight of medical devices and equipment. Indeed, one of the findings of the Francis Inquiry is that essential medical equipment was not always available or working. A general problem with the approach of the Health and Social Care Act (2012) has been the abolition of ‘national’ elements, such as abolition of the Health Protection Authority. (more…)
We've been here before. On legislation against toxic culture within the NHS: lessons from ENRON for the Francis Report.

Robert Francis has an incredibly difficult task. It is difficult for people who have not qualified in medicine, even managers and leaders of healthcare think tanks, to understand how this situation has arisen. Being a senior lawyer, his approach will necessarily involve “the law is not enough”. The NHS is currently a “political football”, but the overriding objective must be one of patient safety. Whatever your views about managers following financial targets religiously, and regulatory authorities pursuing their own targets sometimes with equal passion, it is hard to escape from the desire for a national framework for patient safety. This is at a time indeed when it is proposed that the National Health and Patient Safety Agency should be abolished, which indeed has oversight of medical devices and equipment. Indeed, one of the findings of the Francis Inquiry is that essential medical equipment was not always available or working. A general problem with the approach of the Health and Social Care Act (2012) has been the abolition of ‘national’ elements, such as abolition of the Health Protection Authority.
That the hospital assumes voluntarily a duty-of-care for its patient once the patient presents himself is a given in English law, but this fact is essential to establish that there has been a breach of duty-of-care legally later down the line. In the increasingly corporate nature of the NHS following the Health and Social Care Act, there is of course a mild irony that there is more than a stench of corporate scandals in the aftermath which is about to explode in English healthcare. Patients’ families feel that they have been failed, and this is a disgrace.
ENRON was a corporate scandal of equally monumental proportions, as explained here:
Mid Staffs NHS Foundation Trust was poor at identifying when things went wrong and managing risk. Some serious errors happened more than once and the trust had high levels of complaints compared with other trusts.
The starting point must be whether the current law is good enough. We have systems in place where complaints can be made against doctors, nurses, midwives and hospitals through the GMC, MWC and CQC respectively, further to local resolution. In fact, it is still noteworthy that many junior and senior doctors are not that cognisant of the local and national complaint mechanisms at all, and the mechanisms used for risk mitigation. There is a sense that the existing regulatory framework is failing patients, and public trust and confidence in medical and nursing, and this might be related to Prof Jarman’s suggestion of an imbalance between clinicians and managers in the NHS.
The Francis Inquiry heard a cornucopia of evidence about a diverse range of clinical patient safety issues, and indeed where early warnings were made but ignored. Prof Brian Jarman incredibly managed to encapsulate many of the single issues in a single tweet this morning:
Any list of failings makes grim reading. There are clear management failures. For example, assessing the priority of care for patients in accident and emergency (A&E) was routinely conducted by unqualified receptionists. There was often no experienced surgeon in the hospital after 9pm, with one recently qualified doctor responsible for covering all surgical patients and admitting up to 20 patients a night. A follower on my own Twitter thread who is in fact him/herself a junior, stated this morning to me that this problem had not gone away:
However, it is unclear what there may be about NHS culture where clinicians do not feel they are able to “whistle blow” about concerns. The “culture of fear” has been described previously, and was alive-and-well on my Twitter this morning:
Experience from other sectors and other jurisdictions is that the law clearly may not be protective towards employees who have genuine concerns which are in the “public interest”, and whose concerns are thereby suppressed in a “culture of bullying“. This breach of freedom of expression is indeed unlawful as a breach of human rights, and toxic leaders in other sectors are able to get away with this, in meeting their targets (in the case of ENRON increased profitability), “project a vision”, and exhibit “actions that “intimidate, demoralize (sic), demean and marginalize (sic)” others. Typically, employees are characterised as being of a vulnerable nature, and you can see how the NHS would be a great place for a toxic culture to thrive, as junior doctors and nurses are concerned about their appraisals and assessments for personal career success. “Projecting a vision” for a toxic hospital manager might mean performing well on efficiency targets, which of course might be the mandate of the government at the time, even if patient safety goes down the pan. Managers simply move onto a different job, and often do not have to deal even with the reputational damage of their decisions. Efficiency savings of course might be secured by “job cuts” (another follower):
Another issue which is clearly that such few patients were given the drug warfarin to help prevent blood clots despite deep vein thrombosis being a major cause of death in patients following surgery. This is a fault in decision-making of doctors and nurses, as the early and late complications of any surgery are pass/fail topics of final professional exams. Another professional failing in regulation of the nurses is that nurses lacked training, including in some cases how to read cardiac monitors, which were sometimes turned off, or how to use intravenous pumps. This meant patients did not always get the correct medication. The extent to which managers ignored this issue is suggestive of wilful blindness. A collusion in failure between management and surgical teams is the finding that delays in operations were commonplace, especially for trauma patients at weekends; surgery might be delayed for four days in a row during which time patients would receive “nil by mouth” for most of the day.
