Home » Posts tagged 'Alistair Burns'
Tag Archives: Alistair Burns
An overview of my book ‘Living better with dementia: champions for enhanced communities”.
I hope you find this overview of my book ‘Living better with dementia: champions for enhanced communities’ useful.
It is written by me.
And the Forewords are Prof Alistair Burns, the England clinical lead for dementia, Kate Swaffer (Alzheimer’s Australia, Dementia Alliance International, and University of Wollongong, Australia), Chris Roberts (Dementia Action Alliance Carers Call to Action, Dementia Alliance International), and Dr Peter Gordon (Consultant Psychiatrist in dementia and cognitive disorders, NHS Scotland).
It will primarily assess where we’ve got to, along with other countries, in improving diagnosis and post-diagnostic care, and assess realistically the work still yet to be done.
My thesis will articulate why the ‘reboot’ of the global “dementia friendly communities” must now take account of various issues to be meaningful. It will argue for a difference in emphasis from competitive ‘nudge’ towards universal legal and enforceable human rights promoting dignity and autonomy.
It will also argue that dementia friendly communities are meaningless unless there is a shift in the use of language away from ‘sufferers’ and ‘victims’, while paying tribute to the successful “Dementia Friends” initiative.
It will, further, argue that dementia friendly communities are best served by a large scale service transformation to ‘whole person care’, and provide the rationale for this. A critical factor for enhancing the quality of life of people living better with dementia will be to tackle meaningfully the social determinants of health, such as housing and education.
The thesis will also argue that dementia friendly communities must also value the behaviours, skills and knowledge of caregivers in wider support networks. This is essential for the development of a proactive service, with clinical specialist nursing input deservedly valued, especially given the enormous co-morbidity of dementia.
This title will be published by Jessica Kingsley Publishers, in early 2015.
Chapters overview
Chapter 1 provided an introduction to current policy in England, including a review of the need for a ‘timely diagnosis’ as well as a right to timely post-diagnostic care. This chapter also provided an overview of the current evidence base of the hugely popular “Dementia Friends” campaign run by the Alzheimer’s Society and Public Health England, to raise awareness about five key ‘facts’ about dementia. It was intended that this campaign should help to mitigate against stigma and discrimination that can be experienced by people living with dementia and their caregivers.
Chapter 2 comprised a preliminary analysis of stigma, citizenship and the notion of ‘living better with dementia’. This chapter explained the urgency of the need to “frame the narrative” properly. This chapter also introduced the “Dementia Alliance International” which has fast become a highly influential campaigning force by people living with dementia for people living with dementia.
Chapter 3 looked at the various issues facing the timely diagnosis and post-diagnostic support of people living with dementia from diverse cultural backgrounds, including people from black, Asian and ethnic minority backgrounds, people who are lesbian, bisexual, gay or transsexual, and people with prior learning difficulties.
Chapter 4 looked at the issue of how different jurisdictions around the world have formulated their national dementia strategies. Examples discussed of countries and continents were Africa, Australia, China, Europe, India, Japan, New Zealand, Puerto Rico and Scotland.
Chapter 5 looked at the intense care vs care debate which has now surfaced in young onset dementia, with a potentially problematic schism between resources being allocated into drugs for today and resources being used to fund adequately contemporary care to promote people living better with dementia. An example was discussed of how the policy of ‘Big Data’ had gathered momentum across a number of jurisdictions, offering personalised medicine as a further potential compontent of person-centred care. This chapter also considered the impact of the diagnosis of younger onset dementia on the partner of the person with dementia as well. A candid description was also given about the possible sequelae of the diagnosis of young onset dementia on employment, caregivers, and in social isolation.
Chapter 6 focused on delirium, or the acute confusional state, and dementia. It considered the NICE guidelines for delirium, and the pitfalls in considering the relationship between delirium and dementia in English policy.
Chapter 7 was the largest chapter in this book, and took as its theme care and support networks. An overview of how patient-centred care is different from person-centred care was given, and how person-centred care differs from relationship-centred care. The literature inevitably has thus far focused on the ‘dyadic relationship’ between the person with dementia and caregiver, but a need to enlarge this to a professional in a ‘triangle of care’ and extended social networks was further elaborated and emphasised. Finally, the importance of clinical specialist nurses in ‘dementia friendly communities’ was argued, as well as the Dementia Action Alliance’s “Carers Call to Action”. Different care settings were described, including care homes, hospitals – including acute hospital care, and intermediate care.
Chapter 8 considered eating for living well with dementia. This chapter considered enforceable standards in care homes, including protection against malnutrition or undernutrition. The main focus of the chapter was how people with dementia might present with alternations in their eating behaviour, and how the mealtime environment must be a vital consideration for living better with dementia.
Chapter 9 looked at a particular comorbidity, incontinence. The emphasis was on conservative approaches for living well with dementia and incontinence. Other issues considered were the impact of incontinence on personhood per se, and the possible impact on the move towards an institutional home.
Chapter 10 argued how the needs for people living better with dementia would be best served by a fully integrated health and social care service. This chapter provided the rationale behind this policy instrument in England. The chapter also considered various aspects of what would be likely to make ‘whole person care’ work, including data sharing, collaborative leadership, care-coordinators, responsible and accountable ‘self care’, and the multi-disciplinary team. This chapter also considered how it was impossible to divorce physical health from mental health and social care, and explained the intention of the longstanding drive towards ‘parity of esteem’ in English policy.
