Home » Posts tagged 'alcoholism'
Tag Archives: alcoholism
Change
Somebody once advised me in my 20s that destiny is when luck meets preparation.
When I was younger, I used to think that you could prepare yourself out of any situation. But wisdom and events proved me wrong. I soon discovered that what you did yesterday though can affect today, and what can affect today can affect tomorrow. The only thing you can predict pretty comfortably, apart from death and taxes, is change. When I was younger, I used to think I could live forever. All this changed when I woke up newly physically disabled, after a six week coma on a life support machine on the Royal Free Hampstead. The National Health Service saved my life. Indeed, the on call Doctor who led the crash team the day of my admission, when I had a cardiac arrest and epileptic seizure was in fact a senior house officer with me at a different NHS trust in London.
This feeling of solidarity has never left me. I do also happen to believe that anything can happen to anybody at any time. I studied change academically in my MBA in the usual context of change management and change leadership. It’s how I came to know of Helen Bevan’s work. I’ve thought a lot about that and the highly influential Sirkin paper. But I don’t think I honestly ‘got‘ change until this year. In 2007, I was forced to change, giving up alcohol for life. I realised that if I were to have another drink ever I would never press the off switch; I would either end up in a police cell or A&E, and die. This is no time for hyperbole. It was this forced change, knowing that I had an intolerance of alcohol as serious as a serious anaphylactic shock on eating peanuts, that heralded my life in recovery. I later came to describe this to both the legal regulator and the medical regulator as the powerful driver of my abstinence and recovery, rather than a ‘fear based recovery‘ from either professional regulator.
But I feel in retrospect my interpretation of this change, as due totally to an externality, is incorrect. As I used to attend my weekly ‘after care’ sessions with other people newly in abstinence from alcohol or other toxins, or from gambling, or sex, I discovered that the only person who can overcome the addiction is THAT person; and yet it is impossible to read about this path of recovery from a book, i.e. you can’t do it on your own. So ‘command and control’ is not the answer after all. Becoming physically disabled, and a forced change of career and professional discipline, and a personal life which had become obsessed by alcohol, meant I had no other choice. I had to ‘unclutch’ myself gear-wise from the gear that I was in, and move into a different gear. But I did find my new life, living with mum, and just getting on with my academic and practitioner legal and business management training intensely rewarding.
In 2014, I attended a day in a hotel close to where I live, in Swiss Cottage. One of the speakers was Prof Terence Stephenson. After his speech, I went up to thank him. I found his talk very moving. He was later to become the Chair of the General Medical Council (GMC). I was later to become regulated once again by the GMC. Two lines of his has kept going through my mind repeatedly since then. The subject of the day was how sick doctors might get salvation despite the necessary professional regulation process. Stephenson claimed: “If you’re not happy about things, I strongly urge you to be part of the change. You being part of the change will be much more effective than hectoring on the sidelines.” This was not meant as any threat. And as I came to think more and more about this I came to think of how much distress my behaviour had caused from my illness, how I wish I had got help sooner, and how looking for someone to something to blame was no longer a useful use of my energies. I am now physically disabled. I get on with pursuing a passion of mine, which is promoting living better with dementia. But if there are any people who are worthy of retribution I later decided then their karma might see them implode with time. Not my problem anyway.
I now try to encourage others where possible if they feel that they have hit rock bottom; I strongly believe that it’s never too late for an addict to break out of the nasty cycle. If you think life is bad, it unbelievably could be much worse. I think businesses like persons get comfortable with their own existence and their own culture, but need to adapt if their environment needs it. I think no-one would wish to encourage actively social care on its knees such that NHS patients cannot be discharged to care, if necessary, in a timely fashion. I don’t think anyone designing the health and care systems would like them to be so far apart deliberately, with such bad communication between patients, persons and professionals. Above all, I feel any change has to be authentic, and driven by people who really desperately want that change. I think change is like producing a work of cuisine; you can follow the recipe religiously in the right order, but you can recognise whether the end result has had any passion put behind it. For me, I don’t need to ‘work hard’ at my recovery, any more. I haven’t hit the ‘pink cloud‘ of nirvana, but I am not complacent either. Change was about getting from A to B such that I didn’t miss A, I was in a better place, and I didn’t notice the journey. If I had super-analysed the change which was required to see my recovery hit the seven year mark this year, I doubt I would have achieved it.
The story of me
I’ll be giving a talk on Thursday 25th September 2014 on my personal experiences of alcoholism and interacting with the GMC, at a meeting called “Regulation, Respect and Health Practitioners” in London.
This is a draft of the text of my talk.
** Please check against delivery. **
Thank you for inviting me to speak for about 15 minutes on my viewpoint of the creation of a healthier regulatory process to benefit doctors and patients.
My speaking here comes at a time when there is a genuine drive for care and compassion in national policy in healthcare.
I believe that there should be a mutual respect between junior and senior clinicians, and the clinical regulator. In fact, I think this respect should be cherished and nurtured.
Last month, I had a hearing arranged by the Medical Professionals Tribunal Service (“MPTS”) to hear my application for restoration to the GMC register. This was just weeks after my 40th birthday.
I was asked by one of the panelists there what I had learnt most from my time off the register.
It is, of course, a necessary requirement that all Doctors on the GMC register have kept their skills up to date. This is so that Doctors can fulfill their obligations of performance, skills and knowledge. One of the benefits of having had at least five years out is that I’ve read the doctors’ code of conduct, “Good medical practice”, very many times. But I gave an answer which I don’t regret now for a moment.
I said, “Most of all, I finally know what is like to be a patient.”
I was erased in July 2006. At the time, it was uncertain what my ultimate diagnosis was, but a number of psychiatrists were in no doubt that I was suffering from an alcohol dependence syndrome. After I erased, I then spent heavily drinking alcohol a year in a pub. I used to go to local pubs at opening time, and leave at closing time. They say that unemployment is a big risk factor for mental illness.
Not being regulated at all by the medical profession was a big part of losing what I had perceived to be my identity. There was absolutely no structure or goal to my life. My life hit rock bottom. But, as an alcoholic, you soon realise that, however low you have gone, you can always go even further.
