Home » Posts tagged 'Brian Jarman'
Tag Archives: Brian Jarman
Are we actually promoting the NHS ‘choice and control’ with the current caredata arrangements?
In the latest ‘Political Party’ podcast by Matt Forde, an audience member suggests to Stella Creasy MP that wearing a burkha is oppressive and should not be condoned in progressive politics. Stella argued the case that she can see little more progressive than allowing a person to wear what he or she wants.
The motives for why people might wish to ‘opt out’ are varied, but dominant amongst them is a general rejection of commercial companies profiteering about medical data without strict consent. This is not a flippant argument, and even Prof Brian Jarman has indicated to me that he prefers a ‘opt in’ system:
Patients are not fully informed about how their information will be used. For such confidential data they should have to opt in @legalaware
— BrianJarman (@Jarmann) January 28, 2014
If people are properly told the pros and cons they can decide if they want to accept the cons, for the sake of the pros @sib313 @legalaware
— BrianJarman (@Jarmann) January 27, 2014
There are potential benefits, but also risks and if the risks happen they’re irreversible. Hence it’s safer to have opt-in. @legalaware
— BrianJarman (@Jarmann) January 27, 2014
Opting out can be argued as not being overtly political, though – it is protecting your medical confidentiality. People may (also) have political reasons for doing this, but the choice is fundamentally one about your right to a private family life. The government (SoS) has accepted this, and that is why it is your NHS Constitution-al right to opt out – you don’t have to justify it and if you instruct your GP to do it for you, she must.
It’s argued fairly reliably that section 251 of the NHS Act 2006 maps exactly onto Section 60 of the Health and Social Care Act 2001. Section 60 was implemented the following year under Statutory Instrument 2002/1438 The Health Service (Control of Patient Information) Regulations 2002. It is argued that the Health and Social Care Act 2012 did not modify or repeal those provisions of the HSC Act 2001 or the NHS Act 2006, nor did it modify or repeal any related provision of the Data Protection Act 1998. SI 2002/1438 remains in force. However, noteworthy incidents did occur under this prior legislation, see for example this:
Whatever motive you have for arguing against care.data, whether the whole principle of it, the HSCA removing any requirement for consent, the fact that it is identifiable data being uploaded from GP records (i.e. not anonymised or pseudonymised), or that the data will be made available, under section 251, for both research and non-research purposes, to organisations outside of the NHS, etc, the matter remains that the is no control over your data unless you opt-out.
Proponents of the ‘opt out’ therefore propose their two lines of action: either prevent your identifiable data being uploaded (9Nu0) and so effect a block on the release of linked anonymised or pseudonymised (potentially identifiable) data, which otherwise you cannot prevent or control; or block all section 251 releases (9Nu4), whether or not you apply the 9Nu0 code.
The point is, they argue, that you – the patient – cannot pick and choose, when, to whom, or for what purposes your data will be released. You cannot prohibit your data from being released for purposes other than research, or to organisations out with the NHS. This is completely at odds to the ‘choice and control’ agenda so massively advanced in the rest of the NHS. While it has been argued that the arguments against commercial exploitation of these data should have been made clearer beforehand, it’s possibly a case ‘I know we’re going there, but I wouldn’t start from here.’
Compelling arguments have been presented for the collection of population data. It’s argued wee need population data to do prevention and to monitor equity of access and use. It’s an open secret that the current Government is continuing along the track of privatising the NHS; arguably making it all the more important to have good data so we know what is happening. Having more of this data at all starting in the private sector, under this line of argument, is much less transparent, as it’s hidden from freedom of information from the start.
It’s, however, been argued that “the route to data access” has in fact changed. Under Health and Social Care Act (2012), it was intended that either the Secretary of State (SoS) or NHS England (NHSE) could direct HSCIC to make a new database, and – if directed by SoS or NHSE – HSCIC can require GPs (or other care service providers) to upload the data they hold. care.data represents the single largest grab of GP-held patient data in the history of the NHS; the creation of a centralised repository of patient data that has until now (except in specific circumstances, for specific purposes) been under the data controllership of the people with the most direct and continuous trusted relationship with patients. Their GP.
HSCIC is an Executive Non Departmental Public Body (ENDPB) set up under HSCA 2012 in April 2013. NHS England, the re-named NHS Commissioning Board, was established on 1 October 2012 as an executive non-departmental public body under HSCA 2012. Therefore, to suggest that the government has ‘little control’ over these arm’s-length bodies is being somewhat flimsy in argument – they were both established and mandated to implement government strategy and re-structure the NHS. There are also problems with the “greater good” argument; being paternalistic, the opposition to caredata spread bears similarity to the successful opposition to ID cards. This argument presumes that patients will benefit individually, when – and it ignores the fact that it is neither necessary or proportionate –and may be unlawful under HRA/ECHR – to take a person’s most sensitive and private information without (a) asking their permission first, and (b) telling them what it will be used for, and by who. Nobody is above the law, critically.
The fact is that the data gathered may increment the data available to research but that in its current form, care.data may actually not be that useful – it includes no historical data, for starters. And all this of course ignores the fact that care.data (and the CES that is derived from linking it to HES, etc.) will be used for things other than research, by people and companies other than researchers. That is the linchpin of the criticism. Finally, the Care Bill 2013-14 – just about to leave Committee in the Commons – will amend Section 251, moving responsibility for confidentiality from a Minister (tweets by Ben Goldacre here and here).
