Home » Choice and control
If you say ‘no decision about me without me’ too much, it’ll become meaningless
It seems to have become a ‘bomb proof mantra’.
No self-respecting policy wonk on the healthcare circuit can be seen without the words ‘no decision about me without me’ stitched into the lapel of their jackets.
But if you repeat something enough times, people will believe you.
Conversely, it might become meaningless.
It of course is motherhood and apple pie, and not an ethos which you could fundamentally disagree with. Normally, that is.
This current parliament saw parliament introduce section 75 of the Health and Social Care Act (2012), and its associated regulations. It was a significant departure from previous statutory instruments enacted under previous governments.
This current Government wish to demonstrate in flashing lights their commitment to ‘localism’. This plainly became very hollow when Jeremy Hunt saw fit to contest the Lewisham case in both the High Court and Court of Appeal, against the loud wishes of stakeholders, at taxpayers’ expense.
The NHS in England is still reeling from this catastrophic policy decision, touted by a number of high profile think tanks and their corporate masters. It gave rocket boosters to competitive tendering to the private sector.
In any market, there are winners and losers. For every winner, there’s a loser. There’s a finite amount of cake we are being told. So in this climate it is no wonder that providers, including social enterprises, wish to seek an unique selling point in marketing.
The slogan “no decision about me without me” happily trips off the tongue for the purpose. There is very hard for any reasonable person to argue against the design of research programmes and the service without the views of the end-users.
But this all depends on your precise definition of ‘involvement’. For example, I have been successfully living with two chronic long term conditions, physical disability and mental recovery from a severe alcohol dependence. But in this climate of ‘co-production’ and ‘distributed leadership’, and even shared decision-making, nobody has had the decency to ask me for my opinions about these services.
One can adopt the stance that it is up to me to make my views know, rather than be merely a passive recipient of a service. And of course I do make my views known in non-symbolic ways.
The fact is that patients are all too often liable to made into cannon fodder for other people’s purposes. This might to be to sell a product or service in dementia.
Or they could be used to promote how wonderful ‘community services’ are in a London borough, for the personal gain of those promoting them, but at the expense of shifting resources away from severely under-resourced secondary care hospital units.
And not all stakeholders can be correct, and have an equal say in strategy. Reams and reams and reams have been written on this in the field of ‘corporate social responsibility’. For example, some social enterprises have found real difficulty in rationalising the drive to maximising shareholder dividend with community value and outcomes, however so defined.
And how corporates show responsibility (or rather “don’t behave badly”) has become a hotbed for corporate strategists. For example, Prof Michael Porter, a strategy Chair at the Harvard Business School, published a highly influential review with Mark Kramer on society and strategy.
Large charities – operating strategically in a corporate-like manner – can, it can be argued under this construct, be obtaining their “moral fitness to practise” by involving people they raise large funds for in their mission, whether that is for ‘friendly communities’, ‘care’ or ‘research’.
So the pen is indeed mightier than the sword. Like pornography though, I can recognise real involvement and empowerment when I see it.
Some people aspiring, rather than battling or fighting, to live with dementia do wish to have ownership and control their dreams.
But in this crazy world of ‘dyadic relationships’, and other similar convoluted terms, some persons with dementia for example have their own beliefs, concerns and their expectations. They are not joined at the hip to the carers.
“No decision without me about me” is one of the latest political catchphrases in relation to the health service, in our jurisdiction, and describes a vision of healthcare where the patient is – if not an equal partner – then certainly an active participant in treatment decisions.
In 2002 the independent Wanless report recommended that, in order to cope with rising demand and costs, the NHS should move to ensure that all patients were “fully engaged” in managing their health status and healthcare.
It has a laudable aim, but, like many of these slogans, is at real danger of trivialising what is a profoundly serious policy issue.
Personal budgets for dementia. What’s the harm in them, and are the right people benefiting?
Personal budgets held by individual people might allow more flexibility in choice and control over health services. So what’s the harm in them?