Chapter 11 considered the importance of the social determinants of health. A focus of this chapter was on education, and its impact on a person living with dementia. However, the main focus of this chapter was housing, including ‘dementia friendliness, downsizing, and green or public spaces.
Chapter 12 considered whether ‘wandering’ is the most appropriate term. The main emphasis of this chapter were the legal and ethical considerations in the use of ‘global positioning systems’ in enhancing the quality of life of persons with dementia and their closest ones.
Chapter 13 considered a number of important contemporary issues, with a main emphasis on human rights and “rights based approaches”. While there is no universal right to a budget, the implementation of personal budgets was discussed. The chapter progressed to consider a number of legal issues which are arising, including genetic discrimination in the US jurisdiction, dementia as a disability under the equality legislation in England, and the importance of rights-based approaches for autonomy and dignity. Finally, the issue of engagement was considered.
Chapter 14 was primarily concerned with art and creativity. This chapter took as its focus on how living with dementia could lead to art and creativity, and how the cultural needs of people living with dementia could best be furnished through laughter, poetry and art galleries or museums. This focus also looked at the exciting developments in our understanding of the perception of music in people living with dementia, and how music has the potential to enhance the quality of life for a person living well with dementia.
Chapter 15 looked at the triggering of football sporting memories in people living well with dementia. This chapter considered the cognitive neuroscience of the phenomenon of this triggering, and presented a synthesis of how the phenomenon could be best explained through understanding the role of emotional memory in memory retrieval, how autobiographical memories are represented in the human brain usually, the special relevance of faces or even smells such as “Bovril”.
Chapter 16 looked at the impact of various innovations in English dementia policy, giving as examples including service provision (such as the policy on reducing inappropriate use of antipsychotics or the policy in timely diagnosis) and research. This chapter also contemplated the principal factors affecting how innovations can become known, and what ultimately determines their success.
Chapter 17 looked at how leadership could be promoted by people living with dementia. This chapter considered who might lead the change, where and when, and why this change might be necessary to ‘recalibrate’ the current global debate about dementia. This chapter considered how change might be brought about from the edge, how silos might be avoided, the issue of ‘tempered radicals’ in the context of transformative change to wellbeing as an outcome; and finally how ‘Dementia Champions’ are vital for this change to be effected.
Please note that Beth is not endorsing this book – this image is entirely separate and is taken from the main event for G8 dementia – we’re all proud of Beth’s work meanwhile!
Living well with corporate capture. What is the future of the Prime Minister’s Dementia Challenge?
“Citizens have become consumers with status proportional to purchasing power, and former public spaces have been enclosed and transformed into private malls for shopping as recreation or “therapy.” Step by step, private companies, dedicated to enriching their owners, take over the core functions of the state. This process, which has profound implications for health policy, is promoted by politicians proclaiming an “ideology” of shrinking the state to the absolute minimum. These politicians envisage replacing almost all public service provision through outsourcing and other forms of privatisation such as “right to provide” management buyouts. This ambition extends far beyond health and social care, reaching even to policing and the armed forces.”
And so write Jennifer Mindell, Lucy Reynolds and Martin McKee recently about ‘corporate capture’ in the British Medical Journal.
Alistair Burns, England’s clinical lead on dementia, recently concluded a presentation on the clinical network for London with the following slide:
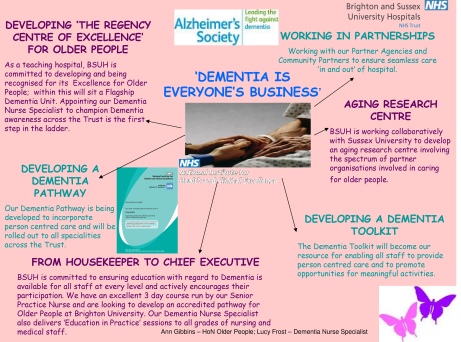
Alistair clearly does not mean ‘Dementia is everyone’s business’ in the “corporate capture” sense. Instead, he is presumably drawing attention to initiatives such as Brighton and Sussex Medical School’s initiative to promote dementia awareness at all levels of an organisation (and society).
The comparison with diabetes is for me interesting in that I think of living well with diabetes, post diagnosis, as conceptually similar to living well with dementia, in the sense that living well with a long term condition is a way of life. And with good control, it’s possible for some people to avoid hospital, becoming patients, when care in the community would be preferred for a number of clinical reasons. Where I feel the comparison falls flat is that I do not think that it is possible to measure outcomes for living well with dementia easily. Sure, I have writen on metrics used to measure living well with dementia, drawing on the work of Sube Banerjee, Alistair’s predecessor. It might be possible to correlate good control with a blood test value such as the HBA1c, and it steers the reward mechanism of the NHS for rewarding clinicians for failure of management (e.g. laser treatment in the eye, foot amputation, renal dialysis), but the comparison needs some clinical expertise to be pulled off properly. The issue of breaking down ‘barriers’ between primary and secondary care is an urgent issue, and ‘whole person care’ or ‘integrated care’ may or may not help to facilitate that. But a future government must not get too enmeshed in sloganising if it means forgetting basic requirements of foot soldiers on the ground, such as specialist dementia nurses including Dementia UK’s ‘Admiral nurses’.
