Home » Health and Social Care Act 2012
Can the English NHS enter a ‘period of calm’ if it wishes to introduce integrated care?
Sir David Nicholson, KCB, CBE, is Chief Executive of NHS England.
In 2010 Nicholson jokingly described NHS reform plans, the implementation of the Health and Social Care Act (2012), as the biggest change management programme in the world – the only one “so large that you can actually see it from space.”
Andy Burnham MP gave a speech to The King’s Fund on 24 January 2013, entitled “‘Whole-Person Care’ A One Nation approach to health and care for the 21st Century”.
And the Conservative Party, with Jeremy Hunt MP as Secretary of State for Health, have been eyeing up ‘integration‘ too.
So, like many areas of policy such as the private finance initiative, personal budgets or ‘efficiency savings’, there might be considerable consensus amongst the main political parties about implementing a further transformational change in the English NHS.
In that famous King’s Fund speech, Burnham comments, “Second, our fragile NHS has no capacity for further top-down reorganisation, having been ground down by the current round. I know that any changes must be delivered through the organisations and structures we inherit in 2015. ”
This is coupled with, “While we retain the organisations, we will repeal the Health and Social Care Act 2012 and the rules of the market.”
The Health and Social Care Act (2012) as a legislative instrument, whatever the political bluster, had three main legislative aims.
It aimed to implement competitive tendering in procurement as the default option, thus expediting transfer of resources from the public sector to the private sector; it beefed up the powers of the economic regulator (“Monitor”) for this “market”; and it produced a preliminary mechanism for the managed decline of financially unviable entities in the NHS.
Therefore repealing the Act can be argued as a necessary and proportionate move for taking out the ‘competition jet engines’ of the NHS “market”.
Experience from a number of jurisdictions provides that the legal challenges in allowing integration (and bundling) within the framework of competition law are formidable.
There is a clinical case for integrated care, in allowing more co-ordinated care of the person across various disciplines, for example medical, psychiatric or social, for both health and disease.
If community services are ‘wired up’ with hospital services, provided that community services are not starved of money at the same time as hospital services, there is a good rationale in that the health of certain people, followed closely in the community, might not freefall so badly that they require admission to a medical admissions unit.
There is also a financial argument that integrated or whole person care might work, but clearly no political party will wish to prioritise this ahead of quality of clinical care, particularly given the current tinderbox of cuts in medical and social care.
But whichever way you look at it, ‘whole person’ care involves a huge cultural change; this has repercussions for how all professions conduct themselves in their care, especially with regards to community care, and has consequences for training of staff in NHS England.
And it is impossible to think that, whichever political party ultimately becomes responsible for introducing a whole person or integrated care approach, it won’t cost money.
For example, setting up the infrastructure for data sharing, whether clinical or for the purposes of unified budgets, has a long history of being expensive.
Estimates of the cost of the reorganisation just gone are a bit confused, but they tend to range between £2.5 and £3 bn.
The risk of turbulence can be, to some extent, mitigated against by known people at the helm, such as Andy Burnham or Liz Kendall, but the last thing the general public will wish is another period of massive upheaval.
It can be argued that these changes are ‘a good idea’, and it’s only a question of explaining the benefits to the general public, but, following the Health and Social Care Act and caredata, the track record of this current Government is nothing to write home about.
Twitter: @legalaware
Are we actually promoting the NHS ‘choice and control’ with the current caredata arrangements?
In the latest ‘Political Party’ podcast by Matt Forde, an audience member suggests to Stella Creasy MP that wearing a burkha is oppressive and should not be condoned in progressive politics. Stella argued the case that she can see little more progressive than allowing a person to wear what he or she wants.
The motives for why people might wish to ‘opt out’ are varied, but dominant amongst them is a general rejection of commercial companies profiteering about medical data without strict consent. This is not a flippant argument, and even Prof Brian Jarman has indicated to me that he prefers a ‘opt in’ system:
Patients are not fully informed about how their information will be used. For such confidential data they should have to opt in @legalaware
— BrianJarman (@Jarmann) January 28, 2014
If people are properly told the pros and cons they can decide if they want to accept the cons, for the sake of the pros @sib313 @legalaware
— BrianJarman (@Jarmann) January 27, 2014
There are potential benefits, but also risks and if the risks happen they’re irreversible. Hence it’s safer to have opt-in. @legalaware
— BrianJarman (@Jarmann) January 27, 2014
Opting out can be argued as not being overtly political, though – it is protecting your medical confidentiality. People may (also) have political reasons for doing this, but the choice is fundamentally one about your right to a private family life. The government (SoS) has accepted this, and that is why it is your NHS Constitution-al right to opt out – you don’t have to justify it and if you instruct your GP to do it for you, she must.
It’s argued fairly reliably that section 251 of the NHS Act 2006 maps exactly onto Section 60 of the Health and Social Care Act 2001. Section 60 was implemented the following year under Statutory Instrument 2002/1438 The Health Service (Control of Patient Information) Regulations 2002. It is argued that the Health and Social Care Act 2012 did not modify or repeal those provisions of the HSC Act 2001 or the NHS Act 2006, nor did it modify or repeal any related provision of the Data Protection Act 1998. SI 2002/1438 remains in force. However, noteworthy incidents did occur under this prior legislation, see for example this:
Whatever motive you have for arguing against care.data, whether the whole principle of it, the HSCA removing any requirement for consent, the fact that it is identifiable data being uploaded from GP records (i.e. not anonymised or pseudonymised), or that the data will be made available, under section 251, for both research and non-research purposes, to organisations outside of the NHS, etc, the matter remains that the is no control over your data unless you opt-out.
Proponents of the ‘opt out’ therefore propose their two lines of action: either prevent your identifiable data being uploaded (9Nu0) and so effect a block on the release of linked anonymised or pseudonymised (potentially identifiable) data, which otherwise you cannot prevent or control; or block all section 251 releases (9Nu4), whether or not you apply the 9Nu0 code.