Barry Schwartz’s famous book “The paradox of choice”, summarising a lot of other evidence, contests the assumption that maximising collective welfare of citizens is achieved through maximising individual freedom.
On May 8th 2015, there’ll be a change in government in the UK (unless the arithmetic happens to throw up another Conservative-Liberal Democrat coalition, which is quite unlikely). It is likely that all the major political parties will wish to implement a form of ‘integrated’ or ‘whole person care’, with the merging of health and social care. It is a moot point how early on people, if at all, will be offered the chance of a ‘unified personal budget’.
A particular group of people for whom personal budgets may be considered are persons with dementia. It is therefore perhaps a bit disappointing that some of the same issues which existed many years ago are still lurking in some form even now.
No matter how much effort you put into ‘compassion’ or ‘Dementia Friends’, the care system is never going to be acceptable in the light of dangerous financial cuts to social care.
The “one size fits all” philosophy seems to be pervasive in the Government approach to personal health budgets, whichever Government pursues it. It’s as if it doesn’t matter who is the singer is because the song is the same: like Pharrell’s “Happy” was originally recorded by Cee Lo Green (allegedly).
Certain people with early dementia might be particularly prone to impulsive or risk-taking behaviour, so there is a reasonable question whether some persons with dementia – despite full legal capacity – are “safe” to have personal health budgets themselves. But this I feel strengthens my argument for a proper system of delivery of personal health budgets, not undermining them. When personal budgets work for dementia, as explained by Colin Royle here, they work very well.
A potential danger is that somebody is given a list of ‘options’ for care support planning, and effectively told to get on with it. It can be difficult to get to the precise details of resource allocation systems, and, without knowing such details, it is difficult to ascertain whether they legally constitute a process acting to the detriment of the group of people with dementia. This leaves individual local authorities open to an accusation of indirect discrimination, offending the Equality Act (2010). There are various sources of factors which might cumulatively cause certain people to be more disadvantaged than others: e.g. an ability to ‘self-assess’ one’s needs in a questionnaire (with age being a confounding factor).
Personal budgets might be offered in a number of ways: namely those which were directly commissioned and managed by the local authority, third party managed accounts, direct payments or a mixture of these things. Concerns might come from all sorts of quarters: such as actual budget holders who don’t feel that the resources allocated meet their needs, or the professions who don’t feel that certain candidates are suitable in the first place.
This is perhaps one of those uncommon instances where ‘cutting out the middle man’ is in fact a dangerous idea. The actual calculation of resource allocation for an individual candidate is emphasised rather than the calculation of running the whole system adequately, in much the same way that the improvement in wellbeing in a personal budget might accrue from having a choice at all rather than the actual proposed care intervention.
Take, for example, this passage:
“Quality support planning needs the investment of time. In the ideal world, presented by those who ‘run with’ the agenda, everyone is able to take an active part in making decisions for themselves and choosing their own care to meet their needs, as defined by themselves. The reality is that some groups have not been able to engage in the process of taking an active role in their own support planning; they are effectively excluded. This may be because they lack the capacity to manage a direct payment or organise a personal budget themselves, or because they lack support systems around them, such as family to help them do this.”
Clearly not everyone has benefited from the “Prime Minister’s Dementia Challenge”. For example, the Dementia Advocacy Network went bust at the end of last year. And yet this is precisely the time when people with dementia, and caregivers, need emotional support, and need to be safeguarded against forms of abuse including financial and legal. It appears that people who have benefited most from personalisation are those with the best advocacy and loudest voices.
Even with the most-straightforward appearance of self-assessment application procedures for personal budgets might require an enormous amount of professional support. There are various reasons why persons with dementia might have special obstacles in their uptake of personal budgets, as articulated well by the Mental Health Foundation: two for example include a residual stigma and discrimination against such citizens, and also the fact that some citizens might not have a reliable correct diagnosis in the first place.