But the question of who gives the correct diagnosis of dementia, or even verifies it, won’t go away.
Having done Dementia Friends myself, a Public Health England the Alzheimer’s Society joint initiative, I feel the initiative is extremely well executed from an operational level. I think it’s pushing it for a member of the public to think that an old and doddering lady crossing the lady might have dementia and requires help, as medicalising ageing into dementia is a dangerous route to take. The £2.4 million programme is funded by the Social Fund and the Department of Health. Public Health England are planning to undertake an evaluation of the Dementia Friends Campaign launched on 7 May 2014, which will include tracking data and prevention message testing.
There are a number of important clinical points here. There are crucial questions as to whether persons themselves with a possible diagnosis, friends and/or families themselves want a diagnosis of dementia. A diagnosis of dementia in anyone’s book is a life-changing event. The concerns of the medical profession have been effectively rehearsed. Notwithstanding, the ambition that, by 2015, two thirds of the estimated number of people with dementia should have a diagnosis, with appropriate post diagnostic support has been agreed with NHS England. To support GPs and other primary care staff, a Dementia Roadmap web-based tool has been commissioned by the Department of Health from the Royal College of General Practitioners. The roadmap has now been officially launched, and will provide a framework that local areas can use to provide local information about dementia from health, social care and the third sector to assist primary care staff to more effectively support patients, families and carers from the time of diagnosis and beyond. Feedback from relevant stakeholders will be most interesting.
People with dementia need to be followed up across a period of time for a diagnosis of dementia to be reliably made, and ‘in the right hands’, i.e. of a specialist dementia service. Whilst NHS England are working with those areas with the longest waits, with the aim of ensuring that anyone with suspected dementia will not have an excessive wait for a timely assessment, there has to be monitoring of who does that timely assessment and whether it produces an accurate result. At an extreme example, clinical diagnoses of rarer dementias, particularly younger onset, can only be done effectively by senior physicians with reference to two clinical histories, two clinical examinations, neuroimaging (e.g. CT, MRI, or even fMRI or SPECT), lumbar puncture/cerebrospinal fluid (if not contraindicated), cognitive psychology, EEG, or even – extremely rarely – a brain biopsy. But this would be to propose an Aunt Sally argument – many possible cases of dementia can be tackled by primary care with appropriate testing perhaps in the future, and certainly adequate resources will need to be put into primary care for training of the workforce. Or else, it is literally a ‘something for nothing’ approach. Some people have ‘mild cognitive impairment’ instead, and will never progress to dementia.There are 149,186 dementia friends currently. This number is rapidly increasing. The goal is one million.Furthermore, there are many people given a diagnosis of dementia while alive who never have it post mortem. And the diagnosis can only be definitively made post mortem. Seth Love’s brilliant research (and he is an ‘Ambassador’ to the Alzheimer’s BRACE charity) is a testament to this. Anyway, NHS England and the Department of Health are working with the Royal College of Psychiatrists to encourage more Memory Services to become accredited.
And when is screening not officially screening? This continues to require definition in England’s policy. The original Wilson and Jungner (1968) principles have appear to have become muffled in translation. The CQUIN has led to over 4,000 referrals a month, but this will only contribute to improving diagnosis rates for dementia if this is not producing a tidal wave of false positives. For quarter 3 2013/14, 83% of admitted patients were initially assessed for potential dementia. Of those assessed and found as potentially having dementia, 89% were further assessed. And of those diagnosed as potentially having dementia, 86% were referred on to specialist services. But we do need the final figure. This policy plank for me will also go back to the issue of whether policy is putting sufficient resources into the diagnostic process and beyond. Stories of people being landed with a diagnosis out of nowhere and given not much further information than an information pack are all too common. A well designed system would have counselling before the diagnosis, during the diagnosis, and after the diagnosis.
Ideally, an appointed advisor would then see to continuity of care, allowing persons with dementia to be able to feel confident about telling their diagnosis to friends and/or family. The advisor would ideally then give impartial advice on social determinants of health, such as housing or education. Policy may be slowly moving in this direction. In April 2014 NHS England published a new Dementia Directed Enhanced Service (DES) for take up by GPs to reward practices for facilitating timely diagnosis and support for people with dementia. Patients who have a diagnosis of dementia will be offered an extended appointment to develop a care plan. The care planning discussion will focus on their physical and mental health and social needs, which will include referral and signposting to local support services. From 10 signatories in March 2012, to date, there are now 173 organisations representing nearly 3,000 care services committed to delivering high quality, personalised care to people with dementia and their carers.
But all this requires money and skill. There is no quick fix.
The areas of action for the Prime Minister’s Dementia Challenge are: dementia friendly communities, health and care and improving research.
