Home » Search results for 'care.data'
Search Results for: care.data
Can you steal Big Data for dementia research like a Big Mango?
A ‘Big Mango’ has just gone missing, but will people notice if Big Data suddenly goes missing for the purposes of research into dementia?
A large ceramic mango is of course tangible property, whereas the information itself of ‘Big Data’ isn’t. But the recent furore over ‘caredata’ has illustrated how meticulously careful if you have to be about consent.
Twitter is amazing.
During infectious disease outbreaks, data collected through health institutions and official reporting structures may not be available for weeks, hindering early epidemiologic assessment.
In contrast, data from informal media are typically available in near real-time and could provide earlier estimates of epidemic dynamics. Many people for ‘breaking news’ nowadays prefer to do a Twitter search than wait for a news bulletin.
Rumi Chanara and colleagues (Chanara et al., 2012) assessed correlation of volume of cholera-related HealthMap news media reports, Twitter postings, and government cholera cases reported in the first 100 days of the 2010 Haitian cholera outbreak.
Trends in volume of informal sources significantly correlated in time with official case data and was available up to 2 weeks earlier. They found that informal data can be used complementarily with official data in an outbreak setting to get timely estimates of disease dynamics.
The English law does pride itself, however, on some sort of law on the protection of information (hence the enactment of the Data Protection Act 1998).
Long before that, Oxford v Moss (1979) 68 Cr App Rep 183 was an English criminal law case, dealing with theft, intangible property and information. The court ruled that information could not be deemed to be intangible property and therefore was incapable of being stolen within the Theft Act 1968.
The defendant, Moss, was a University student and managed to obtain a proof copy of his forthcoming exam paper. It was accepted that he always intended to return the proof itself, and therefore could not be convicted of theft of the proof itself, however he was charged with stealing information belonging to the Senate of the University.
How confidential medical data are dealt with has been cause for a broohaha recently.
Informed consent is an ‘opt-in‘ model:people have to sign up to donate organs. In this model, donors must also be made aware of what they are signing up for and have the option of withdrawing their consent at any point.
Informed consent contrasts with presumed consent (used in association with organ donation, the assumption that an individual is happy to donate organs after death unless he or she has explicitly said that they do not wish to).
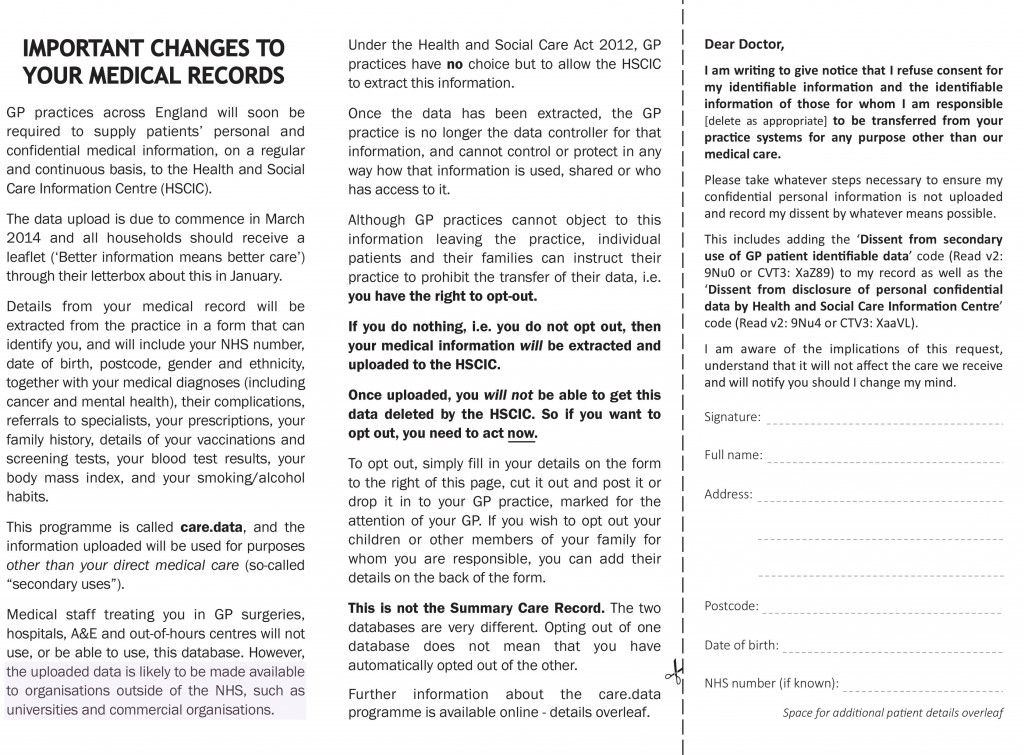
At the beginning of February 2014, it was reported that the Information Commissioner’s Office had been concerned that the information provided to patients on care.data is not clear enough about how to opt out of the programme.