I had been first referred to the GMC a few years earlier. At the beginning of the process, no-one ever told me how long the regulatory process would last. This uncertainty about the future was a huge part, I feel, in my subsequent precipitous decline in mental health. I was erased ultimately for deficiencies in conduct and performance, and poor health, in 2006.
Whilst I was not punished for being ill, it was clear that the professional regulator could in no way condone my undisputed shortfalls in conduct and performance. The question about whether the clinical regulator views health to be intimately linked to professional conduct and performance is an important one. I do. This matter is also relevant to ‘revalidation’. I feel a junior must not ignore his own personal ill health first selfishly, above the needs of patients. He needs to get help as soon as possible. With the benefit of hindsight, I so wish I had sought help sooner.
When I was erased, I felt I became “public enemy number one”. However, they say that self-pity is a huge risk factor for drinking relapse. It was at one level a private shame . My father, who later passed away in 2010, was deeply humiliated by the whole experience, even though he had caused none of it. My father had been a GP for about 25 years. Therefore he adored the GMC. He felt GMC was “God”. But God moves in mysterious ways? As a loving father, he stuck by me throughout. As did my mother, with whom I still live.
The whole thing was, however, also a very public shame. You can still find reams and reams of it adorning Google. The avalanche of news reports about this, while creating a moral panic, virtually invariably never mentioned my severe alcohol illness. But that, as such, doesn’t matter to me any more even though I am keen on one aspect. I am still keen to remind myself of the distress I caused while I was powerless over alcohol. That’s why I have never asked for any of it to be deleted off Google in this jurisdiction.
I’ve never had a salaried job for the last eight years following erasure. In the only two job interviews I had for legal posts I was asked about my Google footprint of the GMC case.
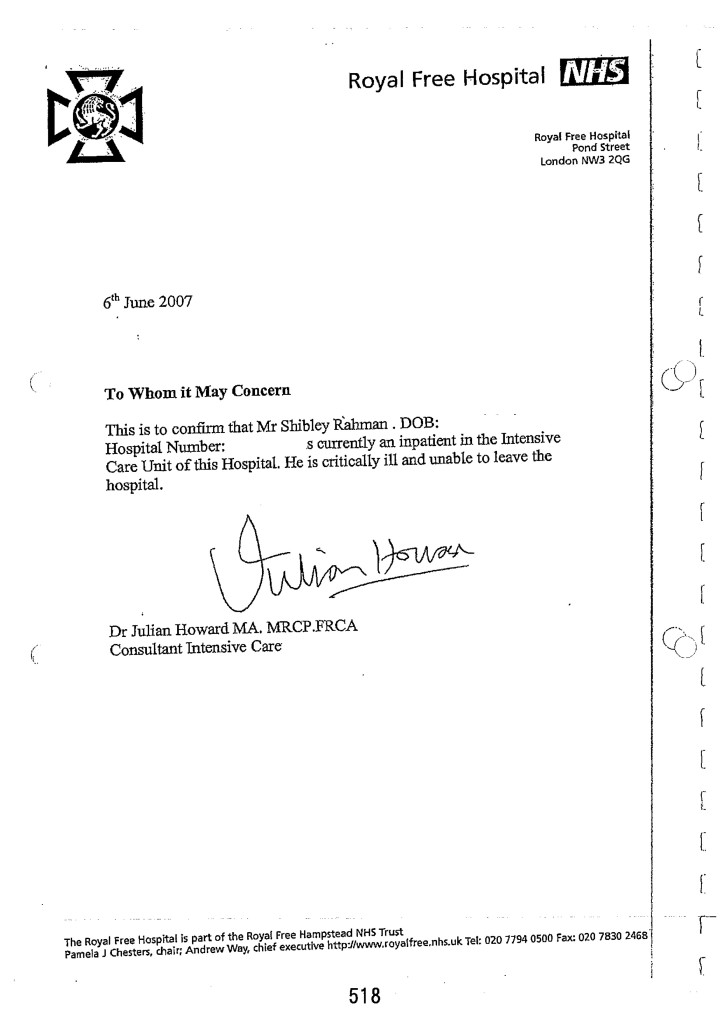
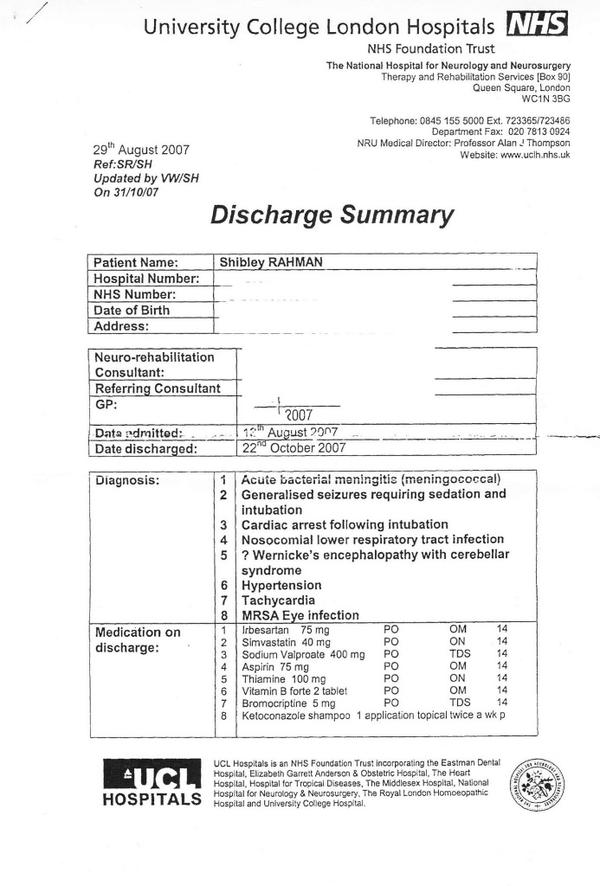
On a day at the beginning of June 2007, I was ‘blue lighted’ into the Royal Free. I had had an epileptic seizure, but the crash team lost my airway. They tried to intubate me, but I then had a cardiac arrest, from which I was successfully resuscitated. I literally owe my life to the NHS. I was kept alive for six weeks, while completely unconscious in a coma. When I woke up, I could not walk or talk. I became newly physically disabled. But the neurorehabilitation team at the National Hospital for Neurology and Neurosurgery, where I was in fact a junior doctor, then taught me how to walk and talk again. I remember how the occupational therapist taught me how to shop in a supermarket. I learnt, from scratch, how to perform basic tasks, such as making a cup of tea.
