Home » Posts tagged 'care'
Tag Archives: care
Party politics may be failing the NHS and care, but democracy isn’t
There is a sense of the ‘unfinished revolution’ as Philip Gould might have put it. UK politics perhaps feels like ‘work in progress’, or ‘just in time’, to borrow management speak.
The pre-match build up has been quite exhilarating. The seleb nature of politics is exemplified that Alex Salmond is still box office despite Nicola Sturgeon being the head of the party. And that Ed Miliband wants a knock-out with David Cameron, even though David Cameron doesn’t wish to attend the weigh-in.
I have for ages railed against the consumerist nature of politics, thinking that you have to road test and focus group your offerings. It is often joked that John Major MP’s government was the first New Labour government, but here we see the seeds of a policy which has become quite controversial – the private finance initiative.
Whilst ‘PFI’ has undoubtedly helped to rebuild a physical infrastructure for the NHS which is to be welcomed, there’s no doubt that it is an accounting trick of sorts, and has a ‘buy now pay later’ feel for it.
Previous Labour and Tory governments have not been good at managing the negotiations for PFI, and it is the taxpayers who ultimately lose out.
Anyway, the lack of pay increases in the nursing profession nor the number of acute NHS Trusts in deficit did not warrant a mention in George ‘You’ve never had it so good’ budget speech.
Who really runs Britain? This is a question that Robert Peston, son of a Labour peer, asked not so long ago. The problem is that, as far as the NHS is concerned, we are not being given much of a choice.
We’re being given no choice about the implementation of personal budgets. We’re being given no choice about PFI loan repayments. We’re being given no choice about the £20 billion ‘efficiency savings’ aka cuts.
The ultimate in exercise of democracy is supposed to be your vote. The late Tony Benn made a great play of the fact all of us could exercise a democratic vote, even if we did not have sufficient money to buy influence as in corporate lobbying.
But this vote is only as good as the choice on offer. We are presently not being given a choice as to whether we would pay more taxes to see social services not cut to the bone.
Many of us feel that we were not given much choice about the eye watering contracts which were shunted across to the private sector in the lifetime of previous governments.
There remains a dearth of skilled opinions and ‘thinking’ about the NHS aside from some exceptional independent people. There remains no skilled socialist health association apart from a small body of middle-old age people who do not generate policy in a democratic manner and who have little influence on any of the political parties.
Only platforms, it seems such as ‘Our NHS’, are able to put their neck over the parapet, but I feel this is not enough. I feel some sympathy for the National Health Action Party, which is able to take the bull by the horns; but even they will be the first to admit they will have to fight hard to get elected representatives in parliament.
I would like to be able to support something such as the NHS Reinstatement Bill, for example I would love to see somebody responsible for the running of the NHS, but my humblest submission is that another top down reorganisation of the NHS would be traumatic.
But we would be deluded to expect that another reorganisation of some sort is unlikely. The change required in combining health and care, even if it is cost neutral somehow, cannot be labelled as anything other than ‘radical’.
Rather like being a consumer for music, however, I prefer making up my own soundtrack on Spotify, rather than buying whole albums. However, there aren’t any tracks from UKIP which I am interested in.
Party politics, I believe, are failing the majority of people in Britain. There seems to be little link between what people want and what people actually get, irrespective of ‘broken promises’, and this appears to be especially the case now for the NHS and care.
For example, the Liberal Democrats are now unashamedly campaigning on mental health when their cuts, albeit implemented locally, have seen social care truly on its knees.
The ultimate farce will be when a sizeable number of SNP MPs are weighed up against Labour losses, to see whether the Tories, UKIP, the Democratic Unionist Party, Greens and National Health Action Party can provide a ‘government of minorities’ to form a government.
It may not even be a coalition, nor ‘supply and confidence’ – it might simply be vote by vote.
And are we expected to run the NHS on the basis of this?
“Living better” with dementia is desirable, but what does it mean for care?
After having thought about it for more than one year, I’ve concluded that the term ‘living well with dementia’ is not the right one. For a start, it implies some objective, sometimes unattainable, standard. Also, I feel that some people are clearly not well with dementia with the dreadful state of post-diagnostic care and support in some parts of the country, or personal symptoms which are difficult to manage (not living well with dementia from a lack of ability to communicate verbally, or intense ‘night terrors’). Each person living with dementia is more than the dementia, and I am mindful of not projecting an over sanitised portrayal of the dementias.
Somebody I truly admire in her work and general campaigning on dementia is Beth Britton. Beth has already made a huge impact in the co-production group at the CQC, and will, I am sure, make a massive impact on the Carers’ Commission. Having founded D4Dementia in May 2012, the blog was a finalist in the Roses Media Awards 2012 and has developed a huge following in the UK and internationally. The blog is genuinely loved and supported by thousands of families, carers, people with dementia, health and social care professionals, policy makers, leaders and anyone looking for a highly informative, personal and authoritative perspective on dementia.
I will publish my book ‘Living better with dementia: looking to the future’ later this year (around June – July 2015) with Jessica Kingsley Publishers. I feel that this book, although adopting both a domestic and international viewpoint, fits in very nicely with Beth’s corpus of impressively high quality work.
Chapter 1 provides an introduction to current policy in England, as it currently stands, including a review of the need for a ‘timely diagnosis’ as well as a right to timely post-diagnostic care. This has been a vocal concern of Baroness Sally Greengross, the current Chair of the All Party Parliamentary Group for dementia.
In England, the issue of the ‘timely diagnosis’ is an exquisitely sensitive one.
We’re lucky Beth, Ming Ho and Sal Marciano have contributed to this debate: viz:
Other carers, Beth Britton, Sally Ann Marciano and Ming Ho contributed their experience emphasising that support is essential and that good outcomes for the whole family, in addition to those of the person with dementia, should be taken into consideration.
This chapter also provides an overview of the current evidence base of the hugely popular “Dementia Friends” campaign run very successfully by the Alzheimer’s Society and Public Health England, to raise awareness about five key ‘facts’ about dementia. It was intended that this campaign should help to mitigate against stigma and discrimination that can be experienced by people living with dementia and their caregivers. The ‘proof of the pudding’ will come when the outcome of turning communication into action is assessed objectively.
Chapter 2 comprises a preliminary analysis of stigma, citizenship and the notion of ‘living better with dementia’. This chapter explains the urgency of the need to “frame the narrative” properly. This chapter also introduces the “Dementia Alliance International” group, which has fast become a highly influential campaigning force by people living with dementia for people living with dementia.
It is hoped that openness in discussion will help to mitigate against a deeply entrenched stigma by some.
Beth advises, in the Huffington Post, that:
As Margaret Thatcher joins the many people with dementia who have passed before her, and debates rage about her political legacy, I would argue that this is a time to talk as openly about her most recent experiences as it is to reflect on her career. An opportune moment for us all to think about what having dementia means, whether you are a former prime minister, a doctor, a professor, a grocer, a bus conductor or a refuse collector. Dementia brings a whole new meaning to being ‘all in this together’.
Chapter 3 looks at the various issues facing the timely diagnosis and post-diagnostic support of people living with dementia from diverse cultural backgrounds, including people from black, Asian and ethnic minority backgrounds, people who are lesbian, bisexual, gay or transsexual, and people with intellectual difficulties. Attention is paid to the various intricate ways in which exact culture can impact not only on the timely diagnosis of dementia but also in the post-diagnostic care.
Chapter 4 looks at the issue of how different jurisdictions around the world have formulated their national dementia strategies. Examples discussed of countries and continents are Africa, Australia, China, Europe, India, Japan, New Zealand, Puerto Rico and Scotland. There is remarkable convergence in the efforts of various jurisdictions, and it is here I first introduce the critical importance of collaboration. A major plus here has been the contribution of the Alzheimer’s Disease International in their work on the need for national dementia policies, and how to implement them.
Chapter 5 looks at the intense care vs care debate which has now surfaced in young onset dementia. There is a potentially problematic schism between resources being allocated into drugs for today and resources being used to fund adequately contemporary care to promote people living better with dementia. An example is discussed of how the policy of ‘Big Data’ had gathered momentum across a number of jurisdictions, offering personalised medicine as a further potential component of “person-centred care”.
This chapter also considers the impact of the diagnosis of younger onset dementia on the partner of the person with dementia as well. It can never be considered that a diagnosis is given in isolation:
As Beth remarks,
For us, devoid of any additional support or resources, we simply had to learn about dad’s dementia as it progressed, inevitably making mistakes along the way, but always trying our best to understand what his life was like and what he needed. Through the work I do now, I aim to use that knowledge to improve the lives of all those who are touched by dementia, increasing awareness and education in society as a whole, and transforming the care given to people with dementia and their families.
A candid description in my book was also given about the possible sequelae of the diagnosis of young onset dementia on employment, caregivers, and in social isolation.
Chapter 6 focuses on delirium, or the acute confusional state, and dementia. It attempts to explain why delirium and dementia might converge in policy, after all. There are general issues of whether it is possible to inject incentives into the system at critical points. However, in parallel with this, there is an active debate as to why delirium (however so labeled) is not picked up sometimes in hospital, why people who experience an episode of delirium can do quite badly in the long run, and what to do in the special case of a person living with dementia with delirium superimposed on that.
Chapter 7 is the largest chapter in this book, and takes as its theme care and support networks. I make no apologies about the length of this chapter, as I have been hugely influenced by the Dementia Action Alliance Carers Call to Action in the last year.
Beth comments that:
Most carers are totally unprepared for what caring will involve and have no idea when their caring role will end. They often ‘fall into’ caring, simply by taking on small responsibilities that escalate, triggering experiences that untrained family carers can find very difficult to cope with.