Anyway, the implementation of this has been completely chaotic, as I described briefly here on this Socialist Health Association blog. What now happens is anyone’s guess.
The author should like to thank Prof Ross Anderson, Chair of Security Engineering at the Computer Laboratory of the University of Cambridge, Phil Booth and Dr Neil Bhatia for help with this article.
Jeremy Hunt fiddles while Rome or A&E burns, and a smear campaign continues
There is nothing as inevitable as death and taxes, apart from Channel 4 ‘scoops’ on the NHS and Conservative smear campaigns against Andy Burnham.
Ed Miliband’s narrative in the last few weeks or so has been about ‘facing up to bullies’. In this context, it is hard to imagine that he is going to reshuffle Andy Burnham MP out of Health. It is well known that Burnham knows this brief backwards, and is considering how to throw forward the issues about NHS financing with introducing innovative ‘whole person care’ to remould the design of primary and secondary care services.
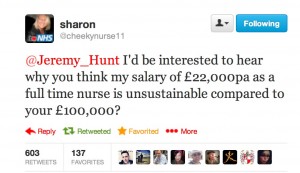
You would have thought that Channel 4 and the Conservative Party would be more interested ‘in the national interest’ about the fact that cuts in the NHS are leading to over-pruned staff, and this can risk patient care. You would have thought that they would have been interested in a debate about a £3bn top-down reorganisation and £2bn ‘efficiency savings’ pumped back to the Treasury (not frontline care). This issue of pay unsurprisingly has demoralised NHS staff in comparison to NHS managers who have received a formidable pay increase.
This has struck a raw nerve with some people especially:
It is all part of a relentless campaign of attacks on the NHS, in the name of ‘investigative journalism’ where the evidence is either missing or distorted to suit the purposes of the broadcaster.
Dr Jacky Davis said of the previous Channel 4 programme, not the report last night, on the “Our NHS” blog:
On September 11th Channel 4 news broadcast a lengthy piece on the NHS, ominously entitled ‘Death on the Wards’. It presented new figures from Professor Sir Brian Jarman about alleged high mortality rates in UK hospitals. There was a clear intention to shock the viewers. The ‘s’ word was repeatedly used by the two presenters and after describing Jarman’s figures as ‘absolutely shocking’ Victoria Macdonald then attempted to put the words into the mouth of Sir Bruce Keogh (Medical Director of the English NHS) when she asked him ‘When you saw those data were you shocked?’ To his credit Sir Bruce sensibly claimed that he needed ‘to think about it’, a basic precaution that the broadcasters would have done well to emulate.
The piece was peppered with worrying claims including one that ‘the NHS is fundamentally failing’ along with claims about patients’ likelihood of dying in a UK hospital as opposed to one in the USA. Finally the presenter compared the average UK hospital with the Mayo Clinic in the US (one of the world’s most prestigious hospitals with an annual revenue of over $8 billion) without any suggestion that comparing a Mini to a Rolls Royce might be ingenuous at best and negligently misleading at worst. This was followed by a panel discussion involving Professor Jarman, Tory MP Charlotte Leslie and [Corrected: this should have read a 'a representative'] of Cure the NHS which was set up after the Mid Staffs disaster. Not a single person to speak up for the NHS or question the data.
Instead, all of this gives an appearance of a message which is being controlled very strongly from Conservative Central Office, though media outlets will of course strongly deny this. Many viewers are sick of reporting of this which is either inaccurate or misses out half of the relevant evidence, with the obligatory appearance from Brian Jarman whose research has been strongly criticised in the medical press. It is common knowledge that the BBC is accused to have devoted hardly any time to accurate, complete and balanced reporting of the acceleration in NHS privatisation, as shown in minimal coverage of a rally in Manchester recently which had attracted 60,000 people.
And yet the true facts are disgusting as to what has actually happened to acute care under this Government’s watch. The number of A&E units missing targets has trebled in a year, as the Government was accused of presiding over an unprecedented “summer A&E crisis”. Between July and September, 39 departments failed to meet the Government’s key target of seeing 95 per cent of patients within four hours, new quarterly figures from NHS England show. Last year only 14 units missed the target for the same period.
It is reported that the Shadow (and former) Health Secretary “Andy Burnham is facing calls to quit after claims he tried to “block” the publication of a devastating report into hospital neglect before the last election”, but in fact these “calls” have come from Tory MPs and a very unpleasant media campaign from certain recurrent protagonists in the media. Nothing would give these people greater delight than ‘gaining a scalp’ when they should be sorting out the mess of service provision of acute medical care in England.
It is also reported that, “Britain’s most powerful civil servant Cabinet Secretary Sir Jeremy Heywood was last night examining whether he needs to set up a Whitehall investigation into whether civil servants breached their code of conduct.”
However this is only because he has been written to. If Heywood has read the letter, he will indeed be considering this issue. He has not decided to investigate this issue yet.
A set of emails were released after Conservative MP Stephen Barclay made a Freedom of Information request to the Care Quality Commission, relating to the Basildon and Thurrock University Hospitals NHS Foundation Trust. Barclay has campaigned on this issue vocally in the past (see for example his article in the Telegraph “The only way to cure the NHS is to change the way we police failures”). The terminology of “cure the NHS” is also striking given the name of the campaigning group “Cure the NHS“, the leader of which was indeed cited by Jeremy Hunt in parliament in one of his numerous speeches demoralising current staff in the NHS. This patient campaigning group – like Channel 4 and the BBC – has also been keen in the past to quote Brian Jarman’s statistics which have received widespread criticism in the academic press. Mid Staffs Foundation Trust is now set to ‘dissolve’. All the sensationalist bravura has actually achieved absolutely nothing in itself.
