Home » Posts tagged 'dementia friendly communities'
Tag Archives: dementia friendly communities
Thought diversity is necessary for people living well with dementia to get a fair hearing
It is not uncommon for ‘special event days’ on dementia to feature one or two people living with dementia. Sometimes there are logistic difficulties in providing fair representation of people living with dementia at international conferences, even.
People living well with dementia who instead attend these events witness these events stuffed full of ‘experts’ or directors providing their missives. They often complain that the minimal representation which is actually provided is tokenistic.
Deep down, there is a concern that people living with dementia are merely superficially involved as bit part actors in the weaponisation of a Pharma-led “war against dementia”. There are very few ‘good news stories’ about people successfully living well with dementia, say still in employment or contributing value in some important way.
But how big institutions act can be rather different in behaviour than that on the ground.
James Kouzes and Barry Posner indicated in “The Leadership Challenge” that there are several decision-making myths:
1. The chief executive decides.
2. Decisions are made in the room.
3. Decisions are largely intellectual exercises.
4. Managers analyse and then decide.
5. Managers decide and then act.
Both domestic and international policy for living well with dementia, rather, has converged on the notion that persons living with dementia should be included at an early stage in key features of service provision and research into dementia.
For this strategy to bear fruit in England in 2015-20, it is not adequate to have minimal involvement with people with dementia, while the script is in effect written by large charities and corporates.
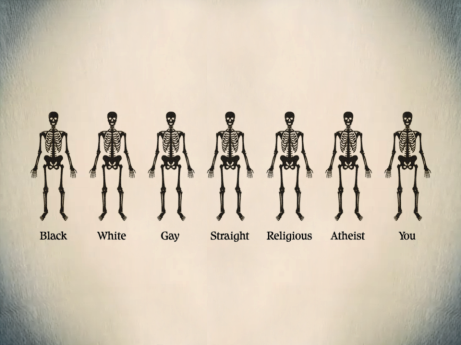
There has been recent interest in “thought diversity“, often called “cognitive diversity”, in giving full attention to the plurality of different opinions about issues. It is thought that this is not simply an alternative to an anti-discrimination policy, but is fundamental to all features of fairness, equality, justice and integrity.
I feel thought diversity from people living well with dementia is essential to mitigate against the risk of undue influence on policy from ‘experts’, some of whom have not even met a person living with dementia. Conversely, when people living with dementia get together to discuss issues important to them, such as through the virtual cafés of the Dementia Alliance International (a global umbrella organisation for people living with dementia), the power of decisions collectively made can be much more convincing. This is akin to the well rehearsed phenomenon of “crowdsourcing” or “friend sourcing”.
My disappointment with the policy strand of ‘dementia friendly communities’ in any jurisdiction is that it does not really appear to have captured the public’s imagination for social change, in the same way that Marshall Ganz describes for the Obama Campaign.
I think vital to making this a box office issue is to emphasise that dementia is not a fringe policy issue. There are possibly about close to 900,000 people living with dementia in the UK as we speak.
Torie Osborn in the National Civic Review provided an elegant way of moving forward:
“A new era of cross-cutting change making has arrived. It favors linking communities and sectors together into public and political will for solutions on big, thorny issues affecting everyone—issues that America has not tackled head on for a long time, if ever, such as rising inequality in the global economy and climate change.”
But this has necessarily reframed the diversity narrative – perhaps, as discussed by Osborn, more to “Yes we can!”
Here the “Yes we can!” is being shouted from the rooftops by people living with dementia themselves.
Also, I feel the insights from people living with dementia are essential in formulating the policy of how a community might be improved to improve the wellbeing, say perhaps in housing design. Such decisions are likely to be of a much higher standard in quality, in keeping with previous research, for example, from the the Intelligence Advanced Research Projects Activity (“IARPA”).
This is not simply about hoping for the best, in getting a range of opinions, hoping that some opinions will gain legs. It is known that the first person to speak in a meeting often influences all subsequent opinions. The same effect could occur, for example, if a CEO of a regulator or a dementia charity talks at the top of a billing of a special event or world conference, with people living with dementia stuffed later down the programme (or even last).
Or if there is a room of ten people, and one with a disparate view, the nature of joint decision making will mean that the nine will tend to make the tenth person conform to a group view. This phenomenon is well known from the studies of decision making in legal juries.
Exactly the same issues crop up again in the development of “dementia friendly communities” policy. While there are huge problems with this policy, possibly inadvertently causing division rather than true integrity and inclusion, it is possible the best we have currently both domestically and internationally. Change is often much easier from within, as Maya Angelou amongst others famously said.
NHS Improving Quality (“NHSIQ”), NHS Confederation and NHS Horizons have now a great opportunity in building on this work of “thought diversity”, building on the momentum which is thought to have begun in late 2010. Deloitte were noteworthy first movers in this field with their report, “Diversity’s new frontier” published by the Deloitte University Press.
An introduction to thought diversity on the NHSIQ website is here.
It is perhaps helpful to look at this widely shared webinar on ‘thought diversity’ which indicates the direction of travel of this in encouraging creativity and innovation in health policy.
I am struck by the true nature of the ‘rebel’. Carmen Medina (@milouness) worked for the US Central Intelligence Agency (“CIA”) for over thirty years. There she will have been exposed to how decisions are made often on an urgent basis.
There, I am sure she will have been exposed to the ‘confirmation bias’. This is a thinking shortcut (or cognitive heuristic), where you tend to arrive at decisions which best corroborate your assumptions, rather than seeking out alternative hypotheses.
Whilst one interpretation of people living with dementia being happier shoppers in the high street comprises the ‘dementia friendly community’, other versions of it emphasise that it is not friendliness as such which is critical. Such ‘friendliness’ can inadvertently become patronising, but true equality and upholding of human rights hold the key to the autonomy and dignity of people living well with dementia.
Without a real mission for implementing ‘thought diversity’, there is a real danger that captains of industry will in effect construct policy on dementia friendly communities, without any real genuine consultation, and ‘use’ their one or two representatives with dementia on key boards to confirm their bias.
And the situation is, unbelievably, worse than that. There is currently no person living well with dementia who is a regular invited member of the World Dementia Council. Once the (?first) UK general election is over on May 7th 2015, I am hoping the head of the Civil Service will give a direction to the Prime Minister to facilitate this urgently needed appointment.
I am of course hoping that my thoughts in this blogpost are not brushed under the carpet by people working for Simon Stevens, current CEO of NHS England, when he comes to review the progress of dementia policy in keeping with the ‘Five Year Forward View’, which he has indeed contributed to.
There are indeed specific ways cited within the report from Deloitte how ‘thought diversity’ can be harnessed. In their application for the improvement of dementia friendly communities, one obvious step is to seek out whole teams of people living well with dementia who are able to meet and come to opinions on crucial subjects.
People with dementia can lead on such teams, and the conflicts to be mitigated against here are within people living with dementia, who may have opposing views about what a dementia friendly community is, and the contrast in aims of dementia friendly communities between people living with dementia and people not living with dementia. But, if it works well, thought diversity can provide the sharing of knowledge, expertise, problem-solving approaches, which is thought to be aim of English policy in the next few years in dementia.
As Margaret Heffernan is reported to have said,
“Diversity, in this context, isn’t a form of political correctness, but an insurance policy against internally generated blindness that leaves institutions exposed and out of touch” ;
as Deloitte put it, institutions are prone to appearing out of touch, including senior policy wonks comprising some form of ‘ideological echo chamber’.
This is perhaps epitomised as, “a revolution from the heart” (Martin Luther King).
True equality for people living with dementia is identifiable.
Ultimately, the hope is that the policy of ‘dementia friendly communities’ is resilient enough to withstand shocks, such as high street stores going into insolvency. I strongly feel that thought diversity is a necessary management step in giving people living well with dementia a fair hearing so that they can lead.
Money is tight, but the person remains pivotal in dementia care and support
There’s no question that there is a greater number of people who are old needing to be looked after by care and support services in England.
But dementia is not simply a disease of older people, one of the critical messages of “Dementia Friends”.
Indeed, much of the budget goes into the health and care of younger people, as health technologies, say for treating cardiovascular disease through stents, get better.
The reality is there is pressure on service and the workforce simultaneously in dementia, as the Nuffield Trust and Health Foundation have argued in a sophisticated way.
Earlier in this year, in an article for ETHOS Journal “Living well = greater wellbeing”, I argued a joined up approach would now be needed to deliver a better standard of care and support for people living well with dementia.
In 2010, the UK government became among the first countries to officially monitor people’s psychological and environmental wellbeing. Academic research and policy developments have recently converged upon the notion of ‘living well with dementia’, which transcends any political ideology. This means promoting the quality of life of any person with dementia. It views each person as a unique individual and champions his or her involvement in making decisions whenever possible.
England actually leads the way with the ground-breaking ‘first mover’ exploration by academic Tom Kitwood of ‘personhood’ in the late 1980s: “It is a standing or status that is bestowed upon one human being, by others, in the context of relationship and social being. It implies recognition, respect and trust”.
It’s estimated that there are at least 800,000 people currently living with dementia in the UK. These individuals are likely to come into contact with a number of different people and services in an extensive network including carers (paid and unpaid, including family caregivers), care home staff, transport services, social housing, welfare and benefits and the police to name but a few.
I am, indeed, grateful for Paul Burstow MP’s excellent reply to my article.
The current Government in England has made substantial progress with policy in dementia in my opinion.
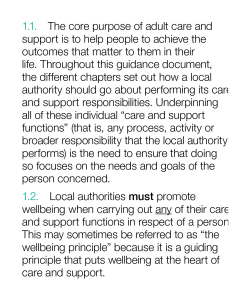
The current Care Act (2014) could not be clearer.
In the statutory guidance, the importance of wellbeing is signalled extremely strongly.
It is important for commissioners not to lose sight of this, and not to treat ‘living well with dementia’ not as a slogan but as a reality.
Helping people to live well has been a key aim of the current Government, and I hope future governments, perhaps implementing ‘whole person care’, will retain this strong focus.
Enabling people to live well leads to a fairer society. The value of people living with dementia for society cannot be denied either.
But people in power and influence have a rôle to play.
The Alzheimer’s Society has played its part in addressing stigma and discrimination through its successful ‘Dementia Friends’ campaign. I myself am a “Dementia Friends Champion”, and proud to run my sessions.
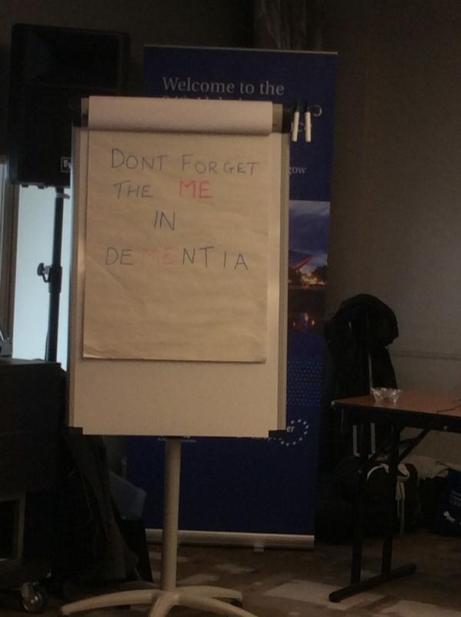
One of the key messages in this campaign is that ‘there is more to the person to the dementia’.
This message is currently a critical global one, across many jurisdictions. Here is friend and colleague Kate Swaffer with a huge banner in Australia to the same effect.
And dementia and loneliness already occur together all too often.
