Home » Staffing
It is puerile, in fact dangerous, to suggest the solution to NHS underfunding is private competition
In terms of any other sectors, market competition in perfect markets can often drive down prices and drive up quality.
Prof Michael Porter, one of the heads of department at Harvard, at the Harvard Business School, talks about ‘five forces of competition’, which is close to being taught on every single MBA course in the world.
The ‘Keogh trusts’, demonstrated to be working extremely poorly under the watch of the current Government and their Secretary of State, all have one thing in common. They all demonstrated dangerous levels of understaffing. In fact, the solution has been to remedy these inadequate levels.
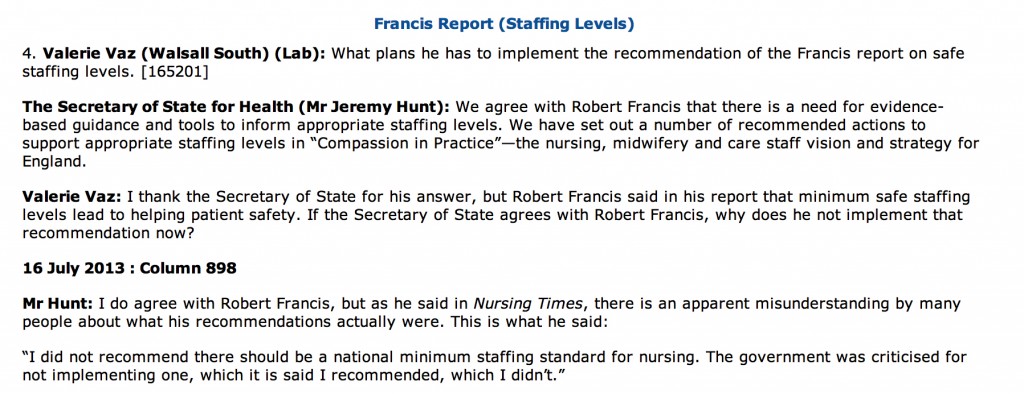
Jeremy Hunt has been steadfast in his refusal to implement a minimum level of staffing, preferring to talk of ‘safe staffing’ levels instead.
And yet junior nurses in the National Health Service often remark that their aspirational ‘6Cs’, which include ‘compassion’ so beloved of this current government, are undermined by unsafe staffing.
Even in the private sector in a checkout till on McDonalds, assistants are unable to cope with the demand to buy BigMacs if there is an insufficient number of colleagues. The inconvenience of having queues for Big Macs is one thing. An inability of clinical staff to work safely, putting patients at risk, is another thing.
It is of course unPC to blame the private sector, but NHS Foundation Trusts who have to make regular loan repayments as a major part of their budget may feel that they can get away with understaffing.
They invariably can’t, even if their CEOs move onto different jobs within an average timescale of two to three years.
The pervasive undercurrent in such arguments is that there should be an ideological ‘parity’ between the public and private sector.
And yet public concern at campaigners remain exasperated about private providers, who can fail to be transparent and who can fail to disclose their staffing figures, can hide under the ‘commercial confidentiality’ cloak in freedom of information requests. Jeremy Hunt, on behalf of the coalition, has stubbornly refused to legislate for this aspect of parity.
The competition argument for the National Health Service has always ignored the traditional powerful arguments of Porter’s ‘five forces’.
They include supplier power, in that the NHS being such a large organisation is able, theoretically, to benefit from ‘economies of scale’ (in a way, bulk buying).
It is not a real market, in that a patient is not a ‘real customer’ wanting to shop around. He (or she) wants simply to go to his most local hospital for an acute life-saving treatment, not go half way up the M1 to the hospital with the best coffee shop and Wifi.
And if the private sector were so confident about their brand, why do they prefer to use the NHS brand?
Would it be puerile to suggest that chronic underfunding of the NHS, sold in the media and by the thinktanks as ‘unsustainable’, could lead the NHS brand to be so tarnished that private sector operators like knights in shining armour might one day feel confident to show their brand for a desperate public?
Sean Worth may call our arguments puerile, but a lack of rigorous implementation of practitioner models of competition in the private sector, derived from the giant automobile sector in the US, coupled with an inability to mention the root cause of unsafe operational issues in the NHS, is far more dangerous argument to run.
The transfer of resources from the NHS to the private sector, also known as “privatisation”, is directly legislated for in section 75 Health and Social Care Act (2012).
This ‘top down reorganisation’, which David Cameron said would never happen, has so far cost about £3bn so far.
And the most disingenious aspect of the argument is perhaps in this argument arguing for private provision and performance in the NHS is that the Act of parliament, all 493 pages of it, does not contain a single clause on patient safety, apart from one abolishing the National Patient Safety Agency.
But many of us agree, on the left, Sean is a very pleasant man.
Machine politics by incremental soundbite is not a way for Jeremy Hunt to manage the NHS
 Jeremy Hunt’s tenure at the Department of Health has so far been pretty inglorious.
Jeremy Hunt’s tenure at the Department of Health has so far been pretty inglorious.
Hunt tweeted on December 13 2013, “Shocking Labour not supporting measures in Care Bill that will prevent another Mid Staffs. Have they learned nothing?”
The Care Bill is however intensely complicated. The Government plans to widen the powers of trust special administrators face opposition both within and outside Parliament. There can, of course, be grounds for hospital reconfigurations where this improves the quality of patient care, however it is essential that this takes place with proper regard to due process.
And yet Jeremy Hunt has allowed himself to be completely at the mercy of health services journalists, some of whom are not particularly bright and who have little understanding of the English law. Specialist registrars in medicine, the rank below a Consultant, can only wonder whether they wish to become a NHS consultant working in such demanding conditions.
It is clear that the Secretary of State for Health, too, cannot have that clear an understanding of the current law, as he has now lost in the second and third highest courts in England and Wales.
However, by courting certain people, Jeremy Hunt has ensured that he cannot be attacked by key personnel in the clinical regulators.
The NHS would be nowhere without the opinions and views of patient campaigners, particularly in the discussion over reconfigurations. The quality of their work continues to be astounding. The news about the Mid Staffs Trusts reconfigurations is expected shortly.
A similar issue has arisen with NHS consultant cover.
If Jeremy Hunt wants a NHS Consultant to do 24 hours for example, he presumably will have to pay another NHS Consultant to act ‘as cover’ for the next 24 hour period. Otherwise, this will offend ‘patient safety’ so beloved of many who had themselves not prevented a Mid Staffs previously.
If Jeremy Hunt wants NHS Consultants to be there seven days a week, he will presumably also pay for the formidable army of dieticians, occupational therapists, physiotherapists, speech and language therapists, nurses, healthcare allied professionals, ward clerks, and so it goes on, too. The costing figures estimating what this might cost have been virtually non-existent so far.
If Jeremy Hunt wants a NHS Consultant to do the work instead of Specialist Registrars, he must ensure that they are adequately trained and revalidated on specialist procedures such as insertion of a central line, chest drain or pacing wires, and pay for this.
Otherwise, Jeremy Hunt is all talk and no action.
It’s been long known that Tony Blair wished the civil service to be more ‘innovative’ and not act like technicians. The deprofessionalisation which the NHS finds itself now is a genuine problem.
If private providers really want ‘an equal playing field’, is it not reasonable to request private providers such as Circle, Serco or Virgin to pay for Specialist Registrar training posts in their ‘NHS hospitals’? They are, after all, using the NHS logo.
Otherwise, despite the brand loyalty, the time possibly has to come where the ‘National Health Service’ gets rebranded as a ‘whole person care service’ (or similar). The NHS is unrecognisable to how it used to be recently, and the legitimised use of the NHS logo is simply causing confusion from members of the public. This is unless of course politicians can unit on re-framing the NHS away from a pseudomarket, but as a service which is comprehensive, universal, and free-at-the-point of need.
As it is, we’re left with Jeremy Hunt and some health services journalists, and the clinical regulators, trying to move policy incrementally by soundbite, often by completely ignoring the professionals who matter: the doctors, nurses and allied health professionals. They should spend less time managing the media, and more time managing the NHS.
It’s all gimmicks, gimmicks, gimmicks.
The legal problem for Keogh is potentially an unilateral variation of contract and this needs a solution
“Society has moved on, and people expect more from their services.”
This was the fairly harmless way in which Sir Bruce Keogh, the Medical Director, commenced his interview with Jeremy Vine on “The Andrew Marr Show” this morning. And that of course is motherhood and apple pie at its best.
Keogh may not actually have a problem at all on his hands, as the vast majority of NHS Trusts in England have been doing some form of 24/7 for years. In fact, it’s well known that many NHS consultants who have received ‘clinical excellence awards’ have been working 24/7 for ages, without even batting an eyelid.
Keogh then dropped the bombshell that, historically, we’ve been very good at providing services five days a week, but there was an evidenced problem with mortality in hospitals at the weekends. Keogh also proposed that junior doctors are feeling particularly stressed at the weekends, because of the complexity of diagnosis and treatment, and Keogh felt that, “We should worry about that because we could be training our next generation of doctors better.”
A major drive has been to have more Consultants ‘on the ground’ 24/7, though most people concede that to run a full offering, there will need to be to some extent 24/7 input from physiotherapists, OTs, speech therapists, dieticians, allied health professionals, and possibly even secretaries and NHS managers.
Nonetheless, Keogh was able to formulate a perfectly cogent case for NHS Consultants being there 24/7: “If you have more Consultants present, you don’t have as many inappropriate admissions. Secondly, they… get more appropriate treatment. This will cost 1.5-2% of the annual costs of running a hospital.”
Keogh introduced the fact that this new approach would require more specialists, and this would cost money. “We need to find the money from somewhere. One of the most expensive costs is the cost of workforce. We’re about to produce 1800 more specialists.”
This is what Andy Burnham MP, Shadow Secretary of State for Health, has asked about time and time again. Even Burnham has probably got fed up of banging his head against this particular brick wall.
However, the most revealing part of the interview was when this morning’s presenter of the Marr Show, Jeremy Vine, asked about the actual practical issue: as to whether the NHS could simply change contracts.
Keogh responded, “Most of my consultant colleagues are in at the weekend anyway.”… “All people in the NHS, from the managerial community, think it’s the right thing to do.”
This drew polite short shrift from Vine, “The fact that there are some nice consultants is neither here nor there.”
Clearly the entire NHS cannot be run on the goodwill of Keogh’s pals. Keogh instead offered that,
“This isn’t about money, it’s about flexible working practices, and better recruitment. We believe the arguments for this are compelling.”