I always had loved medicine. I got the second highest First in neuroscience in my undergraduate course in Cambridge. I got my PhD in 2001 in identifying an innovative way of diagnosing behavioural variant frontotemporal dementia. I later passed my diploma of the membership of the Royal College of Physicians. I have published three books for junior physicians negotiating each of the three components of this demanding examination for core medical training.
My late father, however, emphasised to me that that coma, in many respects, saved my life. I agree with him now. It heralded the start of my period of abstinence from alcohol. I have now been in recovery from alcohol continuously for seven years. I take one day at a time. I am content now.
Since my coma, I have obtained my Bachelor of Law, Master of Law and my Master of Business Administration, and completed my pre-solicitor training. I adore the law as well, and I am fully signed up to the legal doctrine of proportionality, where the law must balance competing interests where they exist. I became regulated in 2011 by the Solicitors Regulation Authority after an extensive due diligence process.
Last month, my application for restoration onto the GMC Medical Register was approved.
This is not, however, by any means the ‘endpoint’ to my new life. I am not only keen to learn lessons for myself from the experience, but I am now also keen to help others. This is why I regularly attend, voluntarily, the ‘suspended Doctors group’ for “The Practitioner Health Programme”. I am under a psychiatrist, whom, without being hyperbolic, I feel saved my life.
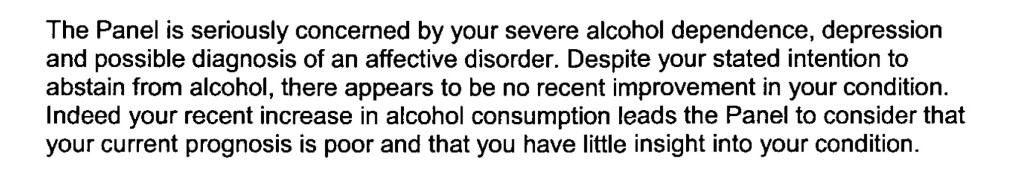
I look back on the psychiatry reports of me when I was ill during 2004-2006 with utter disbelief. I was hugely in denial – had no insight into all how I at all junctures minimised the catastrophic effects of my active drinking. The “paradox” for dealing with a drink problem is that you cannot ‘do it’ on your own, and yet you must get help for the problem and realise your powerlessness over it. For me, it’s very simple – I can’t ever have a casual drink ever again. One alcoholic drink is one too many, and yet one drink is never enough. It ruined my life.
For me, the critical key to success is having a close circle of people in a social network, including an after care group in my local hospital, would be able to spot and intervene early in problem behaviour. For the first time in 2007, after my coma, I fully engaged with my General Practitioner. I had numerous ‘false starts’ in dealing with my alcoholism between 2004 and 2007.
I personally found the pressure of being investigated and dealing with my illness, during this period, unbearable. A part of me wishes, in retrospect, that I had been “better managed” in terms of performance at the time. Witness statements report me as looking ‘alcoholic’ and ‘dishevelled’ while on the wards, when my performance was clearly poor. A part of me wishes I had been “made to go to occupational health”, when these problems first surfaced.
But a part of me strongly resists my transference of blame onto other parties. As I admitted to my restoration panel, I made plenty of mistakes of my own: for example, I never engaged properly with my own G.P. until my coma.
I was most obviously, prior to my coma, a clear threat to patient safety. And it states clearly in s.1 (1A) Medical Act 1983, the GMC must promote patient safety. So I strongly believe the original sanction was the correct one.
But now, next month, as a different person, I’ll be presenting my research, based on an online survey, on the funding of dementia care. This will be at the prestigious Alzheimer’s Europe conference in Glasgow. This January, I published a popular book entitled, “Living well with dementia”. I feel that, with my truncated medical training thus far, and my postgraduate degrees in law, medical research and business management, I can be an asset to the public health and health policy arm of the medical profession.
For me, my return to the GMC register, after completion of the identity check, will be a huge privilege.
Sadly, it can be rather too easy for colleagues to gang up on individuals and ringfence problems, rather than solving the problems at root to make the health and care services better. I am sure that many juniors feel: “there for the grace of God go I”.
One cannot away from the enormity of the problem of unwell Doctors in the NHS, however. I felt totally abandoned during the regulatory process and could have done with more support at a time when I especially needed it? In conclusion, the public including staff would like to have pride in the medical profession and its regulator. I too would like to see this goal come to fruition one day.
Being restored to the GMC Medical Register has been a massive dream come true
I spent nine years at medical school, and about very few as a junior doctor.
I’ve now been in recovery for just over seven years.
But in that time I do remember doing shifts starting at Friday morning and ending on Monday night. I remember the cardiac arrest bleep in Hammersmith at 4 am, and doing emergency catheters at 3 am in Norfolk.
I had an unusual background. I loved medical research at Cambridge. In fact, my discovery how to diagnose the behavioural variant of frontotemporal dementia is cited by the major international labs. It is in the current Oxford Textbook of Medicine.
Being ensnared by the General Medical Council in their investigation process devastated my father. He lated died in 2010. I remember kissing him goodbye in the Intensive Care Ward of the Royal Free, the same ward which had kept me alive for six weeks in 2007.
I of course am completely overwhelmed by those events widely reported, especially in the one in 2004. The newspapers never report I was blind drunk. The media when they do not mention my alcohol dependence syndrome are missing out a key component of the jigsaw.
Until I die, I will never be safe with one alcoholic drink. I will go on a spiral of drinking, and that one event I am certain would either see me in a police cell or in A&E.
One event did change my life. I was blue lighted in, after a year of heavy drinking after I was erased by the GMC in 2006, having had a life-threatening epileptic fit. The crash team attempted emergency intubation, but I ended up having a cardiac arrest which was successfully resuscitated.
I do not wish to enter any blame games about what happened a decade ago. It turns out that the Trust which reported me as dishevelled and alcoholic, and having poor performance simultaneously, is in the Daily Mail this morning for a running a ‘chaotic’ A&E department.