According to Prof Brian Jarman, an expert statistician whose interests data and public health, the arrangements concerning ‘caredata’ do not sound like informed consent.
“The Data Protection Act (DPA) usually requires organisations by default to offer opt-in. Yet for the confidential care.data opt-out is the only option. This suggests a lack of informed consent. The leaflet sent to people in their junk mail gives little information about the drawbacks. To have informed consent patients need to be told of the risks as well as the benefits.”
This was a bit of a public grab, but possibly competing in publicity with the latest finding that thieves have just made off with a 10 metre high, 10 tonne mango replica from a town in northern Queensland, Australia.
A crane was used to rip the three-storey giant fruit from the concrete platform on which it had stood since 2002.
Just as people are now vigilant about the theft of giant mangos, the theft of Big Data has come under justifiable scrutiny.
Already there has been the massive plastic card data theft in South Korea, affecting about 60 million cards; the Target Corp. credit card disaster involving up to 40 million customers; the hacking of 16 million German e-mail accounts; data securitybreaches at Nieman Marcus Inc. and Easton-Bell Sports Inc.; and a group of Russian hackers who compromised the computer systems of Western energy and defense companies, governments, and academic institutions.
Cybercriminals, of course, abuse less obvious vulnerabilities, such as those in site-building software. In these cases, they often buy malware rather than develop it themselves.A specialised field, the grab of Big Data has particular relevance to people worried about hackers of a giant database of NHS clinical data.
So are Big Data important? An article in Wired Magazine “The End of Theory: The Data Deluge Makes the Scientific Method Obsolete ” cited provocatively that, “All models are wrong, but some are useful.”
So proclaimed statistician George Box 30 years ag.
In this article, it was stated that the scientific method is built around testable hypotheses but some of the models have not actually been that good, in comparison with real data.
Mendel and Newton are cited.
According to McKinseys, the amount of data in our world has been exploding, and analyzing large data sets—so-called big data—”will become a key basis of competition, underpinning new waves of productivity growth, innovation, and consumer surplus”.
In October 2012, it was reported that Massachusetts General Hospital would receive $5.4 million from the nonprofit Cure Alzheimer’s Fund, in what the fund said was the largest single private scientific grant ever invested in Alzheimer’s whole-genome sequencing.
The Alzheimer’s Genome Project would obtain complete genomic sequences of more than 1,500 patients in families that have Alzheimer’s, and will include over 100 brain samples. The genomes of family members with Alzheimer’s will be compared to those members who have been spared the disease to identify sites in the genome that influence risk for Alzheimer’s.
And it does seem as if people are generally moving with the times,.
In January 2014, for the “Nuffield Council on Bioethics: The linking and use of biological and health data” a response by the Wellcome Trust from January 2014 provided a number of interesting points.
“The linking and use of biological and health data is central to a wide range of biomedical research. There is a strong need to ensure a legal and regulatory environment in which these data can be used and linked for the purposes of research that aims towards improving health.”
However, the following was also noted.
“There are legitimate ethical concerns about the privacy implications of the use and linking of such data and future developments in using these data cannot necessarily be anticipated. Participants’ wishes are paramount, and there is a need for strong governance mechanisms for the use of participant data in research that can appropriately protect participant confidentiality.”
Google Health had to give up, however, with their initiative:
“Now, with a few years of experience, we’ve observed that Google Health is not having the broad impact that we hoped it would. There has been adoption among certain groups of users like tech-savvy patients and their caregivers, and more recently fitness and wellness enthusiasts. But we haven’t found a way to translate that limited usage into widespread adoption in the daily health routines of millions of people.”
Of course the grab of a giant mango can only put down to a publicity stunt; sharing of data for the public good in no way constitutes theft if done with the informed consent of people involved, although regulators have ingenious ways of making certain things permissible as they wish.
Stealing a giant mango is hardly likely to be legislated for in the near future, however.
On international collaborative data sharing and dementia. Surely “it’s good to talk”?
Plans to harvest private data from patients’ NHS files are causing a ‘crisis of public confidence’, the Royal College of GPs said this week. The professional body said it was ‘very worried’ that the public had not been properly informed about the scheme, which is due to begin this spring. Conversely, NHS managers and public health experts say the data will be used for important research and to show up poor care – and that all the data will be made anonymous. But other experts, in information security, say patients will be identifiable from their data – which will be passed on to private companies including insurance firms, and the professional regulatory code for ethics puts valid informed consent as of prime importance. A growing number of GPs oppose the care.data scheme, and say their patients will refuse to give them information for fear it will be harvested.