Whether this toxic culture was isolated and unique to Mid Staffs, akin to how corporate failures were rather specialist in ENRON, is a question of importance. What is clear that there has been a fundamental mismatch between the status and perception of healthcare entities where certain individuals have “gamed” the situation. Alarmingly it has also been reported that the University Hospitals of Morecambe Bay NHS Foundation Trust have also had a spate of failures in in maternity, A&E and general medical services. The Sarbanes-Oxley Act (2002) was enacted in the US in response to a number of high-profile accounting scandals. In English law, the Financial Markets and Services Act (2010), even during Labour’s “failure of regulation” was drafted to fill a void in financial regulation. There is now a clear drive for someone to take control, in a manner of crisis leadership in response to natural disasters. Any lack of leadership, including an ability to diagnose the crisis at hand and respond in a timely and appropriate fashion, against the backdrop of a £2bn reorganisation of the NHS, are likely to constitute “barriers-to-improvement” in the NHS.
This issue is far too important for the NHS to become a case for privatisation. It is a test of the mettle of politicians to be able to cope with this. They may have to legislate on this issue, but David Cameron has shown that he is resistant to legislate even after equally lengthy reports (such as the Leveson Inquiry). It is likely that a National Patient Safety Act which puts on a statutory footing a statutory duty for all patients treated in the NHS, even if they are seen by private contractors using the NHS logo, may be entitled to a formal statutory footing. The footing could be to avoid “failure” where “failure” is avoiding harm (non-maleficence). Company lawyers will note the irony of this being analogous to s.172 Companies Act (2006) obliging company directors to promote the “success” of a company, where “success” is defined in a limited way in improving shareholder dividend and profitability under existing common law.
The law needs to restore public trust and confidence in the nursing and healthcare professions, and the management upon which they depend. The problem is that the GMC and other regulatory bodies have limited sanctions, and the law has a limited repertoir including clinical negligence and corporate manslaughter with limited scope. At the end of the day, however, this is not a question about politics or the legal and medical professions, it is very much about real people.
The advantage of putting this on the statute books once-and-for-all is that it would send out a powerful signal that actions of clinical and management that meet targets but fail in patient safety have imposable sanctions. After America’s most high-profile corporate fraud trial, Mr Lay, the ENRON former chief executive was found guilty on 25 May on all six fraud and conspiracy charges that he faced. Many relatives and patients feel that what happened at Stafford was much worse as it affected real people rather than £££. However, the Sarbanes-Oxley Act made auditors culpable, and the actions of managers are no less important.
This is not actually about Jeremy Hunt. Warning: this is about to get very messy. That Mid Staffs is not isolated strongly suggests that an ability of managers and leaders in Trusts to game the system while failing significantly in patient safety, and the national policy which produced this merits attention, meaning also that urgent legislation is necessary to stem these foci of toxicity. A possible conclusion, but presumption of innocence is vital in English law, from Robert Francis, and he is indeed an eminent QC in regulatory law, is that certain managers were complicit in clinical negligence at their Trusts to improve managerial ratings, having rock bottom regard for actual clinical safety. This represents a form of wilful blindness (and Francis as an eminent regulatory QC may make that crucial link), and there is an element of denial and lack of insight by the clinical regulatory authorities in dealing with this issue, if at all, promptly to secure trust from relatives in the medical profession. The legal profession has a chance now to remedy that, but only if the legislature enable this. But this will be difficult.
‘Work in progress’ : Andy Burnham’s 2012 conference speech throws up tough challenges
Andy Burnham has vowed to reverse the “rapid” privatisation of NHS hospitals in England if Labour wins power. In particular, Mr Burnham said he feared the new freedom for hospitals to earn 49% of their income from private work would “damage the character and culture” of the NHS and take it closer to an American model.
The issue of fragmentation of the NHS is a genuine problem in the NHS, as enacted this year. This is manifest in a number of different guises, such as lack of clarity as to which private entity owns what for local services, the abolition of statutory bodies involved in healthcare (such as the National Patient Safety Agency and the Health Protection Agency), and the phenomenon of “postcode lottery” in healthcare provision.