And the indeed the problem is not in introducing new contracts for new Consultants in the NHS. You can simply introduce new terms and conditions for them. It is what to do with existing Consultants with existing employment contracts.
The general position in English employment is that a party cannot unilaterally vary the terms of a contract. The position reflects the principle that a unilateral material change of terms may equate to a fundamental ‘repudiatory’ breach of contract. A repudiatory breach is one that is so fundamental to the contract that the aggrieved party may terminate it and sue for damages. Of course, it could be that there is no change in contract as ‘consultants are doing this anyway’. But it is not unheard of for all NHS staff, of all ranks, to do work effectively for free (for example checking up on liver function tests in a cirrhotic patient with a queried life-threatening subacute peritonitis.) However, the position is not so straight forward where a party is allowed to amend a contract unilaterally by virtue of a term in that contract.
If an employer tries to impose a variation of contract, they will potentially be in breach of contract.
To decide whether they are, two initial questions have to be asked:
- Is the term being varied a term of the contract? And, if so, does the employer have the right to unilaterally vary it?
- Working hours will invariably an explicit term of that employment contract between a NHS consultant and a Trust.
However, terms enabling unilateral variation are allowed in contracts and are not that hard to find. Two widely used examples in the commercial world are those granting sellers the power to change the price of their goods and those granting lenders the right to vary the rate of interest charged.
There are a number of ways that an employer can change/vary your employment contract legally. By obtaining your consent to vary/change the contract of employment. This can be done either orally or in writing, although it is better in writing. Any employer can imposing changes/variations to your employment contract with your implied consent. An example of this would be if your employer brought in new terms and conditions, and you did not raise any objection to them after they had been brought in and you continued to work in accordance with the new terms and conditions. Here it’s going to be critical to see what the precise reaction of the BMA is, often referred to in the BBC and the professional press as “the Doctors’ Union”. By relying on an existing clause in an employment contract that gives the employer the contractual right to vary/change the contract. These clauses are more commonly referred to as “variation clauses” or “flexibility clauses”. For a variation clause to be enforceable, it must be clear, specific and unambiguous. These clauses are terms in a contract that give employers the right to change some other condition of employment, eg relocation to a hospital as part of a regional network of Trusts.
If this Government, or indeed any Government, wished to ‘steamroller’ this policy of 24/7 for NHS consultants, there are two possible basic approaches, both of which entail legal risks and potential damage to general employer/employee relations. The employer make a unilateral change to the existing contract by simply announcing the change and implementing it forthwith or with notice. Or the employer could simply terminate the existing employment contract with proper notice (whilst complying with the statutory dismissal procedures), and offer re-engagement on a new contract which reflects the amended terms If the employer adopts the first approach, the employee may accept the change despite an initial protest. However, employees may continue to protest, insist on the terms of the original contract, and either bring a claim for breach of contract or resign and claim “constructive dismissal”.
Alternatively, they could work under the new terms, but “under protest” which means they reserve their right to claim breach of contract or, in limited cases, unfair dismissal. The employer would be unlikely to have a defence to these claims and the tribunal may not only award compensation for the loss previous employees have suffered as a result of the change or dismissal but also make an award that these employees are in fact reinstated to their job on their original terms. If approach two is adopted, the employee is being dismissed and can therefore still claim unfair dismissal. However, if there is a reasonable consultation process an employer would be more likely to be able to defend a claim on this basis than under approach one and more likely to minimise any compensatory payments. Importantly, however, the change will not be revoked and the employee will have to bring any action within three months of the dismissal.
All of these legal issues of course assume that NHS Consultants, if they were in such a professional situation, would be properly legally advised. The cost in legal fees, and legal claims in general, is not an unknown notion for the NHS currently given the estimated £3bn implementation of the Health and Social Care Act (2012) which outsourced the NHS, set up a stronger insolvency regime for ‘failing hospitals’, and gave greater powers to the economic regulator of the NHS (“Monitor”).
This has been criticised previously in the GP magazine:
“From then on, each management level may resort to bullying those below in order to force these unworkable policies through, complete with personal threats of what will happen if their orders are not obeyed or targets not hit. This is when managers can throw their weight around by insisting that ‘this is government policy’ and therefore ‘you will carry this out’ — if only to make their own jobs secure. We have here the NHS version of constructive dismissal: the setting of impossible targets, which are then cascaded throughout the entire organisation. And because these goals are ultimately unattainable, compliance has to be attempted through intimidation rather than the use of logical argument. I’m sure that this scenario explains why bullying in the NHS has now become endemic.The solution is simple: creating an impossible target should be treated in law both as bullying and constructive dismissal. Those who do it should be sacked from the NHS and told never to return.”
As for the basic issue, it is perhaps laudable that Keogh and the NHS, under this administration or any other, should wish hospitals to be run 24/7 like any other organisation. The legal issues will have to be overcome, but the major issue is still resources. The comparable situation in a supermarket would be like having the doors open but with fewer cashier assistants, no people supervising cashiers, no people doing “store fills” (they’re the people who ensure the store shelves are well stocked and that the shop is clean and tidy for when you, as customers are in the store), checkout supervisors, bakery managers (if the bakery is an essential part of your offering), and so on.
Disclaimer: This blogpost should not be construed in any way as a professional legal opinion. It is simply an academic comment.
Fears and smears – wilful inattention from healthcare journalists?
In an article today in the Independent, subtitled “Fears and smears”, Ed Miliband MP writes:
“They want to distract attention from the issues that matter. With the support of a determined section of the press, they have decided that mudslinging matters more than the futures of millions of families across this country.”
Discussion of the NHS is an incredibly sensitive area and yet it has been done incredibly badly by many journalists and politicians.
Mid Staffs was an unacceptable disaster. It was THE low point in the NHS.
Relatives of loved ones have shown incredible bravery and resilience in the face of an unbelievably tragic intolerable event.
For many, the issues in Mid Staffs appeared to be simply brushed under the carpet for political purposes, and real patients and relatives suffered.
The claim over professional codes and a duty of candour
On Thursday, Jeremy Hunt gave an answer on Mid Staffs on the BBC programme ‘Question Time‘. Regarding making it easier for people to speak out, “people are going to be given protection in their professional codes which have happened before.”
Mr Hunt is therefore speaking as if this has sprung up from nowhere.
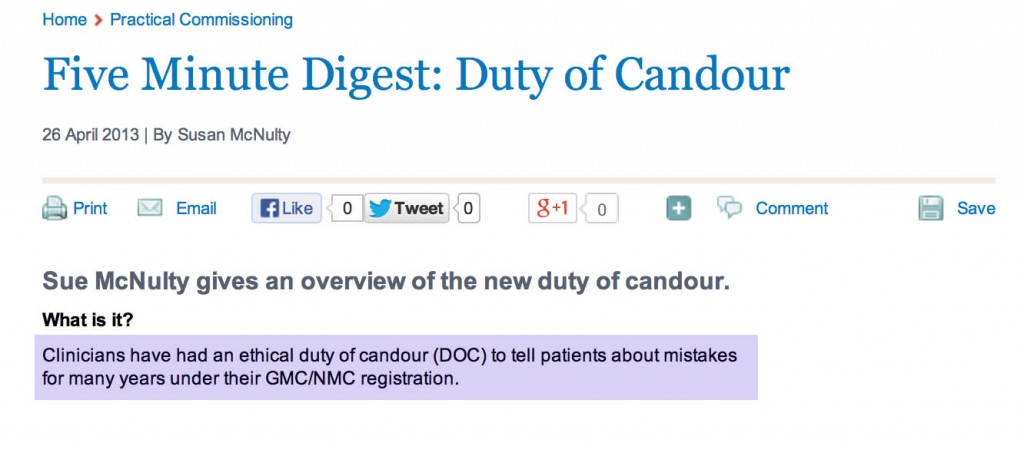
Not true, even from the briefest scan of ‘Five Minute Digest – Duty of Candour’ in ‘Pulse Today‘:
The claim that Burnham opposed an inquiry
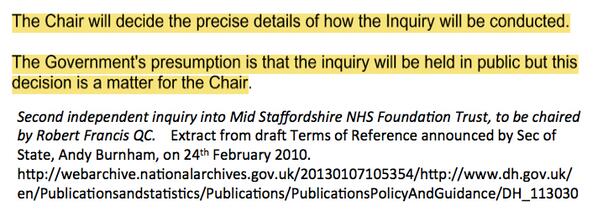
There are two inquiries – when you read the rest of this article, be mindful that
- November 2009 – Robert Francis QC begins hearing evidence in private as part of his independent inquiry
- February 2010 – Robert Francis QC publishes his independent inquiry report into the poor care at Mid Staffordshire Foundation Trust
- May 2010 – Change of government and Health Secretary
- November 2010 – The public inquiry begins to hear evidence
- December 2011 – The public inquiry finishes hearing evidence after more than 12 months
In Question Time last week, regarding Mid Staffs, Mr Hunt explained, “Your party opposed a public inquiry. Andy Burnham decided to oppose a public inquiry.”
The Executive Summary of the Report of the public inquiry, published in 2013, is here.
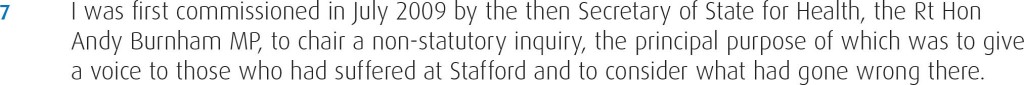
The way the original private inquiry was set up by Andy Burnham MP, the then Secretary of State for Health, is described in the 2013 Francis report as follows.
A new Government was elected in the UK in May 2010. The way in which Andrew Lansley MP, the then Secretary of State for Health, set up a public inquiry is provided in the 2013 Francis report as follows.
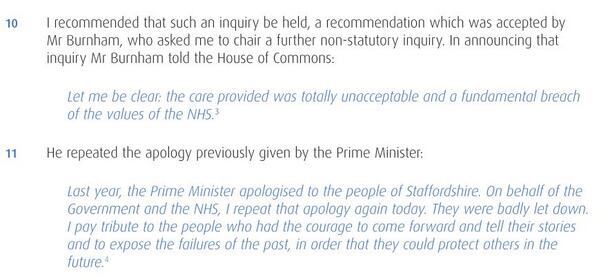
This actually came as no surprise, as Andy Burnham MP had already stated that the second Inquiry would be held in public, as cited here.