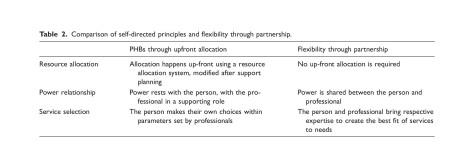
Self-directed support (SDS) has as its central feature a personal budget arrived at through an ‘up-front’ allocation of money; though up front allocation to give people power is one element of SDS amongst others and therefore it would be unfair to generalise across all the resource allocation systems techniques. It was introduced as formal policy in 2008, with an original target that all service users should have a personal budget for social care by 2011. In a recent helpful article, “Personalization of health care in England: have the wrong lessons been drawn from the personal health budget pilots?“, various well-known methodological problems with the original pilots are considered. The authors do, however, propose an extremely constructive way of moving forward, what they call “flexibility through partnership”.
Cheekily, the authors observe:
“As Gadsby points out ‘It seems that in many cases, additional resources[in the PHB group] were provided that enabled individuals to pay for extra services or one-off goods. It is perhaps unsurprising, therefore, that overall improvements were found in wellbeing amongst budget holders’”.
Without advocacy services, then, we really do run the danger of running a two tier service, and this is extremely dangerous, aside from the swathe of legal aid cuts. For a government which prides itself on parity, particularly for empowering new private providers to enter a liberalised market, any proposed system of personal budgets will require the same quality and opportunity for flexibility to all user groups including those who have no recourse to advocacy. A strengthened social care system would go a long way here.
Nobody has a single right answer for personal budgets in dementia so it might not be able to have the exclusive kite mark to match. It’s clear whilst there might be excellent ways of implementing them, there are plenty of bad ways too.
Unfortunately, time is running out a bit, and political leadership and adequate funding – including for advocacy services – are now both essential.
And who will benefit? If they work well, they will shift power to the people able to make ‘correct decisions’ in care, but I feel that the whole system has to be fit-for-purpose not the budget mechanism itself. That’s where the State comes in. Who the correct advocates are, as they might not necessarily be carers including unpaid caregivers (though they might be.) Ultimately, the most offensive irony would be to make the tool that offers choice and control compulsory, but this could be expected from politicians who like to give an illusion of choice.
There are still deeply engrained issues about whether people will have enough money to meet their needs. It might be easier to hide downsizing of budgets if they’re called a yet further new name. There are obviously huge problems with merging one universal system intended to be comprehensive and free at the point of need with one which is not and means-tested; and this would not necessarily benefit the person with dementia. And at worst, the wrong type of broker, not professional advocates including social workers, could be profiting but not providing overall benefit. Introducing any transactions into a system absorbs resources, however you attempt it.
We now have to be very careful with resolution of this potentially useful policy plank – otherwise it might be a case of ‘You’ll do’, rather than ‘I do’.
Kate Swaffer’s “Prescribed Disengagement”, “the sick role” and living with dementia
“Re-investing in life after a diagnosis of dementia” was a blogpost written by Kate Swaffer on January 20th 2014.
Kate’s experiences are fairly typical unfortunately.
“Following a diagnosis of dementia, most people are told to go home, give up work, in my case, give up study, and put all the planning in place for their demise such as their wills.”
“Their families and partners are also told they will have to give up work soon to become full time ’carers’. Considering residential care facilities is also suggested.”
“All of this advice is well-meaning, but based on a lack of education, and myths about how people can live with dementia. This sets us all up to live a life without hope or any sense of a future, and destroys our sense of future well being; it can mean even the person with dementia behaves like a victim, and many times their care partner as a martyr.”
Kate Swaffer has termed this “Prescribed Disengagement”, and it is clear to Kate from the huge numbers of people with dementia who are standing up and speaking out as advocates that there is still a good life to live even after a diagnosis of dementia.
Kate, who herself is a person living actively with a dementia, has suggested quite, at first sight, startling advice.
She advises everyone, “who has been diagnosed with dementia and who has done what the doctors have prescribed, is to ignore their advice, and re-invest in life.”
“I’m not talking about money, but about living well and continuing to live you pre-diagnosis life for as long as possible. Sure, get your wills and other end of life issues sorted out because dementia is a terminal illness, but there is no need not to fight to slow down the deterioration.”
