Home » Posts tagged 'Dementia Action Alliance'
Tag Archives: Dementia Action Alliance
Money is tight, but the person remains pivotal in dementia care and support
There’s no question that there is a greater number of people who are old needing to be looked after by care and support services in England.
But dementia is not simply a disease of older people, one of the critical messages of “Dementia Friends”.
Indeed, much of the budget goes into the health and care of younger people, as health technologies, say for treating cardiovascular disease through stents, get better.
The reality is there is pressure on service and the workforce simultaneously in dementia, as the Nuffield Trust and Health Foundation have argued in a sophisticated way.
Earlier in this year, in an article for ETHOS Journal “Living well = greater wellbeing”, I argued a joined up approach would now be needed to deliver a better standard of care and support for people living well with dementia.
In 2010, the UK government became among the first countries to officially monitor people’s psychological and environmental wellbeing. Academic research and policy developments have recently converged upon the notion of ‘living well with dementia’, which transcends any political ideology. This means promoting the quality of life of any person with dementia. It views each person as a unique individual and champions his or her involvement in making decisions whenever possible.
England actually leads the way with the ground-breaking ‘first mover’ exploration by academic Tom Kitwood of ‘personhood’ in the late 1980s: “It is a standing or status that is bestowed upon one human being, by others, in the context of relationship and social being. It implies recognition, respect and trust”.
It’s estimated that there are at least 800,000 people currently living with dementia in the UK. These individuals are likely to come into contact with a number of different people and services in an extensive network including carers (paid and unpaid, including family caregivers), care home staff, transport services, social housing, welfare and benefits and the police to name but a few.
I am, indeed, grateful for Paul Burstow MP’s excellent reply to my article.
The current Government in England has made substantial progress with policy in dementia in my opinion.
The current Care Act (2014) could not be clearer.
In the statutory guidance, the importance of wellbeing is signalled extremely strongly.
It is important for commissioners not to lose sight of this, and not to treat ‘living well with dementia’ not as a slogan but as a reality.
Helping people to live well has been a key aim of the current Government, and I hope future governments, perhaps implementing ‘whole person care’, will retain this strong focus.
Enabling people to live well leads to a fairer society. The value of people living with dementia for society cannot be denied either.
But people in power and influence have a rôle to play.
The Alzheimer’s Society has played its part in addressing stigma and discrimination through its successful ‘Dementia Friends’ campaign. I myself am a “Dementia Friends Champion”, and proud to run my sessions.
One of the key messages in this campaign is that ‘there is more to the person to the dementia’.
This message is currently a critical global one, across many jurisdictions. Here is friend and colleague Kate Swaffer with a huge banner in Australia to the same effect.
And dementia and loneliness already occur together all too often.
The wider community is essential. This is about compassion. It is also about the right people showing the right leadership.
But this should not just simply include household names, although the distress caused by lack of inclusion of people with dementia in high street shops cannot be underestimated.
This community must include all caregivers and professionals.
And central to this recognition of the role of the wider community is a new deal for carers.
As the number of people living with chronic conditions grows rapidly, so does the number of carers. There is a huge army in England currently consisting of selfless individuals giving of themselves to support a loved one.
According to Carers UK, family carers currently save the Government £119 billion every year.
Carers themselves need help.
Carers are invaluable as I discuss here.
And we need to make sure in the next Government that all paid caregivers are given a statutory minimum wage, which could also be a living wage.
We are a society which values footballers more than caregivers for people with dementia. This is simply abhorrent.
I thank the current Government for progress made in this direction, but more has to be done whoever holds office and power next year.
We need collectively to support the Dementia Action Alliance Carers Call to Action. By achieving the shared vision, the aim is to have positive impact on people with dementia and carers and improve their quality of life.