There is huge interest internationally in the subject of ‘what makes a good care home’, as Beth comments:
For me the gold-standards that every family should be looking for from a care home are person-centred care, compassion, dignity and respect. You want to know that your loved one will be treated as an individual in every possible aspect – not just another box to tick on a care plan. You also want to know that they will have access to anything and everything that constitutes therapeutic dementia care, and not just a range of set ‘activities’ that they have no interest in participating in.
The idea of families and professionals working side by side is a very powerful one.
Beth takes this idea up here:
This shows that when families and professionals work side-by-side it often creates a unique, and holistic, model of care. Relatives can also benefit from the support and knowledge that professionals caring for their loved one can provide in challenging times.
It should never be the case that those who have spent years being educated in their subject feel that their clinical training and evidence based approach carries greater weight, or that families adopt the viewpoint that their emotional ties and personal experience is all that is needed to effectively care for their loved one.
In my book, an overview of how patient-centred care is different from person-centred care is given, and how person-centred care differs from relationship-centred care. I feel, personally, that the literature has thus far excessively focused on the ‘dyadic relationship’ between the person with dementia and caregiver, but a need to enlarge this to a professional in a ‘triangle of care’ and extended social networks was further elaborated and emphasised.
Different care settings are described, including care homes, hospitals – including acute hospital care, and intermediate care. This chapter first introduces the critical role of clinical nursing specialists in dementia in providing proactive case management in a person-centred care philosophy.
However, Beth is right, in my opinion, to bring up the notion that “care homes are not police states“; rather care homes could be open to scrutiny whilst being part of an extended community.
Britton has her suspicions about the events that led to this crisis, but she is unable to prove them. Based on that experience, she supports the idea of CCTV in care home rooms on an opt-in basis: “A camera might not have saved his life, but it would have told us what happened. However, I don’t think they should be put everywhere for everyone. We don’t want to turn care homes into a police state.”
Chapter 8 considers eating for living well with dementia. This chapter considers enforceable standards in care homes, including protection against malnutrition or undernutrition. The main focus of the chapter is how people with dementia might present with alterations in their eating behaviour, and how the mealtime environment must be a vital consideration for living better with dementia. Eating well with dementia is clearly not all about finger snacks and the such like.
Chapter 9 looks at a particular co-morbidity, incontinence. Focusing on the various co-morbidities will be an opportunity of a whole person approach for a person living with dementia, during health as well as illness. The emphasis of this chapter is on conservative approaches for living well with dementia and incontinence. Other issues considered here are the impact of incontinence on personhood per se, and the possible impact on the move towards an institutional home.
Incontinence for a person living well with dementia is not all about pads. We have to, as a society, wish to talk about incontinence for people living with dementia, and I am hoping this chapter is a help.
I feel Beth has been instrumental – in her work – in breaking down societal taboos, for example:
How do you feel about the idea of needing someone to dress you, wash you, help you to the toilet or change your incontinence pads, feed you, give you medication, move you around, and enable you to watch the TV programmes of your choosing or listen to the music that you love?
This is day-to-day life for the many people who receive care. Such dependence can happen at any age, but it becomes more likely as you get older, making the need for care something people fear the most as they approach their mature years.
Chapter 10 argues how the needs for people living better with dementia would be best served by a fully integrated health and social care service in the form of “whole person care”. This chapter provided the rationale behind this policy instrument in England. This chapter argues how the needs for people living better with dementia would be best served by a fully integrated health and social care service. Currently too many NHS patients cannot be discharged out of social care in a timely fashion.
We certainly do need to be looking forward to the future now.
As Beth says,
In 15 years’ time we must have a health and social care system that is (finally) fully integrated. The UK should be leading the way in providing aged care, and recognising and fully supporting the role of family carers. More broadly, I want to be living in a society that makes ageing something we embrace and nurture, not something to be sneered at, marginalised and locked away.
Chapter 11 considers the importance of the social determinants of health. The framework, I argue, is eminently sensible for organising one’s thoughts about dementia friendly communities. The focus of this chapter is housing. I focused on design of buildings in my previous book ‘Living well with dementia’, but I wished to articulate here the wider context of the importance of housing for a person living well with dementia. Housing for living well with dementia is not just about buildings, and is pivotally enmeshed with the person centred care philosophy of projected English policy.
With such a broad brush tool as equality and “dementia friendly communities”, the scope for squashing diversity is enormous. Few topics enter the realms of “one glove does not fit all” to the same degree as the potential use of global positioning systems for dementia. Chapter 12 considers whether ‘wandering’ is the most appropriate term. The main emphasis of this chapter is the legal and ethical considerations in the use of ‘global positioning systems’ in enhancing the quality of life of persons with dementia and their closest ones. A central theme of this chapter is what might be best for the piece of mind of the person in a caring role might not be entirely synchronous as the wishes of the person himself or herself with dementia. To show how extreme the term “wandering” potentially becomes, I am aware of some friends of mine living with dementia who simply wish to go for a pleasant walk, but are frightened of being labeled as “wanderers”.
Chapter 13 considers head-on a number of important contemporary issues, with a main emphasis on human rights and “rights based approaches”. While there is no universal right to a budget, the implementation of personal budgets is discussed. This policy strand is indeed very complex. The chapter progresses to consider a number of legal issues which are arising, including genetic discrimination in the US jurisdiction, dementia as a disability under the equality legislation in England, and the importance of rights-based approaches for autonomy and dignity.
Nonetheless, “personalisation” remains a powerful strand in policy across many successive governments.
As Beth notes – in an apolitical way:
The first and most important thing to stress is that everyone is an individual, so what works for one person won’t work for another. True quality of life is only achieved through personalisation, therefore it is vital that everything you help someone with dementia to do, achieve or enjoy is what they have or would choose for themselves.
Too often the debate about dementia can be engulfed in a diatribe about ‘cost’ not ‘value’. Persons living better with dementia wish to contribute effectively with the outside world, and the feeling is mutual. Chapter 14 is primarily concerned with art and creativity, which can be incredibly empowering for some people trying to live better with dementia. This chapter takes as its focus on how living with dementia could lead to art and creativity. This chapter also looks at the exciting developments in our understanding of the perception of music in people living with dementia, and why music has the potential to enhance the quality of life for a person living well with dementia through its intrinsic features as a reward.
Too often the focus in international policies is on medications.
I believe the interest in ‘reminiscence’ is very well deserved.
Beth describes it thus:
Dad’s room was filled with pictures, cushions depicting farmyard scenes and life-like soft toy animals – everything chosen because it told some part of his story. At the heart of that was dad’s memory box displaying captioned photographs charting dad’s life from his birth to mine, alongside emblems that represented his home county and favourite football team.
All of these reminiscence therapies combined to keep dad’s identity alive, much in the same way that resources like Memory Bank can do for people who are living with dementia today. These aids help to focus on the uniqueness of the individual, and provide focal points for conversation that ensure each person’s story is brought to life.
Chapter 15 looked at the triggering of football sporting memories in people living well with dementia. This chapter considers the cognitive neuroscience of the phenomenon of this triggering, and presents a synthesis of how the phenomenon could be best explained through understanding the role of emotional memory in memory retrieval, how autobiographical memories are represented in the human brain usually, the special relevance of faces or even smells such as “Bovril”. The triggering of football memories may have some neuroscientific commonalities with the triggering of musical memories, and it will be interesting in the future to identify carefully which people living better with dementia benefit from such reminiscence approaches.
Chapter 16 looks at the impact of various innovations in English dementia policy, giving as examples including service provision (such as the policy on reducing inappropriate use of antipsychotics or the policy in timely diagnosis) and research. This policy goes through the current evidence for this evidence in particular detail, and considers how culture change may be effected internationally for quality in this policy area. This chapter tries to convey the complexity of the issue, and to explain in a fair way why deep down in this policy plank are traditional concerns to do with ‘continuity of care’ and ‘valid consent’.
Chapter 17 looks at how leadership could be promoted by people living with dementia themselves. I first introduce the need for this in Chapter 2. Chapter 17 considers who might lead the change, where and when, and why this change might be necessary to ‘recalibrate’ the current global debate about dementia. This chapter considers how change might be brought about from the edge, how silos might be avoided, the issue of ‘tempered radicals’ in the context of transformative change to wellbeing as an outcome; and finally how ‘Dementia Champions’ are vital for this change to be effected.
Finally, I attempt a Conclusion at Chapter 18.
Continuity of care and support is vital in dementia policy. We are a long way from that.
In a way, the second ever English dementia policy poses more of an acid test than the first one. The reason for this is because we already have a set of yardsticks by which the first five years can be assessed, with a view to projecting forewards.
I don’t doubt the enthusiasm with which we have tried to close the ‘diagnosis gap’ in England. The heart of this is the high quality diagnosis, as stipulated in the original policy co-authored by Prof Sube Banerjee at Brighton and Sussex Medical School. What we have tended towards, rather, is a culture of high volume mediocre quality. And people readily admit they would rather wait that little bit longer to get the correct diagnosis.
I do not subscribe to the idea that anyone can easily make a diagnosis of dementia. When a diagnosis of dementia is finally given, it’s given not just to the person with dementia, but to his or her friends, or her family. As Kate Swaffer says, she is not a person with dementia primarily; she is a person with friends, family and feelings.
This approach prioritising the person has to be right from the word go. We are all persons, but we become patients when we become ill enough to present to the health and care services or not. We become paying consumers when we part with money. We are consumers if we spend any resources from the pot of money paid into from national insurance.