It also turns out that another Trust in London which reported me as dishevelled and alcoholic, and having poor performance simultaneously, had its A&E department shut down this week.
I was in denial and had no insight. Hindsight is a wonderful thing, but I needed sick leave and a period of absence and support. But I do not wish to blame anyway for those events I wish had never happened some time ago.
But the GMC referrals were absolutely correct. I had a proper medical plan put in place for me when I awoke from my coma. I followed religiously my own GP’s advice too.
I am now physically disabled, and have had no regular salaried job since 2005. But I am content. I live in a small flat with my mother in Primrose Hill. I regularly go out to cultural events. I maintain my interest in dementia, going to a fourth conference this year for Alzheimer’s Europe in October, where I have been chosen to give one of the research talks. It’s actually on an idea which David Nicholson inspired me over.
I’ve done four books on medicine, including one on living well with dementia. The Fitness to Practice panel in their judgment note my contribution there, which I am pleased about.
The Panel also crucially made the link in their judgment that my poor performance in conduct and competence coincided with my period of illness, the alcohol dependence syndrome, for which I am now under a psychiatrist.
I go to AA sometimes, and the weekly recovery support group at my local hospital. Being in contact with other people who are starting the same process of getting their life back continues to inspire me. I also attend the suspended doctors group for the Practitioner Health Programme, which helps me understand myself too.
I believe that there is no higher law than somebody’s health. I understand the pressures of why trainees preventing them from seeking help in the regulatory process.
But I do have an unusual perspective. First and foremost, I am a patient myself, and proud of it.
Secondly, I am regulated by the Solicitors Regulation Authority. I can become a trainee solicitor, if I want to be. I had a careful due diligence process in 2010, and I thank the legal profession for rehabilitating me.
Thirdly, I will now be regulated once again by the General Medical Council pending a successful identity check on October 7 2014. Having my application to be restored to the UK medical register is a massive honour for me. I caused a lot of hurt to others during my time with the medical profession last time, and this time I would like things to be different, and be of worth.
This, I hope, will mean a lot to my late father.
I am grateful to all the people at the Medical Practitioners Tribunal Service, and to the GMC prosecutor for presenting a fair case on behalf of the GMC who need to promote patient safety.
I am encouraged that the GMC’s new Chair, Prof Terence Stephenson, “gets” change for the better for the profession, and has an excellent track record as a clinical leader.
I love my law school, BPP Law School. They got me through this. I have become a non executive director of their Students Association now. There’s a lot of work to be done there, but I am lucky that there are two colleagues there of mine who are simply the best: Shahban Aziz and Shaun Dias.
I am now about to be regulated by two professions. I could not be happier.
Thanks for your support. I couldn’t have done it without you.
Out of sight, out of mind
Please note: This blogpost has been edited since the first publication, due to a factual inaccuracy of mine this morning where I stated the Tavistock Clinic was private.
It is not private. I do sincerely apologise for this mixup. It was an entirely accident error of mine.
I have also changed the word ‘aggressive treatments’ to ‘thorough interventions’ on the advice of two different people.
I am further posting Kate’s very helpful comment below the end of this article.
I am extremely grateful to Kate for her comment.
________________________________________________________________________________________
I have previously written openly about my personal experiences as a sick doctor and beyond (please see here). Thank you if you were one of the 2000 or views of that blogpost on that particular day.
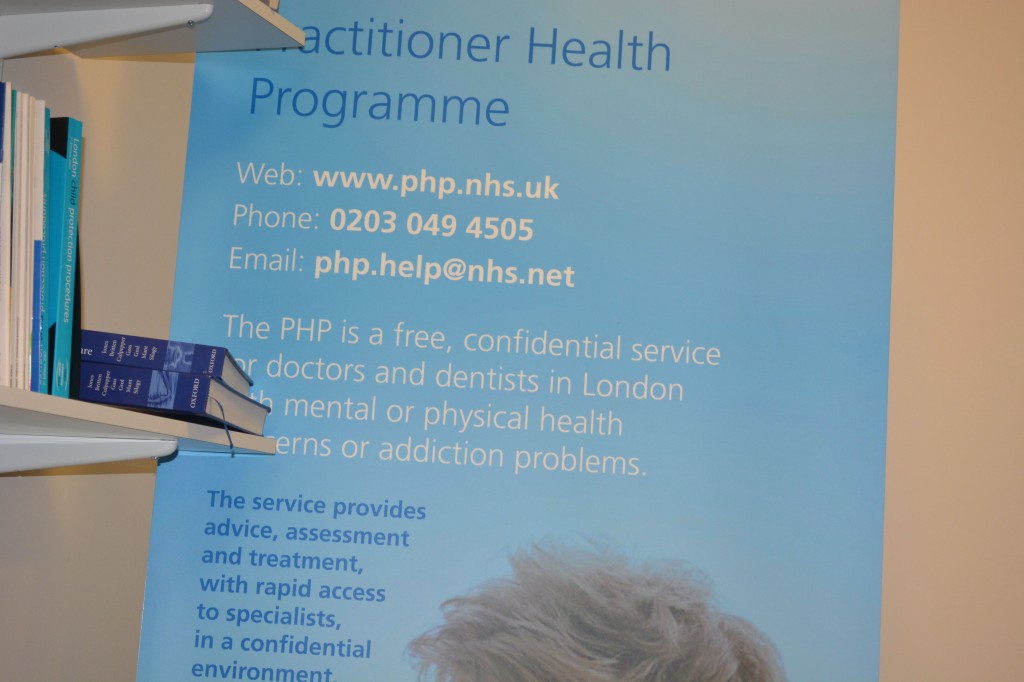
In 2008, the Department of Health under the previous government funded a two year pilot to commission and provide a specialist, confidential, service, the Practitioner Health Programme (PHP).
The service was free to all doctors and dentists in London with:
- mental health or addiction concern (at any level of severity); and,
- physical health concern (where that concern was potentially impacting on the practitioner’ performance).
The PHP complemented existing NHS GP, occupational health and specialist services. It demonstrated the need for the service (over 500 patients have now been treated, many with complex problems) and how savings could be achieved through swift, safe return to work.