The awful spectacle of this whole political debacle is that in English health policy this is all incredibly important. Phil Hammond (GP not Secretary of State for Defence) and Heather Wood have both been instrumental in bringing to the fore what had tragically happened to this Trust, and what does need to be remedied in parts of the NHS, for example.
Isabel Hardman, in a narrative which now sounds like intensely boring stuck record, reports that:
The knives are clearly out for the Shadow Health Secretary – and if MPs are calling for him to resign just before a reshuffle, it suggests they want to leave him wounded in the run-up to the 2015 election, rather than leave his post.”
But reporting malicious gossip rather than English health policy is clearly not going to benefit the patients of NHS England.
The problem, is that the central claim – that Burnham himself personally engaged in a ‘cover up’ – might well be potentially legally defamatory on the balance of probabilities under English law.
On the information publicly provided by Andy Burnham in a ‘Labour List’ post, provided as he was totally fed up with the gun-ho nature of the smears, it appears that there is prima facie no evidence of a cover-up. There is only evidence that there was anger at CQC/DH protocols not being observed. (THIS IS NOT AN OFFICIAL LEGAL OPINION).
Indeed, there are wider issues about the legitimacy of the need to publish potentially defamatory information in such a hurry, ahead of a reshuffle, under the “Reynolds Criteria”.
But there is currently a long-running dispute in the law whether such comments should be covered by defences such as legal parliamentary privilege. Hence Burnham’s litigation experts are asking Jeremy Hunt to ‘put it to proof‘.
A Conservative health spokeswoman, and countless people in the past ad nauseam, is reported to have said there was “overwhelming evidence that Labour ministers leant on the quality watchdog to tone down and cover up NHS failure for political purposes”.
In the absence of knowing what the civil service were ‘up to’ at the time (and many of these staff might have moved on) at the Department of Health, it is actually impossible to make this claim.
The irony is that, when the PM addressed Parliament originally over the Francis Report into Mid Staffs, he said categorically that he ‘did not want scapegoats’, despite patient campaigners having a hit list or ‘wall of shame’ of those people which they wished retributive justice to be administered on.
In his centrepiece Conservative party conference speech this week, Hunt lambasted Burnham for “covering up” poor care during his time as health secretary yet again despite the fact these smear tactics have failed to impact any polling on the NHS for Labour and the Conservatives. And in the meantime performance of A&E actually has been reported to deteriorate.
Hunt repeated the narrative of Channel 4, in regurgitating Jarman’s statistics which many have panned in the academic press, and ratcheting up the pace on Twitter. It has long been appreciated he does his own tweets, in the same way that Andy Burnham does.
Burnham insisted that those “damaging emails” showed only that he was concerned that rules about disclosure had been broken.
In a furious open letter, Burnham wrote:
It is impossible to see how you can claim this mounted to a cover-up. I therefore ask you, by the end of today, to provide me with evidence to substantiate your assertion.If you fail to provide such evidence, I will require a full retraction and public apology. If that is not forthcoming I will consider further action.
However, Baroness Young, who is now chief executive of Diabetes UK, last week was at the Conservative Party conference in Manchester, and responded to Mr Hunt’s claim at a debate held by the think tank “Reform”:
BY:
“I just want to put the record straight because within your speech today, Jeremy, particularly the press release that accompanied it, you continued to misrepresent my evidence to the Francis inquiry and to misrepresent that the situation the letter from Andy Burnham to me and I really am very angry about it.
“I have already written to you and the prime minister previously to point out the fact that the way that you are abusing my evidence to the Francis inquiry in a partial manner misrepresents entirely the situation that existed at that time.
“I think it’s unfortunate that you’ve used a partial quote from me to imply that the CQC was pressurised into concealing this because it simply was not the case. If I was pressurised at all either politicians or by civil servants it was about the process by which CQC went about its regulatory work. At no point was I ever asked to or indeed did tone down the evidence. I really do find it very unsatisfactory on a number of counts that this continues to be pedalled in public and in newspapers. I’m not sure what it is that you don’t understand about me saying I was never put under pressure to subdue the findings of the CQC as a regulator.
“The most distressing part of this is that we are constantly harking back to what the political classes were doing rather than looking forward and giving CQC and others involved in healthcare as much support as possible in improving and building on the problems of health systems rather than constantly undermining the work that was done in the past.”
JH: “I really do need to respond to that. Do you have the words that you said under oath to the Francis inquiry?”
BY: “I have a full copy of the Francis inquiry.”
JH: “Will you read out the words you said to Francis inquiry.”
…
BY: “I was paraphrasing the best bit about the pressure coming from civil servants rather than ministers and I’m now quoting ‘it was primarily because what we wanted to do (ie our regulatory processes) not so much what we wanted to say because I don’t think we were really under a lot of pressure not to say things’. That cannot be clearer, that was from my Francis evidence a long, long time before this hoo-ha arose.”
JH: “First of all I think it was deeply wrong that you should have been under pressure from civil servants, who are under the orders of ministers, in terms of what you do in connection to the whistleblowing issue.