And so on. This analysis of money is a sideshow only as far as to how to service is delivered is actually matters. If you have services in dementia and support commissioned in a highly piecemeal manner, at worst from clinical commissioning groups who don’t know what wellbeing is, nor what they’re looking for, it can be a mess.
The hunt is definitely on for effective commissioning as well as any commissioning at all. The next Government will have to provide much better clarity on this, and some objective guidelines on how, say, the delivery of wellbeing might be ensured on an ongoing basis, not just at the start and finish of a commissioning contract.
But it is the fragmented approach from different providers which is a threat. Low pay of carers, not meeting the national minimum wage, or zero hour contracts, is a problem, and the reason specifically why private providers can be an issue here is that large corporates with scrupulous employment practices can hide behind a veil of being unperturbed from freedom of information legislation.
It is very easy to argue that entire health policy, and even dementia policy, is not political. I don’t believe this is justifiable for a minute. How we prioritise care at all is a reflection of our collective solidarity as a society, and our success in ‘pooling risk’. If I know for example I have a high genetic risk of developing a dementia from my genetic make up, my insurance premiums is likely to go through the roof unless there is tight anti-genetic discrimination law in place in England (which there isn’t).
Having a piecemeal system promotes lack of continuity of care. I think this is fatal for any new English dementia strategy. I think this piecemeal system, whether an artefact of private markets or not, or political ideology, can adversely affect people living with dementia and carers in a number of different ways.
First of all, the caregiver relationship, whether paid or unpaid as carer, fundamentally depends on that caregiver knowing the person with dementia. The happiest relatives I have ever spoken to are the ones who report that they haven’t had a regular changing of the guard as regard carers. This is important for building meaningful relationships with time, as people with Alzheimer’s disease for much of their time, even if they have weak memories for events have strong enduring memories for emotions. Besides, change here can be very distressing, and mental distress can impact on lack of physical wellbeing (although ill being is not necessarily the same as lack of wellbeing).
Secondly, continuity of care by a physician or an appropriate specialist in clinical psychology acts as a safeguard to check the actual diagnosis is right. Some initial cognitive impairments do not progress – they remain mild. A ‘wrong diagnosis’ of dementia does not necessarily mean someone has goofed up as such – it could mean that something that was predicted to progress didn’t. The drive to diagnosing dementia, particularly with financial incentives, could mean we accidentally mislabel mild cognitive impairment as dementia, and this is clearly a tragedy for all involved.
Therefore, a diagnosis disclosure can never be a single hit and run event. There needs to be follow up from the system, whether it’s by the same GP, a hospital physician or psychiatrist, a different member of the memory clinic possibly somewhere totally different; a second ‘set of eyes’ to see whether the initial diagnosis is correct. Granted I agree that knowing what the diagnosis is can be the key to opening services, being armed with information and hence empowered, and all the usual arguments, but the diagnosis must be correct. There is no alternative on this.
Say, for example, you are in fact depressed, not living with dementia, and a clinician in a hurry informs you you are living with dementia. You have presented in response to the question, “Do you have problems with your memory?”. Such a misdiagnosis is likely to make you even more depressed; and not receiving effective treatment for depression, whether as a psychological therapy or medication, or otherwise.
Thirdly, somebody who knows a person well will be able to spot when a person with dementia changes in any way. This could be a ‘difference’, such as the development of a sweet tooth, a ‘deterioriation’ such as in memory, or even an ‘enhancement’ as in acquisition of a love of music, or artistic and creative talents. You can only ascertain this with time. This is where the idea of the review has to change fundamentally.
I don’t feel this review should take place in the hands of medics who repeat scans and tests, ask a few random questions, and document the decline (as dementia is progressive if it is not ‘reversible’ such as vitamin deficiency). Implementation of a ‘year of care’ for dementia, or a national network of clinical specialist nurses, will be able to manage a caseload of individuals living well in a pro-active fashion, each with an individualised care plan; where the goal is to live well, not to firefight in a crisis.
Fourthly, the fundamental crunch time for a person living with dementia is an inability to retain information for a decision, an inability to make that decision, and an inability to communicate that decision. The starting point is that we can make decisions or have ‘capacity’. This capacity can come or go; and it’s dangerous if we get into the mindset that capacity is all or nothing, but that is the legal shortcut we have in place.
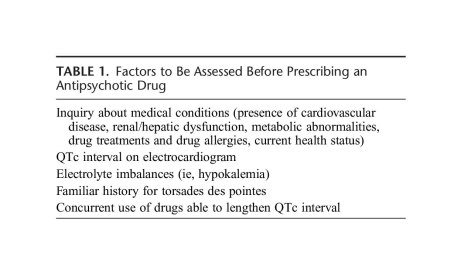
But this capacity needs review on a regular basis, as it fundamentally changes our view as to whether a person can consent or not. People living with diffuse lewy body dementia, for example, can notice themselves one day they’re performing quite well, other days not so well. If we don’t get into the good practice of reviewing capacity and consent on a regular basis, through continuity of care, we will easily arrive at a situation where people are languishing inappropriately on medications. It’s generally felt that, while appropriate for some, antipsychotics prescribing is too high, often inappropriately; some side effects such as drooling of the mouth can be very distressing. It’s currently, rightly, a plank of policy to address the inappropriate prescription of antipsychotics particularly in care homes.
In summary, the ideal would be somebody to accompany a person from the point of diagnosis to the time of end of life; not chopping and changing. I was told by a senior specialist nurse at the National Hospital for Neurology and Neurosurgery, Katy Judd, that one of the most disturbing phenomena for persons with dementia and families is when their ‘contacts’ have ‘moved on’ on such a frequent basis. There clearly needs to be proper signposting with the system, known as care coordinators, but we need to avoid the situation where there is an abundance of signposts and a dearth of frontline care.
But I feel fundamentally continuity of care and support is critical. Having the same mutual followers on a social network on Twitter has the potential to improve wellbeing, and having somebody there by you that you trust is likely to have the same effect. People living with dementia who are stimulated psychologically by positive experiences are likely to find their experience fundamentally of a different nature to those who don’t.
For these reasons I feel that, whatever tactics are used, and whichever government is in office and/or power in England, for the next few years, an overall strategy of prioritising the continuity of care is pivotal.
An overview of my book ‘Living better with dementia: champions for enhanced communities”.
I hope you find this overview of my book ‘Living better with dementia: champions for enhanced communities’ useful.
It is written by me.
And the Forewords are Prof Alistair Burns, the England clinical lead for dementia, Kate Swaffer (Alzheimer’s Australia, Dementia Alliance International, and University of Wollongong, Australia), Chris Roberts (Dementia Action Alliance Carers Call to Action, Dementia Alliance International), and Dr Peter Gordon (Consultant Psychiatrist in dementia and cognitive disorders, NHS Scotland).
It will primarily assess where we’ve got to, along with other countries, in improving diagnosis and post-diagnostic care, and assess realistically the work still yet to be done.
My thesis will articulate why the ‘reboot’ of the global “dementia friendly communities” must now take account of various issues to be meaningful. It will argue for a difference in emphasis from competitive ‘nudge’ towards universal legal and enforceable human rights promoting dignity and autonomy.
It will also argue that dementia friendly communities are meaningless unless there is a shift in the use of language away from ‘sufferers’ and ‘victims’, while paying tribute to the successful “Dementia Friends” initiative.
It will, further, argue that dementia friendly communities are best served by a large scale service transformation to ‘whole person care’, and provide the rationale for this. A critical factor for enhancing the quality of life of people living better with dementia will be to tackle meaningfully the social determinants of health, such as housing and education.
The thesis will also argue that dementia friendly communities must also value the behaviours, skills and knowledge of caregivers in wider support networks. This is essential for the development of a proactive service, with clinical specialist nursing input deservedly valued, especially given the enormous co-morbidity of dementia.
This title will be published by Jessica Kingsley Publishers, in early 2015.
Chapters overview
Chapter 1 provided an introduction to current policy in England, including a review of the need for a ‘timely diagnosis’ as well as a right to timely post-diagnostic care. This chapter also provided an overview of the current evidence base of the hugely popular “Dementia Friends” campaign run by the Alzheimer’s Society and Public Health England, to raise awareness about five key ‘facts’ about dementia. It was intended that this campaign should help to mitigate against stigma and discrimination that can be experienced by people living with dementia and their caregivers.
Chapter 2 comprised a preliminary analysis of stigma, citizenship and the notion of ‘living better with dementia’. This chapter explained the urgency of the need to “frame the narrative” properly. This chapter also introduced the “Dementia Alliance International” which has fast become a highly influential campaigning force by people living with dementia for people living with dementia.
Chapter 3 looked at the various issues facing the timely diagnosis and post-diagnostic support of people living with dementia from diverse cultural backgrounds, including people from black, Asian and ethnic minority backgrounds, people who are lesbian, bisexual, gay or transsexual, and people with prior learning difficulties.
Chapter 4 looked at the issue of how different jurisdictions around the world have formulated their national dementia strategies. Examples discussed of countries and continents were Africa, Australia, China, Europe, India, Japan, New Zealand, Puerto Rico and Scotland.
Chapter 5 looked at the intense care vs care debate which has now surfaced in young onset dementia, with a potentially problematic schism between resources being allocated into drugs for today and resources being used to fund adequately contemporary care to promote people living better with dementia. An example was discussed of how the policy of ‘Big Data’ had gathered momentum across a number of jurisdictions, offering personalised medicine as a further potential compontent of person-centred care. This chapter also considered the impact of the diagnosis of younger onset dementia on the partner of the person with dementia as well. A candid description was also given about the possible sequelae of the diagnosis of young onset dementia on employment, caregivers, and in social isolation.