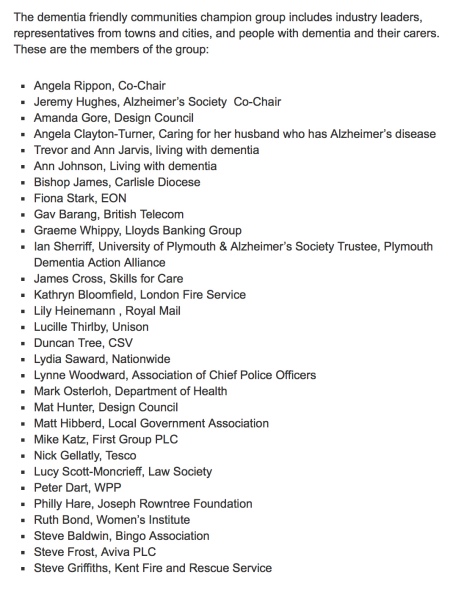
In November 2012, The Secretary of State for Health announced a £50 million dementia-friendly environments capital investment fund to support the NHS and social care to create dementia-friendly environments. The term ‘dementia friendly communities’ is intrinsically difficult, for reasons I have previously tried to introduce. A concern must be the ideology behind the introduction of this policy in this jurisdiction. The emphasis has been very much on making businesses ‘business friendly’, which is of a plausible raison d’être in itself. This, arguably, is reflected in the list of chief stakeholders of the dementia friendly communities champion group.
It happens to fit very nicely with the Big Society and the ‘Nudge’ narrative of the current government. But it sits uneasy with the idea that it is in fact a manifestation of a small state which bears little responsibility apart from overseeing at an arm’s length a free market. The critical test is whether this policy plank might have improved NHS care. 42 NHS and 74 Social Care National pilot schemes were approved in June 2013 as national pilots. Most of the projects have now been completed, and they will be evaluated by a team of researchers at Loughborough University over the coming months. The evaluation will provide knowledge and evidence about those aspects of the physical care environment which can be used to provide improved care provision for people with dementia, their families and carers. But the policy has had some very exciting successes: for example the ‘Sporting Memories Network’, an approach based on the neural re-activation of sporting autobiographical memories, recently scooped top prize for national initiative in the Alzheimer’s Society Dementia Friendly Communities Awards 2014.
And meanwhile, the care system in England is on its knees. Stories of drastic underfunding of the care system are extremely common now. An army of millions of unpaid family carers are left propping up a system which barely works. There appears to be little interest in guiding these people, with psychological, financial and/or legal burdens of their own, to reassure them that all their hard work is delivering an extraordinary level of person-centred care.
But this for me was an inevitable consequence of ‘corporate capture’. The G8 World Dementia Council does not have any representatives of people with dementia or carers.
That is why ‘Living well with dementia’ is an important research strand, and hopefully one which Prof Martin Rossor and colleagues at NIHR for dementia research will give due attention to in due course. But all too readily research into innovations, ambient assisted living, design of the ward, dementia friendly communities, assistive technology, and advocacy play second fiddle to the endless song of Big Pharma, touting how a ‘cure’ for dementia is just around the corner. Yet again.
So what’s the solution?
The answer lies, I feel, in particularly what happens in the next year and beyond.
The Prime Minister’s challenge on dementia was developed as a successor to the National Dementia Strategy, with the challenge of delivering major improvements in dementia care, support and research. It runs until March 2015. Preparatory work to produce a successor to the Challenge from the Department of Health (of England) is now underway in order that all the stakeholders can fully understand progress so far and identify those areas where more needs to be done. The Department of Health have therefore commissioned an independent assessment of progress on dementia since 2009.
There are a number of other important pieces of work that are underway, which will provide information and evidence about progress and gaps. For example, according to the Department of Health, the All Party Parliamentary Group on Dementia chaired by The Baroness Sally Greengross OBE are producing a report focused on the National Dementia Strategy, and the Alzheimer’s Society has commissioned Deloitte to assess progress and in the autumn will be publishing new prevalence data. Indeed the corporate entity known as Deloitte Access Australia (a different set of management consultants in the private sector) produced in September 2011 a report on prevalence of dementia estimates in Australia. Deloitte themselves have an impressive, varied output regarding dementia. But of course they are not interested in dementia solely. “Deloitte” is the brand under which tens of thousands of dedicated professionals in independent firms throughout the world collaborate to provide audit, consulting, financial advisory, risk management, tax, and related services to select clients.
But also it appears that the Alzheimer’s Society, working with NHS England, has commissioned the London School of Economics to undertake a review into the accuracy of dementia prevalence data. The updated data is expected to be published in Autumn 2014. Apparently, once all this work has been concluded a decision will be made on the focus and aims of the successor to the PM’s challenge.
The current Coalition government has been much criticised in parts of the non-mainstream media for the representation of corporate private interests in the Health and Social Care Act (2012).
I believe people who are interested in dementia, including persons with dementia, caseworkers and academics, should make their opinions known to the APPG in a structured articulate way in time. I think not much will be achieved through the pages of the medical newspapers. And only time will tell whether the new dementia strategy will emerge in time before the next general election in England, to be held on May 7th 2015. However, even the most ardent critics will ultimately. The present Government should be congratulated for having made such a massive effort in educating the country about dementia, which is a necessary first step towards overcoming stigma and discrimination. The Alzheimer’s Society has impressively delivered its part of it, it appears, but future policy will benefit from much more ‘aggressive inclusion’ of other larger stakeholders (e.g. the Joseph Rowntree Foundation, Dementia UK) and smaller stakeholders.