In the actual Communiqué from the G8 dementia Conference, the drive of sharing of “Big Data” was formally acknowledged. In the actual webinar, there was in fact screening of a session by corporate investors on the need to minimise risk from their investments to have the regulatory framework in place to avoid concerns over international data sharing.
Indeed, BT have taken active interest in dementia.
This eye catching headline is from the BT website: :
:
This report cites that, “the goal of finding a treatment to cure or halt dementia by 2025 is “within our grasp”, Prime Minister David Cameron has said, as he announced a doubling in UK funding for research into the disease.”
“The London conference is expected to agree to a package of measures on international information-sharing and collaboration in research. ”
These concerns include data privacy and security, and curiously do not feature above.
But the report does not even mention BT’s own Paul Litchfield, who presented even in the G8 Summit.
Last year, leaders from MedRed and BT were invited by the White House Office of Science and Technology Policy to unveil their new collaboration, the MedRed BT Health Cloud (MBHC), at “Data to Knowledge to Action: Building New Partnerships,” an event held at the Ronald Reagan Building 1300 Pennsylvania Ave NW in Washington, DC, on November 12, 2013.
MBHC is a multiyear, transatlantic effort to make available one of the largest open health data repositories in the world. It has been recognized by the Obama Administration as a high-impact collaboration that supports the Big Data Research and Development Initiative.
Designed to meet the converging needs of the life sciences and healthcare industries, the MedRed BT Health Cloud seeks to enhance integration of U.S. public data sets, such as adverse event reporting data from the U.S. Food and Drug Administration and recently released Medicare data from the Centers for Medicare and Medicaid Services, with data from the UK’s NHS and ‘other healthcare systems’.
Data currently available through the system includes several years of deidentified population health data from England, Scotland and Wales, as well as hundreds of other U.K. and data sources. It features data such as physician encounters, acute care interventions, pharmacy history, and health outcomes data.
It is argued that integration of this data with U.S. data and the addition of advanced analytics hold great potential to help speed the development of products and practices that will advance healthcare and improve the health and well-being of people around the world.
The drive for collaboration in data sharing to find a cure for dementia, most agree, is a worthy policy concern, but so is the current lack of openness in clinical data sharing which has brought about an overwhelming feeling of avoidable mistrust in the public.
The ultimate goal is the use of genomic DNA information for the development of personalised medicine.
A study testing all the DNA in the genome of cancer cells, the first of its kind reported on 7 Februrdy 2014, has identified individuals that may benefit from new treatments currently being tested in clinical trials.
Metastatic cancer – cancer that has spread from the region of the body where it first started, to other areas – is generally regarded as being incurable. In 2013, 39,620 women died from metastatic breast cancer in the US.
Progress in developing effective new chemotherapy or hormonal therapies for metastatic cancer has been slow, though there have been developments in therapies targeting specific genetic mutations in breast cancer.
We’ve all been shown Facebook adverts containing highly focused suggestions for purchases known on our known habits.
McKinseys have high hopes for the future of Big Data, indeed.
“Patients are identified to enroll in clinical trials based on more sources—for example, social media—than doctors’ visits. Furthermore, the criteria for including patients in a trial could take significantly more factors (for instance, genetic information) into account to target specific populations, thereby enabling trials that are smaller, shorter, less expensive, and more powerful.”
Of course, widespread internet access is an essential part of this technological revolution.
As regards BT, data sharing and dementia, surely it’s “good to talk” with the public who are, after all, central stakeholders?
Somebody had better tell Sid.
Should we more worried about a Trust in deficit or a deficit in trust?
“You can cut all the flowers but you cannot keep Spring from coming.”
? Pablo Neruda
For all the witch Hunts for looking for someone or something to blame, the number of constructive solutions has been unimpressive.
Some might say some of the media are part of the problem, not the solution, an anonymous friend said. But there are clearly ‘debates to be had’ about the news stories about the NHS which emerge into our popular press in short bursts.
Twitter trolls are people who land from nowhere, insult you and then disappear. They are the internet version of a random person sitting next to you on a crowded London bus, punching you in the face, and then getting off at the next stop.
And that’s the way we’re engaged in a debate about the NHS.
The French curiously have an opposite in their language to the word ‘inevitability’. It is called ‘evitability’. Part of the reason, I feel, that people feel so depressed is that they do not feel that they have actual control over the NHS policy in England from all the mainstream political parties.
Healthcare is expensive, but the NHS, when compared by percentage of GDP spent on health with countries with similar outcomes, is very good value for money. And yet it turns out that almost one in three NHS trusts in England is now forecasting they will end the financial year overspent, official figures show.