In the Dementia Action Alliance “Carers Call to Action”, carers of people with dementia:
- have recognition of their unique experience – ‘given the character of the illness, people with dementia deserve and need special consideration… that meet their and their caregivers needs’ (World
Alzheimer Report 2013 Journey of Caring are recognised as essential partners in care – valuing their knowledge and the support they provide to enable the person with dementia to live well - have access to expertise in dementia care for personalised information, advice, support and co-ordination of care for the person with dementia
- have assessments and support to identify the on-going and changing needs to maintain their own health and well-being
- have confidence that they are able to access good quality care, support and respite services that are flexible, culturally appropriate, timely and provided by skilled staff for both the carer and the person for whom they care
But we do need some sort of standards, whether aspirational or regulatory, for example?
This situation had become known to Norman Lamb by February 2013:
In light of the recent Stafford Hospital Scandal, an independent review was carried out, underlining irregularities in staff training. According to today’s BBC report, as of March 2015, UK care staff and assistants in care homes, hospitals, and private homes are to be required to complete a training certificate within 12 weeks of starting a new position.
The current UK stance is that there is no minimum standard of training. With over 1million care workers in the country, it came as alarming news to Care Minister, Norman Lamb, to discover that these untrained workers were completing skilled tasks normally undertaken by medical professionals such as taking bloods. He confirmed the responsibility for the certificate would “…rest with employers and I think that’s where the training responsibility should lie.”
I expect the next Government will wish to think about a register for paid carers to help the fight against neglectful care which can tragically happen. It can be hard to achieve a successful prosecution of ‘wilful neglect’, but likewise carers need to be able to do their job with dignity and without fear.
The broad consensus has been for some time “that the principles of person-centred care underpin good practice in the field of dementia care”. Their principles assert:
- the human value of people with dementia, regardless of age or cognitive impairment, and those who care for them
- the individuality of people with dementia, with their unique personality and life experiences among the influences on their response to the dementia
- the importance of the perspective of the person with dementia
- the importance of relationships and interactions with others to the person with dementia, and their potential for promoting well-being.
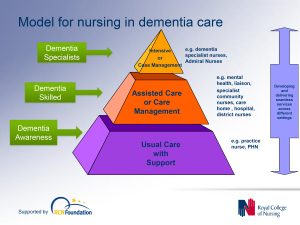
In a presentation called “Developing nursing in dementia care” in May 2014 influential expert Rachel Thompson outlined a “Commitment to the care of people with dementia in hospital settings”, calling for increase in specialist nurse roles –building evidence and supporting leaders.
I believe strongly this need has not gone away. Indeed, it is stronger than ever.
Thompson there mentions the SPACE principles to support good dementia care
Staff who are skilled and have time to care.
Partnership working with carers.
Assessment and early identification of dementia.
Care plans which are person centred and individualised.
Environments that are dementia-friendly.
The financial case for ‘Admiral nurses’, an innovation from Dementia UK, is compelling; see for example the recent report from the University of Southampton Centre for Innovation and Leadership in the Health Sciences.
As is the case from the academic and clinical nursing literature on the importance of proactive case management in avoiding admissions to hospital care.
Claims that nine in ten care homes and hospitals fail to provide the proper treatment are indeed astonishing. That particular Care Quality Commission review found widespread neglect, lack of care, poor training and failings in communication.
In the same way there can be enormous disparity between a ‘bad’ and ‘good’ care home, there can be a subtle difference between a ‘very good’ and a ‘superb’ care home.
We, one day, need to be able to celebrate the ‘outstanding’ in care homes: for example, person-centred activities or environment generally might make all the difference?
The next Government, whoever it is, will need to have the confidence to implement an organic, stakeholder-driven systemic innovation in dementia.
I have long felt that the health and care services need more than a minimum ‘protected funding’. As Roy Lilley, experienced health commentator, remarks, ‘more effort can be put into weighing the pig than actually fattening it’.
This is the danger we run if we do not place adequate resources into service provision and training.
However, even within these domains, I believe that innovation has, potentially, an important and responsible part to play (as indeed I argued in the Health Services Journal this year).
There is no question that money is tight.
But we need also to have a minimum in frontline services to maintain an adequate standard of care, as indeed is supposed to be enforced from the regulation of all clinical professions.