None of this is helping with the morale at the current situation in Staffordshire, especially with regards to recruiting excellent staff to work in their units. Mid Staffs and surrounding areas have also in the meantime embarked on successful programmes of cultural change, and therefore this slamming of Mid Staffs in the media can only be seen for petty nasty electoral reasons. And, most significantly, many people in Staffs themselves are now very upset. It is said that Sir Hugo Mascie Taylor, involved in the current Staffs reconfiguration, has repeatedly made the point that the key reason for the propsals to change services here are because of the reputational damage inflicted on Mid Staffs, and the way this has made recruitment more difficult.
It also very much emerges that, if there is anything to investigate, it is the civil service culture of the Department of Health. And meanwhile none of this helps the current crisis in A&E. Despite the government’s pledge to protect frontline services with real-terms increases in funding, Monitor, the NHS watchdog, has proposed that in 2014-15 hospitals should be paid 4% less for operations than they were the previous year. While hospitals were braced for a cut of about £1bn in funding, the Foundation Trust Network, which represents all 160 hospital trusts in England, calculates that Monitor is now asking for another £500m in savings – roughly £3m from each trust.
Chris Hopson, chief executive of the Foundation Trust Network, said cuts to frontline services would be deeper than expected and questioned whether the NHS could invest in much needed changes to the way hospital services work, as had been recommended by the Francis report into failings at Mid Staffordshire NHS Trust. The need to correct funding shortfalls was also identified in the Keogh report on mortality, recently, in 14 NHS Trusts. Indeed, countless studies have shown a link between unsafe levels of staffing and poor patient safety, and this is the real debate. He is quoted as follows:
The level of efficiency savings the NHS has delivered over the last three years is unprecedented, but this level of performance cannot be sustained year on year till 2021. We need a reality check here – in the end you get what you pay for, and trusts can’t perform miracles out of thin air.
And actual staff are totally sick of it all now.
The head of health at the union Unite, Rachel Maskell, is reported to have said:
Jeremy Hunt is responsible for either undermining the Treasury position or trying to act in an even more draconian way than the Treasury with regards to staff who work across the NHS. He blames the staff on a regular basis; now he wants to further cut their terms and conditions.
Mark Porter, chairman of the BMA Council, is also reported to have said:
Doctors fully recognise the economic constraints the NHS is facing, but for the government to imply that unless NHS staff endure what is effectively another year of pay cuts they will put patient safety at risk is insulting at best, given doctors are working harder than ever before and have borne the brunt of the government’s efficiency drive.
Correction: Perhaps some other things are inevitable after all. The NHS ‘efficiency drive’ will continue, the smear campaign against Andy Burnham will continue, the malaise over what is happening to the NHS will continue for a bit, Brian Jarman’s methodologically problematic weak statistics will continue to get quoted on the BBC and Channel 4.
But – in a latest twist to the story, Andy Burnham’s (Labour) lawyers are completing the pre-action protocol for civil litigation against Jeremy Hunt on the law of the tort of defamation under English law.
If this all proceeds to formal legal proceedings, I will not be able to make any comment on it.
And Andy Burnham will still be in a job.
The war over Jarman’s data
1. Introduction
The fiasco over the HSMR is now of totemic proportions.
In many ways, the battle over the Channel 4 headline story of Wednesday saying “for the first time” that hospital mortality rates in the UK were considerably higher than other jurisdictions has become more totemic than the notorious “War over Jennifer’s Ear“. To give him credit, Prof Brian Jarman (@Jarmann) is always very helpful on Twitter. There can be a temptation to play the man not the ball, but Jarman has a very distinguished professional record as a member of the medical profession as part of the St. Mary’s Hospital/Imperial College centres in London. By his own admission, his first degree was in physics, and his PhD on Fourier analysis of seismic wave propagation. He changed to medicine age 31. There is absolutely no doubt that Prof Brian Jarman is an incredibly bright man. On the basis of presumption of innocence under English law, it is critical to assume that Prof Jarman did not intend to mislead the general public through the reporting of his claims over hospital mortality statistics. This is indeed consistent with the positioning of excellent patient safety campaigning groups who overall feel that a discussion over the statistics is a genuine offense to the misery of relatives (and families) who have suffered. There is perhaps an issue of whether Jarman was particularly reckless in how such data might be presented before a fearful public, and possibly how Jarman’s data are presented in the media, following the Telegraph and similar reports and this week’s Channel 4 presentation, in the future might be the best surrogate guide to Jarman’s true intentions.
The Channel 4 website report, “NHS hospital death rates among worst, new study finds“, is here.
“NHS chief Sir Bruce Keogh says he is taking very seriously figures revealed by Channel 4 News which show that health service patients are 45 per cent more likely to die in hospital than in the US.”
According to this Channel 4 website report:
“The figures prompted Sir Bruce Keogh, medical director of the NHS, to say he will hold top-level discussions in a bid to tackle the problems. I want our NHS to be based on evidence. I don’t want to disregard stuff that might be inconvenient or embarrassing…I want to use this kind of data to help inform how we can improve our NHS,” he told Channel 4 News.I will be the first to bring this data to the attention of clinical leaders in this country to see how we can tackle this problem.”
2. The methodology of the “hospital standardised mortality ratios” (HSMRs)
The methodology of the ‘hospital standardised mortality ratios‘ is well known to Sir Bruce Keogh. The wider criticisms of the HSMR have been extensively discussed in the medical press, see for example “Using hospital mortality rates to judge hospital performance: a bad idea that just won’t go away” (in the BMJ, April 2010).