The wider community is essential. This is about compassion. It is also about the right people showing the right leadership.
But this should not just simply include household names, although the distress caused by lack of inclusion of people with dementia in high street shops cannot be underestimated.
This community must include all caregivers and professionals.
And central to this recognition of the role of the wider community is a new deal for carers.
As the number of people living with chronic conditions grows rapidly, so does the number of carers. There is a huge army in England currently consisting of selfless individuals giving of themselves to support a loved one.
According to Carers UK, family carers currently save the Government £119 billion every year.
Carers themselves need help.
Carers are invaluable as I discuss here.
And we need to make sure in the next Government that all paid caregivers are given a statutory minimum wage, which could also be a living wage.
We are a society which values footballers more than caregivers for people with dementia. This is simply abhorrent.
I thank the current Government for progress made in this direction, but more has to be done whoever holds office and power next year.
We need collectively to support the Dementia Action Alliance Carers Call to Action. By achieving the shared vision, the aim is to have positive impact on people with dementia and carers and improve their quality of life.
In the Dementia Action Alliance “Carers Call to Action”, carers of people with dementia:
- have recognition of their unique experience – ‘given the character of the illness, people with dementia deserve and need special consideration… that meet their and their caregivers needs’ (World
Alzheimer Report 2013 Journey of Caring are recognised as essential partners in care – valuing their knowledge and the support they provide to enable the person with dementia to live well - have access to expertise in dementia care for personalised information, advice, support and co-ordination of care for the person with dementia
- have assessments and support to identify the on-going and changing needs to maintain their own health and well-being
- have confidence that they are able to access good quality care, support and respite services that are flexible, culturally appropriate, timely and provided by skilled staff for both the carer and the person for whom they care
But we do need some sort of standards, whether aspirational or regulatory, for example?
This situation had become known to Norman Lamb by February 2013:
In light of the recent Stafford Hospital Scandal, an independent review was carried out, underlining irregularities in staff training. According to today’s BBC report, as of March 2015, UK care staff and assistants in care homes, hospitals, and private homes are to be required to complete a training certificate within 12 weeks of starting a new position.
The current UK stance is that there is no minimum standard of training. With over 1million care workers in the country, it came as alarming news to Care Minister, Norman Lamb, to discover that these untrained workers were completing skilled tasks normally undertaken by medical professionals such as taking bloods. He confirmed the responsibility for the certificate would “…rest with employers and I think that’s where the training responsibility should lie.”
I expect the next Government will wish to think about a register for paid carers to help the fight against neglectful care which can tragically happen. It can be hard to achieve a successful prosecution of ‘wilful neglect’, but likewise carers need to be able to do their job with dignity and without fear.
The broad consensus has been for some time “that the principles of person-centred care underpin good practice in the field of dementia care”. Their principles assert:
- the human value of people with dementia, regardless of age or cognitive impairment, and those who care for them
- the individuality of people with dementia, with their unique personality and life experiences among the influences on their response to the dementia
- the importance of the perspective of the person with dementia
- the importance of relationships and interactions with others to the person with dementia, and their potential for promoting well-being.
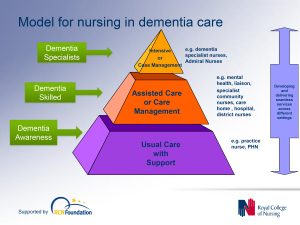
In a presentation called “Developing nursing in dementia care” in May 2014 influential expert Rachel Thompson outlined a “Commitment to the care of people with dementia in hospital settings”, calling for increase in specialist nurse roles –building evidence and supporting leaders.
I believe strongly this need has not gone away. Indeed, it is stronger than ever.
Thompson there mentions the SPACE principles to support good dementia care
Staff who are skilled and have time to care.
Partnership working with carers.
Assessment and early identification of dementia.
Care plans which are person centred and individualised.
Environments that are dementia-friendly.
The financial case for ‘Admiral nurses’, an innovation from Dementia UK, is compelling; see for example the recent report from the University of Southampton Centre for Innovation and Leadership in the Health Sciences.
As is the case from the academic and clinical nursing literature on the importance of proactive case management in avoiding admissions to hospital care.
Claims that nine in ten care homes and hospitals fail to provide the proper treatment are indeed astonishing. That particular Care Quality Commission review found widespread neglect, lack of care, poor training and failings in communication.
In the same way there can be enormous disparity between a ‘bad’ and ‘good’ care home, there can be a subtle difference between a ‘very good’ and a ‘superb’ care home.
We, one day, need to be able to celebrate the ‘outstanding’ in care homes: for example, person-centred activities or environment generally might make all the difference?
The next Government, whoever it is, will need to have the confidence to implement an organic, stakeholder-driven systemic innovation in dementia.
I have long felt that the health and care services need more than a minimum ‘protected funding’. As Roy Lilley, experienced health commentator, remarks, ‘more effort can be put into weighing the pig than actually fattening it’.
This is the danger we run if we do not place adequate resources into service provision and training.
However, even within these domains, I believe that innovation has, potentially, an important and responsible part to play (as indeed I argued in the Health Services Journal this year).
There is no question that money is tight.
But we need also to have a minimum in frontline services to maintain an adequate standard of care, as indeed is supposed to be enforced from the regulation of all clinical professions.
It is easy to jump on a ‘person-centre care’ bandwagon, but all too easily this can turn into selling courses and products for person-centred care.
Putting the person at the heart of how you behave with a person with dementia does not need to cost money. Tom Kitwood articulated it brilliantly.
But, whatever the budget constraints of the health and care and future, I believe personhood should be pivotal for living well with dementia.
This should include the whole person.
If we involve people living with dementia in the design of research and services, I feel, a lot of my concerns will be addressed. The ‘Dementia Without Walls’ project from the Joseph Rowntree Foundation, in collaboration with other stakeholders, has truly been outstanding, for example.
I am grateful to the current Government for taking us a long way down the journey. But we’ve only just begun.
Stigma in dementia poses crucial questions for dementia friendly communities
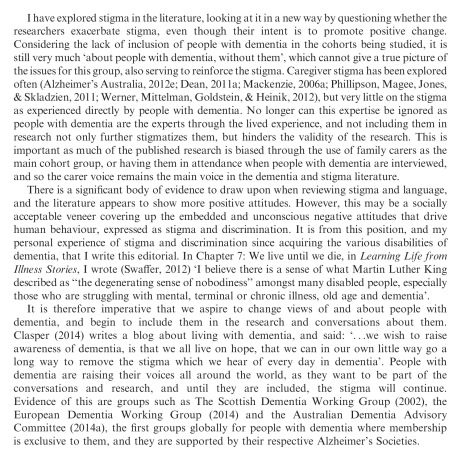
The literature on stigma is comprehensive.
But Kate Swaffer added to it beautifully in the journal ‘Dementia’, with an article today – on open access – entitled “Dementia: Stigma, language and dementia friendly”.
Kate refers to a blogpost by Ken Clasper, a Dementia Friends Champion, which asks, sensibly, what we are trying to achieve with more ‘awareness’.
And if you scroll down to the end of this tour de force on stigma and dementia, you’ll see exactly why Kate is able to opine with such legitimacy and authority.
I conceded a long time ago – in March 2014, in fact – on this blog that the policy plank of ‘dementia friendly communities’ is an incredibly complex one.
The discussion of stigma seems to be one of perpetuity. We’ve seen numerous attempts at it, including the original work of Goffman (1963) on stigma and ‘spoiled identity’.
It’s been re-incarnated as a Royal College of Psychiatrists campaign on stigma.
This morning there was another bite of the cherry.
The report, New perspectives and approaches to understanding dementia and stigma, published by the think tank International Longevity Centre UK (ILC-UK) is produced by the MRC, Alzheimer’s Research UK, and Alzheimer’s Society; it was also supported by Pfizer.
I’ve thought how I could possibly respond to Kate. And I can’t, as Kate is in every sense of the word an ‘expert’.
But it did get me thinking.
It got me thinking of the happy times I had with Chris and Jayne last week at the Alzheimer Europe conference in the city of my birth in Glasgow.
‘There’s more to the person than the diagnosis” is one of the key five messages of ‘Dementia Friends’, an initiative from the Alzheimer’s Society predominantly (and Public Health England). This is mirrored in a tweet by Chris from this morning.
Chris is also a “Dementia Friends Champion“, and lives well with dementia.
Last week, I attended a brilliant all-day workshop chaired by Karishma Chandaria, Dementia Friendly Communities manager for the Alzheimer’s Society. The progress which has been made on this policy plank is substantial, and I am certain that the next Government will wish to support this policy initiative in the English for 2015-20.
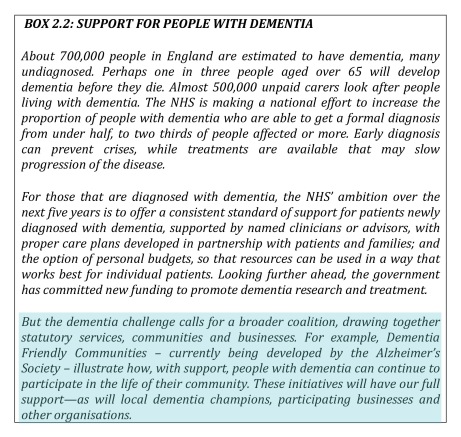
It is stated clearly in Simon Stevens’ “Five Year Plan” for NHS England.
It is a core thread of the Prime Minister’s Dementia Challenge.
And the ‘coalition of the good’ has seen the dementia friendly communities policy plank develop drawing on work from ‘Innovations in dementia’ and the Joseph Rowntree Foundation.
And to give the Alzheimer’s Society credit, where it is certainly due, there has been launched an open consultation for a British Code of Practice (currently ongoing), to which anybody can contribute.
But this code of practice does, again, have the potential to be very divisive. It might be painful to make dementia friendly communities, such as the large one in Torbay, ‘fit into this box’.
Torbay in many ways is a beacon of innovation for integration between NHS and care. There is genuine “community bind”, with citizens, shopkeepers, transport, police, for example, contributing.
The article on the BBC website about Norman McNamara (January 2012) predates the Prime Minister’s Dementia Challenge, (which started in March 2012.)
Any top down way of making bottom-up social groups ‘conform’ will be hugely problematic in the implementation of this approach to dementia-friendly communities, potentially.
The methodology of dementia friendly communities has to be truly inclusive: it is all or nothing.
I agree with Kate, and like her I wish to avoid protracted circular definitions of ‘stigma’. For me, I recognise stigma when you see it, like how the Supreme Court of the US recognises erotica and pornography as per Jacobellis v Ohio [1964].
It is possibly easier to define stigma by its sequelae, such as avoiding wishing to talk about dementia in polite conversation, or not wishing to see your GP about possible symptoms of a dementia in its early stages, or not wanting to socialise with people with dementia who happen to be in your family.
We know these are real phenomena, as demonstrated, for example, by the loneliness of many people on receiving a diagnosis of possible dementia.
And we know stigma can harbour deep-seated irrational prejudice, like the incorrect notion that dementia is somehow contagious like a ‘superbug’.
Stigma can be exhibited in pretty nasty ways in language: such as “snap out of it” or “victim”.
My discussion of whether people living with dementia are ‘sufferers’ tends to go round and round in circles with people who disagree with me.
Suffice to say, I agree it is possible for a person living with dementia, such as a person who has received a diagnosis of Lewy body dementia and who has to put up with terrible “night terrors” and exhaustion the following day.
I think if you live independently, but with full insight into your symptoms, it can be exasperating. I have never been in that position though, and it would be invidious of me to second-guess.
