Home » Other
Presentations by Shibley Rahman at the Alzheimer Europe conference 2014 on autonomy and dignity
This year’s Alzheimer Europe conference is on ‘Autonomy and dignity’ between 20-22 October 2014.
I think it is timely that this conference is taking place at this important stage of the development of English national policy.
The direction of travel is a fully integrated health and care system, where people are signposted to information quickly and can make appropriate decisions.
The person living with dementia must come first; but we are also moving to a situation where a number of different people, such as friends, family, unpaid caregivers, paid carers, social care practitioners or nurses, might help to influence a personal care plan.
Ideally, a person living with dementia will be given in the future good care and support, in accordance to his or her known wishes, from the point at which a correct diagnosis is made.
Autonomy is part of the medical construct for ethical behaviour; beneficence, justice and non-maleficence are critical too.
With the ideal of autonomy, it’s vital that no ‘coercion’ takes place for people with dementia who are able to make autonomous decisions.
There should never be an illusion of people living with dementia where they are able to make decisions, when those decisions are clearly made on their behalf.
Dignity is pivotal to all dementia policy in England, and the law must be robust in safeguarding vulnerable people too.
I am looking forward to presenting two posters on language and the perception of #G7 dementia.
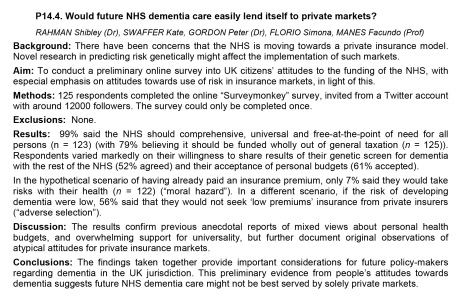
I am also privileged in that I have been chosen to present one of the few oral presentations. I am doing on this on the future of healthcare systems for dementia in England, arguing that policy aims, in particular universality and equity of access, will not be satisfied from a private insurance market.
I will be joined by my close friends Jayne Goodrick and Chris Roberts.
[photo by kind permission of Chris R]
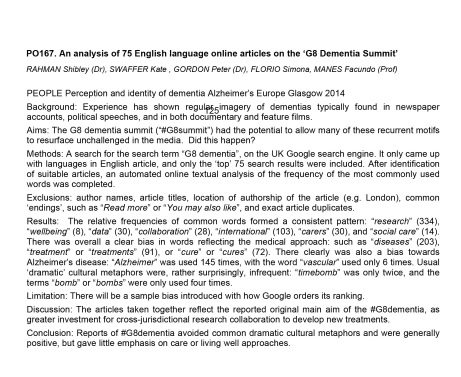
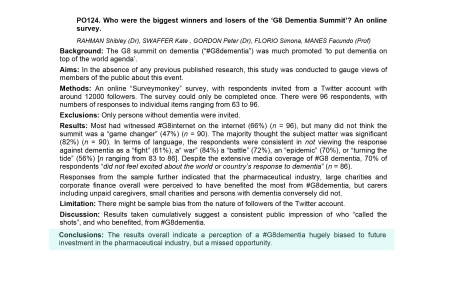
Please feel free to consider the research I’ll be presenting on behalf of myself, Kate Swaffer (living with a dementia and student at the University of Wollongong), Dr Peter Gordon (Consultant Psychiatrist), Simona Florio (Healthy Living Club, Stockwell), and Prof Facundo Manes (Chair of Behavioural Neurology, University of Favorolo, Buenos Aires; Co-Chair for research in dementia and aphasias for the World Federation of Neurology).
Private markets vs universality (oral presentation)
Language used in media presentation of the main #G7dementia event held in London
Perceived functions of #G7dementia
Trivialising dementia – too much inappropriate rocking of the boat?
When I wrote my highly successful book, “Living well with dementia”, using the phrase deliberately from the 2009 English dementia strategy document for England, I never knew the phrase was being bastardised so much for often very trivial initiatives in dementia.
On the other hand, I had huge delight in seeing its immediate relevance to a carers’ support group I went to last week.
I feel deeply hurt that the serious issues in my book, such as advocacy for mental capacity, the presentation of the cognitive neurology of the dementias, or the use of ambient-assisted technology have not been widely discussed amongst the wider community.