The 2009 Boorman review of the health of the NHS workforce reported that:
- the direct costs of ill-health in NHS staff are in the region of £1.7 billion p.a.;
- the agency staff bill for the NHS is around £1.45 billion p.a. (spending closely related to sickness absence and staff turnover); and 2,500 ill-health retirements (some possibly preventable) each year cost the NHS £150m p.a.
The Chief Executive of the General Medical Council, Niall Dickson, commenting on the PHP said:
“We know of the stress and anguish experienced by doctors who become sick and how this can affect their work. There is not enough good support at local level and the PHP programme has shown what can be done.”
It is now pretty widely felt that prevention and early intervention could save the NHS millions of pounds, and employers can achieve huge savings by supporting doctors and ensuring they remain fit to practise, whilst maintaining or improving quality. The potential savings for employers far outweigh the likely cost of establishing a nationwide service (estimated at around £6 million). There is therefore a real economic case, as well as averting tragedies in human lives training in the NHS.
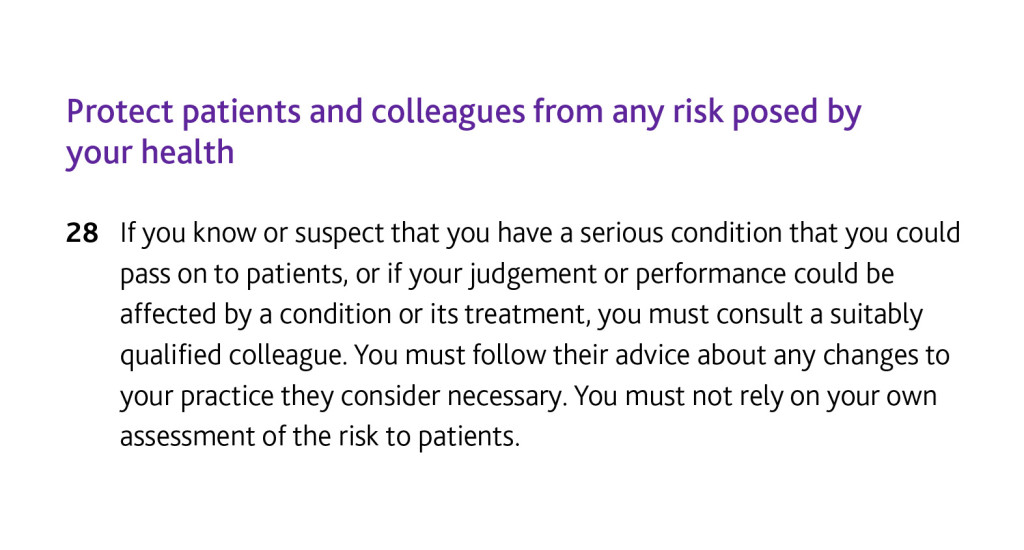
If you’re a sick Doctor, ‘Good medical practice’, the GMC’s code of conduct, is triggered under domain 2 for quality and safety by the following clause.
In my own particular case, it is recorded in two detailed witness statements that I tried to discuss in detail the alcohol problem that was concerning me with two Consultant Physicians in London.
In neither case was I offered a programme of alcohol management. I confided in them personal details.
It is a real pity that I did take up an offer by a Consultant who recommended the Tavistock Clinic, as I erroneously thought it was private not public. Notwithstanding that, no offer of sick leave was made, but that is my fault for not having let the discussion get that far.
But I really don’t wish to play any ‘blame game’ – for example I failed in not being under a General Practitioner at the time, as I was at that stage absolutely petrified that that GP would have reported me to the GMC subjecting me to years of investigation. I had years of investigation anyway, but without the critical help I needed.
Being under a General Practitioner for a medical professional is a requirement of their Code of Conduct according to rule thirty.
I think many aspects of my dire situation reflects a fundamental misunderstanding of the medical profession thinking that if a sick Doctor is ‘aware’ of his problem he has full insight into the distress the problem is causing to friends, family and beyond.
I feel that, had my problem been aggressively dealt with earlier, the subsequent failures in my alcohol management would not have occurred (three years later).
My erasure for me was perceived by me as the ultimate personal failure for having been through a public hearing, treated still in the media as a “show trial”, and a personal failure for not having got clinically better. On a note of wider contrition, however, I have no objection to the issues I was found proven to this day, and I think the GMC ultimately made the correct sanction.
Media reports, despite public humiliation, distressing not just for me but my late father at the time, make no reference to my underlying medical problems. I was sectioned in May 2006 due to alcoholism. It’s as if the establishment wishes purposefully to airbrush doctors being sick.
I was distraught on my erasure, for having no solution to my mental health problems in sight. The regulatory process exacerbated my misery, with psychiatrists not being able to rule out at anxiety and depressive component while I was heavily drinking.
I know I was ‘aware’ of my problem with empty drunk bottles of red wine, but it doesn’t mean that I had the motivation to take time off work then to do something about it.
Likewise, the GMC code (see clause twenty eight above) assumes that the sick Doctor has full insight.
In my case, it had a very unpleasant end.
Not just this, days before my 33rd birthday,
but this six week coma and two month neurorehabilitation (the full discharge diagnosis from a place where I used to be a junior clinical physician once with no health problems.)
I think it is incredibly hard for anyone to understand outside of the system how you get raped of your dignity and integrity by the regulator when you fail to improve from mental illness. And often this mental illness is exacerbated by the regulatory process, as 86 deaths of Doctors awaiting Fitness to Practice during the same period of my investigation might appear to testify.
As I never had a performance assessment or clinical supervisor during my regulatory process, despite four different consultants concluding I had a severe alcohol problem at least between August 2004 and spring 2005, I feel I was put into managed decline long before the final hearing in July 2006.
I think personally the system for sick doctors undergoing the regulatory process from the General Medical Council could be much better, but that might be just be an unfortunate personal experience: ‘there’s nothing to see here’.
But a good first management step for me would be to roll out the Practitioner Health Programme to a jurisdiction wider than London. Lives truly depend on it, and the general public deserve better from seniors in the medical profession. This, for me, is absolutely necessary to maintain trust in the medical profession, domain 4 of the current GMC Code of Conduct. The GMC need to make the dealings open in this regard, fundamentally.