I think if you are close to someone in the latter stages of dementia, you can suffer.
But I’ve written about this all, indeed on this blog, before here.
The only thing that is new is Peanuts’ cartoon (original citation here).
In that workshop, I also sat through Joy and Tone Watson’s brilliant “Dementia Friends” session. Joy lives with dementia. And their session was brilliant.
This was the final ‘exhibit’.
I attended a special group session on stigma with Toby Williamson from the Mental Health Foundation during that day. In that session, it was mentioned that ‘rôle models’ of people living well with dementia might help to break down stigma.
Or maybe guidance for the media might help? One cannot help wondering if an article such as in the Daily Mail today might actually put off people from seeking a diagnosis of dementia (completely unintentionally).
But I did bring up something on my mind.
“Stigmata” literally means signs.
But dementia can be, like other disabilities, quite invisible.
Somebody might have insidious change in personality and behaviour, noticed by somebody closest to him or her, with no obvious changes in cognition (nor indeed in investigations).
I showed this in my paper published in Brain in 1999, currently also in the Oxford Textbook of Medicine.
The condition I refer to is in fact one of the more prevalent causes of dementia in the younger age group, called the “behavioural variant of frontotemporal dementia“.
If the signs are ‘visible’, then you are obliged legally to make reasonable adjustments for any disability. In England, this includes dementia under the guidance to the Equality Act (2010).
As Toby Williamson says, if you’re obliged to build a ramp for somebody in a wheelchair for a place of work, there’s an equal obligation to produce adequate signage for people who have navigation problems as a result of a dementia such as dementia of the Alzheimer’s type.
There are reams and reams of evidence on equality and the built environment (for example the Design Council or Commission for Architecture and the Built Environment).
I personally think it’s brilliant you can go into certain shops, and the customer-facing staff will, potentially, be able to recognise if a person does need time and space to pay for items.
This is also been tackled in the Scottish jurisdiction through Alzheimer Scotland.
Also, corporate lawyers should be advising large employers about the scope for unfair dismissal claims by people dismissed as they are about to arrive at a diagnosis of dementia (particularly young onset dementia).
The timeline is roughly this. Somebody has health problems – he or she is invited to leave and given a pay off – these health problems turn out to be a diagnosis of probable dementia – by this time the dismissal is not unfair.
I feel confident the ‘dementia friendly communities’ policy strand in England, and across other jurisdictions, is here to stay. I share, though, Kate’s concerns that about the relative ease with which this policy has lifted off, say, compared to how one might feel about ‘gay friendly communities’ or ‘black friendly communities’. One has to be extremely careful about any policy plank which alerts people to divisions, “them against us”.
This is what I know best as the “don’t think of elephants phenomenon” and then you think of elephants.
This policy, anyway, currently has huge momentum. Marc Wortmann is currently Executive Director of Alzheimer’s Disease International (ADI), the organisation providing a global voice for dementia and the founder of World Alzheimer’s Month. Wortmann has been instrumental in propelling dementia friendly communities to the foreground of world policy.
But, in firing up ‘dementia friendly communities’ (a term which I think is sub-optimal’), v 2.0, there is plenty of time to get it right.
‘Invisible dementia’ friends?
One of the most difficult issues in mental health is how it is very hard to do ‘outreach’ for people with certain conditions.
You can’t, as such, force people with alcohol dependence syndrome in remission or relapsing to go to support groups such as Alcoholics Anonymous.
A real issue for national policy is how there are individuals who do not wish to have a diagnosis of dementia.
Some feel that they do not memory symptoms severe enough actually to warrant a diagnostic label of dementia. And – to be fair – they could be living with a ‘mild cognitive impairment’ instead.
In an ideal world, you’d want specialist services to be able to work out whether a person is likely to be developing a dementia. This might include the appropriate thinking tests (called ‘cognitive neuropsychology’), a brain scan (such as CT or MRI), or even other investigations (such as fluid off the spinal cord, or blood tests).
Such individuals do a ‘cost benefit analysis': of thinking how much they achieve by telling their friends that they might be developing a dementia, and receiving support or medical treatment, compared to being alienated and being offered no support or treatment.
The fact is that the drugs used primarily to treat dementia do not slow progression, and can help with symptoms for earlier forms of the condition for a few months on average.
So, public health policy faces a situation where some people with dementia prefer to have their diagnostic label ‘invisible’ to others. And this is why this new public health advertisement is so intriguing.
The ad can be criticised in that it gives a very stereotyped picture of a person with dementia: old, pictured against a background of sinister music.
This ad is clearly aimed at increasing the diagnostic rates, which is ultimately one of the key factors by which The Baroness Greengross and the rest of the All Party Parliamentary Group will assess the impact of “The Prime Minister’s Dementia Challenge”.
Oddly enough, the ad says, “He’d started to forget things. It could not just have been old age”. This is one of the five messages of ‘Dementia Friends’, a Public Health initiative delivered by the Alzheimer’s Society.
However, the ad screws up in the sense that dementia does not only present with memory symptoms: in fact people with early stages of semantic dementia, primary progressive non fluent aphasia, behavioural variant frontotemporal dementia, and posterior cortical atrophy can present with plum normal memory.
This leads naturally onto another related faultline in national policy.
One of the common questions apparently asked in Dementia Friends sessions is “How can you tell a person definitely has dementia by looking at them?”
The actual answer is that you can’t.
And there are clearly ethical limitations to asking people to ‘out themselves’ in saying they are living with dementia, and as such mental health policy mostly does not engage in outreach.
So if you’re building ‘dementia friendly communities’, for the aim of embracing equality (which you have to do anyway under the law), are you somewhat ignoring diversity?
Thanks for this picture shared by Kate Swaffer.
[The picture in the top left corner is from the "Invisible Friends" project, which is something totally different.]
If no two people are the same, how can we build ‘dementia friendly communities’?
Even identical twins act differently.
This is because they are shaped by the environment in unique ways, even if they have exactly genetic sequence as the blueprint which designed them.
It therefore cannot be any surprise that no two individuals in society are in the same, as you can easily witness with the range of opinions on your timeline on Twitter.
A person with a dementia might be very different to another person with a dementia.
There are a hundred different causes of dementia, tending to affect people in different age groups in distinct ways at different rates? Let’s pick one type of dementia, the most common cause, Alzheimer’s disease.
A 83 year-old with Alzheimer’s disease might have a number of different problems, for example memory – or even with problems in planning, aspects of language, or behaviour.
And of course it’s pretty likely that 83 year-old might be living with another different condition too, such as heart disease.
Your perception of that 83 year-old might vary from your next-door neighbour, according to, perhaps, your own personal experiences of dementia, good, bad or neither.
So, in raising awareness over the uniqueness of individuals through “Dementia Friends” or “Dementia Champions”, there’s an inherent contradiction.
How do we build ‘dementia friendly communities’, given one’s desire to embrace diversity?
I have for some time explained elsewhere why I think the term is a misnomer. I don’t see the point of “asthma friendly communities” or “chronic demyelinating polyneuropathy communities”, worthy though they are.
I think when you pick off any of the ‘protected characteristics’ in the Equality Act, such as ‘disability’, ‘sexual orientation’ or ‘age’, you have to be careful about not inadvertently homogenising groups of people, worthy though the cause of ensuring that they do not suffer any unfair detriment is.
It could be that people in the early stages of Alzheimer’s disease, due to how the condition tends to affect the brain, could have particularly problems with spatial memory or navigation. Therefore, it would be desirable perhaps to have places with clear landmarks such that such individuals can navigate themselves around.
But take this situation to an extreme. Would society feel comfortable with people with dementia having their own cafés?
The story of Rosa Parks is well known.
After working all day, Parks boarded the Cleveland Avenue bus around 6 p.m., Thursday, December 1, 1955, in downtown Montgomery. She paid her fare and sat in an empty seat in the first row of back seats reserved for blacks in the “coloured” section.
The bus driver moved the “coloured” section sign behind Parks and demanded that four black people give up their seats in the middle section so that the white passengers could sit.
Rosa did not move.
A legitimate learning objective of ‘dementia awareness’ sessions is to think about what a person with dementia might or might not be able to do.
But if we then meet this learning objective, that people with dementia are all unique, we should steer away from stereotypes that people with dementia act ‘a certain way’.
This, I personally believe, is a big failing of this ‘dementia friendly communities awareness video’.
How Can We Include People With Dementia in Our Community? from NEIL Programme on Vimeo.
It’s time we talked about ‘dementia friendly communities’
This could be the video from any corporate. The point is that the video contains very familiar concepts and memes which can be marketed very easily.
I have reviewed the development of the policy of ‘dementia friendly communities’ in the penultimate chapter of my book ‘Living well with dementia’.
The description of “dementia friendly communities” given by the Alzheimer’s Society is provided as follows:
“The dementia friendly communities programme focuses on improving the inclusion and quality of life of people with dementia… In these communities: people will be aware of and understand more about dementia; people with dementia and their carers will be encouraged to seek help and support; and people with dementia will feel included in their community, be more independent and have more choice and control over their lives.”
This definition doesn’t make sense to me as it ignores networks – networks (including social networks such as Facebook and Twitter) are particularly important to those whose physical or mental health might pose formidable barriers to being physically in any one place in a community.
But when you ask “what is a dementia friendly community?” inevitably the question becomes re-articulated “what constitutes a community, and what counts as it being ‘friendly’ to ‘dementia’?”
And immediately you see the problems. How large is a community? Or put another way what constitutes the boundaries of the community? In theory, a community could be members of a part of the Lake District, or the Square Mile. Being ‘friendly’ demands the question ‘how long is a piece of string’? Without some clarity, this construct is ‘motherhood and apple pie’ and a perfect tick-box vehicle for commissioners to demonstrate that they’ve done something about “dementia friendliness”.
But simultaneously shutting down a day centre will immediately take out any feel good factor of commissioning decisions, leaving people with dementia sold down the river.
And which dementia? There are about a hundred different causes of dementia, the most common one being globally Alzheimer’s disease, characterised typically in the early stages with real problems with learning and encoding new memories (and subsequent retrieval).
So it’s conceptually possible to talk about dementia-friendly communities where you put up signage everywhere so people with Alzheimer’s Disease, who have spatial navigation difficulties, can get a bit of help.
But not all memory problems are dementia, and not all dementias present with memory problems.
But what those people with frontal dementia who have perfect memory, but who present with a slow change in behaviour and personality according to their closest ones?
How should we make communities ‘friendly’ to them?
The policy construct immediately experiences an obstacle in that it talks about ‘dementia’ as one great mass, an error previously made for ‘the disabled’. But this criticism is of course by no means fatal – as conventional communities also contain a huge range of people of all different characteristics, anyway. But is then the concept too broad as to be meaningful, such as “male friendly communities”?
Something which Kate Swaffer, an Australian who has significant experience in campaigning for advocacy for people with dementia, and who herself lives with dementia, recently shared on Twitter was this eye-catching caption.
And you see the difficulty? How do we design a ‘community’ which is ‘friendly’ to ‘dementia’, if you believe like me that once you’ve met one person with dementia, you’ve met one person with dementia?
It’s clearly impossible to legislate for someone to be ‘friendly’ to another person in a society, however loosely defined, but it is worth at least acknowledging the existant law.
You can’t have a policy that discriminates against a group of people to their detriment, with that group of people defined by a ‘protected characteristic’ under equality law in this jurisdiction. Dementia can fall under this protected characteristic definition, as legally it can come under the definition of disability; any discrimination of disabled people is unlawful.