“Alzheimer’s Disease International have a Charter that says “I can live well with dementia”, and this is not a joke, it can be done. They are serious about, and I am serious about it.”
And this advice from a person with dementia poses severe difficulties for the traditional narrative of dementia, needing medicalisation as a long-term condition.
In the 1950s, a founding father of medical sociology, Talcott Parsons, described illness as deviance -as health is generally necessary for a functional society – which thrust the ill person into the sick role (Parsons, T. The Social System. 1951. Glencoe, IL: The Free Press).
This role afforded the afflicted certain rights, but also certain obligations, which were described by Parsons in his four famous postulates:
- The person is not responsible for assuming the sick role.
- The sick person is exempted from carrying out some or all of normal social duties (e.g. work, family).
- The sick person must try and get well – the sick role is only a temporary phase.
- In order to get well, the sick person needs to seek and submit to appropriate medical care.
It is worrying that people with dementia should be forced to adopt an ‘out of sight out of mind’ position in society. This may be a reaction to the stigma and discrimination that people with dementia can experience.
These postulates, and societal attitudes towards illness, were vividly captured in the films such as Doctor in the House and Carry on Doctor.
The patient, in gown or pyjamas (thereby identifying and labelling them as ill), listened anxiously to the dispassionate words of the august surgeon who kindly attended their bedside, desperate for any clue as to when he or she might be released from hospital back into ‘normal’ society.
Dr Kate Granger (@KateGranger) recently described the powerful effect of pyjamas here.
I think all drs should be made to lie in a hospital bed wearing PJs & be stood over. See what it feels like. #vulnerability #powerbalance
— Kate Granger (@GrangerKate) February 26, 2014
Dementia is not on the whole ’caused’ by a ‘bad lifestyle’ – many individuals with dementia have had a strong genetic component of sorts. However, changes in the environment can be helpful for a long term condition such as dementia.
Marked environmental change for a person with dementia can of course be extremely unsettling, causing both physical and mental distress. However, appropriate signage in the environments, attractive design of homes and wards, and supportive built environments, can all, for example, improve wellbeing in dementia.
The medical profession has accordingly had to adapt to the demise of the traditional sick role. We no longer expect the subservient patient to submit to our bedside capture.
Subjecting persons with dementia to a whole variety of drugs that do not work that well for many, such as potentially anti-depressants, anti-psychotics or anti-memory loss is a subtle attempt at medicalisation capture, but is indeed living on borrowed time as other professions take over where the medics have failed.
Whole person or integrated care will do a lot here to help.
Assistive technology and internet technologies can in combination encourage independence as well as participation with wider social networks, but criticially may now bee at the convenience of persons in coming with health and illness services, rather than the convenience of the service.
Kate Swaffer advises other people with dementia that they should consider empowerment perhaps through groups who genuinely care.
I’m of course proud that the Scottish Dementia Working Group is serious about it. The European Dementia Working Group is serious about it. The Alzheimer’s Australia Dementia Advisory Committee is also serious about.
People with dementia make up the membership of these groups. And please don’t forget the Dementia Alliance International group, plus Kate’s page here which also highlights how to help with their important fundraising initiatives at a practical level.
Does electronic surveillance of persons with dementia conflict with personhood?
Families, friends, and carers of people with dementia may be faced at some time with the problem of what to do if the person begins to wander. Wandering is quite common amongst people with dementia, and can be very worrying for those concerned for their safety and living well. The problem of wandering in dementia is not trivial. It causes stress to carers, referrals to psychiatric services and hospital admissions, problems in the hospital environment, and an unknown number of deaths.
The last Labour government developed a reputation for being authoritarian in the domain of civil liberties, reaching a peak, arguably, with its legislation for terrorists for detention without trial. Governments of all shades have at some point or other wished to stamp their liberal or libertarian credentials, and indeed in relation to the free market. For example, an outsourcing company within the lifetime of this government got into trouble over allegations to do with prisoner tagging.