The term “self-fulfilling prophecy” was coined in 1948 by Robert Merton to describe “a false definition of the situation evoking a new behavior which makes the originally false conception come true”. He illustrated the concept with a run on a bank (a fictitious “parable”); his main application was to racial discrimination. The term has since entered social science and even everyday English, a rare feat for a sociological neologism.
So we are told that more NHS organisations are now in difficulty, compared with the same point last year. So what are we going to do about it?
There is no alternative (shortened as TINA) was a slogan often used by the Conservative British Prime Minister Margaret Thatcher. In economics, politics, and political economy, it has come to mean that “there is no alternative” to economic liberalism—that free markets, free trade, and capitalist globalisation are the best or the only way for modern societies to develop. The phrase may be traced to its emphatic use by the nineteenth-century classical liberal thinker Herbert Spencer.
But this lack of control, partly due to the quite manipulative way the debate tends to be framed by ‘influential’ thinktanks and media outlets, can lead to general dysphoria, perhaps apathy or depression. This is clearly relevant if members of the chattering political classes wish to seek out reasons why many potential voters feel disenfranchised.
A similar phenomenon is now happening with gusto, regarding NHS policy. That’s because we’re not offered any solutions, and feel powerless in controlling events.
Services have also been told to put aside £15bn in efficiency savings by 2015, in order to cushion themselves against further rises in demand.
This is clearly relevant to the ability of the NHS to hire new nurses. Many organisations are spending heavily on agency staff, with a 60 per cent rise in the total bill for locum doctors in the past three years, with doctors being paid up to £1,500 a shift.
Many of the worst problems are in London, where Barts Health NHS trust is predicting a deficit of £50m by the end of the financial year, and has drawn up plans to reduce the numbers of nursing staff on the wards.
Although the NHS has been protected from savings cuts, the demands from an ageing population and increasing costs of drugs mean services are struggling to meet demands on them, according to some ‘experts’.
The idea “reform is inevitable due to the ageing population” is immediately harpooned by issues when you look at the small print. For example, the cost savings from expensive cholinesterase inhibitors used to treat the symptoms of Alzheimer’s Disease to modest effect might be better put to use in guiding persons with inexpensive interventions to promote living well with dementia.
Professor John Lister, a health expert at Coventry University, said: “There are going to be more hospitals running into trouble due to debt problems.
“Some of the debts are astronomical. Repayments would have been tough enough in normal times but the recession and the need to cut £20billion from NHS spending has been the straw that broke the camel’s back.”
It’s a bit hit-or-miss whether you get a full account of events from such news items. For example, many articles couch the staffing of the NHS as a luxury, completely ignoring the issue that there is a minimum safe level of staffing on wards, whether Jeremy Hunt wishes to legislate for this or not.
Controversial private finance initiative which allowed more than 20 hospitals to borrow at high interest rates to secure new buildings have left some struggling to pay off the expensive mortgages, repayments can be up to five times the building costs.
The assumption that an ageing population makes the NHS unsustainable is not completely backed up by evidence. Indeed, increased life expectancy can increase the economic contribution of individuals, and need not be accompanied by increased morbidity – a concept known as ‘compression of morbidity’.
But should we more worried about a Trust in deficit or a deficit in trust?
David Cameron also promised to safeguard the NHS, lead the greenest government ever, create a fairer and more equal society, clamp down on tax evasion and clean up politics…
Regarding ‘clause 118′ giving special powers for a firestorm of NHS reconfigurations, Grahame Morris, Labour MP for Easington, recently commented,
“If the clause is agreed, we can expect tensions to be further exacerbated, and it should serve as a warning to us that the lack of meaningful consultation in the trust special administrator process leaves a huge democratic deficit and a black hole in accountability. ”
By the time the Health and Social Care Bill passed into law, becoming an Act, on 20th March 2012, it had garnered almost universal condemnation, with unprecedented agreement between the medical Royal Colleges, the British Medical Association, the Royal College of Nursing, the Royal College of Midwives, and many others – not forgetting nearly 180,000 signatures on the ‘Drop the Bill’ Government e?petition (the second?most signed petition on the site).
With the new construct of ‘accountability’ in the NHS, including for example Health and Wellbeing Boards and HealthWatch, it is hard to see how competitive tendering decisions can be challenged effectively without recourse to the law courts.
And now the Information Commissioner’s Office is concerned that the information provided to patients on care.data is not clear enough about how to opt out of the programme. The fiasco over care.data was possibly avoidable if the information leaflet had not been so badly prepared, and NHS England had given the appearance of seeking informed consent from individuals in the general public.
I think a Trust in deficit and a deficit in trust are all part of the same problem – a rational debate about the NHS being completely misrepresented in the media such that things which could be avoided are presented as inevitable.