Andy Burnham clearly wishes “Labour values” of collaboration and solidarity to be pervasive in an equitable National Health Service, rather than competition, where there are winners and losers. This is particularly interesting from a business management sense, as it has long been a source of academic interest in innovation management how the “innovators’ dilemma” is solved in the private sector. This is the practical business question posed by Prof Clay Christensen, professorial fellow in innovation at Harvard, as to how it is possible, that, amongst private entities in the market place, business entities can secure competitive advantage, while working together sharing knowledge in seamless collaboration.
It seems pretty likely that, even if Labour win the 2015 general election and the Health and Social Act (2012) is repealed, commissioning will exist in some form, with Labour taking forward ‘best practice’ from the experiences of clinical commissioning groups (CCGs). There is no inkling that, whilst certain structures are in the process of being abolished for some time (such as the PCTs and SHAs), the CCGS and NHS Foundation Trusts will follow suit. Indeed, Professor Brian Edwards, special adviser to the Institute of Healthcare Managers, said he was “appalled and frustrated” at news the Francis Report would not be published until January 2013, and called it “a cruel blow” to the families of victims. This report discusses the failings at hospitals in Mid Staffordshire between 2005 and 2009, and is anticipated to be invaluable in developing further NHS foundation trusts.
Integration in person-centred care has always been a hallmark of excellent medical care, and Burnham keens to bring this out as a dominant theme in components of his new Health Bill in 2015 or 2016 if elected. When patients present to their G.P., they simply do not present as isolated medical diagnoses. For example, if an elderly patient, who may incidentally have a probable diagnosis of dementia, falls, a GP would be concerned with the patient is at risk of a fracture due to underlying osteoporosis, has poor eyesight due to a cataract for example, or leads a life in a cluttered home environment due to lack of social care. There are a plethora of problems which are likely to cause an individual to come into contact with the NHS, and the integration of health and social care is indeed entirely in keeping with Nye Bevan’s original aspiration for the NHS. The ideal would be of course to have an integrated health and social care service, but much time (and money) has been lost by the Coalition kicking the Dilnot review ‘into the long grass’ when we were already supposedly meant to be looking for greater efficiencies through the Nicholson Challenge.
Moves are clearly afoot as to who is providing the services, with various morphologies in terminology (for example “NHS preferred provider”, “any willing provider”, or “any qualified provider”). Closer to home for the current delegates in Manchester, patients will be taken to hospital by a bus company after the North West Ambulance Service (NWAS) failed to win a contract. It will not affect 999 emergency call-outs. Arriva, which run bus services throughout Greater Manchester, will replace NWAS which currently runs the service but was outbid by Arriva after the the service was put out to tender.
Chris Ham, Chief Executive of the Kings Fund, has concerns which are perfectly fair, in response:
“Andy Burnham has outlined a vision for the future of health and social care which accentuates the differences between the Labour Party and the government on the NHS. He is right to stress the need for fundamental change in health and social care services. Our own work has made the case for radical changes to ensure the NHS is fit to meet the challenges of the future as the population ages and health needs change.
This includes moving care closer to people’s homes and re-thinking the role of hospitals which must change to improve the quality of specialist services and better meet the needs of older patients. We also welcome his emphasis on delivering integrated care – the challenge now is to move integrated care from the policy arena and make it happen across the country at scale and pace.
However, while the long term vision is ambitious, the details of Labour’s plans are sketchy. A number of questions will need to be answered in the policy review announced today. For example, it is not clear how local authorities could take on the role of commissioning health care without further structural upheaval. And despite the Shadow Chancellor’s pledge earlier in the week, it is not clear how Labour would ensure adequate funding for social care.”
Text of speech given this morning in Manchester.
Conference, my thanks to everyone who has spoken so passionately today and I take note of the composite.
A year ago, I asked for your help.
To join the fight to defend the NHS – the ultimate symbol of Ed’s One Nation Britain.
You couldn’t have done more.
You helped me mount a Drop the Bill campaign that shook this Coalition to its core.
Dave’s NHS Break-Up Bill was dead in the water until Nick gave it the kiss of life.
NHS privatisation – courtesy of the Lib Dems. Don’t ever let them forget that.
We didn’t win, but all was not lost.
We reminded people of the strength there still is in this Labour movement of ours when we fight as one, unions and Party together, for the things we hold in common.
We stood up for thousands of NHS staff like those with us today who saw Labour defending the values to which they have devoted their working lives.