It could be a case of: all change please. But a huge amount has been done.
The “dementia prevalence calculator”: for a person to access a timely diagnosis, or for private markets to access the person?
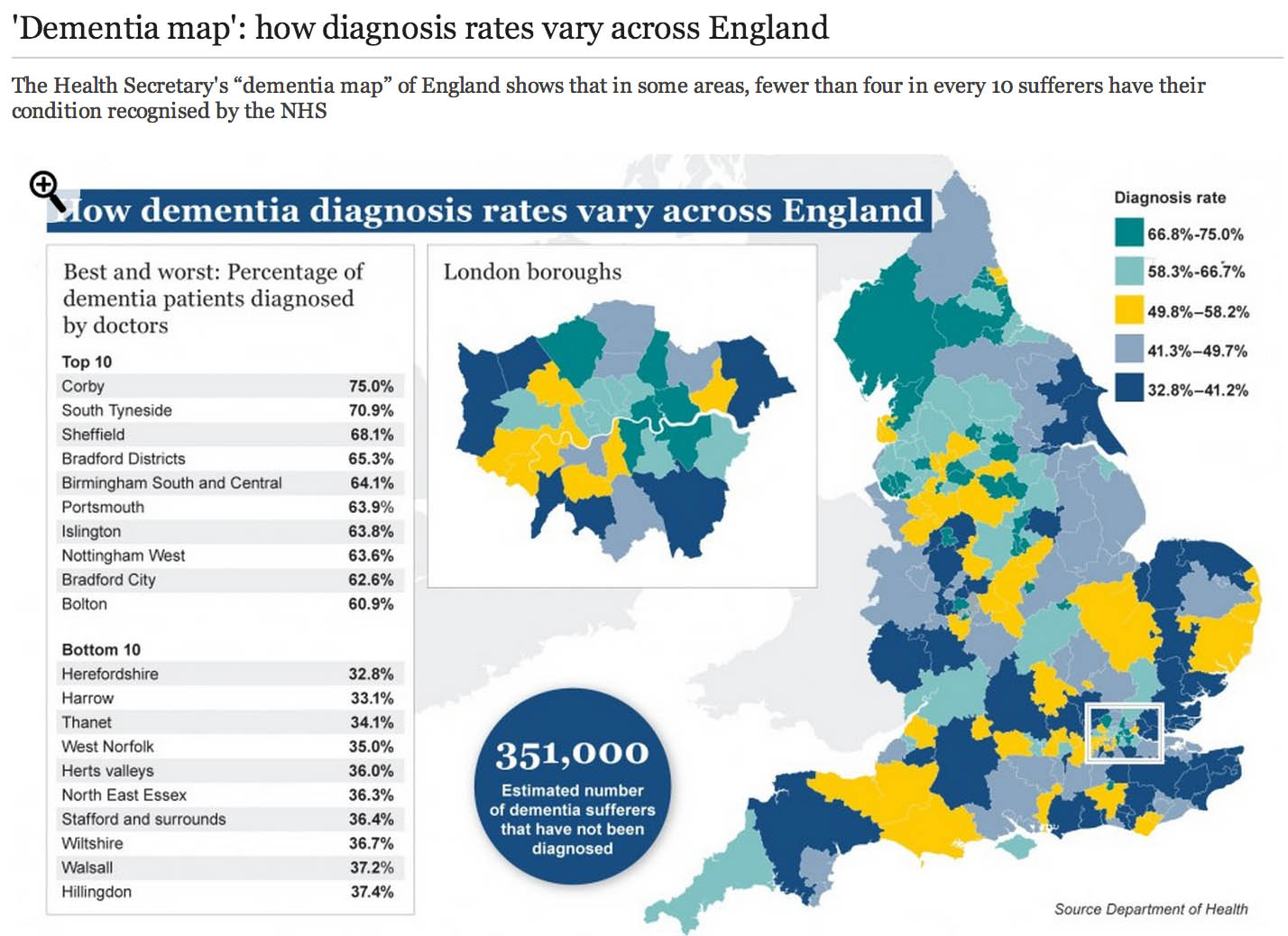
The market philosophy has gripped the NHS by the jugular through policy developments from successive governments. It is argued that all health care systems in the world have to design effective allocative mechanisms for the available “scarce health care resources”. The “dementia prevalence calculator” tool also enables health and care communities to: calculate local dementia diagnosis rates, forecast local dementia prevalence, view trajectories and set “ambitions” (aka targets) for improvement in diagnosis rates and compare diagnosis rates with other localities. Its main problem has been that it has been crowbarred in through various side windows, except nobody knows why public health experts didn’t call for this calculator to come in through a front door. One can now view and compare diagnosis rates on the “Ambition Map”, and link to the “Knowledge Portal” to access a wealth of resources to improve dementia diagnosis rates, and diagnosis pathways. All of this will have taken time, effort and money to set up, so the question of whether it’s worth it, given ‘scarce resources’, is clearly in the public interest. Here is one such example of the Department of Health’s attempts and their partners to disseminate information about “the dementia map”.