Chapter 6 focused on delirium, or the acute confusional state, and dementia. It considered the NICE guidelines for delirium, and the pitfalls in considering the relationship between delirium and dementia in English policy.
Chapter 7 was the largest chapter in this book, and took as its theme care and support networks. An overview of how patient-centred care is different from person-centred care was given, and how person-centred care differs from relationship-centred care. The literature inevitably has thus far focused on the ‘dyadic relationship’ between the person with dementia and caregiver, but a need to enlarge this to a professional in a ‘triangle of care’ and extended social networks was further elaborated and emphasised. Finally, the importance of clinical specialist nurses in ‘dementia friendly communities’ was argued, as well as the Dementia Action Alliance’s “Carers Call to Action”. Different care settings were described, including care homes, hospitals – including acute hospital care, and intermediate care.
Chapter 8 considered eating for living well with dementia. This chapter considered enforceable standards in care homes, including protection against malnutrition or undernutrition. The main focus of the chapter was how people with dementia might present with alternations in their eating behaviour, and how the mealtime environment must be a vital consideration for living better with dementia.
Chapter 9 looked at a particular comorbidity, incontinence. The emphasis was on conservative approaches for living well with dementia and incontinence. Other issues considered were the impact of incontinence on personhood per se, and the possible impact on the move towards an institutional home.
Chapter 10 argued how the needs for people living better with dementia would be best served by a fully integrated health and social care service. This chapter provided the rationale behind this policy instrument in England. The chapter also considered various aspects of what would be likely to make ‘whole person care’ work, including data sharing, collaborative leadership, care-coordinators, responsible and accountable ‘self care’, and the multi-disciplinary team. This chapter also considered how it was impossible to divorce physical health from mental health and social care, and explained the intention of the longstanding drive towards ‘parity of esteem’ in English policy.
Chapter 11 considered the importance of the social determinants of health. A focus of this chapter was on education, and its impact on a person living with dementia. However, the main focus of this chapter was housing, including ‘dementia friendliness, downsizing, and green or public spaces.
Chapter 12 considered whether ‘wandering’ is the most appropriate term. The main emphasis of this chapter were the legal and ethical considerations in the use of ‘global positioning systems’ in enhancing the quality of life of persons with dementia and their closest ones.
Chapter 13 considered a number of important contemporary issues, with a main emphasis on human rights and “rights based approaches”. While there is no universal right to a budget, the implementation of personal budgets was discussed. The chapter progressed to consider a number of legal issues which are arising, including genetic discrimination in the US jurisdiction, dementia as a disability under the equality legislation in England, and the importance of rights-based approaches for autonomy and dignity. Finally, the issue of engagement was considered.
Chapter 14 was primarily concerned with art and creativity. This chapter took as its focus on how living with dementia could lead to art and creativity, and how the cultural needs of people living with dementia could best be furnished through laughter, poetry and art galleries or museums. This focus also looked at the exciting developments in our understanding of the perception of music in people living with dementia, and how music has the potential to enhance the quality of life for a person living well with dementia.
Chapter 15 looked at the triggering of football sporting memories in people living well with dementia. This chapter considered the cognitive neuroscience of the phenomenon of this triggering, and presented a synthesis of how the phenomenon could be best explained through understanding the role of emotional memory in memory retrieval, how autobiographical memories are represented in the human brain usually, the special relevance of faces or even smells such as “Bovril”.
Chapter 16 looked at the impact of various innovations in English dementia policy, giving as examples including service provision (such as the policy on reducing inappropriate use of antipsychotics or the policy in timely diagnosis) and research. This chapter also contemplated the principal factors affecting how innovations can become known, and what ultimately determines their success.
Chapter 17 looked at how leadership could be promoted by people living with dementia. This chapter considered who might lead the change, where and when, and why this change might be necessary to ‘recalibrate’ the current global debate about dementia. This chapter considered how change might be brought about from the edge, how silos might be avoided, the issue of ‘tempered radicals’ in the context of transformative change to wellbeing as an outcome; and finally how ‘Dementia Champions’ are vital for this change to be effected.
Please note that Beth is not endorsing this book – this image is entirely separate and is taken from the main event for G8 dementia – we’re all proud of Beth’s work meanwhile!
A lot more unites us in English dementia policy than divides us, potentially
It’s sometimes hard to see the big picture in the policy of England regarding dementia.
I don’t mean this in terms of the three key policy strands of the strategy, which is currently the Prime Minister’s Dementia Challenge. This extra layer was added onto the English dementia strategy, “Living well with dementia”, from 2009-2014.
There will be a renewal of this strategy next year. We currently don’t know what Government will be in office and power in 2015. But I am hoping the overall direction of travel will be a positive one. I would say that, wouldn’t I?
There are 3 dementia challenge champion groups, each focusing on 1 of the main areas for action: driving improvements in health and care, creating dementia friendly communities and improving dementia research.
But it is in my political philosophy to encourage a pro-social approach, not a fragmented one.
I’d like to see people working together. This can all too easily be forgotten in competitive tendering for contracts.
And things can be just as competitive in the third sector as for corporates.
This is the clinical lead for dementia in England, Prof Alistair Burns, who has oversight over all these complicated issues.
But we need to have a strong focus for the public good, especially as regards looking after the interests of people living with dementia, and their closest including all caregivers. State-third sector initiatives can work brilliantly for particular outcomes, such as encouraging greater sharing of basic information about dementia, but all concerned will hopefully feel that the people whose interests we want to protect the most benefit from a plural space with many stakeholders.
There is definitely a huge amount which has been achieved in the last few years. I do definitely agree with Sally Greengross, Chair of the All Party Parliamentary Group for dementia, that we should really take stock of what has worked and what hasn’t worked so well in the last five years, in our wish to move forward.
I say this, as it has come to my attention while reviewing the current state-of-play in policy and in research that there are potentially problematic faultlines.
1. One is diagnosis.
On the one hand, some people feel that we are under diagnosing dementia, and that there are people languishing in England waiting for a diagnosis for weeks or months.
Chris Roberts, himself living with a dementia, and a greater advocate for people living with dementia, often warns that it is essential that, despite the wait, that the diagnosis is correct.
I know of someone else in the USA who has battled on for years while waiting for a diagnosis of dementia, despite having symptoms of dementia.
On the other hand, there are concerns, particularly if teams in primary care are financially incentivised for doing so, that there might be a plethora of over diagnosed cases.
The concern here is that there might be alternative interests for why such people might be diagnosed, such as being recipients of compounds from drug companies which attach to proteins in the brain, and which might be useful in diagnosing dementia.
Or we are building a ‘new model army’ of people who are ageing, but being shoehorned into the illness model because of their memory problems?
2. Another is potential ‘competition’ between dementia charities.
Essentially, all dementia charities in England want the same thing, and will need to attract an audience through various ‘unique selling points’ through that awful marketing terminology.
But in the next few years we may see commissioning arrangements change where the NHS may involve the third sector doing different complementary rôles, such as advising and providing specialist nursing, in the same contractual arrangement.
The law might force people to work together here.
3. Another is the ‘cure versus care’ schism.
This debate has accelerated in the last few years, with the perception – rightly or wrongly – that cure – in other words the drive to find a magic bullet for dementia – is vying for attention with care. This narrative has a complicated history in fact, in parallel with moves in the US which likewise have overall seen a trend towards some people wishing for a ‘smaller state’.
But claims about finding a cure for dementias have to be realistic, and, while comparisons can be made with HIV and cancer about the impact of a cure has for absolving stigma potentially, such a debate has been done incredibly carefully.
For example, attention for cures and collaboration between Pharma and ‘better regulation’ constitute a diversion of resources away from care, potentially. In the NHS strategy for England, with social care on its knees, a drive towards personalised medicine on the back of advances from the Human Genome Project can end up looking vulgar.
I’ve also seen with my own eyes how the ‘cure vs care’ schism has seen different emphases amongst different domestic and international dementia conferences, with some patently putting people with dementia in the driving seat, and some less so (arguably).
4. Another is the exact emphasis of ‘dementia friendly communities’.
It is impossible to object to the concept of inclusivity and accessibility of communities, with recognition of the needs of people living with the various dementias.
But the term itself is possibly not quite right; as Kate Swaffer says, a leading international advocate on dementia, you would never dream of ‘black friendly communities’ or ‘gay friendly communities’ as a term.
Another issue is what the precise emphasis of dementia friendly communities is: whether it is an ideological ‘nudge’ for companies and corporates to enable competitive advantage, or whether it is driven by a more universal need to enshrine human rights and equality law.
As Toby Williamson from the Mental Health Foundation mooted, the need for an employer to make reasonable adjustments for cognitive disAbility is conceptually and legally is actually the same as the need for an employer to build an access ramp for a person who is in a wheelchair and physically disabled?
There can also be a problem in who wishes to be “the dominant stakeholder”. Is it the person with dementia? Or unpaid caregiver? Or paid carer? Or professional such as CPN, physio, OT, speech and language therapist, neurologist, physician or psychiatrist? Is it a dementia adviser or specialist nurse?
If we are to learn the lessons from the Carers’ Trust/RCN “Triangle of Care”, it is essential to learn from all stakeholders in the articulation of a personalised care and support plan? I feel this is important in whole person care if we are to have such plans in place, which recognise professional pro-active clinical help, in trying to assist in avoidable admissions to hospital.
But here we have to be extremely careful. An admission to hospital or appearance at A&E should not always be sign of ‘failure’ of care in the community.