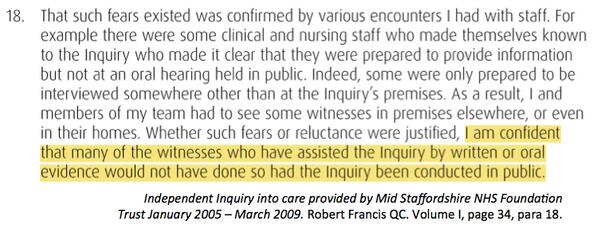
Francis himself did not want the first inquiry to sit in public for the first time, and is even reported as being satisfied with the arrangements, as cited here.
The problem here is in the media at large the genuine message that Burnham set up the first inquiry in 2009 ‘to give patients a voice’ has been swamped by the toxic meme from some, and they know who they are, that ‘Burnham blocked an inquiry’.
The claim that Burnham never apologised
Another blatant classic lie is that Burnham has never ‘apologised for Mid Staffs’.
This is addressed too, as cited here.
The claim that Burnham resisted an inquiry under the Inquiries Act
Burnham obviously did not have any powers as Secretary of State for Health after the General Election of May 2010. The decision for the second public inquiry comes after that date.
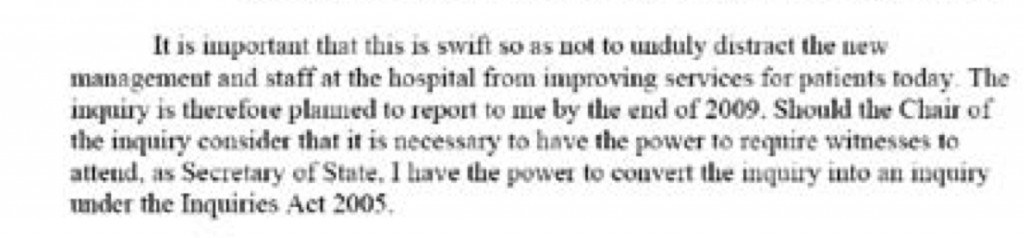
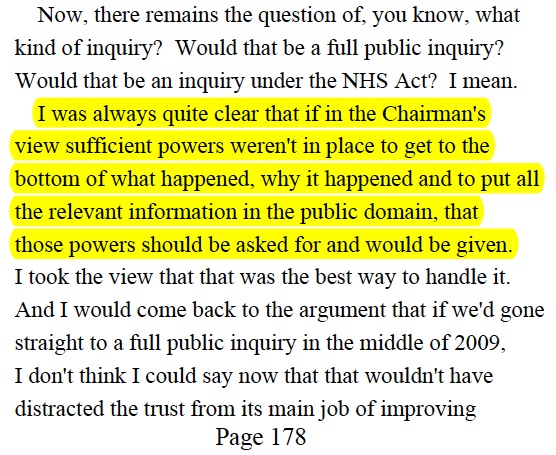
It has been claimed furthermore that Andy Burnham MP resisted his inquiry to take place under the auspices of the Inquiries Act, but Burnham did actually leave it all times to be directed by Francis, the Chair of the Inquiry.
This legally is a somewhat obtuse claim, as it was a Labour government which enacted the Inquiries Act in 2005 in the first place.
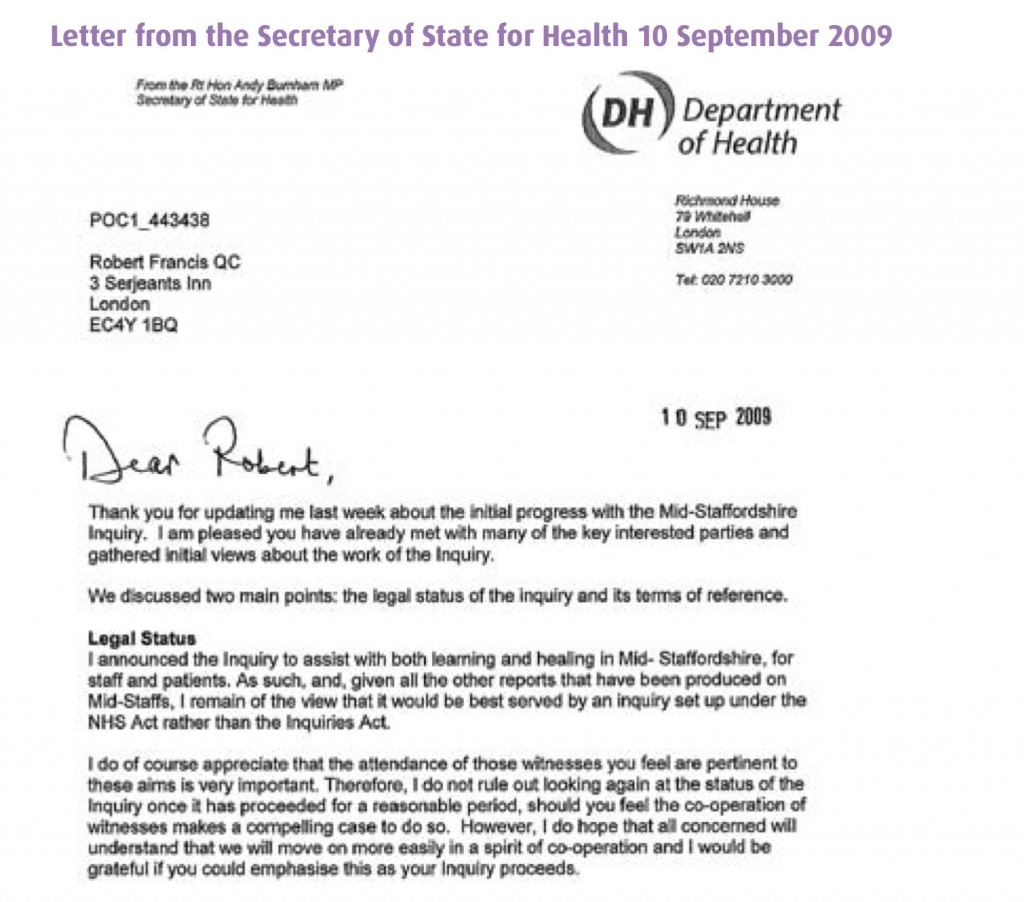
In Appendix 1 of the bundle of documents entitled “Independent Inquiry into care provided by Mid Staffordshire NHS Foundation Trust January 2005-March 2009 Volume 1″ Appendix 2, Andy Burnham MP as the then Secretary of State for Health in his Written Ministerial statement (21 July 2009) first cites his perceived need to set up an inquiry “swift so as not to unduly distract the new management and staff at the hospital from improving services for today”, but that he has the power to convert the Inquiry to one under the Inquiries Act should the Chair of the Inquiry (Robert Francis QC) should demand it.
This exact text of the statement is indeed evidenced in Hansard, for 21 July 2009 Column WS188 as per here.
In Appendix 2 of the bundle of documents entitled “Independent Inquiry into care provided by Mid Staffordshire NHS Foundation Trust January 2005-March 2009 Volume 1″ Appendix 2, Andy Burnham MP as the then Secretary of State for Health repeats (10 September 2009) his willingness for his inquiry to be set up under the Inquiries Act not the NHS Act.
This is the evidence that Burnham gave to Francis 2 on 6 Sep 2011, page 178:
Indeed, parsimoniously, the option of ‘converting another form of inquiry’ into an Inquiry as under the Inquiries Act at any time is clearly good application of the law, under section 15 Inquiries Act (2005).
The claim that ‘wilful neglect’ legislation is a fundamental new shift in the law
The Berwick Report itself was all about constructive organisational learning, and only introducing a statutory crime of ‘wilful neglect’ for the most extreme cases.
Some vocal campaigners in Mid Staffs clearly desire targeted retributive justice, but the media thus far have refused to cover why the law of ‘wilful neglect’ in the form of section 44 Mental Capacity Act (2005) has failed to see a flurry of successful criminal prosecutions in Mid Staffs. We have instead discusssed it here. ‘Wilful neglect’ is NOT a fundamental new shift in the law, unless it can now be applied to adults with full capacity.
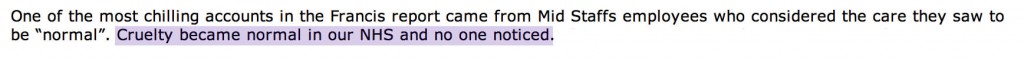
The claim that ‘there was a culture of cruelty in the NHS and no-one noticed”
Staff in various NHS Trusts have voiced loudly their resentment as being targeted in some sort of ‘hate campaign’.
Jeremy Hunt last week specifically referred to how a culture of cruelty ‘became normal in our NHS’, not in any particular Trust.
as cited in Hansard 19 November 2013.
Summary
The problem in this imbalance of irresponsible reporting is that it creates a culture of fear in NHS nurses, even in those ‘who have nothing to hide’. It is not a mature discussion of the technical problems in the law. It is instead ‘red meat’, ‘dog whistle’ politics of the worst kind, of a particular political inclination. As a result of memes about the Inquiry, candour and putting clinical staff in the clink, an irresponsible media has diverted attention from important issues.
By allowing copious air time for lies, the important discussion of why A&E is experiencing difficulties, a lack of a stated minimum level of safe staffing, why social care cuts have been so dangerous, or why NHS 111 has failed so dramatically, have not been explored in any level of acceptable detail.
Sadiq Khan MP tried valiantly to bring up how staffing levels had been so low, and ‘without the doctors and nurses, it’s all talk and no action.” But the stench of the narrative above diverted him from discussing the critical issues as much as he would have liked, although he did get in an official statistic about a cut in nursing numbers.
Real staff are none-the-wiser. Patient campaigners are led down the river without a paddle. Voters are completely bamboozled.
This is an unholy disgusting mess from those responsible. Call it wilful inattention.
Thanks to the public tweets of @gabrielscally for many of the extracts cited in the article.
There may not be enough sunlight to go round to ‘disinfect’ the NHS
Today was by far one of Jeremy Hunt’s best performances on the NHS in the House of Commons.
Having been criticised recently by two former Secretaries of State for the Health, Alan Milburn and Stephen Dorrell, the room for manoeuvre was very slim.
On the issue of ‘that number’ for safe staffing, Hunt had a trick up his sleeve with apparent support for not setting levels. The concern about setting a minimum number was that this would not reflect the skill mix of nursing staff on the wards, and might unwittingly end up being a quasi-target.