Different companies have been pitching their products – tiny cameras, wearable sensors, connectivity services – mainly at the US and other rich countries where abductions and violent crime are mercifully rare. Google recently, to much media attention, launched with great fanfare its ‘Google glasses’. Indeed, a Scottish friend of mine recently logged onto her Facebook in Bilbao in Spain, and Facebook cunningly producing a sponsored advert for a hotel in Bilboa. When you make a tweet, you have an option of activating the ‘location detector’ of your tweet. This article is not about terrorism or the use of smart apps to book hotels, but the point is merely that a plethora of converging evidence might suggest that a technology explosion may be going hand in hand with a surveillance culture, and it is perhaps no big surprise that this is also having an effect on dementia care.
I asked Alex Andreou, who has written with remarkable authority and passion about his own mother living with dementia in the Guardian newspaper, what he thought of the general issue of electronic surveillance of persons with dementia?
“I would welcome it. Terrifying when I see reports about people lost.”
When I reassured Alex that I would not mention this name, Alex said, “I don’t mind if you do.”
Sussex Police has been trialling the scheme at a cost of £400 a month, and hopes it will save the force thousands of pounds by avoiding call-outs which can take up a lot of police officers’ time and can involve the use of search helicopters. A number of local authorities are already using similar devices to track sufferers, but this is believed to be the first time a police force has taken on such a scheme in May 2013. If the trial is successful, there are ambitions to roll it out across the county to a much larger population. The idea is that people with dementia can wear the tracking device around their neck, clipped to a belt or on a set of house keys. It works through a Global Positioning System (GPS) – a space-based satellite navigation system that is used by ‘sat-navs’ in vehicles. It is linked to a 24/7 response service which the wearer can call at a press of a button. The device is called “MindMe”, and family and friends can log into the system whenever they like to find out where the person is.
It is claimed that the Police regularly have to search for missing people with dementia, and that it is genuinely heartbreaking to see the torment that their families are put through and to see the impact it has on the person with dementia when they are found. A £15 (€18; $23) pair of transmitters would, for example, sound an alarm if the person gets separated. GPS trackers not intended as a general panacea, but they do mean that patients can be found more quickly. This is thought to be useful for several reasons. Firstly, rapid recovery reduces risk. Typically, carers delay calling for help, wanting to avoid involving the police if possible. Half of all people with dementia who are missing for more than 24 hours can die or become seriously injured. However, 40% of those with dementia get lost at some point, and about 5% get lost repeatedly. It is this 5% who are the most obvious candidates for a tracker. The first episode of getting lost is usually not predicted, and is often followed by restrictions on freedom and increased observation, reducing the perceived need for a device.
On November 11th 2013, Norman McNamara, a campaigner for awareness of the dementias himself who himself is living with a dementia, announced that, that Ostrich Care would be making available free GPS trackers to all persons who are diagnosed with dementia, and to registered carers (in the UK, not uniquely to the Torbay area.) A monthly ‘maintenance fee’ still has been made though. The info from Ostrich Care is here (ht: Jane Moore).
But in reality there is no right answer. The situation is complex. Decisions about limiting a person’s liberty should remain a matter of ethical concern even when technology finally makes the practical management of wandering easier. This approach has as its backdrop evolving body of work on technology and dementia, known as “assistive technology”, where collaboration and engagement with “users” has been a guiding principle. The earlier literature on electronic surveillance monitoring pointed out that the technique could be associated with objectification, infantilisation, and disempowerment, which are negative phenomena. The acceptability of surveillance monitoring has generally been researched among formal and informal carers only, with the views of those living with dementia curiously under-represented.
The whole issue can raise strong emotions. Dot Gibson, general secretary of the National Pensioners Convention, has been reported as feeling that the Sussex Police scheme is “inhumane”, “barbaric” and flouts fundamental human rights. This criticism has been bundled with a general criticism of the care system, with Gibson adding, “This is trying to solve a human problem with technology”.
According to Gibson:
“Using electronic tags on dementia sufferers raises very important issues about the individual’s human rights. They haven’t committed any crime – they’ve just grown old. This is just about saving money rather than treating people with dignity. Rather than tagging people we need better social care out in the community. Dementia patients need human interaction not tagging.”