5. Yet another source of division is that we all do our own things.
This is problematic, if we do our own things. We end up being secretive about which people we’re talking to. Or which conferences we’re going to.
Or if countries don’t talk to each other, even if they have similar aims in diagnosis, and post-diagnostic care and support (including the global dementia friendly communities policy). Or if we don’t share lessons learnt (such as, possibly, the beneficial impact of treating high blood pressure on dementia prevalence in one country).
Or if certain people become figureheads in dementia. But no man is an island.
I still feel that there’s a lot more that unites us than divides us.
Anyway, I’ll leave it to people on the frontline, and in communities, much more able than me, to work out what they want.
The ‘NHS Five Year Forward Plan’ is a clever marketing stunt, and is barely a statement of strategy
There’s no “magic money tree”, except when you’re signing off HS3 on a ‘nod and a wink’ for £7 billion, or interventions in Iraq and Afghanistan for £30 billion.
As a piece of marketing, for Simon Stevens to set out a stall for the rôle of the NHS in a global economy, “the five year plan” was nice and succinct. As a piece of strategy, it is dreadful. It’s dreadful – even if you decide to take the view that health policy is entirely market-driven or “value-based”, and not in any way written through a sophisticated clinical prism.
The irony of a “five year plan” for the National Health Service is pretty quick to see. “Five year plans” were, of course, used by Stalinist Russia. Nazi Germany preferred ‘four year plans’ as a strategy for war readiness, in comparison.
It is reported that the “Five Year Forward View”, published last week by NHS England, is a collaboration between six leading NHS groups including Monitor, Health Education England, the NHS Trust Development Authority, Public Health England, the Care Quality Commission and NHS England.
And yet ironically the future of two of the contributing organisations is under doubt. In a fringe meeting earlier this at the Labour Party Conference, it was again mooted what the precise function of Monitor might be. This is because it is definite that an incoming Labour Party government, in its first Queen Speech, will repeal the Health and Social Care Act (2012), a much loathed piece of legislation. This leaves the precise functions of Monitor uncertain.
One possibility which Burnham is seriously contemplating is whether Monitor, if it continues to exist, serves to regulate the integration of services as would be expected in ‘whole person care’. Burnham intends to introduce ‘NHS preferred provider’, which could insist on the NHS being the lead provider in contracts for as long as ten years in the ‘prime contractor model‘.
And the future of the Care Quality Commission was put on a cliff-edge with the report of the Sir John Oldham Commission, again to do with whole person care. It would make much more sense to reform the regulators to oversee health and care with a single regulator in future. This would again be in line with the regulation of health and care professionals, much needed, and proposed by the English Law Commission, but kicked into the long grass by the current Government as it ran out of time.
The “5 year Forward View” to all intents and purposes reads like a marketing document, a wish-list for further privatisation of the NHS. It may ‘pack a punch‘, from the BBC which has unreservedly succeeded in throttling any discussion of the NHS reforms. But talk of ‘accountable care organisations’, as developed in Spain and the United States, and the emphasis on preventive health packages so keenly sold by multinational corporates, are paradigmatic of a wish-list of a privateer.
The document is a naked shill, intended to carry on the ‘case for change’ which has been made exhaustively by think tanks such as the King’s Fund which, some might say, were instrumental in giving the catastrophic policy of market competition in the National Health Service some legs in the first place.
But the runes are clearly there.
Take, for example, the seemingly-modest proposal of “integrated care commissioning”. The policy of personal budgets in the full glare of sunlight looks incredibly anaemic. Unanswered questions exist how a universal health system is going to be successfully merged with a means-tested care system. NHS England tried, unsuccessfully, to head this issue off at the pass as far back as in 2012.
Personal health budgets, which Simon Stevens has continued to speak moistly of, are the perfect vehicle for introducing ‘top ups’ and ‘copayments’, threatening the fundamental principle of universal, free-at-the-point-of-need.
And moves, not contained in the ‘5 year plan’, spell out an ominous direction of travel. It has just been announced that the much maligned contract for processing ATOS, given under the last Government to ATOS, is to be given to a company called Maximus, which has a proven track record in handing long term care packages in other jurisdictions.
“Independent” think tanks have never shrugged off successfully the “power of the prepaid cards”, see for example the DEMOS initiative. It has always been vehemently denied that there will be no merging of universal credit and healthcare provision, although Liam Byrne’s account of Jennie Macklin in Australia painted a rather different story in an article in the Guardian provocatively entitled “Let’s help disabled people achieve their full potential“.
Like a multi-national corporate document, the “5 year plan” is high on marketing but poor on strategy. A good example of this is given on page 36 in relation to a ‘threat’ facing the National Health Service, that of recurrent pay freezes to the majority of nurses whilst the economy is reputed to be recovering.
The seemingly innocuous line, at the end of page 35, reads: “For example as the economy returns to growth, NHS pay will need to stay broadly in line with private sector wages in order to recruit and retain frontline staff.” But it is well known that any wish to pay nurses a wage that reflects the value that runs through their work like letters in a stick of rock will be strongly resisted by the Treasury, while the Conservative Party will prefer further to tattoo the words of low taxes onto his breast plate of ideology.
There are other clear examples of the document clearly lacking in clarity. For example, page 33 sees a promotion of ‘personalised medicine’, how the NHS and “our partners” (meaning in the third and private sector, actually) might deliver the genome based ‘revolution’. Again, the document’s thrust is one of marketing, not clear strategy. There is no mention of the changes in resource allocation which would be required to serve this revolution, essentially seeing hardworking taxpayers subsidise the shareholder dividends or surpluses of large corporate-like charities. There is absolutely no mention of the changes in the legislative framework that would be needed, as in the United States, to prevent genetic information non-discrimination. But here again the document serves its marketing function – as a prospective prospectus for would-be investors wishing to spot lucrative opportunities in the NHS as a data mine.
Like there is no mention of “NHS preferred provider”, unsurprisingly there is no mention of “whole person care”. And yet, even if Labour fail to win an outright majority, it will seek to implement this being the largest party in Government. And this policy is set to see a profound change in the landscape of health and care provision for England.
In any business strategy, one is obliged to think of the political, economic, social, technological, legal and environmental headwinds (affectionately known as “PESTLE” to business strategists). A good example of social changes in the five years might have been, for example, a change in direction of the NHS being seen as resentment as costing much money, despite its striking efficiency, but one which values its workforce (for example in the salary of most of its nurses).
Looking at the political headwinds, it is quite incredible for example there is no mention of trade agreements such as TTIP and the investor-to-state dispute settlement clauses. If this ‘5 year forward plan’ had been at all serious, it would have been included, not least as it is a headwind which could drastically throw off course further the direction of travel of the NHS as a state-run health service.
Simon Stevens’ vision is a ‘charismatic vision’ of sorts. But a vision does not have to be particularly credible for it to get populist appeal or succeed. It just needs to be communicated clearly, with supine and compliant supporters in the trade media.
If the document were a ‘heads up’ for how we could afford a NHS through general taxation which was genuinely universal and free at the point of need, this document would have served a function. As it is, the document is a lubricator for mechanisms which could optimise the part that the private sector has to play, with no mention of the dogs being unleashed in the global marketplace – in much the same way Cameron refused to signpost “the top down reorganisation”. It is impossible for a strategy document for the NHS simply to airbrush out the political and legal factors which will be at play in the lifetime of the next Government. As it is, the NHS ‘5-year forward view’ is a basic piece of marketing, which as a strategic plan scores 0/10.
Transforming dementia care is long overdue. Specialist clinical nurses in dementia are now vital.
In the G8dementia, particularly by large corporate-like charities, dementia has been compared to the cancers. Whilst there are many problems with this comparison medically, the aim is for research and service expectations to be met in dementia on an equal footing to those for cancer. There are different types of dementia and different types of cancer, and there is, according to NICE, no current treatment for Alzheimer’s disease, the most common type of dementia globally, which slows the progression of disease. The aim however is undeniably a laudable one. In terms of service provision, the hope is that medical conditions can be detected early (and not at the last minute), and over time care and support can be introduced and implemented in a non-panicky way. The low hanging fruit is for providers at the front end of the service to game the NHS QOF/CQUIN system to design ‘innovative’ packages which might diagnose certain forms of dementia, such as the profound short term learning and memory problems in early Alzheimer’s disease. But getting out of this ‘quick fix’ mentality is going to be essential for the long-term sustainability of dementia services in England I feel. I believe strongly that clinical nursing specialists would not just be a big help here: they are indeed vital. England will really benefit from senior people in dementia taking the bull by the horns, in keeping with a refreshing approach to the long term conditions (LTCs) in general, as helpfully described by the King’s Fund in this policy pamphlet from 2010.
But I have now spoken to two very senior specialist clinical nurses in the NHS. One who has been at the heart of policy for nursing in the last few years, and the other one who has been at the heart of one of the top clinical firms in cognitive disorders here in London for a few decades. They both said exactly the same thing to me: “What we’re fed up about is the fast turnover of services and personnel within them. It’s difficult to find the same person twice. And we’ve got too many people signposting services, and not enough people providing frontline care.” There is undoubtedly a rôle for a trained person who can help to navigate a person with dementia and his or her caregivers around a profoundly complicated system. I’ve heard that “dementia advisers” can be brilliant at a local level, but can easily come to the limits of the skills they can sometimes offer. The system is too bitty and disorganised at the moment; and persons with dementia (some of whom who become ‘experts by experience) and caregivers have a key rôle in optimising design of service and revision provision for dementia in the future.