But you can easily argue that the policy fosters a spirit of solidarity far beyond rigid compliance with the law. Such solidarity of course seems somewhat at odds with the backlash against any form of state planning from this government and previous governments.
I’ve thought long and hard about the need to try not to dismiss worthy initiatives in dementia policy. For example, whilst I am concerned about the error rates of ‘false diagnosis’ of people with dementia, I would be equally concerned if NHS England did nothing to try to identify who the undiagnosed with dementia currently are.
Likewise, my natural instinct is to think about whether the charity sector is distorted with initiatives such as ‘Dementia Friends’. According to the Government’s website, by 2015, 1 million people will become Dementia Friends. The £2.4 million programme is funded by the Social Fund and the Department of Health. The scheme has been launched in England, and the Alzheimer’s Society is hoping to extend it to the rest of the UK soon. Linking the global policy of dementia friendliness to one charity, when other similar initiatives currently exist (such as the Purple Angels, Joseph Rowntree Foundation, University of Stirling, WHO, and RSA), means that many dementia charities may get unfairly ‘squeezed’.
I do, however, intuitively and desperately wish this policy to succeed. For example, at my stall yesterday at the SDCRN 4th Annual Conference (the Scottish Dementia Clinical Research Network), a person called Hugh actually bothered coming up to me to tell me how much being a ‘Dementia Friend’ meant to him. He talked about friends of his who were ‘Dementia Champions’. He spoke with tremendous affection about his late wife had lived with dementia for eight years, and the importance of community work to him.
And it is very difficult to deny that initiatives such are this are truly wonderful.
A real concern, though, is that by conceding one is building a ‘dementia friendly community’, even with all the best will in the world, the term itself doesn’t for me suggest or promote real inclusivity. It still sadly implies a ‘them against us’. I think I have this attitude because I’m physically disabled, and I would balk at the term ‘disabled friendly community’. It’s incredibly important that this policy is not London-driven friendly communities with more than a twang of tokenism.
I am therefore leaning towards a viewpoint expressed by Simon Denegri, Chair of INVOLVE, and NIHR National Director for Public Participation and Engagement in Research:
@SDenegri “i’m not sure I know what dementia friendly communities are. I’m not sure I even like the term” #SDCRN
— shibley (@legalaware) March 24, 2014
And surely you’d want businesses and corporates to be ‘dementia friendly’? But which corporates, and why dementia? Surely you’d want them to be friendly with rare muscle wasting diseases, or cancer, for example? Shouldn’t carers get their own “carers friendly communities”?
This poses big problems for our perception of inclusive communities.
Alastair shared a lovely picture which sums up the problem for me.
@legalaware so many disability or dementia friendly ideas are also opportunities for inclusion. pic.twitter.com/72ugSoItGl
— Alastair Somerville (@Acuity_Design) March 27, 2014
You can easily see why certain corporates such as banks might wish to help out with this policy, because people with dementia can be at risk of financial abuse, but is this a genuine drive to help people with dementia or is it a pitch to secure competitive advantage like ‘ethical banking’.
Apart from isolated stories such as of dedicated no-hurry lanes in supermarkets, for example, surely one would have expected supermarkets to have pulled out all the stops with adequate signage everywhere? Many large supermarkets have about thirty lanes where it’s easy for the best of us to get lost. I don’t think I’ve ever been to a dementia-friendly supermarket where the signage would be of a good enough quality to prevent a person with mild Alzheimer’s Disease becoming spatially disoriented.
“Dementia friendly communities” lend themselves easily to ‘diversity marketing’, however. Diversity marketing is a marketing paradigm which sees marketing (and especially marketing communications) as essentially an effort in communication with diverse publics. As an acknowledgement of the importance of diversity marketing is that AT&T Inc. has a post for this discipline at vice president level. It is reported that, starting in the 1980s, Fortune 500 companies, government agencies, universities and non-profits organisations began to increase marketing efforts around diversity, according to Penn State University.
I asked my friends on Facebook whether there was anything particular ‘immoral’ about this diversity marketing in relation to dementia friendly communities, and their responses were as follows.
In other words, there is no ‘right answer’.
It’s clear to me that this policy, as it is currently being delivered, needs much greater scrutiny in terms of where the benefits have been, and for whom.
“Dementia friendly communities”: would a rose by any other name smell as sweet?
“What’s in a name? that which we call a rose
By any other name would smell as sweet”
Act II Scene 2 Romeo and Juliet William Shakespeare
“Their families and partners are also told they will have to give up work soon to become full time ’carers’. Considering residential care facilities is also suggested.”
“All of this advice is well-meaning, but based on a lack of education, and myths about how people can live with dementia. This sets us all up to live a life without hope or any sense of a future, and destroys our sense of future well being; it can mean even the person with dementia behaves like a victim, and many times their care partner as a martyr.”
“Labelling” as a sociological construct has been used to inform medical practice, since the 1960s in order to draw attention to the view that the experience of ‘being sick’ has both social as well as physical consequences.
Becker’s (1963) original work on the social basis of deviance argues that, ‘social groups create deviance by making the rules whose infraction constitutes deviance’.
Applying these ‘rules of deviance’ to individuals or groups means labelling them as ‘outsiders’. He goes on to argue that, ‘deviance is not a quality that lies in the behaviour itself, but in the interaction between the person who commits an act and those that respond to it’.
Goffman’s (1968) work is less concerned with the social process of labelling a particular action or pathological state as deviant, than with the stigmatising consequences of that process for an individual – what he referred to as ‘The management of everyday life’.
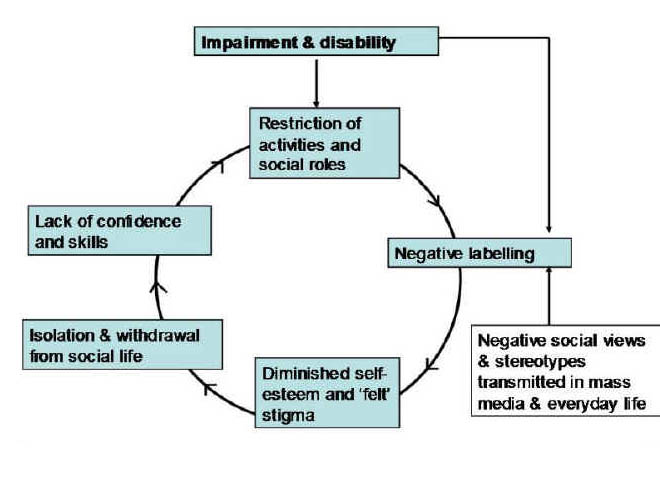
Various theories have led to a concept of a ‘stigma cycle’ [as depicted, for example, in Taylor and Field (2007)]:
I remember when an able-bdied leftie went on a diatribe on a private thread concerning how “the disabled” had been treated. Being physically disabled, however, I really got a feeling of she was talking on behalf of “us” as one large homogeneous group. I felt offended. I blocked her. I concede readily now this was a complete over-reaction.
But there’s no point being prissy or being overly-PC?
Indeed, it is said that the “dementia friendly communities” programme focuses on improving the inclusion and quality of life of people with dementia.
But using a label “dementia”, which in fairness is a commonly used term (and a medical diagnosis), runs the risk of eliminating diversity in a range of cognitive abilities.
The abbreviated Mini-Mental State Examination (1974) is the widely used ‘screening’ test for dementias, particularly those which load heavily on a memory component such as Alzheimer’s disease.
It is marked out of a maximum of 30, and a “low but normal” score is considered about 24, some feel.
And not all dementias are to do with memory problems. However, it might be more pragmatic, and potentially less stigmatic, to identify particular symptoms with which initiatives could be desired:
@legalaware @shirleyayres @julianstodd cold they be memory friendly networks? Never like defining ppl by diagnosis
— Alastair Somerville (@Acuity_Design) March 18, 2014
but one person’s problem with spatial navigation could be another person’s problem with memory… and so it goes on.
A problem here is that people who currently are ‘living well’ might resent ‘special treatment'; but the aim with equality and parity initiatives generally is to ensure that certain people are not disadvantaged and simply put on an equal footing.
In recent years, the Greek term ‘‘stigma’’ has emerged from this same risk paradigm to describe certain products, places, or technologies marked as undesirable and therefore shunned or avoided, often at high economic, social, and personal costs.
Traditionally, both distrust and avoidance of risk have been found to be more common among disenfranchised groups.
However, most people would agree that a cynical use of the ‘dementia friendly communities’ as merely a kitemark to secure business advantage, even if it encourages corporates to participate, is suboptimal.
The neighbourhood-centered definition of community still makes partial sense, even in these days of global Internet connectivity.
According to Barry Wellman, professor of sociology and the director of NetLab at the University of Toronto, once people stop seeing the same villagers every day, their communities are not groups but social networks.
“Most members of a person’s community are not directly connected with each other, but are sparsely knit, specialized in role, varying in connectivity, and unbounded (like the Internet). Like the Internet, they are best characterized as a “network of networks”.”
Wellman further argues, “In such a world, social networking literacy is as vital as computer networking literacy for creating, sustaining, and using relationships, including friends of friends. ”
And the ‘networks’ angle plugs neatly into the policy drive for technological innovations for dementia.
@legalaware @julianstodd I agree interesting to see how apps like @Streetclub @streetlife_uk & @SocialMirrorApp are connecting communities
— Shirley Ayres (@shirleyayres) March 18, 2014
Alzheimer’s Australia instead prefers the term “Dementia friendly societies”, which makes one wonder whether there’s an enormous important difference between community and society.
“Dementia friendly societies has been defined in a number of different ways; … we will be using the definition proposed by Davis et al. – a “cohesive system of support that recognises the experiences of the person with dementia and best provides assistance for the person to remain engaged in everyday life in a meaningful way”. ”
And indeed social cohesiveness has come from a number of different converging arms of evidence.
It was in recognition of the importance of community participation that the 2000 NHS Plan described a new vision for the English NHS in which “the service user is centrally placed and is required to be consulted on all matters of policy and service development”
Furthermore, in order to move beyond the ‘tokenism’ levels of participation and begin to achieve genuine citizen power, it was discussed that “users” need to feel empowered and as such have the ability and opportunity to shape the methods used for their involvement.
But inevitably issues about the name of this policy, while clearly well meant, revert to a discussion of stigma.
It is said that ‘a cure for dementia’ would be an important societal breakthrough as was the drive for a treatment for HIV/AIDS.
Stigma had stood out as a major barrier to HIV prevention and treatment services in Nigeria.A fear of different types of stigma that stand as barriers to access.
But a key lesson here was that a number of different stigmas were described in addition to community stigma – for example, self stigma, familial stigma, institutional stigma and organisational stigma surfaced as issues that influence access.
Whilst much of this analysis is clearly an academic one, whether the term itself ‘dementia friendly communities’ itself exacerbates or diminishes division in a ‘them against us’ way is worthy of some scrutiny. For what it’s worth, ‘dementia awareness’ is difficult to argue against, as it is motherhood and apple pie stuff, but whether people have an accurate working knowledge of what the dementias are, and what can be done for people with dementia, as a result of this policy is an altogether different issue. I am not so convinced about this – nor who the exact beneficiaries have been.