In terms of medical ethics, “autonomy” relates to self governance or personal control. One of the main aims of implementing these surveillance monitoring devices is the promotion of increased independence. Most carers, whether relatives or paid staff, want the best for the person they support. Alongside doctors’ duties of beneficence, non-maleficence, and justice, respect for patient autonomy is invoked as a cardinal principle. The legal courts in various jurisdictions have confirmed the principle of respect for patient autonomy in the language of rights of self-determination. This is not merely viewed as a a rejection of a paternalistic tradition of ‘doctor knows best’, but includes differing philosophical positions including those of Kant.
There are a number of possible reasons why a person with dementia might wander, and this is related to which parts of the mind or brain are affected at any particular time. Here is yet another example where it is unhelpful to think of ‘dementia’ as one big homogeneous group. There are hundreds of different causes of dementia, and this might impact on why a person with dementia wanders. However, any patient living with dementia can of course become acutely confused, just like any other person (particularly in the elderly age group due to some underlying infection, for example.) Various important causes include a changed environment, excess energy, searching for the past, expressions of boredom, where it might be difficult to establish an underlying ‘medical cause’.
Dementia of the Alzheimer type is the most common type of dementia worldwide. Memory problems are the hallmark of dementia of Alzheimer type. Indeed, wandering may be due to a loss of short-tem memory. A person may set off to go to the shop or a friend’s house, and then forget where they were going or why. Or they forget that their partner has told them that they were going out for a while and set off in search of them. In another type of dementia known as Lewy Body dementia, visual hallucinations can occur: in other words, seeing things which aren’t there. An inability to distinguish hallucinations from reality may cause the person to respond to something that they dreamed, thinking that this has happened in real life. Lewy Body dementia tends to affect the younger age group (by younger, I mean below the age of 60).
In advanced dementia, whatever the cause of dementia, people can lose their regular ‘body clock’ or circadian rhythm. People with dementia may suffer from insomnia, or wake in the early hours and become disoriented. They may think it is daytime and decide to go for a walk. Poor eyesight or hearing loss may mean shadows or night sounds become confusing and distressing. Also, in advanced dementia, walking may actually ease discomfort, so it is important to find out if there is any physical problem or medical condition and try to deal with it. Tight clothing, excessive heat or needing to find a toilet can all cause problems. Also, changes that have occurred in the brain may cause a feeling of restlessness and anxiety. Agitation can cause some people to pace up and down or to wander off with no apparent purpose. They may fail to recognise their own home, and insist on leaving.
Some caregivers appear to like the idea of electronic tracking devices if these can ensure that the wanderer is found more swiftly. Some argue that for, the sake of safety, a slight loss of liberty might be a price worth paying. In the case of someone with moderate to severe dementia who wanders, electronic surveillance monitoring arguably satisfies an ethical principle and decreases stigma. Being lost and half dressed in the middle of the night near a dual carriageway to any reasonable unlooker is hugely stigmatising, and electronic surveillance monitoring could avoid this. However, there is a concern that wandering as a behaviour of the dementias, like many aspects, is generally becoming overly medicalised, or turned into a medical problem. The inevitability of this is to turn it into a medical problem in need of a medical solution. This in turn potentially legitimates social control efforts in the name of ‘protecting’ wanderers.