It is easy to jump on a ‘person-centre care’ bandwagon, but all too easily this can turn into selling courses and products for person-centred care.
Putting the person at the heart of how you behave with a person with dementia does not need to cost money. Tom Kitwood articulated it brilliantly.
But, whatever the budget constraints of the health and care and future, I believe personhood should be pivotal for living well with dementia.
This should include the whole person.
If we involve people living with dementia in the design of research and services, I feel, a lot of my concerns will be addressed. The ‘Dementia Without Walls’ project from the Joseph Rowntree Foundation, in collaboration with other stakeholders, has truly been outstanding, for example.
I am grateful to the current Government for taking us a long way down the journey. But we’ve only just begun.
You need risk to live well with dementia
“Risk” is one of those entities which bridges the financial world with law and regulation, psychology or neuroscience. The simplicity of the definition of it in the Oxford English Dictionary rather belies its complexity? 
It was a pivotal part of my own Ph.D. in the early diagnosis of the behavioural variant of frontotemporal dementia, awarded by the University of Cambridge in 2001. I was one of the very first researchers in the world to identify that ‘risk seeking behaviour’ is a key part of the presentation of many of these individuals, against a background of quite normal other psychological abilities and investigations including brain neuroimaging scans.
‘You need to break eggs to make an omelette’ is one formulation of the notion that you have to be able to make mistakes to achieve an overall goal. That particular sentence is, for example, used to convey the way in which you might have to put up with ninety nine turkeys before striking gold with one truly innovative idea. ‘Nothing ventured nothing gained’ is another slant of a similar idea. Interestingly, this phrase is often attributed to Benjamin Franklin. Franklin has an established reputation of his own as a ‘conceptual innovator‘.
It’s also a very interesting policy document on risk in dementia from the UK Department of Health, from 10 November 2010, a really useful contribution. This guidance was commissioned on behalf of the Department of Health by Claire Goodchild, National Programme Manager (Implementation), National Dementia Strategy. The guidance was researched and compiled by Professor Jill Manthorpe and Jo Moriarty, of the Social Care Workforce Research Unit, King’s College London.
Prof Alistair Burns, England’s clinical lead for dementia, has written a very focused and relevant Foreword to this piece of work. Here Alistair is, pictured with me earlier this week at the Dementia Action Alliance Annual Conference hosted in Westminster, London (“DAA Conference”). The event was a positive celebration of the #DAACC2A, “Dementia Action Alliance Carers’ Call to Action”, which embodies a movement where, “carers are acknowledged and respected as essential partners in care, and are supported with easy access to the information and the advice they need to assist them in carrying out their role.”
Risk enablement, or as it is sometimes known, positive risk management, in dementia involves making decisions based on different types of knowledge. However, people living with dementia and caregivers, quite often an eldest child or spouse, can handle risk in different ways. I feel that understanding living well with dementia is only possible through understanding the background to a person living with dementia, and his or her interaction with the environment. I’ve indeed written a comprehensive book on it, and I am in the process of writing a second book on it, which brings under the spotlight many of the key stakeholders, I believe, who contribute to “dementia friendly communities”.
Risk enablement is based on the idea that the process of measuring risk involves balancing the positive benefits from taking risks against the negative effects of attempting to avoid risk altogether. For example, the report cites the example of the risk of getting lost if a person with dementia goes out unaccompanied needs to be set against the possible risks of boredom and frustration from remaining inside. There are clearly various components of risk which might affect a person living with dementia. Risk engagement therefore becomes a constructive process of risk mitigation, an idea highly familiar to the law and regulation through the pivotal thrust of ‘doctrine of proportionality‘, that legislation must be both necessary and proportionate.