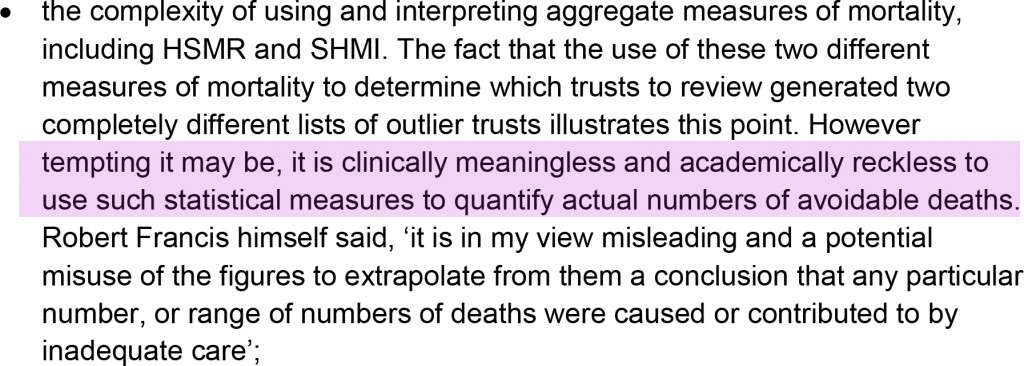
In the widely publicised “Review into the quality of care and treatment provided by 14 hospital trusts in England: overview report” published from earlier this year, it is stated:
Jarman’s ‘discovery’, in a flourish worthy of ‘Gone with the Wind’ perhaps, is described thus:
“What he found so shocked him, he did not release the results. Instead, he searched – in vain – for a flaw in his methodology and he asked other academics to see if they could find where he might have gone wrong. They, too, could not find fault.”
The question remains: what happened in the intervening nine years which prevented any activity culminating in professional peer review?
3. These data were indeed presented as far back as 2004
The Channel 4 reporting was sensational as illustrated in this excerpt from the Channel 4 report by Victoria Macdonald:
“So now he is releasing the findings. And they are shocking. The 2004 figures show that NHS had the worst figures of all seven countries. Once the death rate was adjusted, England was 22 per cent higher than the average of all seven countries and it was 58 per cent higher than the best country.”
The data are even known to the Department of Health as evidenced by Jarman himself here:
 A tweet shared by Brian Jarman provides a link to the presentation of the data in 2004.
A tweet shared by Brian Jarman provides a link to the presentation of the data in 2004.
The starting point of the report was to go to the Mayo Clinic:
“Because of confidentiality issues we are not allowed to name the other countries. But America stands out in the data for its lower mortality rates. So we went to find out why. At the Mayo Clinic Hospital in Phoenix, Arizona, they are in the best two per cent in the country. It is an impressive hospital, with piano music playing in the lobby and sunshine streaming into the rooms.”
4. Concerns about the data
Any (reasonable) reviewer of these data, particularly given the bold and significant nature of the claims therein, will be concerned about the ‘quality’ of the data, in much the same way Jarman is concerned about the ‘quality’ of healthcare. This is particularly so if one adopts the approach of ‘treating the data’ rather than ‘treating the clinical patient’, which many clinicians would not advocate anyway in isolation.
This ‘confidentiality issue’ about the manner in which these data were provided is confirmed in a recent tweet by Jarman:
 In the absence of clarity of what these confidentiality issues precisely are, it is hard to deduce fully what it is exactly that is so prohibitive for Jarman publishing his data. Many senior academics indeed converge on the notion that the publication of these data would be a useful contribution to the field, provided that the publication were properly refereed from two perspectives. These perspectives are that the statistical techniques used are sound. The second perspective is from a clinician’s perspective that the correct public health policy issues have been identified, and analysed correctly using available global evidence, and the citation of relevant background assumptions and confounding factors. Whilst it is hard to conceive that Governments have been withholding publication of data on public policy grounds (and arguably there is no more important a policy issue than a country’s mortality), it is possible that individual private companies may not wish to disclose fully confidential data. In the private sector even, such lack of disclosure of confidential data has led to accusations of fraud and discussion of mitigation, because of the sensitivity of such data to the markets in the dividend signalling theory. Academics have suggested to Jarman on Twitter that it might be possible to publish these data using the techniques of anonymisation or pseudo-anonymisation, as is prevalent in contemporaneous scientific research, but again no answer has been readily provided.
In the absence of clarity of what these confidentiality issues precisely are, it is hard to deduce fully what it is exactly that is so prohibitive for Jarman publishing his data. Many senior academics indeed converge on the notion that the publication of these data would be a useful contribution to the field, provided that the publication were properly refereed from two perspectives. These perspectives are that the statistical techniques used are sound. The second perspective is from a clinician’s perspective that the correct public health policy issues have been identified, and analysed correctly using available global evidence, and the citation of relevant background assumptions and confounding factors. Whilst it is hard to conceive that Governments have been withholding publication of data on public policy grounds (and arguably there is no more important a policy issue than a country’s mortality), it is possible that individual private companies may not wish to disclose fully confidential data. In the private sector even, such lack of disclosure of confidential data has led to accusations of fraud and discussion of mitigation, because of the sensitivity of such data to the markets in the dividend signalling theory. Academics have suggested to Jarman on Twitter that it might be possible to publish these data using the techniques of anonymisation or pseudo-anonymisation, as is prevalent in contemporaneous scientific research, but again no answer has been readily provided.