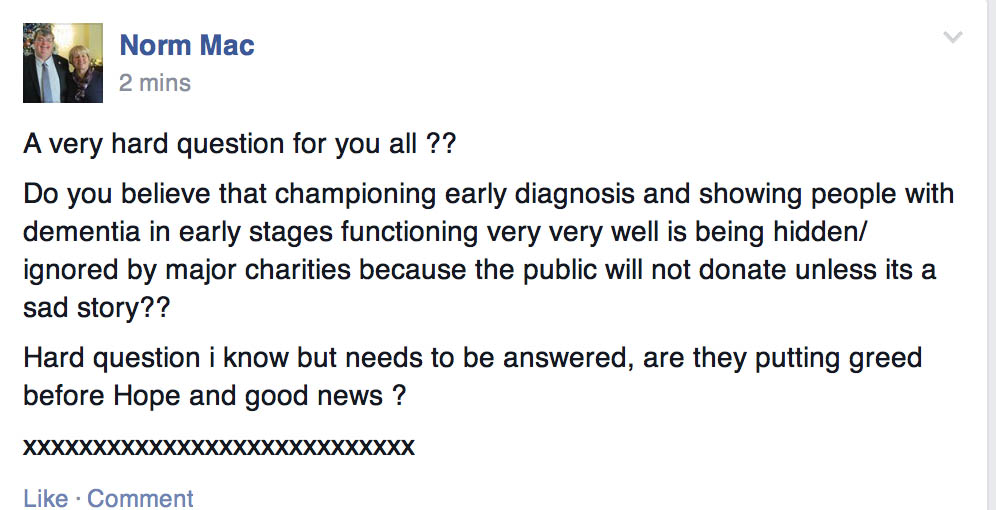
Do you think the media tries actively to hide people living very well with early dementia?
Do you think the media tries actively to hide people living very well with early dementia?
Don’t shoot the messenger, but this is effectively a question which Norman McNamara, well known campaigner and a person living with dementia, asked on a public forum as follows.
But when you think about it, you rarely get ‘success’ stories about or written by people living well with an early dementia.
This phenomenon, to be fair, might be part of a wider picture, of the media tending to focus on bad news stories, or “shocks”.
Not to generalise, but often irresponsible journalists have tended to sensationalise news stories anyway, “not letting facts get in the way of a good story”.
It is thought that there are currently about 900,000 people currently living with dementia in the UK. Some of them are living well by the law of averages?
But the question asked poses wider issues of more potential concern. Does the public need to be ‘scared’ in order to donate to a cause?
Might it be effective to use the words “bomb”, “timebomb” and “flood” to shock people into action through donation to a dementia charity?
The focus of efforts can of course be the elusive “cure”, with proponents arguing that cures for dementia have been denied resource monies compared to, for example, the cancer charities.
It can also be argued that there is a genuine shock in the story, that it would be quite inappropriate to sanitise the dementia narrative. For example, almost every week there’s a new revelation about cuts in social care.
As it happens, I had been thinking about a similar issue: on the nature of the term “dementia friendly communities”.
A friend of mine, whose mother lives with dementia, said to me: “Whenever I see that a café is ‘dementia friendly’, I get immediately reassured.”
On the other hand, another close friend of mine, living with dementia, said: “I find the concept of dementia friendly communities intensely patronising.”
When I asked her why, she said it is simply inappropriate to think of people with dementia as one huge group as they have differing needs and abilities.
Maybe the term ‘community’ is meant to reflect this diversity though?
I am physically disabled, and I have often thought about whether I would welcome a national policy called “disabled friendly communities”.
In a way, giving a whole group of people a label negates personhood and individual identity. On the other hand, criticism of the term might be overly politically correct, and one should be intuitively positive about any initiative which is inclusive for people in society?
The late Tony Benn used to explain his views on equality in terms of not forcing people to be equal. Benn argued that a more useful way to conceptualise the situation was to think of removing obstacles that made people more unequal.
But I feel the question that Norman poses is an appropriate one. If we are to embrace truly the notion of a ‘dementia friendly communities’, we need to embrace the idea too that some people with dementia are inspirational and can be leaders themselves.
The notion of presenting people living well with dementia is therefore a very important one, and to omit them from the narrative would be a very dangerous pursuit.
That is, it would be if such a pursuit were deliberate: presumption of innocence, and all that.
The BBC’s current political editor, Nick Robinson, calls this ‘bias by omission’, and, whilst we share rather different political perspectives perhaps, on this I feel Norman and Nick are together right.
A proposed use of @theRSA’s “Steer” for a behavioural change for dementia friendly communities
I am about to present to you a proposal for a change in behaviour from ‘dementia friendly communities’ to putting the boot on the other foot, persons with early dementia leading communities with their beliefs, concerns and expectations. I would be enormously grateful for any feedback on my ideas, which I’m deadly serious about it.
For example:
@elaineahpmh Wonderful blog from @legalaware http://t.co/bMUIsro7oc essential reading for #physiotalk tonight, thx shibley.
— sue parroy (@thehealthmaze) March 17, 2014
Many thanks already for these other kind remarks on Twitter:
@SHensonAmphlett @legalaware @dementia_2014 @mason4233 excellent, inspiring article 
— Pam Luckock (@luckockp) March 16, 2014
Fantastic & thought provoking article by @legalaware – Empower people with early dementia to lead: http://t.co/5wabLxC3KC via @dementia_2014
— SuzieHenson-Amphlett (@SHensonAmphlett) March 16, 2014
@legalaware @thersa @dementia_2014 it’s a very useful & thought provoking take on strengths of those with dementia – one for work Monday!
— Brian Grady (@WBC_BGrady) March 15, 2014
@dementia_2014 brilliant post. Thank you x
— Rosemary (@CarerWatch) March 16, 2014
Anyway here it is.
Introduction
It’s virtually impossible for anyone to lead on “dementia friendly communities” in a charismatic way because of the lack of clear vision so far in what a dementia friendly community is. And yet there are clearly structural fault lines in which this debate has been approached by a number of influential parties. At worst, the policy has been engulfed by commercial considerations of people seeking to make an ‘economic case’, finding clear routes by which becoming ‘dementia friendly’ can generate business or profit. The policy fundamentally has huge flaw in it currently. It treats people living with dementia as one big mass of people, with no consideration of the hundred or so different types of dementia.
Consequently, absolutely no effort is made as to considering what people with dementia can do, rather than what they can’t do. For the purposes of my leaflet, I propose further work using the foundations laid by the RSA’s “Social Brain” project in light of the #powertocreate initiatives at the heart of the RSA’s philosophy. I feel that a powerful breakthrough will be made if we can try to extend the woefully small body of work on self-s of thinking and Self in the neuroscientific literature. The current constructs of ‘dementia friendly communities’ are so bland that they might work equally well for ‘cancer friendly communities’. I also feel that if we try to allow people with early dementia a chance to harness abilities rather than disabilities, this might produce a useful entry route for collective decision making by people with early dementia.
A problem with disengagement
Ambitious, but quite pragmatic about this promise, the RSA is an organisation recently committed to the pursuit of what it called a “21st century enlightenment”. Founded in 1754 during the actual historical Enlightenment, its purpose – realised through its projects, public lectures and Fellowship activity – is to identify and release untapped human potential “for the common good” and in so doing foster a society in which citizens are more capable of acting confidently, altruistically and collaboratively.
The ultimate question for the RSA’s “Social Brain project” is whether a change in how we think of ourselves can lead to a change in our culture overall, which in turn can lead to effective responses to our shared problems. I am going to take one ‘problem’ how we encourage a sense of community in persons living well with early dementia. In the original ‘Enlightenment’, knowledge about how the world functions led to changes in the way human beings conceived of themselves. Most notably, the success of scientific knowledge led to people beginning to view themselves as not governed by divine powers, but as capable of shaping their own destinies through the power of reason. There has been a massive explosion in our understanding of the brain, and indeed the dementias. The Social Brain project is interested in how new knowledge about brains and behaviour might lead to a similarly powerful invigoration of people’s ability to shape their own destinies.
Take, for example, the life and work of Kate Swaffer regarding dementia.
Kate has clearly taken it in her own hands to shape her own destiny, campaigning on dementia. She lives with a dementia in Australia herself, and refuses to be ‘talked at’ or ‘talked about’. Her blog produces insights into living with dementia which should be compulsory reading for medical professionals who have little experience in personhood.
This is an extract from Kate’s blog.
Following a diagnosis of dementia, most people are told to go home, give up work, in my case, give up study, and put all the planning in place for their demise such as their wills.
Their families and partners are also told they will have to give up work soon to become full time ’carers’. Considering residential care facilities is also suggested.
All of this advice is well-meaning, but based on a lack of education, and myths about how people can live with dementia. This sets us all up to live a life without hope or any sense of a future, and destroys our sense of future well being; it can mean even the person with dementia behaves like a victim, and many times their care partner as a martyr.
Many of you know I have labelled this “Prescribed Disengagement”, and it is clear from the numbers of people with dementia who are standing up and speaking out as advocates that there is still a good life to live even after a diagnosis of dementia.
My suggestion to everyone who has been diagnosed with dementia and who has done what the doctors have prescribed, is to ignore their advice, and re-invest in life.
This ‘prescribed disengagement’ can be further exacerbated by any ‘dementia friendly communities’ where the key outcome is a badge or a sticker in the window, rather than ascertaining the beliefs, concerns or expectations of persons living with one of the dementias.
A growing democratic deficit with persons with early dementia?
Dementia describes different brain conditions that trigger a loss of brain function. These are all usually progressive and eventually severe. Alzheimer’s disease is the most common type of dementia, affecting 62 percent of those diagnosed. Other types of dementia include; vascular dementia affecting 17 percent of those diagnosed, mixed dementia affecting 10 percent of those diagnosed. Symptoms of dementia include memory loss, confusion and problems with speech and understanding.
What goes wrong in thinking, and the underlying problems in the brain, is now reasonably well established for the commonest form of dementia at least.
A good review is provided by Peña-Casanova and colleagues from 2012. The progression of brain pathology determines the cognitive expression of the disease. Thus, in accordance with the initial involvement of a part of the brain close to the ear medial temporal lobe, thinking changes in Alzheimer’s Disease typically start with specific difficulties in encoding and storage of new information. There is therefore quite a lot which persons with Alzheimer’s Disease can do, not of course meaning to dismiss in any way such problems with new information. A similar argument can be made for other types of dementia such as posterior cortical atrophy or progressive primary aphasia.
That persons currently living with an early dementia are not supposed to be the prime recipients of the mass of news stories about dementia is witnessed in the use of the words ‘timebomb’, ‘flood’ or ‘tide’ by influential politicians. A democratic deficit (or democracy deficit) occurs when ostensibly democratic organisations or institutions (particularly governments) fall short of fulfilling the principles of democracy in their practices or operation where representative and linked parliamentary integrity becomes widely discussed. It’s said that the phrase democratic deficit is cited as first being used by the Young European Federalists in their Manifesto in 1977, which was drafted by Richard Corbett. The phrase was also used by influential thinker Prof. David Marquand in 1979, referring to the then European Economic Community, the forerunner of the European Union.
As Dr. Jonathan Rowson puts it at the beginning of his report with Iain McGilchrist “Divided brain, divided world”, we are fundamentally social by nature:
“The notion that we are rational individuals who respond to information by making decisions consciously, consistently and independently is, at best, a very partial account of who we are. A wide body of scientific knowledge is now telling us what many have long intuitively sensed – humans are a fundamentally social species, formed through and for social interaction, and most of our behaviour is habitual.”
There’s little doubt over the broad definition of a “dementia-friendly community” as one in which people with dementia are empowered to have high aspirations and feel confident, knowing they can contribute and participate in activities that are meaningful to them. However, there is little attempt to demarcate the limits of that community, possibly unnecessary when you consider that multinational corporations are capable of using the term globally?
A lack of a wish to put people with early dementia in the driving seat in dementia friendly communities is indeed maintained by persistent references by think tanks to dementia as a “disease”, whereas policy has been firmly been moving towards considering people as individuals.