I will inevitably buy a new car, but the longer I drive my current one only delays the inevitable. But allowing a storm to flood my car could speed up my search for a new car. In this case, God’s inevitability overruled my delay.
Likewise, from Cornwall to London, to Cardiff, Leeds and Northumberland, is it true that local authorities across England and Wales have been ignoring the Environment Agency’s protests and waving through developments on flood-prone land?
Are we actually promoting the NHS ‘choice and control’ with the current caredata arrangements?
In the latest ‘Political Party’ podcast by Matt Forde, an audience member suggests to Stella Creasy MP that wearing a burkha is oppressive and should not be condoned in progressive politics. Stella argued the case that she can see little more progressive than allowing a person to wear what he or she wants.
The motives for why people might wish to ‘opt out’ are varied, but dominant amongst them is a general rejection of commercial companies profiteering about medical data without strict consent. This is not a flippant argument, and even Prof Brian Jarman has indicated to me that he prefers a ‘opt in’ system:
Patients are not fully informed about how their information will be used. For such confidential data they should have to opt in @legalaware
— BrianJarman (@Jarmann) January 28, 2014
If people are properly told the pros and cons they can decide if they want to accept the cons, for the sake of the pros @sib313 @legalaware
— BrianJarman (@Jarmann) January 27, 2014
There are potential benefits, but also risks and if the risks happen they’re irreversible. Hence it’s safer to have opt-in. @legalaware
— BrianJarman (@Jarmann) January 27, 2014
Opting out can be argued as not being overtly political, though – it is protecting your medical confidentiality. People may (also) have political reasons for doing this, but the choice is fundamentally one about your right to a private family life. The government (SoS) has accepted this, and that is why it is your NHS Constitution-al right to opt out – you don’t have to justify it and if you instruct your GP to do it for you, she must.
It’s argued fairly reliably that section 251 of the NHS Act 2006 maps exactly onto Section 60 of the Health and Social Care Act 2001. Section 60 was implemented the following year under Statutory Instrument 2002/1438 The Health Service (Control of Patient Information) Regulations 2002. It is argued that the Health and Social Care Act 2012 did not modify or repeal those provisions of the HSC Act 2001 or the NHS Act 2006, nor did it modify or repeal any related provision of the Data Protection Act 1998. SI 2002/1438 remains in force. However, noteworthy incidents did occur under this prior legislation, see for example this:
Whatever motive you have for arguing against care.data, whether the whole principle of it, the HSCA removing any requirement for consent, the fact that it is identifiable data being uploaded from GP records (i.e. not anonymised or pseudonymised), or that the data will be made available, under section 251, for both research and non-research purposes, to organisations outside of the NHS, etc, the matter remains that the is no control over your data unless you opt-out.
Proponents of the ‘opt out’ therefore propose their two lines of action: either prevent your identifiable data being uploaded (9Nu0) and so effect a block on the release of linked anonymised or pseudonymised (potentially identifiable) data, which otherwise you cannot prevent or control; or block all section 251 releases (9Nu4), whether or not you apply the 9Nu0 code.
The point is, they argue, that you – the patient – cannot pick and choose, when, to whom, or for what purposes your data will be released. You cannot prohibit your data from being released for purposes other than research, or to organisations out with the NHS. This is completely at odds to the ‘choice and control’ agenda so massively advanced in the rest of the NHS. While it has been argued that the arguments against commercial exploitation of these data should have been made clearer beforehand, it’s possibly a case ‘I know we’re going there, but I wouldn’t start from here.’
Compelling arguments have been presented for the collection of population data. It’s argued wee need population data to do prevention and to monitor equity of access and use. It’s an open secret that the current Government is continuing along the track of privatising the NHS; arguably making it all the more important to have good data so we know what is happening. Having more of this data at all starting in the private sector, under this line of argument, is much less transparent, as it’s hidden from freedom of information from the start.
It’s, however, been argued that “the route to data access” has in fact changed. Under Health and Social Care Act (2012), it was intended that either the Secretary of State (SoS) or NHS England (NHSE) could direct HSCIC to make a new database, and – if directed by SoS or NHSE – HSCIC can require GPs (or other care service providers) to upload the data they hold. care.data represents the single largest grab of GP-held patient data in the history of the NHS; the creation of a centralised repository of patient data that has until now (except in specific circumstances, for specific purposes) been under the data controllership of the people with the most direct and continuous trusted relationship with patients. Their GP.