Risk enablement, it is argued, goes far beyond the physical components of risk, such as the risk of falling over or of getting lost, to consider the psychosocial aspects of risk, such as the effects on wellbeing or self-identity if a person is unable to do something that is important to them, for example, making a cup of tea. Therefore, the report proposes that “risk enablement plans” could be drawn up which summarise the risks and benefits that have been identified, the likelihood that they will occur and their seriousness, or severity, and the actions to be taken by practitioners to promote risk enablement and to deal with adverse events should they occur. These plans need to be shared with the person with dementia and, where appropriate, with his or her carer or caregiver. Thus advancing the policy construct of ‘personalisation’ offering choice and control, risk assessment tools are envisaged by the authors to help support decision making, and should include information about a person with dementia’s strengths and of his or her views and understanding about risk. Risk could apply to making a cup of tea, or going for a walk. We know that people living with dementia handle risks in different ways. For some people, a person living with dementia excessively walking beyond a local jurisdiction might be a known problem. For all the different causes of dementia medically, and for all the different ways in which individuals react to a dementia at different stages of the condition, a person can live with dementia in a sharply distinctive way.
Risk therefore in a hugely meaningful and substantial way has moved away from the “safety first” circles? And it fundamentally will depend on how an unique person living with his or her dementia embraces the environment in reality.
The idea that you need risk to live well with dementia is brought into sharp focus here by Chris Roberts, a friend of mine, speaking at the DAA Conference. I have recently begun to take risks in a highly enjoyable game for my #ipad3, which Chris indeed introduced me to, called, “Real Racing 3″. Here, Chris also talks about the crass way in which he was originally told his diagnosis, and lack of information about his condition given at the time of diagnosis. Therefore, Chris, I feel, brings into sharp focus a number of problem areas, which hopefully Baroness Sally Greengross and colleagues will address in a new five year strategy for England for 2015-20.
In “Big Dementia”, who cares about dementia carers?
Without the work of unpaid carers, the formal care system would be likely to collapse. Some feel that the State gets a “very good deal” out of this current system. The ongoing support from unpaid carers will be a particular issue for the care system in the future, as changing demographic patterns, shifts in family composition, labour force participation and increased geographical mobility will affect the availability of the unpaid care workforce. There are also significant issues emerging in care work.
It can be argued that some carers in dementia, whether unpaid carers or paid care workers, are perceived rather unfairly by society, and this is a matter of real national concern. The issue of researching personalised medicines, and pooling clinical drug trial data, across a number of different jurisdictions, is a curiously international phenomena. It feeds into the ‘big is better’ narrative, which is of course a key aspect of why large multinational companies like ‘Big Data’. But converting our response to dementia to a solution for Big Pharma is not solely the answer. The answer is not simply ‘Big Dementia’, much as that might be attractive for the corporates. It is just as crucial to consider who cares about dementia carers. The two are not necessarily mutually exclusive of course. In an ideal world, we should like to offer the best care for people with dementia, as well as effective symptomatic treatment as well as a cure. However, it’d be a disaster if we could hold our hands up, and say that we could in all reality offer neither. As the international economies recover after the global financial crash, caused by the effects of poor global regulation of securitised mortgage products, it might seem fitting that the international landscape can be tweaked to make dementia profitable for Big Pharma. However, it is clear that our own national parliament, in the recent ‘dementia care and services’ debate on 7 January 2014, wishes to have a frank and sincere debate about who cares for the carers. As a society, this is dependent on economics within our control. If people need to talk about about the ‘cost’ of dementia relentlessly, there might be an equal and opposite need to talk about the value of carers; and this needs to be a national debate.
The usual tired mantra from politicians would of course be trotted out, particularly from those of a certain political inclination, that as the economy improves our living standards will improve. But it has been a concern of all main political parties that living standards for the many are not expected to rise as the economy recovers. In this jurisdiction, there’s a particular phenomenon of how the very wealthy seem to have been relatively immune from the global financial crash. This ‘cost of living crisis’ has been partly attributed to big corporates colluding legally to maintain prices to promote shareholder dividend rather than customer value. In England, the Health and Social Care Act (2012) was legislated by the current government to promote a quasi-market in the NHS in England. The aim was to introduce competition, bolster an economic market regulator, and to produce a mechanism for fast managed decline of ‘failing’ NHS Foundation Trusts. Clinical commissioning groups (CCGs) and health and wellbeing boards were also introduced new parts of the NHS in England. CCGs plan and buy local health services, while health and wellbeing boards influence the local decisions that shape health, public health and social care. In this new political and socio-economic landscape, it has been particularly striking, but encouraging, that the shared vision of the “Dementia Action Alliance” is of an England and Wales where the health and wellbeing of carer of a person with dementia are of equal priority to those of the person for whom they care. Ideally, for competition to thrive, it should not be in the hands of a few corporates and corporate-like charities, but all stakeholders should be given a fair slice of the action.