Social control through the medical gaze encourages an environment of pharmacological surveillance and physical confinement. We all know of the dangers of the approach of the “chemical cosh”. Neuroleptic drugs have harmful side effects and show only modest efficacy in managing some behavioural problems in dementia. Physical restraints, such as safety belts and bedrails, are used in nursing homes all over the world, with a prevalence somewhere averaging around 50%. There is growing awareness that the use of these means can have significant psychological and physical disadvantages, such as increased cognitive decline and decreased mobility and has even led to death in some cases. Therefore, it is argued legitimately that the use of physical restraints should be diminished. Counsel and Care’s famous publication ‘The Right to Take Risks’ (1993) lists at least twenty forms of restraint commonly used at present, ranging from literally tying someone down to the use of sedatives, locks, glass panels in doors, threats and poverty. Despite the negative press associated with electronic surveillance monitoring devices in some quarters then, this new technology, developed and perfected as a result of its uses in prisoner tagging, may offer somehope of a more humane solution to a difficult problem. Here, language is crucial, as “surveillance monitoring” is a preferable term to “tagging”, as it is completely objectionable to use language for people with dementia normally reserved for criminals. You cannot be ‘convicted’ of having a diagnosis of dementia. Whilst some ideologically might feel nervous of a somewhat libertarian-facing solution, the risks and restrictions of alternatives to surveillance monitoring, should perhaps be borne in mind.
Over the last decade, a new ethos in the management of wandering has evolved with a move towards promotion of safe walking, rather than the prevention of wandering, in order to balance a person with dementia’s need for autonomy with the need to minimise risk. Other non-pharmacological approaches include: behavioural approaches; carer interventions; exercise; music therapy; sensory therapies (aromatherapy, multi-sensory environment); environmental designs and subjective barriers (visual modifications that may be interpreted as a barrier but are not physically so). Evidence on the effectiveness and acceptability of the above interventions is limited. The availability of all alternatives will frequently depend on resources, attitudes and policies of health professionals, institutions and governments, and the precise legislative and regulatory framework. For example, in the Netherlands, the Health Care Inspectorate promotes the use of surveillance technology as a way to diminish the use of more severe means of restricting freedom. In 2009, already 91% of the nursing homes were using some kind of surveillance technology in the care for people with dementia. In most developed countries, the legislation regarding the use of physical restraints is based on, among other things, guidelines of the United Nations and the World Health Organization and the European Convention on Human Rights (Council of Europe, 1950; General Assembly of the United Nations, 1948; World Health Organization, 2005).
Although surveillance monitoring might increase liberty in some senses, it has the potential to decrease autonomy and tracking devices might settle the anxieties of others without attending to the needs of the person with dementia. There are considerations from medical law and medical ethics too on the place of the family. Where the adult patient is unable to consent, both medical ethics and law allow for consultation with relatives. Indeed, consultation with the family is the default position in cases of adult patient incompetence. The general tradition of ethics can be denoted through primary concern with individuals; in fact, medicine’s traditions have a tendency to be individualistic. It could be that ‘taking friends and families seriously’ challenges that individualistic approach. For illustration, the doctor-patient relationship is structured in a manner similar to a contract between two individuals, and the doctor has a duty to the person/patient. Contrary to individualist perceptions of autonomy, “communitarians” acknowledge the significance of the person’s relations. This is of course particularly relevant if one wishes to pursue in English policy and elsewhere the notion of “dementia friendly communities”. If it can be mooted that liberals focus on what separates people from one another, communitarians see persons as fundamentally attached to each other. For such an approach to work, those advising concerned relatives need to be trained in not only dementia care but also in understanding and negotiating the different ethical perspectives of carers and professionals.
This is important so that professionals do not seem to be assume some high moral ground of civil libertarianism, as well as to allow recognition that our autonomy is exercised in the embrace of others. So in my opinion the use of surveillance technology, as either an infringement of human rights or as contrary to human dignity, as it reduces or infringes privacy and removes personhood, is only a small part of the issue. There is a danger that resorting to technology in general might result in a reduction in the essential human contact between caregivers and residents and could lead to a further decrease in staff in long-term care facilities. However, if this is a known risk, this can be mitigated against, and adoption of electronic surveillance monitoring might led to the evolution of a more secure environment (thereby reducing caregiver stress), but also increase liberty and dignity when compared with forms of physical restraint. The ‘threat to personhood’ is an important consideration, and the law itself regarding mental capacity as currently drafted in the English jurisdiction could indeed be too a blunt weapon. However, policy in general has been driving to empowering persons with dementia to have more choice and control than previously, and this policy driver is not at all insignificant.