The aspiration that one might shape communities around the needs and aspirations of people living with dementia “alongside the views of their carers” tends to assume somewhat that persons with dementia and carers will have similar views and attitudes. Each community will have its own diverse populations and focus must include understanding demographic variation, the needs of people with dementia from seldom heard communities, and the impact of the geography, e.g. rural versus urban locations.
A lot of media attention has latterly gone into the notion of respectful and responsive businesses and services. An aspiration to promote awareness of dementia in all shops, businesses and services so all staff demonstrate understanding and know how to recognise symptoms is fine, provided that such ‘badges of honour’ are not consigned to leaflets which people make available passively.
If one is not careful, this policy can see an insidious strand of ‘Nudge’ invoking a nasty whiff of corporate bias in influencing consumer behaviour. For example, a member of public might start making shopping choices according to those people who haven’t accorded themselves the label of being ‘dementia friendly’. Such arrival of consumer choices by elimination is known as ‘elimination by aspects’, a highly influential theory of economist Anne Tversky whose work contributed to the Nobel Prize in Economics in 2002. Such an approach reinforces power to a top down Élite, and not putting persons with dementia at the heart of communities.
Dementia friendly communities cannot simply be about ‘Nudge’
There are some nudges that appear to actively engage individuals. For example, where choices are contextualised as public commitments, changes in behaviour tend to be more pronounced. This looks like active engagement whereby a person thinks for herself in order to change her own behaviour. But this change in behaviour is actually driven by various emotions that are triggered in the automatic system; emotional responses such as wanting to maintain one’s reputation, avoiding the shame of not sticking to one’s commitment, and wanting to appear consistent (for one’s behaviour to align with what one has said). Reputation has previously been identified by Professor Michael Porter at Harvard as a key factor through which corporates wish to prove their citizenship in ‘corporate social responsibility’.
However, it is commonly argued that “the Nudge approach” can only work on very simple behaviours: ones where the automatic system can be guided without any input from the controlled system. Very few behaviours are indeed simple enough to be influenced in this manner.
Libertarians, such as New York University Professor Mario Rizzo and California State University Northridge Professor Glen Whitman, have publicly expressed heir political reservations as concerns about nudges being “vulnerable” to becoming tools that support new, straightforwardly paternalist policies. They specifically warn that ‘nudge projects’ could grow expansively, absorb public resources, and primarily further the ends that choice architects (notably, government bureaucrats) deem valuable. At worst, this is what has happened with the mass roll-out of the corporate involvement of dementia friendly communities.
A desire by persons with early dementia to be engaged in dementia friendly communities
Norman McNamara, living with a type of dementia known as diffuse Lewy body disease, has campaigned tirelessly in raising awareness of dementia, and this work does not merit any criticism at all. I know several people who’ve drawn enormous benefit from the fact that shops are showing the ‘Purple Angel’ sign in their shop window, offering genuine reassurance. But a problem is a lack of interest by some funding bodies and politicians in giving persons with early dementia up to date information about the neuroscience and research in dementia, and encouraging feedback on such information. Involving people with early dementia is not as impressive as persons with dementia making decisions to fulfil their own plans with appropriate support. Take for example Chris Roberts’ desire to set up a café.
“There are 100s of thousands of us in the same positition with nowhere to go or nowhere to be left! We could popin for an hour or for the day. We could practically run the place our selves, some where we could chat and share, watch tv, play cards, draw, we would arrange our own activities not led by someone who thinks they know what we want! ?no one leaves till they are collected, could it be so easy, there are 1000?s of empty buildings in every major city in the uk .”
When I spoke to Chris over the phone over this, Chris reported to me that it’ll always be the case that some persons with dementia do not wish to become particularly involved in the democratic process. This of course is not particularly surprising, given that it is estimated that up to a million people will not bother voting in the UK general election to be held on May 7th 2015. Significantly, Chris is less keen himself personally to be a recipient of funding or grants, as he appreciates that involving a financial backer could immediately make him accountable to another party, diverting energy from the real purpose of this project – as community action.
Real engagement is nonetheless possible. Marian and Shaun Naidoo have been commissioned by the combined commissioning group to undertake “Connected Compassionate Communities” in Birmingham and Solihull. The overarching aim of this action research project is to improve the lives of frail older people and the people who care for them.
In the preliminary stages of this project, feedback from all stakeholders who have an interest in improving a care pathway for dementia. Marian and Shaun concluded the following:
“there is no doubt that many people have a positive experience of diagnosis and do live well with dementia. Conversations with people within this process identify concerns with regard to lack of awareness and knowledge at every stage of the pathway. This was perceived across all sectors. Many people experienced delays in diagnosis, lack of connected support and stigma. The scope for developing better services through trust and greater engagement remains.”
Asking the right questions – how much do we really know about ‘self awareness’ in persons with early dementia?
According to Ballenger (2006), a major problem lies in the very character of biomedicine, in its inability to deal adequately with uncertainty. The efforts of the medical professions have been hampered through a range of different perspectives on the nature of dementia as a ‘disease process’, the lack of an effective treatment for symptoms or preventing further progress of the disease, and the ambiguous consequences of receiving a diagnosis as far as support from the medics are concerned. Social stigma further complicates this struggle, as individuals diagnosed with dementia can often find themselves disempowered, disassociated, and excluded from social networks.
Nonetheless, despite the tremendous loss of identity that occurs over the course of a dementing illness, it is also established that a sense of Self can survive, as demonstrated by the uniqueness of each person living with a dementia (Dworkin, 1986).
In a study of individuals diagnosed with early stage Alzheimer’s disease, the common failure to recognise the individual’s continuing awareness of Self was found to lead to low expectations for therapeutic intervention, to interactions that are limited to the task at hand (such as activities of daily living). This cumulatively led to less than optimal experiences for a given level of dementia.
Clare (2003) has identified a range of responses to changes in memory function, from ‘‘self maintaining,’’ in which these persons work to maintain existing identities, to ‘‘self-adjusting,’’ in which individuals develop a new sense of self by incorporating changes into their new identity. Saunders (1998) found that “dementia patients still perform a great deal of identity construction and maintenance (p. 85).” According to Saunders, these accounts demonstrate a fluctuation in self-perception by individuals with dementia as they cope with the memory changes they experience. But clearly one should never try to inflict information about dementia to persons with dementia, if there is any risk that this might cause distress or offends autonomy in persons living with early dementia. But then it becomes a ‘catch 22’ – you need to raise awareness due to the stigma to do with dementia, but the stigma or genuine fear causes persons with dementia and caregivers wishing to engage with the science of the condition even remotely.
In this regard, Portacolone and colleagues in the journal “Aging and Mental Health” in an article entitled “Time to reinvent the science of dementia: the need for care and social integration” provide extremely useful insights.
“To rethink its basic orientation, the recent biomedical trend in dementia needs to mature out of its stage of confidence. Ballenger suggested a more self-reflective and explicitly ambivalent biomedicine – an ‘aging’ biomedicine willing to open to other fields and disciplines concerned with dementia. Along those lines, other speakers suggested we rethink the biomedical paradigm of healing and replace it with a holistic paradigm of care, empathy, as well as cultural and social integration. This reframing can be facilitated through a dialogue between biomedicine and bioethics, public health, social sciences, and the medical humanities, as illustrated by the richness and depth of the discussions generated at the workshop. To assist this reframing, we begin with a reflection on the main elements of the struggle that is compelling biomedicine to rethink its original orientation: the unsettled definition of dementia comes first, followed by the ambiguous benefits of the diagnosis, the ethical conflicts on consent and clinical trials, and finally the need to give more attention to the perspective of the person with dementia. The conclusion discusses the opportunities of a new holistic paradigm founded by a dialogue between biomedicine and public health, social sciences, medical humanities, and bioethics.”
And it could be we’re all looking at different parts of ‘dementia friendly communities’ from different viewpoints.
In the story of “The Elephant in the Dark”, the medieval Farsi-speaking poet Rumi masterfully portrayed the limitations places on beliefs by noisy sensory perception (Tourage, 2007). Late one evening, an Indian circus arrived at a village. The more curious villagers sneaked into the elephant’s stable. In absolute darkness, they made observations by touching the elephant’s body When they returned to their families, their accounts, constrained by their limited sensory experiences, gave widely divergent images of the elephant.
Rumi concluded that “light” —an external source of objective reference—is necessary for formation of reliable beliefs about the external world. Without objective reference, beliefs will be purely subjective. It is an impossible task, I feel, to look at ‘dementia friendly communities’ for persons living with an early dementia, with putting the views of those people at the heart of the decision-making process.
Public engagement with persons with dementia does not necessarily need to involve the traditional media, but it probably helps!
We currently live in a time when the scientific establishment, the government andfunding bodies, are voicing concern about the relationship between science and the public. The call is for improvements in this.
It’s interesting to try to identify where the ‘barriers to communication’ are. The media’s role in the public understanding of science has been much criticised by scientists, but it could be the case that bad dancers are in fact blaming the floor. But likewise it is perfectly possible that people ‘controlling the message’, i.e. journalists, have exerted a disproportionate top down control on what the message is. I suspect that this is precisely what has happened in the case of ‘dementia friendly communities’, where the mainstream media are used to dealing with well resourced communications departments of large charities. Nonetheless, blogs and microblogs such as Twitter have been invaluable in democratising the message.
Examinations of the professional and social forces at work reveal a high degree of collaboration and mutual reliance between scientists and journalists, even though the differences between journalistic and scientific practices can sometimes lead to unbearable disputes. The media do provide the forum in which the relationship between science and the public is pursued, and it is in this forum that the public make moral judgments about science. For example, there has recently be a tsunami of opinion pieces as to whether you’d like to have a blood test which could predict with certain accuracy your chances of developing a dementia (even though the original paper in Nature Medicine was about something rather different.)
However, despite the media’s activity in the communication of science, they have no brief or responsibility for improving the public understanding of science, and in some cases are not particularly well suited to the task. Science writers rarely ‘bend’ articles to get space in their paper, but they may emphasise aspects or use language that gives scientists the creeps. For example, the number of ‘breakthroughs which stop dementia in its tracks’ have recently been endless. These articles can often be irrelevant to most people currently living with early dementia. And yet persons with early dementia would benefit enormously from accurate information about the science of dementia?
In my opinion, there is a serious democratic deficit which could emerge between persons with dementia and researchers. I’ve heard first-hand of medical doctors not explaining the diagnosis of dementia to their patients, instead preferring to give them an ‘information pack’. Likewise, academic researchers seem all too keen to sign up persons with dementia to various research studies, without even writing to them stating the findings from the very same studies.
Human behaviour, to state the obvious, is going to be at heart of engaging any citizen. A strand of modern thinking in “citizen-centric politics” can be traced to political thinking in the wake of the Second World War—notably Hannah Arendt’s “The Human Condition” (1958). Arendt pursued a strong version of political engagement which she considered to be a profound cultural achievement rather than something emerging naturally from human nature. She regarded “citizenship” as a distinctive and consciously adopted role, played out by citizens interacting and debating in a discrete public realm in which everything “can be seen and heard by everybody and has the widest possible publicity”. These days, a public interactive website would suit that function well. It could serve as a platform with some immediacy in providing learning resources explaining in a suitable way for people with dementia with neurocognitive needs what the common dementias are, and how they typically affect thinking. If this were coupled with a blog or Twitter, the end result of a social movement could be very powerful indeed.