As far as the Consultants who contributed to my 2006 erasure were concerned, I have been out of sight and out of mind. In fact, I haven’t spoken to them for a decade and needless to say they have not wished to contact me.
I may be newly physically disabled following 2007.
I don’t personally wish the GMC any ill will. I believe in rehabilitation being a regulated student member of the law profession now – but do they?
I am back now.
Kate’s really helpful comment:
The Med Net service IS FREE and confidential.
When medical trainees encounter difficulties, college tutors, clinical tutors, programme directors and educational supervisors are encouraged to signpost them to Med Net. It was very positive that the consultant, who was not your educational supervisor, took sufficient pastoral interest in your welfare to give you the Med Net contact details. Ultimately, it is down to junior doctors to contact the service. Had you sought an appointment with your trusts OH team, they’d have given you the same contact details. It would have still been down to you to make contact. (< Indeed. Thanks , noted )
Alcohol-related disorders are outside the Mental Health Act, so it is impossible to compel people to undergo “treatment”. “Treatment” is an unfortunate term, as there is little that therapists can do until an individual wants help or becomes so incapacitated that they cease using. Even then, the notion of “treatment” as something that is done “to” people is inappropriate. This is one of the reasons why addictive disorders are outwith the MHA. Compulsion doesn’t work. “Aggressive treatment” is a particularly unhelpful concept more appropriate for the treatment of leukaemia rather than substance misuse disorders. Intense cycles of chemo-irradiation may induce remission in oncology, but intense input achieves nothing in addiction.
Kate then said it was a pity that I did not take up the offer of that Consultant, which I absolutely agree with.
My experience of being a sick Doctor
“Anything can happen to anybody at any time.”
This one principle does guide what I think about people and health.
It’s what I think when a friend of mine living with dementia suffers a bereavement. It’s what I think when a friend of mine gets told he has bladder cancer.
It’s also how I come to rationalise my six week coma in 2007 due to acute bacterial meningitis. I was rushed into the intensive care unit of the Royal Free Hospital Hampstead, having been resuscitated successfully by somebody I used to work with in fact. He knows who he is.
His team stopped me fitting in an epileptic seizure. His crash team got a pulse back on their third cycle of jumping down on my chest after I had been flatlining in cardiac asystole. He managed to put a tube down me as I had stopped breathing.
I then spent six weeks in a coma, and my mother and late father came to visit me every day in intensive care, and in the neurorehabilitation unit (Albany Ward) at the National Hospital for Neurology and Neurosurgery, London (a hospital in which I had worked in 2002 in a rotation which included an interest of mine, dementia).
I am now living with physical disability. I can now walk, and I remember my protracted time in a wheelchair. I remember people’s reactions to you in the street. I remember how ‘available’ black cabs would simply drive past. I was, in effect, taught how to work again by inpatient and community physiotherapy.
Due to my meningitis, I could barely speak; the “speechies” helped me with that. I had difficulty planning a cup of tea; the “OTs” helped me with that.
I can relate to all the current NHS concerns how you become stripped of identity in the modern NHS: you become a bed number, or at best a surname.
But in many ways, as my late father kept reminding me shortly before his own death in November 2010, that meningitis in a way saved my life.
I then engaged properly with the NHS as a patient. I used to see my GP regularly.
As a medical student, I had felt as if I was too busy to see my own GP. Big mistake.
As a young house officer in hepatology, I used to be surrounded with very pleasant patients; but for whom I had to perform an abdominal paracentesis, as they were often bright yellow due to liver failure (but awaiting a liver transplantation).
I slowly became alcoholic and isolated. I have often been asked when did I start to drink heavily. This is very difficult for me to place, as most people like me go through a phase of problem drinking.
My official diagnosis for the alcoholism is severe alcohol dependence syndrome in remission. I have now not drunk alcohol for seven years. I know I am an alcoholic as it is unsafe for me to have an alcoholic drink. If I have an alcoholic drink, I would either end up in A&E or in a police cell. I am incapable of having a social drink.
Receiving a medical diagnosis for my mental health condition, in my particular case, helped me to rationalise the cause of my problems which had caused so much distress to others including especially my mother and late father.
I was listening to LBC last night and the presenter was joking that he had a listener rung up “I am an alcoholic. I haven’t had a drink for 35 years.” But seriously folks, it is like that.
I am now regulated by the legal profession. I spent 9 years at medical school, doing my basic degrees for medicine and surgery, and my PhD in the early diagnosis of frontal dementia. As a junior in the medical profession, walking around as the most junior member pushing the Consultant’s trolley and writing in the notes, the thought that you might be ill did seem an alien one.
And yet I was extremely ill. For all people in addiction, there becomes a time when you are in complete denial and lack complete insight. That’s when it is impossible for you to be regulated.
I also have a lot of sympathy for the regulators who regulate people who I think can be best be described as a “dry drunk patients” – i.e. they spend months or even years dry before relapsing. They are, I feel, “living by the seat of their pants”, or “whiteknuckling” it.
The alternative is recovery – where you are not merely abstinent, but where you embrace a life which is utterly content, but in the absence of your addiction of choice.
I indeed find this hard to explain to people who have never experienced addiction. I do not wish to compete with ‘patient leaders’, or think tanks who go on and on and on and on about patient involvement.
But I do wish to recommend to you, if you are in their catchment area, the Practitioners Health Programme (PHP). An incredible ambition of Prof Clare Gerada, the programme is a lifeline to doctors who are ill. It’s been shown in numerous numerous surveys that an ill doctor under-functions as much ‘use’ as a doctor who is completely out of the service. I would simply say to anyone who is ill in the medical profession, put your own health ahead of your career. Your patients deserve that too. Do not be blinded by your own career. I am proud to attend regularly PHP.
I don’t do much apart from hundreds of blogs for the SHA, or campaigning for people living with dementia. But I am at least at last content.
Update: I (Dr Shibley Rahman) was returned to the GMC Register for the UK 26 August 2014. I had been in recovery from alcohol since the onset of my coma due to meningitis in June 2007.
#MyNameIs not being invited to #NHS14Expo on #NHSChangeDay to talk about #dementia
One of the more nauseating aspects of #NHS14Expo were people asking me as usual why I hadn’t gone to #NHS14Expo.