The point is, they argue, that you – the patient – cannot pick and choose, when, to whom, or for what purposes your data will be released. You cannot prohibit your data from being released for purposes other than research, or to organisations out with the NHS. This is completely at odds to the ‘choice and control’ agenda so massively advanced in the rest of the NHS. While it has been argued that the arguments against commercial exploitation of these data should have been made clearer beforehand, it’s possibly a case ‘I know we’re going there, but I wouldn’t start from here.’
Compelling arguments have been presented for the collection of population data. It’s argued wee need population data to do prevention and to monitor equity of access and use. It’s an open secret that the current Government is continuing along the track of privatising the NHS; arguably making it all the more important to have good data so we know what is happening. Having more of this data at all starting in the private sector, under this line of argument, is much less transparent, as it’s hidden from freedom of information from the start.
It’s, however, been argued that “the route to data access” has in fact changed. Under Health and Social Care Act (2012), it was intended that either the Secretary of State (SoS) or NHS England (NHSE) could direct HSCIC to make a new database, and – if directed by SoS or NHSE – HSCIC can require GPs (or other care service providers) to upload the data they hold. care.data represents the single largest grab of GP-held patient data in the history of the NHS; the creation of a centralised repository of patient data that has until now (except in specific circumstances, for specific purposes) been under the data controllership of the people with the most direct and continuous trusted relationship with patients. Their GP.
HSCIC is an Executive Non Departmental Public Body (ENDPB) set up under HSCA 2012 in April 2013. NHS England, the re-named NHS Commissioning Board, was established on 1 October 2012 as an executive non-departmental public body under HSCA 2012. Therefore, to suggest that the government has ‘little control’ over these arm’s-length bodies is being somewhat flimsy in argument – they were both established and mandated to implement government strategy and re-structure the NHS. There are also problems with the “greater good” argument; being paternalistic, the opposition to caredata spread bears similarity to the successful opposition to ID cards. This argument presumes that patients will benefit individually, when – and it ignores the fact that it is neither necessary or proportionate –and may be unlawful under HRA/ECHR – to take a person’s most sensitive and private information without (a) asking their permission first, and (b) telling them what it will be used for, and by who. Nobody is above the law, critically.
The fact is that the data gathered may increment the data available to research but that in its current form, care.data may actually not be that useful – it includes no historical data, for starters. And all this of course ignores the fact that care.data (and the CES that is derived from linking it to HES, etc.) will be used for things other than research, by people and companies other than researchers. That is the linchpin of the criticism. Finally, the Care Bill 2013-14 – just about to leave Committee in the Commons – will amend Section 251, moving responsibility for confidentiality from a Minister (tweets by Ben Goldacre here and here).
Anyway, the implementation of this has been completely chaotic, as I described briefly here on this Socialist Health Association blog. What now happens is anyone’s guess.
The author should like to thank Prof Ross Anderson, Chair of Security Engineering at the Computer Laboratory of the University of Cambridge, Phil Booth and Dr Neil Bhatia for help with this article.
Size isn’t everything…. except in Labour’s competition policy
 There are a few squares to circle when it comes to how Labour negotiates the future direction of health policy for the National Policy Forum later this year.
There are a few squares to circle when it comes to how Labour negotiates the future direction of health policy for the National Policy Forum later this year.
One of them will have to be Labour’s future direction on “competition”. The basic knub of it is that people or entities which are competing will end up performing better, however that this is measured, to the benefit of the end user (called ‘customer’ traditionally in business or ‘person’ or ‘patient’ in healthcare.)
Ideologically, competition is associated with the neoliberal approach, where market forces will ultimately equilibrate to the benefit of the population. This has been likened to a Darwinian ‘survival of the fitness’.
However, the analogy is not entirely useless. In such a construct, it is perfectly possible that certain living beings become extinct. There may be no love lost over an ancient reptile no longer contributing its DNA to the animal race, but there could be a problem if a NHS unit for a very rare disease becomes financially unviable and goes extinct.
So Labour does have a slight problem on its hands. People disagree on the extent to which the section 75 Health and Social Care Act, which secured competitive tendering as the default option for commissioning NHS contracts (mainly to the private sector), was a a natural extension of the market philosophy which had occurred under the competition and co-operation facility of Labour.
People generally agree that the original arguments about quality and competition in the NHS were extremely badly argued with hindsight, in promoting “the market”. On the whole, members of the general public agree that there might be a rôle for competition in driving up standards in cleanliness of surgeries, such that you might prefer to be a patient of a particular surgery, while trusting a Doctor to be driven by professional standards not by profit.
The idea of the NHS logo becoming a kitemark for private providers long pre-existed this Government, and was alive and well under the previous Labour government. On the other hand, Andy Burnham MP has emphatically pledged that Labour will roll back the market when it comes into government in May 2015.
The repeal of the Health and Social Care Act (2012) is a big thumbs down to its three main planks of policy. One is definitely ‘unfinished business’, as anyone following the arrangements for Trust Special Administrators will see in the insolvency regimes. The other two are intrinsically the full entrenchment of the market through section 75, and its regulation through enhanced powers for an economic regulator called Monitor.
So can it be that Labour per se objects to competition? Historically, this cannot be the case.
Labour wishes to promote collaboration, which is in keeping with socialistic principles of solidarity and co-operation. However, two major areas of criticism emerge from many stakeholders over competition especially from the Unions, who represent many hardworking Doctors and nurses inter alia.
Firstly, the focus of the attack seems to be on corporates rather than SMEs or social enterprises. Indeed, markets tend to break down when large corporates collude in legal price behaviour meaning the end user does not benefit. This has contributed to a ‘cost of living crisis’ in energy and rail fares.
The market especially breaks down when specific corporates or charities collude with the State, producing a near monopolistic effect. This historically has been more likely the greater their size. This effect can be particularly detrimental when this impacts on policy, some of which is best left to non-market forces like subject experts or professionals.