In that, I feel the book has failed.
I welcome proposals for the next Government to maximise money into actual service, and to re-establish health funding in line with other comparator countries.
Commissioning in dementia is now not based on what is best for the person for the person with dementia, but what is best for your Twitter commissioner friends.
I look forward to the Health and Wellbeing Boards playing a pivotal rôle in establishing some sort of normality for what commissioning in living well with dementia might be as a value-based outcome.
The strangehold of “shiny”, “off the shelf” “innovative packages”, in the drive for the current Government to ‘liberalise’ the financial market in dementia has acted for a cover for disturbing, unacceptable cuts in dementia service provision in the last few years.
I remember ‘boat rocking’ the first time around from the elegant work of Prof Debra Meyerson.
I do not wish to promote frontline professionals, many of whom have spent seven years at least at medical school or in their nursing training, to become lambs to the slaughter in the modern NHS and social care.
Keeping it real, we know that real frontline professionals in medicine and social care, even if they are not in a downright toxic environment requiring whistleblowing, can find it dangerous being risk appetitive.
Indeed, being risk appetitive, while great for innovation and leadership, can literally be deadly for patient safety.
The next Government has enough on its hands with enforcing care home standards and sanctioning for offences against the national minimum wage for paid carers as it is.
We have to think for a second for the vast army of paid workers in the NHS, as well as the rather well paid people who like their shiny new boxes, I feel.
The schism between the social media and what is happening at service level I think is most alarming, and perhaps symptomatic about how the health and social care services have begun to work in reality.
All too often, I am having first hand experience of busy frontline nurses being dragged in front of entrepreneurs in their local dementia economy to hear shills beginning, “I don’t have first hand experience of caring in dementia, but…”, before the hard sell.
This is tragically being reflected on the world stage too, though I do anticipate that the G7 legacy event from Japan which is looking carefully at their experience with care and support post diagnosis, next year, will be brilliant.
It is important for leaders in dementia to have authenticity.
I have severe doubts and misgivings about what gives the World Dementia Envoy the appropriate background and training in dementia for him to be in this important post.
It is all too easy for ‘thought leaders’ in corporate-like medical charities to have no formal qualifications or training in medicine, nursing, or social care, and opine nonetheless about weighty issues to do with policy.
I am concerned that the global ‘dementia friendly communities’ policy plank appears to have been straightjacketed through one charity in England, when it is patently obvious that various other charities such as the Joseph Rowntree Foundation have made a powerful contribution.
The media have largely not engaged in a discussion about living well with dementia, but engaged simply with Dementia Friends or a story arising out of that.
I am alarmed about the lack of plurality in the dementia research sector.
I think the All Party Parliamentary Group (“APPG”) for dementia have done some valuable work, but their lack of momentum on specialist nurses including Admiral nurses, spearheaded by the charity Dementia UK, seriously offends me.
I am sick of how the notion of ‘involvement’ of people with dementia has been abused in service provision mostly, although I am encouraged very much by initiatives such as from DEEP and Innovations in Dementia.
I think there have been genuine improvements in engaging people with dementia in research, through a body of work faithfully peer-reviewed in the Dementia Journal looking at heavy issues such as the meaning of real consent.
I am now going to draw the line of tokenistic involvement of people with dementia to front projects without any meaningful inclusion.
And in fairness, this tokenistic involvement is, I am aware, happening in various jurisdictions, not just England.
All too often, “co-production” has become code for ‘exploitation’ rather than ‘active partnership’.
The prevalence of dementia is actually falling in England, it is now thought.
The ‘dementia challenge’ was our challenge to making sure that we adequately safeguarded against people rent seeking from dementia since 2012.
In that, I think we have spectacularly failed.
I am overall very encouraged, however, with the success of the huge amount of work which has been done, including from the highly influential Alzheimer’s Society, and from the communitarian activism of “The Purple Angels”.
All this ‘radicalism’ has taken on a rather ugly, conformist twang.
Now is though time to ‘take stock’, as Baroness Sally Greengross, the current chair of the APPG on dementia, herself advised, as the new England dementia strategy is being drafted ahead of the completion of the current one in March 2015.
Is the use of GPS “trackers” for people living with dementia necessary and proportionate?