The concept of building a ‘communicative power’ for persons with early dementia
Some argue that ‘communicative power’ lies at the heart of the communication model of the political process. Habermas borrows the concept of communicative power from Hannah Arendt, while somewhat reformulating it. Arendt emphasises that power is always something exercised in common, not by an individual: power corresponds to the human ability not just to act but to act in concert.
During the last few decades of the 20th century, the debate on citizens’ participation in their own governance has tended to move away from the Arendtian constraints towards exploring and applying more fluid and nuanced approaches. The German critical theorist Jürgen Habermas proved a seminal influence on the debate, arguing for what he termed ‘communicative rationality’, whereby competent and knowledgeable citizens engage with one another in good faith, and through the giving (or assuming) of reasons arrive at a shared understanding about a situation.
“insofar as the democratic process, as it is institutionally organised and conducted, warrants the presumption that outcomes are reasonable products of a sufficiently inclusive deliberative process”
How can we bring about a sustainable authentic ‘behavioural change’ in allowing persons with dementia to lead in dementia friendly communities?
Nudge has clearly had its limitations, which is why the RSA has developed “Steer” through the “Social Brain” project. Drawing on a range of research from several disciplines, Steer enables people to appraise situations and make judgments about when they should trust, or be wary of, their gut instincts, rational convictions or environmental influences. The full rationale of the RSA’s articulation of “Steer” is provided in Grist (2010).
It is always extremely exciting when there is original evidence of behavioural change taking the debate forward. For example, the RSA recently a conducted a study entitled “Cabbies, Costs and Climate Change” (2011). The recommendations arising from the project as a whole are outlined in detail in their final report. They include making habitual behaviour (rather than just behaviour) the focus of interventions, making fuel efficiency a pass/fail criterion on the driving test, changing driving habitats to encourage fuel efficiency, incentivising taxi drivers to become ambassadors for fuel efficiency, providing more salient feedback, and making taxis greener.
This is an example of a beneficial behavioural change. Could such a behavioural change be effected for persons living with an early dementia?
It has previously been reported that people living with dementia face psychological and emotional barriers to being able to do more in their community, alongside physical issues. These common barriers are said to include a lack of confidence, being worried about getting lost, mobility issues and physical health issues, and not wanting to be a burden to others. It is therefore odd that there has been given such scant regard to electronic dementia-friendly communities – indeed communities run mainly by and for persons with early dementia.
For example, in the voluminous Alzheimer’s Society report “Building dementia friendly communities: a priority for everyone”, the definition of community is strikingly narrow.
“The term ‘community’, within this report, relates to the area in which people live, including the shops and cafes they visit, the places they enjoy for recreation or leisure and the wider public spaces that surround them. It can be described as the various interfaces and interactions that a person with dementia and their carers require in their locality in order to live well.”
However, the definition provided by the Joseph Rowntree Foundation in its seminal report “Creating a dementia friendly York” is considerably wider, and includes the term ‘social networks’.
“A dementia-friendly community has been described by people with dementia in this project and in others to which we have contributed as one that enables them to:
• find their way around and feel safe in their locality, community or city
• access the local facilities that they are used to (such as banks, shops,
cafés, cinemas and post offices, as well as health and social care services)
• maintain the social networks that make them feel still part of their community.”
The tone of their report is altogether different. Instead of involving people with dementia, the Joseph Rowntree Foundation talk about people with dementia “at the heart of the process”. They frame the components of their dementia friendly communities using ‘The Four Cornerstones Model’ construct.
“With the voices of people at the heart of the process, we believe that communities need to consider four ‘cornerstones’ to test the extent of their dementia friendliness.
These are:
Place – how do the physical environment, housing, neighbourhood and transport support people with dementia?
People – how do carers, families, friends, neighbours, health and social care professionals (especially GPs) and the wider community respond to and support people with dementia?
Resources – are there sufficient services and facilities for people with dementia and are these appropriate to their needs and supportive of their capabilities? How well can people use the ordinary resources of the community?
Networks – do those who support people with dementia communicate, collaborate and plan together sufficiently well to provide the best support and to use people’s own ‘assets’ well?
Collective endeavours need coordination and mutual understanding, which often takes time, effort, and experience to establish.
And yet collective decision-making is central to the wellbeing communities, towns, and city neighbourhoods. This painstaking and often divisive civic process can be especially difficult for the many towns, counties and rural areas that have little or no coverage in print media, such as a local newspaper. There is little reason to believe to think collective decision-making would fail in a supportive electronic environment such as a Wiki, for persons with early dementia.
The power of the internet and solidarity
Imagine life without the technologies many rely on every day: the computer, smartphone, #ipad, or similar. In many western cultures, we have grown so accustomed to the use of these tools for communication, discourse, and social activities that it is hard to envision us without them. By collaborating in social networks, computer users around the globe now contribute to a new way of learning. This learning allows reshaping of knowledge, information, and culture, and informs how we create and share content “between individuals, groups, and societies”.
Solidarity is a key aspect of such collaborative networks.
As the RSA point out in the report “Beyond the Big Society – Psychological foundations of active citizenship”, ‘solidarity’ is a hugely complex notion, and there is a large literature on the subject. However, the authors conclude that it is broadly about integration, about the extent to which we feel we are on ‘common ground’ with and have a sense of mutual commitment with the people with whom we share space, time and resources.
As Sarah Ammed puts it:
“Solidarity does not assume that our struggles are the same struggles, or that our pain is the same pain, or that our hope is for the same future. Solidarity involves commitment, and work, as well as the recognition that even if we do not have the same feelings, or the same lives, or the same bodies, we do live on common ground. While statistics on community cohesion (social solidarity between different cultural groups) in the UK suggest some progress in developing solidarity in our most culturally and ethnically diverse places, this progress occurred in conjunction with more than a decade of strong and sustained economic growth, low unemployment and massive investment in public services. Community cohesion could easily become a hot political and social issue as the cuts to public spending begin to bite, and competition for services and resources intensifies. For the Big Society to flourish, policymakers will need to work very hard to better understand and help develop new ways of strengthening social solidarity, particularly in our most culturally and ethnically diverse communities, where levels of social solidarity tend to be lowest and levels of multiple deprivation and social exclusion tend to be highest.”
The need for further exploratory research for the implementation of Steer: persons with early dementia
There is clearly a need to look at how the principles of ‘Steer’ could facilitate collective decision making in persons with early dementia. As part of the exploratory research, a structure as successfully implemented in research for police officers as reported in 2012 could be utilised.
Persons with early dementia will be able to produce a range of opinions as to work best for them, and it is possible that some views might fractionate according to a precise cognitive diagnosis. But that’s where the medicalisation ends. The impetus behind asking persons with dementia what they feel in relation to the world around them is a necessarily unique experience.
We could begin the process if people with early dementia decided to engage with a website providing information about dementia pitched suitably at them, making reasonable adjustments for their abilities. We could then begin to explore whether and how the principle of RSA’s “Steer approach” to behaviour might be applied in communities for people living with an early dementia.
We could then invite a larger number of people with early dementia to participate in a series of two face-face deliberative workshops. The intention was to explore Steer principles with participants, who would then experiment with applying them, and keeping diaries of their experiences, before sharing and examining these in a second workshop. This way, we could produce a rich corpus of data, which gave considerable insight into the challenges facing police and the ways in which RSA’s engaged approach to behaviour change might be able to help them better rise to these challenges.
Persons with early dementia are an important section of the public with whom we should engage over the science of dementia
It’s clearly critical for us as a society to evaluate critically, question and debate in a focused way the key issues in science and society. A large number of people in the public live successfully with an early dementia. Finding ways to illustrate the Steer principles in relation to dementia, including film-making, theatre productions, exhibitions, discussion and policy-influencing events and multimedia, could be hugely exciting.
As well as a societal and moral drive for the need to discuss the science of dementia with people with dementia, there is also potentially a legal imperative.
A “mental health condition” is considered a disability if it has a long-term effect on your normal day-to-day activity. This is defined under the Equality Act 2010. Your condition is ‘long term’ if it lasts, or is likely to last, 12 months, and ‘normal day-to-day activity’ is defined as something you do regularly in a normal day. There are many different types of mental health condition which can lead to a disability, legally; and dementia can be one of them.
There is no justification for people with dementia to be treated in an inferior way to people without, hence the purpose of the discrimination legislation in England and Wales. It’s important to appreciate that for the greatest part of our history, the political, social and economic life of most societies were controlled by a single nobility “held in place.” Those outside the elite who questioned this monopoly on power would suffer various unpleasant penalties. On the other hand, creativity is essential to change our society for the better. And, in fact, there is a large body of evidence to highlight that persons with dementia can be incredibly creative, But, if we, as a society, only tap into an elitist pool of creativity then we impede our own ability to tackle the myriad of problems we face. Politics, sadly, is the very opposite of creativity. Politics, as it is currently conceived, is inherently elitist, and corporate-like charities may have agendas with politicians which are consequently at odds with the persons with dementia they appear to seek to involve.
Conclusion: a ‘power to create’ something unique
In relation to the strong ethos of ‘power to create’, which many argue William Shipley, founder of the RSA, would have signed up to, Anthony Painter covers this beautifully in his blogpost “We need to talk about power” from 8 January 2014:
“Morozov argues that the nature of political community matters. The institutional structure matters if you want the power to create to be really dispersed rather than concentrated. That’s why we need to talk about power, its form, the ethos that seeks to deploy it, and its purpose: our purpose as individuals who wish, need, and should create.”
I feel passionately a power to create a medium in which persons with early dementia can think about their own Self, based on a genuine engagement with individuals over the current neuroscience of dementia, will be a critical start. I think, armed with this knowledge, people can be armed with the tools as to how best to go about making decisions.
This is as much as giving persons with dementia “a voice”, in as much as befriending them in large numbers important though that is. The ‘communicative power’ of an electronic website, providing resources on the neuroscience of dementia and tools for people with dementia to engage with ‘Steer’, I think could bring about an important behavioural change in not just ‘involving’ people with early dementia – but also making sure they ultimately lead in their own communities.
References
Alzheimer’s Society (2013) Building dementia friendly communities: a priority for everyone.
Arendt, H. (1958) The Human Condition, University of Chicago Press: Illinois, p. 50.
Ballenger, J.F. (2006) Self, senility, and Alzheimer’s disease in modern America: A history. Baltimore, MD: Johns Hopkins University Press.
Clare, L. (2003) Managing threats to self: Awareness in early stage Alzheimer’s disease, Social Science & Medicine, 57, pp. 1017–1029.
Dworkin, R. (1986). Autonomy and the demented self, The Milbank Quarterly, 64(2), pp. 4–16.
Grist, M. (2010) Steer: Mastering our Behaviour through Instinct, Environment and Reason, RSA: London.
Habermas, J. (1984) (translated McCarthy, T.), The Theory of Communicative Action, Beacon Press: Boston, 1984.
Joseph Rowntree Foundation (2012) Creating a dementia-friendly York. Accessible at: http://www.jrf.org.uk/sites/files/jrf/dementia-communities-york-full.pdf (viewed 15 March 2014).
Portacolone, E., Berridge C., Johnson, K, Schicktanz, S. (2014) Time to reinvent the science of dementia: the need for care and social integration, Aging Ment Health, 18(3), pp. 269-75.
London Arts and Health Forum. (2014) Connected Compassionate Communities: An Action Research Project, West Midlands – deadline 13 July. Accessible at: http://www.lahf.org.uk/connected-compassionate-communities-action-research-project-west-midlands-deadline-13-july (viewed 15 March 2014).
Painter, P. (2014) Blogpost: “We need to talk about power” Accessible at: http://www.rsablogs.org.uk/2014/enterprise/talk-power/ (viewed 15 March 2014).