And we spoke for the country – for patients and people everywhere who truly value the health service Labour created and don’t want to see it broken down.
Conference, our job now is to give them hope.
To put Labour at the heart of a new coalition for the NHS.
To set out a Labour alternative to Cameron’s market.
To make the next election a choice between two futures for our NHS.
They inherited from us a self-confident and successful NHS.
In just two years, they have reduced it to a service demoralised, destabilised, fearful of the future.
The N in NHS under sustained attack.
A postcode lottery running riot – older people denied cataract and hip operations.
NHS privatisation at a pace and scale never seen before.
Be warned – Cameron’s Great NHS Carve-Up is coming to your community.
As we speak, contracts are being signed in the single biggest act of privatisation the NHS has ever seen.
398 NHS community services all over England – worth over a quarter of a billion pounds – out to open tender.
At least 37 private bidders – and yes, friends of Dave amongst the winners.
Not the choice of GPs, who we were told would be in control.
But a forced privatisation ordered from the top.
And a secret privatisation – details hidden under “commercial confidentiality” – but exposed today in Labour’s NHS Check.
Our country’s most-valued institution broken up, sold off, sold out – all under a news black-out.
It’s not just community services.
From this week, hospitals can earn up to half their income from treating private patients. Already, plans emerging for a massive expansion in private work, meaning longer waits for NHS patients.
And here in Greater Manchester – Arriva, a private bus company, now in charge of your ambulances.
When you said three letters would be your priority, Mr Cameron, people didn’t realise you meant a business priority for your friends.
Conference, I now have a huge responsibility to you all to challenge it.
Every single month until the Election, Jamie Reed will use NHS Check to expose the reality.
I know you want us to hit them even harder – and we will.
But, Conference, I have to tell you this: it’s hard to be a Shadow when you’re up against the Invisible Man.
Hunt Jeremy – the search is on for the missing Health Secretary.
A month in the job but not a word about thousands of nursing jobs lost.
Not one word about crude rationing, older people left without essential treatment.
Not a word about moves in the South West to break national pay.
Jeremy Hunt might be happy hiding behind trees while the front-line of the NHS takes a battering.
But, Conference, for as long as I do this job, I will support front-line staff and defend national pay in the NHS to the hilt.
Lightweight Jeremy might look harmless. But don’t be conned.
This is the man who said the NHS should be replaced with an insurance system.
The man who loves the NHS so much he tried to remove the tribute to it from the Opening Ceremony of the Olympic Games.
Can you imagine the conversation with Danny Boyle?
“Danny, if you really must spell NHS with the beds, at least can we have a Virgin Health logo on the uniforms?”
Never before has the NHS been lumbered with a Secretary of State with so little belief in it.
It’s almost enough to say “come back Lansley.”
But no. He’s guilty too.
Lansley smashed it up for Hunt to sell it off with a smile.
But let me say this to you, Mr Hunt. If you promise to stop privatising the NHS, I promise never to mispronounce your name.
So, Conference, we’re the NHS’s best hope. Its only hope.
It’s counting on us.
We can’t let it down.
So let’s defend it on the ground in every community in England.
Andrew Gwynne is building an NHS Pledge with our councillors so, come May, our message will be: Labour councils, last line of defence for your NHS.
But we need to do more.
People across the political spectrum oppose NHS privatisation.
We need to reach out to them, build a new coalition for the NHS.
I want Labour at its heart, but that means saying more about what we would do.
We know working in the NHS is hard right now, when everything you care about is being pulled down around you.
I want all the staff to know you have the thanks of this Conference for what you do.
But thanks are not enough. You need hope.
To all patients and staff worried about the future, hear me today: the next Labour Government will repeal Cameron’s Act.
We will stop the sell-off, put patients before profits, restore the N in NHS.
Conference, put it on every leaflet you write. Mention it on every doorstep.
Make the next election a referendum on Cameron’s NHS betrayal.
On the man who cynically posed as a friend of the NHS to rebrand the Tories but who has sold it down the river.
In 2015, a vote for Labour will be a vote for the NHS.
Labour – the best hope of the NHS. Its only hope.
And we can save it without another structural re-organisation.
I’ve never had any objection to involving doctors in commissioning. It’s the creation of a full-blown market I can’t accept.
So I don’t need new organisations. I will simply ask those I inherit to work differently.
Not hospital against hospital or doctor against doctor.
But working together, putting patients before profits.
For that to happen, I must repeal Cameron’s market and restore the legal basis of a national, democratically-accountable, collaborative health service.