The wellbeing of carers of dementia in England is related to both its national economy and law, and this is something which is not within the powers of the G8 arena. In keeping with previous Conservative governments, George Osborne has warned that “self-defeating” increases to the minimum wage could “cost jobs”, and John Major, the Prime Minister 1990-7 had argued strongly the dangers of the national minimum wage. Many of the same arguments are likely to resurface as the UK Labour Party will undoubtedly raise the importance of the “living wage”, prior to the general election to be held on May 7th 2015. Cabinet ministers including Business Secretary Vince Cable and Work and Pensions Secretary Iain Duncan Smith are reportedly pressing, currently, for an “above-inflation rise” of 50p or more. Mr Osborne said he too wanted to see the £6.31 hourly minimum wage rise, but he said it should be left to the Low Pay Commission to set the appropriate level.
As Norman Lamb said in the parliamentary debate the other day, “We ask carers to do some of the most difficult work that one can ever imagine but the rewards and the training and support they get is minimal.”
An emerging political consensus has promisingly emerged that “we can never get good care on the back of exploiting very low-paid workers”, as Lamb put it. It turns out that carers are currently paid the national minimum wage if they are lucky. That is, of course, a breach of the minimum wage legislation. According to an authoritative study Dr Shereen Hussein, of King’s College London, estimates that there are between 150,000 and 220,000 care workers in this position. And this is using conservative assumptions – the real number could be higher. The flouting of national minimum wage has, however, become alarmingly widespread. There are a variety of employment practices that result in the minimum wage being circumvented, the most common of which is when councils sign contracts with private providers who recruit staff to provide short slivers of care in the home. A quarter of an hour can be all that a care worker gets to wash, change, feed and talk to someone with dementia. Dignity for the client is often the first casualty: a variety of groups representing the vulnerable, as well as some of the more scrupulous employers, fear that rushed care contracted by the minute often means inadequate care. Previous findings suggest almost half of councils still set 15 minutes as their minimum time slot.
Furthermore, many paid care workers are on zero-hours contracts. Unison’s ethical care charter aims to put an end to poor pay and working conditions in home care services. Under the charter, for example, Islington council has agreed to implement the charter’s main principles of getting rid of zero hour contracts, ensuring travel time is counted in employees’ paid hours and implementing the London living wage, as well as setting up occupational sickness schemes. Islington, alongside Southwark council, has been an early adopter of the recommendations put forward by Unison in the their report into home care. Published in 2012, the report found that good carers were being lost to “easier jobs that pay more, like in supermarkets” after finding themselves unable to support their family on an inadequate and unreliable salary.
Many paid care workers also do not get paid for travelling between the appointments they undertake, but clearly care workers must be paid when they are travelling from one home to another. Furthermore it is common for remuneration systems to pay only pay per minute actually spent with clients, not the travel time between them. Dozens of these work-related journeys could be made each week as it’s a core part of the job. Not being paid for this time means those who care don’t get paid for a full day’s work.
It is also important for councils commissioning care work to be absolutely clear with those they contract with that they expect total compliance with the law. If a council is commissioning in a way which almost becomes complicit in a breach of the law, that is completely unacceptable. On the other hand, NHS Wiltshire has commissioned an “outcomes based continuing healthcare service” designed to improve quality, reduce cost and link up with social care – but which completely restricts patient choice. The “Help to Live at Home” service has been commissioned jointly with Wiltshire Council. Contracts for the £23m service. The provider a patient receives will depend on where in the county they live. All health and social care services will be delivered by that provider and payment will depend on achieving a set of agreed outcomes.