5. The utility (and futility) of cross-jurisdictional comparisons
The financial situation of the Mayo Clinic itself is known to be strong, with a colossal amount of income per patient at the Mayo Clinic compared to a patient in the English National Health Service:
“But a copy of the clinic’s consolidated financial report obtained by the Pioneer Press shows total revenue of $8.48 billion in 2011. That was an increase of $533 million, or nearly 7 percent over revenue of $7.94 billion during the previous year. Income from operations increased by 18 percent, growing from $515.3 million in 2010 to $610.2 million last year, according to the financial report. “This is very strong,” said Steve Parente, a professor of finance at the University of Minnesota’s Carlson School of Management. “In terms of pure operations, they’re doing quite well….Their grants and contracts are going up, too,” said Parente, who reviewed the financial report.””
A pertinent issue is whether the hospital episode statistics are themselves reliable. Prof Jarman quoting other reports feels that they are reliable (see tweet). However, this is in contradistinction from other reports sourced at the Royal College of Physicians of London (as described in a previous Guardian article):
“Currently the public can use the NHS Choices website to help them choose a hospital for treatment. NHS Choices, and the information used by Dr Foster, is based on “Hospital Episode Statistics” (HES) data, which the NHS says is “authoritative and essential”. However, NHS insiders say the information, usually collected by administrative staff from patient records, is unreliable.Professor John Williams, director of the health information unit at the Royal College of Physicians, carried out a study into HES data and found a significant number of operations were recorded inaccurately. He has called for a change in the way data is collected, saying flaws in the HES database were exposed as long ago as 1982.”
Hospital death rates, particularly if followed over time, can give useful warning of problems, as Sir Bruce Keogh has stated. Dr Jacky Davis in a subsequent Channel 4 interview (see below) was asked about the ‘smoke detector’ use of HSMRs as being pivotal in warning about problems.
 It is, for example, argued that the issues in Mid Staffs would not have been exposed, but for the HSMRs. This argument is relatively convincing, but it is also argued that any reader of the local papers in Mid Staffs would have been aware of the problem long before the official HSMR figures emerged. Dr Jacky Davis in her C4 interview on Thursday, in reply, admitted that this ‘smoke detector argument’ might be true, but explained further ‘if there’s smoke going up you have to make sure – is there a fire there?‘. This is intuitively true, as well as the notion that the mortality rate in any given hospital will depend on the numbers of people who are actually dying ‘on site’. In general of course variation of data in other jurisdictions are likely to relate to regional variation of the care of palliative care patients, for example, and also where the funding for medical care is coming from (for example, the location of death may be an artifact of the conditions of private insurance funding.)
It is, for example, argued that the issues in Mid Staffs would not have been exposed, but for the HSMRs. This argument is relatively convincing, but it is also argued that any reader of the local papers in Mid Staffs would have been aware of the problem long before the official HSMR figures emerged. Dr Jacky Davis in her C4 interview on Thursday, in reply, admitted that this ‘smoke detector argument’ might be true, but explained further ‘if there’s smoke going up you have to make sure – is there a fire there?‘. This is intuitively true, as well as the notion that the mortality rate in any given hospital will depend on the numbers of people who are actually dying ‘on site’. In general of course variation of data in other jurisdictions are likely to relate to regional variation of the care of palliative care patients, for example, and also where the funding for medical care is coming from (for example, the location of death may be an artifact of the conditions of private insurance funding.)
However, arguably reliable comparison of such data internationally is fraught with difficulties, as Prof Walter Holland and colleagues found out when they published the European Atlas of Avoidable Deaths in 1988. Prof Holland is an eminent expert in public health and a visiting Chair at the London School of Economics. Since total mortality rates in the UK are similar, or lower, than in the United States, as a large proportion of the population in both countries die in a hospital such a difference seems unlikely, according to Holland. To compare hospital mortality rates between hospitals, whether in one or more countries, arguably it is necessary to take into account such factors as availability of discharge facilities, e.g. hospices, hospital admission criteria, length of time in hospital, and many other procedural and cultural factors, according to the eminent Holland.
Comparison of outcomes for individual conditions is even more difficult because of differences in diagnostic and coding procedures which have been illustrated many times. In a famous paper “Evidence of methodological bias in hospital standardised mortality ratios: retrospective database study of English hospitals” published in the BMJ in 1999, this coding problem was identified thus:
“Our findings suggest that the current Dr Foster Unit method is prone to bias and that any claims that variations in standardised mortality ratios for hospitals reflect differences in quality of care are less than credible.8 12 Indeed, our study may provide a partial explanation for understanding why the relation between case mix adjusted outcomes and quality of care has been questioned.24 Nevertheless, despite such evidence, assertions that variations in standardised mortality ratios reflect quality of care are widespread,25 resulting, unsurprisingly, in institutional stigma by creating enormous pressure on hospitals with high standardised mortality ratios and provoking regulators such as the Healthcare Commission to react.20“
In our jurisdiction, for example, the proportion of surgery done as elective day cases is reported to be quite high. Unfortunately the data presented by Jarman in his original 2004 presentation and the Wednesday Channel 4 package are inadequate alone for anyone to determine the validity of the conclusions or the methods used. This is a striking media story but unfortunately has not been subjected to proper scrutiny. This will be essential for policy in English health policy, particularly in the critical issue of patient safety, to progress; and progress it must not on the basis of emotion or soundbites.