So what’s the point of these data? Burns concedes that estimating the number of people who have dementia is important for both local planning and national guidance. Burns freely admits too there have been problems in the past:
“Most current estimates of dementia prevalence (the number of people affected by the disorder) and incidence (the number of people developing it over a defined period, usually one year) are based on studies dating back to the 1980s.”
It’s become clear that a huge “democratic deficit” has engulfed the English dementia policy. The problem for Prof Alistair Burns, who is a genuinely a nice and well-meaning man, is that he can become indundated with various complaints from academics and practitioners. An example is the G8 dementia summit which was presented as a ‘once in a lifetime opportunity’ to talk about dementia. What did, however, happen was that it became a ‘once in a lifetime opportunity’ for various myths to be propagated by the media, using highly charged words such as ‘shocking’, ‘devestating’, ‘crippling’, ‘horrible’, ‘horrific’, portraying the notion that people now on receiving a diagnosis of dementia are just counting their hours until their death. It, likewise, cannot be overstated that the drugs for memory or attention simply do not have a huge effect in the vast majority of patients, and certainly after about fifteen years of published studies on these “cholinesterase inhibitors”, the evidence that they slow down the rate of loss in critical parts of the brain is not terrific. Academics in dementia are currently collaborating across geographical boundaries, so the idea of there now being suddenly a world collaboration is FALSE. A cure for a single dementia is FALSE as there are hundreds of different causes of dementia. Dementia charities of course can mobilise individuals with dementia to contribute in pan-global drug trials in what has been euphemistically been called ‘co-production’, discovering new drugs based on the basis of personal DNA genomic information. Looking at your genetic make-up might tell a practitioner or drug-company your risk of subsequently developing dementia, and so it goes on. The issue is not subjecting the designers of English dementia policy with time-consuming vexatious ‘attacks'; it is hopefully that we can all have an open, transparent discussion of some of the ‘unintended consequences’ of the English dementia policy currently in progress.
In March 2012 the Prime Minister, David Cameron, published his challenge on dementia which set out an ambitious programme of work to push further and faster in delivering major improvements in dementia care and research by 2015, building on the National Dementia Strategy (published on 3 February 2009). Central to the challenge is the requirement that from April 2013, there needs to be a quantified ambition for diagnosis rates across the country, underpinned by robust and affordable local plans (NHS Mandate). This is of course so remarkable in itself in the State having such a strangehold on policy which should in theory be devolved as locally as possible to experts and professionals. A painfully obvious point to those who have done a medical degree is that there will be variation in some rates of particular dementias across the country anyway. For example, in some populations with a predominantly Asian immigrant population with certain risk factors, they might be at high risk of vascular dementias. As it happens, near Warsaw in Poland is thought to have a high prevalence of dementia due to copper overload due to a genetic cluster of an inherited copper metabolism problem called Wilson’s disease. But presumably certain dementia charities and certain politicians want you ‘to get angry’ at those GPs who are underdiagnosing dementia, because they are somehow colluding in keeping this information away from you. This is by the way against their professional code, but you cannot expect people without a medical background who are quite senior in charities or politics to know that necessarily.
I have found that having lack of ability to have a balanced debate (due to enormous information asymmetries) has been quite dispiriting, and clearly hampered by the virtual lack of published research papers in the medical professional literature. Hopefully, the University of Stirling will be able to diminish this ‘research gap’, now that they have been awarded a major grant to investigate this issue properly with no vested interests. This is the only paper on Medline from 1996 if you search for the term “dementia prevalence calculator”. And there is no doubt that the claims of some of the drugs used to treat early dementia in the NHS have been overinflated. Luckily, largely thanks to the work of Glenis Willmott MEP who has been leading negotiations as the European Parliament’s rapporteur on the clinical trials regulation, pharmaceutical companies and academic researchers will be obliged to upload the results of all their European clinical trials to a publicly accessible database, if a deal reached this week is approved, according to a recent report. Indeed, Pharma have got it right about “openness”, but not in the sense of using regulation to allay fears about patient privacy and confidentiality – Big Pharma need to share with the general public their results, and their particular motives and intentions for dementia policy especially if the descriptions are otherwise not easily forthcoming.
I openly admit to being extremely disappointed at one particular plank of English dementia policy: the “dementia prevalence calculator”. It’s incredibly easy to get hold of the marketing shills for CCGs about how they can overcome “the diagnosis gap” for the reported lack of diagnosis of dementia; but there again, the discussion of how there are hundreds of different types of dementia in different age groups is not forthcoming, together with a less than candid explanation of how risk factors for dementia might be tackled. For something so fundamental to English dementia policy, it was deeply distressing to see Prof Carol Brayne’s question on where the Prime Minister saw his “Challenge” progressing on dementia to be passed ‘down the line’ like a rugby ball going backwards with effortless ease first to Mr Jeremy Hunt and then with Dr Margaret Chan. To get a decent grasp on why there has been such a drive to improve dementia rates, you have to go across the Atlantic and research terms such as “needs based resource allocations” in health maintenance organizations (sic). These papers are written entirely from the business model perspective, so do not have any intention of wishing to address remotely the professional concerns of senior clinicians in dementia.