This is the introduction to “Living better with dementia: how champions can challenge the boundaries”, chapter 12, “Do GPS trackers have a rôle to play in living better with dementia?”
“We live in a ‘surveillance society’. If you happen to log in on Facebook, Facebook can identify your location exactly, and then can offer you a choice of cheap hotels there. The idea that a GPS system (“global positioning system”), as a tracker, can identify you where you are might seem like an invasion of privacy, but not much of an invasion of privacy than Facebook, arguably. And indeed a non-invasive system might be better than a method of physical restraint for certain people with dementia. It would be hard to justify a tracking device in a person who is not a candidate for physical restraint though conceivably?
Tracking for people with dementia raises strong emotions, not helped with some of the discussion acting at the extremes, such as a hypothermic person with dementia found in a ditch due to a GPS tracker. But the conflation of ‘tracking’, with ‘tagging’ as per frequent offenders in the criminal law, is an unfortunate one. At a time when there are international drives towards decreasing stigma in people with dementia, people warn about the mission creep that is offered with tracking: for example, one wonders how long it might be for a GPS tracker to become an implantable micro-chip. The word ‘tracking’ itself, however, is a misnomer, in that these trackers do not actively ‘follow’ people, but can pinpoint someone’s location through the method of ‘trilateral’. Satellite detectors happen to be there, in the same way that public telephone boxes happen to be there. Public telephone boxes take on a different atmosphere if highly illegal activity happen to be taking there, and there is a proportionate need to intervene. But intervene in what? Here we are talking about a criminal activity, rather than intervene in a person at risk of causing harm to himself or herself? The question that someone can consent to doing himself or herself avoiding being at personal harm, exercising too his or her own ethical right to autonomy, and a clear definition of consent depends on a clear definition of capacity. A human right to privacy which is inalienable albeit qualified may transcend capacity, causing further disquiet in legal circles. And, besides, people who do happen to travel beyond their physical zone might not be doing so out of any particular malice: a person with dementia may simply have problems with spatial navigation. Presumption of innocence is pivotal in the law is pivotal, and laying blame on innocent people is unacceptable – even subtlely through terms laced with innuendo such as “wandering”.
One wonders whether the legal definition of capacity across a number of jurisdictions, which depends on an “all-or-nothing” construct, can cope with those dementias where cognitive abilities fluctuate or cognitive demands vary. Is legal capacity to make a sandwich the same as capacity to write a paper on human rights? And who is best to make a decision about fitting a GPS tracker? It must surely cause concern if a caregiver would wish to fit one simply because it makes the monitoring of an individual an easier job, rather than the person with dementia wishes to be more independent. It is therefore clear that there is no right answer to GPS systems in dementia, especially as the term “dementia” itself is a portmantaneau term for lots of different clinical conditions, with different types and ‘severities’. Whether GPS trackers are necessary and proportionate for any one person living with dementia is a rather abstract question, given that there are so many different subtypes of dementia making some more prone to travel beyond their locality than others. With GPS tracking in dementia, we see yet another example where ‘one glove fits all’ approach is a dismal failure.”
No pledge is too small. Please sign up for my @DementiaFriends session on Aug 14 in Central London.
The aim of ‘Dementia Friends’ is to sign up people who wish to learn about dementia.
There are probably close to one million people living with dementia in the UK. There are probably also somewhere in the region of a hundred different causes of ‘dementia’.
These diseases of the brain cause problems in thinking – not necessarily memory, could be language, planning, complex visual perception, attention, decision making, distorted ideas.
Sadly, there’s a lot of misinformation about dementia.
This initiative from the Alzheimer’s Society, supported by Public Health England, is a remarkable initiative from the current Government to educate the general public on dementia. With greater education, it is hoped, barriers in society which lead to stigma and discrimination might be broken down.
Stigma is particularly significant, as stigma can lead to social isolation.
I will be giving an information session at BPP Law School on 14 August 2014, at 3.45 pm. On the day, you’ll need to ask the main Reception which room we’re in.
Whilst I am an academic in dementia, the session will be very basic. The aim is to explain in a completely unthreatening way some basic facts about dementia.
Because of the security of the law school in Central London, you’ll need to sign up in advance.