6. A wider issue
Prof Jarman has consistently stated that he is in favour of a NHS funded by taxation, which is different from the attitude of libertarians and the Mayo Clinic, as shown here:
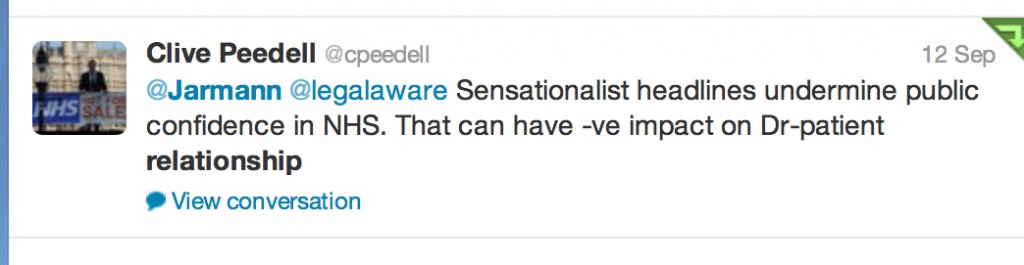
 Critics of Jarman have felt that his criticisms of some foci of the delivery of care undermine the daily work of clinicians across the country, and may even undermine the doctor-patient relationship so pivotal for the work of clinicians in real life (see for example here).
Critics of Jarman have felt that his criticisms of some foci of the delivery of care undermine the daily work of clinicians across the country, and may even undermine the doctor-patient relationship so pivotal for the work of clinicians in real life (see for example here).
 Jarman and supporters feel, however, that for ages criticisms of poor quality of care in the NHS have been suppressed, and that there is a professional duty to speak up about such poor care to improve the NHS. However, critics of Jarman feel that such an approach ‘in the wrong hands’ is merely providing ammunition for further marketisation and privatisation of the NHS, and that Jarman is carrying out the ‘handy work’ for politicians to see this ideological goal come into fruition.
Jarman and supporters feel, however, that for ages criticisms of poor quality of care in the NHS have been suppressed, and that there is a professional duty to speak up about such poor care to improve the NHS. However, critics of Jarman feel that such an approach ‘in the wrong hands’ is merely providing ammunition for further marketisation and privatisation of the NHS, and that Jarman is carrying out the ‘handy work’ for politicians to see this ideological goal come into fruition.
 This debate is intense with accusation and counter-accusations, but the volume of criticism regarding the NHS article headlining Channel 4 news on Wednesday is a testament to how the public will not accept unqualified comparisons of the NHS with other jurisdictions either. The ensuing analysis has further put the spotlight on Jarman’s data, but this can be no bad thing either. The medical and nursing professions, and their regulatory bodies, will wish for all involved to maintain the reputation, trust in and confidence in their work, but this is only possible if the work is ‘fit for purpose’. Politicians can slag off the NHS to an extent to which clinicians would likely become disciplined for, and it is this contradiction which raises eyebrows.
This debate is intense with accusation and counter-accusations, but the volume of criticism regarding the NHS article headlining Channel 4 news on Wednesday is a testament to how the public will not accept unqualified comparisons of the NHS with other jurisdictions either. The ensuing analysis has further put the spotlight on Jarman’s data, but this can be no bad thing either. The medical and nursing professions, and their regulatory bodies, will wish for all involved to maintain the reputation, trust in and confidence in their work, but this is only possible if the work is ‘fit for purpose’. Politicians can slag off the NHS to an extent to which clinicians would likely become disciplined for, and it is this contradiction which raises eyebrows.
7. Conclusion
Notwithstanding, it is clear that the fundamental mistake is that it was perceived by some that the Channel 4 report represented irresponsible journalism in that the assumptions were not accurately stated, it suffered from bias by omission by lack of explanation about the surrounding issues (not least presenting Keogh as somebody who tacitly endorsed the uncritical issue of the HSMR, which is false), and basically left a very ugly taste in many people’s mouths. It did no favours for the reputation of, trust in, and confidence in Channel 4 news reporting either that night (Wednesday), but in fairness to Channel 4 news they hosted an interview with @DrJackyDavis – Co-Chair of the NHS Consultants Association – the following evening (Thursday).
However, it is impossible to deny the value of the discussion which has ensued after this dreadful report. The policy situation is precarious, aggravated by certain Ministers of the Crown lying blatantly in the whole saga over a period of months in the current Government.
The Health and Social Care (2012) was not about patient safety: implications for the Keogh report
The Health and the Social Care Act (2012) is a massive tome. It actually reads, for lawyers who are well acquainted with such statutory instruments, like a huge patchwork quilt of commercial and corporate law strands. While voluminous, at 473 pages, it has two critical clauses. The first is section 75, and its concomitant now famous Regulations, which provides the statutory basis for procurement contracts in the NHS to be put up for price competitive tendering as the default option, thus fixing the NHS in a competitive market of an economic activity. This is of course the mechanism for outsourcing NHS services into the private sector, and indeed the vast majority of contracts have now been won by the private sector. This was widely predicted, as the private sector have skills and resources to make slicker bids, irrespective of the bid they ultimately deliver, to transfer a much higher proportion of “NHS services” into the profit-making private sector. All of this costs the NHS more money sadly, as while it may not matter to you ‘who provides your services’, you’re in trouble if the private provider goes bust, and you’re not paying for anything at anywhere near cost-price because of the mark-up for profit. This section 75 clause acts in tandem with section 164(1)(2A) which allows any NHS hospital to receive up to 50% of its income from private sources. Thus the Act, and the £2.4 NHS “reforms”, have been a bonanza for the private sector, and disastrous from the perspective of a state-provider of universal, comprehensive healthcare.