Like all 500 pages of the Health and Social Care Act (2012), there was no open discussion of the need to “turbo boost” the outsourcing of NHS contracts to the private sector. Likewise, meaningful discussion of the perils of ‘case finding’ and ‘screening’ in dementia have largely been throttled at source (though Dr Martin Brunet has been raising awareness of the perils of incentivising GPs to up their rates of dementia diagnosis through ‘case finding’ in primary care, of course drawing attention to the hugely stigmatising “false diagnoses of dementia”). Nonetheless, through the combined efforts of the European ALCOVE project (including Prof Burns and Dr Karim Saad), it’s been successfully argued that,
“Dementia happens to people, living in their families and their communities. It does not happen just to their brains. When people have worrying symptoms they want health care professionals who can spot the signs, take their concerns seriously, diagnose the problem accurately, so they can get the most up to date treatment and advice.”
This is a helpful slide from Prof Dawn Brooker’s presentation for the UK Dementia Congress Conference 2013 entitled, “Benchmarking against ALCOVE recommendations for timely diagnosis in dementia”:
This discussion embarrassingly even led to Prof Burns trying to find Dr Brunet at his practice for a frank chat about the policy, but Martin unfortunately was away that day.
Of course, if you’re going to introduce a policy to ‘up the dementia rate’, it possibly will run into problems given that the actual prevalence of dementia has appeared to be falling. The first UK Cognitive Function and Ageing Study (CFAS), known as the Medical Research Council (MRC) CFAS, began in 1989. One of a suite of European prevalence and incidence studies (forming the EURODEM collaboration), it was designed to test for geographical differences within the UK, across populations with widely varying characteristics, including vascular health. The study published by Matthews and colleagues (2013) in the Lancet confirmed that later-born populations have a lower risk of prevalent dementia than those born earlier in the past century. The general prevalence of dementia (overall numbers of people) in the population might be subject to change. Factors that might increase prevalence include: rising prevalence of risk factors, such as physical inactivity, obesity, and diabetes; increasing numbers of individuals living beyond 80 years with a shift in distribution of age at death; persistent inequalities in health across the lifecourse; and increased survival after stroke and with heart disease. By contrast, factors that might decrease prevalence include successful primary prevention of heart disease, accounting for half the substantial decrease in vascular mortality, and increased early life education, which is associated with reduced risk of dementia. Where possibly primary care will have the greatest impact will be in tackling the risk factors they do anyway for cardiovascular disease, i.e. better diabetic control, tackling cholesterol, smoking, ‘poor diet’, or high blood pressure. This in itself is not a valid reason to avoid improving diagnosis rates of dementia (especially these are treatable risk factors for vascular dementias.)
Health maintenance organizations (HMOs) have been argued by their supporters as a “cost-effective’ way to provide health care. In the United States, in allocating resources in the HMO, the rationing of preventive services appears to be one of the principal questions where the potential benefits (i. e., efficacy) of a service are considered in relation to costs of healthcare. The direct counterpart of the HMO in English health policy, following the enactment of the Health and Social Care Act (2012), is the “clinical commissioning group”, which act as state insurance schemes for pooling risk in population samples.
Just because there’s no effective treatment, there’s still a business case to be made for ‘opening up new markets’ of persons with dementia. For example in the NHS Outcomes Framework 2013/4 domain CB_A9 covers an estimated diagnosis rate for people with dementia, with an aim of “improving the ability of people living with dementia to cope with symptoms, and access treatment, care and support.“. The rationale is therefore stated as:
“A diagnosis enables people living with dementia, and their carers/families to access treatment, care and support, and to plan in advance in order to cope with the impact of the disease. A diagnosis enables primary and secondary health and care services to anticipate needs, and with people living with dementia, plan and deliver personalised care plans and integrated services, thereby improving outcomes.”
According to articulation of neo-liberal ideology, the main justification of the reforms is to make resource allocation “more efficient, more innovative and more responsive to consumers’ preferences” than centrally integrated health systems (Ven 1996, p. 655). The effect of this change in philosophy is the introduction of activity-based resource allocation and funding as a system of paying hospitals and other health care providers on the basis of the work they perform rather than previously applied defined budgets based en bloc global contractual considerations. This new system relies on cost-and-volume and cost-per-case contractual relationships, in which payments are closely linked with the services offered, and clearly the information from “dementia prevalence calculators” is useful here. Conceptually, “dementia prevalence calculators” have been presented on equity grounds, i.e. tackling the inequity of a postcode-lottery diagnosis of dementia. However, this makes a fundamental assumption that there cannot be geographical variations in the prevalence of dementia. I repeat the point – any practising physician would know that this assumption is entirely erroneous, as vascular dementia prevalence rates for cardiopaths for diabetic hypertensive individuals in Tower Hamlets in a ghee-laden diet might be hypothesised to be quite high? The actual drive for the ‘dementia prevalence calculator’ is to open up new active markets, in a form of ‘payment of results’. According to Gay and Kronedfeld (1990), the gradual evolvement of an activity based resource allocation can be traced to the United States, where from 1983 most reimbursement for health care providers had been based upon the Diagnosis-Related Group (DRG) where patients within different categories were classified as clinically similar and were expected to use the same level of hospital resources.