HSCIC is an Executive Non Departmental Public Body (ENDPB) set up under HSCA 2012 in April 2013. NHS England, the re-named NHS Commissioning Board, was established on 1 October 2012 as an executive non-departmental public body under HSCA 2012. Therefore, to suggest that the government has ‘little control’ over these arm’s-length bodies is being somewhat flimsy in argument – they were both established and mandated to implement government strategy and re-structure the NHS. There are also problems with the “greater good” argument; being paternalistic, the opposition to caredata spread bears similarity to the successful opposition to ID cards. This argument presumes that patients will benefit individually, when – and it ignores the fact that it is neither necessary or proportionate –and may be unlawful under HRA/ECHR – to take a person’s most sensitive and private information without (a) asking their permission first, and (b) telling them what it will be used for, and by who. Nobody is above the law, critically.
The fact is that the data gathered may increment the data available to research but that in its current form, care.data may actually not be that useful – it includes no historical data, for starters. And all this of course ignores the fact that care.data (and the CES that is derived from linking it to HES, etc.) will be used for things other than research, by people and companies other than researchers. That is the linchpin of the criticism. Finally, the Care Bill 2013-14 – just about to leave Committee in the Commons – will amend Section 251, moving responsibility for confidentiality from a Minister (tweets by Ben Goldacre here and here).
Anyway, the implementation of this has been completely chaotic, as I described briefly here on this Socialist Health Association blog. What now happens is anyone’s guess.
The author should like to thank Prof Ross Anderson, Chair of Security Engineering at the Computer Laboratory of the University of Cambridge, Phil Booth and Dr Neil Bhatia for help with this article.
Sledgehammers and nuts: opt-outs and data sharing concerns for the NHS?
You couldn’t make it up.
“a substantial number of GPs are so uneasy about NHS England’s plans to share patient data that they intend to opt their own records out of the care.data scheme.”
“The survey of nearly 400 GP respondents conducted this week found the profession split over whether to support the care.data scheme, with 41% saying they intend to opt-out, 43% saying they would not opt-out and 16% undecided.”
Simon Enright, Director of Communications for NHS England, tweeted to indicate methodological issues with concluding too much from this ‘snapshot survey':
@legalaware disappointing that Pulse did self-selecting sample with potential question bias in survey.
— simonenright (@simonenright) January 26, 2014
And of course Simon Enright is right. But one has to wonder how much GPs themselves have been informed about the debate about data sharing concerns. GPs are trained to explore, and in fact examined on exploring, the ‘beliefs, concerns and expectations’ of their patients; so it would be unbelievable to assume that no one had had this particular conversation with a patient.
GPs tend to be a very knowledgeable and versatile group of medical professionals, and indeed many have an active interest in public health.
But here there’s been another problem at play? All of the patients who I know, because of the known issues in waiting for an appointment to see their GP for ‘routine matters’, have decided to opt-out by simply dropping in to sign a form with the receptionist. But that sample could even be more unreliable than the Pulse survey.
For all of the huge budget that’s set aside for NHS England’s interminable activities on patient engagement in the social media and beyond, you’d have thought a spend on explaining data sharing would’ve been money well spent?
Views on an individual’s right to ‘opt out’, described in a previous blogpost of mine, vary.
There are many good arguments for proposing the sharing of care data, but the lack of willingness of industry, primary care or public health to discuss openly how data sharing might be necessary and proportionate, under the legal doctrine of proportionality, is utterly bewildering.
What has resulted is an almighty mess.
In as much as there is a ‘root cause’ of this problem, an unwillingness to make the arguments for data sharing with the general public is a good candidate.
Julie Hotchkiss, a public health physician, has for example written to Tim Kelsey about the matter today.
Dear Mr Kelsey
re:Care.data
I think there is so much to be gained by collation of personal health data – for epidemiological observation (prevalence, time trends, variation), allowing data-linkage enjoyed by other countries such as Sweden, to aid commissioning of health services as well as, of course, for direct patient care. For all these reasons I support in principle the care.data initiative. However I have grave concerns about how the data might be used. I am aware that many, many people share these concerns, and many of these have been expressed in the press in recent weeks. Many of my colleagues (long term NHS employees) are saying they will opt out. There are a number of senior voices in the Public Health world who are urging people to opt out.
NHS England is in a unique place to be able to address these concerns – but in many ways the horse has bolted, and I fear we may never get it back in the stable. PLEASE now put your energies and resources into a full and frank consultation, including IT experts, medical colleges, academia and for goodness sake – the general public! The fact that no such awareness raising and consultation has taken place makes people suspicious. They already don’t blindly trust the NHS / government anymore. So if you want to get health professionals and academics behind you in order to have a greater number of voices advocating for care.data please address the following concerns – in a published document- as soon as possible.
- definitive ownership of the data
- responsibility for data quality
- assurance (ideally in legislation) that ownership or data management will remain with a governmental agency and not be out-sourced
- will the HSC IC own the data, and allow access through a form of brokerage (allowing specific views/queries) or access to the full data set)?