There is a big difference between “care workers” and “unpaid carers”. A phenomenon worth keeping an eye on is that of “family caregiving” which has been on an upward trend in various jurisdictions, in part due to the economic recession. Some families lack the financial capabilities to pay professional caregivers. In fact, a huge group of carers comprise the “unsalaried family caregivers”. Family caregivers of people with dementia, often called the “invisible second patients”, are critical for people living with dementia. The effects of being a family caregiver, can be both positive and negative, with high rates of burden and psychological morbidity as well as social isolation, physical ill-health, and financial hardship. Indeed, it is mooted that comprehensive care of a person with dementia can include building a partnership between all health professionals and family caregivers. Many family caregivers of people with dementia might also employed, of whom many have reported that they missed work; a proportion may have even that turned down promotion opportunities or given up work to attend to caregiving responsibilities. There is furthermore no doubt that the benefit system is confusing, and it had been hoped that universal credit would be a method of simplying that. If you care for someone with dementia, you are normally advised to check that you are both getting all the benefits and tax credits you are entitled to. For example, you may be able to claim Personal Independence Payment or Attendance Allowance for the person with dementia, and Carer’s Allowance for the carer. You, or the person you look after, may be entitled to a discount on your council tax. Again, the situation can be complicated, and many people get simply put off from applying for the benefits for which they could be entitled due to sheer complexity and/or lack of guidance.
So, how will we eventually know when carers are being looked after? We will hear that carers of people with dementia are confident that their own health and wellbeing needs and requirements are recognised and supported, so that no carer feels alone, and are given regular breaks. This is in keeping with how local and national guidance for working time should be implemented anyway. Carers of people with dementia are also recognised as essential partners in care, assuming an approach which could be best called “coproduction”. Furthermore, carers of people with dementia would also have access to expertise in dementia care for information, advice, support and co-ordination of care. The “Dementia Action Alliance” has been the coming together of over 800 organisations to deliver the National Dementia Declaration; a common set of seven outcomes informed by people with dementia and their family carers. The Declaration provides an ambitious and achievable vision of how people with dementia and their families can be supported by society to live well with the condition
It would be incredibly valuable to have carers have a voice on CCGs and health and wellbeing boards, especially since commissioners are supposed to be promoting wellbeing pursuant to the Care Bill currently being discussed in the House of Commons and the House of Lords. The demands of caring for someone with dementia are great and many carers say they feel totally unsupported. How to include unpaid care workers in this commissioning debate is undoubtedly a difficult issue, but one which simply cannot be ultimately parked for convenience.
“Big Dementia” may not provide all of the answer, unless care is combined with cure.
#G8summit: Hazel Blears MP (@HazelBlearsMP) praises patients and carers, and calls for research into living well with dementia
On Thursday 28 November 2013, MPs debated the G8 summit on dementia. The debate was chosen by the Backbench Business Committee following a representation from Tracey Crouch. The application for debate was also sponsored by Hazel Blears and Paul Burstow.
This discussion, by parliamentarians, was in fact a very fair and balanced consideration of the practical issues facing the contemporary scene of dementia.
A lot has hopefully moved on from the attitude that, “Dot has gone a bit dotty”.
Diagnosis of the dementias is only part of the story.
The subsequent ‘treatment’ and ‘cure’ for dementia have been actively debated, but this parliamentary debate acknowledged that we have come on ‘leaps and bounds’ for enabling individuals with dementia potentially to live positively with dementia.
There’s clearly a complex parapluie of factors at play here. Does a current lack of cure for dementia lead to more stigma, or does stigma contribute to a current lack of cure for dementia?
The UK is leading the discussion of dementia for the G8, but embarrassingly does not have a strategy yet for 2025 compared to some of its international colleagues.
There has been an increase in investment in dementia research, but this has come from a very low base, representing less than 1% of the annual science budget. It is hoped that this budget will increase, including funding for prevention as well as quality-of-life and wellbeing.