The fundamental problem, if you apply Prof Michael Porter’s influential theory of competition from Harvard, is that smaller sized companies experience formidable barriers to entering the market. For example, they cannot compete on the basis of marketing spend or resources for investment. All too easily they can go out of business – hence the complete banality of claiming to have ‘an equal playing field’. A titchy SEO simply cannot compete with a large multi-national corporate especially if that corporate is already skilled at doing slick commercial pitches.
This is significant in considering the overall shape of how Labour policy is shaping up for 2015. It’s not a general attack on business that Ed Miliband has in mind, but an attack on those large corporates who are abusing their power.
Secondly, large companies under law have a duty for their directors to promote profitability with due regard to their environment, but profitability is generally considered to be dominant by legal experts in this jurisdiction. Social enterprises form an umbrella of different entities, which do not necessarily have to have this duty (for example in talking about a surplus not profit).
There can of course be bad charities or bad other entities in the third sector, just as there can be bad private or public limited companies. Part of the challenge for Labour is to think about how it can reconcile the views of Andy Burnham, who wishes to roll back the market, and Alan Milburn who sees competition as a means of promoting progress. It is crucial to remember that Alan Milburn is not a member of the Shadow Health team: that team is led by Andy Burnham MP.
Hedge funds or private equity will nor necessarily wish to confine their investments to large corporates anyway. Smaller companies may be more nimble and more likely to produce a return on investment, and, should Labour wish to find a place for such activity in the NHS somewhere, Burnham and Milburn might see a way in which their profits can be ploughed back into the general health economy of the NHS. Whilst the NHS has been demonised by lazy journalists and politicians as being ‘monolithic’, with the same old canards put to out to trot (or whatever the phrase is), the NHS can in business management terms benefit from its economies of scale, making it more competitive.
So it might be that Alan Milburn and Andy Burnham are able to define the parameters in which there is a place for competition in the NHS. It could be that many large corporates do not wish to collude in an oligopolistic way at all, and act responsibly in the NHS.
However, Andy Burnham, in promoting his “NHS preferred provider” can provide a way in which social enterprises can legitimately contribute to competition, and even have some input from the multinational corporates in contracts under “the prime contractor model.” This of course can be done within the parameters of maintaining a NHS which is comprehensive, free at the point of need, in as much as some rationing has been taking place, but to avoid a rampant market with powerful private providers cherrypicking profitable work.
But the point is that the positions of Milburn and Burnham are not complete polar opposites. Whilst loyalties to the two individuals can be quite fierce, they both occupy a very senior of level of influence in the Labour Party, and will have a massive say on the future direction of the English NHS. But it is yet again significant to remember that Alan Milburn is not a member of the Shadow Health team: that team is led by Andy Burnham MP.
Should you pay your taxes to fund corporate welfare?
 Far from reforming the NHS with a view to improving patient safety, the 493 pages of the Health and Social Care Act (2012) and the concomitant £3bn implementation produces the mechanism for awarding ‘NHS contracts’ to the private sector – an extension of corporate welfare.
Far from reforming the NHS with a view to improving patient safety, the 493 pages of the Health and Social Care Act (2012) and the concomitant £3bn implementation produces the mechanism for awarding ‘NHS contracts’ to the private sector – an extension of corporate welfare.
These private companies carry out NHS functions using a NHS logo, so as far as the ‘end user’ is concerned (formerly called ‘the patient’), the service is being run by the NHS.
This is sold as the private company running the service more efficiently,except somehow this square peg has to fit into the round hole of the fact that the private company has to provide the service at an acceptable level of profit to them. Invariably, they are awarded the contract because they are slick at making pitches.
One of the challenges for the new incoming Labour government will be getting rid of compulsory competitive tendering.
But a difficulty that the incoming government will face is not depriving all those hard-working corporate lawyers from lucrative competition and procurement law work, at a time when their revenues had been soaring and high street firms had been closing down by the day.
Another desirable move would be to ensure that contracts, awarded for ‘best value’, have some sort of ongoing performance management mechanism built in. This is because increasingly contracts of the ‘prime contractor’ variety, where various component contracts are subcontracted out, will be of a long duration. We already know from experience with various private outsourcing contracts that some companies are facing or have faced criminal investigations for fraud.
Some other companies have been directly criticised by MPs for unacceptable performance, such as the handling of welfare benefits.
One of the Dragons in Dragons Den advised in his audiobook that a good business model for ‘sustainability’ makes use of Government grants.
It follows as night follows day that all governments want to offer you low taxes. For example, a homeowner in Sussex with rising property prices with lower taxes might wish to vote Tory. Sod the food banks.
But an interesting situation is now developing where taxes are being used act as corporate welfare handouts for companies awarded outsourcing contracts in the NHS.
In this construct, working for the NHS is seen as inferior, wages in working for the NHS are lower, and there’s no pride for working for the NHS brand. But this is all sold weirdly as an ‘equality of opportunity’ to suit a competitive capitalist market.
And who would dare to rubbish the NHS brand? Let me think.
Before you attack benefit scroungers, time to think where your taxes from all your hard work are in fact going.
Benn, Bevan and Burnham: continuity of care?
One of the lasting legacies of the introduction of the Andrew Lansley Health and Social Care Act (2012) is that it was a massive betrayal of trust. It explicitly did not appear in the Conservative manifesto. It was clearly a Lansley ‘vanity project’ which cost billions to implement.
While the purpose of this Act was promoted in a number of different marketing ways, the Act, nearing five hundred pages, is in fact incredibly simple.
It sets up a market based on competitive tenders. It sets up a beefed up economic regulator. It sets up the climate for ‘liquidation camps’ that only Frederich Hayek could have been truly proud of.
That was basically not a vision that most people had for the NHS in these demanding times.
With not a single clause on patient safety, save for abolition of the National Patient Safety Agency, it was clearly not drafted to prevent another Mid Staffs.
With this level of mistrust, there are people who think integrated care is a shoehorn for a private insurance system.
And yet paradoxically the latest NHS reforms seems to have taken a lot of wind out of the sails of a move towards an insurance-based system as proposed by Reform a few years ago. Whilst Kaiser Permanente seems to still quite chummy with certain think tanks, it’s clear the voters in majority want a properly funded national health service funded out of taxation.