Whilst the construct of economic competition and the NHS has been virtually ubiquitously conceded to be a failure, it is possible that NHS Trusts will not wish to compete ‘in a race to the bottom’ over staffing levels.
How these data will be presented in a meaningful way is anyone’s guess.
But the beauty with this approach is that it avoids Government centrally specifying indirectly the staffing budget for NHS Foundation Trusts. So, if these Trusts later go ‘bust’ due to an inability to balance the books due to a massive PFI loan, it’s not perceived as the Government’s direct fault.
If Trusts run bargain basement staffing levels, Government is not to blame.
And result! They still get their £30bn ‘efficiency savings’?
And the hardworking nurses who get made redundant, even having passed their ‘good character’ test?
Nothing to do with me, mate.
He also had some further issues ‘under control’. The review into patient complaints, co-authored by Prof Tricia Hart, had successfully concluded that the current NHS complaints system is inadequate. Something’s going to be done about it apparently.
Hunt further decided that, whilst he would impose a statutory duty of candour for organisations, he would go no further than the current position of the clinical regulators requiring candour in the professional clinical code from individuals.
Of course, the ‘acid test’ is whether any of this works in practice.
There is still a sizeable yet relatively small number of people who feel that some people in the NHS do not demonstrate any candour at all.
So why isn’t this deception fraud? Quite simply, that’s because it’s not under the Fraud Act (2006), strictly defined in law as exposing someone to a loss financially (or producing a material gain).
It may be one day that the legislature considers a statutory offence of fraudulent misrepresentations in official clinical notes.
There were some further issues.
‘Healthcare assistants’ were rebranded ‘nursing assistants’, which means that their legal regulatory requirements might one day be defined with greater clarity. Hunt argued that requiring them to have a certificate ensured a level of competence.
But have Hunt’s remarks fundamentally changed things?
Possibly yes, if NHS FT CEOs are not able to do a ‘merry go round’ of jobs even after demonstrable failure.
Will this work? Well… probably not.
Will it be a revolution of the kind to make Russell Brand envious?
Probably not, if there are still toxic parts of the NHS, Hunt’s medicine cannot reach.
If Hunt were a medic, he’d understand this in terms of drug bioavailability. But he’s not.
As an associate justice of the U.S. Supreme Court, a man called Louis Dembitz Brandeis (1856-1941) tried to reconcile the developing powers of modern government and society with the maintenance of individual liberties and opportunities for personal development.
He coined the famous phrase, “Publicity is justly commended as a remedy for social and industrial diseases. Sunlight is said to be the best of disinfectants; electric light the most efficient policeman.”
The Berwick Report was fundamentally about organisational learning after mistakes.
Everyone makes mistakes, and sometimes these mistakes are harmful to the team’s efforts. However, it is argued developing a strong culture of transparency and accountability can focus your teams efforts where they belong: doing brilliant work.
The alternative is a blame culture.
Perhaps for the most serious offences, ‘wilful neglect’ (which is very hard to prove, if the case law of section 44 Mental Capacity Act is anything to go by) will get people ‘out of the system’.
Today, noticeably Sir Brian Jarman was absent.
The day’s media coverage was not accompanied by a torrent of media reporting about ‘needless deaths’.
Even Sir David Nicholson in August 2013 had got fed up. He was calling for more balance in the way the media handles the NHS in an interview he gave.
“It’s either all fantastic or all terrible, when in fact both things happen simultaneously.”
“There were managers versus doctors, doctors versus nurses, surgeons versus medics…”
He had made a speech where he said:
“Over the last few months, it’s as though a wheel has been spun every so often… ‘Let’s all attack nurses’ or another week it’s ‘let’s have a go at general practitioners’.”
Nicholson had therefore progressively been highlighting the need to stop the witch hunts and take a more grown up view of the situation.
In corporate culture, the giant ENRON was brought down by off-balance-sheet transactions: transactions deliberately designed to conceal from trustees, regulators and the market the extent of the risk to which shareholders were exposed. Their lawyers and accountants connived to make the deception as lawful as they could, but it remained a concealment.
This is exactly the same problem the NHS faces.
So regulation strives to shine a light into those awkward nooks and crannies, but it is a cumbersome light source and there is a large body of professionals dedicated to dimming its flame and to diverting its glare.
Any company needs to be transparent about its corporate decisions including its business plans. It must be transparent.
That is why nobody can make out why the Government is so evasive about making private companies accountable to the same freedom of information disclosure requirements as the NHS.
This parity is clearly in the public interest, with a new liberalised market with equality of provider, when ‘commercial sensitive’ decisions can impact on patient safety.
Not my crap speak. Theirs.
On 4 March 2013, a Conservative Stephen Barclay MP used the sunlight as disinfectant allegory. Barclay opined that the Prime Minister had said that sunlight is the best disinfectant, “and that applies on our hospital wards. It is best for us to have well-informed patients and staff who are able to voice their concerns.”.
Later on 16 July 2013, another Conservative David Tredinnick MP asked, “Sadly, the problems at George Eliot hospital go back well over a decade, so these special measures will be very welcome, but is not one of my right hon. Friend’s fundamental problems dealing with a culture of secrecy, where in the past a board with a problem would talk to a strategic health authority board and nobody would know what was going on? Is not sunlight the best disinfectant?”
And not to be outdone, a third Conservative, Stephen Dorrell MP, reverted to disinfectants and transparency.
Dorrell remarked today, “Is not the central driver of my right hon. Friend’s recommendations to ensure that never again shall we have closed institutions in a closed system where that is possible, and that the key way forward is to throw sunlight into institutions that have too often been unchallenged?”
If the complaints system works, then that’s great. If NHS FTs compete to produce good levels of safe staffing, that’s great.
If NHS CEOs don’t go round the circuit with massive salaries but terrible performance, that’s great.
If you can stop people going to hospital unnecessarily, by pumping more money more effectively into the outsourced NHS, that’s great.
If some managers no longer bully, even though nobody wants to change the faulty Public Interest Disclosure Act (1998), that’s great.
If private providers decide ‘to do the right thing’ in the name and transparency, and decide not to hide behind a corporate veil of commercial sensitivity so as to publish data on staffing, that’s wonderful.
But that’s a lot of ‘if’s.
And there may not be enough sunlight to go round.
Why speaking out safely and safe staffing are important moral issues for the NHS
 A culture where staff and patients can speak openly about successes and failures in the NHS, as well as more specifically on safe staffing issues, is essential for the NHS to move forward. Perhaps most intriguingly, the failure of the English law to cherish the need to ‘speak out safely’ in the NHS can be tracked back to four Acts of parliament ranging in the last thirty years uptil the present day.
A culture where staff and patients can speak openly about successes and failures in the NHS, as well as more specifically on safe staffing issues, is essential for the NHS to move forward. Perhaps most intriguingly, the failure of the English law to cherish the need to ‘speak out safely’ in the NHS can be tracked back to four Acts of parliament ranging in the last thirty years uptil the present day.
The focus recently has tended to be about whether things would or would not work, and have either been economic or regulatory in perspective.
The Health and Social Care Act (2012), all 493 pages of it, is fundamentally a statutory instrument which proposes the mechanism for competitive tendering in the NHS (through the now infamous section 75), the financial failure regimes, and the regulatory mechanisms to oversee an emboldened market. It is therefore a gift for the corporate lawyers. It does, though, successfully mandate in law the abolition of the National Patient Safety Agency in s. 281.
There is therefore not a single clause on patient safety in this voluminous document. Patients, and the workforce of the NHS, are however at the heart of the NHS.
The language has been overridden by economic concepts misapplied. “Sustainability” is a very good example. Too often, sustainability has been used as a synonym for ‘maintained’, usually as a precursor for an argument about shutting down NHS services. It quite clearly from the management literature means a future plan of an entity with due regard to its whole environment.
Discussion about regulators can lead to a paralysis of policy.
No sanctions against Doctors have yet been made by the GMC over Mid Staffs, which does rather appear to be a curious paradox given the widespread admissions of undeniably ‘substandard care’. The regulator needs to have the confidence of the public too. One of their rôles is commonly cited to be to ‘protect the public‘, and this is indeed enshrined in law under s.1(1A) Medical Act (1983).
It is of regulatory interest how precisely the GMC ‘protected the public’ over Mid Staffs, whatever the operational justifications of their legal processes in this particular case.
Strictly speaking, promoting the safety of the public might include promoting the ability of clinical staff ‘to speak out safely’, and this could be an important manifestation of a core legal objective of that particular regulator?
On the other hand, confidence in the regulator is never achieved by any regulator on the basis of conducting “show trials“. This can be always be a big danger, as GMC cases on occasions attract wider general media interest. This will, of course, be to the detriment of defendants with complicated mental health issues.
There is little fundamental dispute about the need for clinicians to be open about medical errors in their line of work. Even the Compensation Act (2006), if you need to cite the law, provides that an apology does not mean an admission of liability in section 2.
There can be disputes about upon whom the ‘duty of candour’ should fall, whether this might be the Trust or an individual clinician, and who is going to enforce it.
But just because there are legal issues about the practicality of it, a civilised society must use the law to reflect the society it wishes for.
There is currently, for example, a statutory duty for company directors to maximise shareholder dividend of a company with due regard to the environment (as per s.172 Companies Act (2006)). There is no corresponding duty for hospitals to minimise morbidity or mortality on their watch.
“Whistleblowers” are often accused of raising their complaints too late.
Whistleblowers can find themselves becoming alien for NHS organisations they are devoted to.
Often, there is a ‘clipboard mentality’ where ‘colleagues’ will raise issues to discredit the whistleblowers. Often these ‘colleagues’ are protecting their own back. Regulators should not collude in such initiatives.
And yet it is clear that the Public Interest Disclosure Act 1998 fails both patients and whistleblowers.
There are ways to bring about change. Most often regulation is not in fact the answer.
A cultural change is definitely needed, and this appears to go beyond corrective mechanisms through English jurisprudence.
This in the alternative requires staff and patients from within the NHS prioritising speaking out safely.
The information which can be provided by ‘speaking out safely’ should be treated like gold dust – and be used for improvement for patient safety in the NHS, as well as in the performance management of all clinicians involved.
Arguably the precise information is much more useful than an estimate such as the ‘hospital standardised mortality ratio’ which does not operate on a case-by-case basis anyway.