As a person progresses along “a dementia journey”, a term itself which attracts some considerable criticism, his or her own needs will tend to change from living well independently with dementia to benefiting from increasing levels of support, and then increasing levels of care. Two big events could happen along this ‘journey': the loss of decision-making ability (mental capacity), and the preference to move into a residential home of sorts. The timing of these events can be very hard for people with dementia or their caregivers to predict. There can also be worsening problems in communication between people with dementia and those closest to them, including friends and family. If a person living with dementia needs suddenly to enter hospital as a ‘crisis’ at 4 in the morning, he or she might be blue-lighted in with an infected full bladder causing a deterioration in cognition and behaviour, without a care plan in sight.
Diagnosing dementia is clearly not enough, but a timely diagnosis can be helpful. Professional physicians, nurses and other staff will always consider their professional including moral obligations in how likely the diagnosis is, how much a person wants the diagnosis, and how much to investigate a possible diagnosis. And there are too many cases of the possible diagnosis being given in a busy clinic, often summarised as an ‘information pack'; at worst, some people lost to the system for years before anything new happens.
It is likely that England will develop ‘integrated care organisations’. This does not involve building new departments and new buildings, but is a shift in organisational mindset such that GPs with a specialist skill in dementia service provision can work alongside other trained professionals and caregivers, with the person with dementia. This ‘working together’ is nothing new. It has been brilliantly described in the policy work of the Carers’ Trust in their recent documents ‘A triangle of care’ and ‘A road less rocky’. Caregiving can be intensely rewarding, but can also be hard work with caregivers having specific needs of their own. Caregivers will also be at the very heart of any personalised care plans. A professional who might be involved is a speech and language therapist. There is a national shortage of experienced speech and language therapists which is a tragedy as some forms of dementia, for example logopenic primary progressive aphasia, might be characterised by substantial problems in language in the relative absence of problems in domains such as episodic memory.
As a dementia progresses, a clinical psychologist will be in a brilliant position to work out why a person might have practical problems in real life due to identifiable problems in thinking, such as planning. A planning problem might be manifest as a person being able to make a cup of tea, or to organise a planning trip. Or, a clinical psychologist will be able to tell a team that what appeared to be an optician-related matter with eyesight is in fact a higher order perceptual problem as found in the rarer posterior cortical atrophy type of dementia (where memory can be normal early on.) An occupational therapist can use his or her own expertise here. Whichever way you look at it, dementia service provision needs are likely to be met from clinical teams who are an integral part of the ‘dementia friendly community’, who have been somewhat disenfranchised out of the conversation so far compared to high-street customer-facing corporates. Professionals, even in the context of meeting their regulatory obligations, have, I feel, a massive rôle to play in providing personal communities even if they do not assume legal duty of care. It is now known that activities can not only enhance wellbeing, but can also possibly slow the rate of progression (although the evidence base for this finding is not particularly robust yet.)
In the last few years, since the Health and Social Care Act (2012), was introduced, there has been massive turmoil in the National Health Service (NHS), leading at worst to fragmented services resulting from slick pitches from well funded private providers unable to deliver on their contracts. And yet if the NHS were given the correct management and leadership skills, they could be at the heart of providing world class care in dementia. Economies of scale, with free knowledge transfer, can be advantages of large organisations. Given that there are a million people in the next few years living with dementia, the NHS should be planning ahead for this, not just counting the number of new diagnoses as a manifestation of glorified bean-counting. The drive to diagnosis has been a classic example of where the target has become the means to an end in itself.
Earlier this year in July 2014, it was reported that cancer care in the NHS could be privatised for the first time in the health service’s biggest ever outsourcing of services worth over £1.2bn. The four CCGs were involved, which care for 767,000 patients, are also seeking bidders for a separate £535m contract to provide end-of-life care. Whoever wins the cancer contract will then have to “transform the provision of cancer care in Staffordshire and Stoke”. The prime provider will “manage all the services along existing cancer care pathways” for the first two years after which “the provider will assume responsibility for the provision of cancer care, in expectation of streamlining the service model”, according to details posted by the CCGs on the main NHS procurement website.
Macmillan Cancer Support were able to bring clinical nursing specialists (CNS) to the table: the “Macmillan nurses”. This robust model, which had proper financial backing, has proven to work extremely well in the cancer setting (some details are here). A massive contribution of the CNS is widely thought has been thought to be the “proctive case management”, and not only is this is sound clinical sense but could in the long run save the NHS millions, averting emergency hospital admissions which have been pre-empted. The case for proactive case management has also been established in other neurological conditions such as multiple sclerosis. CNS have been described well for the community, but also have a rôle to play in hospitals. Indeed, continuity of care between the community and hospital will be vital, not least because people living with dementia can find unfamiliar people and physical environments extremely distressing. Warrington has seen the introduction of designs which put people living with dementia at ease and the valuing of specialist trained staff. The service provision there is a beacon of success, and shows what can be done if the NHS has a vision and motivation to succeed in this.
CNS could have been a pivotal component of the answer given to Lorely Burt, Liberal Democrat MP for Solihull, this week to the Prime Minister in the weekly PMQs. But it sadly was not.
Clinical nursing specialists, including the well respected “Admiral nurses” from the ‘Dementia UK’ charity, have been recognised as being crucial to developing world class care in dementia too here from our own English nursing strategy. Over 4o00 have signed a petition for more Admiral nurses on the internet. A much under-reported item of research from the Centre for Innovation and Leadership in the Health Sciences at the University of Southampton, established improved clinical outcomes and significant return on investment from CNS in dementia. Again, work in progress suggests that the proactive case management approach has a lot to offer here. A paper from Prof Steve Iliffe and Prof Jill Manthorpe and colleagues is particularly noteworthy here. The beneficial impact of CNS in averting emergency admissions is being well described for cancer by Prof Alison Leary, Chair of Healthcare and Workforce Modelling, and colleagues (see, for example, here). If in the next five-year English dementia strategy there is a strong commitment to flagship clinical integrated services with well established and respected clinical nursing specialist models implemented, this could really revolutionise dementia service provision. And it’s now becoming increasingly that commonalities in what works well, especially in relation to involving caregivers, is working across a number of LTCs. This is a golden opportunity for senior policy specialists in dementia to put the emphasis on sustainable models of care rather than shiny box gimmicks, and to design a system which will be of real benefit to patients with dementia and their closest ones.
Could the “social impact bond” help to improve services in dementia care?
This blogpost first appeared on the ‘Living well with dementia’ blog yesterday.
It’s impossible to ignore the occasional spate of reports of ‘care home scandals’, including Winterbourne View and Orchid View.
Whilst a direction of travel might be to advance people living ‘successfully’ as long as possible independently, there’ll be some people for whom a care home might be appropriate. There are particular aims of policy designed to support living well with dementia, such as combating loneliness and providing meaningful leisure activities, which can possibly be achieved through high quality care homes.
It’s pretty often that you hear of social care being “on its knees”, due to drastic chronic underfunding. A concern about attracting investment from the private sector is that this will help to accelerate the lack of financial resource allocation from the State. And yet this is the opposite to the argument of resources ‘leeching’ out of the public sector into the private sector.
In terms of the ‘business model’, there are concerns that, to maximise shareholder dividend, staff will not be incentivised to ‘care well’, if they are barely meeting the requirements of the national minimum wage. Whilst the employer emphasises ‘flexibility’ of zero hours contracts, for many such contracts are symbolic of a lack of commitment for sustained employment by the employer.
So the idea of bonds being used to prop up dementia care, currently one of the three big arms of the Prime Minister’s Dementia Challenge, has gained some momentum, for example here. Bonds are effectively “IOUs“, and concerns remain for them as in the private finance initiative – such as who actually benefits, the prolonged threat of penalty for not being able to meet your loan repayments, the issue of who decides the outcomes by which performance will be assessed, and who actually manages or controls the enterprise.
Social Impact Bonds (SIBs) are depicted as “a way of enabling innovation, creating flexible contracts around social outcomes and providing linked investment“. But for some, they are a vehicle for enabling ‘privatisation by stealth’.
The current Labour opposition officially is trying to distance itself from any mechanisms promoting the privatisation of the NHS, and yet it is known Chris Ham and Norman Lamb wish to publish a report imminently on the possible use of SIBs in policy under the auspices of the King’s Fund.
This is the title slide of Hazel Blears’ presentation for the Alzheimer’s Show on Friday.
And here is a section of her talk.
[apologies for the sound quality]
Hazel has a strong personal attachment to campaigning on dementia, and is particularly interested and influential in the direction of travel, not least in her rôle as Vice Chair of the All Party Parliamentary Group on dementia, a cross party group made up of MPs and Peers with an interest in dementia.
Andy Burnham MP, Shadow Secretary of State for Health, has made it clear that it is his firm and settled intention to repeal the Health and Social Care Act (2012). The current Prime Minister’s Dementia Challenge is to come to an end officially in March 2015.
Dementia UK set up some time ago its innovative ‘Admiral Nurses’ scheme, to provide specialist nurses who could help people with dementia and family carers to improve the quality of life of people with dementia and family carers.
Burnham has also let it be known that he intends to subsume social care within the NHS under the construct of ‘whole person care’. Whichever various formulations of ‘whole person care’ you look at, you tend to find a ‘care coordinator’ somewhere. The exact job description of the care coordinator, nor indeed which specialisms might be best suited to accomplish this rôle, is somewhat unclear presently.
But it is all too common to hear of people being diagnosed with dementia being ‘lost in the system’, sometimes for years without follow up.
A “care coordinator” might help to boost access to the following services: emotional support, enable short breaks for people with dementia and anyone in a caring role, promote nutritious meals, ensure medications are given on time, ensure the correct medications have been subscribed (for example avoiding antipsychotic medications in individuals who might be unsuited to these), advice about suitable housing (including downsizing), ensure all physical commodities are properly medically managed; and so the list goes on.