It’s quite simple.
I wasn’t invited.
@nursingtimesed @tommyNtour Wasn’t invited.
— shibley (@legalaware) March 4, 2014
I had a chat with Martin Rathfelder, the Director of the Socialist Health Association, about it. I’m currently on their Central Council.
Like one of my followers @RoyLilley, I have a vague interest in English health policy – as evidenced perhaps by my 300 blogposts on the matter this year?
“You would have loved it Shibley! You should’ve come!”
Arrggghhh.
But then Martin suggested a number of routes by which I could legitimately come next year – one of them was joining a CCG, or becoming a NHS Foundation Trust governor.
I do have a cursory interest in postgraduate medicine, and have in fact written some books on it.
Martin also suggested I could capitalise on an interest in long term conditions.
As is well known, I survived a six week coma due to meningitis in 2007. That’s how I became physically disabled. I’ve been in recovery from alcohol ever since, and successfully regulated (and rehabilitated) by the Solicitors Regulation Authority who oversee lawyers.
Martin also suggested dementia as an inroad.
I have an interest in this too.
My paper in Brain in 1999 was the first to explain the symptoms of frontal dementia.
It has been quoted over 300 times by major labs.
It’s even in the current Oxford Textbook of Medicine in their chapter on dementia.
My pal Prof John Locke politely suggested that, as I had actually done a MBA, I was more than capable of marketing my own book.
In fact, in that MBA I also did come top of innovation in the year (though I did come top of both domestic and international marketing too).
Or is it because I am a total social recluse?
Tell that to my 11.7K followers on @legalaware, including David Nicholson, NHS England’s CEO.
David’s Twitter is @DavidNichols0n and his colleagues Clare Gerada (@clarercgp) and Alistair Burns (@ABurns1907) who also follow me.
Tell also fellow followers @helenbevan and @JoeMcCrea1966, two of the principal architects of #NHSChangeDay.
Or is it that I didn’t do a pledge for #NHSChangeDay?
No – I did a pledge. It’s here.
I’ll think about Martin’s advice.
On a happier note, I’ve been given a desk to do my research questionnaire on perception of #G8Dementia at a one day conference in Scotland.
Glasgow of course was where I was born. I like their dementia policy too.
And they’ve given me a chance to talk about my evidence-based book on living well with dementia – it’s here, and my marketing opportunities are non-existent.
Of course, I wasn’t actively excluded.
And one final note.
My book on ‘Living well with dementia’ is here – go and buy it, I beg you! Pleeeeeezzzzzzzzzz
Rant over.
It was honour to speak to a group of suspended Doctors on the Practitioner Health Programme this morning about recovery
It was a real honour and privilege to be invited to give a talk to a group of medical Doctors who were currently suspended on the GMC Medical Register this morning (in confidence). I gave a talk for about thirty minutes, and took questions afterwards. I have enormous affection for the medical profession in fact, having obtained a First at Cambridge in 1996, and also produced a seminal paper in dementia published in a leading journal as part of my Ph.D. there. I have had nothing to do with the medical profession for several years now, apart from volunteering part-time for two medical charities in London which I no longer do.
I currently think patient safety is paramount, and Doctors with addiction problems often do not realise the effect the negative impact of their addiction on their performance. No regulatory authority can do ‘outreach’, otherwise it would be there forever, in the same way that Alcoholics Anonymous or Narcotics Anonymous do not actively go out looking for people with addiction problems. I personally have doubts about the notion of a ‘high functioning addict’, as the addict is virtually oblivious to all the distress and débris caused by their addiction; the impact on others is much worse than on the individual himself, who can lack insight and can be in denial. Insight is something that is best for others to judge.
However, I have now been in recovery for 72 months, with things having come to a head when I was admitted in August 2007 having had an epileptic seizure and asystolic cardiac arrest. Having woken up on the top floor of the Royal Free Hospital in pitch darkness, I had to cope with recovery from alcoholism (I have never been addicted to any other drugs), and newly-acquired physical disability. I in fact could neither walk nor talk. Nonetheless, I am happy as I live with my mum in Primrose Hill, have never had any regular salaried employment since my coma in the summer of 2007, received scholarships to do my MBA and legal training (otherwise my life would have become totally unsustainable financially apart from my disability living allowance which I use for my mobility and living). I am also very proud to have completed my Master of Law with a commendation in January 2011. My greatest achievement of all has been sustaining my recovery, and my talk went very well this morning.
The message I wished to impart that personal health and recovery is much more important than temporary abstinence, ‘getting the certificate’ and carrying on with your career if you have a genuine problem. People in any discipline will often not seek help for addiction, as they worry about their training record. Some will even not enlist with a G.P., in case the GP reports them to a regulatory authority. I discussed how I had a brilliant doctor-patient relationship with my own G.P. and how the support from the Solicitors Regulation Authority (who allowed me unconditionally to do the Legal Practice Course after an extensive due diligence) had been vital, but I also fielded questions on the potential impact of stigma of stigma in the regulatory process as a barrier-to-recovery.
I gave an extensive list of my own ‘support network’, which included my own G.P., psychiatrist, my mum, other family and friends, the Practitioner Health Programme, and ‘After Care’ at my local hospital.
The Practitioner Health Programme, supported by the General Medical Council, describes itself as follows:
The Practitioner Health Programme is a free, confidential service for doctors and dentists living in London who have mental or physical health concerns and/or addiction problems.
Any medical or dental practitioner can use the service, where they have
• A mental health or addiction concern (at any level of severity) and/or
• A physical health concern (where that concern may impact on the practitioner’s performance.)
I was asked which of these had helped me the most, which I thought was a very good question. I said that it was not necessarily the case that a bigger network was necessarily better, but it did need individuals to be open and truthful with you if things began to go wrong. It gave me a chance to outline the fundamental conundrum of recovery; it’s impossible to go into recovery on your own (for many this will mean going to A.A. or other meetings, and discussing recovery with close friends), but likewise the only person who can help you is yourself (no number of expensive ‘rehabs’ will on their own provide you with the ‘cure’.) This is of course a lifelong battle for me, and whilst I am very happy now as things have moved on for me, I hope I may at last help others who need help in a non-professional capacity.