A new-found desire to speak openly might also include a wider policy discussion about safe staffing levels. Regulating a minimum staffing level might shut down important debates about ‘what is safe’, such as the skill mix etc. And yet there are equally important issues about how to prioritise this in the law.
The hypothesis that unsafe staffing levels or poor resources generally lead to poor patient safety in some foci of the NHS has not been rejected yet. It’s essential that managers allow staff to be listened to, if they have genuine concerns. Not everything is vexatious.
Most of all, society has to be seen to reward those people who have been strong in putting the patient first.
Small steps such as Trusts in England supporting the Nursing Times’ “Speak Out Safely” campaign are important.
Critically, such support is vital, whatever political ideology you hail from.
It could well be that the parliamentary draftsmen produce a disruptive innovation in jurisprudence, such that speaking out safely is correctly valued in the English law, and thenceforth in the behaviour of the NHS.
Hopefully, an initial move with the recent drafting of a clause of the “legal duty of candour” in the Care Bill (2013) we will begin to see a fundamental change in approach at last.
This country is for hard-working people. But not hard-working nurses?
 When your script is written by a hard-nosed hedgie or private equity fund owner, it can be easy to lose sight of the basic fact that it’d be impossible to run the NHS without nurses.
When your script is written by a hard-nosed hedgie or private equity fund owner, it can be easy to lose sight of the basic fact that it’d be impossible to run the NHS without nurses.
“Aspiration” has been a powerful slogan for all main political parties in the UK, with a history of its own. Historically, Labour has drifted away over decades from ‘working class people’ to ‘middle class people’, so much so people have asked what Labour really can offer those at the lowest end of the pay scale.
“Hard-working” is not necessarily synonymous with “being very well-paid”. There are hundreds of thousands of healthcare professionals, staff grades or experienced specialist nurses, who are extremely hard-working. Many of them are not well-paid. Professional footballers and employees in the City tend to be well paid. Nurses tend to have their job as their source of income. Some people have various sources of income, naming no names.
Unsurprisingly, the Unions have criticised Government moves to halt a 1% pay rise for all NHS staff in England. The Department of Health said the increase was “unaffordable” alongside the current system which sees many staff automatically receive incremental annual rises. This is, of course, a totally bizarre argument when you consider that around £3 bn was returned into the Treasury only last year.
It was decided that these savings should not be pumped back into frontline care, staggering when you consider the close link between patient safety and safe staffing. Health trusts are currently under pressure to make savings and the NHS wage bill accounts for around 40% of its budget.
The Conservative party conference was plastered with the phrase “hard-working” – “For Hardworking People” beaming from the platform – and a host of frontbench speakers milked the term for every last iota of rhetorical impact. It’s hard to know exactly where this odd meme came from, but it might be something to do with George Osborne decided to tweet #hardworking in his popular tweets.
Of course, “hard-working” – whether it is a predicate of “families” or “people” – is potentially ‘low-hanging fruit’ in political communications. It has various layers of meaning, however.
‘Hard-working’ also relates to the issue of how hard nurses actually work. Whilst nurses work shifts, there is no sense that any professional nurse should wish to leave punctually at the end of the shift, if there is a patient with unmet needs (and who hasn’t been safely ‘handed over’ to nurse colleagues). In previous discussions about rewarding nurses, it has been mooted, for example, that ward managers should be incentivised to stay at the bedside rather than being forced to choose administrative roles if they want to progress their careers. However, it is generally the case that individuals do not enter the nursing profession to make ‘loadsamoney'; there are other income-generating routes which are far easier. That is why people who have had an easier life, through politics, aren’t fooling anyone by dressing up in a nurse’s outfit for a day and for some cameras.
Take for example the issue of ‘hard-working’ in the context of compassion delivered by nurses. It is hard to know what the link between ‘hard-working’ and ‘compassion’ might be, except nurses who are looking after busy wards with not enough time even to go to the toilet report genuine frustrations in having time to deliver ‘compassionate’ care.
The word “hard-working” generally connotes something else: the virtue of the dedicated employee, who is ever available, an asset to company and country, never shirking, never clock-watching. This is particularly case in relation to the work ethic of nurses. Nurses work in teams, and has a strong ethic of collaborative working. If however a nurse agrees on professional grounds that the working environment is unsafe, and needs to ‘speak out safely’ against this, this can be professionally difficult.
There is nonetheless a slight twang from the Right that “hard-working” is linked to the neoliberal conception of the entrepreneurial self. This self never stops working; writing blogs, professional networking, setting up innovative businesses. However, this belief falls down with the fundamental finding that many ‘hard-working’ nurses on the left-of-centre in politics also voluntarily do such activities. A related issue there is that the Right do not have a monopoly on entrepreneurialism or innovation.
The word “collaboration” implies working together for the greater good but actually encompasses far more. Several pre-conditions must be in place for collaboration to be successful. Collaboration must have shared objectives. The value system among the participants must be similar. Communication must be honest, respectful, and purposeful. Nurses are especially good at this aspect of their working hard.
Indeed, most people in the general public acknowledge that nurses are caring and hard working in the face of challenging conditions, research has shown. A poll by YouGov revealed that 76% of those asked think nurses do their best and care about their patients. However, 82% of the 1,968 people surveyed also said nurses should be given the chance to speak more freely, with only 14% believing that this is already the case.This finding implies that nurses have a strong sense of professional ethic for their patients, and not just ‘doing time’ to receive the salary.
Another desirable quality of ‘hard-working’ is the notion of thrift. This boils down to an old notion of second world war pluck. Given the perceived necessity for tightening our belts and knuckling down and applying the old elbow grease in order to dig. It will be ‘hard-working’ people who, in a ‘war-like’ spirit get ‘Blighty’ out of this mess. For this, the alleged ‘profiligate spending of Labour’, which turns out to be £860 billion recapitalising the banks and sufficient public spending to ensure the highest satisfaction ratings of the NHS ever, is the enemy. Austerity is the cause under which we can all unite together?
The NHS is now expected to deliver 65% of its planned efficiency savings by year end, officials have told MPs. However, hard-working nurses, working at demands which far outweigh safe resourcing levels, will be a recipe for a disaster, as Mid-Staffs showed. The Care Quality Commission has issued the hospitals with warning after carrying out inspections, and the Keogh mortality report (and the Francis reports) have given plenty of examples of how even hard-working, well-meaning nurses, can’t cope. Of course it can be demoralising for ‘hard-working nurses’ to come home after their shift to listen to a diatribe of abuse about hospital standardised mortality statistics once they come home from work.
Notably, the term “hard-working” brings with it a status in front of your bosses. You might believe yourself to be “hard-working”, but to really know for sure you’d have to be told it by a rich person. Wealthy health service managers will now be able to pocket salary increases of 4%, which could boost annual pay packets by over £6000. By contrast, it was revealed this week that a 1% rise for NHS staff in England had been scrapped. A manager on £100,000 could be in line for a £4000 salary boost, while an NHS director could get up to over £6000.
In one sense, it evokes a “dignity of labour”, related to a productivist ideology of a historical layer of skilled workers; “Protestant work ethic” or the “Presbyterian work ethic”. Osborne’s decision to visit factories and skilled manual workers in particular may suggest he was aiming to evoke this sense. The problem with this approach, putting enormous emphasis on ‘productivity’, is that it conceptualises healthcare in the same terms as the efficiency of making an iPad. Heavily based in the Frederick Winslow Taylor management school of efficiency and productivity, it tends to ignore the professional ethic of nurses, or the value that they bring in their professional work which is hard to measure.
The “hard-working” theme is thus a populist-right appeal which encodes a series of policies designed to profoundly transform British society. However, it turns out to be a sham when you consider how it gives the appearance of not including ‘hard-working nurses’.
The general secretary and chief executive of the Royal College of Nursing, Dr Peter Carter, said that Chancellor George Osborne said it was “affordable” to give NHS staff a 1% pay rise in this year’s spending review. Dr Carter added that the Government was “emotionally blackmailing hard-working staff”.
All a bit of a shambles. But quid novi?
NHS 247 – don’t mention the Staffing!
 According to a recent newspaper article, the latest workforce statistics obtained by Nursing Standard magazine from the Health and Social Care Information Centre reveal that there are 348,311 nurses, midwives, school nurses and health visitors working either full-time or part-time in England. That is 2,991 fewer full-time posts than when the coalition government came to power. United Lincolnshire Hospitals NHS Trust, Basildon and Thurrock University Hospitals NHS Foundation Trust and Burton Hospitals NHS Foundation Trust are “plugging gaps” by hiring nurses from abroad. Basildon and Thurrock is looking to recruit 200 nurses from the Philippines and Spain. The international campaigns launched by the trusts reflect a growing trend to search beyond the UK for staff.
According to a recent newspaper article, the latest workforce statistics obtained by Nursing Standard magazine from the Health and Social Care Information Centre reveal that there are 348,311 nurses, midwives, school nurses and health visitors working either full-time or part-time in England. That is 2,991 fewer full-time posts than when the coalition government came to power. United Lincolnshire Hospitals NHS Trust, Basildon and Thurrock University Hospitals NHS Foundation Trust and Burton Hospitals NHS Foundation Trust are “plugging gaps” by hiring nurses from abroad. Basildon and Thurrock is looking to recruit 200 nurses from the Philippines and Spain. The international campaigns launched by the trusts reflect a growing trend to search beyond the UK for staff.
According to reports from Whiston, management staff have defended their recruitment policy after it transpired that Whiston Hospital’s A&E was understaffed by around eight per cent. An investigation by the BBC found that 11 of the 131 positions at the hospital’s casualty department remained unfilled. It is believed the shortfall is regularly made up by employing bank and agency staff, in line with other reports from around the country. The revelations about staffing levels, made following a Freedom of Information Act request, have unsurprisingly prompted nursing leaders to criticise current staffing levels. Meanwhile, according to reports from Croydon, a staffing crisis at Croydon University Hospital A&E has left it with the second largest shortfall of permanent employees in the country. That ward has a third fewer permanent workers than its NHS trust believes it needs, with the biggest gap in the supply of nurses. Croydon Health Services NHS Trust employs 151 permanent A&E staff, a shortfall of 48. Only Barking, Havering and Redbridge University Hospitals NHS Trust had a bigger deficit of staff, according to official statistics obtained through Freedom of Information requests. The trust stressed holes were plugged with temporary and agency staff, although these typically cost more than full-time employees. It claimed employing temporary staff did not impact on standards of care, unsurprisingly.