- detailed Information Governance arrangements, e.g. requirements for Section 251 approval?
- what Research Governance / Ethical approval arrangements are being put in place?
- what will organisations have to pay,? and if so is this a handling fee or will they get ownership of the data?
- criteria for granting access to data and legally binding restrictions on usage of the data
- exactly to what extent will records be identifiable (for instance the long-established practice at ONS of suppressing cells with fewer than 5 individuals from disclosure)
Although I expect a response, more than this I expect published documents to detail all these issues. I’m sure there are many other details specialists in health research, Information Governance, medico-legal matters and civil libertarians would require in order to be assured that this was something in which they could participate.
Kind regards
Julie Hotchkiss, Fellow of the Faculty of Public Health
Another question for Tim Kelsey may be, potentially, whether the data from care.data will be processed according to the National Statistics Code of Practice.
It is somewhat unclear why the public health community have not had themselves a discussion with the general public, despite some advocates of this community now complaining very loudly about the presentation of ideas leading to the ‘opt out campaign’.
But they will need to confront the stench of public mistrust aimed at various politicians. Examples of events leading to this profound distrust include the NSA/Snowden affair, and relevations at GCHQ.
The corporate capture in some areas of public health is not a topic which public health physicians have wished to talk about. However, these authors somehow managed to sneak an excellent discussion of the phenomenon here in the British Medical Journal.
There have been calls for much tighter regulation of “data brokers”, as corporates wish to rent-seek this plethora of data. What always appeared to have been lacking was an “intelligent debate” with the general public about data sharing. Nonetheless, the social media, for example “Open democracy: our NHS” websites, have for a very long time been publishing relevant articles on this subject.
There was also the small issue of how the £3bn implementation of the Health and Social Care Act (2012) came into being, which led to a turbo-boost of the outsourcing and privatisation of the NHS. Members of the academic public health community were slow on the uptake there too – some would say “completely asleep on the job”, perhaps not as far as their own research interests are concerned, but on the specific issue of potential violation of valid consent for individuals.
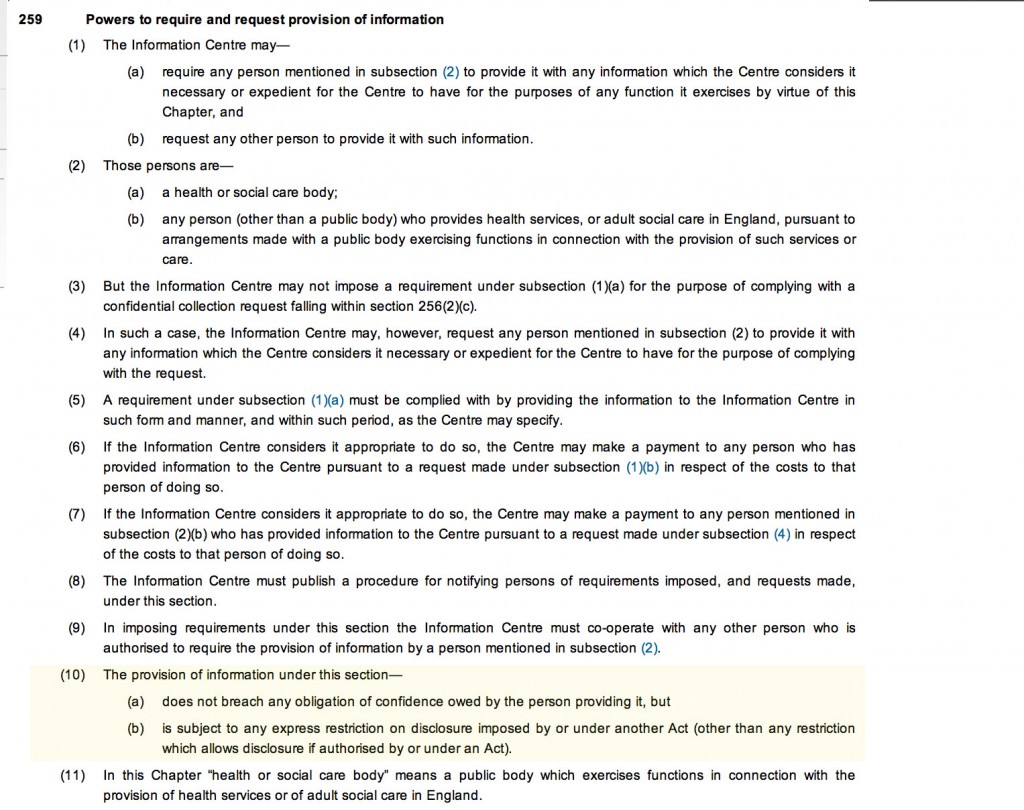
And guess what the Health and Social Care Act (2012) also contains a legal ‘booby trap’, which many did not see fit merited discussion with the general public.