Peña-Casanova J1, Sánchez-Benavides G, de Sola S, Manero-Borrás RM, Casals-Coll M. (2012) Neuropsychology of Alzheimer’s disease. Arch Med Res, 43(8), pp. 686-93.
Roberts, C. (2014) Blogpost: “Immediate day care rant”vAccessible at: http://mason4233.wordpress.com/2014/03/08/intermediate-day-care-rant/ (viewed 15 March 2014).
Rowson, J., Lindley, E. (2012) RSA Projects: reflexive coppers: adaptive challenges in policing, RSA: London.
Rowson, J, McGilchrist, I. (2013) RSA Projects: Divided brain, divided world, RSA: London.
Rowson, J, Young, J. (2011) RSA Projects: Cabbies Costs and Climate Change, RSA: London.
Rowson, J, Mezey, M.K., Dellot, B. (2012) RSA Projects: Beyond the Big Society – Psychological foundations of active citizenship, RSA: London.
Saunders, P. A. (1998) ‘‘My brain’s on strike’’: the construction of identity through memory accounts by dementia patients, Research on Aging, 20(1), 65–90.
Swaffer, K. (2014) Re-investing in life after a diagnosis of dementia. Accessible at: http://kateswaffer.com/2014/01/20/re-investing-in-life-after-a-diagnosis-of-dementia/ (viewed 15 March 2014).
Thaler, Richard H.; Sunstein, Cass R. (2008). Nudge: Improving Decisions about Health, Wealth, and Happiness, Yale University Press.
Tourage, M. (2007). Rumi and the hermeneutics of eroticism. Leiden, The Netherlands: BRILL. doi:10.1163/ej.9789004163539.i-260.
UK Government. When a mental health condition becomes a disability Accessible at: https://www.gov.uk/when-mental-health-condition-becomes-disability (viewed 15 March 2014).
Wellcome Trust website. Public engagement Accessible at: http://www.wellcome.ac.uk/funding/public-engagement/ (viewed 15 March 2014).
Nudge, dementia friendly communities and consumer behaviour
Should companies be looking to make money out of the concept of ‘dementia friendly communities’ and should charities be using this concept to position themselves against their competitors? If we’re not a nation of shopkeepers, we might be increasingly becoming a nature of consumers rather than citizens. With the promise of unified personal budgets, this consumer-oriented nature of healthcare is likely to gather some momentum. But the relentless drive towards consumerism, I feel, does threaten to play havoc with this policy plank.
As a useful starting point, I feel it’s helpful to consider the work of ‘dementia friendly York’, led the Joseph Rowntree Foundation to propose a model for realising a dementia-friendly community. With the actual voices of people at the heart of the process, they believe that communities need to consider four ‘cornerstones’ to test the extent of their dementia friendliness.
These are:
- Place – how do the physical environment, housing, neighbourhood and transport support people with dementia?
- People – how do carers, families, friends, neighbours, health and social care professionals (especially GPs) and the wider community respond to and support people with dementia?
- Resources – are there sufficient services and facilities for people with dementia and are these appropriate to their needs and supportive of their capabilities? How well can people use the ordinary resources of the community?
- Networks – do those who support people with dementia communicate, collaborate and plan together sufficiently well to provide the best support and to use people’s own ‘assets’ well?
I have in fact mentioned this in the penultimate chapter of my book ‘Living well with dementia’ available in all good bookshops.
But the way the corporates wish to play this policy I feel has more than a slight twang of ‘Nudge’ about it. “Nudge: Improving Decisions about Health, Wealth, and Happiness” was, of course, the highly publicised book written by Richard H. Thaler and Cass R. Sunstein from the Chicago Law School.
At the heart of nudge theory is the concept of “nudge“. This was originally defined by Richard Thaler and Cass Sunstein as follows:
“A nudge, as we will use the term, is any aspect of the choice architecture that alters people’s behavior in a predictable way without forbidding any options or significantly changing their economic incentives. To count as a mere nudge, the intervention must be easy and cheap to avoid. Nudges are not mandates. Putting fruit at eye level counts as a nudge. Banning junk food does not.”
One of the main justifications for Thaler’s and Sunstein’s endorsement of libertarian paternalism in “Nudge” draws on facts of human nature and psychology.
Sunstein and Thaler use their notions of nudges within the context of choice architecture to propose policy recommendations that they believe are in the spirit of libertarian paternalism. They have recommendations in the areas of finance, health, the environment, schools, and marriage.
I feel that “nudge” has somehow diffused through the ecosystem of ‘dementia friendly communities’ in a rather unhelpful way through the influence of corporate citizens. Thaler and Sunstein believe these problems in decision-making can at least be partially addressed by improving the choice architecture.
They cite ‘daylight saving time‘ – when you “change the label of the time on the clock” when the clocks go backwards as a simple ‘nudge’ with the effect of changing behaviour. Indeed, uring his time as an American envoy to France, Benjamin Franklin, author of the proverb, “Early to bed, and early to rise, makes a man healthy, wealthy and wise”, anonymously published a letter suggesting that Parisians economize on candles by rising earlier to use morning sunlight. This 1784 satire proposed taxing shutters, rationing candles, and waking the public by ringing church bells and firing cannons at sunrise. There is apparently ‘no such thing as a neutral policy’?
The way in which this initiative is presented at all is interesting. If we’re talking about “nudge”, we’re talking about ‘libertarian paternalism’. Libertarian paternalism is the idea that it is both possible and legitimate for private and public institutions to affect behavior while also respecting freedom of choice. Private organisations can use ‘nudge’ on their own, but can of course be vicariously applied through private organisations. Private organisations and the Department of Health are currently implementing “Dementia Friends” – a wide-ranging scheme, with good motives.
To help ‘nudge’ succeed in various guises, it helps if influential people are there somewhere. The current Prime Minister David Cameron, launched the plank of the global dementia friends policy plank as the branded ‘Dementia Friends’, which is led by the Alzheimer’s Society. Through this people will be given free awareness sessions to help them understand dementia better and become Dementia Friends. This is also led by ‘top influencer’ Jeremy Hughes, the current CEO of the Alzheimer’s Society.
The scheme aims to make everyday life better for people with dementia by changing the way people think, talk and act. The Alzheimer’s Society wants the Dementia Friends to have the know-how to make people with dementia feel understood and included in their community. It is hoped that, by 2015, 1 million people will become Dementia Friends. The £2.4 million programme is funded by the Social Fund and the Department of Health.
To help to implement this policy, quite heavily promoted by parliamentarians, the ‘bandwagon effect’ will help – and this is known of course to Thaler and Sunstein. The general rule is that conduct or beliefs spread among people, as fads and trends clearly do, with “the probability of any individual adopting it increasing with the proportion who have already done so”. As more people come to believe in something, others also “hop on the bandwagon” regardless of the underlying evidence.
Or people could join ‘dementia friends’ through simple “peer pressure”. People are heavily influenced by the actions of others. Sunstein and Thaler cite a famous study by Solomon Asch where people, due to peer pressure, answer certain questions in a way that was clearly false (such as saying that two lines are the same length, when they clearly are not).
First of all, it’s helpful to say we’re not talking where people necessarily make deep active decisions to join ‘Dementia Friends’. We’re not even talking about the Joseph Rowntree Model of “The Four Cornerstones”. I’m applying my analysis to how a member of the public, for the purposes of interacting with a high street chain offering involvement with this initiative, might behave as a ‘consumer’.
The simplest example of a successful nudge in the “choice architecture” of Nudge is the default option. A default option is simply what happens if you do nothing. Normally, nothing happens, but sometimes even when you do nothing, something happens. (Choice architecture describes the way in which decisions may (and can) be influenced by how the choices are presented (in order to influence the outcome.)
The latest incarnation of this initiative is that our high streets, from the end of February 2014, have set to become more dementia friendly following a commitment from major British businesses. It’s said that, thanks to the Alzheimer’s Society and the Department of Health, our high streets are set to become more dementia friendly following a commitment from major British businesses: Argos, Homebase, Marks and Spencer, Lloyds Pharmacy and Lloyds Banking Group.
This is of course interesting in the context of how consumers make decisions about with whom to shop. Firms will be competing, and becoming “dementia friendly” could be a way of simplifying the process of customer behaviour or choice.
The well known “elimination by aspects”, described in the “Nudge” book, is followed by decision makers during a process of sequential choice and which constitutes a good balance between the cost of a decision and its quality. At each stage of decision, the individuals eliminate all the options not having an expected given attribute, until only one option remains. This short cut was first used by Anne Tversky (1972).
For example, “I want to buy a kettle from a catalogue?” Do I choose Argos or Catalogue R Us, if I want to choose a dementia friendly supplier? Answer: Argos.
And the Alzheimer’s Society have not been the only ones making use of the application of this choice architecture. The end of February 2014 was also big for the Torbay Dementia Action Alliance. Apparently now in Torquay and Babbacombe you probably can spot “purple angel sticker”s in a fair number of shop windows.
But the real important question to ask: who is benefiting here exactly?
While nudges can appear desirable when judged from a short-term perspective, in which they are assessed primarily in terms how effectively they steer behaviour, they can appear problematic from a long-term perspective that renders the process of decision-making rather infantile and primitive.
Libertarians, such as New York University Professor Mario Rizzo and California State University Northridge Professor Glen Whitman, have publicly expressed heir political reservations as concerns about nudges being “vulnerable” to becoming tools that support new, straightforwardly paternalist policies. They specifically warn that ‘nudge projects’ could grow expansively, absorb public resources, and primarily further the ends that choice architects (notably, government bureaucrats) deem valuable. At worst, this is what has happened with the mass roll-out of the corporate involvement of dementia friendly communities.
It’s also mooted that the nudge approach can only work on very simple behaviours: ones where the automatic system can be guided without any input from the controlled system; for example, placing a picture of a pair of eyes above an honesty box for coffees and teas can increase payments because people feel on some unconscious level ‘watched’. A voluntary choice to shop with a particular supplier because of a ‘dementia friendly’ emblem is a pretty basic low-level decision, so it’s anyone guess whether ‘nudge’ is indeed appropriate or not.
Also, veering for the ‘nudge’ approach may be taking the wind from the sales of other valid approaches, such as ‘Steer’ from the Royal Society of Arts, Commerce and Entreneurship. Four example, reduction of dementia friendly communities in this specific scenario for the market place could opt a citizen in the general public from engaging with critical pillars of progressive politics which indeed promote a genuine sense of dementia communities and leadership, viz:
- Autonomy – citizens need to be able to take control of their own lives in order to achieve their fullest potential wherever this is possible.
- Responsibility – citizens need to be capable of playing their part in ensuring common goods such as a clean environment and trusting social relationships.
- Democratic engagement – citizens need to be able to view forms of governance (whether national or local) as open to them and as reflecting their interests.
- Communal action – citizens need to have ways and means of negotiating and collaborating with one another over achieving common goods and dealing with shared problems.
(RSA Steer Report)
I believe it’s important for people to look at what the principles which guide their own behaviour. This might genuinely involve embracing the philosophy of living well with dementia – or not. And reducing the marketplace into those companies which are dementia friendly or not may benefit the companies more than members of the public, when it comes to the basic issue of people ‘understanding dementia’. Of course, it will be argued that the dementia awareness programmes are currently wide ranging. But I think we have to set our ambitions a lot higher than tokenistic dementia friendliness, important though that the policy is (of befriending), and go much more to the heart of ‘The Four Cornerstones’ model.
Turning ‘dementia friendly communities’ as ‘nudge’ on the high street doesn’t do anything for me.