Against this backdrop, care of older people is possibly not what anyone would want it to be currently.
Labour has indeed a long legacy in the NHS history, but is clearly now looking to the future. It is argued that ‘whole person care’ can complete Bevan’s vision, uniting the NHS with social care. This would mean one service looking after the whole person – physical, mental and social. Indeed Andy Burnham at this year’s Party conference recalled the “spirit of 45″. This vision would be symbolic for beginning to bring to a close the marketisation and privatisation of the health service.
Labour have pledged to repeal the Health and Social Care Act 2012, which is fragmenting the service.
And yet a decade ago the Health and Social Care (Community Health and Standards) Act 2003 Commencement (No. 1) Order 2003 was the most controversial piece of legislation to come out of the then government’s 10 year strategy for the NHS in England. This piece of legislation, which abolished government control of NHS trusts by turning them into competing independent corporations called foundation trusts, was a major policy reversal. The concern then was it could lead to considerable local variation in services and endangers one of the NHS’s founding principles–to provide equal care for equal need.
Beep, beep – this vehicle is reversing.
Labour has set up an independent commission under Sir John Oldham to examine how health and social care can be integrated. Ed Miliband feels that this is is the biggest challenge in the history of the NHS. This in part addresses the gap between NHS and care demand which is expected in coming years, and current funding.
There is absolutely no doubt that integration is being damaged by the government’s “free market ideology”, a point freely conceded by the corporate competition lawyers.
The great attraction of the Whole-Person approach, with the NHS taking responsibility for coordination, is that it can be in a position to raise the standards and horizons of social care, lifting it out of today’s cut-price, minimum wage business.
It is clear from Tony Benn’s brief interview with Emma Crosby that Benn has concerns. Benn in his latest diaries, “Autumn blaze of sunshine”, talks of various medical issues which have caused him to come into contact with the caring professions. Benn most obviously feels that valuing care workers has not been a priority of English society by any stretch of the imagination. Benn most obviously wants this to be addressed in some form in a future Labour government.
There has been much said about valuing social workers, but the profession of social care work have been equally vocal about voicing their hard-felt concerns. It is possible that social care careers could be more valued and young people able to progress as part of an integrated Whole-Person workforce. This is yet to be seen.
So an NHS providing all care – physical, mental and social – could be held to account by powerful “patient rights”.
The approach, unlike the Health and Social Care Act (with the exception of the surgeons), has been welcomed by professionals in the Royal Colleges. For example, the Royal College of Psychiatrists has argued that ‘a parity approach’ should enable NHS and local authority health and social care services to provide a holistic, ‘whole person’ response to each individual, whatever their needs. They have also argued that this should ensure that all publicly funded services, including those provided by private organisations, give people’s mental health equal status to their physical health needs.
Central to this approach is the fact that there is a strong relationship between mental health and physical health, and that this influence works in both directions. Poor mental health is associated with a greater risk of physical health problems, and poor physical health is associated with a greater risk of mental health problems. Mental health affects physical health and vice versa.
And it’s clear that ‘whole person care’ is not some weird science fiction. A number of local authorities have already signed up to become “whole person care innovation councils” in a programme led by Labour’s shadow health secretary Andy Burnham. The councils are already taking the first steps towards turning into reality Mr Burnham’s vision of a single health and social care service. Under these Labour plans more care will be provided directly in people’s homes, there will be a greater focus on prevention and better co-ordination between different branches of the system.
In the 21st Century, the challenge is to organise services around the needs of patients, rather than patients around the needs of services. That means teams of doctors, nurses, social workers and therapists all working together. This ideally means care being arranged by a single person who you know – ending the frustration of families being passed around between different organisations and having to repeat the same information over and over again.
This seems to be the sort of thing which Tony Benn would like too.
But it is a marked shift in gear. It means a greater focus on preventing people getting ill and more care being provided directly in people’s homes so they avoid unnecessary hospital visits. Keeping frail individuals out of hospital will clearly be one of the ‘next big things’ in English health policy, whoever is in government after May 7th 2015.
It will be quite a culture shock to move the NHS from an organisation being pump-primed for global multi-national expansion. But the NHS has been through worse changes. This one might actually be useful.
The Health and Social Care (2012) was not about patient safety: implications for the Keogh report
The Health and the Social Care Act (2012) is a massive tome. It actually reads, for lawyers who are well acquainted with such statutory instruments, like a huge patchwork quilt of commercial and corporate law strands. While voluminous, at 473 pages, it has two critical clauses. The first is section 75, and its concomitant now famous Regulations, which provides the statutory basis for procurement contracts in the NHS to be put up for price competitive tendering as the default option, thus fixing the NHS in a competitive market of an economic activity. This is of course the mechanism for outsourcing NHS services into the private sector, and indeed the vast majority of contracts have now been won by the private sector. This was widely predicted, as the private sector have skills and resources to make slicker bids, irrespective of the bid they ultimately deliver, to transfer a much higher proportion of “NHS services” into the profit-making private sector. All of this costs the NHS more money sadly, as while it may not matter to you ‘who provides your services’, you’re in trouble if the private provider goes bust, and you’re not paying for anything at anywhere near cost-price because of the mark-up for profit. This section 75 clause acts in tandem with section 164(1)(2A) which allows any NHS hospital to receive up to 50% of its income from private sources. Thus the Act, and the £2.4 NHS “reforms”, have been a bonanza for the private sector, and disastrous from the perspective of a state-provider of universal, comprehensive healthcare.
Patient safety is in fact only mentioned once in the Act, in clause 281. That is in reference to the abolition of the National Patient Safety Agency. The National Reporting and Learning System which was hosted by NPSA has a two year stint at Imperial College Hospital NHS Trust, while a tender process is scoped and developed by the Board. NPSA’s responsibilities concerning patient safety will transfer to the NHS England.