Last week, the Royal College of Physicians published its “Future Hospital Commission” report (“Report”). Generalist and specialist care in the future hospital came under some scrutiny in this report, but not in a way which addresses where there can possibly be more Doctors ‘on the ground’. Generalist care includes acute medicine, internal medicine, enhanced care and intensive care. Specialist components of care will be delivered by a specialist team who may also contribute to generalist care. A critical question is, in the average DGH, which of the ‘specialists’ are going to chip in with the acute general medical take. Currently, it is not uncommon for respiratory, gastroenterology and endocrinology physician consultants to run the acute general medical take, but (generally) neurologists and cardiologists do not take part.
“Patients should receive a single initial assessment and ongoing care by a single team. In order to achieve this, care will be organised so that patients are reviewed by a senior doctor as soon as possible after arriving at hospital. Specialist medical teams will work together with emergency and acute medicine consultants to diagnosis patients swiftly, allow them to leave hospital if they do not need to be admitted, and plan the most appropriate care pathway if they do.”
The “24/7″ aspect of ‘Future Hospitals’ is emphasised in various places in the report, for example:
“Acutely ill medical patients in hospital should have the same access to medical care on the weekend as on a week day. Services should be organised so that clinical staff and diagnostic and support services are readily available on a 7-day basis. The level of care available in hospitals must reflect a patient’s severity of illness. In order to meet the increasingly complex needs of patients – including those who have dementia or are frail – there will be more beds with access to higher intensity care, including nursing numbers that match patient requirements. There will be a consultant presence on wards over 7 days, with ward care prioritised in doctors’ job plans. Where possible, patients will spend their time in hospital under the care of a single consultant-led team. Rotas for staff will be designed on a 7-day basis, and coordinated so that medical teams work together as a team from one day to the next.”
Against this is the backdrop of the Nicholson “efficiency savings”, as reported (for example) here in the Guardian:
“The prime minister, David Cameron, his health secretary, Andrew Lansley, and the NHS’s most senior figures have all stressed that the government’s drive to make £20bn of efficiency savings in England by 2015 should not prompt hospitals and primary care trusts to cut services provided to patients. Instead, they say, the money should be saved through reducing bureaucracy, ending waste, adopting innovative ways of working and restructuring services.
Yet the growing evidence from the NHS is that its frontline is being cut, and that NHS organisations are doing what they were told not to do – interpreting efficiency savings as budget and service cuts. While restricting treatments of limited clinical value – such as operations to remove unsightly skin – is uncontroversial, reducing patients’ access to drugs, district nurses, health visitors or forms of surgery they need to end their pain arouses huge concern.”
Shaun Lintern, in a typically excellent article in the Health Services Journal, threw some light on this in relation to the report by Professor Sir Bruce Keogh, in July 2013:
“The NHS has little idea whether staffing levels at English hospitals are safe, Keogh review panel members have admitted. The report by NHS England medical director Sir Bruce Keogh said data for eight of the 14 hospital trusts examined by the review suggested there was no problem with nursing levels on wards.But when the review teams carried out their inspections they found “frequent examples of inadequate numbers of nursing staff in some ward areas”. In his report Sir Bruce said: “The reported data did not provide a true picture of the numbers of staff actually working on the wards.” The review suggests high level data on workforce levels may present an unrealistic impression of staff available on hospital wards on any given shift. This could lead to NHS trusts drawing false assurances from workforce data while their wards go understaffed. At several of the trusts examined the review team found staff feeling unable to voice their concerns to senior managers.”
Julie Bailey and #CuretheNHS, as well as a number of prominent patient groups such as #PatientsFirstUK, as well as certain regulatory authorities such as the #CQC, have all emphasised the need for ‘safe staffing’ for the NHS to succeed. Prof Sir Brian Jarman has time-and-time-again emphasised the pivotal impact of safe staffing on the hospital standard mortality ratio, as for example in this seminal article from the BMJ in 1999, on page 1517:
“In model A higher hospital standardised mortalityratios were associated with higher percentages of emergency admissions, lower numbers of hospital doctors per hospital bed, and lower numbers of general practitioners per head of population. The numbers ofhospital doctors of different grades were also considered as explanatory variables, but total doctors per bed was found to be the best predictor.”
A symptom of a poorly staffed NHS (in certain autonomous units) would be the system completely falling apart from the strain of increased numbers during the Winter period. A ‘solution’ proposed by NHS England has been some of £2.4 billion surplus will be plugged into a ‘quick fix’ of the situation, and/or hospitals can employ temporary bank staff. This may in the short term attempt to mitigate against a dangerous situation. According to the GMC(UK)’s “Good medical practice” (at point 56):
“56. You must give priority to patients on the basis of their clinical need if these decisions are within your power. If inadequate resources, policies or systems prevent you from doing this, and patient safety, dignity or comfort may be seriously compromised, you must follow the guidance in paragraph 25b.”
Many senior consultants do not wish to speak out safely currently against poor resources. This is reflected in this tweet/comment by Dr Kim Holt:
 This further emphasises the need for (all) staff to speak out safely against dangerous clinical care (hence the critical importance of the “Nursing Times Speak Out Safely” campaign.) From the consultant physician front, with the ‘input’ from operations and flow managers, there are currenltly reports of insufficient doctors and nurses being able to see patients in A&E in a timely fashion. It seems that the response to this, while NHS managers have remained consistently immune from materially significant blame for poor clinical care, has been for medical consultants to shunt patients, including vulnerable frail patients, out of A&E into MAU (or even, at worst, medical outlier wards), without patients having ever been clerked. That would be therefore direct evidence of a ‘gaming’ managerial culture directly impacting on how NHS consultants on the ‘shop floor’ have to react in the face of cuts and pressures from clinical demand. Whilst it might be sexy for all politicians and the Royal College of Physicians of London to talk about 24/7, no government minister has gone public to say how they will literally achieve ‘more for less’. Where will the extra money come from? Presumably existing staff will have to do more work for the same pay, and still have to comply with the law governing working (i.e. the Working Time Regulations passporting the European Time Directive).
This further emphasises the need for (all) staff to speak out safely against dangerous clinical care (hence the critical importance of the “Nursing Times Speak Out Safely” campaign.) From the consultant physician front, with the ‘input’ from operations and flow managers, there are currenltly reports of insufficient doctors and nurses being able to see patients in A&E in a timely fashion. It seems that the response to this, while NHS managers have remained consistently immune from materially significant blame for poor clinical care, has been for medical consultants to shunt patients, including vulnerable frail patients, out of A&E into MAU (or even, at worst, medical outlier wards), without patients having ever been clerked. That would be therefore direct evidence of a ‘gaming’ managerial culture directly impacting on how NHS consultants on the ‘shop floor’ have to react in the face of cuts and pressures from clinical demand. Whilst it might be sexy for all politicians and the Royal College of Physicians of London to talk about 24/7, no government minister has gone public to say how they will literally achieve ‘more for less’. Where will the extra money come from? Presumably existing staff will have to do more work for the same pay, and still have to comply with the law governing working (i.e. the Working Time Regulations passporting the European Time Directive).
Whilst their Report is to be welcomed, the Royal College of Physicians have effectively delivered a ‘motherhood and apple pie’ document for Government. It sounds nice and does not even address issues relating to the home patch? One of them will be for the Council of the College to consider whether it wishes for ‘specialist’ Consultants to ‘chip in’ with the acute medical take 24/7. They have after all at some stage passed the Diploma of the Royal Colleges of Physicians (UK)?
Meanwhile, for all the methodological criticisms of Jarman’s work, it can only be assumed that he genuinely wishes to improve the quality of care of NHS hospitals in England, and that he sincerely wishes to prevent the staggering distress of those foci of poor care where evidenced previously in the NHS. His words, on @RoyLilley’s “NHSmanagers.network” blog, could not have been clearer.
To deny the need for safe nursing staffing levels is to defend the indefensible
 Later today, a review of patient safety in the NHS by an acclaimed US expert, Don Berwick, is expected to recommend minimum staffing levels for hospitals, a “zero harm culture“, regulation of health care assistants (HCAs), and a “legal duty of candour ” for NHS entities and/or staff within them to admit their mistakes. The Berwick review will be published around 11 am for journalists and ‘interested parties’, and 3.30 pm for everyone else, it is anticipated. A “zero harm culture” is a reasonable policy goal, but there has to be a safe number of pilots and cabin crew to make the plane fly safely, and you have to check there’s enough fuel in the tank.
Later today, a review of patient safety in the NHS by an acclaimed US expert, Don Berwick, is expected to recommend minimum staffing levels for hospitals, a “zero harm culture“, regulation of health care assistants (HCAs), and a “legal duty of candour ” for NHS entities and/or staff within them to admit their mistakes. The Berwick review will be published around 11 am for journalists and ‘interested parties’, and 3.30 pm for everyone else, it is anticipated. A “zero harm culture” is a reasonable policy goal, but there has to be a safe number of pilots and cabin crew to make the plane fly safely, and you have to check there’s enough fuel in the tank.
On the publication of the recent Francis report, David Cameron said:
“The Government has so far resisted calls to introduce mandatory staff ratios for hospitals in the wake of the Mid Staffordshire scandal arguing that it would not necessarily improve patient care and could lead to organisations seeking to achieve staffing levels only at the minimum level.”
One of the most horrific things I have watched in the last few months is the undignified spectacle of campaigners ‘at each other’s throats’, discussing the issue of patient safety. Forgetting for a moment the well known indecency of the Care Quality Commission having given clinical departments a ‘clean bill of health’ before a disaster happened, the way in which some campaigners have avoided the need for a safe nursing staff level has truly offended me. In part, this is due to the fact that some campaigners are blatantly political. However, this has been to conflate an objective discussion of patient safety with a need for party loyalty which has completely not discussed the need for safe nursing levels. Any senior nurse or Sister will tell you about the ‘How many registered experienced nurses do I have on duty for this shift?” test question before nurses start their 2 pm – 9 pm shift, for example. Cutting nursing numbers makes the atmosphere for the nurses who are left turn from providing quality care for which they have trained to do into a method of ‘firefighting’, with an attitude of ‘I hope nothing goes wrong on my watch.” It is all very well for management consultants from outside of the profession to bleat on about ‘compassion’, and indeed this is low hanging fruit given the almost ubiquitous desire for compassion from the caring services, and an under-resourced service will have its consequences. The usual criticism of this argument is ‘there’s no excuse for lack of compassion’, but indeed in a well resourced National Health Service, this should not even be an issue. But it is – particularly as NHS Trusts locally implement ‘McKinsey efficiency savings’. It is easy to demonstrate financial solvency in the balance sheet, but it is possibly easier for Trusts to hide substandard care in both mortality and morbidity, which is why there is such a need for accurate data without the horrific shroud-waving we have seen in recent weeks.