You’ll have to register on the @DementiaFriends website [here], but once you’ve done so you can register for the event here.
The people who attend are normally well informed, friendly and enthusiastic. You’ll be invited to have a badge should you wish to become a ‘Dementia Friend’.
More importantly, you’ll be asked to think of a commitment and action, and no pledge is too small.
It might be for example to ask your local paper to avoid using the term ‘dementia sufferers’, as this term might exacerbate stigma.
An example is here.
No one person has taught me more about living well with dementia than Kate Swaffer
When I posted this on my Facebook yesterday
it was on the back of a joke that Chris Roberts and Kate Swaffer, both friends of mine, had GPS trackers on me.
I intend to tackle the potential beneficial use of GPS trackers for some people living with dementia at significant risk of travelling way beyond their local environment.
And travelling beyond my comfort zone is exactly what happened to me at the end of last week.
I ended up at the Alzheimer’s Show in Manchester, to give a 20 minute skit on my book ‘Living well with dementia‘.
Tommy Dunne and Chris Roberts, bosom buddies, sat together in a little section of the workshop. I could spot they were listening to every word.
Jayne Goodrick asked me a gentle question – unlike the question I asked from Prof Stuart Pickering Brown the day previously,
“I’d like to ask Prof Pickering Brown, but this question applies to the rest of the panel too, how the millions spent on Big Data and identifying genetic factors for Alzheimer’s disease and frontotemporal dementia, like TREM2, can be rationalised in the context of a social care system on its knees, with zero hour contracts and breaches of the national minimum wage?”
I had of course pre-warned the panel that the question would be incomprehensible, as I am disabled.
Jayne said the question was ‘coded’, but Prof Pickering Brown likewise answered in code.
And he took the question well – I had a chance to thank him for all the work he does on frontotemporal dementia, and he asked me to pass on his personal regards to Prof John Hodges.
John is one of THE leading experts in frontotemporal dementia, well respected around the world in academia.
More importantly, he is looking forward to my new book, “Living better with dementia: how champions can challenge the boundaries”.
Chris especially feels, and Tommy agrees, that a much more suitable title would be ‘Living better with dementia.”
Now that Chris has explained it, I completely agree. “Living well with dementia” implies imposition of your judgment as to what living well is.
And whatever your objective level of living might be, nobody can deny a need to live better.
It took me some time to get it, but I did in the end.
A bit like how the penny dropped with Tommy’s joke about urinating with the door open.
But I loved ‘The Alzheimer’s Show’ as it felt truly as if I was amongst friends – and I met people whom I have only met on Twitter, who were truly lovely : Suzy Webster, Natasha Wilson, Chris Roberts, Jayne Goodrick, Tommy Dunne.
And I met some wonderful friends from before: Louise Langham, Carers’ Coordinator for CC2A, and Rachel Niblock.
And I met some brilliant people who’d been following me on Twitter, such as Tracey from CareWatch.
I phoned Nigel Ward, the Show Director, and he was brilliant as usual: “Why did you phone me Shibley? There’s no signal in here, and I was only in the next-door cubicle?”
Anyway, I’ve been on and off in the dementia field for seventeen years, which has taken me on various ups and downs, including three months on the dementia and cognitive disorders firm under Prof Martin Rossor as a junior doctor at the National Hospital for Neurology and Neurosurgery, Queen Square.
It’s also seen me go via a 2 year 10 months PhD at the University of Cambridge. I was the first person in the world to demonstrate reliably risky decision-making behaviour in persons with the behavioural variant frontotemporal dementia. It’s a finding which has been resilient for the last fifteen years, having been replicated and explained through neuroimaging.
I am not really into ‘co-production’, mainly having seen it being used as a cover for legitimising some people’s pre-formed agendas.
But I have been heavily influenced by Kate Swaffer who received a diagnosis of dementia some years ago.
The contents of my new book, to be submitted by the end of October 2014, reflect mutual interests of ours. Kate is more than a cook, former nurse, brilliant blogger, and advocate for Alzheimer’s Australia.
I am honoured she is a close friend of mine. She is not motivated by any narcissistic twang.
She is brilliant.
She has taught me more about dementia than anyone I know.
And it’s her birthday today.