The Health and Social Care Act 2012 (c. 7) is an Act of the Parliament of the United Kingdom. It is the most extensive reorganisation of the structure of the National Health Service in England to date. It proposes to abolish NHS primary care trusts (PCTs) and Strategic Health Authorities (SHAs). The Act’s proposals were not discussed during the 2010 general election campaign and were not contained in the 20 May 2010 Conservative – Liberal Democrat coalition agreement, which declared an intention to “stop the top-down reorganisations of the NHS that have got in the way of patient care”. However, within two months a white paper outlined what the Daily Telegraph called the “biggest revolution in the NHS since its foundation”. The white paper, Equity and Excellence: Liberating the NHS, was followed in December 2010 by an implementation plan in the form of Liberating the NHS: legislative framework and next steps. The bill was introduced into the House of Commons on 19 January 2011, and received its second reading, a vote to approve the general principles of the Bill, by 321-235, a majority of 86, on 31 January 2011.
The British Medical Association opposed the bill, and held its first emergency meeting in 19 years, which asked the government to withdraw the bill and reconsider the reforms. A later motion of no confidence in Lansley by attendees at the Royal College of Nursing Conference in 2011, however, succeeded, with 96% voting in favour of the motion. Nurses have consistently been opposed to the the “efficiency savings” measures being undertaken across the NHS, with many raising concerns of their material impact on frontline medical services. “People will die”, Richard Horton, editor of The Lancet, warned in March 2012, as he predicted “unprecedented chaos” as a result of the reforms, with a leaked draft risk-assessment showing that emergencies would be less well managed and the increased use of the private sector would drive up costs.
The Bill is now Law, and where are the measures to deal with this longrunning problem of patient safety, particularly in the acute setting? There are none. The media was sent into overdrive in portraying the NHS has a “death machine”, despite the best attempts of nurses and Doctors to run the service under difficult conditions. The publication of the damning Keogh Report (“Report”), which spelt out the failings of 14 hospital trusts which did not quote “13,000 “needless deaths” since 2005″, is despite exhaustive pre-briefing to the media. The Report depicts a situation in certain trusts where patient safety is poor, with no reference to what action has been taken by the Government and their civil service to remedy this since the General Election in May 2010, which the Conservatives lost. Sir Bruce Keogh, the NHS’s Medical Director, will describe how each hospital let its patients down through poor care, medical errors and failures in management, but the Report is as if the clinical regulatory bodies do not exist, the General Medical Council, the Nursing and Midwifery Council and the Care Quality Commission. How they have escaped blame for this reported ‘scandal’ is incredible, although one suspects the media will catch up with them eventually. It might be that the media for whatever reason known to them do not feel the clinical regulators are in “the firing line”, despite being supposed to be responsible for patient safety, in the same way that lawyers are not responsible for the global financial crisis despite being supposed to regulated on the safety of financial instruments.
From a management point of view, the Keogh Report serves a function for convincing the public of a need to take patient safety extremely seriously. However, to sell the Keogh Report as “Do you now see the need for the NHS reforms?” maybe hitting a target but missing a crucial point. The NHS reforms are all to do with outsourcing and eventual privatisation of the NHS. They are nothing to do with patient safety, as even right-wing think tanks and their spokesmen have previously conceded in public. In fact, it is worse than that. The £2.4 reorganisation which nobody voted for, but which private healthcare companies extensively lobbied for, was a reckless missed opportunity to put resources into something other than frontline care, and the opportunity cost of this piece of legislation will continue to haunt the general public for many years. Unfortunately, the media and the members of the Establishment, some members of which have tenuous links with the institutional shareholders in private healthcare companies, will be more than aware of this hard fact. The Conservatives are desperate to pin every conceivable woe of the NHS on Andy Burnham, and every interview which Burnham now does must feel like “Groundhog Day” for him. He has nothing much more in his defense. Meanwhile, the Conservatives are exasperated that they have been unable to get the Burnham scalp, but there are as yet unresolved issues about what Government departments have done about NHS complaints in the last three years since May 2010. The bottom line is that the Health and Social Care Act is nothing to do with patient safety: even safety campaigners in the NHS know this, and they know of the even worse battle now facing them, of a fragmented privatised NHS which is even harder to regulate from that point of view. The NHS reforms, and more specifically the Health and Social Care Act which underpins them, have nothing to do with patient safety. More disturbingly, the Keogh report, when eventually published, will not stop ‘another Francis’, and it is entirely the Government’s fault we are in this stupid ridiculous position.
The section 75 NHS regulations exposed muddled thinking all round; but is there really no alternative?
It’s easy to lose sight of Labour’s fundamental question in terms of the economic model; viz, whether the State should, in fact, intervene in any failing #NHS healthcare (in a financial sense). That is what distinguishes it from neoliberal models of healthcare, including the New Labour one. It is a reasonable expectation that the healthcare regulators will uphold professional standards of the medical and nursing professions, whether in the public or private sector.
One of the most memorable experiences in my whole journey of the section 75 NHS regulations was Richard Bourne, the Chair of the Socialist Health Association, asking me what would probably happen at the end of the day. I originally replied saying that I was not an astrologer, but, as I thought about that question more, I became totally convinced it was a very reasonable question to ask. In management, private or public, when one is uncertain about the outcome, a perfectly valid tool is the ‘scenario analysis’, where one considers the various options and their likelihood of success. Also, if you really don’t know what the eventual outcome is, which might be the case, say, if you have to produce a complicated budget for the whole of the next year, you can to some extent ‘hedge your bets’ by doing a rolling forecast which updates your plan on the basis of virtually contemporaneous information.
Section 75 NHS regulations had become a very ‘Marmite issue’. Richard was right to pick up on the fact that the world would not necessarily implode with the successful resolution by the House of Lords of the second version of the regulations. On the other hand, the event itself marked a useful occasion for us all to take stock of where the overall ‘direction of travel’ was heading. Wednesday’s charge, led by Lord Phil Hunt, was as ‘good as it gets’. Reasons for why Labour in places produced a lack lustre attack is that some individuals themselves were alleged to have significant conflicts of interest, or some elderly Peers were unable to organise suitable accommodation so that they could negotiate the ‘late night’ vote. Lord Walton of Detchant, whom all junior neurologists will have encountered in their travels at some point in the UK, said convincingly he had a look at the Regulations, and felt that they would be OK even given the ‘torrent’ of communication he had personally received about it.