It can’t simply be a question of the “numbers”, “stupid”. It is methodologically tricky to make cross-comparisons between hospitals, especially across a number of different jurisdictions with varying emphasis on private healthcare provision. Differences may be caused not by the staffing level of nurses per se, but by other unmeasured factors associated with higher levels of staffing by registered nurses or other unmeasured characteristics of the hospitals’ nursing workforce, such as proven competence in that particular specialty. The level of staffing by nurses is an incomplete measure of the quality of nursing care in hospitals. Other factors, such as effective communication between nurses and physicians and a positive work environment, have been found to influence patients’ outcomes. For example, the quality of “hand over” in nurses from shift to shift may have a bearing on whether clinical issues are picked up upon, e.g. a particular patient is getting ‘sicker’ and requires more frequent clinical observations; or simply that a patient’s CT scan of the thorax has been postponed for a fourth day in a row?
Politicians generally are not clinicians putting aside for a moment the rather rare cases of Dr Dan Poulter or Lord David Owen, and so can, generally, only be blamed for things which fall under their jurisdiction (or things which do not fall under their jurisdiction, as Justice Silber explained to the Secretary of State last week.) The Government has been criticised for presiding over cuts to nursing posts at a time of increasing concern over patient safety in NHS hospitals. Nearly 5,000 nursing places have been cut since the Coalition took power in 2010, with 800 lost in April this year alone. While NHS England plan to recruit more than 4,100 new nurses next year – a 2 percent increase – the health sector’s own economic regulator, Monitor, said last month that the recruitment drive was a “short-term fix” and will be followed by a further 4 per cent cut to nursing posts over 2014-15 and 2015-16. It has been argued that each ward is different, with a different case mix and layout, and staffing levels should therefore be locally determined. It has also been argued that if authorities set a local staffing levels the “floor” will soon become the “ceiling” and it will not be long before all hospitals plummet towards the bargain basement. This is where who provides the healthcare service does become relevant, in contradistinction to the Tony Blair dictum, which I have previously discussed on this blog. A private healthcare provider, even a NHS Trust which is funded through the PFI initiative, is able to hide staffing employment data on the grounds that this information is “commercially sensitive”.
The Nursing Times “Speak out safely” campaign has also been at the forefront of calling for a culture where the concerns of staff are valued and taken seriously. Also, the “Safe Staffing Alliance“, which includes the Royal College of Nursing, Unison, the Patients’ Association and the directors of nursing at a number of English hospitals, has campaigned for national minimum staffing levels since its foundation last year. The “Safe Staffing Alliance” is made up of NHS directors of nursing, senior healthcare academics, leaders of professional organisations and the Patients Associatiobm and oints to the current variation in staffing levels. Recent research by King’s College London shows that in some NHS hospitals registered nurses will provide care to an average of five named patients during a shift, while in other hospitals nurses have up to 11 patients to care for. Research has found considerable variation between and within hospitals even when specialty and patient dependency are taken into account.
- Registered nurse staffing levels vary considerably in English hospitals. In some National Health Service (NHS) hospitals registered nurses will provide care to an average of five named patients during a shift, whilst in other hospitals nurses have up to 11 patients to care for. Whilst a degree of variation in staffing between units is expected and necessary because of differences in patient needs and the type of care provided, research has found considerable variation between and within hospitals even when speciality and patient dependency are controlled for.
- Some wards can be well-staffed while other wards are dangerously understaffed. When the numbers are added up across a hospital the overall staffing levels can appear to be adequate. Planning safe nurse staffing levels is a recognised problem in many countries, including the US, Belgium, China, Korea and the UK. Care Quality Commission reports consistently warn that quality and staffing vary considerably within NHS hospitals.
- Neglected care (or care not done because of time pressures) is correlated to low registered nurse staffing levels on a ward. There are more errors in care, failure to rescue increases, and care is more likely to be ‘left undone’ when there are fewer registered nurses on a ward.
- Understaffing has cost implications for hospitals. Emergency admissions are higher where there are fewer registered nurses and nurses are likely to suffer more injuries and stress, exacerbating staffing problems and costs.
- Some specialties – such as older people’s care – typically suffer lower staffing levels and more dilute skill-mix. 50% of the nursing workforce caring for older people is made up of care assistants who are not trained nurses.
From “Registered Nurse staffing levels and patient outcomes: Overview of research evidence” published by the NNRU, King’s College London February 2013.
Even Robert Francis QC revisited the explosive issue of staffing levels last week:
However, during a public appearance last week, Mr Francis said he had seen evidence from the Safe Staffing Alliance – a confederation of nursing and patient groups set up earlier this year – that had convinced him the issue should be revisited.
Mr Francis stated: “It’s evidence… [that] ought to be considered with regard to whether there is some sort of benchmark, which at least is a bit like a mortality rates – an alarm bell which should require at least questions to be asked about whether it is possible for a service to be safe.”
He stressed the level should not be viewed as “the adequate level of staffing, but the level below which you cannot be safe”.
The ‘hospital standardised mortality ratio‘ as the warning trigger is for mortality, so clearly pretty distal in the chain of events, very blatantly. Francis has called for simple effective measures which are simple, meaningful, and for breaches against which can be sanctioned. His discussion of this issue of objective findings of poor staffing levels, in this context, is about 55 minutes in when you play this video:
Benchmarking can be a useful tool, but if used at an aggregated trust level it can mask underlying risks. Many directors of nursing have witnessed turnaround teams who suggest staffing can be reduced, on the basis of a comparative overall trust nurse-to-bed ratio. However, the recently published Keogh mortality report identified low nursing levels in many of the trusts they investigated (see my previous blogpost). The tragedy is that minimum safe staffing levels were recommended six months ago by Robert Francis in the report on Mid Staffs. However, the Government is yet to introduce a national standard for nurse to patient ratios, despite constant warnings from medical professionals.
Another campaign has been set up to lobby government to introduce a mandatory minimum staffing ratio of four patients to each registered nurse. It is reported in Nursing Times that:
Members of the 4:1 Campaign said they were “acutely aware of the pressures experienced by staff everyday through understaffing and the negative consequences this has on direct patient care and experience”.
“We believe a mandatory minimum staffing ratio of 4:1 should be introduced by the government to ensure that patients are cared for safely and effectively,” they state in a letter to Nursing Times.
“Research articulating the link between high patient-nurse ratios and poor patient health outcomes is strong and the experience of 1:4 ratios from California and the Australian state of Victoria demonstrate the immense benefits to patients and hospital staff where mandatory staffing ratios have been implemented.”
Further research in this jurisdiction is needed to refine the measurement of the nursing case mix on the basis of discharge data, and to elucidate the factors influencing the staffing levels of nurses and the mix of nursing personnel in hospitals. Given the evidence that such staffing levels are associated with adverse outcomes, as well as the current and projected shortages of hospital-based registered nurses, systems could be developed for the routine monitoring of hospital outcomes that are sensitive to levels of staffing by nurses. Beyond monitoring, hospital administrators, accrediting agencies, insurers, and regulators should take action to ensure that an adequate nursing staff is available to protect patients and to improve the quality of care. The professional regulatory bodies, such as the General Medical Council and the Nursing Midwifery Council, have not found themselves deliberating on wider matters of insufficient resource allocation, unless they happened to be effected by clinicians holding professional registration. Other clinical regulatory bodies might be more effective in regulating this particular domain, which clearly impacts upon the ‘quality’ of clinical care.
 Since earlier this year, UNISON, the UK’s largest health union, has been challenging the government over its refusal to implement what is potentially an important recommendation in the Francis Report – the introduction of minimum staff to patient ratios. Most professionals believe that this simple intervention would provide safer, more caring environment for all. That call had been backed by a new survey from the union of more than 1,500 nurses, midwives and healthcare assistants, which shows that 45% of respondents are looking after eight or more patients on their shift. Research shows that looking after this number increases the risk of patient harm. While in political circles, we have heard a lot from the hedge funds and private equity funds about liberalising the economic activity in the NHS, it would be timely to take careful note of the frontline staff regarding what they will help them to deliver safe and compassionate care.
Since earlier this year, UNISON, the UK’s largest health union, has been challenging the government over its refusal to implement what is potentially an important recommendation in the Francis Report – the introduction of minimum staff to patient ratios. Most professionals believe that this simple intervention would provide safer, more caring environment for all. That call had been backed by a new survey from the union of more than 1,500 nurses, midwives and healthcare assistants, which shows that 45% of respondents are looking after eight or more patients on their shift. Research shows that looking after this number increases the risk of patient harm. While in political circles, we have heard a lot from the hedge funds and private equity funds about liberalising the economic activity in the NHS, it would be timely to take careful note of the frontline staff regarding what they will help them to deliver safe and compassionate care.
Remember them?
Safe staffing, Keogh and the Nursing Times “Speak out safely” campaign
Despite clear differences in opinion about what has happened in the past, patient groups, Andy Burnham, Jeremy Hunt, the Unions, bloggers, experts, other patients, whistleblowers, and relatives at face value appear to want the same thing: a safe NHS where you do not go into hospital as a risky event in itself. The issue of safe staffing in nursing has become the totemic pervasive core issue of secondary care safety, and no amount of parliamentary time one suspects will ever do proper justice to it. In reply to a question from Valerie Vaz, who is herself on the Health Select Committee, Jeremy Hunt immediately quoted the Nursing Times and the Francis Report (from Tuesday 16 July 2013):
The aim of the Nursing Times’ Speak Out Safely (SOS) campaign is to help bring about an NHS that is not only honest and transparent but also actively encourages staff to raise the alarm and protects them when they do so.
They want:
- The government to introduce a statutory duty of candour compelling health professionals and managers to be open about care failings
- Trusts to add specific protection for staff raising concerns to their whistleblowing policies
- The government to undertake a wholesale review of the Public Interest Disclosure Act, to ensure whistleblowers are fully protected.