Patient safety is in fact only mentioned once in the Act, in clause 281. That is in reference to the abolition of the National Patient Safety Agency. The National Reporting and Learning System which was hosted by NPSA has a two year stint at Imperial College Hospital NHS Trust, while a tender process is scoped and developed by the Board. NPSA’s responsibilities concerning patient safety will transfer to the NHS England.
The Health and Social Care Act 2012 (c. 7) is an Act of the Parliament of the United Kingdom. It is the most extensive reorganisation of the structure of the National Health Service in England to date. It proposes to abolish NHS primary care trusts (PCTs) and Strategic Health Authorities (SHAs). The Act’s proposals were not discussed during the 2010 general election campaign and were not contained in the 20 May 2010 Conservative – Liberal Democrat coalition agreement, which declared an intention to “stop the top-down reorganisations of the NHS that have got in the way of patient care”. However, within two months a white paper outlined what the Daily Telegraph called the “biggest revolution in the NHS since its foundation”. The white paper, Equity and Excellence: Liberating the NHS, was followed in December 2010 by an implementation plan in the form of Liberating the NHS: legislative framework and next steps. The bill was introduced into the House of Commons on 19 January 2011, and received its second reading, a vote to approve the general principles of the Bill, by 321-235, a majority of 86, on 31 January 2011.
The British Medical Association opposed the bill, and held its first emergency meeting in 19 years, which asked the government to withdraw the bill and reconsider the reforms. A later motion of no confidence in Lansley by attendees at the Royal College of Nursing Conference in 2011, however, succeeded, with 96% voting in favour of the motion. Nurses have consistently been opposed to the the “efficiency savings” measures being undertaken across the NHS, with many raising concerns of their material impact on frontline medical services. “People will die”, Richard Horton, editor of The Lancet, warned in March 2012, as he predicted “unprecedented chaos” as a result of the reforms, with a leaked draft risk-assessment showing that emergencies would be less well managed and the increased use of the private sector would drive up costs.
The Bill is now Law, and where are the measures to deal with this longrunning problem of patient safety, particularly in the acute setting? There are none. The media was sent into overdrive in portraying the NHS has a “death machine”, despite the best attempts of nurses and Doctors to run the service under difficult conditions. The publication of the damning Keogh Report (“Report”), which spelt out the failings of 14 hospital trusts which did not quote “13,000 “needless deaths” since 2005″, is despite exhaustive pre-briefing to the media. The Report depicts a situation in certain trusts where patient safety is poor, with no reference to what action has been taken by the Government and their civil service to remedy this since the General Election in May 2010, which the Conservatives lost. Sir Bruce Keogh, the NHS’s Medical Director, will describe how each hospital let its patients down through poor care, medical errors and failures in management, but the Report is as if the clinical regulatory bodies do not exist, the General Medical Council, the Nursing and Midwifery Council and the Care Quality Commission. How they have escaped blame for this reported ‘scandal’ is incredible, although one suspects the media will catch up with them eventually. It might be that the media for whatever reason known to them do not feel the clinical regulators are in “the firing line”, despite being supposed to be responsible for patient safety, in the same way that lawyers are not responsible for the global financial crisis despite being supposed to regulated on the safety of financial instruments.
From a management point of view, the Keogh Report serves a function for convincing the public of a need to take patient safety extremely seriously. However, to sell the Keogh Report as “Do you now see the need for the NHS reforms?” maybe hitting a target but missing a crucial point. The NHS reforms are all to do with outsourcing and eventual privatisation of the NHS. They are nothing to do with patient safety, as even right-wing think tanks and their spokesmen have previously conceded in public. In fact, it is worse than that. The £2.4 reorganisation which nobody voted for, but which private healthcare companies extensively lobbied for, was a reckless missed opportunity to put resources into something other than frontline care, and the opportunity cost of this piece of legislation will continue to haunt the general public for many years. Unfortunately, the media and the members of the Establishment, some members of which have tenuous links with the institutional shareholders in private healthcare companies, will be more than aware of this hard fact. The Conservatives are desperate to pin every conceivable woe of the NHS on Andy Burnham, and every interview which Burnham now does must feel like “Groundhog Day” for him. He has nothing much more in his defense. Meanwhile, the Conservatives are exasperated that they have been unable to get the Burnham scalp, but there are as yet unresolved issues about what Government departments have done about NHS complaints in the last three years since May 2010. The bottom line is that the Health and Social Care Act is nothing to do with patient safety: even safety campaigners in the NHS know this, and they know of the even worse battle now facing them, of a fragmented privatised NHS which is even harder to regulate from that point of view. The NHS reforms, and more specifically the Health and Social Care Act which underpins them, have nothing to do with patient safety. More disturbingly, the Keogh report, when eventually published, will not stop ‘another Francis’, and it is entirely the Government’s fault we are in this stupid ridiculous position.