I certainly don’t wish to rehearse yet again the arguments for why the section 75 NHS regulations appears to be farming out the NHS to the private sector, but in the 1997 Labour manifesto, where Tony Blair was likely to win, Labour promised to abolish the purchaser-provider split. It didn’t. Labour likewise is promising now the repeal the current reincarnation of the Health and Social Care Act. It might not. There is substantial brand loyalty to Labour, over the NHS, such that the Conservatives would find it hard to emulate the goodwill of the public towards it that is shown to Labour. Given that the market has been implemented in the NHS, the Conservatives and Liberal Democrats are now arguing that they wish to make the market ‘a fair playing field’, which is of course a reasonable aspiration provided that a comprehensive NHS can be maintained for the public good.
Many have no fundamental objection to running a NHS most efficiently. I often find that health policy experts who have little clinical knowledge find themselves going on wild goose chases about efficiency in the NHS. For example, I remember the biggest barrier to progressing with a patient with an acute coronary syndrome is that it would be impossible to get a troponin blood result off the HISS computer system for hours, such that you would be forced to track somebody down from the laboratory itself. Co-ordinated care can mean better care. The best example I can think of is where a GP prescribes Viagra for a man with erectile problems in the morning, the patient collects all his new medication from the local chemist, the patient then takes the first tablet around lunchtime, the patient has sex with his partner in the evening, but unfortunately attends A&E in the evening for angina (chest pain). Modern advice (for example here) would argue that an emergency room should take a very cautious approach in administering nitrates, a first line medication for angina, within 24 hours of a dose of viagra. What a Doctor would do in this particular scenario is not something I wish to discuss, but it is simply to demonstrate that patient care would benefit from ‘joined up’ operational processes, where the emergency room doctor had knowledge of what had been prescribed etc. that day.
So, it probably was no wonder that there was ‘muddled thinking’ all round. Baroness Williams is a case in point. She acknowledges that many in the social media think that she personally, with the Liberal Democrats en masse, has ‘sold out’ on the NHS. And yet she talks about a deluge of misinformation from organisations such as 38 degrees who cannot be shot for being the messenger for a concerned public; that presumably is consistent with the Liberal Democrats yearning for ‘a fair society’? Lord Clement-Jones attacked the person not the ball, advancing the argument that lawyers will always provide a legal opinion which favours the client. However, many agree with David Lock QC in his concerns on how the legislation could be interpreted to go further than the previously existant legislation from Labour over the Competition and Cooperation Panel. Indeed, Labour in the late 2000s had tried to legislate for public contracts, with attention to how their statutory instruments might be consistent with EU competition law.
However, the muddled thinking did not stop there. Only a few people consistently explained why the regulations were a ‘step too far’, and it is no small achievement that the original set of regulations had to be abandoned. The general public themselves can be legitimately blamed for muddled thinking. The general impression is that they resent bankers being awarded bonuses, resent the explosion of the deficit due to the banking crisis, but did not wish the banks to implode. The general impression is also they are happy with the previously high satisfaction ratings of the NHS, do not wish the NHS budget to be cut, and yet do not want ‘failing NHS trusts’ to be shut down altogether. Meanwhile, the Francis report exposed sheer horror in how some patients and their relatives or families experienced care from the NHS, and there are concerns that similar phenomena might be exposed in other Trusts. All of this is totally cognitively dissonant with the idea of ‘efficiency savings’ in the NHS, with billions of surplus being given back to the Treasury instead of frontline patient care. The issue about whether private companies should be allowed to make a profit from healthcare is a difficult one, when compared to an issue of whether parents can have a ‘choice’ as to whether to send their children to independent schools. However, many members of the general public would prefer any profit made in the NHS to be put back into patient care, rather than lining the pockets of shareholders or producing healthy balance sheets of private equity investors. The section 75 NHS regulations has done nothing for a discussion about how to maximise patient safety, nor the value of employees in the NHS. Managers in the NHS appear to be pre-occupied with ‘excellence awards’, innovation and leadership, but appear to have lost sight of the big picture of the real distress shown by some working at the coal face in the NHS.
Monitor, the new economics healthcare regulator, has a pivotal part to play; but they are an economic regulator ensuring fair competition, so it is hard to see as yet how they can best secure value for the patient rather than dividend for the providers. This is a Circle to be squared (pardon the pun). Possibly the only way to ensure that the NHS does not become a ‘race to the bottom’ (where “I don’t care who provides my healthcare as long as it’s the most efficient” becomes “I don’t care who provides my healthcare as long as it’s the cheapest and delivers most profit for the private provider)” is to ensure that people who are clinically skilled are involved in procurement decisions, or in regulatory decisions. This is the only way where yet another one of Earl Howe’s promises might be fulfilled; that local commissioners can commission services, even if they are only available from the NHS, if it happens that ‘there is no alternative’. Possibly doom-and-gloom is not needed yet, but it cannot be said that Lord Warner did much to inspire faith as the only Labour peer to vote against Labour’s “fatal motion”. Many people did indeed share the sense of despair felt by Lord Owen before, during and after the debate. However, Labour has to react to the present and think about the future. It cannot rewind much of the past, for example current PFI contracts in progress. The public have already exhausted themselves with the debate over ‘who is to blame over PFI?’, where both Labour and Conservatives have contributed in different ways to the implementation of PFI, and there are still some who believe that the benefits of infrastructure spending through PFI are yet to be seen. But blaming people now is probably a poor way to use precious resources, and there is a sense of ‘in moving forward, I wouldn’t start from here.’ Labour has to think now carefully of what exactly it is that it intends to repeal and reverse. Its fundamental problem, apart from sustainability, is to what extent the State should ‘bail out’ parts of the system which, for whatever reason, aren’t working; but this is essentially the heart of the neoliberal v socialism debate, without using such loaded language?