Best wishes, Shibley
My talk [ edited ]
It was honour to speak to a group of suspended Doctors on the Practitioner Health Programme this morning about recovery
It was a real honour and privilege to be invited to give a talk to a group of medical Doctors who were currently suspended on the GMC Medical Register this morning (in confidence). I gave a talk for about thirty minutes, and took questions afterwards. I have enormous affection for the medical profession in fact, having obtained a First at Cambridge in 1996, and also produced a seminal paper in dementia published in a leading journal as part of my Ph.D. there. I have had nothing to do with the medical profession for several years now, apart from volunteering part-time for two medical charities in London which I no longer do.
I think patient safety is paramount, and Doctors with addiction problems often do not realise the effect the negative impact of their addiction on their performance. No regulatory authority can do ‘outreach’, otherwise it would be there forever, in the same way that Alcoholics Anonymous or Narcotics Anonymous do not actively go out looking for people with addiction problems. I personally have doubts about the notion of a ‘high functioning addict’, as the addict is virtually oblivious to all the distress and débris caused by their addiction; the impact on others is much worse than on the individual himself, who can lack insight and can be in denial. Insight is something that is best for others to judge.
However, I have now been in recovery for 72 months, with things having come to a head when I was admitted in August 2007 having had an epileptic seizure and asystolic cardiac arrest. Having woken up on the top floor of the Royal Free Hospital in pitch darkness, I had to cope with recovery from alcoholism (I have never been addicted to any other drugs), and newly-acquired physical disability. I in fact could neither walk nor talk. Nonetheless, I am happy as I live with my mum in Primrose Hill, have never had any regular salaried employment since my coma in the summer of 2007, received scholarships to do my MBA and legal training (otherwise my life would have become totally unsustainable financially apart from my disability living allowance which I use for my mobility and living). I am also very proud to have completed my Master of Law with a commendation in January 2011. My greatest achievement of all has been sustaining my recovery, and my talk went very well this morning.
The message I wished to impart that personal health and recovery is much more important than temporary abstinence, ‘getting the certificate’ and carrying on with your career if you have a genuine problem. People in any discipline will often not seek help for addiction, as they worry about their training record. Some will even not enlist with a G.P., in case the GP reports them to a regulatory authority. I discussed how I had a brilliant doctor-patient relationship with my own G.P. and how the support from the Solicitors Regulation Authority (who allowed me unconditionally to do the Legal Practice Course after an extensive due diligence) had been vital, but I also fielded questions on the potential impact of stigma of stigma in the regulatory process as a barrier-to-recovery.
I gave an extensive list of my own ‘support network’, which included my own G.P., psychiatrist, my mum, other family and friends, the Practitioner Health Programme, and ‘After Care’ at my local hospital.
The Practitioner Health Programme, supported by the General Medical Council, describes itself as follows:
The Practitioner Health Programme is a free, confidential service for doctors and dentists living in London who have mental or physical health concerns and/or addiction problems.
Any medical or dental practitioner can use the service, where they have
• A mental health or addiction concern (at any level of severity) and/or
• A physical health concern (where that concern may impact on the practitioner’s performance.)
I was asked which of these had helped me the most, which I thought was a very good question. I said that it was not necessarily the case that a bigger network was necessarily better, but it did need individuals to be open and truthful with you if things began to go wrong. It gave me a chance to outline the fundamental conundrum of recovery; it’s impossible to go into recovery on your own (for many this will mean going to A.A. or other meetings, and discussing recovery with close friends), but likewise the only person who can help you is yourself (no number of expensive ‘rehabs’ will on their own provide you with the ‘cure’.) This is of course a lifelong battle for me, and whilst I am very happy now as things have moved on for me, I hope I may at last help others who need help in a non-professional capacity.
Best wishes, Shibley
My talk [ edited ]
I am finally discharged from Queen Square!
Monday was a highly emotional day for me. I was finally charged from the Neurorehabilitation clinic at the National Hospital for Neurology and Neurosurgery, Queen Square.
I must say that my medical team looking after me are fantastic. A dedicated team of clinicians, including neurologists at various stages of their training, the occupational therapists, the physiotherapists, and the speech-and-language therapy (SALT) people looked after me. My father and mother used to visit me religiously every day. My mother still has memories of coming to see me during visiting hours, with cooked food. My father passed away in November 2010.
The Hospital makes me extremely proud, as I practised neurology there long before I came alcoholic. I had the pleasure and honour of being on the movement disorders, cognitive disorders and dementia, neurogenetics and general neurology teams. I think the National Hospital for Neurology and Neurosurgery, Queen Square, is the best hospital in the world. Therefore, while it gives me great happiness in that I no longer have seizures (my last one was on admission in 2007) and I am now physically almost back to normal, it is of massive unhappiness I will probably never go there again.
I still actively research in dementia, working for a leading UK charity in Alzheimer’s Disease. I love it there, as I make contributions to their groundbreaking work on quality-of-life and wellbeing in dementia environments. I will be writing an open letter to the General Medical Council, having done my two degrees in law and MBA by that stage, with 57 months in recovery in 2013. The GMC can have a careful read of the transcripts now which provide that their Consultant gave in the hearing, that if erased my drinking would explode. This is exactly what happened, and it’s well known within medicine that you’re at extremely high risk of meningitis if you drink heavily.
I currently have the privilege of being able to complete my legal training, and I still have unanswered questions of my own about the treatment of sick doctors.
I look forward to the challenge. My father insisted that I should fight this fiercely, on a matter of principle. Thankfully, I have an excellent consultant. The BBC will be interested to follow my submissions particularly. I think both the medical and legal professions are wonderful, though, notwithstanding what I’ve said. I must thank the regulators for law for looking at my case fairly which allows me to pursue my current dreams.

Rehab
I did a period in rehab once. It didn’t work. I have been in recovery now for 45 months. You have to have to understand addiction of alcohol to make it work. Unless you have a willpower and fully acknowledge that alcohol addiction is a lifelong medical condition you have to learn to live with, you can’t make it.
I even tried equine therapy when my late father, my mum and I were really desperate. Don’t ask me what this involved!

Here’s the brilliant track from Amy Winehouse, “Rehab”.