#KoalaHugs
Accusing someone living well with dementia of not having a dementia reveals very serious policy flaws
For all the money that has been pumped into ‘dementia awareness’ internationally, one would have hoped that deeply entrenched attitudes were at last shifting.
The drive for ‘a cure for dementia’ has only added a dangerous level of confusion. Cure for what type of dementia? Do they mean a cure for Alzheimer’s disease, the most common type of dementia worldwide?
In what sort of form will this cure reveal itself? A vaccine preventing people from developing dementia, like a vaccine for cervical cancer? Or an oral tablet which ‘stops dementia in its tracks’?
Soundbites are cheap, but it is not an innocent issue at all. Resources are being diverted away from frontline care, such as specialist nursing, into public-private partnerships designed to reap a shareholder dividend for Pharma developing “innovative drug treatments”, or into dementia information sessions.
It is a bit rich complaining of the dire state of post-diagnostic support ; when millions have been actively pumped into ‘information sessions’. Ideally, you should have wanted a world where both were successfully achieved?
It’s too late for a post mortem on that. There will be a change of government soon.
But I continue to be struck by the steady stream of people in authority, involved somehow in dementia care like care homes or on social media groups, who ‘accuse’ people living well with dementia of not having received a diagnosis of dementia?
If you could prove that beyond reasonable doubt of a false representation, designed to generate money or expose someone to a loss, that would constitute a fraud offence under our Fraud Act (2006) in our jurisdiction.
However well meant such an accusation might be, it can of course be extremely unsettling for the recipient of the accusation. At worst, it could come out as a statement designed to cause offence or menacing, which is a public order offence if done in public.
The issue does reveal itself to me as representative of an underlying fault line in national policy, which was intended to facilitate people talking openly about the dementias to mitigate against stigma and discrimination.
That it might not be obvious that someone is living with a chronic progressive condition of the brain is a really significant faulting in awareness policy for me. I remember being ‘guilty’ of thinking ‘he doesn’t look disabled’ after waiting for ages in the queue for disabled toilet cubicles on trains. Of course, some disabilities unlike mine are invisible: somebody with multiple sclerosis might be living perfectly well with an indwelling catheter.
Likewise, for example, a person living with behavioural variant frontotemporal dementia might have virtually no obvious cognitive deficits in memory, planning or perception, but might have found to have a profound change in behaviour and personality as reported by a friend or member of a family.
How will a member of the public identify a person living well with dementia? If it is ‘invisible’, how then do “dementia friendly communities” work?
I do not subscribe to the approach ‘if you see a doddering old lady at a zebra crossing, think you might help them as a ‘Dementia Friend” as this plugs into ageist stereotypes about what dementias are. One of the critical messages of ‘Dementia Friends’ is that “dementia is not a natural part of ageing“.
The media, and indeed ‘policy leaders’, have also contributed to this unseemly mess of memory problems being synonymous with dementia. If cognitive deficits are not substantial enough to be given a diagnosis of dementia, a ‘mild cognitive impairment’ might be diagnosed. It could be that people accusing people living with dementia not having received a diagnosis of dementia mean that “you can’t have a dementia – maybe you have a mild cognitive impairment?” But even this is problematic, as it has not been made sufficiently clear that there is insufficient evidence that mild cognitive impairment represents a ‘pre dementia’ form, and this analogy with other conditions such as diabetes and renal failure actually falls flat.
It is basically an unholy mess. You can see how if GPs refer lots of ‘possible diagnoses of cancer’, the system will be unable to cope with pressing cases of cancer for management. It’s quite unclear how the ‘possible diagnoses of dementia’ are being followed up by specialist services, confirming the diagnosis, or not, over a period of time. You need this progression confidently to make a diagnosis of dementia, further making the urgent drive – this second – of upping the dementia diagnosis rates, however well intentioned – in reality absurd.
Have things actually improved in the last few years?
In my opinion – no.