A very impressive gamut of organisations have supported the “Nursing Times Speak Out Safely” campaign, including Cure the NHS, the Florence Nightingale Foundation, the Foundation of Nursing Studies, Mencap Whistleblowing Hotline, Patients First, Public Concern at Work, Queen’s Nursing Institute, Royal College of Nursing, Unite (including the Community Practitioners and Health Visitors Association and Mental Health Nurses Association), and WeNurses. Also, for example, according to the Royal College of Midwives, maternity staff must be able to publicly raise concerns about the safety of mother and babies without fear of reprisal from their employers, according to the Royal College of Midwives. This college has been the latest organisation to support the Speak Out Safely campaign. They are calling for the creation of an open and transparent NHS, where staff can raise concerns knowing they will be handled appropriately and without fear of bullying.
The pledge of the Speak Out Safely campaign of Nottingham University Hospitals NHS Trust is a pretty typical example of the way in which this campaign has successfully reached out to all people who have the focused aspiration of patient safety.
“This trust supports the Nursing Times Speak Out Safely campaign. This means we encourage any staff member who has a genuine patient safety concern to raise this within the organisation at the earliest opportunity.
Patient safety is our prime concern and our staff are often best placed to identify where care may be falling below the standard our patients deserve. In order to ensure our high standards continue to be met, we want every member of our staff to feel able to raise concerns with their line manager, or another member of the management team. We want everyone in the organisation to feel able to highlight wrongdoing or poor practice when they see it and confident that their concerns will be addressed in a constructive way.
We promise that where staff identify a genuine patient safety concern, we shall not treat them with prejudice and they will not suffer any detriment to their career. Instead, we will support them, fully investigate and, if appropriate, act on their concern. We will also give them feedback about how we have responded to the issue they have raised, as soon as possible.
It is not disloyal to colleagues to raise concerns; it is a duty to our patients. Misconduct or malpractice should never be tolerated, while mistakes and poor practice may reveal a colleague needs more training or support, or that we need to change systems or processes. Your concerns will be dealt with in an open and supportive manner because we rely on you to ensure we deliver a safe service and ensure patient safety is not put at risk. We also want this organisation to have the confidence to admit to mistakes and to use them as learning opportunities.
Whether you are a permanent employee, an agency or temporary staff member, or a volunteer, please speak up when you feel something is wrong. We want you to be able to Speak Out Safely.”
The Keogh report is in its entirety is an apolitical report, and is very constructive. It identifies problems which Keogh’s team (which currently consists of some brilliantly talented Clinical Fellows) have a realistic chance of tackling. Despite criticisms that Hunt has turned up the ‘political heat’ on this issue, there is a feeling that Labour and Andy Burnham MP should either ‘put up or shut up’. If you park aside the mudslinging over the 13,000 ‘needless deaths’ from irresponsible journalism from parts of the media, the current Department of Health has surely begrudgingly have to be given some credit for instigating appropriate responses such as the Keogh review, and a Chief Inspector of Hospitals. There has been a real effort to clear up the methodology of estimating mortality figures, and while methodology issues will persist, an approach which fully involves and acknowledges the views of patients, whatever their political affiliations, is the only way forward.
As an immediate response to the terms of reference to protect patients from harm, Keogh thrust high up the importance of instigating changes to staffing levels and deployment; and dealing with backlogs of complaints from patients. Keogh identified a basic deficiency in effective performance management in the 14 NHS Trusts under investigation, and these basic performance management techniques are now commonplace in successful corporates. These constitute understanding issues around the trust’s workforce and its strategy to deal with issues within the workforce (for instance staffing ratios, sickness rates, use of agency staff, appraisal rates and current vacancies) as well as listening to the views of staff; Keogh laid down a number of “ambitions”. In ambition 6, Keogh argued that nurse staffing levels and skill mix should appropriately reflect the caseload and the severity of illness of the patients they are caring for and be transparently reported by trust boards.
The review teams especially found a recurrent theme of inadequate numbers of nursing staff in a number of ward areas, particularly out of hours – at night and at the weekend. This was compounded by an over-reliance on unregistered staff and temporary staff, with restrictions often in place on the clinical tasks temporary staff could undertake. There were particular issues with poor staffing levels on night shifts and at weekends. There were also problems in some hospitals associated with extensive use of locum cover for doctors.This observation is interesting as at the end of day an over-reliance on agency staff in both private and public sector from a performance management perspective will guarantee the NHS not getting the best out of its staff, and will further impede hospital CEOs from meeting their ‘efficiency targets’. As set out in the “Compassion in Practice”, Directors of Nursing in NHS organisations should use evidence-based tools to determine appropriate staffing levels for all clinical areas on a shift-by-shift basis. This means that a statutory minimum may be the inappropriate sledgehammer for an important nut. It is proposed that boards should sign off and publish evidence-based staffing levels at least every six months, providing assurance about the impact on quality of care and patient experience. The National Quality Board will shortly publish a ‘How to’ guide on getting staffing right for nursing. Whilst it is easy to argue against a national minimum number for nurses, as one can easily argue that it might encourage a race-to-the-bottom with managers gaming the system such that they only provide the minimum to run their Trust, most people, irrespective of the strong-held and important views of professionals within the nursing profession, believe that running a service with too few nurses is simply too risk for the remaining nurses. At times of high demand, Trusts need to be adaptable and flexible enough to cope, as anyone who has been involved in acute care in national emergencies has been involved (“critical incidents”).
Staffing was a recurrent pathology in the 14 Trusts under investigation. In Basildon and Thurrock University Hospitals NHS Foundation Trust, it was argued that the Trust needs to review current staffing levels for nursing and medical staff. In Buckinghamshire NHS Trust, the panel had a concern over staffing levels of senior grades, in particular out of hours. In Colchester Hospital University NHS Foundation Trust, it was found that staffing in some high risk wards needs urgent review. For the Dudley Group NHS Foundation Trust, inadequate qualified nurse staffing levels were identified on some wards, including two large wards which needed to be reviewed in light of concerns raised by the panel. For North Lincolnshire and Goole NHS Foundation Trust, there were concerns over the staffing of key elements of acute care, including recruitment of staff and maintenance of adequate staffing levels and skill mix on the wards. In North Cumbria University Hospital NHS Trust, inadequate staffing levels was identified, as well as an over-reliance on locum cover in some areas of the Trust.
For East Lancashire NHS Trust, the review team considered that staffing levels were low for medical and nursing staff when compared to national standards. Registrar cover and medical staffing in the emergency department was considered poor (this is medical ‘code’ for an overreliance on juniors at Foundation level), and levels of midwifery staff were considered poor too. Certain clinical concerns raised by staff have not been addressed, including known high mortality at the weekends. Whilst some of these actions will take longer to address entirely, assurance in respect of patient flows in A&E and concerns over staffing in the midwifery unit had already been sought by the CQC. For Medway NHS Foundation Trust, a top priority was made of teviewing staffing and skill mix to ensure safe care and improve patient experience, emphasising yet again that there might be false security to be derived from just looking at the overall number. For Sherwood Forest Hospitals NHS Foundation Trust, significant concerns around staffing levels at both King’s Mill Hospital and Newark Hospital and around the nursing skill mix, with trained to untrained nurse ratios considered low, at 50:50 on the general wards. Finally, for United Lincolnshire Hospitals NHS Trust, inadequate staffing levels and poor workforce planning particularly out of hours were discovered; concern over the low level of registered nursing staff on shifts in some wards during the unnannounced visit out of hours was escalated to CQC. Further investigation is underway.
This is a matter for all the political parties to get to the bottom of urgently. Party affiliations and tribal politics threaten real substantial progress in this area for all those who work in this area. This is not the time for energised disputes about political leadership in organisations. This is most certainly a time for action. Both the Francis report into the failures of care at Mid Staffs, and The Keogh Review into high hospital mortality rates, highlight how important the right skills mix and sufficient numbers of staff are to providing top quality care. Having the right staff cover is increasingly important out of hours – at evenings and weekends. With all political parties urging a need to work ‘harder and smarter’, or generally under the rubric of working more ‘efficiently’, this is a harsh climate, due to shrinking budgets as the cost of healthcare rises, and because of demands for £20 billion of so-called efficiency savings. Of course, the public are not involved in a genuine public debate at the moment which does not depict the ageing population as a budgetary ‘burden’ on the society, instead pumping in a carefree way billions into the HS2 project with its unclear business case. Billions more have been wasted on a chaotic, unnecessary top down reorganisation of the NHS; the National Audit Office has latterly criticised for the Government for going ‘over-budget’ on these bureaucratic reforms. Frontline staff are obviously rightly angry that this is money that they feel this is money that could and should have gone towards actually caring for patients.
The tragedy is that it really feels as if the NHS has never known, or unlearnt at great speed, basic performance management. One can argue until the cows come home how in this managerial-heavy approach to the NHS such management is extremely poorly done in such a way the CIPD would feel ashamed at possibly. The NHS will deserve to have problems in recruiting the best managers for the NHS so long as the climate of performance management, perhaps affected by an obsession for targets, remains deeply unappealing. It is recognised that good performance management helps everyone in the organisation to know hat the organisation is trying to achieve, their role in helping the business achieve its goals, the skill and competencies they need to fulfil; their role, the standards of performance required, how they can develop their performance and contribute to development of the organisation, how they are doing, and when there are performance problems and what to do about them. The general consensus is that, if employees are engaged in their work they are more likely to be doing their best for the organisation. An engaged employee is someone who:
The actual reality is that currently spending pressures mean that many health workers, sadly, are losing their jobs. Financial pressures are building up in the NHS just as the demand for healthcare and its cost is rising – trusts are being asked to make unconscionable savings. Trusts such as Barts Healthcare are in severe trouble, and the contribution of the failed policy of PFI is a massive scandal in itself. This perfect storm will hit standards of patient care hard, and is the direct consequences of decisions made by various recent governments – not by hardworking NHS staff. The only thing which is set up to work in the Act, apart from outsourcing (section 75) and raising massively the private cap (section 164(1)(2A)) of the Health and Social Care Act 2012 is the legal precision of the various failure or insolvency regimes. In any other sector, this would fall under wrongful or fraudulent trading. Except, it’s the NHS. It does economic activity in a very special way. As the shift in economic and political power shifts from a state well-funded comprehensive healthcare system to a fragmented disorganised piecemeal private integrated system in the next few decades, patient safety must take priority even if not a top priority seemingly in business plans. Initiatives such as the Nursing Times ‘Speak out Safely’ campaign is one of those vital ‘checks and balances’ to ensure that the NHS is working with and for patients and not against them. This means the NHS valuing staff as a top priority, as social capital is the most important thing in any organisation.