A great thing about this debate was its acknowledgement that not all dementia is Alzheimer’s disease; this is crucial for us to consider how best to allocate monies for research into other types of dementia too, such as the frontotemporal dementias.
Another brilliant aspect was an appreciation that there needs to be support for carers, for avoidance of ‘crises’ – including support for the ‘Dementia Action Alliance’ – in the run-up to the #G8 dementia and beyond.
You can watch this excellent debate here.
Hazel Blears (@HazelBlearsMP) is the Labour MP for Salford. Her submission to the #G8 debate, as provided in Hansard, is as follows. Hazel is well known to be a ‘champion’ for dementia.
Hazel Blears (Salford and Eccles) (Lab): It is a great pleasure to follow the hon. Member for Chatham and Aylesford (Tracey Crouch), my colleague on the all-party group. It is also a great pleasure to see you in the Chair, Madam Deputy Speaker. This is my first opportunity to contribute to a debate under your chairmanship, and I would like to congratulate you on your election.
While I am handing out congratulations, I would like to congratulate the Prime Minister, too, on the personal commitment he has shown on dementia. [Interruption.] Credit where it is due. Those who have the presidency of the G8 have an opportunity to name a subject around which they would like to mobilise the international community. In playing his card at the G8, the Prime Minister has chosen dementia. I commend him for taking that action. I believe that international collaboration will be the way to achieve the next big leap forward, particularly on the research agenda. I support what the Prime Minister said at Prime Minister’s questions yesterday—that this issue is not a matter only for world leaders, important though they are; it is a matter for every single person in the community, whether they be a world leader, a health Minister or an ordinary citizen. Everybody has a role to play.
I shall start with the people who have dementia, along with their families and their carers. When we promote policy, do collaboration or talk about international research, we must constantly remind ourselves that the people with the disease and their carers and families are usually the most expert people in the system. Therefore, the services that we provide, the quality of care and the innovations we develop have to be shaped and guided by those people. We must empower them to make their voices heard in this debate. When we bring together our creativity, our imagination and the huge brain power in the research community, we must always bring to this issue, too, our own humanity. We must remember that people with dementia are valuable and loved human beings. If we can keep that at the forefront of our minds, we will make progress and be doing absolutely the right thing.
During Question Time yesterday I mentioned a lady called Joy Watson. I met her a little while ago. She is only 55, but she has early-onset dementia. Her family was devastated. When she went into shops, she might be a little confused over her change or what she needed to order, and the shops—and sometimes the customers—would be irritated with her, tutting and asking her to hurry up. She took to wearing a badge, which she designed herself, saying “I have got Alzheimer’s; please be patient with me”. She should not need to do that. Nowadays there is a scheme—I think it is called the purple angel scheme, and Joy is promoting it—so that people can wear a purple angel on their T-shirts as a means of raising awareness in every single part of our community.
In Salford, we have worked on this agenda for a number of years. We have just formed our dementia action alliance, with 30 organisations now committed to action plans to make us, I hope, the first dementia-friendly community in Greater Manchester. As well as health, education and housing bodies, we have the Lowry arts centre and our shopping centres included in the scheme. I think we have the first private-hire taxi firm in the country to be involved in this, Mainline Sevens taxis. It has trained 400 drivers and has an account system so that people with dementia do not have to fiddle with their money when they get in a taxi. All those groups are now dementia aware. That shows the really practical things that can be done.On the research side, I am delighted to say that tomorrow, Salford university will launch the Salford Institute for Dementia, bringing together the faculty of health and social care with departments dealing with the built environment, computers, IT, arts and media—showing the multidisciplinary approach that will apply. That group will draw together and disseminate research on living well with dementia. I think this is a fabulous academic development.
Hazel Blears therefore congratulated the Prime Minister for choosing dementia as a topic he wished to talk about.
It is noteworthy that patients themselves and their carers are the most expert in these complex conditions, and their voices must be heard.
Few will disagree with this.