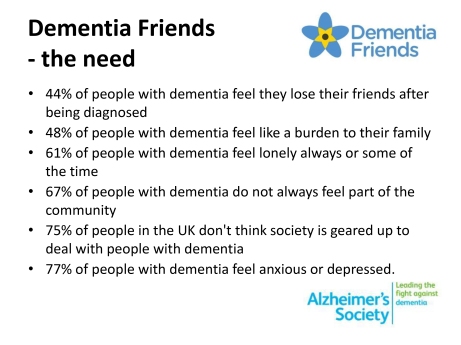
44% of people with dementia feel they lose friends after being diagnosed
Dementia 2012, the first in a series of annual reports from the Alzheimer’s Society, described how well people are living with dementia in 2012 in England, Wales and Northern Ireland.
According to page v of the ‘Executive Summary’. the sample comprised a YouGov poll in December 2011 involving 2070 individuals, but also “drew on existing research and current work”, and polling done by the Society with people in the early stages of dementia in a survey distributed through the Society’s support workers in England, Wales and Northern Ireland. A number for this last group is not stipulated. It is unclear how large the cumulative sample is for each of the key findings, therefore.
This work helps to provide a slide of the key findings underpinning the need for ‘Dementia Friends’, an Alzheimer’s Society and Public Health initiative. For example, one such slide from a presentation available on the internet is:
In detail the findings reported are as follows.
The survey shows that respondents reported losing friends after their diagnosis or being unable to tell them. Nearly half (44%) of respondents said they had either lost most of their friends, some of their friends, or hadn’t been able to tell them.
When asked if they lost friends after their diagnosis of dementia 12% of respondents said yes, most of them, 28% said yes, some of them, and 47% said no.
4% of respondents reported that they haven’t told their friends and 5% didn’t know.
Should we surprised if “44% of people with dementia feel they lose their friends after being diagnosed?”
I remember when I became disabled and went into recovery from severe alcohol dependence syndrome at the same time. Employment was far from my mind. At the time, my friends circle did severely contract, but I should like to think that the friends I am left with are not superficial friends. They are people I suspect would’ve stuck with me through thick and thin anyway.
They are not ‘judgmental’.
Receiving a diagnosis of dementia is not like receiving a criminal conviction. Norman McNamara once joked with me saying he had not been ‘convicted of dementia’ in explaining why he preferred the term ‘GPS trackers’ to ‘GPS tagging’, as a mitigation against wandering.
When I was at the first Alzheimer’s Show in London earlier this year, I met the wife of someone who had received a diagnosis if dementia, and they had not told their friends of their diagnosis for about years.
I suppose that if you have mild memory symptoms as a feature of Alzheimer’s disease, you might not need to tell people that you have a diagnosis, in the same way that you might have an indwelling catheter for multiple sclerosis.
The memory loss may not be immediately obvious.
But this is part of my overall criticism of ‘dementia friendly communities’ – to be ‘friendly’ to people living with dementia, howsoever that is defined, you need to identify such individuals reasonably reliably. I do not buy into this ‘if you see an old biddy have a difficulty, think they might dementia'; particularly since dementia is not confined to older people.
The statistic “44% of people with dementia feel they lose their friends after being diagnosed” becomes even more complicated once you consider various factors which impact upon this finding potentially.
How deep was the friendship in the first place?
And of course what type of dementia? Frontal dementia (behavioural variant frontotemporal dementia) is reasonably common in the younger age group epitomised by progressive behavioural and personality changes.
The thing about this condition, however, is that the person with dementia very often has little or no insight into his change in personality (with the presentation having been noticed by a close friend, or even husband/wife).
Also another feature of conditions affecting the frontal lobes (the part of the brain near the very front of the head) is that such people with problems with the frontal lobe can be extremely bad at making ‘cognitive estimates’.
This was first shown by Prof Tim Shallice and colleagues in the late 1970s: e.g. “how many lamp posts are there on the M1?” “Forty.”
And in the presentation of behavioural variant frontotemporal dementia, it could be obvious to friends that something might be happening as your personality was changing. Therefore, in this scenario, it might be reasonably foreseeable that friends drift away.
Why should people who were friends no longer be bothered? One reason is that ‘they don’t want the hassle’. Maybe staying friends might at later stage involve some sort of requested financial support? Or maybe the former friends don’t want to be involved in ‘uncomfortable discussions’ about dementia?
This is indeed where an initiative to recruit one million ‘Dementia Friends’ through information sessions are useful to dispel the myths and prejudice, as mitigation against stigma and discrimination?