I feel it’s pretty likely there’ll be a ‘first mover advantage‘ effect for any entity which takes up this coordination rôle in dementia care. But the tension between this and the Opposition’s policy is palpable: one cannot talk of this entity being ‘the first to enter the market’, as many wish (and expect) Labour to abolish the internal market in health care.
Such a coordinating entity could well be a recipient of a SIB – but is this like the PFI of social care? PFI by and large has an incredibly negative press amongst members of the general public.
But on the other hand, is it vindictive to prevent a social enterprise from pitching from such a service? If that entity has the technical ‘know how’ to run operations nationally competently and at a reasonable price, would that be preferable to the State running such services when projects such as NHS IT and universal credit have not gone terribly well?
In our jurisdiction, private companies can hide easily being a corporate veil, and are for example currently not readily accountable through freedom of information legislation. This is despite numerous requests to Jeremy Hunt in parliament about parity in disclosure requirements from both private and public providers.
And the track record of some outsourcing companies in the private sector, it is said, has been terrible.
Jeremy Hunt and Norman Lamb are currently in control of NHS and care policy, but there might be a fundamental change in direction from the next Government.
Or there might not be.
Empowering the person living with dementia personally, with more than the diagnosis
This laid down useful foundations, many strands of which were to be embellished tactically under this Government through “The Prime Minister’s Dementia Challenge”. In some ways, its major limitations were unintended consequences not fully known at the time.
The English dementia strategy is intended to last for five years, and, as the 2009-14 ‘five years’ come to an end, now is THE right time to think about what should be in the next one. Irrespective of who comes to deliver this particular one, progress has been made with the current one. I believe that across a number of different strands the focus on policy should delivering care, cure or support, according to what is right for that particular person in his social environment at that particular time.
The problems facing the English dementia strategy now are annoyingly similar to the ones which Banerjee and Owen faced in 2008. Whilst they do not have ‘political masters as such’, they can be said to have had some political success. But that should never have been the landmarks by which the All Party Parliamentary Committee, chaired by Baroness Sally Greengross, were to ‘judge’ this strategy document.
The national dementia strategy back in 2009 had three perfectly laudable aims.
The first is to change professional and societal views about dementia.
There was a perception that some Doctors would sit on a possible diagnosis for years, before nailing their colours to their diagnostic mast. So this need for professionals to be confident about their diagnosis got misinterpreted by non-clinical managers as certain doctors, particularly in primary care, being obstructive in making a diagnosis.
At the time, it was perceived that there also had to be an overhaul in the way doctors think about the disease – a quarter believe that dementia patients are a drain on resources with little positive outcome, according to a National Audit Office (NAO) in July 2007. But this has only been exacerbated, and some would say worsened, by language which maintains “the costs of dementia” and “burden”, rather than the value which people with dementia can bring to society.
Associated with this has undoubtedly been the promotion of the message that ‘nothing can be done about dementia’. Indeed, the G8 dementia summit, collectively representing the views of multi-national pharmaceutical companies and their capture within finance, government and research, spoke little of care, and focused on methods such as data sharing across jurisdictions. It’s likely corporate investors will see returns on their investment in personalised medicine and Big Data, but it is essential for the morale of persons with dementia that they are not simply presented as ‘subjects’ in drug trials (and misuse of goodwill in the general public too). Unfortunately, if elements of Pharma overplay their hand, they can ultimately become losers, an issue very well known to them.
High quality research is not simply about excellent research into novel applications of drugs for depression, diabetes or hypertension, or the plethora of molecular tools which have a long history of side effects and lack of selectivity, but should also be about high quality research into living well with dementia. This is going to be all the more essential as the NHS makes a painful transition from a national illness service back to a national health service, where wellbeing as well as prevention of illness and emergency are nobel public health aims.
This summit was presented with an ultimate aim of producing a ‘cure’ for dementia by 2025, or ‘disease modifying therapies’, with no discussion of how ethical it would be – or not be – for the medical profession to put into slow motion a progressive condition; if it happened that the condition were still inevitable. The overwhelming impression of many is that the summit itself was distinctly underwhelming in what it offered in terms of grassroots help ‘on the gound’.
The G8 dementia summit did nothing to consider the efficacy of innovations for living well with dementia, for example assistive technology, ambient assisted living, design of the home, design of the ward, design of the built environment or dementia friendly communities. It did nonetheless commit to wanting to know about it at some later date.
It did nothing to consider the intricacies of the fundamentals of ‘capacity’ albeit in a cross-jurisdictional way, and how this might impact on advocacy services. All these issues, especially the last one, are essential for improving the quality of life of people currently living with dementia.
A focus on the future, for example genetic analysis informing upon potential lifestyle changes one might have to prevent getting dementia at all, can be dispiriting for those currently living with dementia, who must not be led to feel ignored amongst a sea of savage cuts in social care. The realistic question for the next government, after May 7th 2015, of whatever flavour, is to how to catalyse change towards an integrated or ‘whole person’ ethos; ‘social prescribing‘, for example, might be a way for genuine innovations to improve wellbeing for people with dementia, such as ‘sporting memories‘, to gain necessary traction.
Empowering the person living with dementia with more than the diagnosis is fundamental. It is now appreciated that living well with dementia requires time to take care over appreciating the beliefs, concerns and expectations of the person in relation to his or her own environment. This interplay between personhood and environment for living well with dementia has its firm foundations in the work of the late great Tom Kitwood, and has been assumed by the most unlikely of bedfellows in the form of ‘person centred care’ even by multinationals.
Rather late in the day, and this seemed to be a mutual collusion between corporate-acting charities and the media, as well as Pharma, was a volte face on misleading communications about the efficacy of medications used to treat dementia. NICE, although potentially themselves a target of ‘regulatory capture’, were unequivocal about their conclusions; that a class of drugs used to treat ideally early attentional and mnemonic problems in early dementia of the Alzheimer type, had a short-lived effect on symptoms. of a matter of a few months, and did nothing to slow progression of disease. Policy is obligated though to accommodate that army of people who have noticed substantial symptomatic benefits for that short period of time with such medications such as aricept (one of the medications known as cholinesterase inhibitors)? Notwithstanding that, I dare say a medication ‘to stop dementia in its tracks’, as has been achieved for some cancers and HIV/AIDS, would be ‘motivating’, though I think the parallels medically between the dementias, HIV/AIDS and cancer have been overegged by non-clinicians.
And this was after spending many years researching these medications. The opportunity cost of the NHS pursuing the medical model is not inconsiderable if one is indeed wishing to ‘count the cost’ of dementia, compared to what could have been achieved through simple promotion of living well methods.
Large charities across a number of jurisdictions have clearly been culprits, and are likely to be hoisted by their ptard, as organisations as the Dementia Alliance International, a group of leading people living with dementia, successfully reset the agenda in favour of their interests at the Puerto Rico Alzheimer’s Disease International Conference this year.
The second problem that still needs addressing is diagnosing the conditions which commonly come under “the dementia umbrella”.
[Source: here]
And clearly, the millions spent on Dementia Friends, a Department of Health initiative delivered by the Alzheimer’s Society, provides a basic core of information about dementia. It has a target of one million ‘dementia friends’, which looks unachievable by 2015 now. This figure was based on Japan, where the social care set-up is indeed much more impressive anyway, and which has a much lager population.
The messages of this campaign are pretty rudimentary, one quite ambiguous. The campaign suffers from training up potentially a lot of people with exactly the same information, delivered by people with no academic or practitioner qualifications in dementia necessarily. This means that such ‘dementia friend champions’ are not best placed to discuss at all the difference between the various medical presentations of dementia in real life, nor any of the possible management steps. Egon Ronay it is not, it is the Big Mac of dementia for the masses. But some would say it is better than nothing.
But has training up so many dementia friends actually done a jot about making the general public into activists for dementia, like being a bit more patient with someone with dementia in a supermarket queue? Dementia Friends clearly cannot address how a member of the general public might ‘recognise’ a person with dementia in the community, let alone be friendly to them, just by mere superficial observation of their behaviour. It is actually impossible to do so – laying to the bed the completely misleading notion that schoolchildren have been able to recognise the hallmarks of dementia in their elders, which have been missed by their local GPs.
This first issue about shifting attitudes in perception and identity of dementia is very much linked to the issue of diagnostic rates. A public accounts committee report in January 2008 had revealed that two-thirds of people with dementia never receive a specialist diagnosis. Only 31% of GPs surveyed by the NAO agreed that they had received sufficient training to help them diagnose and manage dementia, and doctors have less confidence about diagnosing the disease in 2007 than they had in 2004.
Have things fundamentally changed in this time? One suspects fundamentally not, as there has always been a reluctance to do anything more than a broad brush public health approach to the issue of diagnosis.
Goodhart’s law is named after the banker who originated it, Charles Goodhart. Its most popular formulation is: “When a measure becomes a target, it ceases to be a good measure.” The original formulation by Goodhart, a former advisor to the Bank of England and Emeritus Professor at the London School of Economics, is this: “As soon as the government attempts to regulate any particular set of financial assets, these become unreliable as indicators of economic trends.”
And now it turns out that recoding strategies are being developed in primary care so as possibly to inflate the diagnostic rates artifactually. But while the situation arises that people in the general public may delay seeing their GP, and thereafter by mutual agreement the GP and NHS patient decide not to go on further ‘tests’, primary care can quite easily sit on many people receiving a diagnosis. The evidence base for mechanisms such as ‘the dementia prevalence calculator’ has been embarrassingly thin.