Shibley tweets at @legalaware.
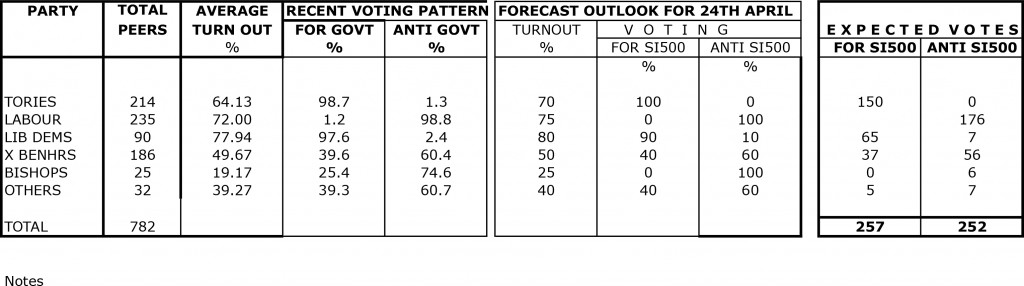
As few as five votes could mean the controversial section 75 NHS instrument get passed by their Lordships
This is by no means a “done deal” by any stretch of the imagination.
I had a pleasant conversation with Suresh Chauhan just now. He has done the research below.
Suresh has tried to forecast the voting outcome on the Lords prayer/debate regarding SI500.
The figures are based on actual turnouts/voting patterns in this parliament.
His assumptions for the forecast are as follows:
- A large number of Conservative peers are alleged to have interests in private healthcare providers. It is noted that it is argued that they have not missed any opportunity to support the Conservative-led government’s NHS main legislation and statutory instruments.
- Many Liberal Democrat peers have been given false reassurances that the new statutory instrument goes no further than existing legislation. This is clearly not true, with the current Government having made the effort of putting onto the statute books such voluminous legislation for the purpose of maximising competitive tendering in the NHS. The Regulation 5 specifically establishes that there should be a competitive process unless for uncommon occasions, so it is utterly irrelevant how bids have been ‘sold’, in terms of ‘best value’, or ‘integrated care’. This is the direct effect of the proposed law, for which there are many reliable authorities who have produced authoritative commentaries, and it is hard to escape this jurisprudence. Furthermore, it is simply not the case that all disputes can be channeled through Monitor. All private providers will have the ability to pursue litigation in the High Court, and it is anticipated that with this legislation (and relative lack of experience and skills in procurement as well as financial resources) CCGs will be coerced into exercising caution. Fear of the bargaining power of suppliers clearly does not promote competition in the patients’ best interests necessarily, and it had been discussed in the parliamentary process that parliament would NOT force stakeholders into a competitive tendering process.
- Behaviour of Crossbenchers is difficult to predict.
- Turnout of Bishops has normally been described as ‘disappointing’.
The key conclusion from this research result is that the vote is likely to be extremely close in reality, and depends on a good turnout from the Labour Lordships.
It is therefore imperative that the Labour peers turn up for this particular vote. Lord Steve Bassam (@stevethequip) is Brighton’s cricketing labour chief whip in the Lords. Lord Bassam is Member of Shadow Cabinet, and very conspicuously an ardent Brighton fan.
I am reliably told that the Labour Lords are though doing their best for the key vote on Wednesday.
It’s going to be extremely challenging for the vote anti-the instrument to be higher than the vote for-the instrument, because of the whipped Liberal Democrat vote.
Mud sticks: the new s.75 NHS regulations once enacted will be the ultimate disaster
The Canadian model is built on a recognition of the limits of markets in distributing medically necessary care. Most markets distribute goods on the basis of supply and demand, with price signals used to affect production and consumption decisions. When price drops, demand should increase, with a near-infinite demand for free goods. Conversely, with fixed supply and high demand, price should rise until enough people get priced out of the market to balance supply against this new (lower) level of demand at the new equilibrium price.
Yet health care markets stubbornly refuse to follow these economic laws. Economists have debated why this is so and whether they can force health care to behave in accordance with theory. In Canada, there is remarkable tension with power being devolved to the provinces, meaning that if anything goes wrong, it is hoped that central government can escape the blame.
This latest set of ‘top-down reforms’ of the NHS are estimated to cost £2bn, and the widespread perception is that the system has been thrown into chaos because of a lack of fundamental understanding of the pre-existing culture of the NHS and overcoming the “barriers to change”. GPs in the UK are likely to be the ‘fall guys’ for this failed implementation. When the US sneezes, the UK catches a cold. We can already see this phenomenon being rehearsed ad nauseam across the pond. For example, in a recent American blogpost, “Who is to blame for the current healthcare crisis?” , Dawn J. Lipthrott comments that, “Doctors are to blame when they try to make up loss by over-scheduling and growing careless, or by failing to communicate with their patients.
The devolution of power to the locality is critical in ensuring that as much blame can be directed locally as possible. Of course, the idea of real local democracy is an illusory one, when you consider the emotional trauma local residents of Lewisham or Mid Staffs, for example, have experienced.
The Royal Free Hospital in its guide to NHS Foundation Trusts writes,
“The introduction of NHS Foundation Trusts represents a profound change in the history of the NHS and the way in which hospital services are managed and provided. NHS Foundation Trusts are a new type of NHS Trust in England. They are part of the Government’s plan for creating a patient-led NHS. The aim of these reforms is to provide high quality care, shaped by the needs and wishes of today’s patients, in the most efficient way. NHS Foundation Trusts have been created to devolve decision-making from central Government to local organisations and communities so they are more responsive to the needs and wishes of their local people. They are also at the leading edge of many of the other reforms and improvements that are creating a patient-led NHS.”