But one of the outcomes which ‘Dementia Friends’ will have to evaluate is whether this project encourages people to ‘befriend’ people with dementia. It is not a mandatory outcome, although people are encouraged to think of this as one of the possible commitments/actions from the information session.
In Japan, befriending has been a successful policy, but the entire care system is much more convincing than our one which has been starved of funds in parallel with Dementia Friends receiving its funding from the Department of Health and Social Care Fund.
But, anyway, would one necessarily expect the friends that one has lost through disclosing a diagnosis of dementia to be matched by friends obtained through ‘Dementia Friends’ in terms of quality? It is of course impossible to answer this question.
This topic is of course closely entwined with the subject of the 2013 report on loneliness. Encouraging participation in wider networks including social networks such as Facebook and Twitter can in the real world help to overcome this.
But with leading politicians continuing to use words such as “horrific”, “evil”, “devastating” in relation to dementia, is it any wonder that, whatever other initiatives, people who have received a diagnosis of dementia are resistant to tell their friends because of the potential reaction?
The statistic “44% of people with dementia feel they lose their friends after being diagnosed” sounds like a typical fundraising slogan, and indeed can be used to justify a national project such as ‘Dementia Friends’.
The proof of the pudding comes in the eating. Will a significantly fewer number feel that they lose friends after being diagnosed (whether they actually lose friends) as a result of “Dementia Friends”? Whilst, as I have explored elsewhere, there is a lot to commend ‘Dementia Friends’, I think it would be wrong to raise this expectation.
And if a significantly fewer number do not feel that they lose friends after being diagnosed, despite “Dementia Friends”, it would be interesting to explore further why. For example, it could be that there are fewer home visits by health professionals, although it is normally argued that ‘anyone who needs a home visit gets one’.
The statistic though acts a useful cover for a quite sinister discussion.
A large scale cultural national transformation is needed to drive whole person care in dementia
I’ll be blunt. It’s my dream for the #NHS to run a proactive not reactive service, promoting the whole person living well with dementia.
The Australian jurisdiction have recently provided some helpful inroads here.
The narrative has changed from one of incessantly referring to people living with dementia as a ‘burden’ on the rest of society. For example, to push a sense of urgency that we have an ‘ageing population timebomb’, the cost of the ageing people with dementia flies completely in the face of other public health campaigns which emphasise, for example, “dementia is not a natural part of ageing”.
“The NHS as a whole and individual hospitals recognise that dementia is a significant, growing and costly problem for them” is the opening gambit of the Alzheimer’s Society “Counting the cost” report.
An easy to use online resource, Valuing People from Alzheimer’s Australia has been developed in collaboration with community aged care providers who have helpful in stablishing a person centred approach to service delivery.
Person centred care is a development to provide ervices provided in a way that is respectful of, and responsive to, the preferences, needs and values of people and those in the care and support network.
I cannot recommend this resource highly enough. The main source is here.
In fact, it summarises succinctly the conclusions I came to after my exploration of personhood in my book ‘Living well with dementia’. The late great Prof Tom Kitwood said of personhood, “It is a standing or status that is bestowed upon one human being, by others, in the context of relationship and social being. It implies recognition, respect and trust”.
If a Labour government is elected on May 8th 2015, the first necessary step is to legislate for the repeal of the Health and Social Care Act (2012) and to enact new legislation to allow for integrated packages provided they are justified by clinical outcome. For this to happen, it will be necessary for Labour to undergo a ‘conscious uncoupling’ from all the baggage of EU competition law. For this, it is essential also that the UK government is able to carve out provisions from the investor protection clauses and/or the rest of the EU-US free trade treaty (TTIP).
The “whole person care model” has become attractive to those who wish to break down silos between different physical health, mental health and social care “silos”. It has been worked up in various guises by various parties.
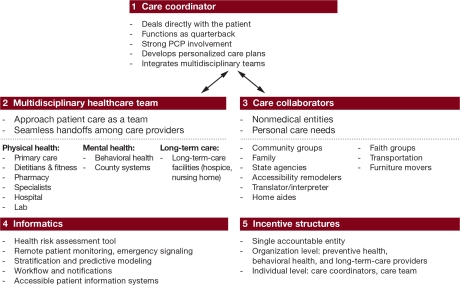
A helpful construct is provided in the document, “Healthcare for complex populations: the power of whole-person care models” originally published by Booz & Company in 2013.