For example, Gill Phillips gives a fairly typical description of someone ‘worried well’ over functional problems at a petrol pump very recently, but the acid test for English policy is whether a person such as Phillips would feel inclined at all to see a Doctor over her ‘complaints’? The danger with equating memory problems with dementia, for example, means that normal ageing, while associated with dementia, can all too easily become medicalised.
And while there are possibly substantial disadvantages in receiving a diagnosis, both personally (e.g. with friends), professionally (e.g. employment), or both (e.g. driving licence), one should consider the limitations of national policy in turning around deep-seated prejudice, stigma and discrimination. And the solution to loneliness, undoubtedly a profound problem, is not necessarily becoming a ‘Dementia Friend’ if this means in reality getting the badge but never befriending a person with dementia? A ‘point of action’ like donating to a large corporate charity may be low hanging fruit for members of the public and large charities, but I feel English policy should be ambitious enough to consider shifting deep-rooted problems.
Such problems would undoubtedly be mitigated against if any Government simply came clean about what has been the increase in resource allocation, if any, for specialist diagnostic and post-diagnostic support services following this drive for improved dementia diagnosis rates. Lack of counselling around the period of diagnosis, with some people being reported as just being recipients of an ‘information pack’, is clearly not on, as a diagnosis of dementia, especially (some would say) if incorrect, is a ‘life changing event’.
Too often people with dementia, and close friends or family, describe only coming into contact with medical and care services at the beginning and end of their experience of a dementia timeline. Different symptoms, and different medications to avoid, are to be expected depending on which of the hundred causes of dementia a person has; for example Terry Pratchett and Norman McNamara have two very different types of dementia, posterior cortical atrophy and diffuse Lewy Body disease respectively. There is going to be no ‘quick fix’ for the lack of specialist support, though there is undoubtedly a rôle for ‘drop in‘ centres to provide a non-threatening environment for the discussion of dementia, encouraging community networks.
Ultimately, the diagnosis of dementia should be right for the person, at the correct time for him or her. This is the philosophy behind ‘timely’ rather than ‘early’ diagnosis, a battle which certain policy-makers appear to have won at last. Empowering the person living with dementia with that diagnosis can only be done on that personal level, with proper time and patience; ensuring sustainable dignity and respect for that person with a possible life-changing diagnosis of dementia.
The third priority of the strategy inevitably will be to improve the quality of care and support for people once they have been diagnosed.
At one end, it would be enormously helpful if the clinical regulators could hone on their minimum standard of care and those people responsible for care, including management. This is likely to be done in a number of ways, for example through wilful neglect, or the proposed anticipated proposals from the English Law Commission on the regulation of healthcare professionals anticipated to be implemented – if at all – in the next Government.
At the other end, there has been a powerful realisation that the entire system would collapse if you simply factored out the millions of unpaid family caregivers. They often, despite working extremely hard, report being nervous about whether their care is as good as it should be, and often do not consider themselves ‘carers’ at all.
There have clearly been issues which have been kicked into the long grass, such as tentative plans for a National Care Service while such vigorous energy was put into the Prime Minister’s Dementia Challenge. “Dementia friendly communities”, while an effective marketing mantra, clearly needs considerably more clarification in detail by policy makers, or else it is at real danger of being tokenistic patronisingly further stereotypes. Nobody for example would dare to suggest a policy framework called “Black friendly communities”. Whilst there are thousands of specialist Macmillan nurses for cancer, there’s about a hundred specialist Admiral nurses for dementia.
We clearly need more specialist nurses, even there is some sort of debate lurking as to whether Admiral nurses are ‘the best business model’. However, the naysayers need to tackle head on how very many people, such as those attending the Alzheimer’s Show this weekend in Olympia, describe a system ‘on its knees’, with no real proper coordination or guidance for people with dementia, their closest friends and families, to navigate around the maze of the housing, education, financial/benefits, legal, NHS and social care systems.
A rôle for ‘care coordinators‘ – sometime soon – will have to be revisited one suspects. But it is clearly impossible to have this debate without a commitment from government to put resources into a adequate and safe care, but while concerns about ‘efficiency savings’ and staffing exist, as well as existing employment practices such as zero-hour contracts and paid carers being paid below the minimum wage, how society values carers will continue to be an issue.
At the end of the day, care is profoundly personal, and repeatedly good care is reported by people who have witnessed continuity of care (away from the philosophy of the delivery of care in 15-minute “bite size chunks”). Unfortunately, the narrative in the NHS latterly has become one of business continuity, rather than clinical professional continuity, but this should ideally be factored into the new renewed strategy as well. I feel that this renewed strategy will have to accommodate actual findings from the literature taken as a whole, which is progressing at a formidable rate.
In a paper from February 2014, the authors review the the safety of the use of antipsychotics in elderly patients affected with dementia, restricting their analysis mainly to the last ten years. They concluded, “Use of antipsychotics in dementia needs a careful case-by-case assessment, together with the possible drug-drug, drug-disease, and drug-food interactions.” But interestingly they also say, “Treatment of behavioral disorders in dementia should initially consider no pharmacological means. Should this (sic) kind of approach be unsuccessful, medical doctors have to start drug treatment. Notwithstanding controversial data, antipsychotics are probably the best option for short-term treatment (6-12 weeks) of severe, persistent, and resistant aggression.” There are very clearly regulatory concerns of the safety of some antipsychotics, and yet the consensus appears to be they – whilst carrying substantial risk in some of very severe adverse effects – may also be of some benefit in some. It will be essential for the new National Dementia Strategy keeps up the only rapidly changing literature in this area, as do the clinical regulators.
Finally, in summary, I believe that there is enormous potential for England, and its workforce, to lead the way in dementia, in a way of interest to the rest of the world. I do think it needs to take account of the successes and problems with the five year strategy just coming to an end, with a three-pronged attack particularly on perception and identity, diagnosis and care. But, unsurprisingly, I believe that there are still a few gear-changes to be made culturally in the NHS, however it becomes delivered in the near future. There needs to be a clear idea of the needs of all stakeholders, of which the needs of persons with dementia, and those closest to them, must come top. There needs to be clear mechanisms for disseminating good practice, and leading on evidence-based developments in dementia wherever they come from in the world. And dementia policy should not be divorced from substantial developments from other areas of NHS England’s strategic mission: particularly in long-term conditions, and end-of-life care. This, again, would be the NHS delivering the right level of help for all those touched by dementia, from the point of diagnosis and well beyond.
Despite the sheer enormity of the task, I am actually quietly confident.
Thanks to Andy Burnham for emphasising “care co-ordinators” which I feel are pivotal to living well with dementia
This morning I had a present for Andy Burnham MP (@andyburnhammp), about to lead the Labour troops into battle for the European elections. The present is of course a copy of my book ‘Living well with dementia’, which is an account of the importance of personhood and the environment for a person living with dementia.
In my article entitled “Living well = greater wellbeing” for the ETHOS Journal (@ETHOSJournal), I highlighted the critical importance of the ‘care coordinator':
“So, if one had unlimited funds, what sort of service could be designed to provide care and support for people with dementia? In my opinion, the answer is a very different one. Ideally, all services, which could include healthcare, housing and legal systems, would adapt quickly and flexibly according to the needs of the individual living with dementia. This would need to be managed by a named, long-term co-ordinator of care and support.”
In reply to my article, Paul Burstow MP commented helpfully:
“The idea of a care navigator able to call on and coordinate all available health and social care, as well as housing support and voluntary sector provision is a persuasive one. It is something that the Richmond Group of charities, among others, have for a long time called for – and it is something I would like to see the Liberal Democrats deliver in the next government. Better managed and coordinated care would be a huge step forward and could make all the difference to dementia sufferers and their often strained carers.”
And Andy gave it much prominence this morning:
The King’s Fund (@TheKingsFund) has previously looked into co-ordinated care for chronic conditions.
In this framework, a “care co-ordinator” acts as a single point of contact and works with the patient, their carer(s) and the multidisciplinary team to develop a care plan.
Once this has been agreed, the co-ordinators work with the team, the patient, the patient’s family and other care providers to deliver co-ordinated and coherent care. Personal continuity of care is actively encouraged, and the care teams work hard to ensure an immediate response to care needs as they arise.
The care co-ordinator becomes he patient’s advocate in navigating across multiple services and settings ??providing care directly in the home environment.
He or she also ??communicates with the wider network of providers (outside of the core multidisciplinary team) so that information about the patient/carer is shared and any actions required are followed up.
The King’s Fund has previously found that the type of person undertaking the care co-ordination function varied greatly.
Most care co-ordinators had been community or specialist nurses, yet the role has also been taken on by non-clinical ‘link workers’ (in Sandwell) and health and social care co-ordinators (in Torbay).
There also appears to be a continuum from the non-clinical approach – primarily providing personal continuity to service users and acting as their advocate to ensure that care is co-ordinated around their needs – to the clinical approach, in which a case manager would also be able to provide clinical care directly.
This, I feel, is significant, as my book ‘Living well with dementia’ has a very non-medical thrust.
It’s very much a n0n-authoritarian, non-hierarchical approach where each person, including the person living with dementia, has an important part to play.
Influences on someone living well with dementia might include design of a home or ward, assistive technologies, ambient-assisted living, “dementia friendly communities”, for example.
With the introduction of ‘whole person care’, it’s possible that the care co-ordinator for a person living well with dementia might become a reality.
In this construct, Andy Burnham MP, Shadow Secretary of State for Health, is trying to stop the overhospitalisation (and overmedicalisation) of people.