But that’s just the start.
Now I need your help to build a Labour vision for 21st century health and care, reflecting on our time in Government.
We left an NHS with the lowest-ever waiting lists, highest-ever patient satisfaction.
Conference, always take pride in that.
But where we got it wrong, let’s say so.
So while we rebuilt the crumbling, damp hospitals we inherited, providing world-class facilities for patients and staff, some PFI deals were poor value for money.
At times, care of older people simply wasn’t good enough. So we owe it to the people of Stafford to reflect carefully on the Francis report into the failure at Mid-Staffordshire Foundation NHS Trust.
And while we brought waiting lists down to record lows, with the help of the private sector, at times we let the market in too far.
Some tell me markets are the only way forward.
My answer is simple: markets deliver fragmentation; the future demands integration.
As we get older, our needs become a mix of the social, mental and physical.
But, today, we meet them through three separate, fragmented systems.
In this century of the ageing society, that won’t do.
Older people failed, struggling at home, falling between the gaps.
Families never getting the peace of mind they are looking for, being passed from pillar to post, facing an ever-increasing number of providers.
Too many older people suffering in hospital, disorientated and dehydrated.
When I shadowed a nurse at the Royal Derby, I asked her why this happens.
Her answer made an impression.
It’s not that modern nurses are callous, she said. Far from it. It’s simply that frail people in their 80s and 90s are in hospitals in ever greater numbers and the NHS front-line, designed for a different age, is in danger of being overwhelmed.
Our hospitals are simply not geared to meet people’s social or mental care needs.
They can take too much of a production-line approach, seeing the isolated problem – the stroke, the broken hip – but not the whole person behind it.
And the sadness is they are paid by how many older people they admit, not by how many they keep out.
If we don’t change that, we won’t deliver the care people need in an era when there’s less money around.
It’s not about new money.
We can get better results for people if we think of one budget, one system caring for the whole person – with councils and the NHS working closely together.
All options must be considered – including full integration of health and social care.
We don’t have all the answers. But we have the ambition. So help us build that alternative as Liz Kendall leads our health service policy review.
It means ending the care lottery and setting a clear a national entitlement to what physical, mental and social care we can afford – so people can see what’s free and what must be paid for.
It means councils developing a more ambitious vision for local people’s health: matching housing with health and care need; getting people active, less dependent on care services, by linking health with leisure and libraries; prioritising cycling and walking.
A 21st century public health policy that Diane Abbott will lead.
If we are prepared to accept changes to our hospitals, more care could be provided in the home for free for those with the greatest needs and for those reaching the end of their lives.
To the district general hospitals that are struggling, I don’t say close or privatise.
I say let’s help you develop into different organisations – moving into the community and the home meeting physical, social and mental needs.
Whole-person care – the best route to an NHS with mental health at its heart, not relegated to the fringes, but ready to help people deal with the pressure of modern living.
Imagine what a step forward this could be.
Carers today at their wits end with worry, battling the system, in future able to rely on one point of contact to look after all of their loved-one’s needs.
The older person with advanced dementia supported by one team at home, not lost on a hospital ward.
The devoted people who look after our grans and grand-dads, mums and dads, brothers and sisters – today exploited in a cut-price, minimum wage business – held in the same regard as NHS staff.
And, if we can find a better solution to paying for care, one day we might be able to replace the cruel ‘dementia taxes’ we have at the moment and build a system meeting all of a person’s needs – mental, physical, social – rooted in NHS values.
In the century of the ageing society, just imagine what a step forward that could be.
Families with peace of mind, able to work and balance the pressures of caring – the best way to help people work longer and support a productive economy in the 21st century.
True human progress of the kind only this Party can deliver.
So, in this century, let’s be as bold as Bevan was in the last.
Conference, the NHS is at a fork in the road.
Two directions: integration or fragmentation.
We have chosen our path.
Not Cameron’s fast-track to fragmentation.
But whole-person care.
A One Nation system built on NHS values, putting people before profits.
A Labour vision to give people the hope they need, to unite a new coalition for the NHS.
The NHS desperately needs a Labour win in 2015.
You, me, we are its best hope. It’s only real hope.
It won’t last another term of Cameron.
NHS.
Three letters. Not Here Soon.
The man who promised to protect it is privatising it.
The man who cut the NHS not the deficit.
Cameron. NHS Conman.
Now more than ever, it needs folk with the faith to fight for it.
You’re its best hope. It’s only hope.
You’ve kept the faith.
Now fight for it – and we will win.