A major problem with dementia care, however it is delivered, is that it is full of divisions: public vs private care, fragmented vs national care, competitive vs integrated models. Operating in silos can’t work because of the nature of the dementias: the mood and cognition of a person with dementia profoundly affects how they might interact with the outside world, for example perform activities in the outside world. And we know that taking part in leisure activities can promote a good quality of life.
Their model is, though, a useful starting point.
Dementia cannot be only addressed by the medical model. In fact, it is my sincere belief that it would be highly dangerous to put all your eggs in the physical health basket, without due attention to mental health or social care. For example, last week in Stockholm, the international conference on Parkinson’s disease, a condition typified by a resting tremor, rigidity and slowness of movement, which can progress to a dementia, often is found to have as heralding symptoms changes in cognition and mood.
So it’s pretty clear to me that we will have to embark on a system of multidisciplinary professionals who could all have a part to play in the wellbeing of a person with dementia, depending on his or her own stage in life, and ability or need to live independently. “Care coordinators” have traditionally been defined incredibly badly, but we do need such an identity to navigate people with dementia, and actors in the care and support network, through the maze.
“Care collaborators” in their construct are very wonkily articulated, like “pre-distribution”, but the concept is not stupid. In fact it is very good. One idea is that people with dementia could act as support as other people with dementia, for people on receiving a diagnosis of dementia. The rationale for this is that people living with long term conditions, such as for example recovery from alcoholism, often draw much support from other people living with other long term conditions, away from a medical model. There needs to be safeguards in the system to safeguard against a lot of unpaid goodwill (which currently exists in the system.)
Informatics would have a really helpful rôle here, being worked up in telecare and assistive technology. But even simple disruptions such as a person living with dementia at risk of falling from problems with spatial depth perception being able to ‘hot email’ a care coordinator about perceived problems could trigger, say, an early warning system. And with various agents in the provision of care being involved in differing extents it will be up to NHS England to work out how best to implement a single accountable tariff. Falls are just the sort of ‘outcome metric’ which could be used to determine whether this policy of ‘whole person care’ for people living with dementia is working. And, even though everyone ‘trots it out’, the performance on avoided hospital admissions could be put into the mixer. It’s already well recognised that people with dementia can become very disoriented in hospital, and, and despite the best efforts of those trying to improve the acute care pathway, people with dementia can often be better off away from hospital in the community. But it’s imperative that care in the community is not a second-rate service compared to secondary care, and proper resourcing of community whole person care is essential for this before any reconfiguration in acute hospital services.
But the private sector has become such a ‘bogey term’ after arguably the current Government overplayed their hand with the £3bn Act of parliament which turbo-boosted a transfer of resource allocation from the public to private sector. Any incoming government will have to be particularly sensitive to this, as this is a risk in strategy for the NHS.
In October 2005, Harold Sirkin, Perry Keenan and Alan Jackson published a highly influential article in the Harvard Business Review entitled “The hard side of change management“. Whilst much play has in fact been made of politicians having to be distant from running the NHS, a completely lubricous line of attack when it is alleged that Jeremy Hunt talks regularly to senior managers and regulators in the NHS, the benefits of clear political leadership from an incoming Labour government are clear.
Andy Burnham MP has already nailed his colours to the mast of ‘whole person care’ on various occasions, and it is clear that the success of this ambitious large scale transformation depends on clear leadership and teamwork from bright managers. Take for example the DICE criteria from Sirkin, Keenan and Jackson:
But this is perfectly possible from an incoming Government. The National Health Service has a chance to lead on something truly innovative, learning from the experience of other jurisdictions such as Australia and the USA.
As alluded to in the new resource from the Alzheimer’s Australia, this cultural change will require substantial ‘unfreezing’ from the current mindset for provision of care for people with dementia. It will require a change in explicit and implicit sources of knowledge and behaviours, and will need to be carefully brought about by learning from the successes and failures of pockets of implementation.
The whole project’s pretty high risk, but the rewards for people living with dementia, and members of the care and support network, are potentially vast. But it does require the implementation of a very clear vision.
[First posted on the 'Living well with dementia' blog]