Meanwhile, the scandal-hit Mid Staffordshire has just become the first NHS foundation trust to be put into administration, The sector regulator Monitor said it has appointed two trust special administrators to “safeguard the future of health services” currently provided at the trust.
The “Local Government Lawyer” magazine writes in February 2013:
“In conclusion, local authorities have unique powers to scrutinise NHS functions, to call for information and explanations, to question proposed plans, and to invite senior managers to attend and provide evidence. However unwelcome their attentions may be, they do have a responsibility to exercise these powers “positively and proactively”, and that includes recognising that the function goes beyond the occasional attention of well-intentioned but lay members, to include demanding the information and providing the professional resource and competence to be able to do the job effectively.”
The notorious Section 75 regulations – set the legal framework for NHS competition under the government’s health reforms. They have already been revised once, after opposition to an original version from both the Liberal Democrats and Labour.The original plans would have seen NHS trusts forced to ask private companies to bid for every service, even if commissioners were satisfied with the way it was being run by the public sector. The new revised regulations insist that Clinical Commissioning Groups must invite bids for services in all cases except those which they are sure can be provided only by the current provider. This will mean only the most difficult and expensive contracts will be held by public sector organisations, as private companies will say they are capable of providing all others.
The concerns were confirmed by a recent Lords committee, which said the revised rules were “substantially the same as the original regulations”. Although many members of the committee said the new wording was an improvement, they also warned: “The wide range of interpretations of the substitute regulations is, we believe, likely to translate into uncertainty about how they will operate.”
Even with the new section 75 NHS regulations, when the private providers take the CCGs to court over the tenders, and the judge rules against the CCG on the process grounds of openness, transparency, Wednesbury reasonableness or even proportionality, and there is a huge public outcry, the Department of Health can easily blame the CCGs for a failure in the procurement process, especially as they do not have a comparable skill-set for doing slick procurement. It is widely believed that the new regulations lack sufficient clarity, so that the litigation option outside Monitor can easily be exercised by private providers.
The LibDems, of course, don’t want any of the mud sticking to them. The Liberal Democrat Lords health spokeswoman Baroness Jolly said she had received assurances from health minister Earl Howe that critics’ fears about the revised regulations were unfounded, and that this would be made clear when healthcare sector regulator Monitor published its guidance on them. That news only came a day after a coalition of influential charities, including Marie Curie Cancer Care, Sue Ryder, and Help the Hospices issued a parliamentary briefing warning that the new rules could mean competitive tendering for NHS services becomes “mandatory in all but the most exceptional circumstances”. On the other hand, the controversial regulations should be withdrawn, according to the BMA ahead of crucial Lords debate on 24th April 2013.
Meanwhile, the media is already gearing up to blame the CCGs. In March 2013, it was reported that one in three GPs who are running new organisations that are about to be given £65bn of the NHS’s budget also help run or hold shares in a private healthcare firm, a study shows. The disclosure has sparked concern that such widespread conflicts of interest will threaten patients’ trust in GPs, who they may see as lining their own pockets out of public funds. Overall 426 (36%) of the 1,179 family doctors on a board of one of the 211 clinical commissioning groups (CCGs) in England have an interest in for-profit firms, including those providing common NHS services such as diagnostics, minor surgery and out-of-hours GP care, an investigation by the British Medical Journal (BMJ) found. Some of them, it is alleged, are senior directors of such firms, while others have a shareholding in major private health companies such as Harmoni and Circle Health, which already earn hundreds of millions of pounds a year for doing NHS work alongside local doctors.
As usual, the LibDems are ferreting around to make sure that none of the mud of the failed section 75 NHS regulations sticks ultimately with them. You have to be either beyond stupid or fraudulent to claim that the current regulations are workable, even with the veneer of ‘integrated care’, as CCGs will be forced into a competitive process unless there are drastic reasons. The whole situation has gone beyond pathetic now, and is not even worthy of a ‘The Thick of It” script. Mud sticks: the new section 75 NHS regulations once enacted will be the ultimate disaster.
My blogposts on section 75 NHS competition regulations and the current situation
Whatever the victories claimed by the political parties, it does not matter what the niceties are about how bids will be considered (integration, “best value”, etc.), it will virtually always be possible there should be a costly competition process. The regulations (made under Section 75 of the Health & Social Care Act [2012]) still require all NHS services to be put out to competition unless the commissioners can prove there is only one provider capable of delivering them. Far from putting competition ‘back in its box’ as some have suggested, these regulations open the floodgates to legal challenges outside of Monitor, and will lead to an extensive and expensive extension of privatisation in the NHS, causing a bitty disjointed service. Whenever you introduce transaction costs into anything, the bill goes massively up.
We are now in April, but since 7 January 2013, I have written a number of blogposts detailing the legal and policy implications of the Health and Social Care Act and the two statutory instruments pertaining to section 75. Soon Caroline Molloy (@carolinejmolloy) will be updating everyone on how you can get involved, such as writing to your MP or a Peer.
Here is a summary of what has been done and what remains to be done:
My main article from early January 2013:
Posts on the first statutory instrument SI 2012/057 which was later discarded:
National Health Service (Procurement, patient choice and competition) Regulations 2013: what is “best value”?
The legal issues in the statutory instrument (2013, No. 257) on NHS procurement in England
Possible letter to send to the Clerk of the Committee
VERY IMPORTANT. Tomorrow is the last day to the write to the Clerk about SI 257
A post on Lord Owen’s Bill and supported by Prof Allyson Pollock:
History:
Initial reaction to SI2013/057:
Rainbow coalition warns about section 75 NHS Regulations
Thank you very much for the positive feedback which I have kindly received for my work above.
Further reading material:
1. A cartoon which brilliantly explains in a nutshell the thrust of these NHS statutory instruments
2. Guardian article by Prof Bob Hudson
3. Open democracy article on amended section 75 regulations by Caroline Molloy
4. Expert legal opinions (commissioned by 38 degrees): original SI 2013/057 regulations and “No. 2″
6. Comments by experts (article by Caroline Molloy)
7. Lords scrutiny committee on No. 2