Having a ‘care plan’ for dementia is potentially advantageous in that it can provide harmonisation with private insurance systems. The ‘Kaiser Permanente Care Management’ program contains guidelines and recommendations on how dementia care should be provided to Kaiser enrollees. The new program is an informational resource only and is not a substitute for clinical judgment based on the individual needs of patients. The program includes nine “key principles” on diagnosing and caring for patients with dementia and support for their caregivers. These principles include early identification and diagnosis, connecting caregivers to vital community resources, developing a care plan, and monitoring and adjusting medication use. With the introduction of “whole person care” (or similar models of integrated care in the next government), it is likely health and social care will be taken down a “final common pathway” of the ‘personal budget’ or ‘individualised’ budget (see this article for a recent discussion of some of the key themes from the English healthcare thinktanks). The commercialisation of care, under the guise of control and budgets, is, in fact, of course a complete anethema to genuine principles of professional person-centred care. And merging a universal system which has lots of highly personal data (NHS) with one that is heavily conditional (benefits) has all kinds of risks. In the long run it could make it still easier to restrict access to healthcare on the basis of economic status or behaviour.
While GPs and the public are clearly none-the-wiser about the goal of upping the diagnosis rates, already work is being done on the barriers and solutions for implementation of personal health budgets in dementia. Claire Goodchild’s report for the Mental Health Foundation from October 2011 still makes for interesting reading. Goodchild argues that, “individualised, tailored support and care that a personal budget can facilitate can have enormous benefits to a person with dementia“. The irony is of course that Big Pharma may not actually end up the big beneficiaries of this drive, unless they can make their medications relevant to individuals with dementia in this brave new world. While the G8 conference was an effective pitch for personalised medicines for Big Pharma, relatively little attention was given to psychological therapies or carers, aside from ‘dementia friendly communities’ which bring competitive advantage to the included corporates (and benefits for persons with dementia too). Personal budgets are all about choice and control; it is unlikely that a person with dementia will be unaware of the personal spending decisions that he or she can make to improve wellbeing (deferred to a carer where that person does not have capacity); but other valid interventions do include the assistive technologies and innovations which curiously did also make a mention in the G8 dementia.
Therefore, at first blush, it might look a bit random having a ‘dementia prevalence calculator’ and then all the shennanigans of the G8 dementia summit, but whilst the English government cannot as such make dementia ‘wealth creating’, it can do its best to open up new markets. It hasn’t been an accident that the question, “Have you had problems with your memory?”, has been suggested for those ‘health MOTs‘ which private healthcare would love to get off the ground. And the big beauty of this plan when NHS budgets are looking to do ‘more with less’ or implement ‘efficiency savings’ (or cuts to frontline care, more accurately) is that the NHS budget itself won’t ‘take the hit‘. It is hoped that with the implementation of whole person care budgets somebody will be able to ‘top up’ payments for care (e.g. “co-payments”), and the patient (or customer) will now pay for care providers in the private sector too. Do the treatments actually have to be proven to work? Absolutely not, if the experience in personal health budgets is anything to go by, but that’s not the point. As David Cameron might say, “Oh come on.. please do keep up!”
Further reading
Gay E.G. and Kronedfeld J.J. (1990). “Regulation, retrenchment – the DRG experience: problems from changing reimbursement practice”. Social Science and Medicine. 31 (10), pp. 1103-1118.
Ven, W.P.M.M., van de. (1996). “Market-oriented health care reforms: trends and future options”. Social Science and Medicine. 43 (5), pp. 655-666.
Exciting times for the Alzheimer's Society
Prof Alistair Burns, Professor of Medicine at Manchester University and the UK’s first ‘dementia Tsar’, gave a very inspiring speech to the UK’s Alzheimer Society.
Prof. Burns made it clear that dementia was a top priority for the Coalition govenment. This is confirmed by the fact hat Ruth Sutherland, acting CEO of the Alzheimer’s Society, was rung up on day 1 of the Coalition government for the views of the Alzheimer’s Society regarding dementia care.
Indeed, dementia care has been identified as a clear target for NHS quality initiatives. This marks a sea change in health policy priorities from only a few years ago, and perhaps can be taken to be an indication of a wish to see the merging of clinical and social care financial issues under the term of the Coalition government, and beyond.
Prof Burns made specific reference to the ‘Acute awareness’ document of the NHS Confederation.

In this, the NHS Confederation provide for the following:
Dementia currently affects over a half a million people in England alone; this number is set to rise considerably as more people live longer. Sixty thousand deaths a year are directly attributable to dementia, and the current cost to the NHS is estimated at £1.3 billion a year. This report looks at the key issues for NHS trusts in improving care for patients with dementia, the majority of whom will have been admitted for another condition. It showcases the innovative work that NHS trusts and cross-agency partnerships are undertaking in this area to enhance patient care and describes how significant improvements can be achieved in terms of both the quality and efficiency of patient care.
The UK Alzheimer’s Society is indeed looking forward to keeping dementia as a top clinical priority for the NHS. Jeremy Hughes, from Breakthrough Breast Cancer, has fully embraced the critical importance of giving full support to researchers to improving clinical practice and outcomes, and has indeed been a big success there. He will be becoming the new CEO of the Alzheimer’s Society from November 2010, heralding a very exciting time for the Alzheimer’s Society.
(c) Dr Shibley Rahman 2010