Section 251 of the NHS Act 2006 (originally enacted under Section 60 of the Health and Social Care Act 2001), allows the common law duty of confidentiality to be set aside in specific circumstances where anonymised information is not sufficient and where patient consent is not practicable. For example a research study may require access to patient identifiable data to allow linkages between different datasets where the cohort is too large for consent.
This would require time limited access to identifiable information where gaining consent from a large retrospective cohort would not be feasible and would require more identifiable data than would be necessary for linkage purposes. However, section 10 of the Data Protection Act (1988) currently allows a right for an individual to prevent damage or distress by data processing.
This is indeed conveniently “triggered” by section 259(10) of the Health and Social Care Act (2010), i.e. “[the provision] is subject to any express restriction on disclosure imposed by or under another Act (other than any restriction which allows disclosure if authorised by or under an Act”:
The trust is further eroded through the loss of data from government agencies, coherently tabulated on this Wikipedia page.
Proponents of democratic socialism have long argued that citizens often are not able to buy influence through competing with large corporates, but can legitimately exert influence through the ballot box.
There is also no doubt that people are talking at cross-purposes. There is a bona fide case for disease registries and surveillance, for example. However, the problems of an individual’s data being shared with lack of informed valid consent in the name of population presumed consent do need to be addressed ethically at least.
Public health physicians who would like to see the law applied to promote public health and research overall cannot condone profiteering from personal data abuses. Tim Kelsey has always been adamant that the English law is strong enough to cope with such threats. The scenario has mooted before of private insurance companies being able to abort insurance contracts (rescission) from data disclosed to them, on the grounds of misrepresentation or non-disclosure, but the position of the NHS England has always been to present such scenarios as far-fetched.
However, the issues appear to have been intelligently debated at European level. The draft “EU General Data Protection Regulation on the protection of individuals with regard to the processing of personal data and on the free movement of such data” (the EU Regulation), was published in 25 January 2012, and has been debated in the European Parliament for most of the time since then.
Under “Albrecht’s proposals“, health data should generally only be able to be processed for the purposes of historical, statistical or scientific research where individuals have consented to such processing. It would be legitimate for processing in the context of research to take place without consent only where: (a) the research would serve an “exceptionally high public interest”; (b) the research involves anonymous data from which individuals could not be re-identified; and (c) the regulators have given their prior approval. Consent, however, is to follow the stricter interpretation, requiring explicit, freely given, specific and informed consent obtained through a statement or “clear affirmative action”. There is, however, legitimate concerns that these proposals might damage the interests of both corporate and public health communities.
It looks very much like chaos has set in since 2010 in running the NHS. Any party can do better than this.
This is of course an almighty mess, and it is hard to know how the whole thing could have been approached better. A plethora of issues have converged seemingly at once, and there is a possibility a ‘big opt out’ would still deliver a result without the matters having been properly discussed. If you think this is bad, consider what would happen in a national discussion of the terms of our membership of the European Union?
by @legalaware
Cameron’s #CostofNHSConfidentialityCrisis
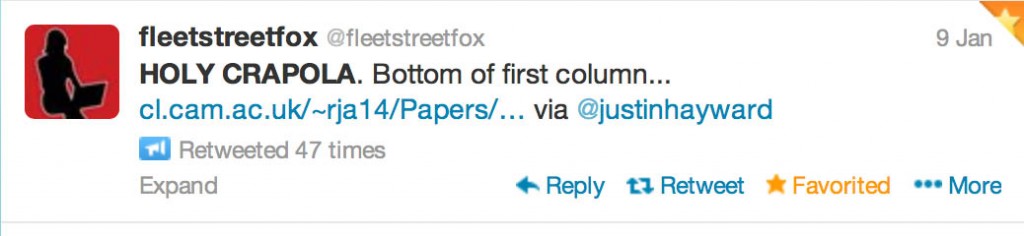
Thanks to @fleetstreetfox for tweeting this last night.
And THIS tweet refers to THAT sentence (see bottom of the first column):
You have just eight weeks to opt out of having your and your family’s confidential medical information uploaded from your GP’s systems, then passed on or sold to others – including private companies.
For more information, see www.medconfidential.org where you can download an opt out form, should you wish to opt out.
And please do pass these links on:
www.medconfidential.org/how-to-opt-out
for a copy of the form and a letter for you to use, if you prefer
www.care-data.info for detailed information on the care.data programme by the GP who wrote the content of the opt out form
for a direct link to a PDF of the form for use on Twitter, etc.
Keep safe.